Abstract
Immune checkpoint inhibitors (ICIs) have revolutionized cancer immunotherapy, with the microbiome significantly influencing treatment outcomes. Analysis of 4663 studies (2014.01-2024.10) identified 71 eligible randomized controlled trials (RCTs) and cohort studies (41 viral, 30 bacterial). Analyses included subgroup assessments by cancer type, microbial taxa, and ICI regimens. Among 4663 identified studies, 71 met inclusion criteria (41 viral, 30 bacterial). Viral status, particularly hepatitis B virus (HBV) and human papillomavirus (HPV), significantly associated with ORR and DCR. Bacterial enrichment correlated with improved survival in hepatobiliary (OS: HR = 4.33, 95%CI: 2.20–8.50) and lung cancers (PFS: HR = 1.70, 95%CI: 1.04–2.78). Multi-microbiome models demonstrated superior outcome prediction, with microbial diversity correlating with improved PFS (HR = 0.64, 95%CI: 0.42–0.98). Viral status showed cancer-specific associations with SAEs. The microbiome serves as a valuable predictor of ICI outcomes. Future studies should emphasize large-scale RCTs, standardized assessment methods, and host-microbiome interactions.
Similar content being viewed by others
Introduction
Over the past decade, the emergence and widespread application of immune checkpoint inhibitors (ICIs) have not only illuminated the promising integration of precision oncology with immunology but also marked a transformative milestone in cancer immunotherapy. Targeted immunotherapeutic agents, such as inhibitors of programmed cell death protein 1 (PD-1), programmed death-ligand 1 (PD-L1), and cytotoxic T-Lymphocyte-Associated protein 4 (CTLA-4), enhance the immune system’s ability to recognize and eliminate tumors by blocking immune checkpoint protein-mediated immune evasion mechanisms in cancer cells. These therapies have significantly improved clinical outcomes and prognoses for patients with various advanced or recurrent cancers1,2. However, response rates vary substantially between patients, with many showing limited or no benefit. This heterogeneity in treatment response creates an urgent need for reliable predictive biomarkers to guide patient selection and optimize therapeutic strategies3,4,5.
Several biomarkers, including PD-L1 expression, tumor mutational burden, DNA mismatch repair deficiency, immune cell and cytokine infiltration, and metabolic tumor volume via [18 F]FDG-PET/CT, have shown clinical value in predicting ICI efficacy6,7,8,9,10,11,12. However, their application is limited by factors such as genomic-immune interactions, tumor heterogeneity, assay variability, spatiotemporal sampling differences, and the absence of standardized scoring systems tailored to specific drugs or tumor types7,13. While combination ICI therapies have shown significant benefits in advanced cancers14, research on biomarkers for these strategies remains insufficient15. These challenges hinder precise patient selection and treatment decisions. Addressing these limitations is critical for advancing the precision of immunotherapy. Consequently, the development and refinement of novel biomarkers have become pivotal not only for improving the efficacy of precision immunotherapy but also for laying a foundation for the exploration of innovative immunotherapeutic strategies.
Advances in symbiotic microbiome genomics and spatial transcriptomics have increasingly clarified the intricate relationship between tumor immunotherapy and the microbiome, opening new avenues for biomarker development. Evidence suggests that variations in microbiome composition, diversity, and metabolic products profoundly regulate immune cell responses and infiltration, thereby influencing ICI efficacy16,17,18,19,20. Preclinical studies have shown that specific gut microbiota, such as Bacteroides fragilis and Bifidobacterium, enhance CD8 + T cell infiltration and effector functions, improving melanoma responses to ICIs21,22. Additionally, ICI responders often exhibit higher gut microbiome diversity, strongly associated with sustained clinical benefit23,24,25,26,27. This may involve mechanisms such as microbiota-induced T cell responses, molecular mimicry between microbial and tumor antigens, and microbial metabolite regulation of immune homeostasis28. However, controversies remain regarding the key microbial species influencing ICI efficacy, the role of microbiome diversity in prognosis, and balancing therapeutic benefits with adverse event risks29,30. As a significant oncogenic factor, viral infections have also garnered attention in the context of ICIs. While systemic ICI therapy may lead to viral reactivation31, studies suggest that certain viral infections not only fail to increase the risk of virus-associated complications but may also enhance ICI efficacy by suppressing viral replication32,33. Given inconsistencies in current research, a systematic evaluation of microbiome composition’s impact on ICI efficacy and safety is critical for advancing precision immunotherapy strategies.
Given the substantial heterogeneity in immunotherapeutic response and the limited predictive accuracy of established biomarkers, we conducted a comprehensive meta-analysis to evaluate the predictive utility of bacterial and viral microbiome components for ICI efficacy and safety across diverse malignancies. The primary objectives are as follows: (1) Evaluate associations between virome and bacteriome composition with objective response rate (ORR) and disease control rate (DCR) in ICIs. (2) Analyze the relationship between different viral infection statuses, tumor types, and ICI regimens on therapeutic response. (3) Evaluate the predictive value of viral infection status for the risk of ICI-associated adverse events. (4) Investigate correlations between bacterial composition and progression-free survival (PFS)/overall survival (OS) in ICI treatments. (5) Examine the influence of microbial diversity on patient prognosis (PFS and OS). Through this comprehensive analysis, we aims to generate evidence-based insights regarding microbiome-derived biomarkers for immunotherapeutic efficacy and toxicity prediction. Ultimately, this work seeks to advance precision immunotherapy by identifying microbiome-based predictive signatures that may inform patient selection for immunotherapy, enhance outcome prediction accuracy, and potentially guide therapeutic microbiome modulation strategies to optimize clinical benefit.
Results
Study characteristics
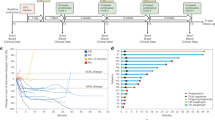
A total of 4663 articles were identified through the initial database search. After screening titles and abstracts, irrelevant studies were excluded, leaving 979 articles for full-text evaluation. Of these, 393 articles were deemed potentially valuable for data extraction. During this process, studies were excluded for the following reasons: reporting only multivariable-adjusted HRs (N = 22), lacking usable efficacy or safety data (N = 268), duplicates (N = 31), and retractions (N = 1). Ultimately, 71 studies were included in the final analysis (Fig. 1). Among the studies evaluating viruses as predictors of ICI outcomes (N = 41)34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71, 29 studies (39 cohorts) reported ORR, with RRs analyzed in 29 cohorts for ORR and 7 cohorts for DCR. Three studies (5 cohorts) assessed ICI safety in relation to viral predictors. For studies evaluating bacterial predictors (N = 30)72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101, 19 studies provided HRs for PFS and OS. Basic characteristics of viral- and bacterial-related studies are summarized in Tables S1 and S2, respectively.
The included studies were published between 2014 and 2024, comprising 63 cohort studies (33 viral-related, 30 bacterial-related) and 8 randomized controlled trials (RCTs) evaluating viral predictors. RCT quality was assessed using the Cochrane ROB tool (Table S3). Most RCTs were open-label designs without blinding but showed low risk of bias for randomization, missing data, and outcome reporting. Cohort study quality was assessed using the NOS (Table S4). Among the 63 cohort studies, 37 cohorts as high-quality studies, NOS scores: ≥9 (N = 1), ≥8 (N = 12), ≥7 (N = 24). 26 cohorts as moderate-quality studies, NOS scores: ≥6 (N = 17), ≥5 (N = 8), >4 (N = 1). All included studies met at least moderate-quality standards. Funnel plot analysis showed that ORR-related cohorts (N = 29) exhibited slight left-sided asymmetry (Fig. S1A), but this funnel plot asymmetry did not reach statistical significance (Egger’s test: t = −0.97, P = 0.34). Meanwhile, substantial heterogeneity existed between studies (τ² = 2.8799), suggesting that this asymmetry likely stemmed from true differences between studies rather than publication bias. The funnel plot for OS-related cohorts (N = 23) displayed mild right-sided asymmetry (Fig. S1B), indicating potential bias or small sample effects. However, the overall Egger’s test results suggested this asymmetry was not statistically significant (t = 0.67, P = 0.51), accompanied by considerable between-study heterogeneity (τ² = 6.5355). PFS-related cohorts (N = 22) demonstrated good symmetry, with Egger’s test also indicating that funnel plot asymmetry was not pronounced (t = 0.31), and publication bias was not significant (P = 0.76) (Fig. S1C).
Microbiota and ICIs efficacy with ORR
Due to variations in endpoints and reported outcomes in studies evaluating the predictive value of viruses and bacteria in ICI efficacy, 34 cohorts reported ORR for microbial exposure vs. control groups, while only 25 and 22 cohorts provided HRs for PFS and OS, respectively. Given these discrepancies, ORR was selected as the primary metric for assessing the predictive value of baseline microbiota on ICI outcomes, including viruses, individual bacterial species, and bacterial communities. The meta-analysis revealed a pooled RR of 1.29 (95% CI: 1.07–1.55, P = 0.049) across 34 cohorts, with moderate heterogeneity (I2 = 55.6%), indicating a significant association between baseline microbiota and ICI efficacy. Subgroup analysis showed a pooled RR of 1.28 (95% CI: 1.11–1.47, P < 0.001) for virus-related cohorts (N = 27), with lower heterogeneity (I2 = 47.9%), suggesting that baseline viral status is a critical predictor of ICI response. In contrast, the predictive value of bacterial communities was relatively limited, with the small number of bacterial-related cohorts (N = 5) reporting ORR underscoring the need for further evidence to confirm this conclusion (Fig. 2A). Additionally, meta-analysis encompassing 21 monotherapeutic ICI (Anti-PD-1/PD-L1/CTLA-4) cohorts demonstrated a combined RR of 1.40 (95% CI: 1.23–1.60, P < 0.001, N = 21), with a heterogeneity index I²of 25.9%. This finding suggests that microbial status may serve as a valuable predictive biomarker for response to single-agent ICI therapy. Notably, this investigation extended to unconventional immune checkpoint blockers (ICBs), including KL-A167 (Shi et al.10) and Bintrafusp alfa (Chiang et al.67). Interestingly, microbial status exhibited a negative correlation with efficacy for these novel ICBs, yielding a RR of 0.58 (95% CI: 0.41–0.82, P = 0.002, N = 4). Nevertheless, given that the analysis incorporated only two specific unconventional ICBs, the relationship between microbial status and clinical outcomes for these emerging therapeutic agents warrants further validation through more comprehensive and diverse clinical investigations (Fig. S1D).
Virus-associated efficacy analysis with ORR
Using ORR as the primary endpoint (N = 29), subgroup analysis was conducted to compare viral-positive versus viral-negative groups, as well as elevated versus reduced EBV DNA levels, as observation and control groups, respectively (Fig. 2B). The viral subgroup analysis revealed a pooled RR of 1.36 (95% CI: 1.09–1.69, P = 0.008) with moderate heterogeneity (I2 = 51.1%), confirming a significant association between viral status and treatment efficacy. Further analysis by viral type identified hepatitis B virus (HBV) and human papillomavirus (HPV) as strong predictors of ICI outcomes, with RRs of 1.36 (95% CI: 1.10–1.67, P = 0.005, N = 9) and 1.61 (95% CI: 1.19–2.18, P = 0.002, N = 7), respectively. Notably, heterogeneity was low in these subgroups (HBV: I2 = 16.7%; HPV: I2 = 0.0%). Subgroup analysis by tumor type revealed differences in the predictive performance of viral status across cancers (RR: 1.36 [95% CI: 1.10–1.67], P = 0.588), likely reflecting the distribution of viral types among tumors. HBV and HPV were key contributors to the overall results. Viral status was notably correlated with ICI efficacy in hepatobiliary cancers, with a pooled RR of 1.71 (95% CI: 1.22–2.38, P = 0.002, I2 = 0.0%), consistent with findings from the HBV subgroup, underscoring HBV as a critical predictive factor for ICI response. Analysis of ICI regimens also highlighted virus as significant predictors of treatment efficacy (P = 0.034). In the ICI monotherapy subgroup, the pooled RR was 1.46 (95%CI: 1.22–1.74, P < 0.001, N = 16), indicating a robust correlation between viral status and treatment outcomes in single-agent ICI. However, viral status did not reach statistical significance as a predictor in combination therapies or specialized ICB regimens. In the subgroup analysis based on sampling sites, tissue-derived samples exhibited a pooled RR of 1.76 (95% CI: 1.33–2.33, P < 0.001, N = 8), indicating that, compared to plasma-based assessments, tumor tissue-derived viral signatures may serve as a more reliable predictor of ORR (Fig. S6A). Supplementary results are provided in Fig. S2–S4 (ORR and 95% CI for virus-positive patients stratified by viral group, tumor type, and ICB regimens) and Fig. S6B (impact of viral status on PFS with HRs). The pooled ORR was 27% (95% CI: 25–29%), demonstrating statistical significance across viral and tumor subgroups with moderate heterogeneity (I2 = 63.6%). These findings underscore the critical role of baseline viral status, particularly for specific viral types and cancer contexts, in predicting ICI efficacy.
Virus-associated efficacy analysis with DCR
Using DCR as a secondary endpoint (N = 7), subgroup analysis was conducted on seven included study cohorts (Fig. 3). The pooled analysis revealed significant heterogeneity (I2 = 82.7%) and a combined RR of 0.99 (95% CI: 0.71–1.39, P < 0.001), indicating substantial variability in the predictive value of viral status for DCR, which may limit its utility as an independent prognostic marker. Analysis by viral type showed contrasting predictive patterns: the pooled RR for HBV was 1.29 (95% CI: 1.10–1.50, P = 0.001, N = 4), demonstrating a significant positive correlation with DCR, whereas the RR for EBV was 0.63 (95% CI: 0.52–0.77, P < 0.001, N = 3), indicating a significant negative correlation with DCR. Both subgroups exhibited low heterogeneity (HBV: I2 = 28.1%; EBV: I2 = 0.0%), suggesting consistent results within these cohorts. Subgroup analysis by tumor type revealed that viral status was a significant predictor of DCR in lung cancer, hepatobiliary cancer, and nasopharyngeal carcinoma (NPC). EBV consistently demonstrated a negative predictive value in NPC (RR = 0.63, 95% CI: 0.52–0.77, P < 0.001, N = 3). HBV showed strong predictive value for DCR in lung cancer (RR = 1.73, 95% CI: 1.13–2.65, P = 0.012, N = 1) and hepatobiliary cancer (RR = 1.69, 95% CI: 1.02–2.80, P = 0.043, N = 1). However, these results were drawn from single cohorts for each tumor type, limiting the statistical power and emphasizing the need for further validation. Subgroup analysis of ICB treatment regimens revealed distinct predictive patterns for viral status. The pooled RR of monotherapy group (4 cohorts) was 1.29 (95% CI: 1.10–1.50, P = 0.001, N = 4), consistent with the predictive value observed for HBV. Conversely, the pooled RR for other ICB treatment regimens was 0.63 (95% CI: 0.52–0.77, P < 0.001, N = 3), aligning with the negative predictive value of EBV. These findings reflect the differing roles of HBV and EBV as predictors in ICB therapies, highlighting their distribution patterns across treatment regimens and tumor types.
Bacteria-associated prognostic analysis with HR
This study evaluated the impact of bacterial status on ICI efficacy using HRs for PFS and OS. A total of 19 studies were included in the subgroup analysis (PFS: 14 studies; OS: 12 studies), comparing bacteria-presence vs. bacteria-absence groups and enriched vs. depleted bacterial communities. Subgroup analysis by tumor type revealed no statistically significant overall predictive effect of bacterial status on OS or PFS. However, the predictive value of bacteria varied across specific tumor types. For OS, bacterial status showed statistical significance in melanoma and mesothelioma, but these findings were based on single study cohorts, limiting their reliability. In contrast, bacterial enrichment in hepatobiliary cancers demonstrated a strong predictive value for OS compared to bacterial depletion (HR = 4.33 [95% CI: 2.20–8.50], P < 0.001, N = 3), with no observed heterogeneity (I2 = 0.0%) (Fig. 4A). For PFS, bacterial status displayed significant prognostic value in several tumor types. In gastrointestinal cancers, bacterial status was negatively associated with PFS (HR = 0.82 [95% CI: 0.70–0.96], P = 0.016, N = 4), suggesting a potential reduction in sustained ICI benefits. Conversely, in lung cancer, bacterial status was positively correlated with PFS (HR = 1.70 [95% CI: 1.04–2.78], P = 0.035, N = 2). Similarly, in hepatobiliary cancers, enriched bacterial communities were linked to significantly improved PFS compared to depleted communities (HR = 2.33 [95% CI: 1.54–3.53], P < 0.001, N = 3), consistent with the OS analysis. In contrast, under a fixed-effect model, enrichment of bacteria showed a potential negative correlation with PFS in lung cancer (HR = 0.75 [95% CI: 0.58–0.96], P = 0.023, N = 5). In mesothelioma and urothelial carcinoma, single studies suggested specific bacterial enrichments were associated with PFS (Fig. 4B), but further research is needed to confirm the generalizability of bacteria as predictive markers.
At the bacterial phylum level (Fig. 5A, B), all included studies focused on single bacterial taxa. Results showed that Verucomicrobia enrichment was significantly associated with OS in one study (HR = 2.63 [95% CI: 1.53–4.52], P < 0.001, N = 1), while Bacteroidetes enrichment was significantly associated with PFS in another study (HR = 2.54 [95% CI: 1.18–5.44], P = 0.017, N = 1). However, as these findings stem from single study cohorts, the predictive value of bacterial phyla for ICI outcomes remains inconclusive and requires further validation. Overall, no significant association was identified between specific bacterial phyla and OS or PFS following ICI treatment. To explore the predictive value of bacteria in greater depth, studies were classified into two subgroups based on bacterial composition: single versus multiple bacterial communities (Fig. 5C, D). Subgroup analysis of OS showed no significant impact of either single or multiple bacterial communities on OS. However, enrichment of multiple bacterial taxa demonstrated a potential negative association with OS (HR = 0.54 [95% CI: 0.29–1.0], P = 0.049, N = 1). Since the upper bound of the CI equals 1.0 and this result is from a single study, further evidence is necessary to confirm its robustness. Similarly, no significant association was observed between single or multiple bacterial communities and PFS. However, under a fixed-effect model, enrichment of multiple bacterial taxa showed a potential negative correlation with PFS (HR = 0.64 [95% CI: 0.42–0.98], P = 0.039, N = 2). Notably, studies evaluating the predictive value of multiple bacterial communities were limited in number and sample size, with high heterogeneity (I² = 81.3%), underscoring the need for further research.
To further evaluate the impact of high-throughput sequencing heterogeneity on the predictive role of bacterial abundance in ICIs, all studies were standardized to a uniform sample environment, stool. The results indicated that metagenomic sequencing associated microbial composition with worse OS (HR = 3.20 [95% CI: 2.10–4.88], P = 0.000, N = 4). In terms of PFS (N = 13), no significant differences were observed between the two sequencing methods. Overall, the differences in sequencing techniques did not reach statistical significance, and high heterogeneity was observed among the studies (Fig. S5A, B).
Safety evaluation
Three studies (N = 5) evaluated the association between viral status and ICI-related adverse events (irAEs) as well as sever adverse events (SAEs). These studies compared the incidence of irAEs (all grades) and ≥Grade 3 SAEs between virus-positive and virus-negative patients, with a particular focus on HBV and HPV. The overall analysis showed no significant correlation between viral status and irAEs across subgroups (RR = 1.04, 95% CI: 0.92–1.17, P > 0.05) (Fig. S6C). Similarly, the pooled analysis for SAEs revealed no significant association (RR = 1.10, 95% CI: 0.57–2.25, P = 0.570) and high heterogeneity (I² = 72.8%) (Fig. S6D). When stratified by tumor type, the analysis of three cohorts focusing on hepatobiliary cancers showed a marginally significant association between viral status and SAEs (RR = 0.62, 95% CI: 0.39–1.00, P = 0.048, N = 3). However, given that the upper bound of the CI equals 1.0, this finding requires further validation with larger sample sizes. Analysis of ICI treatment regimens revealed that, in two monotherapy cohorts, viral status was significantly associated with an increased risk of SAEs (RR = 2.31, 95% CI: 1.35–3.94, P = 0.002, N = 2), suggesting that viral infections may heighten the risk of SAEs. Notably, the ICI combination therapy cohorts overlapped with the hepatobiliary cancer studies, and the results were mutually supportive.
Discussion
This study systematically evaluated the predictive value of the microbiome for the efficacy and safety of ICIs in cancer treatment. The meta-analysis revealed that the relationship between the microbiome and ICI efficacy varied by microbial type, tumor type, treatment strategy, sampling site, and bacterial model configurations. Overall, baseline microbiomes demonstrated a significant predictive effect on ORR to ICIs (RR = 1.29, 95% CI: 1.07–1.55, P = 0.049, N = 34), with viral microbiomes and monotherapeutic ICI showing particularly strong predictive performance. Subgroup analyses further highlighted the role of viruses in predicting ICI efficacy, with a pooled RR of 1.36 (95% CI: 1.09–1.69, P = 0.008, N = 29). Among viral types, HBV and HPV exhibited superior predictive capacity. Viral status also correlated significantly with clinical benefits in hepatobiliary cancers (P = 0.002, N = 10) and in patients receiving monotherapy (P < 0.001, N = 16). Additionally, tumor tissue sampling appeared to enhance the predictive value of viral biomarkers for ORR(RR = 11.76) (95% CI: 1.33–2.33, P < 0.001, N = 8). Supplementary analyses using DCR confirmed the predictive potential of specific viruses, with variability across viral types. HBV was positively associated with ICI efficacy (RR = 1.29, 95% CI: 1.10–1.50, P = 0.001, N = 4), whereas EBV was negatively associated (RR = 0.63, 95% CI: 0.52–0.77, P < 0.001, N = 3). For bacteria, while the overall predictive effect on ICI outcomes was inconsistent, bacterial enrichment was significantly associated with clinical benefits in specific tumor types, including hepatobiliary cancers (P < 0.001, N = 3), gastrointestinal tumors (P = 0.016, N = 4), and lung cancer (P = 0.035, N = 2). Moreover, multi-microbiome predictive models demonstrated a significant association with PFS in ICI treatment (HR = 0.64, 95% CI: 0.42–0.98, P = 0.039, N = 2). In terms of safety, viral presence was not significantly associated with the overall occurrence of (S)AEs. However, viral status showed potential predictive value for SAEs in patients with hepatobiliary cancers and those receiving monotherapy. Although the number of included studies and sample sizes were limited, this study provides preliminary evidence supporting the microbiome’s potential as a predictive biomarker for ICI therapy. These findings lay the groundwork for further research exploring the microbiome’s application in cancer immunotherapy, highlighting its value as an emerging area of study.
This meta-analysis demonstrates that viruses within the microbiome hold significant predictive value for the clinical efficacy of ICIs, with HBV and HPV showing particularly strong associations with treatment benefits. Notably, viral status exhibited robust predictive performance in ICI therapy for hepatobiliary cancers, validating prior studies suggesting that HBV-associated hepatocellular carcinoma (HCC) patients are likely to benefit from ICIs therapy33. Additionally, no significant alterations in viral load were detected in patients receiving consistent antiviral therapy during ICI treatment, with no documented HBV reactivation or HCV recurrence observed71. These findings support the hypothesis that specific viruses can enhance antitumor immune responses102. Virus-associated tumor microenvironment (TME) may be related to the dynamic transformation and activity of immune cells103. At the single-cell level, studies have shown that in HBV-associated TME, effector CD8 + T cells undergo function evolution, correlating with improved survival in advanced HCC. Enrichment and activation of HBV-specific tissue-resident memory CD8 + T cells have also been identified as critical mechanisms for effective immunotherapy in HCC104. Similarly, HBV-specific CD8 + T cells belong to the CD8+ effector/effector memory T cell (CD8+Teff/Tem) subset, exhibiting characteristics similar to circulating effector memory T cells (cTem) and progenitor exhaustion T cells (Tpex). Compared to HBV-T cells, HBV + T cells demonstrate greater potential for migration, infiltration, memory response, and clonal expansion, supporting enhanced immunotherapeutic responses105. Immune-related gene expression profiling in HPV-positive oropharyngeal squamous cell carcinoma has revealed CD8 + T cell enrichment and high checkpoint protein expression in the TME, suggesting that ICIs may activate potent antitumor immunity in these patients106. HNSCC is differentiated into immune-hot and immune-cold types based on HPV infection status, with immune-hot HPV + HNSCC containing various fibroblasts with distinct immunomodulatory functions, particularly IL11+ inflammatory cancer-associated fibroblasts (iCAFs) associated with inflammatory stimuli and CCL19+ fibroblastic reticular cell-like (FRC) cells related to the activation of CD4 + T cells and B cells through lymphotoxin signaling, both of which researchers consider to be associated with positive immunotherapeutic responses107. However, there are discrepancies in the predictive role of viral status. Ho et al. compared the clinical benefits of PD-1/PD-L1 inhibitors in HCC patients with and without HBV/HCV infections, finding no significant differences in TME immune cell infiltration subtypes or immune checkpoint molecule expression levels108. This discrepancy may be related to the balance of inflammation and immune recognition mechanisms within the TME108,109. On one hand, viral infections can activate cytokine networks, promoting antitumor immunity by enhancing immune cell activation. On the other hand, chronic viral infections, as oncogenic factors, may impair T cell-specific recognition of virus-infected or tumor-associated cells. Continuous viral replication and chronic inflammatory responses may disrupt immune homeostasis, leading to immune evasion and tissue damage. Our analysis of DCR revealed opposing trends for HBV and EBV. HBV was positively associated with ICI efficacy, while EBV infection correlated with poorer outcomes. Furthermore, patients demonstrating response to anti-PD-1 therapy exhibited significantly enhanced clinical benefits compared to those characterized by Epstein-Barr virus progression (defined as viral DNA load exceeding 1.5-fold baseline), viral response (defined as DNA load below 0.5-fold baseline), or early clearance of plasma EBV DNA50. These findings align with prior studies indicating that EBV reduces ICI effectiveness through mechanisms such as increasing PD-L1 expression, linking to CD8 + T cell exhaustion, and recruiting immunosuppressive factors110,111,112,113. Interestingly, McMiller et al. found that EBV-negative gastric cancer exhibited activation of the COX-2/PGE2 pro-inflammatory pathway, significantly suppressing responses to anti-PD-1/PD-L1 therapy110. This highlights the complex role of EBV infection in modulating ICI efficacy. While viral status has been proposed as a potential biomarker for ICI efficacy, the variability in findings and mechanistic explanations suggests that its predictive role requires further clarification. Future studies should incorporate larger real-world datasets and well-designed clinical trials to comprehensively explore the predictive value of viral status in ICI therapy.
Notably, numerous investigations have demonstrated a bidirectional immunoregulatory relationship between ICI efficacy and specific bacterial taxa abundance profiles. In melanoma patients responding to immunotherapy, significantly elevated abundances of Ruminococcaceae and Faecalibacterium have been documented compared to non-responders. Conversely, in microsatellite instability-high CRC patients, Fusobacterium nucleatum abundance demonstrated inverse correlation with tumor-infiltrating lymphocyte immunological status114. In preclinical murine models, antibiotic-treated mice demonstrated restoration of anti-CTLA-4 immunotherapeutic responses following selective recolonization with Bacteroides fragilis, with efficacy correlating with bacterial abundance. This phenomenon appears mediated through Bacteroides fragilis-induced enhancement of CD4 + Th1 immune responses within tumor-draining lymph nodes and potentiation of dendritic cell antigen presentation capacity21. Furthermore, anti-CTLA-4 therapy administration did not significantly alter Bacteroides fragilis abundance, highlighting the stability of microbiome-immunotherapy interactions in this context. Subsequent investigations have established that Faecalibacterium spp. exert immunomodulatory effects in murine models receiving anti-CTLA-4 therapy, whereas Dorea formicogenerans specifically enhances anti-PD-L1 therapeutic efficacy76. In human clinical investigations, Chaput et al. demonstrated significant associations between baseline intestinal microbiota composition and therapeutic response in metastatic melanoma patients receiving ipilimumab treatment. Specifically, patients with Faecalibacterium-enriched microbiota exhibited enhanced cellular immunity following ipilimumab administration, characterized by elevated expression of co-stimulatory molecules on CD4 + T cells100. However, this investigation lacked prospective longitudinal assessment of microbiome compositional dynamics during ICI therapy, precluding establishment of causal relationships between microbiota alterations and therapeutic outcomes. Given that microbial analyses in existing studies predominantly involve monotherapeutic immunotherapy regimens, or utilized a mixed ICI system to systematically explore the correlation between microbiota and immunotherapy efficacy, current literature lacks robust subgroup analyses examining associations between specific bacterial taxa and distinct immunotherapeutic agents or combination strategies.
Subgroup analysis of sampling sites revealed differences in the correlation between viral status and ICI efficacy across different sampling sites. Notably, viral detection results from tumor tissues may provide more reliable predictions of ICI treatment outcomes. Intratumoral microbes potentially serve as tumor subtype markers, with viruses specifically distributed within tumor tissues triggering or directly participating in specific immune responses, thus more accurately reflecting the actual tumor immune-related conditions. Multiple studies have successively demonstrated that intratumoral microbiota produce multiple effects including metabolic remodeling and immune regulation, thereby influencing tumor immunotherapy responses27,115,116,117,118. Similarly, immune responses within EBV gastric cancer subtypes are associated with EBV-related CD8 + T cells, regulatory T cells(Treg), NK cells, and macrophage infiltration, accompanied by abundant PD-L1 expression. However, current research findings on the correlation between PD-L1 expression levels and patient survival remain highly controversial, indicating significant heterogeneity in EBV gastric cancer subtype responses to anti-PD-1/PD-L1 immunotherapy119. The development and efficacy evaluation of therapeutic vaccines targeting the TME and its surrounding immune responses further confirm that virus infiltration within tumors can enhance host responses to initial immunotherapy120. Furthermore, considering the proteomic characteristics and immunogenicity of tumor-associated bacteria and viruses, online data atlases represented by MicroEpitope have detailed the correlation between intratumoral microbe-derived epitopes and immune responses in different tumor microenvironments121. This database systematically integrates proteomic information of tumor-associated bacteria and viruses, exploring microbial immunogenicity and its clinical relevance in depth. For example, in lung cancer, the epitope “AEMLREEGY” derived from Mycobacterium tuberculosis is recognized by T cells after presentation by HLA-I molecules, effectively inducing T cell immune responses; while in chronic lymphocytic leukemia, the EBV-derived epitope “LLDFVRFMGV” can specifically activate cytotoxic T cell responses121. In conclusion, microbial detection within tumor tissues offers greater advantages in predicting ICI efficacy, but tumor tissue heterogeneity and potential sampling bias must be fully considered.
This meta-analysis indicates that bacterial status and enrichment levels lack overall predictive value for ICI efficacy but show differential associations with outcomes in specific cancers. Subgroup analyses revealed a positive correlation between bacterial status and survival in hepatobiliary and lung cancers, while a negative correlation was observed in gastrointestinal tumors. Several studies have reported compositional differences in gut microbiota between ICI responders and non-responders, underscoring the significant impact of microbiota variability on ICI efficacy24,122,123,124,125. However, the precise relationship between gut bacteria and tumor progression or prognosis remains incompletely understood. Complex host-microbiota interactions are recognized as correlating with cancer progression, with bacterial toxins and metabolites directly activating oncogenic pathways or suppressing immune-regulatory signals, particularly in colorectal cancer126. Emerging concepts such as the gut-lung axis127 and gut-liver axis128 highlight inter-organ feedback mechanisms mediated by microbiota-immune system interactions. Evidence suggests that dietary interventions and supplementation with probiotics or prebiotics may improve antitumor immune responses129,130. Furthermore, fecal microbiota transplantation (FMT) from ICI responders has shown potential to restore gut microbial balance and enhance therapeutic efficacy131,132,133. Our preliminary research included 10 clinical studies published up to September 2024, demonstrating that FMT combined with ICIs treatment achieved a 43% ORR, significantly superior to the 20–40% response rate of single-agent ICIs therapy reported in previous studies, without significantly increasing toxic risk. Further analysis indicated that treatment efficacy potentially correlates with ICI regimens, FMT donor sources, and FMT administration methods134. However, FMT’s efficacy is influenced by variability in beneficial microbial compositions across cohorts and tumor types, presenting a critical challenge for its application in cancer therapy. The differential associations between bacterial enrichment and survival outcomes across tumor types likely arise from the dynamic interactions among bacteria, the host, and the immune system. For gastrointestinal tumors, the included cohorts primarily focused on Helicobacter pylori, a known gastric cancer pathogen, which may have increased cohort heterogeneity and introduced selection bias. Indirect effects of bacteria on ICI efficacy may depend not only on their oncogenic or tumor-suppressive properties but also on factors such as host condition, tumor heterogeneity, and sampling site or timing. For example, Wu et al. demonstrated that intratumoral Streptococcus predicted responses to combined chemotherapy and ICI therapy in esophageal squamous cell carcinoma (ESCC), proposing that cross-reactivity between bacterial and tumor antigens within the TME, affecting immunotherapy efficacy by increasing the infiltration of granzyme B-positive (GRZB + ) CD8 + T cells in tumors and regulating the ratio between CD8+ Tem and CD4+ Treg117. Due to the limited sample size and availability of cohorts, most bacterial samples in this meta-analysis were derived from fecal specimens, with fewer from extracellular vesicles or tumor tissues. This limitation in sampling sources may have led to an incomplete assessment of the predictive capacity of bacteria. Future high-quality clinical studies are needed to address confounding factors affecting bacterial predictive power, scientifically evaluate the microbiota’s role in ICI efficacy, and explore the mechanisms of microbiota-tumor interactions across different cancer types.
This meta-analysis highlights that multi-microbiome combinations exhibit stronger predictive value for ICI efficacy compared to single microbial taxa. The therapeutic effectiveness of ICIs depends on a healthy gut microbiota, which requires microbial diversity and dynamic equilibrium with the immune system135,136. This complex microbiota-immune regulatory network involves microbial synergy, functional complementarity, metabolite-mediated immune modulation, and microenvironmental remodeling. Numerous studies have shown that increased gut microbiome diversity is closely associated with improved responses to ICIs25,123,137,138. Conversely, the use of antibiotics during ICI treatment has been confirmed as an independent risk factor for poor clinical outcomes, likely due to persistent microbiota diversity loss139,140. However, FMT from ICI responders has demonstrated the ability to restore microbial diversity and re-establish antitumor activity139,141,142. Despite these findings, some studies have reported conflicting results regarding the direct association between microbiota diversity and ICI efficacy30,143. Such discrepancies may arise from cohort heterogeneity, differences in microbiome diversity analysis methods, or inconsistent evaluation criteria. Traditional measurements of species richness and abundance should be complemented by microbial genomic variation analyses for a more comprehensive understanding of diversity. For instance, Liu et al. using metagenomic sequencing, identified highly variable structural variations in microbial genomes, which were associated with ICI treatment outcomes in patients with renal cell carcinoma, non-small cell lung cancer (NSCLC), and melanoma144. Similarly, Derosa et al. analyzed the genomic characteristics of fecal samples from advanced NSCLC patients and successfully constructed a species-level co-abundance network. They identified two competing multi-microbiome groups with distinct functional patterns and metabolic pathways. They identified two competing multi-microbiome groups with distinct functional and metabolic patterns, which drove clinical responses to ICIs and demonstrated exceptional predictive value145. These multi-dimensional studies, integrating metagenomics and functional metabolomics, underscore the critical role of microbiota diversity in predicting ICI efficacy. Moreover, they open new avenues for exploring multi-microbiome interaction networks and the regulatory mechanisms of the tumor-microbiota-immune system axis. Regarding the potential heterogeneity introduced by the choice of transcriptomic or metagenomic sequencing in assessing the predictive value of microbial communities for ICIs, current evidence does not support a significant influence. 16S rRNA sequencing represents the predominant methodological approach for characterizing bacterial community diversity. The relatively conserved nature and manageable amplicon length of the 16S rRNA confers robust analytical stability across high-throughput sample processing workflows. In contrast to 16S rRNA sequencing, whole-genome shotgun metagenomic sequencing provides more comprehensive taxonomic and functional characterization, encompassing broader genomic content and enabling higher-resolution bacterial community profiling. The shotgun metagenome sequencing facilitate identification and characterization of low-abundance viral populations and taxonomically challenging bacterial communities that remain undetectable through single-marker gene methodologies146,147. In our analysis, while both widely implemented 16S rRNA and metagenomic sequencing methodologies generated divergent findings regarding microbial community predictive utility for ICI responses, metagenomic approaches demonstrated superior associations with long-term immunotherapeutic outcome prediction. Previous investigations have demonstrated that at higher taxonomic ranks, 16S rRNA and metagenomic sequencing approaches exhibit substantial concordance in alpha diversity metrics, including community richness, evenness indices, and relative abundance distributions148. However, these methodologies diverge substantially when characterizing fine-scale diversity patterns and community structural attributes, with shotgun metagenomic approaches offering enhanced taxonomic resolution, sensitivity, and specificity at species-level identification149. As investigations evaluating microbiome-based predictive biomarkers for immunotherapeutic efficacy predominantly analyze taxonomic signatures at phylum level and below, the methodological concordance between these sequencing approaches becomes less apparent, although meta-analyses suggest non-significant statistical differences in overall predictive performance. Furthermore, observed discrepancies likely derive from fundamental methodological distinctions between these analytical approaches, including differences in sample preparation, nucleic acid extraction protocols, bioinformatic processing pipelines, and inherent technical biases.
This meta-analysis evaluated the predictive value of viral status for adverse events (AEs) during ICI treatment, revealing that viral status may predict the risk of SAEs in patients with hepatobiliary cancers. Early studies have demonstrated that in patients with chronic HBV infection undergoing ICI therapy, the addition of intensified antiviral treatment can significantly reduce the risk of viral reactivation150,151. This finding provides critical guidance for clinical practice, suggesting that enhanced antiviral therapy could be a key strategy to ensure the safe administration of ICIs in HBV-infected patients. IrAEs are believed to result from immune activation and immune-mediated tissue damage during ICI therapy. However, the relationship between irAEs and viral reactivation remains unclear. Notably, studies have reported that the occurrence of irAEs is associated with increased hepatitis B surface antigen (HBsAg) levels and a higher risk of HBV replication152. These observations underscores the need to investigate the causal relationship and interaction mechanisms between irAEs and viral status. A deeper understanding of these dynamics is essential for developing effective strategies to prevent AEs and viral reactivation during ICI therapy. Although research on the relationship between the microbiota and irAEs is limited, emerging evidence suggests a potential link between gut microbiota composition and the development of specific irAEs. For example, recolonization of Enterobacteriaceae during ICI treatment has been implicated in increasing intestinal inflammatory toxicity through the expression of inflammatory cytokine IL-1β153. This phenomenon is particularly pronounced in dual ICI combination therapies, where it has been associated with an increased incidence of severe AEs30. These findings suggest that the gut microbiota may play a critical role in the development of irAEs, particularly in the context of combination immunotherapies.
Despite providing significant evidence for the role of the microbiome in predicting tumor response to ICIs, this meta-analysis has several limitations. Firstly, the analysis primarily included moderate- to high-quality cohort studies, with a lack of RCTs. This limitation may reduce the ability to control for confounding factors and restrict causal inference. Secondly, endpoints related to viruses and bacteria was incomplete across the included studies, and there was heterogeneity in the selection of endpoints. Specifically, studies on virus lacked long-term follow-up data, limiting the evaluation of sustained predictive value. Studies on bacteria lacked data on AEs following treatment, which may have hindered a comprehensive assessment of the microbiome’s predictive capacity for safety outcomes. Furthermore, the presence and enrichment of bacteria were primarily analyzed using binary classifications based on study descriptions, without standardized sequencing analysis or categorization. This approach may oversimplify complex bacterial community states and fail to capture intricate relationships between bacterial diversity and ICI efficacy, potentially underestimating these associations.
This meta-analysis presents preliminary evidence-based findings on the predictive value of the microbiome for ICI efficacy and safety across various cancer types. The results demonstrate that the microbiome has significant predictive potential for ICI outcomes, particularly in monotherapy settings, with notable variations in the associations between distinct viral and bacterial groups and clinical responses across tumor types. Furthermore, this study underscores the potential value of multi-microbiome predictive models while identifying critical gaps in the research on the microbiome’s role in predicting ICI safety, offering new directions for investigating the interplay between the microbiome and immunotherapy. Despite the limitations of this study, such as the restricted scope of included studies and insufficient depth of subgroup analyses, it systematically summarizes the current applications and future directions for microbiome-based prediction in ICI efficacy. The findings highlight the necessity of conducting large-scale RCTs, standardizing microbiome assessment frameworks and prognostic evaluation criteria, advancing the development of multi-microbiome predictive models, and integrating analyses of host-microbiome interactions. These research priorities are essential for developing optimal strategies and providing robust evidence to clarify the microbiome’s influence on tumor progression and immunotherapy outcomes, paving the way for more precise and effective applications of microbiome-based biomarkers in cancer immunotherapy.
Methods
This meta-analysis was designed and conducted in strict accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. As the study exclusively uses de-identified patient data, it does not require ethical committee approval or informed consent, in compliance with relevant regulations. This study has been registered in PROSPERO(CRD42025630951).
Search strategy
To systematically identify studies examining the relationship between the microbiome and ICI efficacy and safety in cancer treatment, a comprehensive search strategy was developed (see Data S1). The databases searched included PubMed, Web of Science, Medline, Embase, Cochrane Library, Wiley Online Library, ClinicalTrials(ClinicalTrials.gov, or published on conference abstracts, including the European Society for Medical Oncology (ESMO), the American Society of Clinical Oncology (ASCO), and the American Association of Cancer Research(AACR)) covering the period from January 1, 2014, to October 9, 2024. Only human studies were included, with no restrictions on publication type or language.
Eligibility criteria
Three researchers independently performed the literature search, screened titles and abstracts, and conducted full-text evaluations to extract data on treatment efficacy and safety. Discrepancies were resolved through discussions with senior researchers. The inclusion criteria were: (1) RCT or cohort studies involving patients with pathologically confirmed malignancies. (2) Studies including in vivo microbiome profiling with explicit microbiome characteristics. (3) Studies reporting associations between the microbiome and ICI treatment outcomes. At least one of the following efficacy endpoints was required: ORR, DCR, Partial response (PR), Complete response (CR), Stable disease (SD), PFS, OS, and unadjusted hazard ratios (HRs) in univariate analyses. (4) Studies reporting the occurrence of irAEs or SAEs. Exclusion criteria were: (1) Animal studies. (2) Studies lacking data on pre-treatment microbiome profiles and ICI efficacy or safety. (3) Studies without specific microbiome classifications. (4) Studies reporting only adjusted HRs from multivariate analyses.
Data extraction
Three researchers independently extracted data, ensuring accuracy through cross-verification. Baseline characteristics included tumor type, ICI regimens, microbial composition, microbiome sample type, and sequencing approaches. For bacterial studies, microbial composition was categorized based on phyla. Grouped studies included monobacterial vs polybacterial studies, focusing on discussing predictive value of single dominant or microbial community. Additionally, a clear distinction was maintained between microbiome-presence vs. microbiome-absence groups and high vs. low microbiome abundance groups. Given the inconsistent thresholds for classifying bacterial abundance across studies, we defined ‘high’ as exceeding the study-specific average in our analysis. Outcome variables included treatment efficacy indicators and AE/SAE incidence rates. Studies assessing microbiomes after pre-treatment with proton pump inhibitors (PPIs) or antibiotics were included in the analysis.
Risk of bias assessment
The quality of cohort studies was assessed using the Newcastle–Ottawa Scale (NOS), while RCT risk of bias was evaluated using the Risk of Bias (ROB) tool in RevMan 5.4. Quality assessments were independently conducted by three researchers, with disagreements resolved through consensus. For cohort studies, NOS scores <4 indicated low quality, while ≥7 indicated high quality. RCTs were categorized as low, high, or unclear risk of bias (Table S3 and S4). Publication bias, a common issue in meta-analyses, was assessed using funnel plots and Egger’s test to ensure reliability.
Statistical analysis
Meta-analyses were conducted using RevMan (Version 5.4, Cochrane, UK) and R (Version 4.4.1) with packages such as meta (Version 8.0.1), grid (Version 4.4.1), forestplot (Version 3.1.6), and metafor (Version 4.6.0). Primary analyses examined the relative risk (RR) for microbiome-associated ORR and DCR, and HRs for bacteria-associated PFS and OS. Safety analyses focused on AE/SAE incidence rates. Subgroup analyses stratified studies by virus type, cancer type, and ICI regimen for virus-related studies, with ORR and 95% confidence intervals (CIs) extracted as predictive factors. For bacteria-related studies, subgroup analyses were based on bacterial phyla, microbial abundance, cancer type, and sequencing methods, with HRs for PFS and OS used as prognostic indicators. Both fixed-effect and random-effect models were used for pooled analyses, depending on heterogeneity assessed by the Q test and I2. Fixed-effect models were applied for I2 < 50%(low heterogeneity), while random-effect models were used for I2 > 50%(high heterogeneity). Statistical significance was set at P < 0.05.
Data availability
Data sharing is not applicable to this article as no new data were created or analyzed in this study. Code Availability: Code sharing is not applicable to this article.
References
Lenz, H.-J. et al. First-line Nivolumab plus low-dose Ipilimumab for microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer: the phase II checkMate 142 study. J. Clin. Oncol. 40, 161–170 (2022).
Cheng, Y. et al. Effect of first-line serplulimab vs placebo added to chemotherapy on survival in patients with extensive-stage small cell lung cancer: the ASTRUM-005 randomized clinical trial. JAMA 328, 1223–1232 (2022).
Lin, A. et al. CAMOIP: a web server for comprehensive analysis on multi-omics of immunotherapy in pan-cancer. Brief. Bioinform. 23, bbac129 (2022).
Chen, J., Lin, A. & Luo, P. Advancing pharmaceutical research: a comprehensive review of cutting-edge tools and technologies. Curr. Pharm. Anal. 21, 1–19 (2024).
Yi, R. et al. MHC-II signature correlates with anti-tumor immunity and predicts anti-PD-L1 response of bladder cancer. Front. Cell Dev. Biol. 10, 757137 (2022).
Lin, A. et al. TNF-alpha pathway alternation predicts survival of immune checkpoint inhibitors in non-small cell lung cancer. Front. Immunol. 12, 667875 (2021).
Doroshow, D. B. et al. PD-L1 as a biomarker of response to immune-checkpoint inhibitors. Nat. Rev. Clin. Oncol. 18, 345–362 (2021).
Dall’Olio, F. G. et al. Tumour burden and efficacy of immune-checkpoint inhibitors. Nat. Rev. Clin. Oncol. 19, 75–90 (2022).
Tricarico, P. et al. Total metabolic tumor volume on 18F-FDG PET/CT is a game-changer for patients with metastatic lung cancer treated with immunotherapy. J. Immunother. Cancer 12, e007628 (2024).
Shi, C. et al. The role of DNA damage repair (DDR) system in response to immune checkpoint inhibitor (ICI) therapy. J. Exp. Clin. Cancer Res. 41, 268 (2022).
Yi, R. et al. ATM mutations benefit bladder cancer patients treated with immune checkpoint inhibitors by acting on the tumor immune microenvironment. Front. Genet. 11, 933 (2020).
Li, G. et al. Breaking boundaries: Chronic diseases and the frontiers of immune microenvironments. Med Res. https://doi.org/10.1002/mdr2.70006 (2025).
Jardim, D. L., Goodman, A., Gagliato, D., de, M. & Kurzrock, R. The challenges of tumor mutational burden as an immunotherapy biomarker. Cancer Cell 39, 154–173 (2021).
Yap, T. A. et al. Development of immunotherapy combination strategies in cancer. Cancer Discov. 11, 1368–1397 (2021).
Zhang, J. et al. ZFHX3 mutation as a protective biomarker for immune checkpoint blockade in non-small cell lung cancer. Cancer Immunol. Immunother. 70, 137–151 (2021).
Song, P., Peng, Z. & Guo, X. Gut microbial metabolites in cancer therapy. Trends Endocrinol. Metabol. 36, 55–69 (2024).
Guillot, N. et al. Manipulating the gut and tumor microbiota for immune checkpoint inhibitor therapy: from dream to reality. Trends Mol. Med. 29, 897–911 (2023).
Liu, L. et al. Unveiling the power of gut microbiome in predicting neoadjuvant immunochemotherapy responses in esophageal squamous cell carcinoma. Research7, 0529 (2024).
Li, L. et al. Orally administrated hydrogel harnessing intratumoral microbiome and microbiota-related immune responses for potentiated colorectal cancer treatment. Research7, 0364 (2024).
Gao, Z. et al. Heterogeneity of intratumoral microbiota within the tumor microenvironment and relationship to tumor development. Med Res. https://doi.org/10.1002/mdr2.70007 (2025).
Vétizou, M. et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science 350, 1079–1084 (2015).
Sivan, A. et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science 350, 1084–1089 (2015).
Derosa, L. et al. Gut bacteria composition drives primary resistance to cancer immunotherapy in renal cell carcinoma patients. Eur. Urol. 78, 195–206 (2020).
Peng, Z. et al. The gut microbiome is associated with clinical response to Anti-PD-1/PD-L1 immunotherapy in gastrointestinal cancer. Cancer Immunol. Res. 8, 1251–1261 (2020).
Jin, Y. et al. The diversity of gut microbiome is associated with favorable responses to anti-programmed death 1 immunotherapy in Chinese patients with NSCLC. J. Thorac. Oncol. 14, 1378–1389 (2019).
Routy, B. et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science 359, 91–97 (2018).
Situ, Y. et al. The metabolic dialogue between intratumoural microbes and cancer: implications for immunotherapy. EBioMedicine 115, 105708 (2025).
Davar, D. & Zarour, H. M. Facts and hopes for gut microbiota interventions in cancer immunotherapy. Clin. Cancer Res. 28, 4370–4384 (2022).
Goc, J. & Sonnenberg, G. F. Harnessing microbiota to improve immunotherapy for gastrointestinal cancers. Cancer Immunol. Res. 10, 1292–1298 (2022).
Andrews, M. C. et al. Gut microbiota signatures are associated with toxicity to combined CTLA-4 and PD-1 blockade. Nat. Med. 27, 1432–1441 (2021).
Mustafayev, K. & Torres, H. Hepatitis B virus and hepatitis C virus reactivation in cancer patients receiving novel anticancer therapies. Clin. Microbiol. Infect. 28, 1321–1327 (2022).
Yibirin, M. et al. Immune checkpoint inhibitors suppress hepatitis C virus replication in infected patients with solid tumors. Am. J. Gastroenterol. 118, 1609–1617 (2023).
Du, Q., Yuan, J. & Ren, Z. Hepatocellular carcinoma patients with hepatitis B virus infection exhibited favorable survival from immune checkpoint inhibitors: a systematic review and meta-analysis. Liver Cancer 13, 344–354 (2024).
Zhong, L. et al. Hepatitis B virus infection does not affect the clinical outcome of anti-programmed death receptor-1 therapy in advanced solid malignancies: real-world evidence from a retrospective study using propensity score matching. Medicine100, e28113 (2021).
Ren, Z. et al. Sintilimab plus a bevacizumab biosimilar (IBI305) versus sorafenib in unresectable hepatocellular carcinoma (ORIENT-32): a randomised, open-label, phase 2-3 study. Lancet Oncol. 22, 977–990 (2021).
Yang, Y. et al. Camrelizumab versus placebo in combination with gemcitabine and cisplatin as first-line treatment for recurrent or metastatic nasopharyngeal carcinoma (CAPTAIN-1st): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 22, 1162–1174 (2021).
Sun, Y.-T. et al. PD-1 antibody camrelizumab for Epstein-Barr virus-positive metastatic gastric cancer: a single-arm, open-label, phase 2 trial. Am. J. Cancer Res. 11, 5006–5015 (2021).
Bai, Y. et al. Efficacy and predictive biomarkers of immunotherapy in Epstein-Barr virus-associated gastric cancer. J. Immunother. Cancer 10, e004080 (2022).
Zhang, X. et al. Association of hepatitis B virus infection status with outcomes of non-small cell lung cancer patients undergoing anti-PD-1/PD-L1 therapy. Transl. Lung Cancer Res. 10, 3191–3202 (2021).
Shi, Y. et al. Efficacy and safety of KL-A167 in previously treated recurrent or metastatic nasopharyngeal carcinoma: a multicenter, single-arm, phase 2 study. Lancet Reg. Health West Pac. 31, 100617 (2023).
He, W.-Z. et al. Response to programmed cell death protein 1 antibody in patients with Epstein-Barr virus-associated intrahepatic cholangiocarcinoma. Eur. J. Cancer 194, 113337 (2023).
Cheng, Y.-K. et al. Comparative safety, efficacy and survival outcome of anti-PD-1 immunotherapy in colorectal cancer patients with vs without hepatitis B virus infection: a multicenter cohort study. Clin. Transl. Gastroenterol. 13, e00475 (2022).
Himmelsbach, V. et al. Efficacy and safety of atezolizumab and bevacizumab in the real-world treatment of advanced hepatocellular carcinoma: experience from four tertiary centers. Cancers 14, 1722 (2022).
Yau, T. et al. Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 23, 77–90 (2022).
Yau, T. et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: the checkmate 040 randomized clinical trial. JAMA Oncol. 6, e204564 (2020).
Seiwert, T. Y. et al. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol. 17, 956–965 (2016).
Ramadoss, T. et al. Durability of response to immune checkpoint blockade following treatment discontinuation and efficacy of rechallenge in advanced Merkel cell carcinoma. J. Immunother. Cancer 12, e009816 (2024).
Lu, S. et al. An open label, safety study of Asian patients with advanced non-small-cell lung cancer receiving second-line nivolumab monotherapy (CheckMate 870). Ther. Adv. Med Oncol. 14, 17588359221138380 (2022).
Pan, S. et al. Correlation of HBV DNA and Hepatitis B surface antigen levels with tumor response, liver function and immunological indicators in liver cancer patients with hbv infection undergoing PD-1 inhibition combinational therapy. Front. Immunol. 13, 892618 (2022).
Lin, S. et al. Early change of plasma Epstein-Barr virus DNA load and the viral lytic genome level could positively predict clinical outcome in recurrent or metastatic nasopharyngeal carcinoma receiving anti-programmed cell death 1 monotherapy. BMC Cancer 24, 797 (2024).
Kelley, R. K. et al. Pembrolizumab (PEM) plus granulocyte macrophage colony stimulating factor (GM-CSF) in advanced biliary cancers (ABC): final outcomes of a phase 2 trial. JCO 40, 444–444 (2022). 4_suppl.
Tio, M. et al. Anti-PD-1/PD-L1 immunotherapy in patients with solid organ transplant, HIV or hepatitis B/C infection. Eur. J. Cancer 104, 137–144 (2018).
Mehra, R. et al. Efficacy and safety of pembrolizumab in recurrent/metastatic head and neck squamous cell carcinoma: pooled analyses after long-term follow-up in KEYNOTE-012. Br. J. Cancer 119, 153–159 (2018).
Ferris, R. L. et al. Nivolumab vs investigator’s choice in recurrent or metastatic squamous cell carcinoma of the head and neck: 2-year long-term survival update of CheckMate 141 with analyses by tumor PD-L1 expression. Oral. Oncol. 81, 45–51 (2018).
Siu, L. L. et al. Safety and efficacy of Durvalumab with or without tremelimumab in patients with PD-L1-low/negative recurrent or metastatic HNSCC: the phase 2 CONDOR randomized clinical trial. JAMA Oncol. 5, 195–203 (2019).
Abou-Alfa, G. K. et al. Tremelimumab plus Durvalumab in Unresectable Hepatocellular Carcinoma. NEJM Evid. 1, EVIDoa2100070 (2022).
Zhao, H. et al. Expression and prognostic significance of the PD-1/PD-L1 pathway in AIDS-related non-Hodgkin lymphoma. Cancer Med. 13, e7195 (2024).
Tsimafeyeu, I. et al. Nivolumab in patients with metastatic renal cell carcinoma and chronic hepatitis C virus infection. Cancer Immunol. Immunother. 69, 983–988 (2020).
Rojas, L. et al. Human papillomavirus infection and lung adenocarcinoma: special benefit is observed in patients treated with immune checkpoint inhibitors. ESMO Open 7, 100500 (2022).
Liu, H. et al. Comparison of effectiveness and safety of camrelizumab between HBV-related and non-B, non-C hepatocellular carcinoma: a retrospective study in China. Front. Genet. 13, 1000448 (2022).
Hanna, G. J. et al. Frameshift events predict anti-PD-1/L1 response in head and neck cancer. JCI Insight 3, e98811 (2018.
Chow, L. Q. M. et al. Antitumor activity of pembrolizumab in biomarker-unselected patients with recurrent and/or metastatic head and neck squamous cell carcinoma: results from the phase Ib KEYNOTE-012 expansion cohort. J. Clin. Oncol. 34, 3838–3845 (2016).
Bauml, J. et al. Pembrolizumab for platinum- and cetuximab-refractory head and neck cancer: results from a single-arm, phase II study. J. Clin. Oncol. 35, 1542–1549 (2017).
Yuan, G. et al. Interaction between hepatitis B virus infection and the efficacy of camrelizumab in combination with apatinib therapy in patients with hepatocellular carcinoma: a multicenter retrospective cohort study. Ann. Transl. Med. 9, 1412 (2021).
Xu, F. et al. Safety and efficacy of anti-PD-1 inhibitors in Chinese patients with advanced lung cancer and hepatitis B virus infection: a retrospective single-center study. Transl. Lung Cancer Res. 10, 1819–1828 (2021).
Zandberg, D. P. et al. Durvalumab for recurrent or metastatic head and neck squamous cell carcinoma: results from a single-arm, phase II study in patients with ≥25% tumour cell PD-L1 expression who have progressed on platinum-based chemotherapy. Eur. J. Cancer 107, 142–152 (2019).
Chiang, C. L. et al. Efficacy, safety, and correlative biomarkers of bintrafusp alfa in recurrent or metastatic nasopharyngeal cancer patients: a phase II clinical trial. Lancet Reg. Health West Pac. 40, 100898 (2023).
Chang, C. et al. The full management from first-line to third-line treatments in patients with Her-2-negative advanced gastric cancer. Front. Oncol. 12, 949941 (2022).
Chen, C. et al. Clinical outcomes and prognosis factors of Nivolumab plus chemotherapy or multitarget tyrosine kinase inhibitor in multi-line therapy for recurrent hepatitis B virus-related hepatocellular carcinoma: a retrospective analysis. Front. Oncol. 10, 1404 (2020).
Sangro, B. et al. A clinical trial of CTLA-4 blockade with tremelimumab in patients with hepatocellular carcinoma and chronic hepatitis C. J. Hepatol. 59, 81–88 (2013).
Pertejo-Fernandez, A. et al. Safety and efficacy of immune checkpoint inhibitors in patients with non-small cell lung cancer and hepatitis B or hepatitis C infection. Lung Cancer 145, 181–185 (2020).
Gopalakrishnan, V. et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 359, 97–103 (2018).
Grenda, A. et al. Presence of Akkermansiaceae in gut microbiome and immunotherapy effectiveness in patients with advanced non-small cell lung cancer. AMB Express 12, 86 (2022).
Zhu, C. et al. Characterizations of multi-kingdom gut microbiota in immune checkpoint inhibitor-treated hepatocellular carcinoma. J. Immunother. Cancer 12, e008686 (2024).
Zhu, C. et al. Gut microbiota and metabolites signatures of clinical response in anti-PD-1/PD-L1 based immunotherapy of biliary tract cancer. Biomark. Res. 12, 56 (2024).
Frankel, A. E. et al. Metagenomic Shotgun sequencing and unbiased metabolomic profiling identify specific human gut microbiota and metabolites associated with immune checkpoint therapy efficacy in melanoma patients. Neoplasia 19, 848–855 (2017).
Elkrief, A. et al. Intratumoral Escherichia is associated with improved survival to single-agent immune checkpoint inhibition in patients with advanced non-small-cell lung cancer. J. Clin. Oncol. 42, 3339–3349 (2024).
Dora, D. et al. Non-small cell lung cancer patients treated with Anti-PD1 immunotherapy show distinct microbial signatures and metabolic pathways according to progression-free survival and PD-L1 status. Oncoimmunology 12, 2204746 (2023).
Casadei, B. et al. Role of gut microbiome in the outcome of lymphoma patients treated with checkpoint inhibitors-The MicroLinf Study. Hematol. Oncol. 42, e3301 (2024).
Derosa, L. et al. Intestinal Akkermansia muciniphila predicts clinical response to PD-1 blockade in patients with advanced non-small-cell lung cancer. Nat. Med. 28, 315–324 (2022).
Zhao, H. et al. Bifidobacterium breve predicts the efficacy of anti-PD-1 immunotherapy combined with chemotherapy in Chinese NSCLC patients. Cancer Med. 12, 6325–6336 (2023).
Zhang, F. et al. Analysis of the gut microbiota: an emerging source of biomarkers for immune checkpoint blockade therapy in non-small cell lung cancer. Cancers13, 2514 (2021).
Yin, H. et al. The commensal consortium of the gut microbiome is associated with favorable responses to anti-programmed death protein 1 (PD-1) therapy in thoracic neoplasms. Cancer Biol. Med. 18, 1040–52 (2021).
Wang, F. et al. Regorafenib plus toripalimab in patients with metastatic colorectal cancer: a phase Ib/II clinical trial and gut microbiome analysis. Cell Rep. Med. 2, 100383 (2021).
Shoji, F. et al. Gut microbiota diversity and specific composition during immunotherapy in responders with non-small cell lung cancer. Front. Mol. Biosci. 9, 1040424 (2022).
Che, H. et al. Association of Helicobacter pylori infection with survival outcomes in advanced gastric cancer patients treated with immune checkpoint inhibitors. BMC Cancer 22, 904 (2022).
Takada, K. et al. Antibiotic-dependent effect of probiotics in patients with non-small cell lung cancer treated with PD-1 checkpoint blockade. Eur. J. Cancer 172, 199–208 (2022).
Sarkar, J. et al. Fluctuations in gut microbiome composition during immune checkpoint inhibitor therapy. World J. Oncol. 14, 178–187 (2023).
McCulloch, J. A. et al. Intestinal microbiota signatures of clinical response and immune-related adverse events in melanoma patients treated with anti-PD-1. Nat. Med. 28, 545–556 (2022).
Mao, J. et al. Gut microbiome is associated with the clinical response to anti-PD-1 based immunotherapy in hepatobiliary cancers. J. Immunother. Cancer 9, e003334 (2021).
Jingushi, K. et al. Circulating extracellular vesicles carrying Firmicutes reflective of the local immune status may predict clinical response to pembrolizumab in urothelial carcinoma patients. Cancer Immunol. Immunother. 71, 2999–3011 (2022).
Tonneau, M. et al. Helicobacter pylori serology is associated with worse overall survival in patients with melanoma treated with immune checkpoint inhibitors. Oncoimmunology 11, 2096535 (2022).
Jia, K. et al. Helicobacter pylori and immunotherapy for gastrointestinal cancer. Innovation5, 100561 (2024).
Zhang, M. et al. A gut microbiota rheostat forecasts responsiveness to PD-L1 and VEGF blockade in mesothelioma. Nat. Commun. 15, 7187 (2024).
Tomita, Y. et al. Clostridium butyricum therapy restores the decreased efficacy of immune checkpoint blockade in lung cancer patients receiving proton pump inhibitors. Oncoimmunology 11, 2081010 (2022).
Oster, P. et al. Helicobacter pylori infection has a detrimental impact on the efficacy of cancer immunotherapies. Gut 71, 457–466 (2022).
Magahis, P. T. et al. Impact of Helicobacter pylori infection status on outcomes among patients with advanced gastric cancer treated with immune checkpoint inhibitors. J. Immunother. Cancer 11, e007699 (2023).
Liu, N. et al. Eubacterium rectale improves the efficacy of Anti-PD1 immunotherapy in melanoma via l-Serine-Mediated NK cell activation. Research6, 0127 (2023).
Hakozaki, T. et al. The gut microbiome associates with immune checkpoint inhibition outcomes in patients with advanced non-small cell lung cancer. Cancer Immunol. Res.8, 1243–1250 (2020).
Chaput, N. et al. Baseline gut microbiota predicts clinical response and colitis in metastatic melanoma patients treated with ipilimumab. Ann. Oncol. 28, 1368–1379 (2017).
Katayama, Y. et al. The role of the gut microbiome on the efficacy of immune checkpoint inhibitors in Japanese responder patients with advanced non-small cell lung cancer. Transl. Lung Cancer Res. 8, 847–853 (2019).
Song, G. et al. Global immune characterization of HBV/HCV-related hepatocellular carcinoma identifies macrophage and T-cell subsets associated with disease progression. Cell Discov. 6, 90 (2020).
Liu, L. et al. HPVTIMER: a shiny web application for tumor immune estimation in human papillomavirus-associated cancers. iMeta 2, e130 (2023).
Cheng, Y. et al. Non-terminally exhausted tumor-resident memory HBV-specific T cell responses correlate with relapse-free survival in hepatocellular carcinoma. Immunity 54, 1825–1840.e7 (2021).
Guo, X. et al. Contrasting cytotoxic and regulatory T cell responses underlying distinct clinical outcomes to anti-PD-1 plus lenvatinib therapy in cancer. Cancer Cell 43, 248–268.e9 (2025).
Tosi, A. et al. The immune microenvironment of HPV-positive and HPV-negative oropharyngeal squamous cell carcinoma: a multiparametric quantitative and spatial analysis unveils a rationale to target treatment-naïve tumors with immune checkpoint inhibitors. J. Exp. Clin. Cancer Res. 41, 279 (2022).
Jenkins, B. H. et al. Single cell and spatial analysis of immune-hot and immune-cold tumours identifies fibroblast subtypes associated with distinct immunological niches and positive immunotherapy response. Mol. Cancer 24, 3 (2025).
Ho, W. J. et al. Viral status, immune microenvironment and immunological response to checkpoint inhibitors in hepatocellular carcinoma. J. Immunother. Cancer 8, e000394 (2020).
Li, X., Liu, X., Tian, L. & Chen, Y. Cytokine-mediated immunopathogenesis of Hepatitis B virus infections. Clin. Rev. Allergy Immunol. 50, 41–54 (2016).
McMiller, T. L. et al. Immune microenvironment of Epstein-Barr virus (EBV)-negative compared to EBV-associated gastric cancers: implications for immunotherapy. J. Immunother. Cancer 12, e010201 (2024).
Qiu, M.-Z. et al. Dynamic single-cell mapping unveils Epstein‒Barr virus-imprinted T-cell exhaustion and on-treatment response. Signal Transduct. Target Ther. 8, 370 (2023).
Wang, J. et al. EBV miRNAs BART11 and BART17-3p promote immune escape through the enhancer-mediated transcription of PD-L1. Nat. Commun. 13, 866 (2022).
Lee, C.-H. et al. Epstein-Barr Virus Zta-induced immunomodulators from nasopharyngeal carcinoma cells upregulate Interleukin-10 production from monocytes. J. Virol. 85, 7333–7342 (2011).
Cheng, W. Y., Wu, C.-Y. & Yu, J. The role of gut microbiota in cancer treatment: friend or foe?. Gut 69, 1867–1876 (2020).
Battaglia, T. W. et al. A pan-cancer analysis of the microbiome in metastatic cancer. Cell 187, 2324–2335.e19 (2024).
Zhang, T. et al. Intratumoral fusobacterium nucleatum recruits tumor-associated neutrophils to promote gastric cancer progression and immune evasion. Cancer Res. 85, 1819–1841 (2025).
Wu, H. et al. Intratumoral microbiota composition regulates chemoimmunotherapy response in esophageal squamous cell carcinoma. Cancer Res. 83, 3131–3144 (2023).
Mou, W. et al. Intratumoral mycobiome heterogeneity influences the tumor microenvironment and immunotherapy outcomes in renal cell carcinoma. Sci. Adv. 11, eadu1727 (2025).
Kim, T. S., da Silva, E., Coit, D. G. & Tang, L. H. Intratumoral immune response to gastric cancer varies by molecular and histologic subtype. Am. J. Surg. Pathol. 43, 851–860 (2019).
Zhang, K. et al. Heterologous prime-boost with an mRNA vaccine and an oncolytic virus enhances tumor regression through overcoming intratumoral immune suppression. Cell Rep. 44, 115745 (2025).
Li, D. et al. MicroEpitope: an atlas of immune epitopes derived from cancer microbiomes. Nucleic Acids Res. 53, D1435–D1442 (2024).
Lee, P.-C. et al. Gut microbiota and metabolites associate with outcomes of immune checkpoint inhibitor-treated unresectable hepatocellular carcinoma. J. Immunother. Cancer 10, e004779 (2022).
Pederzoli, F. et al. Stool microbiome signature associated with response to neoadjuvant pembrolizumab in patients with muscle-invasive bladder cancer. Eur. Urol. 85, 417–421 (2024).
Zhang, C. et al. Commensal microbiota contributes to predicting the response to immune checkpoint inhibitors in non-small-cell lung cancer patients. Cancer Sci. 112, 3005–3017 (2021).
Ahmed, L. A. & Al-Massri, K. F. Gut microbiota modulation for therapeutic management of various diseases: a new perspective using stem cell therapy. Curr. Mol. Pharm. 16, 43–59 (2023).
Dougherty, M. W. & Jobin, C. Intestinal bacteria and colorectal cancer: etiology and treatment. Gut Microbes. 15, 2185028 (2023).
Georgiou, K., Marinov, B., Farooqi, A. A. & Gazouli, M. Gut microbiota in lung cancer: where do we stand? Int. J. Mol. Sci. 22, 10429 (2021).
Temraz, S. et al. Hepatocellular carcinoma immunotherapy and the potential influence of gut microbiome. Int. J. Mol. Sci. 22, 7800 (2021).
Kawanabe-Matsuda, H. et al. Dietary lactobacillus-derived exopolysaccharide enhances immune-checkpoint blockade therapy. Cancer Discov. 12, 1336–1355 (2022).
Nami, Y., Hejazi, S., Geranmayeh, M. H., Shahgolzari, M. & Yari Khosroushahi, A. Probiotic immunonutrition impacts on colon cancer immunotherapy and prevention. Eur. J. Cancer Prev. 32, 30–47 (2023).
Baruch, E. N. et al. Fecal microbiota transplant promotes response in immunotherapy-refractory melanoma patients. Science 371, 602–609 (2021).
Davar, D. et al. Fecal microbiota transplant overcomes resistance to anti-PD-1 therapy in melanoma patients. Science 371, 595–602 (2021).
Lin, A. et al. From chaos to order: optimizing fecal microbiota transplantation for enhanced immune checkpoint inhibitors efficacy. Gut Microbes 17, 2452277 (2025).
Lin, A. et al. Microbiota boost immunotherapy? A meta-analysis dives into fecal microbiota transplantation and immune checkpoint inhibitors. BMC Med. 23, 341 (2025).
Tan, J. Immunotherapy Meets Microbiota. Cell 163, 1561 (2015).
Clemente, J. C., Ursell, L. K., Parfrey, L. W. & Knight, R. The impact of the gut microbiota on human health: an integrative view. Cell 148, 1258–1270 (2012).
Salgia, N. J. et al. Stool microbiome profiling of patients with metastatic renal cell carcinoma receiving anti-PD-1 immune checkpoint inhibitors. Eur. Urol. 78, 498–502 (2020).
Oey, O. et al. Gut microbiota diversity and composition in predicting immunotherapy response and immunotherapy-related colitis in melanoma patients: a systematic review. World J. Clin. Oncol. 13, 929–942 (2022).
Nie, F. et al. Effects of antibiotics on the anti-tumor efficacy of immune checkpoint inhibitor therapy. Clin. Transl. Oncol. https://doi.org/10.1007/s12094-024-03615-0. (2024).
Tinsley, N. et al. Cumulative antibiotic use significantly decreases efficacy of checkpoint inhibitors in patients with advanced cancer. Oncologist 25, 55–63 (2020).
Routy, B. et al. Gut microbiome influences efficacy of PD-1–based immunotherapy against epithelial tumors. Science 359, 91–97 (2018).
Glitza, I. C. et al. Randomized placebo-controlled, biomarker-stratified phase Ib microbiome modulation in melanoma: impact of antibiotic preconditioning on microbiome and immunity. Cancer Discov. 14, 1161–1175 (2024).
Wind, T. T. et al. Gut microbial species and metabolic pathways associated with response to treatment with immune checkpoint inhibitors in metastatic melanoma. Melanoma Res. 30, 235 (2020).
Liu, R. et al. Gut microbial structural variation associates with immune checkpoint inhibitor response. Nat. Commun. 14, 7421 (2023).
Derosa, L. et al. Custom scoring based on ecological topology of gut microbiota associated with cancer immunotherapy outcome. Cell 187, 3373–3389.e16 (2024).
Bharti, R. & Grimm, D. G. Current challenges and best-practice protocols for microbiome analysis. Brief. Bioinform. 22, 178–193 (2019).
Vogtmann, E. et al. Colorectal cancer and the human gut microbiome: Reproducibility with whole-genome shotgun sequencing. PLOS ONE 11, e0155362 (2016).
Biegert, G. et al. Diversity and composition of gut microbiome of cervical cancer patients: Do results of 16S rRNA sequencing and whole genome sequencing approaches align? J. Microbiol Methods 185, 106213 (2021).
Analysis of the microbiome: Advantages of whole genome shotgun versus 16S amplicon sequencing. Biochemical and Biophysical Research Communications.469, 967–977 (2016).
Yoo, S. et al. Risk of Hepatitis B virus reactivation in patients treated with immunotherapy for anti-cancer treatment. Clin. Gastroenterol. Hepatol. 20, 898–907 (2022).
Zhang, X. et al. Hepatitis B virus reactivation in cancer patients with positive Hepatitis B surface antigen undergoing PD-1 inhibition. J. Immunother. Cancer 7, 322 (2019).
Zeng, Y. et al. The occurrence of immune-related adverse events is an independent risk factor both for serum HBsAg increase and HBV reactivation in HBsAg-positive cancer patients receiving PD-1 inhibitor combinational therapy. Front Immunol. 15, 1330644 (2024).
Gut Microbiota May Mediate AEs. Cancer Discov. 11, 2118 (2021).
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (82172750); the Guangdong Provincial Medical Science and Technology Research Fund(B2023341).
Author information
Authors and Affiliations
Contributions
L.H. wrote the manuscript and prepared all the figures and tables. Y.L., C.Z. and A.J. corrected, collected and organized the related references and revised and finalized the manuscript. L.H., Y.L., C.Z., A.J., L.Z., W.M., A.J., K.L. J.Z. and X.C. researched data for the manuscript. A.L. and P.L. conceived the study content and provided constructive guidance. T.W. inception of study idea and supervision. C.C. and T.W. provided the funding acquisition.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, L., Li, Y., Zhang, C. et al. Microbiome meets immunotherapy: unlocking the hidden predictors of immune checkpoint inhibitors. npj Biofilms Microbiomes 11, 180 (2025). https://doi.org/10.1038/s41522-025-00819-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41522-025-00819-2