Abstract
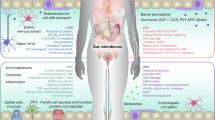
The human gut is colonized by trillions of microbes that influence the health of their human host. Whereas many bacterial species have now been linked to a variety of different diseases, the involvement of Archaea, an evolutionarily distinct group of microbes, in human disease remains elusive. By analyzing 19 independent clinical studies, we demonstrate that associations between Archaea and human diseases are widespread yet highly heterogeneous, with a pronounced and consistent enrichment of Methanobrevibacter smithii in colorectal cancer (CRC) patients. Metabolic modelling and in vitro co-culture identified distinct mutualistic interactions of M. smithii with CRC-causing bacteria such as Fusobacterium nucleatum, including metabolic enhancement. Metabolomics further reveal archaeal-derived compounds with tumor-modulating properties. Together, our results provide mechanistic insights into how the human gut archaeome may participate in CRC-associated microbial networks through metabolic cooperation with bacteria.
Similar content being viewed by others
Data availability
Raw sequencing data for stool samples All sequencing data analyzed in this study were obtained from previously published datasets and are publicly available from the European Nucleotide Archive (ENA) and the NCBI BioProject/SRA databases under the following accession numbers: PRJDB4176, PRJEB6070, PRJEB7774, PRJEB10878, PRJNA389927, PRJEB12449, PRJEB27928, PRJNA447983, PRJNA531273 and PRJNA397112, PRJNA400072, SRA045646 and SRA050230 [https://www.ncbi.nlm.nih.gov/sra/SRA050230], PRJEB32762, PRJEB47976, PRJNA798058, PRJEB29127, PRJNA834801, PRJNA743718, PRJEB53401, and PRJEB17784. The NMR raw data generated in this study are available in Zenodo at https://doi.org/10.5281/zenodo.16311518. The LC-MS raw data generated in this study are available in Zenodo at https://doi.org/10.5281/zenodo.16367666. All additional data generated and analyzed in this study, including Kraken2/Bracken outputs, gapseq outputs (including genome-scale metabolic models, gap-filled models, reaction and gene annotations, as well as pathway and transporter predictions), PyCoMo outputs (including flux variability analyses, metabolite secretion and uptake predictions, and community) are publicly available in our GitHub repository (https://github.com/CME-lab-research/archaeome-disease-profiling/). Source data are provided with this paper.
References
Lecours, P. B. et al. Increased prevalence of Methanosphaera stadtmanae in inflammatory bowel diseases. PLoS ONE 9, e87734 (2014).
Romano, S. et al. Meta-analysis of the Parkinson’s disease gut microbiome suggests alterations linked to intestinal inflammation. NPJ Parkinson’s Dis. 7, 27 (2021).
Fumagalli, A. et al. Archaea methanogens are associated with cognitive performance through the shaping of gut microbiota, butyrate and histidine metabolism. Gut Microbes 17, 2455506 (2025).
Jangi, S. et al. Alterations of the human gut microbiome in multiple sclerosis. Nat. Commun. 7, 12015 (2016).
Scanlan, P. D., Shanahan, F. & Marchesi, J. R. Human methanogen diversity and incidence in healthy and diseased colonic groups using mcrA gene analysis. BMC Microbiol. 8, 79 (2008).
Helen, T. et al. Gut microbiota composition and relapse risk in pediatric MS: a pilot study. J. Neurol. Sci. 363, 153–157 (2016).
Bhute, S.S. et al. Gut microbial diversity assessment of indian type-2-diabetics reveals alterations in eubacteria, archaea, and eukaryotes. Front. Microbiol. 8, 214 (2017).
Jia, L. et al. Metagenomic analysis characterizes stage-specific gut microbiota in Alzheimer’s disease. Mol. Psychiatry 30, 3951–3962 (2025).
Kumpitsch, C. et al. Reduced B12 uptake and increased gastrointestinal formate are associated with archaeome-mediated breath methane emission in humans. Microbiome 9, 193 (2021).
Borrel, G., Brugère, J.-F., Gribaldo, S., Schmitz, R. A. & Moissl-Eichinger, C. The host-associated archaeome. Nat. Rev. Microbiol. 18, 622–636 (2020).
Balch, W. E., Fox, G. E., Magrum, L. J., Woese, C. R. & Wolfe, R. S. Methanogens: reevaluation of a unique biological group. Microbiol. Rev. 43, 260–296 (1979).
Nkamga, V. D., Henrissat, B. & Drancourt, M. Archaea: essential inhabitants of the human digestive microbiota. Hum. Microbiome J. 3, 1–8 (2017).
Hoegenauer, C., Hammer, H. F., Mahnert, A. & Moissl-Eichinger, C. Methanogenic archaea in the human gastrointestinal tract. Nat. Rev. Gastroenterol. Hepatol. 19, 805–813 (2022).
Ruaud, A. et al. Syntrophy via interspecies H2 transfer between Christensenella and Methanobrevibacter underlies their global cooccurrence in the human gut. mBio 11, 10–1128 (2020).
Baradaran Ghavami, S. et al. Alterations of the human gut Methanobrevibacter smithii as a biomarker for inflammatory bowel diseases. Microb. Pathog. 117, 285–289 (2018).
Schwiertz, A. et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity 18, 190–195 (2010).
Pimentel, M. et al. Methane production during lactulose breath test is associated with gastrointestinal disease presentation. Dig. Dis. Sci. 48, 86–92 (2003).
Laura, H. et al. Evaluating breath methane as a diagnostic test for constipation-predominant IBS. Dig. Dis. Sci. 55, 398–403 (2010).
Ghoshal, U., Shukla, R., Srivastava, D. & Ghoshal, C. U. Irritable bowel syndrome, particularly the constipation-predominant form, involves an increase in Methanobrevibacter smithii, which is associated with higher methane production. Gut Liver 10, 932–938 (2016).
Takakura, W. et al. A single fasting exhaled methane level correlates with fecal methanogen load, clinical symptoms and accurately detects intestinal methanogen overgrowth. Am. J. Gastroenterol. 117, 470–477 (2022).
Madigan, K. E., Bundy, R. & Weinberg, R. B. Distinctive clinical correlates of small intestinal bacterial overgrowth with methanogens. Clin. Gastroenterol. Hepatol. 20, 1598–1605 (2022).
Li, T. et al. Multi-cohort analysis reveals altered archaea in colorectal cancer fecal samples across populations. Gastroenterology 168, 525–538 (2025).
Sun, Y., Liu, Y., Pan, J., Wang, F. & Li, M. Perspectives on cultivation strategies of archaea. Microb. Ecol. 79, 770–784 (2020).
Mahnert, A., Blohs, M., Pausan, M.-R. & Moissl-Eichinger, C. The human archaeome: methodological pitfalls and knowledge gaps. Emerg. Top. Life Sci. 2, 469–482 (2018).
Zhou, X. et al. Gut microbiome of multiple sclerosis patients and paired household healthy controls reveal associations with disease risk and course. Cell 185, 3467–3486 (2022).
Woh, P. Y. et al. Reevaluation of the gastrointestinal methanogenic archaeome in multiple sclerosis and its association with treatment. Microbiol. Spectr. 13, e02183-24 (2025).
Franzosa, E. A. et al. Gut microbiome structure and metabolic activity in inflammatory bowel disease. Nat. Microbiol. 4, 293–305 (2018).
Wallen, Z. D. et al. Metagenomics of Parkinson’s disease implicates the gut microbiome in multiple disease mechanisms. Nat. Commun. 13, 6958 (2022).
de la Cuesta-Zuluaga, J. et al. Age- and sex-dependent patterns of gut microbial diversity in human adults. mSystems 4, 10–1128 (2019).
Kuehnast, T. et al. Exploring the human archaeome: its relevance for health and disease, and its complex interplay with the human immune system. FEBS J. 292, 1316–1329 (2025).
Mohammadzadeh, R. et al. Age-related dynamics of predominant methanogenic archaea in the human gut microbiome. BMC Microbiol. 25, 193 (2025).
Jo, S. et al. Oral and gut dysbiosis leads to functional alterations in Parkinson’s disease. NPJ Parkinson’s Dis. 8, 87 (2022).
Yu, J. et al. Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut 66, 70–78 (2017).
Feng, Q. et al. Gut microbiome development along the colorectal adenoma–carcinoma sequence. Nat. Commun. 6, 6528 (2015).
Boktor, J. C. et al. Integrated multi-cohort analysis of the Parkinson’s disease gut metagenome. Mov. Disord. 38, 399–409 (2023).
Bedarf, J. R. et al. Functional implications of microbial and viral gut metagenome changes in early stage L-DOPA-naïve Parkinson’s disease patients. Genome Med. 9, 39 (2017).
Thomas, A. M. et al. Metagenomic analysis of colorectal cancer datasets identifies cross-cohort microbial diagnostic signatures and a link with choline degradation. Nat. Med. 25, 667–678 (2019).
Gupta, A. et al. Association of Flavonifractor plautii, a flavonoid-degrading bacterium, with the gut microbiome of colorectal cancer patients in India. mSystems 4, 10–1128 (2019).
Laske, C. et al. Signature of Alzheimer’s disease in intestinal microbiome: results from the AlzBiom study. Front. Neurosci. 16, 792996 (2022).
Ferreiro, A.L. et al. Gut microbiome composition may be an indicator of preclinical Alzheimer’s disease. Sci. Transl. Med. 15, eabo2984 (2023).
Zeller, G. et al. Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol. Syst. Biol. 10, 766 (2014).
Wirbel, J. et al. Meta-analysis of fecal metagenomes reveals global microbial signatures that are specific for colorectal cancer. Nat. Med. 25, 679–689 (2019).
Misiak, B. et al. Associations of gut microbiota alterations with clinical, metabolic, and immune-inflammatory characteristics of chronic schizophrenia. J. Psychiatr. Res. 171, 152–160 (2024).
Villette, R. et al. Integrated multi-omics highlights alterations of gut microbiome functions in prodromal and idiopathic Parkinson’s disease. Microbiome 13, 200 (2025).
Yachida, S. et al. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat. Med. 25, 968–976 (2019).
Vogtmann, E. et al. Colorectal cancer and the human gut microbiome: reproducibility with whole-genome shotgun sequencing. PLOS ONE 11, e0155362 (2016).
Mira-Pascual, L. et al. Microbial mucosal colonic shifts associated with the development of colorectal cancer reveal the presence of different bacterial and archaeal biomarkers. J. Gastroenterol. 50, 167–179 (2015).
Piccinno, G. et al. Pooled analysis of 3,741 stool metagenomes from 18 cohorts for cross-stage and strain-level reproducible microbial biomarkers of colorectal cancer. Nat. Med. 31, 1–14 (2025).
Abdi, H., Kordi-Tamandani, D. M., Lagzian, M. & Bakhshipour, A. Archaeome in colorectal cancer: high abundance of methanogenic archaea in colorectal cancer patients. Int. J. Cancer Manag. 15, e117843 (2022).
Predl, M., Mießkes, M., Rattei, T. & Zanghellini, J. PyCoMo: a Python package for community metabolic model creation and analysis. Bioinformatics 40, btae153 (2024).
Maier, L. et al. Microbiota-derived hydrogen fuels Salmonella typhimurium invasion of the gut ecosystem. Cell Host Microbe 14, 641–651 (2013).
Spinelli, J. B. et al. Fumarate is a terminal electron acceptor in the mammalian electron transport chain. Science 374, 1227–1237 (2021).
King, A., Selak, M. A. & Gottlieb, E. Succinate dehydrogenase and fumarate hydratase: linking mitochondrial dysfunction and cancer. Oncogene 25, 4675–4682 (2006).
Samuel, S. B. et al. Genomic and metabolic adaptations of Methanobrevibacter smithii to the human gut. Proc. Natl. Acad. Sci. USA 104, 10643–10648 (2007).
Jiang, S.-S. et al. Fusobacterium nucleatum-derived succinic acid induces tumor resistance to immunotherapy in colorectal cancer. Cell Host Microbe 31, 781–797 (2023).
Isar, J., Agarwal, L., Saran, S. & Saxena, R. K. Succinic acid production from Bacteroides fragilis: process optimization and scale up in a bioreactor. Anaerobe 12, 231–237 (2006).
Yu, J. et al. Effect and potential mechanism of oncometabolite succinate promotes distant metastasis of colorectal cancer by activating STAT3. BMC Gastroenterol. 24, 106 (2024).
Zhang, W. & Lang, R. Succinate metabolism: a promising therapeutic target for inflammation, ischemia/reperfusion injury and cancer. Front. Cell Dev. Biol. 11, 1266973 (2023).
Takemoto, N., Tanaka, Y., Inui, M. & Yukawa, H. The physiological role of riboflavin transporter and involvement of FMN-riboswitch in its gene expression in Corynebacterium glutamicum. Appl. Microbiol. Biotechnol. 98, 4159–4168 (2014).
Wang, H. et al. ¹H NMR-based metabolic profiling of human rectal cancer tissue. Mol. Cancer 12, 121 (2013).
Shen, X. et al. Asparagine, colorectal cancer, and the role of sex, genes, microbes, and diet: a narrative review. Front. Mol. Biosci. 9, 958666 (2022).
Mao, Z. et al. Prediagnostic serum glyceraldehyde-derived advanced glycation end products and mortality among colorectal cancer patients. Int. J. Cancer 152, 2257–2268 (2023).
Liu, Y., Lau, H.C.-H. & Yu, J. Microbial metabolites in colorectal tumorigenesis and cancer therapy. Gut Microbes 15, 2203968 (2023).
Avuthu, N. & Guda, C. Meta-analysis of altered gut microbiota reveals microbial and metabolic biomarkers for colorectal cancer. Microbiol. Spectr. 10, e00013–e00022 (2022).
Xie, Z. et al. Metabolomic analysis of gut metabolites in patients with colorectal cancer: association with disease development and outcome. Oncol. Lett. 26, 358 (2023).
Gao, R. et al. Integrated analysis of colorectal cancer reveals cross-cohort gut microbial signatures and associated serum metabolites. Gastroenterology 163, 1024–1037 (2022).
Xu, S. et al. Intestinal microbiota affects the progression of colorectal cancer by participating in the host intestinal arginine catabolism. Cell Rep. 44, 115370 (2025).
Slater, L. C., Fonseca-Pereira, D. & Garrett, W. S. Colorectal cancer: the facts in the case of the microbiota. J. Clin. Investig. 132, e155101 (2022).
Duller et al. Targeted isolation of Methanobrevibacter strains from fecal samples expands the cultivated human archaeome. Nat. Commun. 15, 7593 (2024).
Feng, T. et al. The arginine metabolism and its deprivation in cancer therapy. Cancer Lett. 620, 217680 (2025).
Wu, G., Meininger, C.J., McNeal, C.J., Bazer, F.W. & Rhoads, J.M. Role of L-arginine in nitric oxide synthesis and health in humans 167–187 (Springer, 2021).
Lamaudière, M. T. F., Arasaradnam, R., Weedall, G. D. & Morozov, I. Y. The colorectal cancer microbiota alter their transcriptome to adapt to the acidity, reactive oxygen species, and metabolite availability of gut microenvironments. mSphere 8, e00627-22 (2023).
Naes, S., Ab-Rahim, S., Mazlan, M., Hashim, N. A. A. & Abdul Rahman, A. Increased ENT2 expression and its association with altered purine metabolism in cell lines derived from different stages of colorectal cancer. Exp. Ther. Med. 25, 212 (2023).
Grondin, J. A. & Khan, W. I. Emerging roles of gut serotonin in regulation of immune response, microbiota composition and intestinal inflammation. J. Can. Assoc. Gastroenterol. 7, 88–96 (2024).
Venkateswaran, N. et al. Tryptophan fuels MYC-dependent liver tumorigenesis through indole 3-pyruvate synthesis. Nat. Commun. 15, 4266 (2024).
Xiaojing, L., Binbin, Z., Yiyang, H. & Yu, Z. New insights into gut-bacteria-derived indole and its derivatives in intestinal and liver diseases. Front. Pharmacol. 12, 769501 (2021).
Li, Q. et al. Gut barrier dysfunction and bacterial lipopolysaccharides in colorectal cancer. J. Gastrointest. Surg. 27, 1466–1472 (2023).
Chen, Y. et al. γ-linolenic acid derived from Lactobacillus plantarum MM89 induces ferroptosis in colorectal cancer. Food Funct. 16, 1760–1771 (2025).
Fyrst, H. et al. Natural sphingadienes inhibit Akt-dependent signaling and prevent intestinal tumorigenesis. Cancer Res. 69, 9457–9464 (2009).
Niehaus, E.-M. et al. Apicidin F: characterization and genetic manipulation of a new secondary metabolite gene cluster in the rice pathogen Fusarium fujikuroi. PLoS ONE 9, e103336 (2014).
Ueda, T., Takai, N., Nishida, M., Nasu, K. & Narahara, H. Apicidin, a novel histone deacetylase inhibitor, has profound anti-growth activity in human endometrial and ovarian cancer cells. Int. J. Mol. Med. 19, 301–308 (2007).
Mueller, A.-L. et al. Bacteria-mediated modulatory strategies for colorectal cancer treatment. Biomedicines 10, 832 (2022).
Song, S., Vuai, M. S. & Zhong, M. The role of bacteria in cancer therapy–enemies in the past, but allies at present. Infect. Agents Cancer 13, 9 (2018).
Candeliere, F., Sola, L., Raimondi, S., Rossi, M. & Amaretti, A. Good and bad dispositions between archaea and bacteria in the human gut: new insights from metagenomic survey and co-occurrence analysis. Synth. Syst. Biotechnol. 9, 88–98 (2024).
Mohammadzadeh, R., Mahnert, A., Duller, S. & Moissl-Eichinger, C. Archaeal key-residents within the human microbiome: characteristics, interactions and involvement in health and disease. Curr. Opin. Microbiol. 67, 102146 (2022).
Pimentel, M. et al. Methane, a gas produced by enteric bacteria, slows intestinal transit and augments small intestinal contractile activity. Am. J. Physiol. Gastrointest. Liver Physiol. 290, G1089–G1095 (2006).
Staller, K. et al. Chronic constipation as a risk factor for colorectal cancer: results from a nationwide, case-control study. Clin. Gastroenterol. Hepatol. 20, 1867–1876 (2022).
Tito, R. Y. & Raes, J. Gut archaeal biomarkers in colorectal cancer prediction: a tale of opportunity and prudence. Gastroenterology 168, 457–458 (2025).
Sieber, J. R., McInerney, M. J. & Gunsalus, R. P. Genomic insights into syntrophy: the paradigm for anaerobic metabolic cooperation. Annu. Rev. Microbiol 66, 429–452 (2012).
Campbell, A., Gdanetz, K., Schmidt, A.W. & Schmidt, T.M. H2 generated by fermentation in the human gut microbiome influences metabolism and competitive fitness of gut butyrate producers. Microbiome 11, 133 (2023).
Coker, O. O., Wu, W. K. K., Wong, S. H., Sung, J. J. Y. & Yu, J. Altered gut archaea composition and interaction with bacteria are associated with colorectal cancer. Gastroenterology 159, 1459–1470 (2020).
Cai, M., Kandalai, S., Tang, X. & Zheng, Q. Contributions of human-associated archaeal metabolites to tumor microenvironment and carcinogenesis. Microbiol. Spectr. 10, e02367-21 (2022).
Zengin, Ö.D. & Aydin, S. The hidden influence of methanogens in the gut microbiota. in Methanogens-Unique Prokaryotes (IntechOpen, 2025).
Hannigan, G.D., Duhaime, M.B., Ruffin, M.T., Koumpouras, C.C. & Schloss, P.D. Diagnostic potential and interactive dynamics of the colorectal cancer virome. mBio 9, 10–1128 (2018).
Ye, H. S., Siddle, J. K., Park, J. D. & Sabeti, C. P. Benchmarking metagenomics tools for taxonomic classification. Cell 178, 779–794 (2019).
Wood, D. E. & Salzberg, S. L. Kraken: ultrafast metagenomic sequence classification using exact alignments. Genome Biol. 15, R46 (2014).
Chibani, C. M. et al. A catalogue of 1,167 genomes from the human gut archaeome. Nat. Microbiol. 7, 48–61 (2021).
Almeida, A. et al. A unified catalog of 204,938 reference genomes from the human gut microbiome. Nat. Biotechnol. 39, 105–114 (2021).
Ma, S.Y. et al. Population structure discovery in meta-analyzed microbial communities and inflammatory bowel disease using MMUPHin. Genome Biology 23, 208 (2022).
Zimmermann, J., Kaleta, C. & Waschina, S. gapseq: informed prediction of bacterial metabolic pathways and reconstruction of accurate metabolic models. Genome Biol. 22, 81 (2021).
De Bernardini, N. et al. pan-Draft: automated reconstruction of species-representative metabolic models from multiple genomes. Genome Biol. 25, 280 (2024).
Predl, M., Gandolf, K., Hofer, M. & Rattei, T. ScyNet: visualizing interactions in community metabolic models. Bioinform. Adv. 4, vbae104 (2024).
Shannon, P. et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 13, 2498–2504 (2003).
Lindsey, R. L., Garcia-Toledo, L., Fasulo, D., Gladney, L. M. & Strockbine, N. Multiplex polymerase chain reaction for identification of Escherichia coli, Escherichia albertii and Escherichia fergusonii. J. Microbiol. Methods 140, 1–4 (2017).
Dahal, R. H., Choi, Y.-J., Kim, S. & Kim, J. Differentiation of Escherichia fergusonii and Escherichia coli isolated from patients with inflammatory bowel disease/ischemic colitis and their antimicrobial susceptibility patterns. Antibiotics 12, 154 (2023).
Weinberger, V. et al. Expanding the cultivable human archaeome: Methanobrevibacter intestini sp. nov. and strain Methanobrevibacter smithii ‘GRAZ-2’ from human faeces. Int. J. Syst. Evol. Microbiol. 75, 006751 (2025).
Ney, B. et al. The methanogenic redox cofactor F420 is widely synthesized by aerobic soil bacteria. ISME J. 11, 125–137 (2017).
Nadkarni, M. A., Martin, F. E., Jacques, N. A. & Hunter, N. Determination of bacterial load by real-time PCR using a broad-range (universal) probe and primers set. Microbiology 148, 257–266 (2002).
Probst, A. J., Auerbach, A. K. & Moissl-Eichinger, C. Archaea on human skin. PLoS ONE 8, e65388 (2013).
Hales, B. A. et al. Isolation and identification of methanogen-specific DNA from blanket bog peat by PCR amplification and sequence analysis. Appl. Environ. Microbiol. 62, 668–675 (1996).
Lloyd, W. S. et al. Proposed minimum reporting standards for chemical analysis. Metabolomics 3, 211–221 (2007).
Duvallet, C., Gibbons, S. M., Gurry, T., Irizarry, R. A. & Alm, E. J. Meta-analysis of gut microbiome studies identifies disease-specific and shared responses. Nat. Commun. 8, 1784 (2017).
Wickham, H. ggplot2: Elegant graphics for data analysis. https://ggplot2.tidyverse.org (Springer-Verlag New York, 2016).
Shuangbin, X. et al. Use ggbreak to effectively utilize plotting space to deal with large datasets and outliers. Front. Genet. 12, 774846 (2021).
Acknowledgements
This research was funded in whole or in part by the Austrian Science Fund (FWF) [10.55776/P32697 (given to C.M.E.), excellence cluster “Microbiomes Drive Planetary Health” 10.55776/CoE7 (C.M.E., C.D., and G.G), and SFB ImmunoMetabolism 10.55776/F8300 (C.M.E.)]. C.M.E. has received funding from the European Research Council (ERC) under the Horizon Europe research and innovation programme (Project ID 101199346, ERC-2024-ADG). T.M. is grateful to the Austrian Science Fund (FWF) for excellence cluster 10.55776/COE14, grants DOI 10.55776/P28854, 10.55776/I3792, 10.55776/DOC130, and 10.55776/W1226, the Austrian Research Promotion Agency (FFG) grants 864690 and 870454; the Integrative Metabolism Research Center Graz; the Austrian Infrastructure Program 2016/2017; the Styrian Government (Zukunftsfonds, doc.fund program); the City of Graz; and BioTechMed-Graz (flagship project). This project was funded in part by the FFG and the European Union (EFRE) under grant 912192. T.M. and H.H. acknowledge the Center for Medical Research for laboratory access. C.T. reports a research grant by Bruker Switzerland AG. For open access purposes, the author has applied a CC BY public copyright license to any author-accepted manuscript version arising from this submission. We gratefully acknowledge the computational resources provided by the MedBioNode at the Medical University of Graz, funded by the Austrian Federal Ministry of Education, Science, and Research through the Hochschulrat-Struktur Mittel 2016 grant within BioTechMed Graz. We also thank the ZMF Core Facility Computational Bioanalytics team at the Medical University of Graz for their support. We thank Claire Lamb for assistance with the provision of the Bacteroides fragilis strain. We thank Charlotte Neumann for her help in creating some illustrations for this study. R.M. was supported by the local PhD program MolMed.
Author information
Authors and Affiliations
Contributions
R.M. designed the study, collected data, performed bioinformatics, data analysis, plotting, and drafted the manuscript. A.M. co-designed the study. T.Z. and L.W. performed sample cultivation. C.K. performed qPCR. K.F. assisted with plot preparation. P.M. performed E. coli isolation and confirmation. H.H. and T.M. performed NMR metabolomics. J.S. and C.T. performed MS metabolomics. D.P., K.H., and D.K. performed SEM. M.D performed the machine learning analysis. C.D. helped with data analysis. G.G. and A.L. assisted with sample preparation. G.G., C.T., C.D., and A.L. commented on and revised the manuscript. C.M-E. designed and supervised the study, and drafted and revised the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Sabina La Rosa and the other anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohammadzadeh, R., Mahnert, A., Zurabishvili, T. et al. Cross-domain metabolic interactions link Methanobrevibacter smithii to colorectal cancer microbial ecosystems. Nat Commun (2026). https://doi.org/10.1038/s41467-026-69711-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-026-69711-7