Abstract
Chagas disease (CD) is an emerging public health concern in Europe. In non-endemic countries, congenital transmission is the main route of new infections. Italy is the second-largest host country in Europe for Latin American migrants and the prevalence of the disease is estimated around 3.5%. The aim is to evaluate the cost-effectiveness of a congenital CD screening program in pregnant women at risk of infection living in Italy and their newborns. We conducted a cost-effectiveness analysis from the perspective of the Italian National Health Service, comparing a screening scenario with a no-screening scenario. A Bayesian decision tree model with a lifetime horizon was developed. In the base-case analysis, the screening strategy yielded an incremental cost-effectiveness ratio of €15,193 per quality-adjusted life year gained (95% CI: €14,885–€15,552), falling well within the accepted cost-effectiveness threshold (€30,000–€50,000) in Italy. Probabilistic sensitivity analysis confirmed the robustness of these findings. Here we show that screening for congenital CD is a cost-effective strategy that improves health outcomes and aligns with international public health priorities. Our findings support the implementation of a national screening program integrated within existing maternal care pathways, contributing to the prevention of neglected tropical diseases and the promotion of migrant health.
Similar content being viewed by others
Introduction
Chagas disease (CD), caused by the protozoan Trypanosoma cruzi, is a major emerging parasitic infection worldwide and particularly in Europe, primarily driven by the increasing transnational migration1. Despite its growing public health relevance, CD often remains underdiagnosed2 due to limited clinical experience among healthcare providers, restricted access to screening for at-risk populations, and the prolonged asymptomatic course that characterizes many cases during the chronic phase.
While vector-borne transmission is restricted to endemic regions of North, Central, and South America, non-vectorial transmission routes, including organ and bone marrow transplantation, blood transfusion, and congenital transmission, play a significant role in sustaining CD in non-endemic areas3,4. Among these, mother-to-child transmission represents the primary infection route in non-endemic countries5. The main biological determinant for congenital transmission is maternal parasitaemia, but other factors can be involved (e.g., strain of the parasite, placental factors, cellular immune response)5,6.
CD typically progresses through two main phases. The acute phase is asymptomatic or presents with mild, nonspecific symptoms in 90–95% of cases. If left untreated, the infection transitions into a lifelong chronic phase. In this phase, CD can remain in an indeterminate form (i.e., without clinical manifestations) or progress to symptomatic chronic disease in 30–40% of cases, primarily affecting the cardiovascular or gastrointestinal systems, usually 10–30 years after the initial infection7.
The available etiological treatment consists of antitrypanosomal drugs (benznidazole and nifurtimox)6. Treatment efficacy is >90% in children and therefore in congenital cases, especially when administered within the first year of life8,9. However, effectiveness in chronic cases declines significantly by time10,11. The treatment of women in reproductive age before pregnancy significantly reduces the congenital transmission of CD with no cases of mother-to-child transmission in treated compared with untreated women12. In the absence of trypanocidal therapy, the infection can be transmitted to the fetus during any pregnancy, even in the case of women with chronic infection who no longer reside in endemic regions13,14 or who acquired the infection congenitally in non-endemic areas. Due to safety concerns, treatment during pregnancy and lactation is not recommended6.
CD affects an estimated 6–7 million people worldwide, causing ~12,000 deaths annually15. In 2019, among endemic countries for CD, Bolivia was the country with the highest prevalence rate per 100,000 population (4993.53), followed by Venezuela (1654.73), Argentina (1524.07), Chile (1114.17), Mexico (1030.50), and Brazil (912.36; 95% UI : 788.20–1048.06)16. The chronic phase of CD accounts for 806,000 disability-adjusted life years (DALYs) per year globally, including 6093 DALYs in European countries. Beyond its clinical impact, CD poses a significant economic burden, with estimated global healthcare costs exceeding $627 million per year, of which nearly $17 million is attributable to Europe17.
The estimated prevalence of CD in non-endemic countries varies depending on the region and population studied. A systematic review and meta-analysis estimated the overall prevalence among Latin American migrants in non-endemic countries at 3.5% (95% CI: 2.5–4.7)18. By subgroup, the estimated pooled prevalence of CD was 11.0% (95% CI: 7.7–15.5) in non-targeted screening populations (unselected individuals at reference centers) based on 27 studies. Among blood donors (4 studies), the prevalence was 0.8% (95% CI: 0.2–3.4). In Latin American immigrants living with HIV (4 studies), it was 2.4% (95% CI: 1.4–4.3), while for Latin American pregnant and postpartum women (14 studies), the prevalence was 3.7% (95% CI: 2.4–5.6)18.
Italy is the second largest recipient of Latin American migrants in Europe19. In 2024, Italy reported 382,000 regular residents originating from Latin America. Among them, 3.3% were from Bolivia, 3.9% from Venezuela, 3.9% from Argentina, 0.9% from Chile, 1.4% from Mexico, and 13.6% from Brazil. These figures do not account for undocumented migrants, whose numbers are inherently difficult to estimate, and therefore likely underestimate the true size of the Latin American population in Italy20. Given the potential risk of congenital transmission, pregnancy represents a crucial window of opportunity for screening and early detection of CD13. Although national guidelines for the physiologic pregnancy containing among others, congenital Chagas disease (cCD) screening recommendations, have been issued by the Italian National Institute of Health (ISS), they are currently limited in scope for this topic and lack a coordinated national implementation strategy21. Only few regional and local screening initiatives have been implemented in Italy to detect CD in at-risk pregnant women (e.g., Tuscany, Lazio, Lombardy, and Emilia-Romagna). Our study models the full integration of above mentioned guidelines into a structured national program, extending beyond maternal serological testing to encompass the complete diagnostic and therapeutic management of infected newborns. This distinction is critical for understanding the policy gap and the potential impact of nationwide implementation.
Economic evaluations have assessed CD screening in non-endemic settings, either targeting the general Latin American population19,22,23,24,25,26,27 or focusing specifically on preventing congenital transmission28,29,30. However, no cost-effectiveness analysis has been conducted specifically for the Italian context, despite the country’s significant Latin American migrant population, as also pointed out by the ISS21. In Italy, the National Health Service (NHS) guarantees all citizens universal access to equitable healthcare services under conditions of equality. Citizens receive healthcare services from the NHS without any distinction based on individual, social, or economic conditions; it is funded through general taxation and co-payments required from non-exempt citizens31. Given these characteristics, the NHS represents the best perspective for implementing screening in an ethnic minority, as opposed to other type of health systems. The objective of this study is to conduct a cost-effectiveness analysis of implementing a CD screening program in pregnant women at risk of infection living in Italy and their newborns, aiming to prevent congenital transmission and subsequent disease development.
Results
Base case results
A cohort of 1000 newborns born to Latin American pregnant women was included in the analysis. As expected, the base case analysis revealed that, given the chosen threshold of €30,000 to €50,000 per quality-adjusted life years (QALY) gained, the screening strategy emerged as a cost-effective dominant intervention compared with the no screening option (ICER of €15,192 [95% CI, €14,885–€15,552] per QALY gained). Table 1 presents the mean costs, effectiveness, and base-case results for the simulated cohort.
Sensitivity analysis
Figure 1 illustrates the cost-effectiveness plane (CEP), reaffirming the robustness of the initial findings within the chosen willingness-to-pay (WTP) threshold.
Contour plots further reveal that the majority of simulated points for the two strategies were positioned in the northeast quadrant of the CEP, implying that CD screening program offers greater effectiveness at a higher cost compared to the no screening alternative. Specifically, 76% of simulations fell within this quadrant (Figs. S1 and S2).
Additionally, Figs. S3 and S4 in supplementary materials present the cost-effectiveness acceptability curve (CEAC) and the cost-effectiveness acceptability frontier (CEAF), respectively. The findings suggest that no screening remains the optimal choice for WTP thresholds below €15,192 per QALY gained. Nonetheless, for WTP levels above €15,192 per QALY gained screening option demonstrated the highest probability of being cost-effective (69%). As depicted in Fig. S5, the expected incremental benefit (EIB) was positive at a WTP of €15,300, with a value of 631 for screening vs. no screening option.
In the sensitivity analysis using a context-specific prevalence of 7.5%, the screening strategy remained dominant with an incremental cost-effectiveness ratio (ICER) of €15,042 per QALY and a 73% probability of being cost-effective at a €30,000–€50,000 threshold.
Value of information analysis
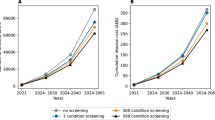
From the probabilistic sensitivity analysis (PSA) simulation, the Expected Value of Perfect Information (EVPI) per patient was estimated at €206 when applying a WTP threshold of €50,000 per QALY gained (Fig. 2). As the WTP threshold decreased, the EVPI also declined, reaching €157 at a WTP level of €30,000 per QALY gained (Fig. 2).
The analysis of the Expected Value of Partially Perfect Information (EVPPI), for a subset of specific parameters (i.e., probabilities, costs, and utilities), resulted in an EVPPI of €30, €2, and €43, respectively (Figs. S6–S8).
Moreover, as illustrated in Fig. S9, the probability of developing the indeterminate form of the disease exhibited the highest ratio, underscoring the substantial expected value of acquiring additional information for this parameter.
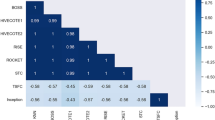
Diagnostic performance analysis
The Markov Chain Monte Carlo (MCMC) performance was gauged using various diagnostic measures to ensure robustness. Trace plots demonstrated that the sampled parameter chains exhibited stable behavior and substantial overlap, indicating convergence. Furthermore, density plots revealed smooth, unimodal distributions, suggesting that the posterior distributions were well-behaved. The Gelman–Rubin diagnostic yielded R-hat values close to 1 for all parameters, further confirming the convergence of the chains. Moreover, the effective sample size (ESS) was close to 15,000 for most parameters, highlighting efficient sampling and reliable estimation of the posterior distribution.
Overall, these diagnostic assessments confirmed that the MCMC algorithm performed effectively, with well-converged chains, high ESS values, and accurately estimated posterior distributions, thereby reinforcing the validity and reliability of the obtained results.
Discussion
The analysis showed that screening for T. cruzi in Latin American pregnant women at risk of infection, tested in secondary care settings, is a cost-effective strategy in Italy at all WTP thresholds considered, for treating newborns with cCD and preventing chronic progression of such disease. The screening alternative is not only cost-effective for the healthcare system compared to the no screening scenario, but it also significantly improves patients’ quality of life, as measured in QALYs.
These results corroborate the findings of previous economic evaluations conducted in similar settings. In the USA context, screening is estimated to save $1324 per birth, translating into a total saving of $636 million for each annual cohort of 480,000 births among women originating from endemic regions30. Sicuri et al. showed that, in Spain, screening pregnant Latin American women and their newborns was more effective and less costly than no screening. The cost-effectiveness ratio was €22/QALY (neonatal model) and €96/QALY (maternal model), compared to €125 and €1675/QALY for no screening28. Imaz-Iglesia et al. conducted a cost-utility analysis comparing four strategies from both the societal and Spanish NHS perspectives. Screening Latin American pregnant women and their newborns proved to be a dominant strategy compared to no screening, both from a societal and a healthcare system perspective29.
These overlaps with the literature indicate that screening programs are both economically viable and beneficial in non-endemic countries with socioeconomic contexts and immigration flows comparable to those of Italy. Despite being the second-largest European host country for Latin American migrants19,32, Italy has yet to implement a national screening program for cCD. Although the ISS has recently issued recommendations for screening, systematic testing still remains limited to regional or local initiatives26,33,34.
From a public health perspective, the implementation of a screening program for cCD offers significant health benefits and is closely aligned with the objectives of the United Nations Sustainable Development Goal 3. Specifically, by preventing the vertical transmission of CD, a major neglected tropical disease, such a program directly supports Target 3.3, which aims to end the epidemics of AIDS, tuberculosis, malaria, and neglected tropical diseases by 2030, and to combat other communicable diseases35. The methodologies applied and the main findings reported in this study provide a structured framework for assessing this screening program from a value-based perspective. Such an approach promotes a sustainable healthcare system by jointly considering treatment quality and associated costs36. This framework can be effectively extended to other screening programs, not only for infectious diseases but also for multifactorial conditions.
From a Public Health perspective, this value-based intervention is particularly relevant when viewed through the lens of equity in a country with universal health coverage, as it targets an ethnic minority that may face communication and economic barriers, as well as a lack of information regarding access to and the services offered by the national health system23,37. To adequately address these issues, it is essential to implement effective and coordinated actions across various levels of the health system, involving multiple professional roles.
At the macro level, national authorities must establish regulations for the implementation of CD screening, ensuring adequate resource allocation. A major challenge at this level is overcoming political and economic barriers, as there might be competing public health priorities. Regional governments should then define the organization of screening. At the meso level, local health authorities and healthcare organizations are responsible for assessing health needs and the collection of data on health outcomes related to CD. They are also in charge of establishing care pathways to ensure access for minority populations, involving both healthcare staff and other stakeholders from the third sector13,38. In the initial phase, this can be problematic due to the limited human resources to allocate, the difficulty in identifying the right interlocutors for assessing health needs and the lack of indicators based on computerized systems that allow for timely monitoring of the situation. Lastly, at the micro level, raising awareness of CD among all healthcare providers, especially primary care physicians, obstetricians, gynaecologists, pediatricians, and infectious disease specialists is of paramount importance to ensure the uptake and proper management of screening programs, thus improving precision medicine interventions34.
This study demonstrates the cost-effectiveness of a secondary prevention intervention, highlighting how the early detection of health needs and timely treatment allow for a more efficient use of resources in a public system with limited resources; this follows the same rationale present in other pathways implemented at the national level, which involve a shift from a purely clinical-care perspective to a broader one that encompasses both preventive and clinical-care aspects39. Moreover, as the cost of managing indeterminate forms was a key driver of model uncertainty, shifting follow-up care to primary health settings, as recommended by WHO, could reduce costs and improve program sustainability10,40,41.
This analysis includes certain limitations. While a Markov model could have offered a more granular depiction of the long-term natural history of CD, we opted for a decision tree model to preserve structural and computational simplicity, particularly within a Bayesian framework. Variations in downstream healthcare costs were handled by assigning condition-specific cost estimates to terminal health states, and parameter uncertainty was addressed through PSA. There is a lack of data on the QALYs of CD patients in non-endemic regions, and the utility values used were derived from studies conducted in endemic areas42. The use of utility values derived from endemic countries may not fully reflect the lived experience and healthcare trajectories of patients in European settings, potentially underestimating the perceived quality-of-life gains associated with early detection and treatment in non-endemic contexts. Notwithstanding, they represent the latest updated available data. Moreover, the potential reduction in congenital transmission in future pregnancies following maternal treatment was not included due to limited and heterogeneous data on this effect, which precluded reliable modeling.
The model assumes 100% treatment efficacy for newborns diagnosed with cCD. While this may slightly overestimate the intervention’s effect, incorporating additional health states to reflect the small proportion of potential non-responders would have added complexity and uncertainty. This approximation is expected to have a negligible impact on the overall cost-effectiveness outcome, particularly given the very high success rates observed in early-treated infants and the conservative nature of all other assumptions, which consistently tend to underestimate the ICER.
In the no screening option, several approximations were made that may underestimate the positive impact of the intervention analysed in this study, as follow: (i) second-level diagnostic tests (e.g., cardiac MRI), which are indicated in selected cases of symptomatic chronic CD, were not included in the model43,44,45; (ii) diagnostic and therapeutic interventions that may be inappropriately prescribed due to the limited awareness of CD among healthcare providers in non-endemic countries were not considered46; (iii) mixed forms of CD, involving both cardiac and gastrointestinal manifestations, were not accounted for. The costs of CD treatment were estimated under the assumption that biotechnology remains constant over time, despite the applied discount rate. Potential cost variations due to advancements in biotechnology could not be anticipated. The costs associated with the nationwide logistical implementation were not considered in this study. However, they are expected to be minimal. This is justified by the fact that the diagnostic tests required for CD screening do not entail additional structural or logistical expenses for the Italian NHS. Another caveat refers to the perspective adopted. The analysis was conducted from the healthcare system perspective and did not include societal costs, such as lost productivity or caregiving burden, which may underestimate the full economic impact on migrants and their families. Nonetheless, adopting a healthcare payer perspective aligns with standard economic evaluation practices for informing policy decisions in publicly funded systems. Furthermore, implementation-related costs (e.g., training of healthcare providers) were not explicitly modeled; notwithstanding, such costs are typically modest relative to the overall program cost and could be integrated into future real-world cost evaluations. In addition, the model did not incorporate the potential screening or treatment of siblings of diagnosed children, which may slightly underestimate the public health benefit of a screening program. Another limit was the assumption of full access and uptake of healthcare services, which may not reflect real-world variability in healthcare access among undocumented or underserved migrant populations. However, this assumption allows for a best-case scenario analysis of the program’s potential under optimal implementation conditions. This analysis did not explicitly model correlations among cost parameters, and prior distributions were based on conventional choices from the health economic modeling literature. However, key model parameters were tested in the PSA using distributional uncertainty. Furthermore, the model assumes that no prior diagnosis or alternative detection occurs outside the screening program; while some cases may be identified opportunistically, particularly in regions like Tuscany with existing initiatives, such events are rare and lack sufficient data to be formally incorporated into the model.
As highlighted in other studies, assessing the quality of life of CD patients in non-endemic regions should be prioritized in future research efforts23,28. Dynamic models that consider demographic and migration flows could therefore be a strategy to adapt the results of this study to different contexts. Finally, further research is needed to assess the acceptability and feasibility of screening from the perspective of both healthcare providers and at-risk populations. Our findings highlight that uncertainty in the probability of progression to the indeterminate form plays a key role in the variability of cost-effectiveness outcomes, suggesting that further research to refine this parameter could strengthen future evaluations. Further studies should also explore subgroup analyses comparing high- and low-prevalence migrant populations to better inform screening prioritization, though such analyses are currently limited by the availability of disaggregated epidemiological data. Future Bayesian modeling efforts may benefit from exploring informative priors, hierarchical structures, or correlation matrices to capture interdependencies among clinical and economic parameters more fully.
This study provides strong economic evidence supporting the implementation of a national cCD screening program for pregnant women at risk in Italy. Beyond its economic justification, implementing a national screening program would contribute to the United Nations Sustainable Development Goal 3, addressing the burden of neglected tropical diseases and promoting migrant health. Our results offer concrete guidance for policymakers, supporting the development of a structured screening strategy in Italy and other non-endemic countries. Integrating cCD screening into existing maternal care pathways could significantly reduce the prevalence and burden of CD, improving health outcomes for both mothers and newborns, while aligning with international public health priorities.
Methods
Target population
This study focuses on evaluating the cost-effectiveness of a screening for the prevention of cCD in our country. The target population of this study consists of newborns born to women at risk in Italy. According to the World Health Organization and ISS21, women are considered at risk if they were born in one of the 21 endemic countries for the infection (i.e., Argentina, Belize, Bolivia, Brazil, Chile, Colombia, Costa Rica, Ecuador, El Salvador, Guatemala, Guyana, French Guiana, Honduras, Mexico, Nicaragua, Panama, Paraguay, Peru, Suriname, Uruguay, Venezuela) or were born to a mother from one of these countries; if they have received blood transfusions in one of the 21 endemic countries; and/or if they have resided in one of the 21 endemic countries for more than six months10. A detailed description of the target population in Italy is provided in the supplementary materials.
Study perspective, setting, and location
The cost-effectiveness analysis was performed according to the Italian NHS perspective.
Intervention and comparator
This economic evaluation involved the comparison between an organized screening program for CD (i.e., intervention) with a scenario in which no formal screening program is implemented (i.e., comparator).
Several screening strategies for cCD are currently reported in the literature47. Since our study analyses this program in the Italian context, we have chosen to use national guidelines provided by the ISS and the protocol implemented in the Tuscany Region, as main references21,48. Infectious disease screenings offered during pregnancy are included in the Essential Levels of Care (LEA) related to territorial healthcare, particularly within the “birth pathway”. Therefore, they are provided by the NHS without co-payment in all regions. These screenings represent an example of secondary prevention. Referring to the CD screening program, in Italy, all pregnant women at risk should be offered serological screening at their first prenatal visit, or at the time of delivery if testing has not previously been performed. Screening is performed in qualified laboratories with external quality control (i.e., secondary care), and positive results are confirmed using a second, different test. Women with a confirmed diagnosis are referred to specialized infectious or tropical disease units (i.e., tertiary care) for counseling and treatment after pregnancy and breastfeeding completion49.
In our model, the intervention consists of a cCD screening program targeting newborns at risk, operationalized through maternal screening during pregnancy. The first step is identifying infants at risk of cCD testing their mothers—specifically, pregnant women born in or with relevant epidemiological exposure to endemic countries—for anti-T. cruzi IgG antibodies. When maternal serology is positive, the newborn is flagged as at risk and enters a diagnostic and therapeutic pathway, including parasitological testing (e.g., PCR, blood smear), serologic follow-up, and, if confirmed infected, prompt antiparasitic treatment within the first year of life21,48,50. This sequence is crucial, as early treatment has near-perfect efficacy and prevents the progression to chronic CD10. Newborns diagnosed with cCD in the intervention arm were assumed to transition directly to the “Newborns healed” health state, based on an assumed treatment efficacy of 100%. This modeling decision is supported by robust clinical evidence indicating that antiparasitic therapy initiated within the first year of life achieves cure rates consistently above 90% and often approaching 100% in real-world settings43,51. Further support comes from studies reporting very low rates of cardiac complications among early-treated infants, highlighting the strong protective effect of prompt treatment52,53,54,55. Introducing additional health states to account for the small proportion of potential non-responders would have unnecessarily increased model complexity and uncertainty, with negligible impact on overall cost-effectiveness outcomes. While this assumption may modestly overestimate the intervention’s benefit, it contrasts with other conservative assumptions in the model, which consistently tend to underestimate the ICER. Further details are provided in the Supplementary Materials.
In the other alternative (i.e., comparator), the natural history of the disease was reconstructed in the absence of a screening program. In the first step of this scenario, cases of cCD remain undiagnosed. The same occurs in real-world clinical practice in non-endemic settings that have not implemented a screening program, due to the asymptomatic presentation or nonspecific nature of clinical manifestations at birth, and lower prevalence of the disease in Europe, which results in less clinical exposure and experience among healthcare providers33,55,56.
Further details on the description of the intervention and comparator are available in the supplementary materials.
Time horizon, discount rate, and threshold
A lifetime time horizon was selected under the assumption that this duration is appropriate for capturing the long-term benefits of the intervention. In the decision-tree framework, terminal branches incorporate the expected lifetime costs and QALY associated with each health state. Regarding the cost-effectiveness threshold, a decision was made to adopt the Eurozone range of €30,000 to €50,000 per QALY, guiding the evaluation of which alternative should be supported57,58.
Model structure
Type of model
A Bayesian decision tree model was developed to compare two distinct strategies, as illustrated in Fig. 3. The model follows a structured process: in the CD screening program arm (i.e., lower pathway), pregnant women undergo screening for CD. If the mother is not infected, the newborn remains unaffected. If the mother is infected, there is a probability that the newborn may also be infected. Infected newborns receive treatment, leading to complete healing. In the no-screening arm (i.e., upper pathway), pregnant women do not undergo screening, and newborns of infected mothers may contract the disease undiagnosed. Without early treatment, infected newborns follow a probabilistic disease progression, which may include remaining in an indeterminate form, developing symptomatic chronic disease (i.e., cardiac or gastrointestinal), or, in rare cases, neonatal death.
The figure depicts the decision-analytic framework used to compare a targeted screening strategy with a no-screening strategy over a lifetime horizon. The model begins at a decision node (square), representing the choice between implementing a screening program for pregnant women from Chagas-endemic countries or not screening. Each branch leads to chance nodes (circles), which represent clinical or epidemiological events with assigned probabilities. Terminal nodes (triangles) represent the end of each modeled pathway, where cumulative costs and health outcomes are calculated.
In the model, death was not explicitly included as a terminal health state for symptomatic forms; instead, its impact was indirectly captured through fixed durations in symptomatic states and associated utility weights reflecting morbidity and reduced survival.
The Bayesian framework facilitates the estimation of a full probability distribution for a two-dimensional outcome, denoted as θ = (c, e), which represents cost and effectiveness combinations. This approach eases (i) the conduction of decision analyses using expected values, and (ii) the implementation of probabilistic sensitivity analyses to assess the degree of uncertainty in the decision-making process. According to Bayes’ theorem, the posterior probability of θ given the observed data (D) can be expressed as:
where p(θ∣D) is the posterior distribution, reflecting updated beliefs about θ after incorporating observed data; p(θ) represents the prior distribution, encapsulating prior knowledge or assumptions about θ before data are observed; p(D∣θ), known as the likelihood, indicates the probability of obtaining the observed data under a given parameter value θ; and p(D), or evidence (marginal likelihood), is the overall probability of the observed data across all possible values of θ, weighted by their prior plausibility.
A key computational challenge in Bayesian inference arises from the need to evaluate the marginal likelihood, which involves integrating over a continuous parameter space. Since this integral is often intractable, numerical techniques such as MCMC are employed to approximate the posterior distribution. MCMC algorithms generate samples from the posterior distribution without directly computing the complex integral in Bayes’ formula, relying instead on iterative sampling methods. In this study, the Gibbs sampler was adopted, a widely applied MCMC algorithm, to draw a large number of samples from p(θ∣D). When the number of simulations (S) approaches infinity, the estimated posterior distribution converges to the true posterior with probability one. To ensure the reliability of the MCMC-generated posterior samples, several diagnostic tools were employed to assess convergence, accuracy, and efficiency. Graphical diagnostics, including trace plots and density plots, were used alongside statistical measures such as the Gelman–Rubin statistic and autocorrelation analysis. The trace plot visually represents multiple parallel MCMC chains, where overlapping trajectories indicate successful exploration of the same posterior distribution. The Gelman–Rubin statistic quantitatively assesses convergence by comparing within-chain variability to between-chain variability. A value close to 1 suggests that the chains have mixed well and have likely converged to the target distribution, whereas values greater than 1 indicate inadequate convergence, suggesting further iterations may be required. To evaluate MCMC accuracy, we examined the ESS, which accounts for the autocorrelation within chains. Since MCMC samples are not independent, ESS provides an estimate of the number of uncorrelated samples that would yield equivalent statistical information. A recommended threshold for stable 95% highest posterior density intervals is an ESS of at least 15,000, ensuring robust inference.
Model inputs
Probabilities were derived from the relevant literature, as were the probabilities of tests or treatments being undertaken. The probability that the mother has or does not have CD, in both the screening and no screening arms, corresponds to the prevalence of the disease among Latin American immigrants in non-endemic countries, as estimated in a systematic review and meta-analysis (3.5%)18. In both arms, the probability of vertical transmission is derived from the results of a systematic review (and meta-analysis), which is 3.5%59. In the screening scenario, for newborns affected by cCD, the efficacy of antiparasitic therapy was approximated to 100%29,60. In the no screening option, for newborns affected by cCD, two scenarios were considered: neonatal death in 2.2% of cases61, or survival with progression to a chronic indeterminate form in the remaining cases. The latter scenario includes two possible outcomes: in 65% of cases, the individual remains in a subclinical state of chronic indeterminate form for life, while in 35% of cases, the individual develops a symptomatic chronic form of the disease5. Among those who progress to a symptomatic form, 33% develop a gastrointestinal form, while 67% develop a cardiac form of CD6.
Only direct costs were included in the model, as for the selected perspective. All examinations, medical procedures, and outpatient evaluations were retrospectively reviewed by experienced infectious disease specialists. For both the two arms, costs related to diagnostic and therapeutic procedures were retrieved from official Italian institutional sources, including national and regional healthcare tariffs and publicly available administrative documents. Overall costs were estimated by multiplying the resources required for each activity by the corresponding unit cost. For treatment-related costs, the estimation also accounted for the posology and the probability of requiring specific resources. Costs were expressed in 2024 Euros (€).
Utility values for each health state were derived from Wilson et al., a study conducted in endemic areas of Latin America, and have been widely used in prior cost-effectiveness analyses of CD, including those conducted in non-endemic countries such as Spain and Japan22,23,42,62,63,64.
The quality weights amounted to 0.9625 for the indeterminate form, 0.7171 for the cardiomyopathy and 0.80 for gastrointestinal forms42. To date, no utility estimates are available from European populations affected by CD.
Further details about the parameters adopted for the base-case analysis are listed in Table 2.
Model outcomes
The model primary outcomes consist of the total QALY, the expected costs, and the ICER between the two options. To determine the expected cost for each branch of the decision tree, individual cost components are weighted by the quantity of healthcare resources utilized by the patient while occupying a specific health state within a given study arm.
Model analyses
To account for uncertainty in the estimated mean outcomes, a PSA was performed. Each model parameter was assigned a probability distribution reflecting its underlying characteristics. A beta distribution was used to model probabilities and utilities, while costs followed a log-normal distribution. A comprehensive list of model parameters, along with their respective ranges used in the PSA, is provided in Table 1. Probability distributions for model parameters were selected based on standard conventions in health economic modeling65,66. For the PSA, 100,000 MCMC simulations were executed using the Gibbs sampling algorithm. This approach involved drawing random parameter sets from their respective probability distributions and computing incremental costs, incremental effectiveness, and ICERs for each set. A sensitivity analysis was conducted on the prevalence of T. cruzi infection, varying it across context-specific values, including an overall estimate derived from a recent Italian study. This estimate captures the current demographic profile of communities, which alongside Bolivians includes substantial numbers of Peruvians, Ecuadorians, and Salvadorans. Using this context-specific prevalence in the sensitivity analysis allowed us to test the robustness of findings under an epidemiological scenario that more accurately represents the present migrant population in Italy33. The results were visualized using standard economic evaluation tools, including the CEP, CEACs, and the CEAF. These visualizations align with the best practice recommendations outlined by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR)67. Specifically, the CEAC illustrates the probability that each intervention would be deemed cost-effective at different WTP thresholds, while the CEAF presents the net monetary benefit associated with each WTP value and the corresponding level of uncertainty regarding the optimal choice. Additionally, EIBs were calculated to compare the screening option with the no screening alternative. To assess the value of reducing uncertainty in the cost-effectiveness of establishing a screening program, the EVPI and the EVPPI were also estimated. The EVPI at a given WTP threshold was determined by computing the difference between the expected value under perfect information (i.e., model parameters are known with certainty) and the expected value under current uncertainty65. This metric helps quantify the potential benefit of conducting further research to resolve uncertainties in the cost-effectiveness of the CD screening program in pediatric patients.
Furthermore, EVPPI was calculated to gauge the value of reducing uncertainty in specific model parameters, highlighting which parameters have the greatest impact on cost-effectiveness estimates and should be prioritized for further investigation. To support this analysis, an information-rank plot was generated, where a bar chart was used to depict the ratio of EVPPI to EVPI across different WTP thresholds, thereby identifying the most influential parameters in terms of expected value of information.
This study adhered to the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) guidelines68, ensuring methodological rigor and transparency. All statistical analyses and simulations were performed using R software (R Development Core Team) using the package BCEA69.
Ethics and inclusion
This study was conducted in Italy, a non-endemic country for Chagas disease, and involved the development of a health economic model based on secondary data from the scientific literature and publicly available administrative healthcare sources. No primary data collection or human participant recruitment took place.
The research did not involve direct collaboration with researchers based in endemic areas. However, several co-authors have longstanding expertise in the clinical management and public health aspects of Chagas disease in both endemic and non-endemic contexts. Moreover, the study design and assumptions were informed by internationally recognized evidence, including prevalence estimates and utility values derived from Latin American settings, with appropriate citations acknowledging those contributions.
The topic of the research, congenital Chagas disease, is of direct relevance to Latin American migrant populations residing in Italy and aligns with national and international public health priorities. The study supports the development of evidence-based policies to enhance equity in healthcare access for migrant communities in non-endemic countries.
All roles and responsibilities among the co-authors were clearly defined at the outset, and contributions were aligned with ICMJE authorship criteria.
There was no transfer of biological materials, cultural artifacts, or traditional knowledge in this work. No stigmatizing or discriminatory risks to individuals or populations arose from this research. The analysis adhered to the highest ethical and scientific standards, and all data used were either publicly available or anonymized secondary sources.
Local research relevant to the subject matter, including regional screening programs and national guidelines issued by Italian health authorities, was thoroughly cited and incorporated into the modeling framework.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data used in the analysis are comprehensively listed in Table 2 in the Methods section. The output data generated from this study are fully presented in the Results section and accompanying Supplementary Materials.
Code availability
All code used to generate the results of this study is available on Zenodo70. The archive contains the R scripts for data preparation and analysis, utility functions, plotting and EVPPI codes, and a README with step-by-step instructions. The code is released under the MIT License.
References
Gonzalez-Sanz, M. et al. Chagas disease in Europe. Trop. Med. Infect. Dis. 8, 513 (2023).
Basile, L. et al. Chagas disease in European countries: the challenge of a surveillance system. Eur. Surveill. Bull. 16, 19968 (2011).
Shikanai-Yasuda, M. A. & Carvalho, N. B. Oral transmission of Chagas disease. Clin. Infect. Dis. 54, 845–852 (2012).
Beatty, N. L. & Klotz, S. A. Autochthonous Chagas disease in the United States: how are people getting infected?. Am. J. Trop. Med. Hyg. 103, 967–969 (2020).
Rassi, A. J., Rassi, A. & Marin-Neto, J. A. Chagas disease. Lancet Lond. Engl. 375, 1388–1402 (2010).
Pérez-Molina, J. A. & Molina, I. Chagas disease. Lancet Lond. Engl. 391, 82–94 (2018).
Pinto Dias, J. C. Natural history of Chagas disease. Arq. Bras. Cardiol. 65, 359–366 (1995).
Russomando, G. et al. Treatment of congenital Chagas’ disease diagnosed and followed up by the polymerase chain reaction. Am. J. Trop. Med. Hyg. 59, 487–491 (1998).
Schijman, A. G. et al. Aetiological treatment of congenital Chagas’ disease diagnosed and monitored by the polymerase chain reaction. J. Antimicrob. Chemother. 52, 441–449 (2003).
World Health Organization. Guidelines for the Diagnosis and Treatment of Chagas Disease. https://www.who.int/publications/i/item/9789275120439 (2019).
Coura, J. R. & Borges-Pereira, J. Chronic phase of Chagas disease: why should it be treated? A comprehensive review. Mem. Inst. Oswaldo Cruz 106, 641–645 (2011).
de Moraes, F. C. A. et al. Prevention of congenital chagas disease by trypanocide treatment in women of reproductive age: a meta-analysis of observational studies. PLoS Negl. Trop. Dis. 18, e0012407 (2024).
Edwards, M. S. & Montgomery, S. P. Congenital Chagas disease: progress toward implementation of pregnancy-based screening. Curr. Opin. Infect. Dis. 34, 538–545 (2021).
Edwards, M. S., Stimpert, K. K., Bialek, S. R. & Montgomery, S. P. Evaluation and management of congenital Chagas disease in the United States. J. Pediatr. Infect. Dis. Soc. 8, 461–469 (2019).
World Health Organization. Chagas disease (American trypanosomiasis). World Health Organization https://www.who.int/health-topics/chagas-disease#tab=tab_1 (2025).
Gómez-Ochoa, S. A., Rojas, L. Z., Echeverría, L. E., Muka, T. & Franco, O. H. Global, Regional, and National Trends of Chagas Disease from 1990 to 2019: comprehensive analysis of the Global Burden of Disease Study. Glob. Heart 17, 59 (2022).
Lee, B. Y., Bacon, K. M., Bottazzi, M. E. & Hotez, P. J. Global economic burden of Chagas disease: a computational simulation model. Lancet Infect. Dis. 13, 342–348 (2013).
Nepomuceno de Andrade, G. et al. Prevalence of Chagas disease among Latin American immigrants in non-endemic countries: an updated systematic review and meta-analysis. Lancet Reg. Health Eur. 46, 101040 (2024).
Rodari, P. et al. Congenital Chagas disease in a non-endemic area: Results from a control programme in Bergamo province, Northern Italy. Travel Med. Infect. Dis. 25, 31–34 (2018).
Istituto Nazionale di Statistica. Resident Population as of January 1, 2024 by Sex and Single Citizenship. https://demo.istat.it/app/?i=RCS&l=it.
Istituto Superiore di Sanità. Antenatal Care for Uncomplicated Pregnancy. PART ONE. Section 1 - Information for Pregnant Women. Section 2 - Screening for Infections in Pregnancy. https://www.epicentro.iss.it/itoss/pdf/LG-Gravidanza-Fisiologica-Parte1_protetto.pdf (2023).
Requena-Méndez, A. et al. Cost-effectiveness of Chagas disease screening in Latin American migrants at primary health-care centres in Europe: a Markov model analysis. Lancet Glob. Health 5, e439–e447 (2017).
Iglesias Rodríguez, I. M. et al. Analysis of the Chagas disease situation in Japan: a cross sectional study and cost-effectiveness analysis of a Chagas disease screening program. Lancet Reg. Health West. Pac. 31, 100574 (2023).
Regione Toscana. Regional Program for the Prevention and Control of Congenital Chagas Disease: Indications for Care during Pregnancy. https://www.regione.toscana.it/documents/10180/13329059/Allegato+parere+n.+46-2015+Prev+e+conrollo+malattia+di+Chagas.pdf/6e153700-0d7b-4d70-b098-faba975c6de8?version=1.0 (2012).
Repetto, E. C. et al. Neglect of a neglected disease in Italy: the challenge of access-to-care for chagas disease in Bergamo Area. PLoS Negl. Trop. Dis. 9, e0004103 (2015).
Campolmi, I. et al. Chagas disease in Italy: updated estimates. Intern. Emerg. Med. 15, 1339–1343 (2020).
Raglio, A. et al. Prevention of congenital Chagas disease by screening of mothers and monitoring of serological tests of neonates: the seven years’ experience. Infez. Med. 31, 243–249 (2023).
Sicuri, E. et al. Economic evaluation of Chagas disease screening of pregnant Latin American women and of their infants in a non endemic area. Acta Trop. 118, 110–117 (2011).
Imaz-Iglesia, I. et al. Economic evaluation of Chagas disease screening in Spain. Acta Trop. 148, 77–88 (2015).
Stillwaggon, E., Perez-Zetune, V., Bialek, S. R. & Montgomery, S. P. Congenital Chagas disease in the United States: cost savings through maternal screening. Am. J. Trop. Med. Hyg. 98, 1733–1742 (2018).
Ministero della Salute. I princìpi del Servizio sanitario nazionale (SSN). https://www.salute.gov.it/new/it/tema/livelli-essenziali-di-assistenza/i-principi-del-servizio-sanitario-nazionale-ssn/ (2019).
Angheben, A. et al. Chagas disease in Italy: breaking an epidemiological silence. Eur. Surveill. Bull. Eur. Sur Mal. Transm. Eur. Commun. Dis. Bull. 16, 19969 (2011).
Antinori, S., Giacomelli, A., Sabaini, F., Casalini, G. & Ridolfo, A. L. Chagas disease in Italy: an update of epidemiological studies. Infez. Med. 31, 421–424 (2023).
Barbiero, A. et al. A questionnaire integrated with the digital medical record improved the coverage of a control program for congenital Chagas disease in Tuscany, Italy. Microorganisms 11, 154 (2023).
United Nations. 17 Sustainable Development Goals (SDGs). https://sdgs.un.org/goals (2015).
Blackstone, E. A. & Fuhr, J. P. Redefining health care: creating value-based competition on results. Atl. Econ. J. 35, 491–501 (2007).
Livingston, E. G., Duggal, R. & Dotters-Katz, S. Screening for Chagas disease during pregnancy in the United States-a literature review. Trop. Med. Infect. Dis. 6, 202 (2021).
Khatri, R. B. et al. Multisectoral actions in primary health care: a realist synthesis of scoping review. PLoS ONE 18, e0289816 (2023).
Ministero della Salute. Linee di indirizzo per la prevenzione e il contrasto del sovrappeso e dell’obesità. https://www.salute.gov.it/imgs/C_17_pubblicazioni_3256_allegato.pdf.
World Health Organization. Providing Care to Populations Affected by Chagas Disease. https://www.who.int/activities/providing-care-to-populations-affected-by-chagas-disease (2025).
World Health Organization. Ending the Neglect to Attain the Sustainable Development Goals: A Road Map for Neglected Tropical Diseases 2021–2030. 1–196 https://www.who.int/publications/i/item/9789240010352 (2021).
Wilson, L. S., Strosberg, A. M. & Barrio, K. Cost-effectiveness of Chagas disease interventions in Latin America and the Caribbean: Markov models. Am. J. Trop. Med. Hyg. 73, 901–910 (2005).
Nunes, M. C. P. et al. Chagas cardiomyopathy: an update of current clinical knowledge and management: a scientific statement from the American Heart Association. Circulation 138, e169–e209 (2018).
Bozkurt, B. et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation 134, e579–e646 (2016).
Refoyo, E. et al. Comparison of noninvasive cardiac test strategies for newly diagnosed Chagas disease in a non-endemic zone. Am. J. Trop. Med. Hyg. 103, 1480–1486 (2020).
Suárez, C., Nolder, D., García-Mingo, A., Moore, D. A. J. & Chiodini, P. L. Diagnosis and clinical management of Chagas disease: an increasing challenge in non-endemic areas. Res. Rep. Trop. Med. 13, 25–40 (2022).
Abras, A. et al. Worldwide control and management of Chagas disease in a new era of globalization: a close look at congenital Trypanosoma cruzi infection. Clin. Microbiol. Rev. 35, e0015221 (2022).
Regione Toscana. Raccomandazioni per il controllo della malattia di Chagas congenita in Toscana. 1–10 https://www301.regione.toscana.it/bancadati/atti/Contenuto.xml?id=5239758&nomeFile=Decreto_n (2019).
Ornaghi, S. et al. Screening of Chagas disease in pregnant women—Recommendation by the Italian National Institute of Health, 2023. Int. J. Gynecol. Obstet. 167, 1269–1271 (2024).
Comitato di Studio per la Parassitologia dell’Associazione Microbiologi Clinici Italiani. Percorso Diagnostico - Parassitosi ematiche e del sistema reticolo endoteliale (SRE). https://crrveq.aou-careggi.toscana.it/relazioni/202201/Percorso%20diagnostico%20delle%20Parassitosi%20Ematiche%20e%20del%20Sistema%20Reticolo%20Endoteliale%20(SRE).pdf (2022).
Hotez, P. J., Bottazzi, M. E., Franco-Paredes, C., Ault, S. K. & Periago, M. R. The neglected tropical diseases of Latin America and the Caribbean: a review of disease burden and distribution and a roadmap for control and elimination. PLoS Negl. Trop. Dis. 2, e300 (2008).
Moscatelli, G. et al. Longitudinal follow up of serological response in children treated for Chagas disease. PLoS Negl. Trop. Dis. 13, e0007668 (2019).
Suasnábar, S. et al. Trypanocidal therapy among children infected by Trypanosoma cruzi. Serological and electrocardiographic changes over a mean twenty-five-years follow-up period. Acta Trop. 222, 106050 (2021).
Lenk, E. J., Redekop, W. K., Luyendijk, M., Rijnsburger, A. J. & Severens, J. L. Productivity loss related to neglected tropical diseases eligible for preventive chemotherapy: a systematic literature review. PLoS Negl. Trop. Dis. 10, e0004397 (2016).
Chryssoula T., Roberto P., & Ilaria S. Manuale Di Infettivologia Neonatale, 3a Ed. (Antonio Delfino Editore, 2022).
Monge-Maillo, B. & López-Vélez, R. Challenges in the management of Chagas disease in Latin-American migrants in Europe. Clin. Microbiol. Infect. 23, 290–295 (2017).
Gravelle, H. & Smith, D. Discounting for health effects in cost-benefit and cost-effectiveness analysis. Health Econ. 10, 587–599 (2001).
Appleby, J., Devlin, N. & Parkin, D. NICE’s cost effectiveness threshold. BMJ 335, 358–359 (2007).
Colombo, V. et al. Trypanosoma cruzi infection in Latin American pregnant women living outside endemic countries and frequency of congenital transmission: a systematic review and meta-analysis. J. Travel Med. 28, taaa170 (2021).
Guedes, P. M. M., Silva, G. K., Gutierrez, F. R. S. & Silva, J. S. Current status of Chagas disease chemotherapy. Expert Rev. Anti Infect. Ther. 9, 609–620 (2011).
Matthews, S. et al. Estimation of the morbidity and mortality of congenital Chagas disease: a systematic review and meta-analysis. PLoS Negl. Trop. Dis. 16, e0010376 (2022).
Regione Piemonte. Tariffario delle prestazioni specialistiche della Regione Piemonte. 1–105 https://www.regione.piemonte.it/web/sites/default/files/media/documenti/2018-10/tariffario_prestazioni_specialistiche_rp.pdf (2018).
Regione Piemonte. Tariffario delle prestazioni di ricovero ospedaliero per acuti. 1–41 https://www.regione.piemonte.it/web/sites/default/files/media/documenti/2018-10/tariffario_prestazioni_ricoveri_rp.pdf (2018).
Agenzia Italiana del Farmaco. Elenchi farmaci di classe A e H. https://www.aifa.gov.it/-/tabelle-farmaci-di-classe-a-e-h-al-15/01/2024 (2024).
Briggs, A., Claxton, K. & Sculpher, M. Decision Modelling For Health Economic Evaluation (Oxford University Press, 2006).
Caro, J. J., Briggs, A. H., Siebert, U. & Kuntz, K. M. Modeling good research practices—overview: a report of the ISPOR-SMDM modeling good research practices task force-1. Value Health 15, 796–803 (2012).
Barton, G. R., Briggs, A. H. & Fenwick, E. A. L. Optimal cost-effectiveness decisions: the role of the cost-effectiveness acceptability curve (CEAC), the cost-effectiveness acceptability frontier (CEAF), and the expected value of perfection information (EVPI). Value Health 11, 886–897 (2008).
Husereau, D. et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. BMJ e067975 https://doi.org/10.1136/bmj-2021-067975 (2022).
Baio, G., Berardi, A. & Heath, A. Bayesian Cost-Effectiveness Analysis with the R Package BCEA (Springer, Cham, 2017). https://doi.org/10.1007/978-3-319-55718-2.
Nurchis, M. C. R and JAGS Code for Bayesian Decision-Tree Cost-Effectiveness Analysis of Trypanosoma cruzi Screening in Italy. Zenodo https://doi.org/10.5281/zenodo.16932137 (2025).
Altcheh, J. et al. Population pharmacokinetic study of benznidazole in pediatric Chagas disease suggests efficacy despite lower plasma concentrations than in adults. PLoS Negl. Trop. Dis. 8, e2907 (2014).
Regione Piemonte. Approvazione del Catalogo regionale delle prestazioni sanitarie di specialistica ambulatoriale, ai sensi della D.G.R. n. 3-8294/2024/XI del 12.03.2024, con conseguente modifica delle DD.D. n. 371 del 16.06.2015 e n. 777 del 30.11.2015 e s.m.i. 180 https://www.regione.piemonte.it/governo/bollettino/abbonati/2024/12/attach/dgr_08294_1050_12032024.pdf (2024).
Regione Lombardia. Tariffario esami di laboratorio; deliberazione del direttore generale N. 343 del 23/06/2021; ultimo aggiornamento 18/03/2022. https://www.consultazioniburl.servizirl.it/ricerca/bollettino (2022).
Azienda Ospedaliera S. Croce e Carle. Farmacia Ospedaliera. https://www.ospedale.cuneo.it.
Acknowledgements
Andrea Angheben acknowledges support from the Italian Ministry of Health Fondi Ricerca Corrente-L2 to IRCCS Sacro Cuore - Don Calabria Hospital.
Author information
Authors and Affiliations
Contributions
P.M.: Conceptualization, Resources, Data Curation, Writing – Original draft preparation, Writing – Reviewing and Editing, Visualization. M.D.: Conceptualization, Resources, Data Curation, Writing – Reviewing and Editing, Visualization. M.C.N.: Methodology, Formal analysis, Resources, Investigation, Writing – Original draft preparation, Writing – Reviewing and Editing, Visualization. A.A.: Resources, Data Curation, Writing – Original draft preparation, Writing – Reviewing and Editing, Visualization. L.O.: Resources, Data Curation, Writing – Reviewing and Editing, Visualization. G.B.: Resources, Data Curation, Writing – Reviewing and Editing, Visualization. G.D.: Validation, Writing - Reviewing and Editing, Visualization, Supervision, Project Administration. M.M.G.: Validation, Writing - Reviewing and Editing, Visualization, Supervision, Project Administration.
Corresponding author
Ethics declarations
Competing interests
Andrea Angheben acknowledges support from the Italian Ministry of Health Fondi Ricerca Corrente-L2 to IRCCS Sacro Cuore - Don Calabria Hospital. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Kenji Hirayama, Inés María Iglesias Rodríguez and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Marraffa, P., Dentato, M., Nurchis, M.C. et al. Cost-effectiveness analysis of screening for congenital Chagas disease in a non-endemic area. Nat Commun 16, 8707 (2025). https://doi.org/10.1038/s41467-025-63760-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-63760-0