Abstract
Parkinson’s disease (PD) is characterized by the selective degeneration of midbrain dopaminergic neurons and aggregation of α-synuclein. Emerging evidence implicates the gut microbiome in PD, with microbial metabolites proposed as potential pathological mediators. However, the specific microbes and metabolites involved, and whether gut-derived metabolites can reach the brain to directly induce neurodegeneration, remain unclear. Here we show that elevated levels of Streptococcus mutans (S. mutans) and its enzyme urocanate reductase (UrdA), which produces imidazole propionate (ImP), in the gut microbiome of patients with PD, along with increased plasma ImP. Colonization of mice with S. mutans harboring UrdA or Escherichia coli expressing UrdA from S. mutans increases systemic and brain ImP levels, inducing PD-like symptoms including dopaminergic neuronal loss, astrogliosis, microgliosis, and motor impairment. Additionally, S. mutans exacerbates α-synuclein pathology in a mouse model. ImP administration alone recapitulates key PD features, supporting the UrdA–ImP axis as a microbial driver of PD pathology. Mechanistically, mTORC1 activation is crucial for both S. mutans- and ImP-induced PD pathology. Together, these findings identify microbial ImP, produced via UrdA, as a direct pathological mediator of the gut-brain axis in PD.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is the second most prevalent neurodegenerative disorder and involves the selective loss of dopaminergic neurons and α-synuclein (α-Syn) aggregation in the substantia nigra pars compacta, which consequently leads to cardinal motor deficits, including tremor, rigidity, and bradykinesia1. Although genetic factors may contribute to the development of PD, most cases are idiopathic, suggesting that environmental factors may also play a crucial role. Several environmental factors, including age, pesticides, metals, viruses, and dietary factors reciprocally interact with PD-related pathological signaling pathways2.
The gut microbiome is strongly influenced by environmental factors, such as diet, antibiotics, inflammation, and age3. The potential interactions between the gut microbiome and PD pathology have been explored extensively in order to unravel the molecular mechanisms underlying sporadic PD. The composition of the gut microbiota is altered in individuals with PD compared with that in control participants4. Fecal microbiota from patients with PD can promote PD-like symptoms in α-Syn overexpressing PD mouse models5, further underscoring the fact that gut microbiome is a crucial environmental factor and that gut-brain axis plays a crucial role in PD pathogenesis. However, the specific microbes that contribute to the key pathological features of PD have not been identified yet.
One central mechanism suggested to support the gut-brain axis interaction involves trans-neuronal α-Syn pathology propagation from the enteric nervous system (ENS) to the brain via the vagus nerve6,7. The gut microbiome can directly influence both gut and brain cell phenotypes via the production of bioactive metabolites8,9. For example, some gut-derived microbial metabolites can penetrate the fetal brain and regulate axonogenesis10. Another class of microbial metabolites, the short-chain fatty acids (SCFAs), promotes α-Syn-induced microglia activation and PD-like pathologies, such as motor deficits5. Although SCFA-induced promotion of α-Syn-mediated neuroinflammation has been observed in various brain regions, including the frontal cortex, putamen, and ventral midbrain, its role in dopaminergic neuronal death has not been investigated yet5. Additionally, other studies have reported a reduction in butyrate-producing bacteria and fecal SCFA levels in patients with PD11,12. Thus, the gut-derived, brain-permeable microbial metabolites that contribute to selective dopaminergic neurodegeneration and α-Syn-related pathology in PD remain to be identified.
A recent large-scale whole-genome shotgun sequencing of fecal samples from 490 individuals with PD and 234 neurologically healthy elderly controls has formed a high-resolution dataset13. This dataset provides a comprehensive understanding of the dysbiotic features of the gut microbiome in individuals with PD. Moreover, analysis revealed a significant enrichment of microbial pathways related to proteolytic and amino acid degradation in PD. Streptococcus mutans, typically found in the oral cavity, as one of the microbial strains within the gut microbiome of individuals with PD that is most significantly associated with this condition13. Importantly, S. mutans possesses a urocanate reductase (UrdA) that converts urocanate to imidazole propionate via the histidine degradation pathway14. In this study, we sought to determine whether the oral microbe S. mutans can colonize the gut and affect PD pathology via microbial UrdA and its metabolite, imidazole propionate.
Results
urdA-coding microbial enzyme, responsible for producing imidazole propionate, is enriched in the gut microbiome of patients with PD
To identify species with differential abundances in the gut microbiome of individuals with PD, we conducted an unbiased metagenome-wide association study by reanalyzing publicly available dataset13. Our analysis confirmed Bifidobacterium dentium and S. mutans as the most significantly associated species with PD, both showing increased abundance in PD (Supplementary Fig. 1a and Fig. 1a). While B. dentium was notably enriched, it is frequently detected in the feces of healthy individuals15,16 and has been implicated in beneficial roles, such as reducing colonic inflammation17, improving the intestinal mucus layer18, and normalizing repetitive and anxiety-like behaviors through serotonergic regulation19. Given these potentially protective roles, we focused our investigation on S. mutans to explore its potential pathogenic role in PD. Specifically, we investigated whether the level of urdA (gene encoding urocanate reductase, an enzyme for imidazole propionate production) is altered in the gut microbiome of individuals with PD. Thus, we analyzed the abundance of urdA and hutH (encoding histidine ammonia lyase responsible for converting histidine to urocanate) using published whole-genome shotgun sequencing datasets of fecal samples from 491 individuals with PD and 234 neurologically healthy elderly controls13. Our analysis showed significantly higher levels of urdA in patients with PD than in neurologically healthy controls, whereas hutH levels showed no significant differences (Fig. 1b, c). Furthermore, urdA from S. mutans, but not from other Streptococcus species, was significantly more prevalent in PD patients (Supplementary Fig. 1b, c), supporting the rationale for investigating the potential role of the UrdA-possessing bacterial strain S. mutans and imidazole propionate in PD pathology.
a Relative abundance of S. mutans in the gut microbiome of patients with PD (n = 491) and age-matched healthy controls (n = 234). Data were log10-transformed and are presented as box plots showing minimum, 25% quartile, median, 75% quartile, and maximum. b, c Normalized gene copy numbers of urocanate reductase (urdA, b) and histidine ammonia lyase (hutH, c) in the gut microbiome from patients with PD and age-matched healthy controls. Box plots represent the median (centre line), 25%–75% quartile (bounds of box), minima and maxima (whiskers), with all individual data points shown. d Schematic illustration of the experimental procedure showing colonization of germ-free (GF) mice with S. mutans or pasteurized S. mutans (P-S. mutans) via oral gavage. Fecal samples were collected from GF mice before (D0) and 28 days after S. mutans colonization. Created in BioRender. Kim, J. (https://BioRender.com/xsj2j6c). e Quantification of live S. mutans in the feces by assessing viable colony formation from GF mice gavaged with vehicle (Veh), S. mutans, or P-S. mutans (n = 7 mice per Veh and P-S. mutans group, n = 8 mice per S. mutans group). CFU, colony forming unit. f (Left panel) Representative anti-TH (tyrosine hydroxylase) immunohistochemistry images of ventral midbrains from GF mice colonized with S. mutans or P-S. mutans, or vehicle control. Brain sections were counterstained with Nissl. Magnified images showing dopaminergic processes in the substantia nigra pars reticulata (SNr) are also presented below. (Right panel) Stereological counts of TH-positive and Nissl-stained dopaminergic neurons in the substantia nigra pars compacta (SNpc). Relative TH fiber density and Nissl-stained neuronal counts in the SNr (n = 7 mice per group). Scale bar = 100 μm, and 25 μm for enlarged images, respectively. g (Left panel) Representative images of inflammatory astrogliosis in ventral midbrains of GF mice colonized with S. mutans, P-S. mutans, or vehicle control, assessed via GFAP immunohistochemistry. Magnified images of the SNpc were presented on the right. (Right panel) Quantification of GFAP-positive area as percentage of total area (% area fraction) (n = 7 mice per group). Scale bar = 100 μm. h (Left panel) Representative images of inflammatory microgliosis in ventral midbrains of GF mice colonized with S. mutans, P-S. mutans, or vehicle control, assessed via Iba1 immunohistochemistry. Magnified images of the SNpc subregions on the right highlight inflammatory microgliosis. (Right panel) Quantification of Iba1-positive area fraction (%; n = 3 mice per group) and microglial soma size, measured from 10 cells per mouse (n = 3 mice per group). Scale bar = 100 μm. i Assessment of bradykinesia in GF mice colonized with S. mutans or P-S. mutans monitored by measuring latency to reach the base in the pole test (n = 7 mice per Veh and P-S. mutans group, n = 8 mice per S. mutans group). j Quantification of ImP concentration in the plasma from GF mice gavaged with Veh, S. mutans, or P-S. mutans. (n = 7 mice per Veh and P-S. mutans group, n = 8 mice per S. mutans group). k Quantification of ImP concentration in the brains from GF mice gavaged with Veh, S. mutans, or P-S. mutans. (n = 4 mice per Veh and P-S. mutans group, n = 6 mice per S. mutans group). Quantitative data are expressed as the mean ± standard error of the mean (S.E.M). **P < 0.01, ***P < 0.001; ns, not significant. P values were determined by the two-sided Wilcoxon rank-sum test (a-c), two-way ANOVA with Tukey’s post hoc test (e), and one-way ANOVA with Tukey’s post hoc test (f–k). Source data and test statistics are provided as a Source Data file. See also Supplementary Fig. 1.
Gut-colonized S. mutans induces dopaminergic neurotoxicity and motor dysfunction
To investigate whether S. mutans colonization in the gut contributes to PD pathology, germ-free (GF) C57BL6/N mice were colonized with S. mutans by administering 109 CFU (Colony-Forming Unit) per mouse via gavage once weekly for 28 days (totaling three gavages) (Fig. 1d). To assess the importance of S. mutans’s metabolic activity, pasteurized S. mutans were administered in the same manner (Fig. 1d). The 28-day S. mutans colonization of GF mice did not affect body weight, cecum weight, or brain weight compared to the vehicle or pasteurized S. mutans-gavaged groups (Supplementary Fig. 1d-f). Successful colonization and survival of S. mutans within the GF mouse gut was confirmed by viable colonies in feces (Supplementary Fig. 1g and Fig. 1e). Additionally, absolute quantification of the V3-V4 regions of the 16S rRNA gene and the S. mutans 16S gene revealed significantly higher S. mutans copy numbers in the S. mutans-gavaged group compared to the pasteurized S. mutans-gavaged group (Supplementary Fig. 1h), suggesting that S. mutans not only colonizes the mouse gut but also thrives in it. The colonization of S. mutans was further examined throughout the length of the intestine (Supplementary Fig. 1i, j) and showed robust colonization preferentially in the distal gut, particularly the ileum and colon, of S. mutans-gavaged GF mice.
PD is defined as the selective loss of dopaminergic neurons. Therefore, we sought to determine whether gut-colonized S. mutans induces neurotoxicity in the midbrain of GF mice. S. mutans monocolonization in GF mice was sufficient to reduce the number of tyrosine hydroxylase (TH)-positive and Nissl-stained dopaminergic neurons in the substantia nigra pars compacta, as well as TH-positive dopaminergic processes in the substantia nigra reticularis, indicating dopaminergic neurodegeneration in the midbrain (Fig. 1f). In contrast, pasteurized S. mutans colonization failed to induce dopamine-cell death (Fig. 1f), supporting the fact that S. mutans must be metabolically active to exert its pathogenicity. Consistent with this, the density of TH-positive dopaminergic axon terminals in the striatum was also reduced in a manner dependent on S. mutans metabolic activity (Supplementary Fig. 1k). However, Nissl-stained neuronal counts in the substantia nigra reticularis (Fig. 1f) and the prefrontal cortex were similar among the three experimental groups (Supplementary Fig. 1l), suggesting that S. mutans-induced neurotoxicity is brain region-specific. Moreover, S. mutans induced reactive astrogliosis in the ventral midbrain but not in the cortex, as demonstrated by a more than 3-fold increase in GFAP staining in the substantia nigra pars compacta compared to that in vehicle-treated controls (Fig. 1g, and Supplementary Fig. 1m). In contrast, metabolically inactive pasteurized S. mutans-treated mice did not show astrogliosis in the ventral midbrain (Fig. 1g). S. mutans also induced microgliosis, as indicated by increased Iba1 staining and enlarged microglial soma size, which are established markers of microglial activation (Fig. 1h). Reflecting these brain pathologies, motor deficits were induced in GF mice colonized with S. mutans, but not in those colonized with pasteurized S. mutans. as assessed by the pole test showing a significantly delayed latency to complete the pole (Fig. 1i). This supports the hypothesis that the metabolic activity of this bacterium plays a critical role. Our results indicate that the PD-associated increase in S. mutans in the gut can induce PD-related changes, such as selective loss of dopaminergic neurons, astrogliosis, microgliosis, and motor deficits.
Gut-colonized S. mutans-produced imidazole propionate enters systemic circulation and reaches the brain
PD-associated S. mutans harbors urdA, which is more abundant in the gut microbiome of patients with PD (Fig. 1b), while its activity is responsible for imidazole propionate production. Thus, we investigated whether gut-colonized S. mutans can produce imidazole propionate in vivo and whether it can enter the circulation, reaching the brain tissue. We observed that the levels of imidazole propionate produced by gut-colonized S. mutans, but not by pasteurized S. mutans, increased in the blood, reaching the brain tissue (Fig. 1j, k), while the concentration of its precursor urocanate was not affected (Supplementary Fig. 1n, o). Taken together, we showed that gut-colonized, metabolically active S. mutans in GF mice produced imidazole propionate, resulting in a marked increase in blood imidazole propionate levels and its penetration into the brain. These results suggested that the PD-associated increase in S. mutans in the human gut may contribute to the elevation of blood and brain imidazole propionate concentrations.
UrdA from S. mutans induces dopaminergic neurotoxicity and motor dysfunction
Given that urdA from S. mutans was significantly more prevalent in PD patients (Supplementary Fig. 1b) and that S. mutans may exert pathogenic effects through additional mechanisms, we heterologously expressed urdA from S. mutans in an Escherichia coli MG1655 strain lacking urdA14. While E. coli MG1655 did not produce imidazole propionate, E. coli expressing S. mutans urdA produced imidazole propionate at levels comparable to those produced by S. mutans (Fig. 2a). Importantly, urdA expression did not affect the growth rate of E. coli (Supplementary Fig. 2a). Colonization levels of both E. coli strains in the GF mouse gut were comparable (Fig. 2b, c, Supplementary Fig. 2b). No significant differences were observed in body weight, cecum weight, or brain weight among the groups (Supplementary Fig. 2c, d, e). Although S. mutans colonized both the distal small intestine and cecum, E. coli primarily colonized the cecum (Supplementary Fig. 2f), yet gut-colonized E. coli expressing urdA effectively produced systemic imidazole propionate, reaching the brain (Fig. 2d, e) without altering urocanate levels (Supplementary Fig. 2g, h). Similar to S. mutans, gut-colonized E. coli expressing urdA induced dopaminergic neurodegeneration (Fig. 2f), astrogliosis, microgliosis (Fig. 2g, h), and motor dysfunction (Fig. 2i). Consistent with dopaminergic neurodegeneration, mice colonized with urdA-expressing E. coli showed a marked reduction in dopaminergic axon terminal density in the striatum, as well as diminished dopaminergic processes in the substantia nigra reticularis (Supplementary Fig. 2i, Fig. 2f). However, neuronal numbers in the substantia nigra reticularis (Fig. 2f) and GFAP expression in the cortex remained unaffected (Supplementary Fig. 2j), again demonstrating region-specificity. Taken together, these findings identify UrdA as a key pathological factor that drives PD-related neurodegeneration, astrogliosis, microgliosis, and motor dysfunction, reinforcing the potential role of gut microbiota in PD pathology.
a Quantification of ImP concentration in the supernatants from the culture media of E. coli MG1655 strains carrying either the empty pUC19 vector (E. coli (Con)) or the recombinant plasmid pUC19-urdA (E. coli (urdA)), and S. mutans after incubation with 1 mM urocanate for 24 h (n = 3 per group). b Schematic illustration of the experimental procedure showing colonization of GF mice with commensal E. coli MG1655 carrying either the empty pUC19 vector (E. coli (Con)) or urdA from S. mutans (E. coli (urdA)) via oral gavage. Created in BioRender. Kim, J. (https://BioRender.com/9pc9rgz). c Quantification of live E. coli in feces by assessing viable colony formation (n = 6 mice per E. coli (Con) group, n = 7 mice per E. coli (urdA) group). CFU, colony forming unit. d, e Quantification of ImP concentration in the plasma (d) and brains (e) from GF mice gavaged with E. coli (Con) or E. coli (urdA) (plasma: n = 6 for E. coli (Con) group, n = 7 for E. coli (urdA) group; brain: n = 6 per group). Box plots represent the median (centre line), 25%–75% quartile (bounds of box), minima and maxima (whiskers), with all individual data points shown.f (Left panel) Representative anti-TH immunohistochemistry of ventral midbrains from GF mice colonized with E. coli (Con) or E. coli (urdA). Magnified images showing dopaminergic processes in SNr are also presented below. (Right panel) Stereological quantification of TH-stained and Nissl-stained dopaminergic neurons in the SNpc, Nissl-stained neuronal counts, and relative TH fiber density in the SNr (n = 6 mice per E. coli (Con) group, n = 7 mice per E. coli (urdA) group). Scale bar = 100 μm. g (Upper panel) Representative images of inflammatory astrogliosis in the ventral midbrains of GF mice colonized with E. coli (Con) or E. coli (urdA) determined by anti-GFAP immunohistochemistry. Magnified images of the SNpc subregions are shown below. (Bottom panel) Quantified % area fraction of GFAP signals (n = 5 mice per E. coli (Con) group, n = 4 mice per E. coli (urdA) group). Scale bar = 100 μm. h (Upper panel) Representative images of inflammatory microgliosis in the ventral midbrains of GF mice colonized with E. coli (Con) or E. coli (urdA) determined by anti-Iba1 immunohistochemistry. Magnified images of the SNpc subregions are shown below. (Bottom panel) The Iba1-positive area fraction (%) (n = 5 mice per E. coli (Con) group, n = 7 mice per E. coli (urdA) group) and microglial soma size were quantified (n = 50 microglia from 5 mice per E. coli (Con) group, n = 70 microglia from 7 mice per E. coli (urdA) group). Scale bar = 100 μm. i Assessment of bradykinesia in GF mice colonized with E. coli (Con) or E. coli (urdA) monitored by measuring latency to reach the base in the pole test (n = 6 mice per E. coli (Con) group, n = 7 mice per E. coli (urdA) group). Quantitative data are expressed as the mean ± standard error of the mean (S.E.M). *P < 0.05, **P < 0.01, ***P < 0.001; ns, not significant. P values were determined by one-way ANOVA with Tukey’s post hoc test (a), two-way ANOVA with Tukey’s post hoc test (c), and unpaired two-tailed Student’s t-tests (d–i). Source data and test statistics are provided as a Source Data file. See also Supplementary Fig. 2.
Gut-colonized S. mutans induces dopaminergic neurotoxicity and motor dysfunction via mTORC1 activation
Next, we sought to determine the molecular mechanisms underlying dopaminergic toxicity induced by S. mutans. Imidazole propionate altered insulin signaling by activating the p38γ-mTORC1 pathway in hepatocytes14. The activation of the mTORC1 pathway has been implicated in aging and neurodegenerative diseases20. Imidazole propionate produced by gut-colonized S. mutans reached the brain (Fig. 1k), therefore, we investigated whether this colonization is sufficient to induce mTORC1 activation in the midbrain. Intriguingly, gut-colonized S. mutans in GF mice, and not pasteurized S. mutans, led to phosphorylation of S6 and 4E-BP1, surrogate markers of mTORC1 activation, specifically in dopaminergic neurons (TH-positive) of the substantia nigra pars compacta, without affecting mTORC1 signaling in non-dopaminergic neurons in the substantia nigra reticularis (Fig. 3a, and Supplementary Fig. 3a) or the prefrontal cortex (Supplementary Fig. 3b). Similarly, gut-colonized E. coli expressing urdA increased S6 phosphorylation in TH-positive dopaminergic neurons of the substantia nigra pars compacta but not in the substantia nigra reticularis (Fig. 3b). This relatively selective mTORC1 activation in dopaminergic neurons was consistent with their observed loss of dopaminergic neurons in the ventral midbrain without involving cortical neuron pathology in GF mice colonized with S. mutans (Fig. 1f). While imidazole propionate exerted relative regional specificity in inducing brain pathology in vivo, mTORC1 activation was still elicited in primary cortical neurons following imidazole propionate treatment in vitro, as evidenced by the phosphorylation of S6K1 at T389 and subsequent downstream signaling events, such as serine phosphorylation of IRS1 (Fig. 3c). These effects were effectively blocked by the mTORC1 inhibitor rapamycin or p38γ inhibitor pirfenidone (Fig. 3c), in line with the previous findings in primary hepatocytes9,14. Additionally, imidazole propionate treatment of primary cultured cortical neurons resulted in ~50.3% neurotoxicity, which was effectively blocked by both rapamycin and pirfenidone treatments (Supplementary Fig. 3c). These results underscored the key role of the imidazole propionate/p38γ/mTORC1 pathway in imidazole propionate-induced neuronal toxicity.
a (Upper panel) Representative immunofluorescence images of S235/S236 phosphorylated S6 ribosomal protein (pS6) and TH in the ventral midbrain coronal sections from GF mice gavaged with Veh, S. mutans, or pasteurized S. mutans (P-S. mutans). pS6 signals originally captured in the red channel are pseudocolored in white for visualization. (Bottom panel) Quantification of relative pS6 signal intensities in TH-positive dopamine neurons of the SNpc (n = 7 mice per group). Scale bar = 100 μm. b (Upper panel) Representative immunofluorescence images of pS6 and TH in the ventral midbrain coronal sections from GF mice gavaged with E. coli (Con) or E. coli (urdA). Original red pS6 immunofluorescence signals are pseudocolored in white. (Bottom panel) Quantification of relative pS6 signal intensities in TH-positive dopamine neurons of the SNpc (n = 6 mice per E. coli (Con) and n = 7 mice per E. coli (urdA) group). Scale bar = 100 μm. c (Upper panel) Representative Western blots of pIRS1 (S636/S639), IRS1, pS6K1 (T389), and S6K1 in mouse primary cortical neurons treated with ImP (100 μM, 24 h) in the presence or absence of the mTORC1 inhibitor rapamycin (Rap, 20 nM, 24 h) or the p38γ inhibitor pirfenidone (Pirf, 1 mM, 24 h). (Bottom panel) Quantification of relative expression levels of pIRS1 (S636/S639) and pS6K1 (T389) (n = 4 per group). d Schematic illustration of the experimental procedure showing antibiotic cocktail treatment to sterilize the gut, cessation of antibiotics (Abx) treatment, and subsequent S. mutans colonization with or without rapamycin intraperitoneal (i.p.) injection. Fourteen days after colonization, mice were subjected to behavior tests and immunohistochemical analysis. Created in BioRender. Kim, J. (https://BioRender.com/yjm4i12). e, f Quantification of imidazole propionate (ImP) concentration in the plasma (e) and brains (f) from the antibiotic-treated mice colonized with S. mutans or Veh and treated with rapamycin (Rap, 4 mg/kg/day) or vehicle (n = 7 mice per Veh group, n = 8 mice per S. mutans group, n = 6 mice per S. mutans+Rap group). Box plots represent the median (centre line), 25%–75% quartile (bounds of box), minima and maxima (whiskers), with all individual data points shown. g (Upper panel) Representative immunofluorescence images of pS6 and TH in the ventral midbrain coronal sections from the antibiotic-treated mice colonized with S. mutans or Veh and administered with rapamycin or vehicle. Original red pS6 immunofluorescence signals are pseudocolored in white. (Bottom panel) Quantification of relative pS6 signal intensities in TH-positive dopamine neurons of the SNpc is shown below (n = 6 mice per group). Scale bar = 100 μm. SNpc and SNr subregions of the VM are indicated by the white dashed line. h (Left panel) Representative anti-TH immunohistochemistry of ventral midbrain coronal sections from the antibiotic-treated mice colonized with S. mutans or vehicle (Veh) and administered with rapamycin or vehicle. Magnified images showing dopaminergic processes in the SNr are presented on the right. (Right panel) Stereological counts of TH-stained and Nissl-stained dopamine neurons in the SNpc. Quantification of Nissl-stained neuronal counts and TH fiber density in the SNr of the indicated experimental groups (n = 5 mice per group). Scale bar = 100 μm, and 25 μm for enlarged images, respectively. i Inflammatory astrogliosis in the ventral midbrains of the indicated experimental antibiotic-treated mouse groups determined by anti-GFAP immunohistochemistry. Magnified images of the SNpc are shown below. Quantified % area fraction of GFAP signals is shown in the right panel (n = 5 mice per group). Scale bar = 100 μm. j Assessment of bradykinesia in the antibiotic-treated mice colonized with S. mutans or Veh and administered with rapamycin or vehicle monitored by measuring latency to reach the base in the pole test (n = 10 mice per Veh and S. mutans group, n = 9 mice per S. mutans+Rap group). Quantitative data are expressed as the mean ± S.E.M. *P < 0.05, **P < 0.01, ***P < 0.001; ns, not significant. P values were determined using one-way ANOVA with Tukey’s post hoc test (a, c, e–j) and unpaired two-tailed Student’s t-tests (b). Source data and test statistics are provided as a Source Data file. See also Supplementary Fig. 3.
To investigate whether mTORC1 inhibition can reverse gut-colonized S. mutans-induced PD pathology, we depleted the gut microbiome of C57BL/6 N mice by administering an antibiotic cocktail (Abx) via oral gavage twice daily for seven days (Fig. 3d). This method, as described previously10,21, effectively reduces the bacterial load (Supplementary Fig. 3d), as monitored by a colony formation assay with fecal samples. Starting on the 8th day, the antibiotic-treated mice were gavaged with S. mutans (109 CFU/mouse) daily for 14 days with or without an intraperitoneal injection of rapamycin (Fig. 3d). S. mutans was undetectable before (Pre-Abx) and seven days after antibiotic treatment (Post-Abx), but its levels markedly increased following colonization. Rapamycin did not affect S. mutans colonization efficiency, as demonstrated by absolute quantification of the S. mutans 16S rRNA gene (Supplementary Fig. 3e). These treatments did not affect body weight or cecal weight (Supplementary Fig. 3f, g). Interestingly, S. mutans-induced decrease in brain weight in the antibiotic-treated mice was reversed by rapamycin treatment (Supplementary Fig. 3h). Although antibiotic-treated mice exhibited higher plasma and brain imidazole propionate levels than GF mice (Figs. 1j, k and 3e, f), S. mutans colonization further increased these levels to ~400 nM (Fig. 3e). Similarly, brain imidazole propionate concentration increased robustly in antibiotic-treated mice colonized with S. mutans (Fig. 3f). Importantly, rapamycin treatment did not reduce the elevated levels of imidazole propionate induced by S. mutans in plasma and brain (Fig. 3e, f). Precursor urocanate levels were similar among all experimental groups and were not affected by S. mutans colonization or rapamycin treatment (Supplementary Fig. 3i, j). The increase in S6 and 4E-BP1 phosphorylation induced by S. mutans in the dopaminergic neurons of the substantia nigra was almost completely reversed by rapamycin treatment (Fig. 3g, Supplementary Fig. 3k), despite comparable elevations in imidazole propionate in the brain of S. mutans-colonized mice with or without rapamycin (Fig. 3f). In support of our hypothesis of mTORC1-dependent neurotoxicity, rapamycin treatment (mTORC1 inhibition) effectively prevented 4E-BP1 phosphorylation, dopaminergic neurodegeneration, astrogliosis, and microgliosis in the ventral midbrain, as well as the loss of dopaminergic processes in the substantia nigra reticularis and dopaminergic axon terminals in the striatum (Fig. 3h, i, and Supplementary Fig. 3k, l, m). Rapamycin also reversed motor dysfunction induced by S. mutans colonization in antibiotic-treated mice (Fig. 3j).
Gut-colonized S. mutans and imidazole propionate promote α-Syn preformed fibrils-induced mTORC1 activation, α-Syn aggregation, dopaminergic neurodegeneration, and motor impairments
PD is characterized by aberrant α-Syn aggregation in Lewy bodies and Lewy neurites22, and mTORC1 activation is implicated in α-Syn aggregation23, therefore, we investigated the potential interaction between imidazole propionate and α-Syn aggregation pathologies. We employed well-established PD neuron models in which α-Syn aggregation and neurotoxicity can be efficiently induced by introducing in vitro prepared α-Syn preformed fibrils (PFF)22. PFF was prepared as previously described24 and their amyloid conformation and aggregate formation were confirmed by Western blot and thioflavin T (ThT) fluorescence assays (Supplementary Fig 4a–c). Subsequently, PFF was sonicated into smaller fragments, and the pathogenic capacity of these sonicated PFF fragments was validated by the induction of pSer129-α-Syn-positive aggregates in primary cortical neurons (Supplementary Fig. 4d). Treatment of primary cortical neurons with a low dose of 0.1 μg/mL α-Syn PFF for seven days resulted in a trend of Lewy-like inclusions and Lewy neurites formation, enriched in pS129-α-Syn (Fig. 4a, b). Treatment with imidazole propionate potentiated the low-dose PFF-induced Lewy inclusion formation (Fig. 4a, b). Co-treatment with 1 μM imidazole propionate resulted in a significant elevation of pS129-α-Syn positive inclusions compared with PFF treatment alone (Fig. 4a, b). Additionally, nanomolar concentrations of imidazole propionate markedly increased neuronal toxicity, as evidenced by PFF-induced neurite fragmentation observed through MAP2 (neuronal markers) immunofluorescence (Fig. 4a, c). To quantitatively assess exacerbated α-Syn aggregation, we analyzed α-Syn levels in Triton X-100-soluble and -insoluble protein fractions by Western blotting. Treatment with 10 nM imidazole propionate in cortical neurons exposed to low-dose PFF led to a marked accumulation of α-Syn aggregates in the Triton X-100-insoluble fraction, indicating a pathological interaction between imidazole propionate and α-Syn seeding (Supplementary Fig. 4e).
a Representative immunofluorescence images showing the α-synuclein (α-Syn) aggregation marker S129 phosphorylated α-Syn (pS129-α-Syn) and neuronal marker microtubule-associated protein 2 (MAP2) in mouse primary cultured cortical neurons treated with the indicated combinations of ImP (1, 10, 100, 1000 nM every three days for six days) and α-Syn PFF (0.1 μg/mL treated once and incubated for seven days), counterstained with DAPI. Scale bar = 20 μm. b Quantification of relative immunofluorescence intensities of pS129-α-Syn in the indicated experimental groups (n = 4 per vehicle (DMSO) group, n = 3 per ImP group). c Assessment of neuronal viability in each experimental group, determined by counting MAP2-positive neuritic beads with a pathological phenotype of fragmentation (n = 4 per vehicle (DMSO) group, n = 3 per ImP group). d Schematic illustration of the experimental procedure showing antibiotic cocktail treatment to sterilize the gut, cessation of Abx treatment, and subsequent intranigral stereotaxic injections (inj.) of α-Syn PFF (10 μg in 2 μL) to model sporadic PD in mice followed by S. mutans colonization. Created in BioRender. Kim, J. (https://BioRender.com/x59j418). e Representative immunofluorescence images of pS6 and TH in the ventral midbrain coronal sections from the PBS-injected control or nigral α-Syn PFF-injected mice colonized with S. mutans or vehicle. Original red pS6 immunofluorescence signals are pseudocolored in white. Nuclei were counterstained with DAPI. Quantification of relative pS6 signal intensities in TH-positive dopamine neurons of the SNpc is shown in the right panel (n = 8 mice per group). Scale bar = 100 μm. f Lewy-like inclusions in the ventral midbrains of the PBS-injected control or nigral α-Syn PFF-injected mice colonized with S. mutans or vehicle, determined by anti-pS129-α-Syn (Lewy body marker) immunohistochemistry. Quantified % area fraction of pS129-α-Syn signals in the SNpc subregion is shown in the bottom panel (n = 6 mice per group). Scale bar = 100 μm, and 30 μm for enlarged images, respectively. g (Upper panel) Representative anti-TH immunohistochemistry of ventral midbrains from the indicated experimental mouse groups. Magnified images showing dopaminergic processes in SNr are also presented on the right. (Bottom panel) Stereological counts of TH-stained and Nissl-stained dopamine neurons in the lesioned hemisphere of the SNpc. Nissl-stained neuronal counts and TH fiber density in the SNr of the indicated experimental mouse group (n = 6 mice per group). Scale bar = 100 μm, and 25 μm for enlarged images, respectively. h Assessment of bradykinesia in the PBS-injected control or nigral α-Syn PFF-injected mice colonized with S. mutans or vehicle monitored by measuring latency to reach the base in the pole test (n = 8 mice per PBS-injected and PFF-injected group, n = 9 mice per PFF + S. mutans group). i Assessment of motor coordination in the indicated experimental mouse groups monitored by measuring latency to fall off in the accelerating rotarod test (n = 8 mice per PBS-injected and PFF-injected group, n = 9 mice per PFF + S. mutans group). Quantitative data are expressed as the mean ± S.E.M. *P < 0.05, **P < 0.01, ***P < 0.001; ns, not significant. P values were determined using one-way ANOVA with Tukey’s post hoc test. Source data and test statistics are provided as a Source Data file. See also Supplementary Fig. 4.
Therefore, we investigated whether gut-colonized S. mutans exacerbates PFF-induced α-synucleinopathy in vivo. After depleting the microbiome with antibiotics for seven days, 10 µg of PFF was stereotaxically injected into the substantia nigra to establish a sporadic PD mouse model with α-synucleinopathy25. Four h later, the mice were colonized with S. mutans daily for 21 days (Fig. 4d). Gut colonization by S. mutans significantly exacerbated the aggregation of insoluble α-Syn induced by nigral PFF injection (Supplementary Fig. 4f). In antibiotic-treated mice, PFF injection alone led to mTORC1 activation in TH-positive dopaminergic neurons in the substantia nigra (Fig. 4e, Supplementary Fig. 4g). This activation was further increased by S. mutans colonization (Fig. 4e, and Supplementary Fig. 4g). Similarly, there was a dose-dependent activation of mTORC1 by imidazole propionate in primary cortical neurons seeded with α-Syn PFF, indicated by a gradual increase in S6K1 phosphorylation (Supplementary Fig. 4h). Furthermore, nigral PFF injection into antibiotic-treated mice led to modest formation of Lewy-like inclusions, which were markedly enhanced by S. mutans colonization (Fig. 4f). In line with these findings, PFF-induced dopaminergic neurodegeneration (Fig. 4g), loss of dopaminergic fibers (Fig. 4g, and Supplementary Fig. 4i), astrogliosis, microgliosis (Supplementary Fig. 4j, k), and motor deficits [assessed by the pole test (Fig. 4h) and rotarod test (Fig. 4i)] in antibiotic-treated mice were significantly aggravated by S. mutans colonization. This rapid onset of PFF-induced PD is unusual compared to the typical ~3 months incubation period required for dopamine cell loss in wild-type mice25. This rapid progression might be associated with gut sterilization by antibiotics, as the same PFF dose and treatment duration in non-antibiotic-treated mice did not result in dopaminergic neuron loss, despite a modest increase in pS129-α-Syn levels (Supplementary Fig. 4l, m). Taken together, these findings suggest that gut-colonized S. mutans and potentially its metabolite imidazole propionate can worsen pre-existing α-synucleinopathy and its related pathologies in PD via mTORC1 activation.
Imidazole propionate contributes to selective dopaminergic neurotoxicity through mTORC1 activation
Given that imidazole propionate is not the sole metabolite produced by S. mutans, we sought to determine whether imidazole propionate alone induces PD pathology in vivo. To evaluate its ability to cross the blood–brain barrier and distribute across different brain regions, we first administered imidazole propionate systemically via intraperitoneal injection of either vehicle or imidazole propionate for three days, a dosage shown to induce nanomolar blood concentrations14. This treatment increased imidazole propionate levels to approximately three pmole/mg in the brain (Supplementary Fig. 5a), without affecting the concentration of its precursor urocanate (Supplementary Fig. 5b), therefore, confirming the penetrability of this metabolite through the blood-brain barrier.
Consistent with the observations in S. mutans-colonized mice, systemic administration of imidazole propionate for 21 days led to mTORC1 activation (Fig. 5a, and Supplementary Fig. 5c), TH-positive dopaminergic neuron reduction in the substantia nigra pars compacta (Fig. 5b), motor dysfunction (Fig. 5c, d), and astrogliosis (Supplementary Fig. 5d). Additionally, the density of TH-positive dopaminergic axon terminals decreased in the striatum of mice administered with systemic imidazole propionate compared to those in the vehicle control (Supplementary Fig. 5e). However, the Nissl-stained neuronal counts in several hippocampal subregions, including the dentate gyrus, CA1, and CA3, were similar between the control and imidazole propionate-treated groups (Supplementary Fig. 5f), consistent with the lack of impairment in cognitive function and spontaneous exploratory activities assessed by the Barnes maze and open field tests, respectively (Supplementary Fig. 5g, h). Although imidazole propionate efficiently penetrated the hippocampus (Supplementary Fig. 5a), it did not cause neuronal death in this region (Supplementary Fig. 5f). This suggests that brain pathologies induced by imidazole propionate are specific to midbrain dopaminergic neuron, although further studies are warranted to evaluate potential long-term effects.
a Schematic illustration of the experimental procedure showing systemic intraperitoneal (i.p.) administration of ImP (20 μg per mouse for three weeks). Created in BioRender. Kim, J. (https://BioRender.com/32jcwkt). b Representative anti-TH immunohistochemistry (Nissl counterstained) of ventral midbrain coronal sections from mice injected with ImP or vehicle (1% DMSO, Veh). Magnified images showing dopaminergic processes in the SNr are also presented on the right. Stereological counting of TH-positive dopaminergic neurons in the SNpc of each experimental mouse group is shown in the right panel (n = 5 mice per Veh group, n = 4 mice per ImP group). Scale bar = 400, and 100 μm for enlarged images, respectively. c, d Pole assessment of bradykinesia phenotype (c) and rotarod assessment of motor coordination (d) in mice injected with ImP or vehicle (1% DMSO) (n = 5 mice per Veh group, n = 4 mice per ImP group). e Schematic illustration of the experimental procedure showing intranigral stereotaxic injection of ImP (single injection of 7 μg of ImP in 2 μL) where rapamycin was injected intraperitoneally one day before ImP injection at 1 mg/kg per mouse daily for a total of four days. Created in BioRender. Kim, J. (https://BioRender.com/rxfm6ng). f Representative immunofluorescence images of pS6 and TH in the ventral midbrain coronal sections from mice with intranigral brain injections of PBS or ImP with or without mTORC1 inhibitor, rapamycin. Original red pS6 immunofluorescence signals are pseudocolored in white. Quantification of relative pS6 signal intensities in TH-positive dopamine neurons of the SNpc is shown in the right panel (n = 7 mice per group). Scale bar = 100. SNpc and SNr subregions of the VM are indicated by the white dashed line. g (Upper panel) Representative anti-TH immunohistochemistry images of ventral midbrains from mice with nigral ImP or PBS injections with or without rapamycin treatment. Magnified images showing dopaminergic processes in the SNr are also presented on the right. (Bottom panel) Stereological counts of TH-stained and Nissl-stained dopamine neurons in the lesioned hemisphere of the SNpc. Nissl-stained neuronal counts and TH fiber density in the SNr of the indicated experimental mouse group (n = 5 mice per group). Scale bar = 100 μm, and 50 μm for enlarged images, respectively. h Inflammatory astrogliosis in the ventral midbrains of the indicated experimental mouse groups determined by anti-GFAP immunohistochemistry. Quantified % area fraction of GFAP signals is shown below (n = 7 mice per group). Scale bar = 100 μm. i, j Pole assessment of bradykinesia (i) and rotarod assessment of motor coordination (j) in the indicated experimental groups (n = 7 mice per group). k Measurement of ImP concentrations in the plasma samples from patients with PD (n = 65) and age-matched neurologically healthy control participants (n = 65). Data transformed to log10 scale and presented as box plots show minimum, 25% quartile, median, 75% quartile, maximum. Quantitative data are expressed as the mean ± S.E.M. *P < 0.05, **P < 0.01, ***P < 0.001; ns not significant. P values were determined using unpaired two-tailed Student’s t-tests (b–d), two-way ANOVA with Tukey’s post hoc test (f–j), and two-sided Wilcoxon rank-sum tests (k). Source data and test statistics are provided as a Source Data file. See also Supplementary Fig. 5.
To further confirm the direct pathogenic effects and molecular mechanism of imidazole propionate on midbrain dopamine neurons, we stereotaxically injected this metabolite into the substantia nigra of mice brains (Fig. 5e). Three days post-injection, we observed mTORC1 activation (Fig. 5f, and Supplementary Fig. 5i), and robust dopaminergic neurodegeneration in the substantia nigra pars compacta and striatum of mice injected with imidazole propionate (Fig. 5g, Supplementary Fig. 5j). This imidazole propionate-induced neurotoxicity appeared to selectively affect dopamine neurons (Fig. 5g), as Nissl-stained neurons in the substantia nigra reticularis remained unaffected (Fig. 5g). Along with mTORC1 activation and dopamine neuron loss, acute brain injection of imidazole propionate resulted in marked astrogliosis and microgliosis (Fig. 5h, and Supplementary Fig. 5k) and severe motor deficits (Fig. 5i, j), similar to those induced by gut-colonized S. mutans or systemic imidazole propionate administration. These brain-injected imidazole propionate-induced pathologies were partially inhibited by rapamycin treatment (Fig. 5f–j). Taken together, our findings suggest a pathological role for gut-derived microbial imidazole propionate in selective dopaminergic neuronal loss in PD, partly mediated by the mTORC1 pathway.
Imidazole propionate levels are elevated in individuals with PD
Our observations indicated that microbial imidazole propionate can represent a contributing factor to PD development. To further explore this, we measured imidazole propionate concentrations in the plasma of 65 individuals with PD (mean disease duration: 9.5 years) and 65 age- and sex-matched neurologically healthy participants (Supplementary Table 1). Individuals with type 2 diabetes exhibited elevated imidazole propionate levels compared with those with normal glucose tolerance14. However, in our cohort, only six patients had type 2 diabetes (Supplementary Table 1), minimizing the potential contribution of this condition to imidazole propionate levels in patients with PD. Our results revealed significantly higher levels of imidazole propionate in individuals with PD than those in neurologically healthy, age-matched controls (Fig. 5k). These findings suggested a potential association between microbial imidazole propionate and PD development in humans.
Discussion
A previous pioneering study has established a causal role of the gut microbiome and its metabolite SCFAs in promoting α-Syn-induced pathologies, including brain-resident microglia activation and motor deficits5. However, evidence suggests that SCFAs have neuroprotective, rather than neuroinflammatory, effects26,27,28,29. Importantly, there are no reports of microbial metabolites that induce selective midbrain dopaminergic neurotoxicity, which is a key feature of PD. This study is the first to demonstrate the pivotal role of the gut microbial enzyme, UrdA and its metabolite, imidazole propionate, in PD pathology.
We provide evidence that imidazole propionate not only penetrates the brain but also serves as a potential direct mediator of the gut-brain axis. We showed that microbial imidazole propionate promoted pre-existing α-Syn aggregation and neurotoxicity. Consistent with this, we observed unexpectedly rapid pathological progression—marked by significant α-Syn aggregation, dopaminergic neuron loss, and motor deficits as early as three weeks after nigral PFF injection. This progression was further exacerbated by gut colonization with S. mutans. This timeline is markedly shorter than the typical 3–6 month incubation period required to induce comparable pathology in wild-type mice25,30,31. We propose that this acceleration may be partly due to antibiotic-induced depletion of the gut microbiota, which is known to compromise blood–brain barrier integrity32, thereby increasing neuronal vulnerability and inflammatory responses. Supporting this, PFF-injected SPF mice that did not receive antibiotics failed to exhibit dopaminergic cell loss or Lewy pathology at the same early time point, aligning with findings from previous studies. These results highlight the potential influence of microbiome status on both the timing and severity of α-Syn pathology in vivo.
Intriguingly, unlike SCFAs, imidazole propionate alone was sufficient to activate dopaminergic mTORC1, induce neurodegeneration specifically in midbrain dopaminergic neurons, and resulted in motor dysfunction. Moreover, the ability of SCFAs to induce α-Syn-mediated neuroinflammation by crossing the blood-brain barrier remains unclear. In this context, imidazole propionate may be one of the first brain-permeable gut-derived microbial metabolites directly implicated in neurodegeneration. However, further research is needed to reveal how this metabolite specifically induces midbrain dopaminergic neurotoxicity and whether it contributes to neuroinflammation. While our current data demonstrate astrogliosis and microgliosis, they do not fully support a definitive claim of neuroinflammation. Additional analyses such as cytokine profiling will be necessary to determine whether the observed gliosis reflects a broader neuroinflammatory response. This represents an important direction for future investigation.
The midbrain-specific pathology may be explained by selective mTORC1 activation within dopaminergic neurons of the substantia nigra pars compacta, without affecting non-dopaminergic neurons in the substantia nigra reticularis or neurons in the cortex. While midbrain dopaminergic neurons appear particularly vulnerable, it remains possible that imidazole propionate also exerts pathogenic effects in other brain regions. Indeed, we observed a synergistic interaction between imidazole propionate and α-Syn seeds in cortical neurons, suggesting that imidazole propionate may facilitate α-Syn pathology formation and propagation beyond the dopaminergic system, implicating it in non-dopaminergic neuronal populations. Building on these findings, future studies should aim to further characterize both motor and non-motor consequences of imidazole propionate and S. mutans colonization. This includes incorporating additional motor assessments, such as the rotarod and narrow beam walking tests, to validate motor impairments, Furthermore, a broader range of behavioral paradigms should be employed to evaluate non-motor symptoms associated with PD (e.g., depression, olfactory deficits, cognitive impairment, anxiety, and constipation) following α-Syn PFF injections into relevant brain regions.
Considering the increased risk of developing PD in individuals with diabetes and the association of this condition with increase in PD severity33, it is plausible that microbial imidazole propionate serves as a potential link between diabetes and PD. This hypothesis is based on our previous findings regarding its role in diabetes14. Based on the recent report demonstrating the interaction between p38γ and α-Syn and the translocation of p38γ to neuronal cell bodies in patients with dementia with Lewy bodies and PD34, the reversal of imidazole propionate-induced neurotoxicity by the p38γ inhibitor pirfenidone suggests a potential therapeutic option for individuals with elevated imidazole propionate levels and consequently high risks of diabetes and PD.
Furthermore, the ongoing development of a bacterial UrdA inhibitor presents a potential therapeutic avenue to limit gut production of the dopaminergic neurotoxic imidazole propionate, based on our observation that UrdA expression in a UrdA-deficient bacterial strain colonized in the gut was sufficient to induce PD-related pathology. However, because we expressed UrdA in an E. coli strain that does not naturally harbor this enzyme, we cannot exclude the possibility that plasmid carriage may impose a fitness cost and alter bacterial physiology independently of imidazole propionate production. Future studies using S. mutans deficient in UrdA will help disentangle these potential confounding effects. Nonetheless, administration of imidazole propionate alone recapitulated the phenotypes observed with either S. mutans or E. coli expressing UrdA from S. mutans, supporting its role as a key driver of the observed effects.
In this study, we evaluated blood and brain imidazole propionate concentrations and their association with PD-related pathology in mice. The clinical association between high urdA gene levels, blood imidazole propionate levels, and PD was also demonstrated. A more accurate assessment of PD risk may be achieved by the combined evaluation of gut microbial urdA gene levels, UrdA-producing bacterial abundance, and blood imidazole propionate concentration as molecular and cellular PD biomarkers. Longitudinal PD cohort studies will be necessary to determine whether the UrdA-imidazole propionate axis serves as a risk factor for α-Syn pathology or a disease-promoting factor, which was not directly investigated in the current study. Overall, our findings underscore the critical role of the gut-derived microbial imidazole propionate as a key mediator in PD pathology and indicated potential therapeutic options targeting the gut-brain axis (Fig. 6).
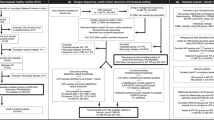
The graphical abstract illustrates that the UrdA-ImP axis is elevated in the gut microbiome of patients with Parkinson’s disease (PD). Using mouse models, we show that this contributes causally to PD pathology through mTORC1 activation. These findings identify UrdA as a potential gut microbiome–based therapeutic target for gut-brain axis disorders such as PD. Created in BioRender. Kim, J. (https://BioRender.com/vg7s2sy).
Methods
Experimental Model and Subject Details
Mice
All animal experiments were conducted in compliance with the ethical guidelines approved by the Ethical Committee of Sungkyunkwan University Animal Care (approval number: SKKUIACUC2023-04-09-1) and the Institutional Animal Care and Use Committee (IACUC) at the POSTECH Biotech Center. Eight-week-old male germ-free (GF) and specific pathogen-free (SPF) C57BL/6 N mice were used in the experiments. GF mice were housed in flexible film isolators with a strict 12-h light cycle and had unlimited access to water and food (Chow diet, Purina #38057). GF status was regularly assessed using aerobic and anaerobic fecal bacterial cultures. Male C57BL/6 N mice, aged two months, were procured from Orient Bio (Suwon, Korea) for additional experiments. Animal numbers were minimized to adhere to ethical standards and to minimize discomfort.
Human subjects
The participants in this study were recruited from the Movement Disorders Clinic at Seoul National University Hospital (SNUH), comprising a total 130 participants (Table S1). Among them, 65 patients had PD and 65 were age-matched healthy controls. Patients with PD were followed up for an average of 9.5 years after sampling to ensure the reliability of the diagnosis. PD was diagnosed based on the clinical diagnostic criteria of the Movement Disorders Society35. Participants in the control group, who were free of PD, were enrolled from the SNUH biorepository and predominantly spouses sharing living environments with patients with PD. The study protocol was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. 2207-085-1340), which waived the requirement for informed consent.
Mouse primary cortical neurons
The Institutional Animal Care and Use Committee of Sungkyunkwan University approved the use of the primary mouse cortical neuronal cultures (approval number: SKKUIACUC2022-07-41-1). Fetal cortex tissue was obtained from ICR mice (15–16 days of gestation) purchased from Orient Bio Animal Company (Suwon, Korea). Upon isolation, the cortex tissue was incubated in 1 × trypsin EDTA (0.05%) for 20 min at 37 °C, followed by washing with 1 × MEM. The trypsinized tissue was then filtered through a 40-μm cell strainer (Falcon #352340), and the resulting neuron mixture was plated on a coated 12-well culture plate. Neuronal cultures were maintained by changing the medium every 3–4 days. Drug treatments and validation experiments were conducted after nine days of culture.
Method details
Gene abundance analysis in the gut metagenome
Raw whole-genome shotgun sequences of patients with PD and neurologically healthy elderly controls were obtained from BioProject ID PRJNA834801 (https://www.ncbi.nlm.nih.gov/bioproject/834801). Individual deep-shotgun metagenomic sequences from 491 individuals with PD and 234 neurologically healthy elderly individuals were used for further metagenomic analysis. To ensure data quality, the Nextera XT adapter and PhiX genome contamination were removed using BBDuk with the following parameters: ‘ftm=5 tbo tpe qtrim=rl trimq=25 minlen=50 ref=adapters,phix’. Subsequent reads were aligned to the human reference genome (GRCh38.p14, latest version) using BBSplit with the default parameters to remove human contamination. Species-level metagenomic functional analysis was conducted using HUMAnN336 with default parameters to profile the functional gene content. The resulting gene counts based on UniRef90 (v201901b) and ChocoPHLAn (v30) were converted into Kyoto Encyclopedia of Genes and Genomes (KEGG) orthologs (KO). K01745(histidine ammonia-lyase, EC:4.3.1.3) was quantified to determine the abundance of hutH.
We examined the abundance of urdA involved in imidazole propionate production as described previously14,37. Briefly, 12,319 non-redundant urdA candidate sequences were identified from 557,951,640 protein-coding genes from the NCBI bacterial genomes (assessed in February 2019). Exact read mapping was performed, focusing on gene regions within 90 nucleotides upstream and downstream of the FAD active sites of urdA, using Bowtie 238 with no mismatches or gap openings. Only samples with at least 10 mapped reads and a mapping length exceeding 100 bp were included to ensure coverage of active sites. In total, 207 samples from the control cohort (out of 234 samples) and 454 samples from patients with PD (out of 491 samples) were included in the urdA abundance calculation after undergoing quality control (FASTX-Toolkit) and human decontamination (hg19). The sequencing depth in each sample was normalized to the total mapped reads to distinguish between true and false urocanate reductases based on the amino acid at position 373, which was previously identified as true urdA activities14,39.
Gene counts from Uniref90 (v201901b) and ChcoPHLAN (v30) were used to quantify the abundance of Streptococcus mutans urdA (UniRef90_Q8DW88) and Streptococcus mitis, S. oralis, and S. parasanguinis urdA (UniRef90_F8DIF2).
Taxonomic profiling
Quality-controlled whole-genome shotgun sequences of patients with PD and neurologically healthy elderly controls were analyzed using MetaPhlAn 4 (v4.0.6, mpa_vOct22) with default parameter (-t rel_ab –unknown-estimation). Multivariable association between clinical metadata and microbial features were assessed using relative abundances in downstream analyses with MaAsLin240 and ANCOM-BC41. Only species present in >5% of samples with a relative abundance >0.05% were considered in differential abundance analysis.
Streptococcus mutans culture and pasteurization
Streptococcus mutans (ATCC 25175) was cultured overnight at 37 °C under anaerobic conditions in brain-heart infusion (BHI) broth supplemented with yeast extract (5 g/L), cellobiose (1 g/L), maltose (1 g/L), L-cysteine (0.5 g/L), and hemin (0.01 g/L), referred to as LYBHI medium. The overnight cultures were reinoculated at a 1:100 dilution the following day to yield consistent colony-forming units (CFU). The starter culture was incubated for six hours, reaching an OD620 of 0.8–0.9 (~5 × 108 CFU/mL). Subsequently, S. mutans cells were harvested by centrifugation and washed once with PBS. For pasteurization, cultures were heat-killed at 75 °C for 2 h with intermittent shaking. After pasteurization, the cells were centrifuged and washed twice with PBS. Viability post-pasteurization was assessed by plating on LYBHI medium and incubating under anaerobic conditions at 37 °C for one week. Pellets were stored at −80 °C and resuspended with PBS immediately before oral gavage.
Engineering and cultivation of Escherichia coli for heterologous overexpression of S. mutans urdA
The urocanate reductase (urdA) gene was amplified from Streptococcus mutans genomic DNA using PCR. Genomic DNA was extracted using the QIAamp DNA mini kit (QIAGEN, 51306), and PCR was performed with PrimeSTAR HS DNA polymerase (Takara, R010A) using primers (forward: 5’-GTGTGTCGACATGAAATTAATTGCTAT-3’, reverse: 5’- GTGTGGTACCTTAGCAGCATTCTGTTAC-3’) incorporating restriction sites for cloning. The PCR product and pUC19 vector were digested with KpnI (NEW ENGLAND Biolabs, R3142) and SalI (NEW ENGLAND Biolabs, R0138) and ligated for heterologous expression in Escherichia coli. The recombinant plasmid was transformed into E. coli MG1655 (ATCC 700926) using the heat shock method and selected on LB agar plates containing 100 μg/ml ampicillin. As a control, E. coli MG1655 carrying an empty pUC19 vector (NEW ENGLAND Biolabs, N3041S) was prepared using the same procedure. The subcloned E. coli was cultured overnight at 37 °C under anaerobic conditions in LB broth supplemented with ampicillin. The following day, the overnight culture was reinoculated at a 1:100 dilution to ensure consistent colony-forming units (CFU). The starter culture was incubated for 6 h, reaching an OD620 of 0.1–0.2 (~5 × 10⁷ CFU/mL). Subsequently, the cells were harvested by centrifugation, washed once with PBS, and administered via oral gavage.
Streptococcus mutans and Escherichia coli MG1655 colonization in the gut
We used antibiotic (Abx) cocktail-treated mice or GF mice for the colonization of S. mutans in the gut, respectively. Specifically, SPF C57BL/6 mice were administered a cocktail of neomycin (Sigma Aldrich, N6386, 100 mg/kg), metronidazole (Sigma Aldrich, M1547, 100 mg/kg), and vancomycin (Sigma Aldrich, V2002, 50 mg/kg) via oral gavage twice daily for seven days. Ampicillin (Sigma Aldrich, A9518, 1 mg/mL) was provided ad libitum in drinking water for seven days. Starting on the 8th day, S. mutans (109 CFU/mouse) was administered via oral gavage daily for 14 days with or without an intraperitoneal injection of rapamycin (4 mg/kg) every two days. GF C57BL/6 mice maintained in sterile flexible film isolators were orally gavaged with S. mutans (109 CFU/mouse) for 28 days (three gavages in total). PFF-induced C57BL/6 mice sterilized by antibiotic cocktail administration for seven days by injecting PFF (10 μg) into substantia nigra pars compacta (SNpc) (L: 1.2, AP: −3.4, DV: −4.3 mm). S. mutans was administered daily via oral gavage for three weeks. For E. coli colonization, GF C57BL/6 mice maintained in sterile flexible film isolators were orally gavaged with E. coli (109 CFU/mouse) every two days to enhance colonization efficiency and improve reproducibility, due to the instability of ectopically expressed plasmids. This repetitive gavage approach was adapted from similar protocols used in previous studies42,43,44. Potential contamination was routinely monitored during and at the end of the colonization period using universal 16S rRNA primers and taxa-specific primers.
Viability assessment of Streptococcus mutans and E. coli after colonization
The viability of S. mutans and E. coli MG1655 in the gut was assessed by quantifying the CFU in fecal and gut mucosal samples. Mucosal samples were obtained from distinct intestinal segments including the jejunum, ileum, cecum, and colon. Each section, except for the cecum, was opened longitudinally and the mucosal surface was scraped with forceps. Phosphate buffered saline (PBS) was used to ensure sufficient sample collection, followed by centrifugation to remove excess PBS. Pellets were then stored at –80 °C before quantification. Fecal and cecal samples were promptly frozen in liquid nitrogen and stored at –80 °C prior to quantification. These samples were then transferred into an anaerobic chamber and resuspended in 200 µL of sterile PBS. Serial dilutions were prepared for each sample and plated either on LYBHI agar plates for S. mutans or LB agar plates for E. coli. After overnight incubation, viable colonies were counted.
Absolute quantification
Primer sequences for S. mutans used in this study have been described previously45. Sm479F: 5′-TCGCGAAAAAGATAAACAAACA-3′ and Sm479R: 5′-GCCCCTTCACAGTTGGTTAG-3′. To quantify S. mutans 16 s rDNA copies, a 479 bp DNA sequence in the 16S rDNA region was amplified using nTaq HOT polymerase (Enzynomics, P750) and ligated into the T vector (Biofact, VT202-020) as a template. Genomic DNA was extracted from fecal and gut mucosal samples using the QIAamp DNA Mini Kit (Qiagen, 51306) and quantified by qPCR using the QGreenBlue Master Mix (Low ROX) (Cellsafe, QBLR). A standard curve was generated from a ten-fold serial dilution of the T vector containing the S. mutans-specific 16S rDNA fragment, allowing the precise quantification of bacterial DNA in the samples. The 16S rDNA copies were calculated by normalizing the copies to the total input weight of the gut sample for DNA extraction.
Systemic and intranigral injection of imidazole propionate
For systemic administration, mice received intraperitoneal injections of 20 μg of imidazole propionate dissolved in 200 μL of water containing 1% DMSO, or an equivalent volume of vehicle (1% DMSO in water) daily for 21 days. To assess the direct effects of imidazole propionate (ImP) on the brain, a separate experiment involved injecting 7 μg of ImP directly into the substantia nigra pars compacta (SNpc) at coordinates L: 1.2 mm, AP: –3.4 mm, DV: –4.3 mm relative to bregma. Rapamycin, an mTORC1 inhibitor, was administered intraperitoneally at 1 mg/kg/day, starting four times the day before SNpc injection, to evaluate its impact on the observed effects.
Metabolite analysis
Human blood samples (n = 130) were collected from the venous blood of the participants during visits. Plasma was obtained by centrifugation and stored at –80 °C until analysis. For the targeted measurement of imidazole propionate, plasma samples were extracted with six volumes of ice-cold acetonitrile containing 100 nM internal standards (urocanate-13C3) in a 1.5-mL polypropylene tube. After vortexing and centrifugation, the supernatant was dried under a nitrogen flow. The dried samples were reconstituted with 5% HCl (37%) in 1-butanol at 70 °C for 1 h and then dried under nitrogen to form n-butyl esters. After derivatization, samples were evaporated and reconstituted in 120 µL water: acetonitrile (9:1). Samples (5 µL) were injected onto a C18 BEH column (2.1 × 50 mm with 1.7 μm particles; Waters, Milford, MA) and separated using a gradient consisting of water with 0.1% formic acid (A-phase) and acetonitrile with 0.1% formic acid (B-phase). Mass spectrometric analysis was conducted using an LX50 Qsight 220 system (Perkin Elmer, Milan, Italy), with imidazole propionate detected by multiple reaction monitoring (MRM) using transitions 197/81. Internal standards were monitored using transitions between 198/95. Calibration curves for imidazole propionate were prepared in methanol and treated similarly to those of the samples.
For imidazole propionate and urocanate measurements in the mouse experimental groups, whole brain samples were prepared by intracardiac perfusion to remove blood from the brain, whereas plasma samples were collected directly from the heart. Depending on tissue size, 10–100 mg of snap-frozen brain tissue was homogenized in 500 µL of methanol containing 100 nM internal standards (imidazole propionate-13C3 and urocanate-13C3) in 1.8-mL polypropylene tubes with ceramic beads. After centrifugation, the supernatant was evaporated under nitrogen and reconstituted with 5% HCl (37%) in 1-butanol before n-butyl ester derivatization. Samples were evaporated again and reconstituted in 150 µL of water:acetonitrile (9:1). Plasma samples from C57BL/6 N GF and SPF mice were extracted with five volumes of ice-cold acetonitrile in 1.5-mL polypropylene tubes. After drying the eluates, the samples were reconstituted as described above. After derivatization, the samples were evaporated and reconstituted in 180 µL of water:acetonitrile (9:1). Samples (5 µL) were then injected and separated as described above. Quantification of imidazole propionate and urocanate was performed via ultra-high-performance liquid chromatography coupled with tandem mass spectrometry (UHPLC-MS/MS) using MRM transitions 197/81 for imidazole propionate and 195/93 for urocanate. Internal standards were monitored using transitions between 198/95. Calibration curves for imidazole propionate and urocanate were prepared in methanol and treated identically to the samples for quantification.
Preparation and quality control of α-synuclein preformed fibrils
Preparation of α-synuclein preformed fibrils (α-Syn PFF) followed the standardized protocol outlined in a previous study24. In summary, recombinant mouse α-synuclein was incubated in PBS with continuous agitation at 1000 rpm and 37 °C using a thermomixer (ATTO WSC-2630, Tokyo, Japan) for seven days to induce fibril formation. The resulting α-Syn aggregates were diluted to a final concentration of 0.1 mg/mL in PBS and sonicated for two minutes at 20% amplitude (1-second pulse on/off, with cooling on ice for 1 minute after every 15 pulses) using a VCX130 sonicator (Sonics & Materials Inc., Newtown, CT). The quality of the recombinant α-Syn protein was assessed by measuring endotoxin levels (Thermo Scientific, cat#88274). 0.013 EU/ml of purified α-Syn PFF was used in this study, adhering to recommended endotoxin thresholds of 0.5 EU/ml according to the guideline from the Michael J. Fox Foundation). Aggregation was verified using a Thioflavin T (ThT) assay and Western blot analysis. Additionally, the pathogenic potential of the sonicated α-Syn PFF was confirmed through functional assays in cultured cortical neurons, demonstrating pS129-αSyn-positive Lewy-like inclusion formation.
Stereotaxic nigral injection of imidazole propionate or α-Syn PFF
For stereotaxic administration of sonicated α-synuclein preformed fibrils (α-Syn PFF, 10 µg), C57BL/6 N mice, aged 2 months and pre-treated with an antibiotic cocktail for seven days, were anesthetized using pentobarbital (60 mg/kg). The stereotaxic injection into the substantia nigra was conducted following a previously established protocol24. In brief, a 26.5-gauge injection cannula was positioned stereotaxically at the substantia nigra (anteroposterior: −3.4 mm from bregma; mediolateral: ± 1.2 mm; dorsoventral: −4.3 mm). The α-Syn PFF solution was infused at a controlled rate of 0.2 µL/min, delivering a total of 2 µL per mouse (5 µg/µL α-Syn PFF in sterile PBS). To ensure adequate tissue absorption, the injection cannula was left in place for an additional five minutes before being carefully withdrawn. Following removal, the incision was sutured, and postoperative recovery and wound healing were monitored daily. Administration of S. mutans (109 CFU/200 µL/mouse via oral gavage) commenced the day after α-Syn PFF injection and continued for three weeks. For subsequent immunohistochemistry and stereological analysis, animals underwent intracardiac perfusion with ice-cold PBS, followed by fixation with 4% paraformaldehyde. Brains were extracted, cryoprotected in 30% sucrose, and processed for microtome sectioning and immunohistochemical analysis.
Immunohistochemistry and TH stereological cell counting
Coronal sections of the fixed and cryoprotected brains, including the substantia nigra or striatum, were cut at a thickness of 35 µm. Sections were incubated with rabbit antibodies against TH (immunostar Cat#22941), GFAP (abcam, Cat#ab7260) and Iba1 (Wako chemicals USA, Cat# 019-19741) at a 1:1000 dilution (Novus Biologicals). Subsequently, the sections were indicated with biotinylated rabbit IgG and streptavidin-linked HRP using a Vectastain ABC kit (Vector Laboratories). The HRP substrate 3,3-diaminobenzidine (DAB, cat# D4293, Sigma-Aldrich) was used to visualize TH-positive cells. Slide-mounted sections were stained with cresyl violet (Abcam, cat# AB246816) for Nissl staining to assess neuronal viability. Immuno-stained and Nissl counterstained coronal brain sections were examined using a Zeiss Axio Imager. M2 microscope stand with a motorized Z-drive and TFT monitor (Carl Zeiss Microscopy, LLC, catalog number 430004-9902-000), equipped with a motorized stage. The total numbers of TH-positive dopaminergic neurons and Nissl-stained neurons in the specified brain subregions were determined using the Optical Fractionator probe in Stereo Investigator software (version 11.06.100, MBF Bioscience, Williston, VT, USA). All counting was performed in a manner blinded to mouse treatments. For stereotaxic injection experiments (Fig. 4g, Fig. 5g, and Supplementary Fig. 4k), the TH and Nissl dopaminergic cell counts were determined for one hemisphere of mouse brains. The percentage area fraction of GFAP-positive reactive astrogliosis and Iba1-positive reactive microgliosis staining was measured respectively within rectangular regions of interest (ROIs) using semi-automated image analysis software, ImageJ. Microglial soma size was measured as described previously46. Images were first converted to 8-bit grayscale, and the scale was calibrated using the pixel-to-micrometer ratio. Microglial somata were segmented by applying an appropriate intensity threshold, and the area of each soma was automatically measured using the ‘Analyze Particles’ function in ImageJ. To exclude noise and non-specific signals, a minimum particle size threshold was set during analysis.
For immunofluorescence labeling, coronal ventral midbrain or striatum sections were blocked (5% goat serum, 1 × PBS, 0.2% Triton-X) for 1 h. The brain sections were incubated with the primary antibody against TH, phospho-S6 (Cell signaling Cat#4858) and phospho-4E-BP1 (Cell signaling Cat#2855) for overnight at 4 °C, fulfilled by incubation in PBS, including fluorescent-labeled secondary antibodies. Fluorescent images were obtained using a fluorescence microscope (Axiovert 200 M; Carl Zeiss).
Behavioral test
Pole test
A bandaged metal rod of 10-mm diameter and 58-cm length was used to perform the pole tests. The mice were allowed to acclimate to the cage for at least 5 min before the test. Once adapted, the mice were placed facing downward at the end of the pole. The time required for the animal to descend the pole and place its forefoot on the floor was recorded. The average duration of the three trials was calculated.
Rotarod test
The mice were trained to walk on a rotarod for two days before the trial. On the third day of the test, the mice were positioned on an accelerating cylinder, while the time taken to fall off and speed at which they fell off were recorded. The speed was gradually increased from 4 to 40 rpm within a 5-minute time frame. The trial ended when the mice fell off the rotarod.
Barnes maze
The testing phase lasted for five days and consisted of two daily trials. Following the two-hole explorations, the mice were gently led to an escape hole and left in a recessed chamber for 90 s. During each test trial, the mouse was placed in the center of the maze and allowed to explore spontaneously for a maximum of 5 min or until an escape hole was discovered. When the mouse failed to locate the escape hole within 5 min, it was guided to it and remained in the recessed chamber for 1 min. The time taken to reach the escape hole location was also recorded.
Open field test
The square box for the open field was divided into 64 equal areas, including the border, peripheral, and central areas. The central region consisted of four central squares (2 × 2), whereas the peripheral area consisted of 12 squares surrounding the central region. The remaining squares represented border areas. Mice were placed in the center of the box and allowed to explore for 15 min. After each test, the open field was cleaned with 70% ethanol. The Smart software (v3.0) was used to measure the locomotor activity by recording the distance traveled, and the time spent at the center was used to indicate anxiolytic behavior.
Imidazole propionate and α-Syn PFF treatment in primary cortical neurons
The isolation and culture of primary cortical neurons from mice were conducted as previously described47. One day prior to cell seeding, culture plates were coated with poly-L-lysine (PLL) and glass coverslips, washed the following day, and exposed to UV light for one h to ensure sterility. Pregnant ICR mice (15 days of gestation) were obtained from Orient Bio (Seongnam, Korea), and fetal brains were harvested. Only the cortical region was dissected for further processing. The excised cortical tissue was incubated in 0.05% trypsin-EDTA at 37 °C for 20 min to facilitate dissociation. Following enzymatic digestion, the tissue was rinsed with MEM, and the cell suspension was filtered using a 40-µm cell strainer (Falcon, cat#352340). The dissociated neurons were then seeded onto the pre-coated 12-well culture plates and maintained with periodic medium changes every 3–4 days.
For short-term treatment, the culture medium was changed to a medium containing DMSO (vehicle) or imidazole propionate (100 μM) and then incubated for 24 h. After nine days of seeding primary cortical neurons in a 12-well culture plate, the cultured medium was changed to medium containing DMSO or imidazole propionate (100 μM), along with either rapamycin (20 nM) or pirfenidone (1 mM), and incubated for 24 h. Cell viability was assessed using the Cell Counting Kit-8 (DOJINDO Molecular Technologies), according to the manufacturer’s instructions.
For long-term treatment, primary cortical neurons were pre-incubated with α-Syn preformed fibrils (PFF) at a final concentration of 0.1 μg/mL for 24 h. Subsequently, the culture medium was changed to a medium containing either DMSO (vehicle) or varying concentrations of imidazole propionate (1, 10, 100, and 1000 nM) every three days; therefore, two changes occurred in total over the course of the experiment.
Preparation of proteins and Western blot
After brief washing with 1 × PBS, mouse cortical neurons were lysed in a lysis buffer containing 1% Nonidet P-40 (NP-40) and 0.5% sodium deoxycholic acid (NaDOC) in PBS, pH 7.4, supplemented with HaltTM Protease Inhibitor (Thermo Scientific Cat# 87786) / HaltTM Phosphatase Inhibitor (Thermo Scientific #78420). The lysates were incubated on ice by vortexing every 30 min 5 min to ensure complete lysis, followed by centrifugation at 4 °C for 30 min at 15,000 × g. The supernatant was collected for downstream analysis, and the protein concentration was determined using the Pierce BCA Protein Assay Kit with BSA standards.
For the preparation of detergent soluble and insoluble fractions48, mouse brain tissues were homogenized and prepared in Lysis buffer containing 10 mM Tris-HCl (pH 7.4), 150 mM NaCl, 5 mM EDTA, and 1% NP-40, supplemented with a protease and phosphatase inhibitor cocktail (Thermo Fisher Scientific). Primary neurons were lysed using the same buffer composition for detergent soluble and insoluble fraction separation, except that 1% Triton X-100 was used as the detergent instead of NP-4049. All samples were incubated on ice for 30 min. After centrifugation of the lysates at 14,000 × g for 20 min at 4 °C, the soluble fraction (supernatant) was collected. The pellets were washed and then lysed using a lysis buffer containing 1% SDS and 0.5% sodium deoxycholate. After centrifugation of the lysates at 14,000 × g for 20 min at 4 °C, the insoluble fraction (supernatant) was collected.
The protein samples were mixed with 2× Laemmli buffer containing β-mercaptoethanol (Bio-Rad) for 5 min at 95 °C. The samples were separated using SDS-PAGE and transferred onto nitrocellulose membranes (cat# 162-0115) for immunoblotting. The membranes were probed with the specified antibodies and immunoblot bands were detected using chemiluminescence (Pierce, Rockford, IL, USA). The ImageJ software (NIH; rsb.info.nih.gov/ij) was used for the densitometric analysis of the bands.
Immunocytochemistry and fluorescence signal quantification
To prepare fixed cells for immunofluorescence analysis, 4% paraformaldehyde in PBS was used for fixation. After fixation, a blocking solution containing 5% normal goat serum (cat#16201, Invitrogen) and 0.1% Triton X-100 (cat#X100, Sigma-Aldrich) in PBS was applied for 1 h at room temperature. Depending on the specific experiment, samples were incubated at 4 °C for 16 h with primary antibodies against pS129-α-Syn and MAP2. The fixed samples were washed with 1× PBS and incubated with fluorescent-labeled secondary antibodies for 1 h. The samples were incubated with DAPI (Sigma-Aldrich; cat #D9542) for 1 min, followed by washing with 1× PBS to stain cell nuclei. Finally, the samples were mounted using Immu-Mount (Thermo Fisher; cat #9990402) and imaged under a microscope (Zeiss, Axiovert 200 M). Fluorescence signal quantification was performed by calculating the mean fluorescence intensity per unit area using ImageJ software (National Institutes of Health, Bethesda, MD, USA). For each image, the MAP2 channel was used to create a mask delineating neuronal cell bodies and processes. The mean fluorescence intensity of the pS129-α-synuclein signal within the MAP2-positive area was measured. Data were normalized to the mean intensity of control samples to obtain relative fluorescence intensities. For assessment of neurotoxicity induced by a-synuclein PFF treatment to cortical neurons, MAP2-positive neurites were identified, and neurite “beading”—defined as fragmentation along otherwise continuous MAP2-labeled neurites—was manually quantified using ImageJ. The total number of beads was counted per field and normalized to the total number of MAP2-positive neurites.
Statistical analysis
The mean ± standard error of the mean (SEM) was used to represent quantitative data. Normality of the data was assessed using the Shapiro–Wilk test. One-way ANOVA was used to compare means among more than two groups based on a single independent variable, whereas two-way ANOVA was applied when analyzing the effects of two independent variables and their interaction. Tukey’s post-hoc analysis was performed for multiple comparisons. For comparisons between two groups, an unpaired two-tailed Student’s t-test was used. The Wilcoxon rank-sum test was used to analyze human gut microbiome datasets or plasma data. Results were considered statistically significant at P < 0.05.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All raw data are provided in the Source Data file. Specific data P values are also included within the Source Data file. Source data are provided with this paper. Further information and requests for resources and reagents should be directed to, and will be fulfilled by Yunjong Lee (ylee69@skku.edu) and Ara Koh (ara.koh@postech.ac.kr). Source data are provided with this paper.
References
Lang, A. E. & Lozano, A. M. Parkinson’s disease - first of two parts. N. Engl. J. Med. 339, 1044–1053 (1998).
Chen, H. L. & Ritz, B. The search for environmental causes of parkinson’s disease: moving forward. J. Parkinsons Dis. 8, S9–S17 (2018).
Hasan, N. & Yang, H. Y. Factors affecting the composition of the gut microbiota, and its modulation. Peerj 7, e7502 (2019).
Romano, S. et al. Meta-analysis of the Parkinson’s disease gut microbiome suggests alterations linked to intestinal inflammation. Npj Parkinsons Dis. 7, 27 (2021).
Sampson, T. R. et al. Gut microbiota regulate motor deficits and neuroinflammation in a model of parkinson’s disease. Cell 167, 1469–1480 (2016).
Fülling, C., Dinan, T. G. & Cryan, J. F. Gut microbe to brain signaling: what happens in vagus. Neuron 101, 998–1002 (2019).
Kim, S. et al. Transneuronal propagation of pathologic α-synuclein from the gut to the brain models Parkinson’s disease. Neuron 103, 627–641. e627 (2019).
Cryan, J. F. & Dinan, T. G. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 13, 701–712 (2012).
Koh, A. & Backhed, F. From association to causality: the role of the gut microbiota and its functional products on host metabolism. Mol. Cell 78, 584–596 (2020).
Vuong, H. E. et al. The maternal microbiome modulates fetal neurodevelopment in mice. Nature 586, 281–286 (2020).
Unger, M. M. et al. Short chain fatty acids and gut microbiota differ between patients with Parkinson’s disease and age-matched controls. Parkinsonism Relat. Disord. 32, 66–72 (2016).
Ryu, G., Kim, H. & Koh, A. Approaching precision medicine by tailoring the microbiota. Mamm. Genome 32, 206–222 (2021).
Wallen, Z. D. et al. Metagenomics of Parkinson’s disease implicates the gut microbiome in multiple disease mechanisms. Nat. Commun. 13, 6958 (2022).
Delgado, S., Suárez, A. & Mayo, B. Bifidobacterial diversity determined by culturing and by 16S rDNA sequence analysis in feces and mucosa from ten healthy Spanish adults. Digestive Dis. Sci. 51, 1878–1885 (2006).
Turroni, F. et al. Exploring the diversity of the bifidobacterial population in the human intestinal tract. Appl. Environ. Microbiol. 75, 1534–1545 (2009).
Engevik, M. A. et al. Bifidobacterium dentium-derived y-glutamylcysteine suppresses ER-mediated goblet cell stress and reduces TNBS-driven colonic inflammation. Gut Microbes 13, 1902717 (2021).
Engevik, M. A. et al. Bifidobacterium dentium fortifies the intestinal mucus layer via autophagy and calcium signaling pathways. MBio 10, e01087–19 (2019).
Engevik, M. A. et al. Human-derived Bifidobacterium dentium modulates the mammalian serotonergic system and gut–brain axis. Cell. Mol. Gastroenterol. Hepatol. 11, 221–248 (2021).
Koh, A. et al. Microbially produced imidazole propionate impairs insulin signaling through mTORC1. Cell 175, 947–961 (2018).
Kassai, H. et al. Selective activation of mTORC1 signaling recapitulates microcephaly, tuberous sclerosis, and neurodegenerative diseases. Cell Rep. 7, 1626–1639 (2014).
Reikvam, D. H. et al. Depletion of murine intestinal microbiota: effects on gut mucosa and epithelial gene expression. Plos One 6, e17996 (2011).
Volpicelli-Daley, L. A., Luk, K. C. & Lee, V. M. Addition of exogenous alpha-synuclein preformed fibrils to primary neuronal cultures to seed recruitment of endogenous alpha-synuclein to Lewy body and Lewy neurite-like aggregates. Nat. Protoc. 9, 2135–2146 (2014).
Zhu, Z. et al. Balancing mTOR signaling and autophagy in the treatment of parkinson’s disease. Int. J. Mol. Sci. 20, 728 (2019).
Kim, H. et al. Activation of the Akt1-CREB pathway promotes RNF146 expression to inhibit PARP1-mediated neuronal death. Sci. Signal. 13, eaax7119 (2020).
Luk, K. C. et al. Pathological α-synuclein transmission initiates parkinson-like neurodegeneration in nontransgenic mice. Science 338, 949–953 (2012).
Hou, Y. C. et al. Neuroprotective effects of short-chain fatty acids in MPTP induced mice model of Parkinson’s disease. Exp. Gerontol. 150, 111376 (2021).
Hou, Y. F. et al. Gut microbiota-derived propionate mediates the neuroprotective effect of osteocalcin in a mouse model of Parkinson’s disease. Microbiome 9, 34 (2021).
Ge, X. et al. Butyrate ameliorates quinolinic acid-induced cognitive decline in obesity models. J. Clin. Investig. 133, e154612 (2023). doi:ARTN.
Liu, J. M. et al. Sodium butyrate exerts protective effect against Parkinson’s disease in mice via stimulation of glucagon like peptide-1. J. Neurological Sci. 381, 176–181 (2017).
Creed, R. B., Memon, A. A., Komaragiri, S. P., Barodia, S. K. & Goldberg, M. S. Analysis of hemisphere-dependent effects of unilateral intrastriatal injection of α-synuclein pre-formed fibrils on mitochondrial protein levels, dynamics, and function. Acta neuropathologica Commun. 10, 78 (2022).
Brahmachari, S. et al. Parkin interacting substrate zinc finger protein 746 is a pathological mediator in Parkinson’s disease. Brain 142, 2380–2401 (2019).
Braniste, V. et al. The gut microbiota influences blood-brain barrier permeability in mice. Sci. Transl. Med. 6, 263ra158–263ra158 (2014).
Komici, K., Femminella, G. D., Bencivenga, L., Rengo, G. & Pagano, G. Diabetes Mellitus and Parkinson’s Disease: A Systematic Review and Meta-Analyses. J. Parkinson’s. Dis. 11, 1585–1596 (2021).
Iba, M. et al. Role of alterations in protein kinase p38 gamma in the pathogenesis of the synaptic pathology in dementia with lewy bodies and alpha-synuclein transgenic models. Front. Neurosci. 14, 286 (2020).
Postuma, R. B. et al. Validation of the MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 33, 1601–1608 (2018).
Beghini, F. et al. Integrating taxonomic, functional, and strain-level profiling of diverse microbial communities with bioBakery 3. elife 10, e65088 (2021).
Molinaro, A. et al. Imidazole propionate is increased in diabetes and associated with dietary patterns and altered microbial ecology. Nat. Commun. 11, 5881 (2020).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. methods 9, 357–359 (2012).
Venskutonyte, R. et al. Structural characterization of the microbial enzyme urocanate reductase mediating imidazole propionate production. Nat. Commun. 12, 1347 (2021).
Mallick, H. et al. Multivariable association discovery in population-scale meta-omics studies. PLOS Computational Biol. 17, e1009442 (2021).
Lin, H. & Peddada, S. D. Analysis of compositions of microbiomes with bias correction. Nat. Commun. 11, 3514 (2020).
Wahlström, A. et al. Production of deoxycholic acid by low-abundant microbial species is associated with impaired glucose metabolism. Nat. Commun. 15, 4276 (2024).
Wei, W. et al. Psychological stress-induced microbial metabolite indole-3-acetate disrupts intestinal cell lineage commitment. Cell Metab. 36, 466–483. e467 (2024).
Eberl, C. et al. Reproducible colonization of germ-free mice with the oligo-mouse-microbiota in different animal facilities. Front. Microbiol. 10, 2999 (2020).
Chen, Z. et al. Development of species-specific primers for detection of Streptococcus mutans in mixed bacterial samples. Fems Microbiol. Lett. 272, 154–162 (2007).
Davis, B. M., Salinas-Navarro, M., Cordeiro, M. F., Moons, L. & De Groef, L. Characterizing microglia activation: a spatial statistics approach to maximize information extraction. Sci. Rep. 7, 1576 (2017).
Shin, J.-Y. et al. Dual inhibition of aminoacyl-tRNA synthetase interacting multifunctional protein-2 and α-synuclein by steroid derivative is neuroprotective in Parkinson’s model. iScience 27, 111165 (2024).
Yun, S. P. et al. Block of A1 astrocyte conversion by microglia is neuroprotective in models of Parkinson’s disease. Nat. Med. 24, 931–938 (2018).
Ham, S. et al. Amyloid-like oligomerization of AIMP2 contributes to α-synuclein interaction and Lewy-like inclusion. Sci. Transl. Med. 12, eaax0091 (2020).
Acknowledgements
This research was funded by the Samsung Research Funding & Incubation Center of Samsung Electronics (Project Number SRFC-MA2301-03 to A.K.), the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2023R1A2C1002876 to A.K.), and the Basic Science Institute (National Research Facilities and Equipment Center) grant funded by the Ministry of Education (No. 2021R1A6C101A390 to A.K.). This research was supported by the Bio&Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (grant number: RS-2024-00361688 to Y.L.) and by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. RS-2024-00349023 to Y.L.). Figures 1d, 2b, 3d, 4d, 5a, 5e, and 6 were created with BioRender. Kim, J. (2025).
Author information
Authors and Affiliations
Contributions
Y.L. and A.K. conceived the study hypothesis, supervised the project, and wrote the manuscript. H.P. and J.C. performed the majority of experiments, conducted data analysis, and contributed to manuscript writing. H.K., Jihye K., and J.-Y.S. also performed experiments and data analysis. Jihyun K., HyoJin K., G.R., I.Y.C., Z.Z., H.W., Ji Hun K., D.K., and K.R.B. contributed to experiments and data analysis. F.B. provided technical and material support. Han-Joon K. provided the PD cohorts. All authors contributed to the final review of the manuscript and figures.
Corresponding authors
Ethics declarations
Competing interests
F.B. is a co-founder of Implexion Pharma AB and Roxbiosens Inc., receives research funding from Biogaia AB and is on the scientific advisory board of Bactolife A/S. A.K. and K.R.B. are a shareholder of Implexion Pharma AB. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Park, H., Cheon, J., Kim, H. et al. Gut microbial production of imidazole propionate drives Parkinson’s pathologies. Nat Commun 16, 8216 (2025). https://doi.org/10.1038/s41467-025-63473-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-63473-4