Abstract
Anchored immunotherapy is a novel approach for retaining drugs within the tumour microenvironment. Tolododekin alfa is a first-in-class anchored Interleukin 12 (IL-12) linked to aluminum hydroxide. Safety and biological activity were evaluated in a Phase 1 clinical trial in patients with accessible advanced solid tumours in Part 1 of a 3-part trial. The primary objectives are safety and tolerability as well as determination of the recommended dose for expansion (RDE). Secondary objectives include pharmacokinetics (PK), pharmacodynamics, preliminary antitumour activity, and immunogenicity. Exploratory analyses include serum and tissue biomarkers. Fifteen patients were enrolled at escalating doses of tolododekin alfa given by injection every 3 weeks. There were no dose-limiting toxicities or treatment-related serious adverse events. PK/Pharmacodynamic measurements demonstrate retention of drug in the tumour. Biological activity demonstrates increased CD8+ T cells, Programmed Cell Death Ligand 1 (PD-L1) expression, and prolonged pro-inflammatory gene expression. Nine patients (60%) achieved stable disease with one partial response. At a median follow-up of 5.2 months, the median duration of stable disease was 5.3 months (range 3.6-7.6 months). Median progression-free survival (PFS) was not estimable (NE) (95% CI, 2.57 months – NE). These findings support continued clinical development of tolododekin alfa. ClinicalTrials.gov registration: NCT06171750.
Similar content being viewed by others
Introduction
Immunotherapy has transformed the therapeutic landscape in oncology, most notably through immune checkpoint blockade for solid tumors and chimeric antigen receptor T cell therapy for hematologic malignancies1,2. In contrast to checkpoint blockade, which prevents T cell inhibition, immune agonists act directly on effector T and natural killer (NK) cells to stimulate proliferation and anti-tumor effector cell functions. While numerous immune agonists have shown robust therapeutic activity in preclinical tumor models, clinical development has been limited by the need for supraphysiologic systemic doses for efficacy, resulting in narrow therapeutic windows and poor pharmacokinetics (PK), requiring frequent administration. For example, high-dose interleukin-2 (IL-2) is approved for treating renal cell carcinoma and metastatic melanoma, but requires high-dose bolus infusions, leading to significant toxicity and requiring intensive care management3,4. Similarly, other promising immune agonists, including those targeting CD28, 4-1BB, CD40, and IL-12, have been hindered by significant systemic toxicity5,6,7,8.
To overcome these challenges, local retention of the agonist at the tumor site is a promising strategy. Localized delivery or tumor-targeted approaches are thought to enhance therapeutic efficacy by maximizing immune activation at the tumor site, which can promote systemic anti-tumor immunity, while minimizing systemic exposure and associated toxicities9,10. Such strategies represent a pivotal opportunity to unlock the full potential of immune agonists in cancer therapy. However, the direct injection of agonists, such as recombinant IL-12, into tumors has not proven successful in reducing toxicity, likely due to rapid diffusion out of the tumor resulting in systemic absorption11. We have developed a drug platform that results in durable local retention within tumors by leveraging stable, non-covalent conjugation to an aluminum hydroxide scaffold12. Tolododekin alfa (formerly ANK-101) consists of stable conjugation of full-length human IL-12 to aluminum hydroxide, which serves as an inert scaffold for drug presentation. The drug is composed of the p35 and p40 IL-12 subunits with an alum-binding peptide (ABP) extending from the C-terminus of the IL-12 chain (Supplementary Fig. 1). The ABP contains serine residues that can be variably phosphorylated to create a negative charge, allowing for interaction with hydroxyl residues on aluminum hydroxide. Brief admixture of the IL-12-ABP with aluminum hydroxide prior to administration generates tolododekin alfa12.
IL-12 is produced by myeloid cells, CD4+ T helper cells, and B-lymphoblastoid cells and regulates innate and adaptive immune responses13,14. IL-12 comprises two subunits: p35, which regulates signaling, and p40, essential for receptor binding. The p40 subunit is shared with other IL-12 family members, such as IL-2313,14. IL-12 induces interferon-γ (IFN-γ) production, promotes Th1 differentiation, and enhances CD8+ T cell and NK cell effector functions, playing a vital role in transitioning from innate to adaptive immunity and mediating tumor-antigen-specific responses13,14. Systemic IL-12 has previously demonstrated therapeutic activity in humans but was associated with unacceptable toxicity and mortality.
In a Phase 1 trial, recombinant IL-12 (3–1000 ng/kg/day) was administered via intravenous (IV) bolus for 5 days every 3 weeks15. While two patients (melanoma, renal cell carcinoma) showed objective responses and four had stable disease (SD), severe toxicities, including elevated hepatic transaminases and stomatitis, limited its use. A subsequent study with twice-weekly IV boluses (30–700 ng/kg) established a maximum tolerated dose (MTD) of 500 ng/kg16. At doses above 500 ng/kg, significant dose-limiting toxicities (DLTs) included elevated transaminases, Grade 4 neutropenia, and hemolytic anemia17. Despite some evidence of activity, systemic toxicity has hindered the clinical development of IL-12.
Preclinical studies of a murine surrogate of tolododekin alfa demonstrated prolonged retention within tumors for several weeks and showed single-agent therapeutic activity across various murine tumor models without evidence of toxicity12. Murine tolododekin alfa promoted effector CD8+ T cell recruitment, enhanced IFN-γ production, increased local PD-L1 expression, and induced durable pro-inflammatory gene expression12. Additionally, a canine version of tolododekin alfa was evaluated in a Phase 1 clinical trial for dogs with advanced melanoma, showing a favorable safety profile with a 29% objective response rate and a 47% durable disease control rate, as well as evidence of an abscopal response with partial regression of uninjected pulmonary metastases in one subject18.
Based on these findings, we hypothesized that tolododekin alfa would have an acceptable safety profile in human cancer patients, and PK modeling predicted drug retention locally and biological activity that would result in local IFN-γ and PD-L1 upregulation. To test this hypothesis and gather preliminary data on efficacy and quality of life, a Phase 1 trial of tolododekin alfa was conducted in patients with advanced, superficially accessible solid tumors. The data herein represent the first-in-human report of an anchored drug conjugate in patients with advanced solid tumors.
Results
Patient characteristics
From February 5 to November 20, 2024, a total of fifteen patients were treated in this dose escalation monotherapy phase (Part 1). The patient characteristics are summarized in Table 1. The median age was 68 years (range, 36–79) with 6 (40%) men and 9 (60%) women enrolled. The baseline ECOG performance status was 0 in 9 (60%) and 1 in 6 (40%) of the patients. All patients had received prior therapy with more than three regimens in 11 (73.3%) of the patients and less than or equal to three prior regimens in 4 (26.7%) of the patients (Supplementary Table 2). All but two patients had progressed on prior immunotherapy. The tumors treated were melanoma (n = 7; 46.7%), head and neck cancer (n = 4; 26.7%), breast cancer (n = 2; 13.3%), and apocrine adenocarcinoma (n = 1; 6.7%).
Treatment
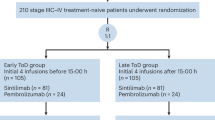
Overall, 31 patients were screened for the trial, and 15 patients were enrolled (Supplementary Fig. 2). All 15 patients are included in the safety analysis set. Thirteen patients are included in the efficacy analysis, as 2 subjects terminated the study prior to initial evaluation. One patient (in cohort 1; 2 µg/mL) withdrew consent after one injection due to social reasons after completing the DLT period. Three patients were removed from treatment prior to completing all four cycles, all for disease progression. Three patients received all four planned cycles, and eight patients received more than four cycles. No patients discontinued study treatment due to an adverse event. The median number of doses administered was 4 (range 1–8) per patient, and the median number of tumors injected per patient was 1 (range 1–6). The median volume injected per patient was 8 mL (range 0.5–32 mL). Further details describing dosing and drug volume injected per patient are described in Table 1.
Safety
The primary endpoint of this study was safety and tolerability. There were no DLTs reported in any patients. There were no Grade 3 or greater treatment-related treatment-emergent adverse events (TEAEs) or serious adverse events (SAEs) in any patient. In addition, no procedure-related TEAEs were observed. There was one Grade 3 SAE of soft tissue infection in a patient treated with tolododekin alfa at the 20 µg/mL cohort, which resolved with systemic antibiotics and was considered unrelated to tolododekin alfa. The most common treatment-related adverse events are summarized in Table 2. The most common of these were fatigue (n = 2) and myalgia (n = 2). In most cases, the onset of inflammation-related adverse events such as fatigue, flu-like syndrome, and pyrexia occurred immediately after administration. Of note, there were three reports of Grade 1 fever in two patients (at both the 20 µg/mL and 120 µg/mL cohorts) that may have been due to mild cytokine release syndrome. Pre-medication with acetaminophen was allowed after the fevers, and this event did not recur with subsequent dosing. There were no significant laboratory abnormalities noted, and there were no changes in the neutrophil-to-lymphocyte ratio (NLR) in any patients Supplementary Fig. 3.
Pharmacokinetics and antidrug antibodies
Determination of the recommended dose for expansion (RDE) was the other primary endpoint for the study and was based on the pharmacokinetic analysis, a secondary endpoint. The PK analyses from all patients after the first cycle of treatment are summarized in Fig. 1A (left) and Supplementary Table 3. A general trend of dose-dependent increases in systemic drug exposure was observed; however, substantial variability was noted in individual PK profiles within and across dose cohorts. Serum concentrations in the first eight patients (Cohorts 1–4) ranged from unquantifiable in four patients to very low levels, with a Cmax range of 19.2–139 pg/mL. In contrast, systemic IL-12-ABP levels were more readily detectable in Cohorts 5 and 6, with a median Cmax of 103 pg/mL (range, 18.2–693 pg/mL) and a median Tmax of 24 h (range, 0.5–168 h). In most patients with measurable PK profiles, IL-12-ABP remained detectable up to the last timepoint (168 h).
A-B Serial serum samples were obtained as per the study protocol, and the mean plasma concentration (±SD) of IL-12-ABP versus time after Cycle 1 (A) and after Cycle 2 (B) is shown, n per cohort is indicated in the figure. Systemic levels of IL-12-ABP are, in general, low, and there was a trend in dose-dependent exposure observed at higher dosing cohorts. C Levels of circulating IFN-γ are shown by treatment cohort following Cycle 1 dosing. A transient and low systemic exposure of IFN-γ with a peak at 48 h after dosing was observed. D Composite dose cohort maps summarizing the systemic levels of a panel of cytokines following treatment with repeated doses of tolododekin alfa. Tolododekin alfa treatment led to minimal changes in systemic cytokine levels, supporting the local immune activation at the injected site by tolododekin alfa. Source data can be found in the Source data file.
To evaluate tumor retention efficiency, the Cmax was expressed as a percentage of the total administered dose (Supplementary Table 4). Results indicated that only a minute fraction of the total dose (0.02–0.67%) was present systemically at Cmax, indicating that tolododekin alfa efficiently anchors the bioactive IL-12-ABP component within tumors.
Following the second treatment cycle, systemic levels of IL-12-ABP were consistently detected in all patients. Similar to observations from Cycle 1, serum concentrations after Cycle 2 remained generally low with a median across all Cohorts of 59.5 pg/mL (range, 13.8-1010 pg/mL). Significant inter- and intra-cohort variability persisted, with a trend of higher IL-12-ABP levels at doses >60 µg/mL (Fig. 1A and Supplementary Table 5). Total systemic exposures following Cycle 2 were notably lower compared to Cycle 1, with all patients exhibiting a Tlast of 48 h (Fig. 1B).
Another secondary endpoint was the immunogenicity of tolododekin alfa. The presence of circulating antidrug antibodies (ADA) against the IL-12-ABP protein was assessed at baseline and after Cycles 1 and 3. Among the first 12 patients (Cohorts 1–5), only two patients tested positive for ADA, with the positivity apparent after Cycle 3 (Supplementary Table 6). These preliminary findings suggest low immunogenicity of the IL-12-ABP protein.
Efficacy
A secondary endpoint was the assessment of preliminary clinical activity. The overall disease control rate was 60.0% by standard RECIST v1.1 criteria (Table 3). Of those with disease control, five subjects maintained their response 24 weeks or longer, and seven participants (47%) were treated to the full 8 cycles of treatment. Spider plots of responses across all treatment cohorts demonstrated that 9 patients had SD across all doses (Fig. 2A). One patient achieved an objective partial response (PR) per RECIST v1.1 after eight cycles. This patient achieved their response at week 24 following the last dose of ANK-101, and therefore, the duration of response was not calculated. Further, another patient had a PR in a target lesion after four cycles, but then subsequently progressed with the appearance of a new lesion. The waterfall response for target lesions is shown in Supplementary Fig. 4. We also evaluated responses in injected lesions and saw a similar pattern of response (Supplementary Fig. 5). One patient remains on active treatment and is being followed for response. At a median follow-up of 5.2 months, the median duration of SD was 5.3 months (range 3.6–7.6 months), which is summarized in the swimmer plot (Fig. 2B). At the time of this analysis, PFS data were immature with median PFS being non-evaluable (95% CI, 2.57-NE). Although serial pathology for response was not included in the study, serial photography documented complete regression in several injected lesions in a patient with metastatic bladder cancer treated with tolododekin alfa at 60 mg/mL (Fig. 2C). A trend was observed correlating higher measured systemic INF-γ with disease control, with patients achieving a best response of SD or PR having a peak median IFN-γ of 191.8 (15.7–2369.1) compared with 28.9 (17.7–6083.0) in those with PD (p value 0.42). Biopsies of injected lesions were available in three patients (melanoma, bladder carcinoma, and head and neck squamous cell carcinoma) after 1 and 3 cycles of treatment, which demonstrated the absence of viable tumor with residual inflammation (Fig. 2D).
A Spider plot depicting % change in sum diameters per RECIST in target lesions across all evaluable dosing cohorts (n = 11 subjects). B Swimmer plot for individual patients across dosing cohorts (n = 15 subjects). C Computed tomography with contrast of Subject 101-601 with head and neck cancer at baseline (left) and at Week 24 (right) following eight cycles of therapy with a −69.3% reduction in tumor volume; arrow indicates target lesion. D Representative H&E images from individual patients pre-and post-treatment with tolododekin alfa at the indicated times show decreased tumor cellularity and increased necrosis. The staining was performed once, and the evaluability of the staining was determined by the pathologist. The inset indicates the total tolododekin alfa dose (µg) injected into the biopsied tumor corresponding to the timepoint. Source data can be found in the Source data file.
Induction of serum cytokines
Exploratory endpoints included assessment of biomarker changes in patients receiving tolododekin alfa. Peripheral blood samples were collected according to the schedule in Supplementary Table 7, and serum was isolated for cytokine analysis. IFN-γ is the primary cytokine produced in response to IL-12 signaling. Post-treatment increases in systemic IFN-γ levels were detected in all patients (Fig. 1C). In Cohorts 1–3, levels of circulating IFN-γ were low, with a median peak of 77.9 pg/mL (range, 17.7–496.4 pg/mL). A dose-dependent upward trend was observed, with Cohorts 4–6 exhibiting a median peak of 559.9 pg/mL; however, levels varied widely (range, 19.0–6083 pg/mL). For most patients, peak IFN-γ levels occurred 48 h after dosing. In patients who received multiple treatment cycles, pre-dose IFN-γ returned to undetectable levels and was reliably re-induced with subsequent doses. Changes in the other cytokines measured were minimal, except for IL-12p70, where the elevated levels were attributed to circulating IL-12-ABP (Fig. 1D). Overall, these findings indicate that tolododekin alfa is biologically active following local administration and induces IL-12-mediated immune activation, supported by evidence of a dose-dependent pharmacodynamic response, and this activity is persistent with repeat dosing.
Remodeling of the tumor microenvironment
Tumor biopsies were collected as outlined in Supplementary Table 8 to assess treatment-related changes in the TME. In biopsies collected 21 days post-treatment, differential gene expression analysis demonstrated consistent upregulation of multiple markers indicative of immune activation and counter-regulatory mechanisms, compared to their paired pre-treatment samples (Fig. 3A, B). Significant increases were observed in gene expression signatures associated with T cells, Th1 cells, CD8+ T cells, exhausted CD8+ T cells, cytotoxic cells, dendritic cells, macrophages, and regulatory T cells. The most highly upregulated genes included those encoding the IL-2 receptor alpha chain (IL2RA); IL12RB2, STAT4 (IL-12 signaling), immune checkpoint molecules (CTLA4, PD-1, TIGIT, PD-L1, PD-L2); chemokines (CXCL9, CXCR3, CCL5); cytotoxic effector molecules (PRF1, GZMA, GZMK), M1 macrophages (CD38 and CD86) (Fig. 3B). These gene expression changes were consistently observed across all evaluable dosing cohorts, in all tumor types assessed, and in both injected and non-injected tumors (Fig. 3C).
A–D Transcriptional analysis (Nanostring IO360TM Panel) of tumor tissue biopsies collected at baseline (C1D1) and 21 days post-treatment after one dose of tolododekin alfa (C2D1), n = 8 patients. A The “All Signatures” forest plot shows the differential expression between time points (C2D1 vs C1D1) for each signature on an unadjusted scale. The vertical axis is shown at fold change equal to zero; the “black triangle” indicates a significant difference in the signature as assessed by univariate analysis (significance is not adjusted for multiple comparisons). B Volcano plot shows the most highly upregulated IL-12 pathway-related genes as indicated, two-sided statistical analysis was performed. C The heatmap displays differential signature score per patient across all evaluable dosing cohorts, in all tumor types assessed, and in both injected and non-injected tumors, after one cycle (C2D1) and after three cycles of doing (C4D1). D Upregulation of the Tumor Inflammatory Score (TIS) and CD8+ T cell gene signatures were associated with treatment outcomes, a total of 8 patients (n = 6 (SD) and n = 2 (PD). Mean ± SEM is indicated in the bar graphs. Two-sided P values were calculated per paired t-test. *indicates p = 0.05, **indicates p = 0.009.
Upregulation of the Tumor Inflammatory Score and CD8+ T cell gene signatures were associated with treatment outcomes, with patients achieving PR or SD exhibiting significantly higher scores compared to those with pharmacodynamics (Fig. 3D). The TME was further characterized using IHC to detect and quantify tumor infiltration by CD8+ T cells, as well as to assess PD-L1 expression by immune cells and tumor cells. Compared to paired baseline biopsies, most post-treatment samples exhibited a marked increase in the infiltration of CD8+ T cells (Fig. 4A) and PD-L1 expression (Fig. 4B), consistent with the NanoString gene profiling results. Upregulation of the PD-L1 combined positive score (CPS) score and CD8+ T cell infiltration were associated with treatment outcomes, with patients reaching PR or SD showing increased PD-L1 CPS score or CD8+ T cell infiltration (Fig. 4C). Treatment induced a clear upregulation of PD-L1 on tumor cells (TPS), immune cells (IC) as well as the CPS (Supplementary Table 9).
Representative IHC images of A CD8+ and B PD-L1 staining of paired tumor biopsies pre- and post-treatment (21 days) from individual patients across different dosing cohorts and tumor types as indicated. The staining was performed once, and the evaluability of the staining was determined by the pathologist. The bar graphs indicate corresponding %positive cells as scored by the pathologist. C CD8+ T cell infiltration by IHC (left two panels) and PD-L1 CPS score (right two panels) are shown for patients with disease control (PR/SD; left side; n = 9) or disease progression (PD; right side, n = 2); both parameters are significantly increased in disease control patients, total n = 11. Mean ± SEM indicated in the bar graphs. Two-sided P values were calculated per paired t-test, *indicates p = 0.023, **indicates p = 0.008. Source data can be found in the Source data file.
In a patient with metastatic bladder cancer treated with 60 µg/mL tolododekin alfa, changes in the TME were observed after the first injection of tolododekin alfa (Fig. 3D). These changes included a ~6-fold increase in the levels of CD8+ T cells (Fig. 4A), and a 10-fold increase in the CPS for PD-L1 expression (Fig. 4B). Biopsies collected from this tumor after Cycle 3 showed a return to pre-treatment levels of CD8+ T cells (Supplementary Fig. 6A) and PD-L1 expression (Supplementary Fig. 6B). However, the lesion exhibited near complete regression with decreased cellularity and increased necrosis, potentially refecting an effective immune response followed by contraction as the tumor was destroyed (Fig. 2D).
Similar post-treatment changes in CD8+ T cell infiltration and PD-L1 expression were observed in patients with other tumor types, including Stage IV metastatic breast cancer (treated at 20 µg/mL), acral lentiginous melanoma (treated at 20 µg/mL tolododekin alfa), cutaneous melanoma (treated at 60 µg/mL), and metastatic HNSCC (treated at 60 µg/mL). In the HNSCC patient, a 4.3-fold increase in CD8+ T cells and a 23.3-fold increase in PD-L1 CPS were observed after the first tolododekin alfa injection (Fig. 4A, B). Consistent with prior observations in the metastatic bladder cancer patient, the lesion appeared highly necrotic with no viable tumor cells detected, further supporting the hypothesis of local immune contracture following tumor cell elimination (Fig. 2D). Taken together, these data suggest that treatment with tolododekin alfa induces a profound reprogramming of the TME, consistent with both the known biology of IL-12 and previous preclinical observations12.
Discussion
Tolododekin alfa is a novel IL-12-anchored drug conjugate designed for prolonged retention within the tumor microenvironment. The goal of this modification was to mediate anti-tumor immunity without on-target, off-tumor toxicity. In this first-in-human study, tolododekin alfa was well tolerated, and there were no DLTs or Grade 3 or greater treatment-related TEAEs or SAEs. The most common treatment-related adverse events were low-grade constitutional symptoms, including fatigue, influenza-like illness, and myalgias (Table 2). Two patients exhibited Grade 1 fever, which may have been related to mild cytokine release syndrome, but both cases resolved without incident and did not recur after pre-medication of the patient with acetaminophen. Of note, there were no significant elevations of hepatic transaminases, neutropenia, the NLR, or other laboratory abnormalities (Supplementary Fig. 3).
The conjugation of IL-12 to aluminum hydroxide occurs through an electrostatic interaction mediated by negatively charged phosphates on the alum-binding peptide and hydroxyl residues on aluminum hydroxide9. Aluminum hydroxide is an inert metal that has been used for nearly a century as a vaccine adjuvant based on the notion that aluminum hydroxide may have immune adjuvant properties. This supposition has recently been questioned, and it seems unlikely that aluminium hydroxide alone is able to activate immune responses, particularly Th1 type responses15. Further, the potential role of aluminum hydroxide as a therapeutic adjuvant may depend on the dose, route of administration, and therapeutic context15. We have previously reported that a murine IL-12 anchored to aluminum hydroxide resulted in significant therapeutic activity across multiple tumor types, but aluminum hydroxide alone had no effect12. Thus, following intratumoural injection, it appears that aluminum hydroxide generally acts as an inert scaffolding allowing retention of local IL-12. Since aluminum hydroxide is not subject to enzymatic degradation, as a delivery platform, it allows for higher local cytokine concentrations and a longer local half-life for drug delivery.
Evidence that the IL-12 anchored drug conjugate was retained at the tumor site was provided in the PK analyses. Following direct injection of tolododekin alfa, systemic levels of IL-12-ABP were generally very low, particularly in the first four dosing cohorts. Systemic levels were higher in cohorts after dose escalation, with the highest Cmax of 1010 pg/mL observed after the second treatment cycle in a Cohort 5 patient who received a total dose of 300 µg. In this patient, the Cmax corresponded to just 0.58% of the total administered dose. By way of comparison, Cmax values at the MTD (500 ng/kg) of IV administered IL-12 were reported to be ~3,000 pg/mL16, which represents ~24% of the total dose assuming a body weight of 70 kg. In all patients, following both the first and second treatment cycles, Cmax levels of tolododekin alfa accounted for only a small fraction (well under 1.0%) of the total administered dose, suggesting efficient tumor retention. The observed low systemic exposure, driven by effective tumor retention, is an expected characteristic of anchored immunotherapy, because the drug is stably linked to aluminum hydroxide. Systemic exposure decreased substantially following the second treatment cycle. This reduction is unlikely attributable to ADA, as no ADA was detected in pre-dose samples. Other plausible explanations include changes in the TME that may have influenced systemic drug absorption. These could involve increased target-mediated drug disposition due to upregulated IL-12R expression, alterations in stromal architecture that impact drug diffusion, enhanced local drug sequestration within the tumor, increased absorption of tolododekin alfa by infiltrating lymphocytes, or increased intratumoural clearance mechanisms.
Durable drug retention was also seen in preclinical studies of murine tolododekin alfa utilizing 125I-SPECT imaging. These indicated that ~40% of the drug conjugate remained in the tumor 28 days after injection12. In a Phase 1 study conducted in dogs with advanced mucosal melanoma, a canine version of tolododekin alfa induced pro-inflammatory gene expression that persisted in some dogs for up to 84 days and was associated with recruitment of T cells to the tumor site, increased local PD-L1 expression, and induced serum IFN-γ19. In this canine study, therapeutic activity was observed without DLTs, suggesting that local drug retention is similar across multiple species. A mixed-effect Pharmocodynamic model based on preclinical data suggested that systemic IFN-γ production and PD-L1 expression in the tumor microenvironment would serve as key indicators of bioactivity in humans20.
The favorable safety profile supports that patients can tolerate up to 250 μg/mL of tolododekin alfa. Previous PK modeling and drug release studies have suggested that further dose escalation is unlikely to yield further drug biodistribution or improve IL-12 signaling19. These data further suggest that continued dose escalation may be unlikely to improve therapeutic activity. Indeed, the prolonged retention of IL-12 locally may be sufficient to mediate anti-tumor activity even at lower administered doses. Consistent with this, we found disease control at all dosing cohorts except for the lowest dose of 2 μg/mL. Thus, 250 μg/mL was selected as the recommended dose for further expansion.
In line with the PK modeling prediction, evaluation of systemic and local pharmacodynamic biomarkers confirmed the biological activity of tolododekin alfa. Indeed, we observed a dose-dependent increase in systemic IFN-γ levels (Fig. 1C) and consistent re-induction of transient IFN-γ with each treatment cycle (Fig. 1D). We also observed remodeling of the tumor microenvironment (TME) across multiple tumor types and dose levels. Upregulation of immune-related gene signatures, particularly those associated with CD8+ T cells and Th1-driven responses, was accompanied by increased infiltration of CD8+ T cells and macrophages, consistent with data from preclinical studies12,19,20,21. Gene profiling showed increased expression of CXCL9, CXCR3, and CCL5, which likely explains how CD8+ T cells and myeloid cells were recruited to the tumor site. Preclinical studies suggested that infiltrating macrophages were skewed to an M1 phenotype21, and Nanostring data suggest trends towards M1 macrophage phenotype (CD38, CD86) (Fig. 3B).
We also demonstrated elevated PD-L1 expression in the tumor microenvironment with CPS scores increasing more than 2- to 3-fold in some patients. Cell population analysis suggested that PD-L1 expression was often most profound on infiltrating myeloid cells rather than on tumor cells (Supplementary Table 9), which may have been in the process of dying and/or immune-mediated elimination. This suggests that tolododekin alfa may be useful in combination with PD-1/PD-L1 checkpoint inhibitors, where increased CPS scores are often associated with increased efficacy. These findings align with preclinical observations and are hallmarks of IL-12-mediated immune stimulation.
Initial results suggest that patients who were heavily pre-treated experienced clinical benefit with a disease control rate of 60%, one PR by RECIST v1.1, and another best objective PR of target lesions. The reason for limited objective responses may relate to traditional computed tomography (CT) imaging underestimating true pathologic responses, as has been reported for other local immunotherapy agents22,23. Consistent with this, we observed pathologic responses in three patients despite having measurable disease by CT imaging (see Fig. 2D). Another reason may relate to the presence of highly advanced disease, as all patients had progressed following multiple lines of prior therapy, and three patients developed disease progression prior to being able to complete all four planned cycles. Disease control was 81.
8% in the patients who completed at least four cycles of treatment. These data are also consistent with the canine IL-12 anchored drug conjugate in dogs with advanced melanoma disease control was associated with a durable overall survival benefit19. Importantly, six subjects remain on treatment and may achieve further benefit. Further studies may need to incorporate scheduled tumor biopsies or the inclusion of the circulating tumor DNA to better assess clinical benefit beyond imaging alone. Patients who achieved disease control also demonstrated significant increases in CD8+ T cell and pro-inflammatory gene signatures, suggesting that biological changes were associated with clinical benefit. The study was not designed to evaluate clinical activity, but the data suggest further studies in a more homogeneous population are warranted. This trial has several limitations. First, this is a small first-in-human study with only a limited number of subjects at any given dose, and also represents a range of underlying tumor histologies and prior treatment exposure. Second, as a locally acting immune agent, there could be local inflammatory changes that could obscure pathologic responses when using standard imaging techniques. In addition, there can be considerable variability in the volume of drug delivered based on investigator technique and histopathologic features of the tumor. There may also be bias in the selection of lesions for injection at different study sites.
In summary, this Phase 1 first-in-human study demonstrated that tolododekin alfa, an IL-12 anchored drug conjugate, is well tolerated at doses up to 250 µg/mL, exhibits durable local tumor retention, induces recruitment of CD8+ T cells to the tumor microenvironment, increases PD-L1 expression, and may have therapeutic activity. Anchoring IL-12 further resulted in delivering nearly ten-fold higher doses of IL-12 compared to systemic IL-12 without systemic toxicity. Tolododekin alfa merits further investigation for advanced cancer alone and in combination with PD-1/PD-L1 checkpoint inhibitors. Anchored drug conjugates provide a new strategy for improving the therapeutic window of active anti-cancer drugs.
Methods
Patients and eligibility criteria
Patient eligibility included age 18 or greater and presence of a histologically confirmed solid tumor malignancy located in a superficial anatomic site (e.g., cutaneous, soft tissue, or lymph nodes). Patients had metastatic lesions and needed to exhibit progression of disease upon standard of care treatments. All patients were required to have measurable disease per RECIST v1.1 criteria. In addition, patients were required to meet established cardiac, hematologic, hepatic, and renal criteria.
The clinical trial was conducted in accordance with the clinical protocol (included in supplementary information), the Declaration of Helsinki, ICH, and all applicable federal and local regulatory requirements. The clinical protocol was approved by the Institutional Review Boards (IRBs) of Mass General Brigham, Dana-Farber Cancer Institute, National Institutes of Health, WIRB-Copernicus Group, and University Health Network Research Ethics Board at all study sites prior to patient screening. All patients were required to provide written, informed consent prior to any study procedures. The clinical protocol was registered at clinicaltrials.gov (NCT06171750) and is included in the Supplementary Information (Supplementary Note 1).
Study design
The study is an open-label Phase 1 multi-center trial with the primary objective of defining the safety and tolerability of tolododekin alfa. This report describes results from Part 1 of the study, which enrolled patients with superficially accessible solid tumors (Parts 2 and 3 are ongoing and focus on patients with visceral tumors and in PD-1 resistant cutaneous squamous cell carcinoma, respectively). A standard 3 + 3 dose escalation design was utilized using six independent cohorts with tolododekin alfa concentration escalation across the following doses: 2 µg/mL, 6 µg/mL, 20 µg/mL, 60 µg/mL, 120 µg/mL, and 250 µg/mL (Supplementary Fig. 7). The first three cohorts used single patients to accelerate dose escalation based on preclinical modeling, suggesting activity would be more likely at doses >60 µg/mL. To optimize dose selection, some cohorts were backfilled with additional patients. Tolododekin alfa was administered by direct injection every 3 weeks, and the volume was adjusted up to 5 mL total at any visit based on the tumor volume as shown in Supplementary Table 1.
Dose escalation and safety assessment
The incidence and description of DLTs and TEAEs were characterized according to the National Cancer Institute Common Terminology Criteria for Adverse Events v5.0. The study required that the first patient at any given dose be monitored for 21 days prior to enrollment of additional patients to confirm no DLTs. An adverse event was considered dose-limiting if it was possibly, probably, or definitely related to tolododekin alfa, occurred in the first 21 days after drug administration, and met the criteria outlined in Supplementary Table 8. In the event of a DLT, the cohort would be increased to six total patients, and if 2 DLTs occurred, the next lower dose would be considered the MTD. In the event that a DLT occurred in the first three cohorts, the cohort would be expanded to a full six patients. The safety was monitored by a Safety Review Committee (SRC), which was provided information on patient safety and efficacy data, laboratory assessments, and PK and PD data, when available. Dose escalation required approval by the SRC.
Manufacture and analytical characterization of tolododekin alfa
Tolododekin alfa (IL-12-ABP bulk drug substance and drug product) is expressed in a clonal Chinese Hamster Ovary cell line utilizing the leap-in transposase Ò technology (ATUM). The molecule is co-expressed with the human kinase, FAM20C, an enzyme responsible for the phosphorylation of serine amino acids embedded in the C-terminal peptide (ABP) of the molecule. The phosphorylated amino acids are responsible for the binding of the IL-12-ABP to aluminum hydroxide (Alhydrogel®) through ligand exchange. Tolododekin alfa is manufactured at the 1000 L process scale, defined by the nominal volume of the production bioreactor. The cells used to inoculate the production bioreactor originate from a single cell bank vial. Cell culture continues in the production bioreactor until harvest criteria are met. A single bioreactor harvest is purified as a single downstream process consisting of conventional chromatography and filtration steps, resulting in the bulk drug substance. The drug product is manufactured sterile in a liquid formulation utilizing 2R glass vials. Both bulk drug substance and drug product undergo a battery of biochemical release assays, including an assessment of the phosphorylation levels of the drug, and are set on long-term stability studies. In addition, Alhydrogel®, formulated in H2O, is purchased from CRODA (Denmark) and vialed in 2R glass vials. Finally, formulation buffer (diluent) is sterile manufactured in 6R vials and provided to the pharmacies. Tolododekin alfa is combined with appropriate amounts of Alhydrogel® and diluent to generate the clinical doses.
Drug administration
Tolododekin alfa (ANK-101) is composed of two components: an IL-12 with an alum-binding peptide (designated IL-12-ABP) and aluminum hydroxide (Alhydrogel®). The IL-12-ABP is mixed with Alhydrogel® at room temperature for 30 min prior to administration and was delivered by intratumoural injection every 3 weeks for four cycles. At any given visit, patients could have multiple tumors injected, provided these were accessible for injection and the total volume of tolododekin alfa did not exceed 5 mL. Drug volume was adjusted for lesion volume based on the nomogram shown in Supplementary Table 1. Ultrasound imaging was allowed to help guide injections when lesions could no longer be palpated clinically or when deemed safer by the investigator. Patients without significant adverse events or confirmed disease progression could be treated with another four cycles of tolododekin alfa every 3 weeks. While the initial protocol provided for patient follow-up for safety monitoring after 8 cycles, exceptions were made for patients to continue tolododekin alfa injections every 3 weeks beyond the 8 cycles based on the investigator’s impression of clinical benefit to the patient. Continued treatment with tolododekin alfa required approval by the U.S. FDA and local IRB, and all patients provided new written informed consent as well as being treated under a separate, single-patient protocol in each case.
Response assessments
Responses were monitored by modified RECIST v1.1 criteria. The criteria were modified in this study to allow patients with progression to remain on study, provided that there were no significant adverse events or evidence of clinical progression (to accommodate possible pseudo-progression). Patients were evaluable for best objective response assessment provided they had baseline measurements, received at least one dose of tolododekin alfa, and had at least one post-treatment measurement. All patients were required to have baseline CT scans of the chest, abdomen, pelvis, and any specific sites of known disease, as well as a magnetic resonance imaging of the brain. Follow-up imaging with CT scans every 12 weeks was also performed.
Pharmacokinetic assessment
Peripheral blood and tumor biopsy samples were collected pre-dose and at specified time points after tolododekin alfa injection (Supplementary Table 7). For PK measurements, IL-12-ABP was measured using a validated Meso Scale Discovery (MSD) based assay with a lower limit of quantification of 10 pg/mL. IL-12-ABP was captured on a pre-coated ECL-capable plate. After the addition of detection reagent, conjugate, and read buffer, the reaction product is detected using an MSD ECL plate reader. A 5-parameter logistic (5-PL) curve fitting with 1/y2 weighting was used to fit the standard curve. The electrochemiluminescence signal produced is directly proportional to the amount of IL-12-ABP in human serum. PK parameters for IL-12-ABP will be calculated from observed serum concentration data by standard non-compartmental analysis for extravascular administration methods for all subjects in the PK analysis set using Phoenix WinNonlin® version 8.3.4 (Certara, NJ, USA).
Pharmacodynamic assessments
Immunogenicity assessments included characterizing the development of ADA toward IL-12-ABP in serum using classical acid-dissociation combined with a bridging ECL-based validated immunoassay. Briefly, first, the acid-dissociated serum samples and PC (anti-IL-12p70, positive control) are incubated with neutralization buffer and master mix of biotinylated IL-12-ABP and ruthenylated IL-12-ABP. An immune complex is formed between the two IL-12-ABP conjugates and the anti-IL-12-ABP antibody present in human serum samples and PCs during the incubation step. This immune complex is then captured onto a streptavidin-coated MSD plate via the Biotin-Streptavidin bond. Excess unbound conjugate complex is removed by further washing of the wells, followed by the addition of MSD 2X read buffer. The assay plate is then read using an MSD ECL plate reader. The electrochemiluminescence signal (RLU) generated during the plate reading is relative to the amount of anti-IL-12-ABP antibodies present in the PCs and samples tested. All the samples were planned for analysis in a three-tier assay, which includes screening, confirmatory, and titer assays.
The serum cytokine analysis was performed using a qualified electrochemiluminescence-based 10-Plex cytokine panel assay for the determination of IFN-γ, IL-1ß, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p70, IL-13, and TNF-α in human serum. All pro-inflammatory biomarkers are captured on an MSD U-PLEX electrochemiluminescence (ECL) plate. After the addition of conjugate and read buffer, the reaction product is detected using an MSD ECL plate reader. The ECL signal produced is relative to the amount of analyte in human serum. The concentrations of all analytes were back-calculated from the non-linear regression of their respective standard curves.
For tumor biopsies, while freshly obtained biopsies were preferred, archival tissue was used as the baseline sample if the tissue was collected within 12 months of C1D1. When possible, tumor biopsies were done on both injected tumors and non-injected tumors. Paired pre-study and on-study biopsies were subsequently formalin-fixed and paraffin-embedded (FFPE), followed by H&E staining, and analyzed for expression of CD8 (clone C8/144B) and PD-L1 (clone 22C3 pharmDXFDA IVD Kit) by immunohistochemistry (IHC).
For NanoString profiling, RNA was extracted from FFPE slides, and approximately 100 ng of total RNA were run on the PanCancer IO 360™ Panel (Bruker Spatial Biology) per the manufacturer’s recommendation. Data analysis was performed via the IO 360 Data Analysis Service. P values are adjusted within each analysis, gene or signature, and on the grouping variable level difference t-test using the Benjamini and Yekutieli False Discovery Rate adjustment to account for correlations amongst the tests. All models are fit using the limma package in R.
Statistical considerations
Statistical methods were primarily descriptive without formal hypothesis testing. For post hoc analyses, all P values were descriptive, and P < 0.05 was considered significant. No adjustments for multiplicity testing were performed. The data cutoff for this report was December 11, 2024. Categorical variables were summarized using numbers and percentages. Continuous variables were summarized by total number (n), mean, standard deviation, median, and range (minimum and maximum). Data are summarized by dose cohort.
Total enrollment in the Part 1 dose escalation was expected to be 12–36 patients based on 3 single participant dose cohorts at the lowest dose levels and up to 3 additional cohorts of 3–6 DLT-evaluable participants, depending on DLT profile at each dose level. The overall objective response was defined by standard RECIST v1.1 criteria. The best overall response (BOR) was defined as the best objective response achieved at any time and was determined for each participant. Disease control was defined as subjects who achieved the best response of complete response, PR, or SD for at least 12 weeks. Duration of SD was calculated from the start of treatment until the date when PD was documented, or the last study visit, or the end of treatment if no PD had occurred.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data regarding the baseline patient information, survival outcomes, and other detailed therapeutic information have been provided in Table 1 and in the Supplementary Information. The clinical protocol, deidentified patient information, and remaining data are available within the Article, Supplementary Information, and Source data file. Source data are provided with this paper.
References
Sun, Q. et al. Immune checkpoint therapy for solid tumours: clinical dilemmas and future trends. Signal Transduct. Target. Ther. 8, 320 (2023).
Mitra, A. et al. From bench to bedside: the history and progress of CAR T cell therapy. Front. Immunol. 14, 1188049 (2023).
Schwartz, R. N., Stover, L. & Dutcher, J. P. Managing toxicities of high-dose interleukin-2. Oncology 16, 11–20 (2002).
Pachella, L. A., Madsen, L. T. & Dains, J. E. The toxicity and benefit of various dosing strategies for interleukin-2 in metastatic melanoma and renal cell carcinoma. J. Adv. Pract. Oncol. 6, 212–221 (2015).
Suntharalingam, G. et al. Cytokine storm in a Phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N. Engl. J. Med. 355, 1018–1028 (2006).
Segal, N. H. et al. Results from an integrated safety analysis of urelumab, an agonist anti-CD137 monoclonal antibody. Clin. Cancer Res. 23, 1929–1936 (2017).
Salomon, R. & Dahan, R. Next generation CD40 agonistic antibodies for cancer immunotherapy. Front. Immunol. 13, 940674 (2022).
Car, B. D., Eng, V. M., Lipman, J. M. & Anderson, T. D. The toxicology of interleukin-12: a review. Toxicol. Pathol. 27, 58–63 (1999).
Wittrup, K. D., Kaufman, H. L., Schmidt, M. M. & Irvine, D. J. Intratumorally anchored cytokine therapy. Expert Opin. Drug Deliv. 19, 725–732 (2022).
Sheth, R. A. et al. Intratumoral injection of immunotherapeutics: state of the art and future directions. Radiology 312, e232654 (2024).
van Herpen, C. M. et al. Intratumoral administration of recombinant human interleukin 12 in head and neck squamous cell carcinoma patients elicits a T-helper 1 profile in the locoregional lymph nodes. Clin. Cancer Res. 10, 2626–2635 (2004).
Battula, S., Papastoitsis, G., Kaufman, H. L., Wittrup, K. D. & Schmidt, M. M. Intratumoral aluminum hydroxide-anchored IL-12 drives potent antitumor activity by remodeling the tumor microenvironment. JCI Insight 8, e168224 (2023).
Watford, W. T., Moriguchi, M., Morinobu, A. & O’Shea, J. J. The biology of IL-12: coordinating innate and adaptive immune responses. Cytokine Growth Factor Rev. 14, 361–368 (2003).
Del Vecchio, M. et al. Interleukin-12: biological properties and clinical application. Clin. Cancer Res. 13, 4677–4685 (2007).
Koolijman, S. et al. Aluminum hydroxide and aluminum phosphate adjuvants elicit a different innate immu ne response. J. Pharm. Sci. 11, 982–990 (2022).
Atkins, M. B. et al. Phase I evaluation of intravenous recombinant human interleukin 12 in patients with advanced malignancies. Clin. Cancer Res. 3, 409–417 (1997).
Gollob, J. A. et al. Phase I trial of twice-weekly intravenous interleukin12 in patients with metastatic renal cell cancer or malignant melanoma: ability to maintain IFN-gamma induction is associated with clinical response. Clin. Cancer Res. 6, 1678–1692 (2000).
Gollob, J. A., Veenstra, K. G., Mier, J. W. & Atkins, M. B. Agranulocytosis and hemolytic anemia in patients with renal cell cancer treated with interleukin-12. J. Immunother. 24, 91–98 (2001).
Barbosa, M. M. P. et al. Preclinical evaluation of an anchored immunotherapy strategy with aluminum hydroxide-tethered interleukin-12 in dogs with advanced malignant melanoma. Mol. Cancer Ther. https://doi.org/10.1158/1535-7163.MCT-24-0317 (2024).
Mistry, H. B. et al. A pharmacokinetic and pharmacodynamic model of an interleukin-12 (IL-12) anchored drug conjugate for the treatment of solid tumors. Mol. Cancer Ther. https://doi.org/10.1158/1535-7613.MCT-24-1051 (2025).
Fabian, K. P. et al. Alum-anchored IL-12 combined with cytotoxic chemotherapy and immune checkpoint blockade enhanced antitumor immune responses in head and neck cancer models. J. Immunother. Cancer 12, e009712 (2024).
Andtbacka, R. H. et al. Talimogene laherparepvec improves durable response rate in patients with advanced melanoma. J. Clin. Oncol. 33, 2780–2788 (2015).
Goldmacher, G. V. et al. Response criteria for intratumoral immunotherapy in solid tumors: itRECIST. J. Clin. Oncol. 38, 2667–2676 (2020).
Acknowledgements
The authors wish to thank all the patients and their families who participated in the clinical trial. The authors also thank Saran Vardhanabhuti, PhD, for statistical support and Lynn Nicole for regulatory guidance. Funding provided by Ankyra Therapeutics, Inc.
Author information
Authors and Affiliations
Contributions
J.E., G.I., S.B., and H.L.K. conceived and designed the trial. G.I. provided administrative support. J.C.P., B.C., M.B., E.W.K., J.E., G.I., R.T., S.B., H.L.K., and J.M.K.: provision of study materials or patients. All authors collected and assembled data, provided data analysis and interpretation, and manuscript writing. All authors provided accountability of work and final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
J.C.P. reports Institutional research funding provided by A2 Biotherapeutics, ALX Oncology, Ankyra Therapeutics, and Inhibrx. B.C. has served in an advisory role for Merck. He has received honorarium from Clinigen Group and Sanofi, and institutional research funding from Bristol-Myers Squibb and the Clinigen Group. B.C. reports a patent for Biomarkers OX40 response. M.B. has served in an advisory role for Adaptimmune, EMD Serono, Genzyme, Glaxosmithkline, IDEAYA Biosciences, Immunocore, Immunovaccine, InstilBio, Iovance Biotherapeutics, LaRoche Posay, Medison, Novartis, Pfizer, Regeneron, Sun Pharma, and Merck. He received honorarium from Bristol-Myers Squibb, Merck, Novartis, Roche, and Sanofi. M.B. also received research funding and provided expert testimony for Merck. E.W.-K. reports he serves as a consultant for Delcath, Boston Scientific, Emblox, and Sirtex. He is the co-founder of Cytosite and AbscoTx. E.W.-K. serves on an Advisory Board for Delcath and as a member of the Independent Data Monitoring Committee for Replimume. J.E., S.B., and G.I. report employment at Ankyra Therapeutics. R.T. holds stock in Ankyra Therapeutics and is a former employee. H.K. has served in an advisory role at Castle Biosciences, Marengo Therapeutics, Midatech Pharma, Tatum Bioscience, and Virogin Biotech. He reports employment at Ankyra Therapeutics and holds stock in Immuneering and Replimune. H.K. reports honorarium at the Society of Immunotherapy for Cancer. J.M.K. served in an advisory role for Amgen, Ankyra Therapeutics, Applied Clinical Intelligence, AXIO Research, Becker Pharmaceutic, Bristol-Myers Squibb, Cancer Network, Cancer Study group, Checkmate Pharmaceuticals, Cytomx Therapeutics, DermTech, Fenix Group International, Harbour BioMed, Immunocore, iOnctura, Iovance Biotherapeutics, IQVIA, Scopus Biopharma, SR One Capital Management, Takeda, Valar Labs, Istari Ocology, Jazz Pharmaceuticals, Lytix Biopharma, Magnolia Innovation, Merck, Natara, Novartis, Oncocyte, Oncosec, PATHAI, Pfizer, Piper Sandler, PyrOjas Corporation, Regeneron, and Replimune. Institutional research funding provided by Amgen, Bristol-Myers Squibb, Checkmate Pharmaceuticals, Harbour BioMed, Immunocore, Immvira, Iovance Biotherapeutics, Lion Biotechnologies, Novartis, Takeda, and Verastem. J.M.K. has received travel accommodation and expenses from Ankyra Therapeutics, Bristol-Myers Squibb, Checkmate Pharmaceuticals, Iovance Biotherapeutics, and Regeneron.
Peer review
Peer review information
Nature Communications thanks Stephane Champiat and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. [A peer review file is available.]
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Park, J.C., Curti, B., Butler, M. et al. Interleukin-12 anchored drug conjugate (tolododekin alfa) in patients with advanced solid tumors: first-in-human Phase 1 trial. Nat Commun 16, 8567 (2025). https://doi.org/10.1038/s41467-025-63579-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-63579-9
This article is cited by
-
Rewiring tumor cytokine networks to enhance immune checkpoint blockade: mechanisms, engineering, and clinical translation
Journal of Experimental & Clinical Cancer Research (2026)