Abstract
Kidney allotransplantation remains the preferred treatment for end-stage kidney disease, yet donor shortages limit its availability. Xenotransplantation using genetically modified porcine kidneys offers a promising alternative. Here, we report key physiological observations from the first-in-human porcine kidney xenograft over a 51 day postoperative follow-up period. The transplanted kidney maintained essential functions, including waste excretion, electrolyte regulation, and production of concentrated urine, while supporting blood pressure and sodium reabsorption despite reduced activation of the renin-angiotensin-aldosterone system. Sodium retention required diuretic therapy, and mild hypocalcemia and hyperphosphatemia occurred in the setting of pre-existing hypoparathyroidism. Markedly increased urinary uric acid excretion led to hypouricemia without evidence of urate nephropathy. This case demonstrates the ability of a porcine kidney to sustain vital metabolic functions in a living human, while highlighting areas for further research. These findings provide a foundation for optimizing post-transplant care and advancing xenotransplantation as a solution to the critical organ shortage.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) affects more than 35 million adults in the United States, with nearly 800,000 people experiencing kidney failure1. Kidney transplantation is the preferred treatment option for kidney failure, offering better survival and quality of life compared to dialysis2. However, the demand for donor kidneys far exceeds supply, leaving most patients reliant on dialysis. More than 70% of individuals with kidney failure do not receive a transplant3,4, and ~10% of those on the waiting list either die or are removed each year due to disease progression5.
Xenotransplantation, using genetically modified pig kidneys, offers a potential solution to the organ shortage crisis by providing an unlimited supply of transplantable organs6. Advances in genetic engineering have helped overcome key immune barriers and reduce the risk of thrombosis and viral transmission7,8,9. Preclinical studies in non-human primates have demonstrated the safety, efficacy, and durability of pig kidney xenografts7,10,11, and short-term experiments in the human decedent model have provided critical insights into their compatibility to humans12,13,14.
Building on these advances, the first pig-to-human kidney xenotransplantation in a living recipient was performed on March 16, 2024, at Massachusetts General Hospital15. This landmark procedure offered an unprecedented opportunity to evaluate porcine kidney function in a living human, free from the physiological limitations of short-lasting brain-dead models.
Here, we report key physiological observations from the first-in-human porcine kidney xenograft over a 51 day postoperative follow-up period, including glomerular filtration, electrolyte and water regulation, acid-base balance, calcium-phosphate homeostasis, uric acid and magnesium handling, and erythropoiesis. This first-in-human case provides critical insights into the metabolic capacity of a pig kidney in sustaining normal human renal physiology, helping to refine future xenotransplantation strategies and expand access to life-saving kidney transplants.
Results
Patient Characteristics
A 62 year-old man with end-stage kidney disease was selected for porcine kidney xenotransplantation after failing a previous kidney transplant and experiencing significant challenges with dialysis access. His medical history included hypertension, insulin-dependent type 2 diabetes, extensive vascular calcification, prior myocardial infarction, peripheral artery disease, and heart failure with preserved ejection fraction. He had also undergone parathyroidectomy for tertiary hyperparathyroidism, resulting in undetectable parathyroid hormone (PTH) levels. At the time of transplantation, he had no residual kidney function.
Blood chemistry analysis of genetically modified pigs
The baseline blood chemistry of Yucatan miniature pigs with the same genotype as the donor pig (ESUS-1784) was assessed to reinforce their suitability as organ donors for electrolyte and metabolic handling post-xenotransplantation (Supplemental Table 1). Compared to wild-type Yucatan pigs (N = 4), these genetically modified pigs (N = 4) exhibited no major differences in electrolyte levels with similar median levels of sodium [138 mmol/L, interquartile range (IQR) 136−140) vs. 137 mmol/L, IQR 135−137 in wild type], potassium (3.9 mmol/L, IQR 3.6-3.9 vs. 4.1 mmol/L, IQR 4.0-4.1 in wild type), chloride (100 mmol/L, IQR 99-102 vs. 98 mmol/L, IQR 97-98 in wild type), bicarbonate (27 mmol/L, IQR 26-28 vs. 26 mmol/L, IQR 25-28 in wild type) concentrations. However, genetically modified pigs had slightly lower baseline creatinine levels (median 0.7 mg/dL, IQR 0.6-0.7 vs 1.2 mg/dL, IQR 1.0-1.4 in wild type).
The genetically modified pigs also exhibited baseline sodium, potassium, magnesium, creatinine, and blood urea nitrogen levels comparable to human reference values, further suggesting the limited risk of metabolic mismatches following xenotransplantation. However, they exhibited a slightly higher bicarbonate concentration (median: 27 mmol/L, IQR 26-27; human mean: 24 mmol/L) and higher serum phosphorus levels (median: 6.2 mg/dL, IQR: 6.0-6.4; human mean: 3.5) relative to humans.
Glomerular Filtration Rate
The xenograft demonstrated early graft function, with a creatinine clearance (CrCl) of 43 mL/min/1.73 m² by post-operative day (POD) 3. Acute kidney injury due to cellular rejection on POD 8 led to a decline in CrCl to below 10 mL/min/1.73 m². Following treatment, kidney function recovered, reaching a CrCl of 64 mL/min/1.73 m² by POD 35 (Fig. 1A). Serum creatinine- and cystatin C-based estimated glomerular filtration rates (eGFR) remained stable after rejection resolution, averaging 44 ± 4 and 42 ± 3 ml/min/1.73 m2, respectively, with a minor decline after POD 48 (Fig. 1B). The mean difference between creatinine-based eGFR and cystain C-based eGFR was 4 ± 5. Trends in serum creatinine and cystatin C levels are shown in Supplemental Fig. 1.
A Trend of body surface area (BSA)-adjusted Cr clearance over time following xenotransplantation. B Trends in GFR, estimated by serum Cr (in green) and cystatin C (in blue), post-xenotransplantation. The acute kidney injury phase caused by rejection is highlighted with a red box. Source data are provided as a Source Data file. Abbreviations: Cr creatinine, GFR glomerular filtration rate, eGFR estimated glomerular filtration rate.
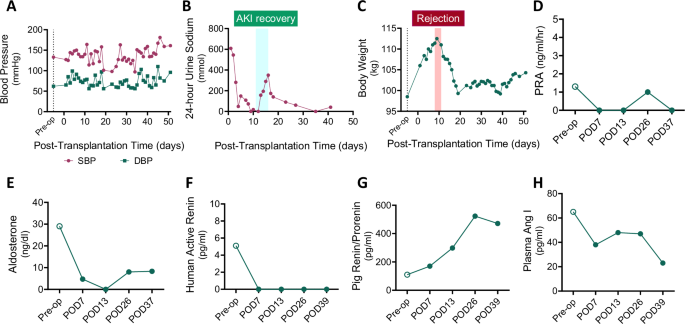
Hemodynamic Regulation and Sodium Handling
Hemodynamic stability was closely monitored due to concerns that porcine renin may have a limited capacity to activate the renin-angiotensin-aldosterone system (RAAS) in humans based on prior experiments in non-human primates16. Despite this, the recipient maintained blood pressure throughout the post-transplant period (Fig. 2A). The xenograft avidly retained sodium, as evidenced by low 24 h urine sodium excretion (mostly <100 mmol/day, except during recovery from acute kidney injury) and low fractional excretion of sodium (Fig. 2B and Supplemental Fig. 2). Signs of volume expansion emerged, indicated by increased body weight, presumably due to underlying heart failure, necessitating antihypertensive medications and diuretics (Fig. 2C). NT-proBNP level was elevated post-transplant (4,916 pg/mL on POD 42), consistent with persistent volume overload in the setting of pre-existing heart failure. The xenograft remained sodium avid despite the use of diuretics, and there was no evidence of transplant renal artery stenosis on repeated renal ultrasounds. A detailed record of anti-hypertensive and diuretic medications is available in Supplemental Table 2.
A Changes in systolic and diastolic blood pressure following xenotransplantation. B Twenty-four hour urine sodium excretion trend. C Fluctuations in body weight post-transplant. Levels of (D) PRA, (E) serum aldosterone, (F) plasma human active renin, (G) plasma pig-derived renin, and (H) plasma angiotensin I are depicted. EDTA plasma was obtained from the recipient before (Pre-Tx, open circle) and four different times after kidney xenotransplantation (closed circles). Values below the detectability limit are shown as 0 in the graphs. The acute kidney injury phase caused by rejection is highlighted with a red box and the recovery phase is marked with a light blue box. Source data are provided as a Source Data file. SBP, systolic blood pressure; DBP, diastolic blood pressure; PRA, plasma renin activity; POD, post-operative days.
Renin-Angiotensin-Aldosterone System
Plasma components of the RAAS were measured before and after xenotransplantation. Post-transplant, plasma renin activity (PRA) was suppressed, and serum aldosterone levels were reduced (Figs. 2D and 2E). Human plasma active renin was undetectable by enzyme-linked immunosorbent assay (ELISA) in the post-transplant period, in contrast to control samples from human kidney allograft recipients (control median: 7.1 pg/ml, interquartile range 1.4-17.0) (Fig. 2F). By contrast, porcine xenograft-derived renin increased markedly post-transplant (range: 170−523 pg/ml) (Fig. 2G). In the absence of detectable human active renin protein, plasma angiotensin I levels decreased post-transplantation as compared to pre-transplantation values (range: 23−48 pg/ml post-operatively vs. 65 pg/ml pre-operatively) (Fig. 2H). These findings suggest that blood pressure was maintained without RAAS activation in the absence of hypovolemia, and the sodium retention observed in the recipient was mediated by RAAS-independent mechanisms.
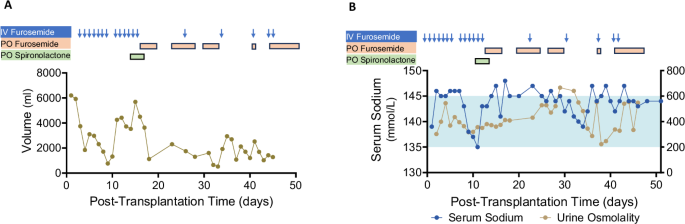
Water Handling
Given concerns about the potential incompatibility of human anti-diuretic hormone (ADH) with the porcine kidney vasopressin V2 receptors, urine output was closely monitored post-transplant. Of note, the patient had no residual kidney function from the native kidneys prior to transplantation. On POD 1, xenograft urine output was 6.2 L/day, gradually decreasing to 2.3 L/day by POD 7. In the setting of acute kidney injury due to rejection on POD 9, urine output declined to 0.8 L/day but recovered after treatment, remaining between 1.2–3.5 L/day thereafter (Fig. 3A).
A Urine output trends shown alongside diuretic administration history. B Serum sodium levels (blue) and urine osmolality (khaki) are shown. The timing of diuretic administrations is indicated by arrows and boxes. The light blue shaded area represents the normal serum sodium range. Source data are provided as a Source Data file.
Serum sodium levels were generally within the normal range but trended toward the high-normal end, with intermittent mild hypernatremia. This occurred in the context of ongoing loop diuretic use and limited fluid intake due to concerns about peripheral edema and elevated body weight (Fig. 3B). Urine osmolality ranged from 223−666 mOsm/kg water, suggesting preserved concentrating capacity of the xenograft and responsiveness to human ADH. However, transiently low urine osmolality with mild hypernatremia was observed between POD 36–39, resolving without intervention (Fig. 3B).
For a comprehensive assessment of xenograft water regulation and electrolyte balance, both electrolyte-free water clearance (CEFW) and solute-free water clearance (CH2O) were measured. The CEFW remained below 2 L/day, and CH2O was negative on most days (Supplemental Fig. 3). A summary of total fluid intake, including crystalloid and colloid administration, is available in Supplemental Table 3.
Acid-Base Balance
The recipient developed moderate metabolic alkalosis, evidenced by high venous pH (7.46-7.48) and elevated serum bicarbonate levels (33-39 mmol/L) in the absence of respiratory alkalosis (pCO2 52−59 mmHg) (Supplemental Fig. 4A). Persistent diuretic use for volume management, high-dose oral calcium carbonate, and pulse-dose intravenous corticosteroids—administered at transplant and during rejection treatment—likely contributed to this imbalance.
Urinary chloride concentration remained elevated ( > 20 mmol/L), while urine pH was low (5.5-6.0) (Supplemental Fig. 4B). In the setting of ongoing diuretics use, serum potassium levels were mostly within the normal range but remained in the low-normal range after POD 36, requiring daily potassium supplementation (Supplemental Fig. 4C). Urinary potassium excretion was elevated, with a urine potassium/creatinine ratio consistently > 18 mmol/g during this period.
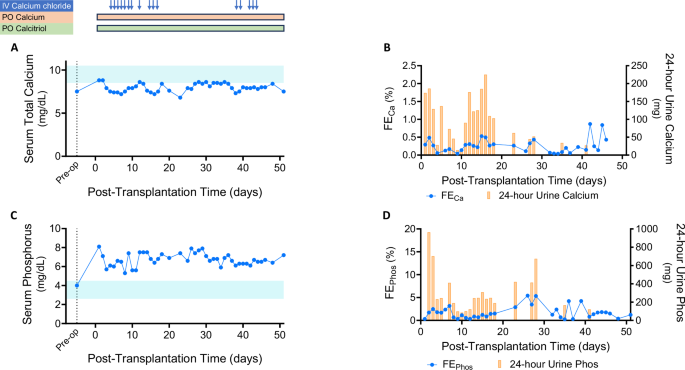
Calcium and Phosphate Balance
Serum calcium levels remained low (8.0 ± 0.5 mg/dL) due to the recipient’s post-parathyroidectomy hypoparathyroidism (Fig. 4A), while serum albumin levels were mostly normal. Fractional excretion of calcium remained below 0.5% and 24 hour urinary calcium excretion was consistently <150 mg, indicating preserved renal calcium-conserving capacity in response to hypocalcemia (Fig. 4B). The patient received intermittent intravenous calcium chloride while hospitalized and continued high-dose oral calcium carbonate and calcitriol therapy (Supplemental Table 4).
A Serum total calcium levels over time (light blue shaded area represents the normal range). The timing of calcium and calcitriol administrations is indicated by arrows and boxes. B Fractional excretion of calcium (blue line) and 24 hour urine calcium excretion (yellow bars) post-transplant. C Serum phosphorus trends (light blue shaded area represents the normal range). D Fractional excretion of phosphorus (blue line) and 24 hour urine phosphorus excretion (yellow bars). Source data are provided as a Source Data file. IV, intravenous; PO, by mouth; FECa, fractional excretion of calcium; FEPhos, fractional excretion of phosphorus.
Serum phosphate levels remained elevated (5.3-7.9 mg/dL) despite high-dose oral phosphate binders (Fig. 4C). Urinary phosphate excretion was limited, with fractional excretion of phosphate ranging from 0.3−4.2%. 24 hour urinary phosphate levels were generally below 600 mg, suggesting that his dietary phosphate intake was not excessive (Fig. 4D). This persisted despite elevated intact fibroblast growth factor 23 (FGF23) levels measured on POD 3, POD 18, and POD 26 (2659, 2449 and 3339 pg/mL, respectively). Intact PTH levels remained undetectable post-transplant. There was also no evidence of detectable PTH-related peptide (PTH-rP) during the follow-up period. Serum 25-OH Vitamin D levels were within the normal range, while 1,25 (OH)2-Vitamin D3 levels, initially low preoperatively, increased to 47 pg/mL with calcitriol supplementation. Collagen type 1b-telopeptide (collagen CTx) levels, a marker of bone resorption, were within the normal range before the transplantation but fell below the reference range post-transplant.
Uric Acid Balance
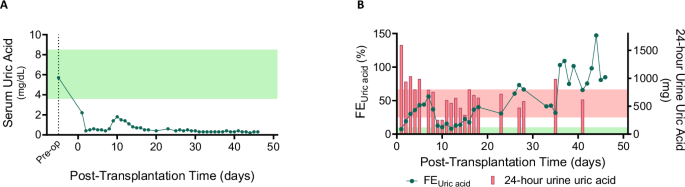
The recipient developed persistent hypouricemia (serum uric acid 0.3-0.7 mg/dL) due to increased urinary uric acid excretion (Fig. 5A). During the early post-transplant period, 24 hour urinary uric acid levels ranged from 0.9 to 1.6 g (Reference range 0.3–0.8 g/day), which later decreased as the recipient’s serum uric acid level reached a new steady state (Fig. 5B). The fractional excretion of uric acid remained elevated, ranging from 7% to 147% (reference range: 5−10%17). Uric acid crystals were intermittently observed on urine microscopy. However, there was no evidence of urate nephropathy on any of the three post-transplant xenograft biopsy samples.
A Serum uric acid levels post-xenotransplantation (light green shaded area represents the normal range). B Fractional excretion of uric acid (green line) and 24 hour urinary uric acid levels (red bars). The light green area represents the normal fractional excretion range, while the light red area represents the normal 24 hour urinary uric acid excretion range. Source data are provided as a Source Data file. FEUric acid, fractional excretion of uric acid.
Magnesium Balance
Serum magnesium levels remained in the low-normal range, requiring intermittent intravenous and daily oral magnesium supplementation (Supplemental Fig. 5A, Supplemental Table 5). Increased urinary magnesium loss was observed, with fractional excretion of magnesium ranging from 2−11% and 24 hour urinary magnesium excretion between 100−250 mg (Supplemental Fig. 5B). Among drugs that may contribute to urinary and gastrointestinal magnesium wasting, the recipient was exposed to tacrolimus, furosemide, and a proton pump inhibitor during this follow-up period. On POD 51, serum magnesium dropped to 1.0 mg/dL, prompting the administration of 2 g of intravenous magnesium sulfate in addition to ongoing oral magnesium gluconate (1000 mg/day).
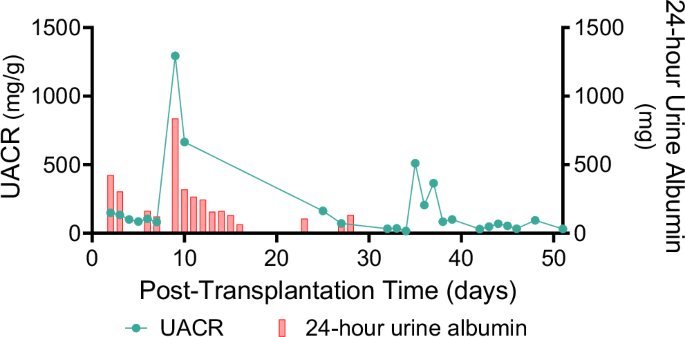
Glomerular Basement Membrane Integrity
In the early post-transplant period, albuminuria ranged from 0.1–0.4 g/day, increasing to 1.5 g/day on POD 9 during acute rejection. Following rejection treatment, urinary albumin loss was minimal, with a urine albumin-to-creatinine ratio (UACR) of 0.0–0.2 g/g (Fig. 6). Electron microscopy of the xenograft demonstrated intact glomerular basement membrane structure and interdigitating podocyte foot processes (Supplemental Fig. 6).
Erythropoiesis
The recipient developed normocytic normochromic anemia [hemoglobin 7.0-8.5 g/dL, mean corpuscular volume (MCV) 92.5–98.2 fL, mean corpuscular hemoglobin (MCH) 28.4−30.4 pg] post-transplant, likely due to surgical blood loss, repeated phlebotomy, procedural interventions, bone marrow suppression from immunosuppressants, and inflammation, including xenograft rejection. There was no evidence of iron, folate, or vitamin B12 deficiency nor signs of systemic thrombotic microangiopathy. Of note, pre-transplant hemoglobin levels ranged from 11.0-12.4 g/dL over 3 months.
A hypo-proliferative bone marrow response was suggested by a low reticulocyte index (0.2–1.7%). The recipient required three units of packed red blood cells during follow-up. He had not been receiving erythropoietin therapy before transplantation, and his plasma erythropoietin level increased from 3.6 mIU/mL preoperatively to 11.8 mIU/mL on POD 13. The potential cross-reactivity of the erythropoietin enzyme immunoassay (EIA) with pig erythropoietin had not been previously evaluated. Given concerns about the limited effectiveness of pig erythropoietin on human erythroid progenitors, darbepoetin (40 mcg weekly) was initiated on POD 15 after confirming iron repletion (transferrin saturation 83 % and ferritin 912 µg/L). Repeat erythropoietin level on POD 26 was slightly elevated at 13.4 mIU/mL. Despite treatment, the recipient remained mildly anemic throughout follow-up.
Discussion
This study provides the first comprehensive evaluation of a porcine kidney xenograft’s function in a living human, offering critical insights into its physiological performance. Over a 51 day follow-up, the xenograft sustained key renal functions, including waste clearance, electrolyte, volume, and blood pressure regulation. However, challenges such as sodium retention, metabolic alkalosis, hyperphosphatemia, and persistent anemia highlight areas requiring further studies. These findings represent a critical step toward optimizing xenotransplantation for broader clinical application.
Waste clearance is one of the pivotal roles of a kidney transplant in maintaining physiologic homeostasis. Preclinical non-human primate models demonstrated that genetically modified porcine kidneys with the same genetic modifications and breed background (Yucatan mini-swine) as our donor (ESUS-1784) could maintain stable creatinine levels in the absence of native non-human primate kidneys18. The clearance function of a xenograft with different genetic modifications and breed background from ESUS-1784 was recently assessed in a brain-dead decedent model, which demonstrated substantial renal clearance of both endogenous and exogenous markers, but raised concerns about cystatin C as a reliable glomerular filtration rate (GFR) marker19. In contrast, this study found no significant discrepancy between creatinine- and cystatin C-based eGFR. These differences may originate from the decedent’s significant muscle loss and high inflammatory status in critical condition20. Our findings suggest that porcine kidney xenografts can maintain substantial renal clearance function in living humans, which can be reliably estimated by either serum creatinine or cystatin C levels.
The recipient exhibited sodium retention and volume expansion, a finding requiring careful interpretation. Given that similar sodium retention was not observed in non-human primates following xenotransplantation18, this may reflect a host-specific response rather than a xenograft-related phenomenon. The most likely explanation in this case is the recipient’s underlying heart failure with preserved ejection fraction (HFpEF). A cardiorenal syndrome component may have contributed to renal hypoperfusion, leading to compensatory sodium retention by the xenograft. Also, given that sodium avidity can occur in allotransplant recipients with underlying heart failure even in the presence of RAAS blockade through RAAS-independent mechanisms—such as sympathetic nervous system activation and reduced natriuretic peptide activity21,22—this finding is more attributable to host-specific mechanisms than to intrinsic porcine tubular physiology. Nevertheless, we cannot exclude the possibility that porcine kidneys possess an inherently greater propensity for sodium reabsorption via RAAS-independent manner.
In contrast, non-human primate models have typically demonstrated volume depletion with transient rise in serum creatinine, attributed to impaired RAAS functionality and ADH incompatibility23. Consistent with this, our recipient’s RAAS axis appeared downregulated, as porcine renin is inefficient at cleaving human angiotensinogen to generate angiotensin I. Notably, no hemodynamic instability or volume depletion was observed. These findings underscore the need for further investigation of sodium handling in future xenotransplant recipients, particularly those without pre-existing cardiac dysfunction. Another interesting observation was the decline in human plasma renin protein levels following transplantation (Fig. 2G). This likely reflects a shift in renin sensing and regulation from the native kidneys to the functioning porcine kidney, which received the majority of renal blood flow24 and became the primary site of renin secretion, albeit porcine renin, which is not effective at activating the human RAAS cascade.
Metabolic alkalosis occurred in the context of loop diuretic use, high-dose steroids, and calcium carbonate supplementation. While these are common contributors to alkalosis in transplant patients, it is noteworthy that porcine kidneys maintain a higher baseline serum bicarbonate level than human kidneys, as shown in a previous study by Hannon et al.25 as well as in Supplemental Table 1. Whether the observed alkalosis reflects these interspecies differences or results from post-transplant medical interventions remains unclear. Monitoring and adjusting alkali load may be important in future xenotransplant recipients.
Our case provides further insight into the water-handling function of a porcine kidney in a living human. Pig kidneys have a lower proportion of long-looped nephrons compared to human kidneys, which may limit their ability to generate a steep osmotic gradient necessary for urine concentration26. Additionally, concerns have been raised about the potential incompatibility of human ADH with porcine receptors, which could impair water reabsorption and lead to excessive urine output. These physiological differences have been observed in previous preclinical models, where pig kidney xenografts exhibited increased urine output and low urine osmolality23. Despite these concerns, our case demonstrated that a porcine xenograft in a living human largely preserved urine-concentrating capacity. This contrasts with a recent decedent study, where extreme polyuria—up to 37 L in 24 h—was reported, accompanied by severe hypernatremia (serum sodium 167 mEq/L on POD 2)19. Notably, the brain-dead recipient had limited endogenous pituitary ADH production and urine output improved with desmopressin. In our recipient, urine output remained stable except during the immediate post-transplantation period and transiently during acute kidney injury from rejection. Daily electrolyte-free water excretion remained below 1.5 L/day and was manageable with oral hydration. However, intermittent episodes of mild hypernatremia occurred, which may have been due to voluntary fluid restriction in response to edema or repeated loop diuretic use—potentially affecting the medullary concentrating ability of the xenograft. These findings suggest that, in the presence of intact pituitary function, a porcine kidney xenograft can effectively regulate water balance in a human, though close monitoring of fluid and electrolyte status remains essential.
Inter-species differences in uric acid metabolism between humans and pigs have been under-recognized in xenotransplantation research. Unlike humans, pigs possess uricase, an enzyme that breaks down uric acid into allantoin. Our human ancestors lost this enzyme during evolution, resulting in the inability to degrade uric acid. Furthermore, humans reabsorb ~90% of the filtered urate along the nephron, leading to higher blood urate levels compared to pigs. In contrast, pig kidneys remove urate by filtration and secretion without significant reabsorption27. As suggested in a perspective article by Percudani et al.28, the urate-preserving characteristic of the human kidney might be an evolutionary renal-protective mechanism to prevent urate precipitation in the kidney, even though this may expose humans to a higher risk of gout. As the donor pig kidney has never been challenged by a high uric acid condition, we closely monitored the impact of a higher uric acid burden on pig xenograft post-xenotransplantation. Even though the tissue biopsy of xenograft did not show any evidence of urate crystal precipitation, high urinary uric acid excretion was observed in the early post-transplant period, which decreased as a new steady state was reached with low serum uric acid levels. Whether high uric acid excretion requires intervention remains unclear. Strategies such as administering exogenous uricase or xanthine oxidase inhibitors warrant further study to assess whether acute and chronic uric acid urinary exposure could impact porcine xenograft function.
Hypercalcemia and mild hypophosphatemia were observed in the non-human primate recipient xenotransplantation models10,18. Given the absence of hyperparathyroidism, hypervitaminosis D, or increased bone turnover, it was considered that PTH receptors in the pig kidney might have increased sensitivity to non-human primate PTH. In the human decedent model, on the other hand, hypocalcemia and hyperphosphatemia were observed19. The decedent’s calcium level remained stable with intravenous calcium supplementation, and the fractional excretion of phosphorus was appropriately increased. Our recipient also developed hypocalcemia and hyperphosphatemia. Notably, our recipient had markedly limited urinary excretion of phosphate even in the setting of sufficient GFR and elevated intact FGF23 levels. The absence of endogenous PTH from post-parathyroidectomy hypoparathyroidism and the use of high-dose calcitriol could have contributed to limited urinary phosphate excretion. Furthermore, it could have unmasked the potential incompatibility of human FGF23 with pig FGF23 receptors or the co-receptor Klotho. In allotransplantation, the absence of endogenous PTH typically has limited impact on renal phosphate excretion when the FGF23-Klotho axis is intact, as FGF23 is the primary phosphaturic hormone. Therefore, we believe the phosphate retention observed in our recipient may reflect a species-specific resistance of the porcine kidney to human FGF23 signaling. Further studies are needed to determine whether an intact human PTH axis can restore normal phosphate regulation in porcine xenograft recipient, and to assess whether the porcine kidney is inherently resistant to human FGF23.
The development of hypomagnesemia is not uncommon among kidney allograft recipients. Renal magnesium wasting occurs frequently during treatment with calcineurin inhibitors and can be exacerbated by diuretic use. Our recipient developed hypomagnesemia post-xenotransplantation in the context of ongoing tacrolimus and loop diuretic use. Additionally, he was taking proton pump inhibitors, which could have induced gastrointestinal magnesium loss. Whether the porcine kidney is more sensitive to the urinary loss of magnesium or whether the hypomagnesemia originates from other etiologies, including drugs, remains unanswered, though the magnitude of hypomagnesemia was similar to what is observed in human kidney transplantation.
Pig erythropoietin shares significant homology with human erythropoietin29, but its ability to activate human erythropoietin receptors remains uncertain. Our recipient experienced hypo-proliferative anemia, a condition previously noted in non-human primate recipients following porcine kidney xenotransplantation. The development of post-transplant anemia likely stemmed from multiple factors, including frequent phlebotomy, drug effects, and transient inflammation, more than a mismatch between pig erythropoietin and human erythroid progenitor cells. However, it remains unclear whether pig erythropoietin was sufficiently effective for the recipient’s erythroid progenitor cells to rapidly respond to acute anemia. Nonetheless, considering the availability of exogenous erythropoietin-stimulating agents for clinical use, any limited activation of human erythropoietin receptors by pig erythropoietin is expected to be clinically manageable.
The donor pig used in this study is from the Yucatan mini-swine strain and underwent a total of 69 genetic modifications designed to enhance xenograft compatibility and safety. These edits included: (1) triple knockout of key porcine xenoantigens (α1,3-galactosyltransferase, Neu5Gc and Sd(a)) to prevent hyperacute rejection; (2) insertion of seven human transgenes encoding proteins involved in complement regulation, coagulation control, immune modulation, and anti-inflammatory responses (e.g., hCD46, hCD55, hEPCR, hTHBD, hCD47, HMOX1, hTNFIP3); and (3) inactivation of all copies of porcine endogenous retroviruses (PERVs) to minimize theoretical risks of cross-species viral transmission15. This editing strategy contrasts with the genetic profile of the donor pig (large white swine) used in the xenotransplantation performed by the NYU group, which incorporated 10 modifications but did not include PERV inactivation and did include growth hormone receptor knockout to limit graft overgrowth30. While these differences reflect distinct approaches to donor optimization, there is currently no evidence indicating that specific variations in gene-editing strategies result in clinically meaningful differences in graft function or immunologic behavior. However, direct comparative studies across models have not yet been performed and will be essential to fully elucidate the impact of these genetic designs on xenograft outcomes.
This study has limitations due to the relatively short follow-up due to the recipient’s unexpected, sudden cardiac death. As a result, it was not possible to evaluate the long-term function of the kidney xenograft, including its potential for endocrine adaptation, tubular plasticity, and immunologic responses to the diverse pharmacologic, infectious, and environmental challenges encountered in daily human life. Longer-term follow-up—ideally exceeding 6 months—would provide further insights into the durability and physiological adaptation of the kidney xenograft in a human host.
The recipient’s multiple underlying comorbidities—including HFpEF and iatrogenic hypoparathyroidism—limit the generalizability of the observed xenograft performance to broader patient populations. Future clinical studies involving recipients without major cardiac or parathyroid pathology will help determine whether findings such as sodium avidity and limited urinary phosphate excretion reflect inter-species incompatibility or are influenced by host-specific factors.
Additionally, this study lacks inulin-, iothalamate-, or iohexol-based direct measurements of GFR. Lastly, exposure to multiple drugs may have introduced confounding effects, limiting our ability to interpret the xenograft’s physiologic regulatory capacity.
This case provides the first in-depth evaluation of a porcine kidney xenograft in a living human, demonstrating functional waste clearance, electrolyte regulation, and hemodynamic stability. While physiological challenges such as sodium retention, ineffective cleavage of human angiotensinogen by porcine renin, hyperphosphatemia, and anemia require further investigation, these findings validate the potential for xenotransplantation to address the critical organ shortage crisis. Ongoing clinical trials with multiple kidney xenograft recipients and longer-term follow-up will be essential to optimize post-transplant care and further investigate the feasibility of xenotransplantation as a scalable solution.
Methods
Screening, inclusion, and ethical considerations for a study participant
A potential xenotransplantation candidate was screened among the kidney transplantation candidates approved for transplant at MGH with ongoing challenges with dialysis, no potential living donor, and an expected waiting time for a deceased donor of longer than 4 years15. Sex and gender were not considered in the study design for recipient selection. This study was approved by the MGH Institutional Review Board (IRB #2023P003631). A selected candidate had multiple in-depth discussions with the MGH transplantation team regarding the current medical status and potential risks/benefits of xenotransplantation. Written informed consent was obtained, according to CARE guidelines and in compliance with the Declaration of Helsinki principles, both for proceeding with the first pig kidney transplantation into a living recipient under a ‘single patient, compassionate use authorization’ from the Food and Drug Administration (FDA), and for publishing potentially identifiable information.
Genetically modified porcine donor
A 1-year-old female Yucatan mini-swine donor (ESUS-1784), carrying 69 genomic edits made using CRISPR-Cas9 technology, was produced and provided by eGenesis, Inc. (Cambridge, MA). Detailed information about the donor genetic composition was previously reported7. In brief, the donor kidney (EGEN-2784) was engineered to eliminate three known glycan xenoantigens, which could trigger an antibody response in humans, and to express human thrombo-regulatory proteins, complement regulatory proteins, and inflammatory and immunity regulating proteins. In addition, 59 copies of porcine endogenous retroviral elements were inactivated. The study design did not account for sex in the selection of donors. The porcine donor was maintained in a biosecure facility, and underwent regular pathogen screening according to FDA recommendations. The animal procedures were reviewed and approved by Biomere Institutional Animal Care and Use Committee (IACUC; protocol 24-04).
Immunosuppressive regimen
The recipient received an immunosuppressive regimen centered on an anti-CD154 monoclonal antibody (tegoprubart), informed by successful preclinical non-human primate studies7,8,18. Induction therapy included rituximab and rabbit anti-thymocyte globulin, followed by maintenance immunosuppression with tegoprubart, an anti-C5 monoclonal antibody (ravulizumab), tacrolimus, mycophenolic acid, and corticosteroids15.
Blood and urine sample analysis and result reporting
Blood and urine samples were obtained at a pre-specified schedule. All tests addressed below were conducted in the MGH Core Laboratory, and the results were reported to the Epic Online Electronic Health Record system. Each measurement was taken from distinct samples without repeated measurements.
Measurement of glomerular filtration rate
The GFR of xenograft was assessed using various methods, including measured creatinine clearance (CrCl) based on 24 hour urine collections, and creatinine- and cystatin C-based GFR estimating formulas. The measured creatinine clearance was corrected for body surface area (BSA) and obtained using the formula below.
Serum creatinine- and cystatin C-based eGFR were calculated using the refit Chronic Kidney Disease Collaboration (CKD-EPI) 2021 equation31.
Measurement of sodium and water balance
Repeated measurements of serum sodium and osmolality, along with urine sodium, potassium, and urine osmolality from spot urine samples, were obtained during the follow-up period. Both electrolyte-free water clearance (CEFW) and solute-free water clearance (CH2O) were calculated as a measure of xenograft water handling.
The CEFW was measured using the formula below:
The CH2O was measured using the formula below:
The fractional excretion (FE) of sodium was calculated using serum and spot urine samples collected in the morning around the same time.
Assessment of acid-base regulation
Serum bicarbonate levels were acquired throughout the follow-up period, and venous pH was measured using blood gas studies. Serial measurements of urinary chloride, potassium, creatinine, and pH were also obtained.
Monitoring of hemodynamic status
The patient’s hemodynamic status was closely monitored during the follow-up period. Initially, an invasive arterial blood pressure monitor was utilized during the immediate postoperative period, followed by a transition to a non-invasive blood pressure monitoring device. Additionally, the trend of body weight changes was tracked.
Renin-angiotensin-aldosterone system measurements
For assessment of the renin-angiotensin-aldosterone system (RAAS) axis, plasma renin activity (PRA) and serum aldosterone levels were measured several times during the follow-up period in the MGH Core laboratory, using liquid chromatography tandem mass spectrometry.
Samples collected for further in-depth analysis of each RAAS component
EDTA-plasma and serum samples were collected from the pig kidney recipient before and after the transplantation. EDTA-plasma samples were collected before transplantation and on post-operative days (POD) 7, 13, 26 and 39. Serum samples were collected before transplantation and on POD 7, 13, 26 and 33. EDTA-plasma and serum samples from five human subjects who underwent kidney allotransplantation were used as controls. A serum sample from a donor pig was used as an additional control.
Measurement of human active renin by enzyme-linked immunosorbent assay (ELISA)
Active human renin was measured in human EDTA-plasma and donor pig serum using a quantitative solid-phase sandwich ELISA (EIA-5125), distributed by DRG Instruments (Marburg, Germany), with a minimum detection limit of 0.8 pg/mL and 0.69% cross-reactivity with human prorenin. When pig serum was tested in this ELISA, the values were below the detectability limit (<0.8 pg/mL). In our previous work with human urine samples, the coefficients of intra- and inter-assay variation for active human renin ELISA were 4.9% and 12.7%, respectively32. Internal controls supplied by the manufacturer were included on each occasion (one for high renin and one for low renin values) to assure consistency of inter-assay performance.
Measurement of pig renin by ELISA
Pig renin was measured in human EDTA-plasma and serum as well as naïve pig serum using a quantitative solid-phase sandwich Pig REN/Renin 1 ELISA Kit ELISA from LSBio (Catalog No. LS-F32145; Lynnwood, WA) with a detection range of 78.125−5000 pg/mL and with an intra-assay coefficient of variation (CV) of <8 % and an inter-assay CV of <10%, respectively. When human control sera were tested in this ELISA, the values were all above the detectability limit suggesting cross-reactivity with human renin/prorenin protein.
Extraction and measurement of plasma angiotensin I by ELISA
Plasma peptides were extracted from human EDTA-plasma using reverse phase phenyl silica columns (HYPERSEP Phenyl 50 mg; Thermo Scientific, Rockwood, TN) as per manufacturer’s instructions. The quantity of Angiotensin (Ang) I peptide in the extract was determined using an enzyme immunoassay (EIA) kit (Catalog No. S-1188, Peninsula Laboratories; CA, USA). Results were reported in pg/mL. According to the manufacturer, there is negligible cross-reactivity with Ang-(1-12), Ang II, Ang-(1-7), Ang-(1-5), Ang III, Ang-(1-9), or Ang A.
Assessment of uric acid and magnesium regulation
Serial measurements of serum uric acid and serum magnesium levels were obtained along with the concentration of uric acid and magnesium in spot urine. 24 hour urinary excretion of uric acid and magnesium were also acquired. The FE of uric acid and magnesium were calculated using serum and spot urine samples collected in the morning around the same time.
Assessment of calcium/phosphorus homeostasis
Serum total calcium and phosphorus levels were obtained along with urine calcium and phosphorus levels from both spot urine and 24 hour urine collection samples. The FE of calcium and phosphate were calculated using these serum and spot urine samples. Furthermore, serum intact parathyroid hormone (PTH), PTH-related peptide (PTH-rP), 25-OH Vitamin D, 1,25 dihydroxy Vitamin D, intact fibroblast growth factor 23 (FGF23), and collagen type 1b-telopeptide (collagen CTx) levels were repeatedly measured before and after the transplantation. Serum PTH levels were measured using electrochemiluminescence immunoassay.
Measurement of proteinuria
The total urinary protein and microalbumin levels were measured from consecutive 24 hour urine samples until POD 18 and then repeated a few more times during the follow-up period. Repeated measurements of urine protein/creatinine ratio (UPCR) and urine albumin/creatinine ratio (UACR) were also obtained from spot urine samples to estimate 24 hour proteinuria and albuminuria.
Assessment of hematopoiesis
Complete blood counts (CBC), including hemoglobin, hematocrit, MCV, MCH, red blood cell count, red cell distribution width (RDW), white blood cell count, and platelet count were repeatedly measured. Blood erythropoietin levels were also repeatedly measured before and after the transplantation. Further anemia work-up was conducted by measuring reticulocytes, serum iron, ferritin, total iron-binding capacity, lactate dehydrogenase, haptoglobin, vitamin B12, and folate levels and by performing a peripheral blood smear.
Electron microscopy
Electron microscopy (EM) was performed on tissues fixed in Karnovsky fixative and evaluated using a transmission electron microscope (FEI Morgagni) with an AMT 2 K digital charge-coupled device camera (Advanced Microscopy Techniques, Woburn, MA).
Data collection and visualization
Data collection was performed using Microsoft Excel (Microsoft 365, Version 2506, Build 16.0.18925.20076). Data were visualized using GraphPad Prism (version 10).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The data reported in this study are provided in the Source Data file. The unreported data cannot be made publicly available due to restrictions based on the US Health Insurance Portability and Accountability Act (HIPAA), ensuring patient privacy, as well as intellectual property protections held by collaborators. To request data, please contact the corresponding author. All data requests will be evaluated at the discretion of legal counsel representing the relevant parties, including the Massachusetts General Hospital, eGenesis, Inc., and any collaborators involved in data generation. We will aim to respond to data access requests within 30 days, subject to the approval of the relevant parties. Source data are provided with this paper.
References
United States Renal Data System. 2023 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. https://usrds-adr.niddk.nih.gov/2023 (2023).
Tonelli, M. et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am. J. Transpl. 11, 2093–2109 (2011).
Stewart, F. et al. Exploring kidney dialysis costs in the United States: a scoping review. J. Med. Econ. 27, 618−625 (2024).
Tullius, S. G. & Rabb, H. Improving the supply and quality of deceased-donor organs for transplantation. N. Engl. J. Med. 378, 1920–1929 (2018).
Lentine, K. L. et al. OPTN/SRTR 2022 annual data report: kidney. Am. J. Transpl. 24, S19–s118 (2024).
Sykes, M. & Sachs, D. H. Transplanting organs from pigs to humans. Sci. Immunol. 4, eaau6298 (2019).
Anand, R. P. et al. Design and testing of a humanized porcine donor for xenotransplantation. Nature 622, 393–401 (2023).
Ma, D. et al. Kidney transplantation from triple-knockout pigs expressing multiple human proteins in cynomolgus macaques. Am. J. Transpl. 22, 46–57 (2022).
Niu, D. et al. Inactivation of porcine endogenous retrovirus in pigs using CRISPR-Cas9. Science 357, 1303–1307 (2017).
Iwase, H. et al. Immunological and physiological observations in baboons with life-supporting genetically engineered pig kidney grafts. Xenotransplantation 24, 10.1111/xen.12293 (2017).
Yamamoto, T. et al. Life-supporting kidney xenotransplantation from genetically engineered pigs in baboons: a comparison of two immunosuppressive regimens. Transplantation 103, 2090–2104 (2019).
Porrett, P. M. et al. First clinical-grade porcine kidney xenotransplant using a human decedent model. Am. J. Transpl. 22, 1037–1053 (2022).
Montgomery, R. A. et al. Results of two cases of pig-to-human kidney xenotransplantation. N. Engl. J. Med. 386, 1889–1898 (2022).
Locke, J. E., Kumar, V., Anderson, D. & Porrett, P. M. Normal graft function after pig-to-human kidney xenotransplant. JAMA Surg. 158, 1106–1108 (2023).
Kawai, T. et al. Xenotransplantation of a porcine kidney for end-stage kidney disease. N. Engl. J. Med. 392, 1933−1940 (2025).
Iwase, H., Yamamoto, T. & Cooper, D. K. C. Episodes of hypovolemia/dehydration in baboons with pig kidney transplants: a new syndrome of clinical importance?. Xenotransplantation 26, e12472 (2019).
Maesaka, J. K., Imbriano, L. J. & Miyawaki, N. Determining fractional urate excretion rates in hyponatremic conditions and improved methods to distinguish cerebral/renal salt wasting from the syndrome of inappropriate secretion of antidiuretic hormone. Front Med. (Lausanne) 5, 319 (2018).
Firl, D. J. et al. Clinical and molecular correlation defines activity of physiological pathways in life-sustaining kidney xenotransplantation. Nat. Commun. 14, 3022 (2023).
Judd, E. et al. Physiologic homeostasis after pig-to-human kidney xenotransplantation. Kidney Int. 105, 971–979 (2024).
Carrero, J. J. et al. Discordances between creatinine- and cystatin c-based estimated GFR and adverse clinical outcomes in routine clinical practice. Am. J. Kidney Dis. 82, 534–542 (2023).
Charloux, A., Piquard, F., Doutreleau, S., Brandenberger, G. & Geny, B. Mechanisms of renal hyporesponsiveness to ANP in heart failure. Eur. J. Clin. Invest. 33, 769–778 (2003).
Triposkiadis, F. et al. The sympathetic nervous system in heart failure revisited. Heart Fail Rev. 29, 355–365 (2024).
Hansen-Estruch, C. et al. Renin-angiotensin-aldosterone system function in the pig-to-baboon kidney xenotransplantation model. Am. J. Transpl. 23, 353–365 (2023).
D’Cunha, P. T., Parasuraman, R. & Venkat, K. K. Rapid resolution of proteinuria of native kidney origin following live donor renal transplantation. Am. J. Transpl. 5, 351–355 (2005).
Hannon, J. P., Bossone, C. A. & Wade, C. E. Normal physiological values for conscious pigs used in biomedical research. Lab Anim. Sci. 40, 293–298 (1990).
Hansen-Estruch, C., Cooper, D. K. C. & Judd, E. Physiological aspects of pig kidney xenotransplantation and implications for management following transplant. Xenotransplantation 29, e12743 (2022).
Simmonds, H. A., Hatfield, P. J., Cameron, J. S. & Cadenhead, A. Uric acid excretion by the pig kidney. Am. J. Physiol. 230, 1654–1661 (1976).
Percudani, R., Capelli, C., Sassi, G. & Mori, G. Evolutionary differences in uric acid metabolism inform about the risks of pig-to-human kidney transplant. J. Am. Soc. Nephrol. 9, 1281−1283 (2024).
Wen, D. et al. Erythropoietin structure-function relationships: high degree of sequence homology among mammals. Blood 82, 1507–1516 (1993).
Peterson, L. et al. Physiological basis for xenotransplantation from genetically modified pigs to humans. Physiol. Rev. 104, 1409–1459 (2024).
Inker, L. A. et al. New creatinine- and cystatin C-based equations to estimate GFR without race. N. Engl. J. Med. 385, 1737–1749 (2021).
Tang, J. et al. Urinary renin in patients and mice with diabetic kidney disease. Hypertension 74, 83–94 (2019).
Acknowledgements
We thank the patient and his family for their extraordinary courage, generosity, and trust, which made this groundbreaking effort possible. Their strength, hope, and partnership were central to every step of this journey. We are also deeply grateful to the team at eGenesis for their unwavering collaboration and scientific innovation that laid the foundation for this achievement. In particular, we acknowledge the contributions of the eGenesis preclinical and clinical translation teams, including Kristen Getchell, Susan Low, Lee Tien and Michael Curtis, whose expertise and dedication made the xenograft organ available for transplantation and supported the clinical application. We further thank the multidisciplinary team at Massachusetts General Hospital—including clinical staff, surgeons, nurses, researchers, ethicists, pharmacists, care coordinators, and administrative leaders—whose tireless commitment and expertise were essential to the care of the patient and the success of this pioneering case. Tegoprubart was provided in kind by Eledon Pharmaceuticals, and ravulizumab was provided in kind by Alexion. We also appreciate Martin Selig (the MGH EM Unit) for obtaining the electron microscopy images of the xenograft. L.V.R. received research support from the National Institutes of Health (grant R01AI143887). S.L. is funded by a U2C/TL1 Harvard Kidney, Urology, and Hematology Training Institute Network Grant (TL1DK143273).
Author information
Authors and Affiliations
Contributions
S.L. and M.C.L. contributed to data collection, data visualization, and manuscript drafting. L.R., W.W.W., K.S., R.P., A.A.J., A.C.B., P.N., H.G., and H.J. provided post-transplant care. L.R., W.W.W., K.S., R.P., A.A.J., A.C.B., P.N., H.G., H.J., E.P.R., T.J.B., and T.K. critically evaluated the data interpretation and provided comments for manuscript revision. L.M. and T.J.B. contributed to the collection of patient samples. M.A.L. and K.F.J. contributed to the medication review and visualization of relevant data. I.R. provided the EM image and a description of the EM methodology. T.B., J.W., and D.B. performed ELISA for in-depth analysis of each RAAS component. All authors critically reviewed and edited the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The clinical study was supported by Massachusetts General Hospital and eGenesis. The source animal and porcine blood chemistry data were provided in kind by eGenesis. No direct salary or financial incentives were provided to the investigators by eGenesis. L.V.R. has served on scientific advisory boards for Apellis, Sanofi, Calliditas, and Novo Nordisk. D.B. and J.W. are coinventors of patents entitled “Active Low Molecular Weight Variants of Angiotensin Converting Enzyme 2 (ACE2)” and “Soluble ACE2 Variants and Uses Therefor.” D.B. is the founder of Angiotensin Therapeutics Inc. and a main shareholder. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Hidetaka Hara and Alp Sener for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, S.A., Lafargue, MC., Williams, W.W. et al. Physiologic Homeostasis in a Living Human after Pig Kidney Xenotransplantation. Nat Commun 16, 8453 (2025). https://doi.org/10.1038/s41467-025-63153-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-63153-3