Abstract
This study was designed to determine the enrollment patterns in breast cancer clinical trials (CCTs) of patients with diverse backgrounds in an equal access setting and to evaluate the factors contributing to low rates of clinical trial accrual in patients of low socioeconomic status (SES). We performed a retrospective review of a prospectively maintained database of new patients seen at the Dan L. Duncan Comprehensive Cancer Center dating from 5/2015 to 9/2021, which included 3043 patients screened for breast CCTs. We compared the rate of CCT availability, eligibility, and enrollment between two patient populations: Smith Clinic, where most patients are of low SES and uninsured, and Baylor St. Luke’s Medical Center (BSLMC) with mostly predominantly insured, higher income patients. We performed logistic regression to evaluate whether differences in age, clinic, race, trial type, and primary language may be underlying the differences in CCT enrollment. More patients were eligible for CCTs at Smith Clinic (53.7% vs 44.7%, p < 0.001). However, Smith Clinic patients were more likely to decline CCT enrollment compared to BSLMC (61.3% declined vs 39.4%, p < 0.001). On multivariate analysis, Black patients had a significantly higher rate of CCT refusal overall (OR = 0.26, 95% CI 0.12–0.56, p < 0.001) and BSLMC only (OR = 0.20, 95% CI 0.060–0.60, p = 0.006). Our data shows that it is likely an oversimplification to assume that equal access will lead to the elimination of CCT disparities. Efforts to diversify CCTs must include consideration of structural and institutional inequities as well as social needs.
Similar content being viewed by others
Introduction
Black cancer patients in the United States have both increased overall cancer mortality and increased cancer-specific mortality1,2,3. In breast cancer, Black women have a 41% higher risk of dying from breast cancer when compared with White women and present on average at a later stage2,4,5. Structural inequities pertaining to access to care, diagnosis timing, and treatment delay affect Black women disproportionately6,7. While these are socioeconomic predictors of the observed poor outcomes, it is also well documented that Black women have a higher incidence of more aggressive breast cancer subtypes (i.e., triple negative breast cancer (TNBC)) than any other ethnic or racial groups8. It is critical to understand the biological basis of the observed poor outcomes of breast cancer among Black women. As we work to design precision-driven interventions for prevention, timely diagnosis, and treatment, achieving cancer health equity is not feasible without improving diversity in cancer clinical trials (CCTs).
In an ideal world, the populations studied in CCTs would be representative of the diversity of patients seen in clinic, and CCTs would be used as a tool to decrease inequity. Unfortunately, well-documented disparities exist within CCTs. The National Institutes of Health (NIH) Revitalization Act of 1993 aimed to increase the number of women and underrepresented racial groups in clinical research through mandated inclusion, yet numbers remain low9. In 2014, only approximately 1% of NCI-sponsored clinical trials were primarily focused on racial and ethnic minorities10. Studies have shown that the average enrollment of Black Americans in CCTs is at best between 5 and 7%, despite Black Americans making up more than 13% of the general population of the United States11,12,13.
When access to CCTs is not a barrier to enrollment, the rate of clinical trial participation by racial and ethnic minorities, especially those of low SES, has not been well studied. Data often comes from safety-net hospitals or private institutions, but rarely are both serving the same catchment area. The Dan L. Duncan Comprehensive Cancer Center (DLDCCC) in Houston, Texas provides access to breast CCTs at two clinical sites: Smith Clinic (SC), within the safety-net Harris Health System, and Baylor St. Luke’s Medical Center (BSLMC). We hypothesized that the racial and socioeconomic gap in clinical trial enrollment would be at least partially improved by similar access to breast CCTs at the two sites.
Results
Eligibility for CCTs
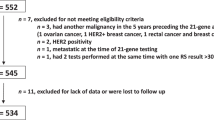
Of the 3043 patients screened for breast CCTs, 366 patients were found to be eligible for CCT, and some patients were eligible for multiple CCTs. There were 431 total offers to CCTs (Fig. 1).
The patient demographics of the 3043 new patients seen at the DLDCCC and screened for breast CCT eligibility from 5/2015 to 7/2021 are shown in Table 1. Notably, 50% of these patients were White at BSLMC in comparison to 11% at SC, and 74% listed English as their primary language at BSLMC versus 47% at SC. Patients at SC were on average younger, and more frequently presenting with TNBC compared to BSLMC.
More patients at SC had a trial available to them (752/1400, 53.7%) versus at BSLMC (734/1643, 44.7%, p-value < 0.001) (Table 1). Patients at SC were also more likely to be eligible for CCTs (191/1400, 13.6%) than patients at BSLMC (175/1643, 10.7%, p-value = 0.011).
Enrollment patterns in CCTs
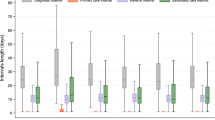
Despite higher eligibility, patients at SC were less likely to accept these CCT offers (74/191 accepted, 38.7%) than patients at BSLMC (106/175 accepted, 60.6%, p-value < 0.001) (Table 1). This difference in acceptance was significant on univariate but not multivariate analysis (Table 2). Age was not found to be significantly associated with trial enrollment.
Univariate analysis of the patients showed that Black patients, Hispanic/Latino patients, and Spanish speaking patients were significantly more likely to decline CCT participation. However, on overall multivariate analysis, only the Black patient category was associated with significantly higher rate of enrollment refusal (odds ratio (OR) = 0.26, 95% CI 0.12–0.56, p < 0.001). (Table 2) On the multivariate analyses across the two clinical sites, patients were significantly more likely to accept biobanking trials than other trial types at SC (OR = 16.90, 95% CI 2.13–363.77, p = 0.018) and at BSLMC (OR = 20.10, 95% CI 3.37–395.53, p-value = 0.007). Patients at SC were also more likely to enroll into preventive trials (OR = 7.88, 95% CI 1.53–59.39, p-value = 0.020). Primary language was not found to be a determining factor in trial enrollment or refusal at either site. Black patients at BSLMC were less likely to enroll in CCTs (OR = 0.20, 95% CI 0.060–0.60, p = 0.006) on multivariate analysis, however this was not significant on multivariate analysis in the SC subset (OR = 0.41, 95% CI 0.11–1.53, p = 0.180). (Supplemental Tables 1 and 2).
Discussion
While patients at SC have equal opportunity when it comes to access to clinical trials, trial enrollment is only at 37% in this clinic site, compared to BSLMC clinic where over 61% of trial eligible patients consent to enrollment. Overall, Black patients were less likely to consent to trial enrollment, and the rate of trial refusal was lowest for biobanking trials across both sites and preventive trials at SC compared to other trials. Speaking a primary language other than English was not found to be a major barrier to enrollment in our population.
Our data shows that it is likely an oversimplification to assume that equal access will lead to a complete elimination of CCT disparities. At SC, which serves a more diverse population with a higher percentage of low income and uninsured patients, the patients were significantly more eligible for breast CCTs. As noted in Table 1, patients at SC had a higher rate of TNBC (29.3% versus 14.3% at BSLMC), which we hypothesize may be one reason for the higher rate of eligibility. More SC patients were eligible for neoadjuvant trials and biobanking trials than at BSLMC (Fig. 1), possibly also due to the higher TNBC rates in this population.
Despite the higher rate of eligibility at SC, these patients were significantly more likely to decline the CCT. Our findings in a highly racially and ethnically diverse patient population supports the literature that shows that Black patients are less likely to agree to participate in clinical trials. The causes of discrepancy between eligibility and enrollment are multifactorial and complex. Studies have shown equal willingness among patients of different races to participate in clinical trials14,15,16,17, yet disparities in enrollment persist. In 2008, Ford18 identified three categories of reasons for low accrual: awareness, opportunity, and acceptance/refusal barriers or promoters.
Awareness barriers include lack of knowledge about the purpose and availability of CCTs13,19. Cancer health literacy has been found in some studies to be significantly lower in Black patients14,20,21, though others found that the role of factual knowledge did not make a significant difference in accrual22. The FDA in 2020 published guidelines and potential approaches to increase the diversity of clinical trial populations, including making diversity of enrollment a priority, involving the community, and educating potential participants23. When CCTs do not recruit a diverse patient population and fail to be made available to racial or ethnic minorities17, the results cannot be assumed to be generalizable to the community at large.
Opportunity barriers include limitations due to socioeconomic status and ineligibility. Research has shown us that CCT participants are less likely to be Black and more likely to be of a higher socioeconomic status24,25,26,27,28. Black patients are more likely to be deemed ineligible for clinical trials13,16,29. This is partially due to a higher rate of comorbidities such as hypertension, vision loss, or diabetes, as well as benign neutropenia—a condition that has not been shown to increase risk of infection16. However, studies have also shown that Black Americans are more likely to be deemed ineligible due to perceived noncompliance or mental status, and that subjective judgements on eligibility more often favor White patients29.
Barriers to acceptance include an understandable mistrust in a medical system that has historically caused harm to people of color, perceived financial burden, logistical difficulties including transportation, and family or cultural pressures. When Black American patients are asked about their reasons for opting out of CCT, studies show us that a lack of trust is one of the most common factors influencing their decision13,22. Barriers relating to logistics or finances are seen more often in safety-net hospitals and clinics19.
At BSLMC, where the population is less diverse, we noted a difference in CCT enrollment by race in multivariate analysis. However, this finding was not significant at SC, which has a more diverse population (Supplemental Tables 1 and 2). This is an interesting exploratory finding that can be further elucidated in future studies but may point to more diverse clinic experiences encouraging CCT enrollment. This could be due to higher trust in the clinic, awareness of clinical trials, or physicians offering trials more equitably. A limitation of our finding is the low number of patients in each category, and future studies would need to clarify these findings with a larger patient population.
Although it is imperative that we continue to shine a light on these important issues, we must be ready to envision and enact both local and national policy changes. Moving forward, we are focusing on community engagement, patient education, and dialogue with our patients to explore specific interventions designed to improve our Black patient population’s views of trial enrollment. Interventions have been attempted around the country to varying levels of success, including patient navigation systems30,31,32, patient education videos12,13, the recent ACCURE trial which included multiple levels of intervention including electronic medical record changes and specific physician roles33, diversifying staff, ensuring trial resources are in multiple languages, and offering financial incentives23. The reason for trial refusal was unfortunately not uniformly captured in the clinical trial database nor in patients’ electronic medical records. This is a limitation of our study; we do not have specific patients’ refusal reasons. In a follow up study that is currently being conducted, we have designed a patient education intervention to collect specific information on patients’ attitudes towards clinical trial enrollment and refusal. This follow-up study will serve as a roadmap for designing patient and community targeted outreach programs to improve our trial enrollment.
Cancer clinical trials have maintained restrictive eligibility criteria that inevitably censor out a large population of patients34. It is crucial that efforts continue on all fronts to improve cancer clinical trial diversity, including clinical trial design and challenging long-standing beliefs on eligibility criteria. Prevention and treatment alike need to be considered when designing an equitable future for cancer care, and as others have shown, these efforts must include consideration of structural and institutional inequities as well as social needs. Research and data collection are only the first steps in a necessary journey toward equity in cancer care.
Methods
Study population and data collection
This is a retrospective cohort study of new patients seen from 5/2015 to 9/2021, which included 3043 patients screened for breast CCTs at DLDCCC clinical sites. The populations receiving care at the two clinical sites differ greatly. At SC, half of the patients earn less than $25,000 annually, 60% are uninsured and use a county financial assistance program known as the “Gold Card,” and 65% are not proficient in English. Fifty-nine percent of SC patients self-identify as Hispanic and 29% self-identify as Black, with White patients making up 10% of the population. At BSLMC, over 95% of the patients have federal and commercial insurance and 68% are White, 13% are Black, and 3% are Hispanic. We collected information on age at the time of screening for CCTs, patient-reported race, and primary spoken language.
The study was conducted according to the ethical guidelines set forth in the Declaration of Helsinki and in concordance with the Heath Insurance Portability and Accountability Act. The study was approved by the institutional review board (IRB) of Baylor College of Medicine. The requirement of patient informed consent was waived by the IRB as the data was deidentified prior to analysis.
DLDCCC is an active participant in several cooperative group consortia including the Translational Breast Cancer Research Consortium (TBCRC), Southwest Oncology Group (SWOG), and NRG oncology (from the parental organizations of NSABP, RTOG, and GOG), and it is frequently the leading site for national investigator initiated clinical trials (IIT). We collected information on whether there were trials available for the patients’ diagnosis, trial eligibility, and the type of trial the patients were screened for. We designated 5 categories of trials based on the intent of the trial (e.g., scalp cooling trial to prevent chemotherapy-associated hair loss) and the stage of therapy that the trial was offered (e.g., COMPASS RD, an adjuvant trial). The categories were preventive, neoadjuvant, adjuvant, metastatic, and biobanking. The same CCTs were open at both sites under the DLDCCC.
Statistical analysis
We first performed Chi-square tests to determine whether there were differences in trial availability, trial eligibility, and trial acceptance rate according to DLDCCC clinical sites. We then performed univariate and multivariate logistic regression to evaluate whether differences in age, clinic site, race, trial type, and primary language may be underlying the observed differences in CCT enrollment rates. We performed logistic regression on the overall dataset as well as by clinic. We calculated odds ratios with 95% confidence intervals to measure the strength of association between the predictors and enrollment. P-values less than 0.05 were considered statistically significant. Analysis was performed using R version 4.1.0.
Data availability
The participants in this study did not give written consent for their data to be shared. Due to the clinical nature of the dataset, it is not available publicly.
References
Singh, G. K. & Jemal, A. Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950-2014: over six decades of changing patterns and widening inequalities. J. Environ. Public Health 2017, 2819372 (2017).
USCS Data Visualizations - CDC. https://gis.cdc.gov/cancer/USCS/#/AtAGlance/.
Reports on Cancer - Cancer Statistics. https://seer.cancer.gov/statistics/reports.html.
Siegel, R. L., Miller, K. D., Wagle, N. S. & Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 73, 17–48 (2023).
AACR Cancer Disparities Progress Report 2022 Cancer Progress Report. https://cancerprogressreport.aacr.org/disparities/.
Hossain, F. et al. Neighborhood social determinants of triple negative breast cancer. Front Public Health 7, 18 (2019).
Wang, F. et al. Racial/ethnic disparities in all-cause mortality among patients diagnosed with triple-negative breast cancer. Cancer Res. 81, 1163–1170 (2021).
Clarke, C. A. et al. Age-specific incidence of breast cancer subtypes: understanding the black-white crossover. J. Natl Cancer Inst. 104, 1094–1101 (2012).
Murthy, V. H., Krumholz, H. M. & Gross, C. P. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA 291, 2720–2726 (2004).
Chen, M. S., Lara, P. N., Dang, J. H. T., Paterniti, D. A. & Kelly, K. Twenty years post-NIH Revitalization Act: enhancing minority participation in clinical trials (EMPaCT): laying the groundwork for improving minority clinical trial accrual: renewing the case for enhancing minority participation in cancer clinical trials. Cancer 120, 1091–1096 (2014).
Al Hadidi, S., Mims, M., Miller-Chism, C. N. & Kamble, R. Participation of African American persons in clinical trials supporting U.S. food and drug administration approval of cancer drugs. Ann. Intern. Med. 173, 320–321 (2020).
Awidi, M. & Al Hadidi, S. Participation of black Americans in cancer clinical trials: current challenges and proposed solutions. JCO Oncol. Pr. 17, 265–271 (2021).
Swaby, J., Kaninjing, E. & Ogunsanya, M. African American participation in cancer clinical trials. Ecancermedicalscience 15, 1307 (2021).
Echeverri, M. et al. Cancer health literacy and willingness to participate in cancer research and donate bio-specimens. Int. J. Environ. Res. Public Health 15, 2091 (2018).
Byrne, M. M., Tannenbaum, S. L., Glück, S., Hurley, J. & Antoni, M. Participation in cancer clinical trials: why are patients not participating? Med Decis. Mak. 34, 116–126 (2014).
Langford, A. T. et al. Racial/ethnic differences in clinical trial enrollment, refusal rates, ineligibility, and reasons for decline among patients at sites in the National Cancer Institute’s Community Cancer Centers Program. Cancer 120, 877–884 (2014).
Wendler, D. et al. Are racial and ethnic minorities less willing to participate in health research? PLoS Med. 3, 0201–0210 (2006).
Ford, J. G. et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer 112, 228–242 (2008).
Hernandez, N. D. et al. African American cancer survivors’ perspectives on cancer Clinical trial participation in a safety-net hospital: considering the role of the social determinants of health. J. Cancer Educ. 37, 1589–1597 (2022).
Wong, S. T. et al. Using visual displays to communicate risk of cancer to women from diverse race/ethnic backgrounds. Patient Educ. Couns. 87, 327–335 (2012).
Watson, M. et al. Family history of breast cancer: what do women understand and recall about their genetic risk? J. Med. Genet. 35, 731–738 (1998).
Meng, J., McLaughlin, M., Pariera, K. & Murphy, S. A comparison between Caucasians and African Americans in willingness to participate in cancer clinical trials: the roles of knowledge, distrust, information sources, and religiosity. J. Health Commun. 21, 669–677 (2016).
Enhancing the Diversity of Clinical Trial Populations—Eligibility Criteria, Enrollment Practices, and Trial Designs Guidance for Industry | FDA. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enhancing-diversity-clinical-trial-populations-eligibility-criteria-enrollment-practices-and-trial.
El-Rayes, B. F. et al. Impact of race, age, and socioeconomic status on participation in pancreatic cancer clinical trials. Pancreas 39, 967–971 (2010).
Sharrocks, K., Spicer, J., Camidge, D. R. & Papa, S. The impact of socioeconomic status on access to cancer clinical trials. Br. J. Cancer 111, 1684–1687 (2014).
Kwiatkowski, K., Coe, K., Bailar, J. C. & Swanson, G. M. Inclusion of minorities and women in cancer clinical trials, a decade later: Have we improved? Cancer 119, 2956–2963 (2013).
Unger, J. M. et al. Patient income level and cancer clinical trial participation. J. Clin. Oncol. 31, 536–542 (2013).
Noor, A. M. et al. Effect of patient socioeconomic status on access to early-phase cancer trials. J. Clin. Oncol. 31, 224–230 (2013).
Penberthy, L. et al. Barriers to therapeutic clinical trials enrollment: differences between African-American and white cancer patients identified at the time of eligibility assessment. Clin. Trials 9, 788–797 (2012).
Battaglia, T. A. et al. Translating research into practice: Protocol for a community-engaged, stepped wedge randomized trial to reduce disparities in breast cancer treatment through a regional patient navigation collaborative. Contemp. Clin. Trials 93, 106007 (2020).
Cartmell, K. B. et al. Patient barriers to cancer clinical trial participation and navigator activities to assist. Adv. Cancer Res. 146, 139–166 (2020).
Fouad, M. N. et al. Patient Navigation As a Model to Increase Participation of African Americans in Cancer Clinical Trials. J. Oncol. Pr. 12, 556–563 (2016).
The Lancet Oncology. Racial disparities in cancer care: can we close the gap? Lancet Oncol. 22, 1643 (2021).
Liu, R. et al. Evaluating eligibility criteria of oncology trials using real-world data and AI. Nature 592, 629–633 (2021).
Acknowledgements
This work was not funded. This work has previously been presented in part in poster format at the San Antonio Breast Cancer Symposium in December 2021 and the ASCO QI symposium in October 2022, as well as in an online-only abstract at the 2022 ASCO meeting in June 2022. We would like to acknowledge and thank all the patients whose deidentified data was used in this study.
Author information
Authors and Affiliations
Contributions
E.P. performed data collection, data cleaning, data analysis, and wrote the manuscript. S.B. performed data analysis and reviewed the manuscript. K.S. performed data cleaning and reviewed the manuscript. K.O. performed data collection and reviewed the manuscript. M.E. performed data collection and reviewed the manuscript. M.K. performed data collection, data cleaning, study planning, IRB submission, data analysis, and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Podany, E.L., Bulsara, S., Sanchez, K. et al. Breast cancer clinical trial participation among diverse patients at a comprehensive cancer center. npj Breast Cancer 10, 70 (2024). https://doi.org/10.1038/s41523-024-00672-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41523-024-00672-0
This article is cited by
-
Bridging the gap: ctDNA, genomics, and equity in breast cancer care
npj Breast Cancer (2025)
-
Social Determinants of Health in Metastatic Breast Cancer Care: A Podcast Exploring Challenges and Opportunities in the United States and Canada
Oncology and Therapy (2025)