Abstract
Falls are a significant cause of injury-related morbidity and mortality among older adults worldwide, with a rising incidence in recent decades. Using data from the Global Burden of Disease Study 2021, we analyzed incidence, mortality, and disability-adjusted life years (DALYs) related to falls in individuals aged 65 years and older from 1990 to 2021. In 2021, there were approximately 45,657,816 new falls globally, reflecting a 182% increase since 1990. While the incidence rate rose, mortality and DALY rates remained relatively stable. Higher incidence was observed in women, but men had higher mortality rates. Regional differences were notable, with Australasia and South Asia showing the highest incidence and mortality burdens, respectively. Low bone mineral density emerged as the leading risk factor. Projections indicate a continued rise in incidence through 2040. These findings highlight the urgent need for targeted prevention strategies to reduce the health burden of falls among older adults.
Similar content being viewed by others
Introduction
Falls are the second leading cause of unintentional injury-related deaths worldwide, following only road traffic injuries1,2. Annually, falls account for about 684,000 deaths globally, exceeding deaths from other major injuries such as drowning and fire-related injuries1. Furthermore, an estimated 37.3 million fall-related incidents require medical intervention, posing a substantial burden on individuals, families, and healthcare systems3. In the United States, over 25% of adults aged 65 years and older experience falls annually, with approximately 37% of these falls resulting in injuries, about 9 million cases, that necessitate medical care or lead to activity limitations4. In terms of disability-adjusted life years (DALYs), the burden attributable to falls surpasses that of chronic respiratory diseases and several types of cancer in older age groups5. Beyond their physical consequences, falls are also frequently associated with psychological effects such as fear of falling, which can significantly impair autonomy and quality of life. With the aging population, the incidence and burden of falls among older adults are expected to rise2,6, underscoring an urgency to investigate the epidemiological patterns, risk factors, and societal impact of falls in the aging population.
Most of the previous related epidemiological research focuses on incidence rates, identification of risk factors, and the evaluation of intervention measures for the falls among older adults7. Systematic reviews indicate that the annual fall incidence among individuals aged 60 and older worldwide is approximately 26%, but regional variations are significant, and data from developing countries are particularly scarce3. Moreover, previous studies are often limited in specific countries or regions, and have short time frames, making it difficult to fully capture global and long-term trends3,8,9,10,11. Many risk factors have been identified, including advanced age, female gender, osteoporosis, visual impairment, depressive symptoms, and medication12. In particular, growing evidence highlights that malnutrition and sarcopenia are critical contributors to increased fall risk by impairing strength, balance, and gait stability13. Osteoporosis is especially prevalent in older adults and contributes to fall-related fractures and mortality14. Furthermore, environmental hazards such as poor lighting, uneven flooring, and a lack of assistive devices also significantly elevate fall risk, particularly in low-resource settings15. However, there still lack studies that systematically compare all risk factors across countries at different socio-economic development levels, as well as analyze how these factors influence disease burden16.
The Global Burden of Disease (GBD) database, led by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington, provides global, territorial, and national data on diseases and injuries from 1990 to 202117. These data cover the disease incidence, mortality, and DALYs across 204 countries and territories from 1990 to 2021, and are stratified by age, sex, and the Socio-demographic Index (SDI). Additionally, the GBD database reports fall-related risk factors, such as low bone density and alcohol use6. Therefore, the GBD database may be an ideal tool allowing a systematic evaluation of the disease burden and trend of falls and fall-related events among older adults, thus providing a scientific basis for the development of effective prevention and intervention strategies.
Considering the rising burden of falls among older adults, the complex distribution of risk factors, and the current lack of systematic and forward-looking studies, here we based on the GBD 2021 data to conduct a comprehensive study integrating trend analysis, predictive modeling, and risk attribution methods, aiming to provide evidence-based support for designing prevention and control strategies for falls among older adults.
Results
Global, regional, and national incidence
In 2021, an estimated 45,657,816 new falls (95% UI: 35,693,807–57,216,793) occurred among adults aged 65 years and older, representing a 182.09% increase from the 16,185,684 cases (95% UI: 12,256,022–20,850,252) in 1990. After age standardization, the global ASIR of falls rose from 5472.52 per 100,000 population in 1990 (95% UI: 4174.00–7025.05) to 6198.42 per 100,000 population in 2021 (95% UI: 4862.87–7753.18). The EAPC in ASIR over this period was 0.38% (95% CI: 0.33%–0.43%) (Table 1).
Among the 21 GBD regions, Western Europe (10,134,329 cases, 95% UI: 8,824,435–11,699,921) reported the highest number of fall-related incidents among older adults in 2021, followed by East Asia (9,381,366 cases, 95% UI: 6,743,859– 12,537,250) (Table S2). After age standardization, Australasia exhibited the highest ASIR (13,400.98 per 100,000 population, 95% UI: 11,593.60–15,527.26), whereas the lowest ASIR was observed in Southern Sub-Saharan Africa (944.24 per 100,000 population, 95% UI: 711.55 –1219.93) (Table S3).
From 1990 to 2021, three regions demonstrated statistically significant declines in ASIR (EAPC < 0): Central Europe (EAPC = −1.13%, 95% CI: −1.22% to −1.04%), Central Latin America (EAPC = −0.78%, 95% CI: −0.92% to −0.64%), and Southern Sub-Saharan Africa (EAPC = −0.46%, 95% CI: –0.59% to −0.33%). In contrast, most other regions exhibited increasing trends, with the most marked rise observed in North Africa and the Middle East (EAPC = 2.09%, 95% CI: 1.96%–2.21%) (Table S4 and Fig. 1a).
EAPCs in the ASIR (a), ASMR (b), and ASDR (c) of falls among older adults across 21 GBD regions. EAPC estimated annual percentage change, ASIR age-standardized incidence rate, ASMR age-standardized mortality rate, ASDR age-standardized disability-adjusted life-year rate, GBD the Global Burden of Disease Study.
Among the 204 countries, China, India, the United States, Germany, and France reported the highest numbers of new falls among older adults in 2021, collectively accounting for more than half of the global total (Table S5). After age standardization, the highest ASIR was observed in Andorra (18,972.97 per 100,000 population, 95% UI: 15,675.88–22,567.12), followed by Croatia (17,649.07 per 100,000, 95% UI: 15,169.77–20,430.68), and Slovenia (16,260.21 per 100,000, 95% UI: 13,909.04–18,827.42) (Table S6 and Fig. 2a).
ASIR (a), ASMR (c), and ASDR (e) of falls among older adults in 204 countries and territories in 2021. EAPCs in ASIR (b), ASMR (d), and ASDR (f) of falls among older adults from 1990 to 2021. ASIR age-standardized incidence rate, ASMR age-standardized mortality rate, ASDR age-standardized disability-adjusted life-year rate, EAPC estimated annual percentage change.
From 1990 to 2021, Türkiye exhibited the most substantial increase in ASIR among older adults, with an EAPC of 4.48% (95% CI: 4.10%–4.86%). Conversely, the steepest decline was observed in Czechia, with an EAPC of −2.80% (95% CI: −2.98% to −2.62%) (Table S7 and Fig. 2b).
Global, regional, and national mortality
From 1990 to 2021, the global number of fall-related deaths among older adults increased by 174.08%, reaching 555,539 in 2021 (95% UI: 446,578–619,898). The ASMR showed a slight increase from 77.20 per 100,000 population in 1990 (95% UI: 66.23–85.63) to 78.36 per 100,000 in 2021 (95% UI: 62.89– 87.54), with an EAPC of 0.25% (95% CI: 0.18%–0.33%) (Table 1).
In 2021, South Asia reported the highest number of fall-related deaths among older adults, with 177,938 deaths (95% UI: 140,865–209,952), which accounted for 32.03% of global deaths, and also the highest ASMR among the 21 GBD regions (184.55 per 100,000 population, 95% UI: 146.20–219.11) (Table S3). Conversely, the lowest ASMR was observed in Central Asia, at 13.85 per 100,000 population (95% UI: 12.15–15.29). Over the 32-year period, the greatest increase in ASMR was noted in High-income North America (EAPC = 2.78%, 95% CI: 2.60%–2.96%), while the most pronounced decline occurred in Central Europe (EAPC = −2.73%, 95% CI: −2.96% to −2.49%) (Table S4 and Fig. 1b).
In 2021, India recorded the highest number of fall-related deaths among older adults, with an estimated 166,518 deaths (95% UI: 130,376–197,202), followed by China (93,378 deaths, 95% UI: 53,996–123,829), the United States (44,185 deaths, 95% UI: 36,467 to 48,318), and Germany (20,653 deaths, 95% UI: 16,540–23,680), all surpassing 20,000 deaths. India also exhibited the highest ASMR among the 204 countries, at 211.43 per 100,000 population (95% UI: 165.60 to 251.96), whereas the lowest ASMR was observed in Azerbaijan, at 6.41 per 100,000 population (95% UI: 4.27–9.10) (Tables S5 and S6 and Fig. 2c).
From 1990 to 2021, the largest increases in ASMR were observed in Georgia (EAPC = 3.88%, 95% CI: 2.73%–5.04%), the United States (EAPC = 2.95%, 95% CI: 2.76%–3.14%), and Australia (EAPC = 2.82%, 95% CI: 2.54%–3.11%). Conversely, the steepest declines in ASMR were reported in Hungary (EAPC = −4.84%, 95% CI: −5.19% to −4.50%), Czechia (EAPC = −3.95%, 95% CI: −4.35% to −3.54%), and Guam (EAPC = −3.26%, 95% CI: −3.78% to −2.74%) (Table S7 and Fig. 2d).
Global, regional, and national DALYs
In 2021, falls among older adults accounted for 16,952,767 DALYs globally (95% UI: 13,899,084–20,380,594), representing a 144.85% increase compared to that in 1990. Despite this absolute rise, the ASDR remained relatively stable over the study period, recorded at 2,300.76 per 100,000 population in 1990 (95% UI: 1917.86–2765.40) and 2296.74 per 100,000 in 2021 (95% UI: 1885.13–2759.42). The EAPC in ASDR was 0.03% (95% CI: 0.01%–0.06%) (Table 1).
In 2021, the highest burden of fall-related DALYs was observed in Asia, particularly in South Asia and East Asia, with India and China contributing the largest proportions. Combined, these two countries accounted for 42.71% of the global total. South Asia exhibited the highest ASDR (4,129.56 per 100,000 population, 95% UI: 3449.78–4826.17) (Tables S2 and S3), while the lowest regional ASDR was reported in Southern Sub-Saharan Africa (511.87 per 100,000, 95% UI: 420.78–629.75). From 1990 to 2021, Central Europe showed the greatest reduction in fall-related ASDR among older adults (EAPC = −1.66%; 95% CI: −1.76% to −1.56%), whereas High-income North America experienced the steepest increase (EAPC = 1.62%; 95% CI: 1.55%–1.69%) (Table S4 and Fig. 1c).
Mirroring mortality trends, India and Azerbaijan recorded the highest and lowest national ASDRs due to falls in 2021, at 4769.39 per 100,000 population (95% UI: 3955.49–5588.90) and 494.17 per 100,000 (95% UI: 371.49–637.95), respectively (Table S6 and Fig. 2e). Hungary demonstrated the most substantial decline in ASDR among all countries (EAPC = −3.46%; 95% CI: −3.67% to −3.24%), whereas the Netherlands exhibited the largest increase (EAPC = 2.13%; 95% CI: 1.56%–2.70%) (Table S7 and Fig. 2f).
Global disparities based on SDI
Among older adults, the highest ASIR of falls was observed in high SDI regions, while the ASMR remained relatively low. In contrast, high-middle SDI regions reported the lowest ASMR and ASDR. However, low SDI regions exhibited the lowest ASIR, but the highest ASMR and ASDR, a pattern that has persisted over the past 32 years. An analysis of EAPCs in ASRs from 1990 to 2021 showed that middle SDI regions experienced the greatest increase in ASIR, but a declining fall-related ASMR (EAPC < 0). The most substantial reduction in ASDR was noted in high-middle SDI regions (Tables 2, S8 and Fig. S2).
At the regional level, the ASIR among older adults was significantly positively correlated with the SDI across the 21 GBD regions from 1990 to 2021. Conversely, ASMR and ASDR were negatively correlated with SDI in low-middle SDI regions, but exhibited a positive correlation in high-middle SDI regions (Fig. 3).
ASIRs (a), ASMRs (b), and ASDRs (c) of falls among older adults across 21 GBD regions with varying SDI levels from 1990 to 2021. SDI socio-demographic index, ASIR age-standardized incidence rate, ASMR age-standardized mortality rate, ASDR age-standardized disability-adjusted life-year rate, GBD the Global Burden of Disease Study.
Global variations by sex and age
In 2021, the global incidence, mortality, and DALY rates related to falls among older adults increased progressively with advancing age for both sexes, reaching their peaks among individuals aged 95 years and older. The ASIR and age-specific incidence rates were consistently higher in females across all age groups. In contrast, males exhibited higher ASMR and age-specific fall-related mortality rates. Among individuals under 75 years old, the fall-related DALY rate was slightly higher in males, whereas in those aged 75 years and older, females demonstrated significantly higher DALY rates, with a sex-specific disparity widening with age (Fig. S3).
From 1990 to 2021, the ASIR of falls among older adults showed an upward trend in both sexes, with a more pronounced increase in males (EAPC = 0.89%; 95% CI: 0.84%–0.95%) than in females (EAPC = 0.26%; 95% CI: 0.21%–0.32%). In contrast, the ASMR increased similarly in both males (EAPC = 0.25%; 95% CI: 0.17%–0.33%) and females (EAPC = 0.25%; 95% CI: 0.16%– 0.34%). The ASDR remained relatively stable, with slight increases in males (EAPC = 0.05%; 95% CI: 0.01%–0.09%) and females (EAPC = 0.06%; 95% CI: 0.03%–0.08%) (Table 1).
The analysis of fall-related ASR trends among elderly males and females across the five SDI categories over the past three decades revealed marked regional differences. In high SDI regions, the elderly males experienced the most pronounced increases in both ASMR and ASDR. In contrast, the elderly females in low SDI regions exhibited the greatest rises in ASMR and ASDR (Fig. S2).
Prediction of fall-related disease burden among older adults
To forecast future trends in the burden of falls among older adults, we applied a BAPC model to project ASRs over the next two decades. From 2022 to 2040, the global ASIR of falls among older adults was projected to increase from 6198.42 per 100,000 population in 2021 to 6460.83 per 100,000 in 2040 (95% UI: 5050.11–7871.54). In contrast, both the ASMR and ASDR were expected to decline, reaching 71.65 per 100,000 population (95% UI: 59.45–83.85) and 2120.02 per 100,000 population (95% UI: 1766.02–2474.03), respectively. These downward trends in ASMR and ASDR were projected to be more pronounced in males than in females (Fig. 4 and Table S9).
Projected global trends in the ASIR (a–c), ASMR (d–f), and ASDR (g–i) of falls among older adults by sex from 2022 to 2040. The dark blue line represents fitted projections beyond 2021, and the outermost light blue shaded area indicates the 95% UI. ASIR age-standardized incidence rate, ASMR age-standardized mortality rate, ASDR age-standardized disability-adjusted life-year rate, UI uncertainty intervals.
Risk analysis
According to the GBD database, the leading risk factors contributing to fall-related mortality and DALYs among older adults include alcohol use, low bone mineral density, occupational injuries, and smoking. Among these, low bone mineral density emerged as the predominant risk factor, accounting for 45.25% of fall-related deaths and 46.04% of DALYs globally in 2021. While the proportions of deaths and DALYs attributable to occupational injuries demonstrated a declining trend from 1990 to 2021, the contributions of other risk factors remained relatively stable (Figs. S4 and S5).
In 2021, the proportion of fall-related mortality and DALYs attributed to low bone mineral density and occupational injuries was notably higher in low and low-middle-SDI regions, compared to other SDI regions, with the highest burden observed in Central Sub-Saharan Africa (Fig. S5). Stratified analyses showed that the proportion of fall-related mortality and DALYs, due to low bone mineral density, increased significantly with advancing age among older men, while remaining consistently high across all age groups in older women. In contrast, the proportion attributable to occupational injuries declined markedly with age in both sexes. Additionally, among the older women, the proportion of fall-related deaths attributed to alcohol use increased substantially with age, a trend not observed in the older men (Figs. 5 and S6).
Discussion
In this study, we found that the global ASIR of falls among older adults increased from 5472.52 per 100,000 in 1990 to 6198.42 per 100,000 in 2021. However, the ASMR and ASDR associated with falls remained relatively stable over this period, showing no significant increase in line with the rising incidence, indicating that improvements in prevention and medical management have helped contain mortality and DALYs. These findings align with the conclusions of the World Health Organization’s Global Report on Falls Prevention in Older Age2. Notably, in high-income countries, enhancements in healthcare infrastructure and emergency response capabilities have reduced fall-related mortality and DALY rates18. The BAPC model, which is widely used and considered reliable for forecasting long-term trends by accounting for age, period, and cohort effects, was employed to project future fall incidence and burden. Based on this model, a continued increase in fall incidence is predicted, albeit at a slower pace, likely reflecting progressive advances in global geriatric care and integrated health systems19,20.
Regions with pronounced population aging, such as Australasia, Western Europe, and High-income North America, reported high ASIRs of falls among older adults. Countries like Croatia and Slovenia also showed the top three ASIRs of falls globally, potentially due to a higher proportion of rural residents and suboptimal housing conditions. Environmental hazards, such as deteriorating infrastructure, slippery surfaces, and inadequate stair safety, are prevalent in older houses, significantly increasing fall risk21,22. These results highlight the critical influence of the housing quality, particularly in rural areas where age-friendly architectural modifications are urgently needed23,24.
Our findings also showed that high SDI regions tended to have higher ASIRs, but relatively lower ASMRs. This apparent paradox may stem from the longer life expectancy and higher level of physical activity among older adults, and their broader accesses to advanced healthcare, which increases fall risks but improves survival outcomes25,26. Simultaneously, a better chronic disease management has extended life spans, though often accompanied by physical frailty making falls more likely to occur27. Importantly, high SDI regions generally possess well-established healthcare infrastructure, including timely emergency services, acute trauma care, and comprehensive rehabilitation systems, thus explaining the discordance between rising ASIR and stable ASMR2,16. In comparison, high-middle SDI countries such as South Korea, Singapore, and Spain reported moderately lower ASIRs, along with some of the world’s lowest ASMRs and ASDRs. This may result from their mature public health infrastructures, relatively lower demographic aging pressures, and deeper family caregiving traditions that enable rapid response to falls17. Conversely, in low and lower-middle SDI regions, despite lower reported ASIRs, limited healthcare access, inadequate emergency services, and scarce rehabilitation resources lead to disproportionately high disability and mortality rates28. On the other hand, older adults in these regions are more vulnerable to osteoporosis, malnutrition, and hazardous living conditions, which compromises the negative outcomes of falls29. Therefore, differences between regions in healthcare capacity and post-fall treatment are important factors that affect the burden of falls. Strengthening primary healthcare capacity, along with the establishment of comprehensive fall prevention, emergency response, and rehabilitation systems, are therefore essential in reducing the fall-related burden, particularly in low SDI regions.
Globally, the burden of falls increases with advancing age, primarily due to physiological decline. Neuromuscular deterioration, sarcopenia, reduced balance, vision decline, and immunosenescence contribute to reduced mobility and an elevated fall risk30. Multimorbidity, including osteoporosis, cardiovascular disease, and cognitive impairment, along with multiple medications, further heightens this risk31. The incidence of falls is consistently higher among older women, likely due to postmenopausal declines in estrogen that accelerate bone loss and elevate fracture risk16. Women usually experience faster muscle deterioration and live longer, resulting in a greater lifetime exposure to falls. In contrast, although older men fall less often, they experience more serious outcomes, such as higher ASMR and DALYs, possibly due to increased rates of head trauma or complications like infections and cardiac events32. These differences are not only biological but also influenced by social and regional factors. In many low- and middle-income countries, older women may have limited access to healthcare services due to traditional gender roles, financial dependency, or lower health literacy, while older men may be less likely to seek medical care or receive rehabilitation after falls33,34. Such disparities may worsen fall outcomes in under-resourced regions. These findings suggest that fall prevention strategies must be tailored by sex and age, and should incorporate interventions targeting immune function, such as physical activity, nutritional support, and anti-inflammatory therapies35. Furthermore, understanding gender differences in both biological vulnerability and healthcare access is essential to design equitable and effective fall prevention strategies in different regions.
Notably, several well-established interventions have demonstrated effectiveness in reducing fall risk among older adults. These include: (1) balance and strength training programs (such as the Otago Exercise Programme or Tai Chi), (2) home safety assessments and modifications (e.g., installation of grab bars, improved lighting, and removal of tripping hazards), (3) regular medication reviews to reduce polypharmacy and avoid the use of psychotropic drugs where possible, (4) correction and management of visual impairments, and (5) appropriate use of assistive mobility devices when needed36,37,38,39. Multifactorial interventions that integrate these components and are tailored to individual risk profiles have consistently shown benefit in both clinical and community settings40.
A significant portion of fall-related mortality and DALYs was attributed to low bone mineral density, underscoring osteoporosis as a major geriatric concern. Osteoporosis brings with complications such as fractures, immobility, chronic pain, and functional decline, all of which can increase the risk of falls41,42. To reduce the health burden of falls, particularly in low and low-middle-SDI countries, high-risk groups such as postmenopausal women, older men, and long-term corticosteroid users should be subjected to early diagnosis and individualized treatment plans incorporating medication, calcium, and vitamin D supplementation, and structured exercise programs43.
As part of the GBD 2021 study, this research shares the widely acknowledged limitations reported in previous literature44,45,46, while also presenting several additional constraints specific to our analysis. First, the analysis is restricted to fall events defined by ICD-9 codes E880-E886.99, E888-E888.9, E929.3, and ICD-10 codes W00-W19.9, potentially underestimating the true incidence, particularly in low SDI regions where falls without adverse consequences or causing minor injuries are often not recorded. This limitation may lead to an underestimation of the true prevalence and impact of falls among older adults, thereby overlooking their broader clinical and policy significance. Even seemingly minor falls can lead to psychological consequences, such as fear of falling and activity restriction, that further increase future fall risk. Future studies should integrate community-based reporting mechanisms and wearable sensor data to better capture the full spectrum of fall events. Second, the consequences of falls are multifaceted, leading to challenges in the calculation of fall-related deaths and DALYs. While the GBD 2021 study uses standardized algorithms and expert-derived models to estimate fall-related DALYs, the approach remains limited in capturing the full spectrum of fall consequences, especially when comorbid conditions (e.g., osteoporosis, dementia) contribute to both fall risk and post-fall outcomes. Therefore, these estimates should be interpreted with caution, and future research incorporating longitudinal and clinical follow-up data may help address these methodological gaps. Third, although this study identifies major risk factors such as osteoporosis, alcohol use, and smoking, the GBD model does not fully capture contextual variables, like education, housing quality, and cultural practices, which may significantly influence both fall occurrence and severity.
Looking ahead, future research should focus on improving data quality and developing practical prevention strategies. Wearable devices and home sensors could help monitor falls in real time and support early intervention. In low-resource settings, building community-based systems and working with local health workers may improve fall reporting and care. It is also important to explore how policies, such as safer housing design and fall prevention programs in care facilities, can reduce risk. Studying the cost-effectiveness of these efforts can help health systems make better decisions. With population aging becoming a global trend, international cooperation is necessary to create affordable and culturally appropriate strategies for fall prevention across different regions.
In conclusion, this study provides a comprehensive assessment of the global burden of falls among older adults, including incidence, mortality, and DALYs, and reveals substantial variations across regions, sexes, and age groups. Although its global incidence is rising, the mortality and disability of falls in elderly adults have remained stable, likely due to improvements in health systems and prevention efforts. High and high-middle SDI countries benefit from well-developed infrastructures and targeted interventions, while low and low-middle SDI countries face elevating risks due to limited healthcare capacity. Age, sex, and osteoporosis remain key risk factors. These findings emphasize the need for early screening, health education, and context-specific strategies to reduce the fall-related burdens of falls and improve the quality of life for the elderly adults.
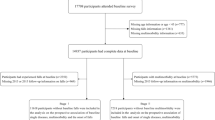
Methods
Data source
The Global Burden of Disease Study 2021 (GBD 2021) provides comprehensive estimates of the burden of more than 370 diseases and injuries across 204 countries and territories from 1990 to 2021. Relevant data were obtained from the GBD Results Tool available via the Global Health Data Exchange (GHDx) platform (http://ghdx.healthdata.org/gbd-results-tool)17,47.
In this study, older adults were defined as individuals aged 65 years and older. According to GBD 2021, falls were defined as sudden downward displacements resulting from slipping, tripping, or other unintentional movements, causing the individual to unintentionally rest on the ground, floor, or a lower level, or to strike an object, and potentially resulting in death, disability, or tissue injury48.
The corresponding International Classification of Diseases (ICD) codes for falls included E880-E886.99, E888-E888.9, and E929.3 in ICD-9, and W00-W19.9 in ICD-10 6,49,50. Fall events were further classified into 47 mutually exclusive and collectively exhaustive injury categories (e.g., fractures, open wounds) to comprehensively capture the ranges of fall-related morbidity and mortality outcomes51.
GBD 2021 employed a range of standardized indicators to quantify the epidemiological burden of falls, including incidence, mortality, and DALYs, along with their corresponding age-standardized rates, and all estimates were reported with 95% uncertainty intervals (UIs)48. Specifically, incidence and incidence rates were estimated using Bayesian meta-regression models, whereas mortality and mortality rates were derived from the Cause of Death Ensemble model (CODEm)52,53.
Years of life lost (YLLs) quantify the burden of premature mortality. YLLs are calculated as the sum of the differences between the standard life expectancy and the actual age at death, multiplied by the number of deaths: YLL = ∑(standard life expectancy − age at death) × number of deaths. Years lived with disability (YLDs) are estimated by multiplying the number of incident cases by the corresponding disability weight and the average duration of the condition until recovery or death. DALYs, a composite measure of overall disease burden, represent the total number of healthy years lost due to both premature death and disability, and are calculated as the sum of YLLs and YLDs51,54,55.
The SDI is a composite metric reflecting regional development, based on the geometric mean of three normalized values: per capita income, mean years of education among individuals aged 15 years and older, and the total fertility rate among individuals younger than 25 years. All 204 countries and territories included in the GBD study are classified into five development categories: low, low-middle, middle, high-middle, and high17.
The GBD Results Tool also provides the proportion of deaths and DALYs attributable to specific risk factors. For falls, the key risk factors include alcohol use, low bone mineral density, occupational injuries, and smoking56, with detailed definitions provided in Supplementary Table S1.
Ethical compliance
This study was a cross-sectional analysis based on publicly available, anonymized data and did not involve identifiable personal information. All research procedures were conducted in accordance with the principles of the Declaration of Helsinki. The Ethics Committee of Nanjing Second Hospital approved the exemption from ethical approval and informed consent. Clinical trial registration was not applicable.
Statistical analysis
To adjust for population age structure, age-standardized rates (ASRs) were calculated per 100,000 population. The age-standardized rate (ASR) was calculated using the formula:
where A represents the number of age groups (seven groups ranging from 65–69 years to ≥95 years), i denotes the i-th age group, ai is the rate to be standardized, and wi is the weight or population size of the i-th age group in the standard population. This method was applied to calculate the ASIR, ASMR, and ASDR, each expressed per 100,000 population57.
Percentage change (PC) was calculated to assess the relative changes in the number of incident cases, deaths, and DALYs due to falls among older adults from 1990 to 2021. PC was calculated using the formula:
Temporal trends in the burden of falls were further evaluated using EAPC, derived by fitting a linear regression model to the natural logarithm of ASRs over time. In this model, β represents the slope of the linear regression line fitted to the natural logarithm of age-standardized rates over time. It serves as the basis for EAPC using the formula: EAPC = (eβ – 1) × 100%. A positive EAPC indicates an increasing trend, whereas a negative EAPC denotes a decreasing trend. Statistical significance was assessed based on the 95% confidence interval (CI) of β; if the CI did not include zero, the trend was considered statistically significant58.
To forecast future trends in ASRs, we employed a Bayesian age-period-cohort (BAPC) model, which uses the integrated nested Laplace approximation (INLA) framework for Bayesian inference. This model disentangles the observed rates into distinct age, period, and cohort effects, which incorporates prior distributions and smoothing penalties to mitigate overfitting and stabilize estimates in regions with sparse data59,60. Projections assume continuity of past trends in the causes of falls and do not incorporate potential interventions or shocks.
The overall study design and workflow are illustrated in Fig. S1. All statistical analyses and visualizations were conducted using R software (version 4.4.1) and GraphPad Prism (version 10.2.0).
Data availability
The data from this study can be accessed openly through the Global Burden of Disease Study 2021 online database, as outlined in the Methods section.
References
WHO. Step Safely: Strategies For Preventing And Managing Falls Across The Life-course (World Health Organization, 2021).
WHO. WHO Global Report on Falls Prevention in Older Age (World Health Organization, 2008).
Salari, N., Darvishi, N., Ahmadipanah, M., Shohaimi, S. & Mohammadi, M. Global prevalence of falls in the older adults: a comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 17, 334 (2022).
CDC. Older Adult Falls Data. https://www.cdc.gov/falls/data-research/index.html (October 28, 2024).
Chen, Q. F. et al. Global burden of disease and its risk factors for adults aged 70 and older across 204 countries and territories: a comprehensive analysis of the Global Burden of Disease Study 2021. BMC Geriatr. 25, 462 (2025).
James, S. L. et al. The global burden of falls: global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev 26, i3–i11 (2020).
Florence, C. S. et al. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc 66, 693–698 (2018).
Wang, J., Chen, Z. & Song, Y. Falls in aged people of the Chinese mainland: epidemiology, risk factors and clinical strategies. Ageing Res. Rev. 9, S13–S17 (2010).
Kim, S. & So, W. Y. Prevalence and correlates of fear of falling in Korean community-dwelling elderly subjects. Exp. Gerontol. 48, 1323–1328 (2013).
Chaabna, K. et al. The epidemiology of unintentional falls among older people in the Middle East and North Africa: a systematic review and meta-analysis. J. Glob. Health 15, 04072 (2025).
Moreland, B., Kakara, R. & Henry, A. Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years - United States, 2012–2018. MMWR 69, 875–881 (2020).
Coulter, J. S., Randazzo, J., Kary, E. E. & Samar, H. Falls in older adults: approach and prevention. Am. Fam. Physician 109, 447–456 (2024).
Roberts, S., Collins, P. & Rattray, M. Identifying and managing malnutrition, frailty and sarcopenia in the community: a narrative review. Nutrients 13, 2316 (2021).
Wei, S., He, Y., Liu, K., Wang, R. & Wang, Y. Priority interventions for the prevention of falls or fractures in patients with osteoporosis: a network meta-analysis. Arch. Gerontol. Geriatr. 127, 105558 (2024).
Clemson, L. et al. Environmental interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 3, CD013258 (2023).
Ambrose, A. F., Paul, G. & Hausdorff, J. M. Risk factors for falls among older adults: a review of the literature. Maturitas 75, 51–61 (2013).
Diseases, G. B. D. & Injuries, C. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2133–2161 (2024).
Kim, S. et al. Temporal trends and patterns in mortality from falls across 59 high-income and upper-middle-income countries, 1990-2021, with projections up to 2040: a global time-series analysis and modelling study. Lancet Healthy Longev. 6, 100672 (2025).
Colon-Emeric, C. S., McDermott, C. L., Lee, D. S. & Berry, S. D. Risk Assessment and prevention of falls in older community-dwelling adults: a review. JAMA 331, 1397–1406 (2024).
Guirguis-Blake, J. M., Perdue, L. A., Coppola, E. L. & Bean, S. I. Interventions to prevent falls in older adults: updated evidence report and systematic review for the US preventive services task force. JAMA 332, 58–69 (2024).
Ying, M., Wang, S., Bai, C. & Li, Y. Rural-urban differences in health outcomes, healthcare use, and expenditures among older adults under universal health insurance in China. PLoS ONE 15, e0240194 (2020).
Crosby, K. M. et al. The influence of assistive technology and home modifications on falls in community-dwelling older adults: a systematic review protocol. Syst. Rev. 12, 204 (2023).
Gillespie, L. D. et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, CD007146 (2012).
Huang, J. W., Lin, Y. Y., Wu, N. Y. & Chen, Y. C. Rural older people had lower mortality after accidental falls than non-rural older people. Clin. Interv. Aging 12, 97–102 (2017).
Prince, M. J. et al. The burden of disease in older people and implications for health policy and practice. Lancet 385, 549–562 (2015).
Montero-Odasso, M. et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing 51, afac205 (2022).
Beard, J. R. et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet 387, 2145–2154 (2016).
Liu, T., Zou, H. & Zou, H. Global burden of vertebral fractures and spinal cord injuries due to falls from 1990 to 2021: a population-based study. Global Spine J. https://doi.org/10.1177/21925682251331442 (2025).
Liang, S. et al. Global burden and cross-country inequalities of nutritional deficiencies in adults aged 65 years and older, 1990-2021: population-based study using the GBD 2021. BMC Geriatr. 25, 74 (2025).
Franceschi, C. & Campisi, J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J. Gerontol. A Biol. Sci. Med. Sci. 69, S4–S9 (2014).
Tian, Y. et al. Bidirectional association between falls and multimorbidity in middle-aged and elderly Chinese adults: a national longitudinal study. Sci. Rep. 14, 9109 (2024).
Stevens, J. A. & Lee, R. The potential to reduce falls and avert costs by clinically managing fall risk. Am. J. Prev. Med. 55, 290–297 (2018).
Patton, S., Vincenzo, J. & Lefler, L. Gender differences in older adults’ perceptions of falls and fall prevention. Health Promot. Pract. 23, 785–792 (2022).
Sebastiani, C. et al. Mapping sex and gender differences in falls among older adults: a scoping review. J. Am. Geriatr. Soc. 72, 903–915 (2024).
Ferrucci, L. et al. Measuring biological aging in humans: a quest. Aging Cell 19, e13080 (2020).
Yang, Y. et al. The impact of Otago exercise programme on the prevention of falls in older adult: a systematic review. Front. Public Health 10, 953593 (2022).
Zhong, D. et al. Tai Chi for improving balance and reducing falls: an overview of 14 systematic reviews. Ann. Phys. Rehabil. Med. 63, 505–517 (2020).
Lektip, C. et al. Home hazard modification programs for reducing falls in older adults: a systematic review and meta-analysis. PeerJ 11, e15699 (2023).
Zhang, X. Y., Shuai, J. & Li, L. P. Vision and relevant risk factor interventions for preventing falls among older people: a network meta-analysis. Sci. Rep. 5, 10559 (2015).
Lee, S. H. & Yu, S. Effectiveness of multifactorial interventions in preventing falls among older adults in the community: a systematic review and meta-analysis. Int. J. Nurs. Stud. 106, 103564 (2020).
Reid, I. R. & McClung, M. R. Osteopenia: a key target for fracture prevention. Lancet Diabetes Endocrinol. 12, 856–864 (2024).
Zhu, B. et al. Differences in the global exposure, mortality and disability of low bone mineral density between men and women: the underestimated burden in men. BMC Public Health 23, 991 (2023).
Wei, F. L. et al. Association between vitamin D supplementation and fall prevention. Front. Endocrinol. 13, 919839 (2022).
Lu, Y. et al. Global, regional, and national burden of spinal cord injury from 1990 to 2021 and projections for 2050: a systematic analysis for the Global Burden of Disease 2021 study. Ageing Res. Rev. 103, 102598 (2025).
Liu, S., Tang, Y., Li, J. & Zhao, W. Global, regional, and national trends in the burden of breast cancer among individuals aged 70 years and older from 1990 to 2021: an analysis based on the global burden of disease study 2021. Arch. Public Health 82, 170 (2024).
Li, L. et al. Global patterns of change in the burden of malnutrition in older adults from 1990 to 2021 and the forecast for the next 25 years. Front. Nutr. 12, 1562536 (2025).
Collaborators, G.B.D.N.S.D. Global, regional, and national burden of disorders affecting the nervous system, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 23, 344–381 (2024).
Murray, C. J. L. & Collaborators, G.B.D. Findings from the Global Burden of Disease Study 2021. Lancet 403, 2259–2262 (2024).
Ye, P. et al. Burden of falls among people aged 60 years and older in mainland China, 1990-2019: findings from the Global Burden of Disease Study 2019. Lancet Public Health 6, e907–e918 (2021).
Ekemiri, K. et al. Global burden of fall and associated factors among individual with low vision: a systematic-review and meta-analysis. PLoS ONE 19, e0302428 (2024).
Diseases, G.B.D. & Injuries, C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020).
Foreman, K. J., Lozano, R., Lopez, A. D. & Murray, C. J. Modeling causes of death: an integrated approach using CODEm. Popul. Health Metr. 10, 1 (2012).
Collaboration, G.B.D.C.K.D. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 395, 709–733 (2020).
Collaborators, G.B.D.D. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1160–1203 (2020).
Collaborators, G.B.D.R.F. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1223–1249 (2020).
Collaborators, G.B.D.R.F. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2162–2203 (2024).
Xie, J. et al. Global burden of type 2 diabetes in adolescents and young adults, 1990–2019: systematic analysis of the Global Burden of Disease Study 2019. BMJ 379, e072385 (2022).
Yang, X. et al. Global, regional, and national burden of blindness and vision loss due to common eye diseases along with its attributable risk factors from 1990 to 2019: a systematic analysis from the Global Burden of Disease Study 2019. Aging 13, 19614–19642 (2021).
Pu, L. et al. Projected global trends in ischemic stroke incidence, deaths and disability-adjusted life years from 2020 to 2030. Stroke 54, 1330–1339 (2023).
Collaborators, G.B.D.A.R. Global burden of bacterial antimicrobial resistance 1990-2021: a systematic analysis with forecasts to 2050. Lancet 404, 1199–1226 (2024).
Acknowledgements
The authors received no specific funding for this work. We thank the Global Burden of Disease Study 2021 collaborators for providing access to publicly available data. The views expressed in this article are solely those of the authors and do not necessarily represent the views of the Institute for Health Metrics and Evaluation or its affiliates.
Author information
Authors and Affiliations
Contributions
F.D. and Y.C.: Conceptualization, supervision, software, validation, writing—review and editing; S.H. and A.Z.: Investigation, writing-original draft; Y.W., D.Q. and C.P.: Investigation, data curation; J.G. and Y.G.: Writing—review & editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, Y., Dai, F., Huang, S. et al. Global, regional, and national burden of falls among older adults: findings from the Global Burden of Disease Study 2021 and Projections to 2040. npj Aging 11, 85 (2025). https://doi.org/10.1038/s41514-025-00275-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41514-025-00275-4