Abstract
ENHANCE-1 was a phase Ib/II study which evaluated eribulin plus pembrolizumab as a treatment for metastatic triple negative breast cancer (mTNBC). All patients had measurable disease and up to 2 prior systemic treatments. We identified 142 patients with available samples and evaluated associations between the pre-treatment tumor-immune microenvironment and response using diagnostic H&Es and multiplexed immunofluorescence with 2 antibody panels. Markers were chosen to evaluate lymphocytes and myeloid cells including: CD4, CD8, FoxP3, CD56, CD20, CD68, CD163, Vimentin, and HLA-DR. While H&E-assessed computational and manual assessments of stromal tumor infiltrating lymphocytes (sTILs) did not associate with response, multiplex immunofluorescence revealed several significant associations. These include enrichment of stromal CD56+ in non-responders and higher stromal CD4 + CD8+ in non-responders in breast samples. Responders exhibited higher stromal macrophage populations CD68 + , CD68+Vimentin + , CD68 + CD163+Vimentin+ as well as higher stromal HLA-DR + . Our results suggest that further studies on immune cell populations other than T-cells as predictive biomarkers for combination therapies in mTNBC are warranted.
Similar content being viewed by others
Introduction
Triple negative breast cancer (TNBC) is a highly aggressive subtype characterized by poor prognosis, early recurrence, and high mortality rates. While first-line (1 L) combination therapies for metastatic TNBC (mTNBC) have shown promise, effective second-line and later (2 L + ) treatment options remain limited, with a median overall survival (OS) of only 8 to 15 months for these patients, highlighting a significant unmet need for new therapeutic strategies to improve outcomes in later-line settings1. Eribulin mesylate, a microtubule inhibitor, has also shown promise in mTNBC treatment by improving OS in patients who have received multiple prior chemotherapy lines. The EMBRACE trial was a phase 3 trial in patients with heavily pretreated metastatic breast cancer, including mTNBC, which showed significantly increased overall survival (OS) at 13.1 months versus 10.6 months in patients treated with eribulin versus physician’s choice2, leading to the inclusion of eribulin into standard treatment guidelines for mTNBC. Subgroup analyses indicated that patients with HER2-negative and triple-negative disease experienced increased survival when treated with eribulin versus capecitabine, with an increase in median OS from 9.4 months to 14.4 months3.
Pembrolizumab combined with chemotherapy is the current standard of care in the first line treatment of mTNBC tumors expressing PD-L1 with CPS ≥ 10. The KEYNOTE-086 study, a phase II trial which evaluated pembrolizumab as a monotherapy in mTNBC patients reported an overall response rate (ORR) of 5% in pre-treated Cohort A, indicating modest efficacy in this subset of patients4. KEYNOTE-355, a phase 3 trial which randomized patients to either pembrolizumab in combination with chemotherapy or chemotherapy alone, showed that the addition of pembrolizumab improved median overall survival from 16.1 months to 23.0 months in patients with a PD-L1 combined positive score of at least 105. In the neoadjuvant setting, KEYNOTE-522 was a phase 3 trial which demonstrated that the addition of pembrolizumab to neoadjuvant chemotherapy significantly increased the pathologic complete response (pCR) from 51.2% to 64.8% in patients with early TNBC6. Additionally, there are ongoing studies evaluating antibody drug conjugates in combination with pembrolizumab, such as the ASCENT-04 study evaluating Trop2 targeted sacituzumab govitecan7,8. Given the individual efficacies of eribulin and pembrolizumab, the ENHANCE-1 trial was conducted as an open-label, single-arm, phase 1b/2 study which aimed to evaluate the safety and efficacy of eribulin plus pembrolizumab as 1–3 L treatment in patients with mTNBC. As ENHANCE-1 was conducted prior to treatment with pembrolizumab as standard of care in TNBC, none of the patients had received prior immunotherapy. Patients with PD-L1 positive tumors exhibited increased ORR (28.4% versus 17.3%)9.
Pembrolizumab is thought to reshape the tumor-immune microenvironment into an immune activated state, enhancing cytotoxic T cell function10, reducing immunosuppressive mechanisms11 and improving tumor antigen presentation12. Eribulin can complement this effect by modulating the tumor-immune microenvironment through vascular remodeling and cytokine profile modulation13, which can alter tumor-associated immune cell infiltration14. We explored potential biomarkers associated with response to pembrolizumab plus eribulin.
In 142 patients enrolled in the ENHANCE-1 trial with available tissue, we perform an exploratory analysis to characterize the tumor-immune microenvironment via assessment of stromal tumor-infiltrating lymphocytes (sTILs) and multiplexed immunofluorescence to search for biomarkers associated with response. The assessment of TILs in breast cancer has gained attention as a potential prognostic and predictive biomarker in breast cancer, with the presence of sTILs being associated with improved clinical outcomes in response to cytotoxic treatments and immunotherapies15. The International TILs Working Group has established guidelines for evaluating TILs in breast cancer using hematoxylin and eosin (H&E) stained sections16. These guidelines outline methods to quantify sTILs as a percentage, which has been shown to correlate with patient prognosis. High levels of sTILs are associated with better overall survival and disease-free survival, particularly in patients with TNBC17,18. We assessed associations of response with sTILs on digitized H&E stained tissue sections with manual assessment by trained pathologists and a deep learning approach known as MuTILs19.
While pathologist assessment of sTILs has shown clinical utility, more granular characterizations of lymphocytes can provide insight for developing next generation biomarkers20. While T cells have been extensively investigated in their role of tumor regulation21,22, innate and adaptive immune cells in the tumor-immune microenvironment can act in concert to regulate tumor growth23,24. Cell types other than T cells can present opportunities for novel therapeutic targeting11. For example, myeloid cells constitute a significant portion of the breast cancer TME25, though the prognostic role of macrophages remains controversial26,27. We characterized granular populations of lymphocytes and myeloid cells using multiplexed immunofluorescence (mIF), which allows us to assess multiple proteins simultaneously while maintaining spatial context. We employed two panels of mIF markers tailored for the breast cancer microenvironment including T-cells, B-cells, NK cells, macrophages, tumor, MHC Class-II and epithelial-mesenchymal transition (EMT). These panels provide a more in-depth view of the immune landscape and tumor biology which contribute to differential therapy response.
Results
ENHANCE-1 trial
ENHANCE-1 was a single arm phase Ib/II trial conducted from 2015 to 2021 which evaluated the efficacy and safety of eribulin and pembrolizumab in 167 patients with mTNBC across 18 sites in the United States (NCT02513472) (Fig. 1A). Patients received 0-2 prior lines in the metastatic setting and were enrolled either into stratum 1 (0 prior lines of therapy—66 patients) or stratum 2 (1-2 prior lines of therapy—101 patients). Patients in stratum 1 could have received prior therapy, including hormonal therapy or chemotherapy in either the adjuvant or neoadjuvant setting, prior to being diagnosed with metastatic disease. Evaluable tissue was available for 142 patients for our study including 58 in stratum 1 and 84 in stratum 2 (clinical characteristics are shown in Fig. 1B, Supplementary Table 1). The samples analyzed were archival FFPE tissues obtained via either core biopsy or a resection which could be from excisional biopsy, lumpectomy or mastectomy. Objective response rate (ORR) was defined as the percentage of patients with either complete response (CR) or partial response (PR) by RECIST 1.1. The ORR was 25.8% in stratum 1 and 22.5% in stratum 2 for the 142 patients analyzed. A summary of the clinical trial findings has been previously published9. Best overall response (BOR) was assessed via RECIST v1.1 with responders (n = 34, n = 15 in stratum 1, n = 19 in stratum 2) defined as patients with complete or partial radiographic responses and non-responders (n = 95, n = 39 in stratum 1, n = 56 in stratum 2) defined as those with stable disease or progressive disease. We excluded patients for which only lymph node tissue or pleural fluid was submitted, resulting in 130/142 samples. While all 130 samples in our study were acquired prior to enrollment in the trial, ENHANCE-1 did not require fresh tissue biopsies immediately prior to trial enrollment. Tissue samples correspond to archival FFPE material acquired prior to enrollment in ENHANCE-1 from a metastatic or primary site. As the tumor-immune microenvironment can be modulated by intervening treatments, we evaluate candidate biomarkers across all patients and in a subset of patients who have not been treated between the time of tissue acquisition and trial enrollment. We refer to these tissues as the TME-naive samples, as they are most representative of the pre-treatment tumor microenvironment. These criteria resulted in 43/142 patient samples in the TME-naive group: 31 from stratum 1 and 12 from stratum 2. PD-L1 combined positive score (CPS), a commonly assessed biomarker for pembrolizumab, was assessed for each patient and was not significantly associated with response across all available samples and in the TME-naive group.
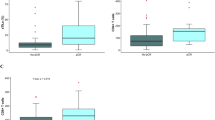
H&E evaluation of sTILs
We evaluated sTILs across H&Es drawn from all available samples with evaluable disease (n = 118/130) and the TME-naive group (n = 41/43). sTILs were evaluated with two methods (see Methods—Tumor infiltrating lymphocytes analysis): pathologist (HG) assessment and with MuTILs, a deep learning model (Fig. 2). In samples where TILs could be evaluated, pathologist-assessed sTILs were not significantly different across response groups when considering all available samples (n = 115/118), but were significant in the TME-naive group (n = 40/41) (Fig. 2A). Restricting to primary site tissue (n = 80/115) did not reveal associations to response in all available samples or in the TME-naive group (n = 18/40) (Fig. 2B). As MuTILs was only trained on breast tissue, we computationally assessed TILs in breast tissue samples from the primary site (n = 73/118), which was correlated to pathologist assessment but not associated with response (Fig. 2C). MuTILs was not significantly correlated to pathologist assessment in the TME-naïve subset restricted to breast tissue samples from the primary site (n = 15/41) and was also not associated with response (Fig. 2D).
Pathologist-assessed sTILs stratified by response across all samples and the TME-naive subset in (A) primary and metastatic sites and (B) the primary site. MuTILs computationally assessed sTILs in breast samples compared to pathologist assessed sTILs and stratified by response (C) and the TME-naive subset in breast samples (D).
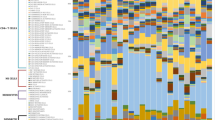
Multiplexed immunofluorescence immune populations
We evaluated lymphocyte and myeloid populations using multiplexed immunofluorescence using 2 panels (Supplementary Data 1). We identified all biologically possible combinations of markers and assessed corresponding intratumoral and stromal populations. We used Cox proportional hazards to model PFS using all samples and each immune population individually with the following covariates: number of treatments between tissue collection and enrollment in ENHANCE-1, stratum and site of tissue (primary versus metastatic). No populations were significantly associated with PFS. We then evaluated associations between immune populations and response (Fig. 3) across all samples and in the TME-naive group. As our study is exploratory and an arbitrary number of cellular phenotypes can be defined from marker combinations, we did not correct for multiple hypotheses. Across all available samples, there were no significant associations with either lymphocyte or myeloid populations and response. In the TME-naive group, we found several significant lymphocyte-related findings including: increased intratumoral CD4 + CD8+ in non-responders (p = 0.021) when only breast samples were considered (Fig. 3A) and increased stromal CD56 + , a marker associated with NK cells, in non-responders (p = 0.047) (Fig. 3B). We also identified significant findings among stromal myeloid cells (Fig. 3C), including increased CD68+ cells in responders (p = 0.009). CD68 + CD163-HLA-DR- and CD68 + CD163 + , which could represent M1 and M2 macrophage populations, were not significantly different across response groups (Supplementary Data 1). Sub-populations CD68 + CD163+Vimentin+ (p = 0.014) and CD68+Vimentin+ (p = 0.005) were increased in responders. Furthermore, we found increased stromal HLA-DR+ in responders (p = 0.039).
Discussion
In our study, only pathologist assessed sTILs in the TME-naive group associated with response. However, the TME-naive subset only consists of n = 43 samples and the association should be treated cautiously. While we found MuTILs to be correlated to pathologist assessed sTILs, the correlation has been shown to be imperfect19. The correlation could be affected by the subjective nature of TIL assessment and the heterogeneity of TIL spatial distributions which could affect accuracy. Additionally, the presence of necrotic debris and karyorrhectic debris, which can be visually similar to TILs, could be enhanced in our heavily pre-treated cohort. While studies have reported associations between sTILs in TNBC and efficacy of immune checkpoint inhibitors17,18,28, one study showed higher sTILs were associated with pCR overall cohort but did not predict the efficacy of PD-1/PD-L1 inhibitors29. The extent of disease (presence of nodal involvement or metastases) and treatment combinations may confound the association of sTILs with efficacy in immune checkpoint inhibitor treated patients with TNBC28.
Our study identified several more granular immune populations associated with response, including the enrichment of intratumoral CD4 + CD8+ and stromal CD56+ in non-responders. The CD4 + CD8+ population was visually assessed by a pathologist (DC) to confirm that these cells expressed both markers (Supplementary Fig. 1). CD4 + CD8+ double positive cells are a rarely studied population30 which has observed in breast cancer and associated pleural effusions31, melanoma32, Hodgkin lymphoma33 and urological cancers34 with conflicting roles and cytokine profiles that vary between cytotoxic and immunosuppressive capacities. For example, using flow cytometry, in patients with renal cell carcinoma, up to 50% of TILs were identified as CD4 + CD8+ with high PD-1 and TIM3 expression, suggesting a dysfunctional phenotype35. In melanoma patients, transcriptional analysis showed that CD4 + CD8+ TILs had consistent expression with CD8 + T-cells but also showed evidence of being poorly cytolytic, transiting towards features of CD4 + T-cells36. In our study, CD4 + CD8+ cells were enriched in non-responders, indicating a possible immunosuppressive effect which could be further elucidated with cytokine profiling. However, the presence of this population should be treated cautiously as limitations in spatial resolution can result in identifying CD4 + CD8+ cells which are tightly clustered CD4+ and CD8+ populations. In addition to CD4 + CD8 + , we found enrichment of stromal CD56 + , a marker of natural killer or NK-T cells, in non-responders, which has been previously associated with poor overall survival in TNBC as well as increased in comparison to non-TNBC37. In vivo animal studies have demonstrated that tumor-infiltrating NK cells exhibit impaired cytotoxic functions, dysfunctional states, and features consistent with exhaustion in the later stages of TNBC38. The dysfunction of these NK cells could be involved in breast cancer progression39. Our observed CD56+ enrichment may reflect a population with reduced functional capacity for cytotoxic activity against tumor cells.
We observed increased stromal HLA-DR expression in responders, which may reflect enhanced immune activation and T-cell recruitment, critical for anti-tumor immunity and response to therapy. One previous study using serial single RNA sequencing found that higher HLA-DR expression in macrophages was enriched in responders in mTNBC patients treated with nab-paclitaxel and pembrolizumab40. Other studies have suggested higher intraepithelial HLA-DR expression was associated with better responses to treatments combining PD-1/PD-L1 inhibitors with chemotherapy in patients with TNBC41,42.
Eribulin has been found to reverse EMT in TNBC cells in vivo and in vitro43. Eribulin has also been associated with EMT changes in patients with mTNBC, shifting tumors to a more epithelial phenotype44. Moreover, increased vascular remodeling and cell adherence induced by eribulin may increase infiltration of immune cells into tumors45. While we do not observe associations between response and tumor vimentin expression, we do observe enrichment of M2 macrophages expressing vimentin (CD68 + CD163+Vimentin + ) in responders and no difference in CD68 + CD163+Vimentin- across response groups. Future studies could evaluate the modulation of vimentin expression, which could be related to pro-inflammatory pathways or cell migration, on macrophages with pre and post paired samples46,47. Combining anti-PD-1 therapy, which primarily reactivates T cells but can influence macrophage polarization, may further enhance this reprogramming effect48,49. Our findings suggest that increased immune stimulatory cells may not necessarily associate with response. Instead, increased immunosuppressive cells, such as Vimentin expressing M2 macrophages, appear to be associated with response, which may be due to the overall suppressive tumor-immune microenvironment in patients with mTNBC and the functional state of immune cells in this context.
Our findings suggest associations between the pre-treatment tumor-immune microenvironment in mTNBC and response to eribulin plus pembrolizumab. However, our study has several limitations. Most importantly, given that the tumor-immune microenvironment is influenced by therapy, and our objective was to characterize the relationship between representative pre-treatment tissue and response to eribulin plus pembrolizumab, our analysis was constrained by the limited number of tissue samples available that had not undergone treatment between tissue collection and trial enrollment. As a result of the limited number of samples and large number of comparisons possible with multiplexed immunofluorescence analysis, our findings were not corrected for multiple hypotheses, raising the possibility of type I error. While not obtaining tissue prior to trial enrollment was a pragmatic decision, our ability to characterize pre-treatment tissue was limited. Another limitation originates from heterogeneity in the tumor-immune microenvironment from treatment prior to tissue collection, as most of the patients were not treatment-naive. The lack of tissue samples post-treatment limited our ability to assess treatment induced immune modulation. Lastly, as the trial was single-armed, there were no comparison arms to assess eribulin-induced changes in the tumor-immune microenvironment over pembrolizumab alone.
Despite these limitations, our results suggest a role for macrophages as a novel biomarker, which is not included in established estimates of sTILs, in patients with mTNBC treated with eribulin plus pembrolizumab.
Methods
Tumor infiltrating lymphocyte analysis
Manual pathologist assessment of stromal and intratumoral TILs was performed according to the International Immuno-Oncology Biomarker Working Group on Breast Cancer16. MuTILs, a deep learning approach, was used to simultaneously classify tissue regions and segment individual cell nuclei to assess sTILs19.
Multiplex immunofluorescence staining and analysis
Patient samples were stained using 2 panels of antibodies (Supplementary Fig. 2, Supplementary Table 2). Panel 1: CD56 (Cell Marque, Cat# 156R-95; 1:200), Granzyme B (Leica, Cat# NCL-L-GRANB; 1:40), PanCK (Biolegend, Cat# 914201; 1:160), CD4 (Abcam, Cat# ab133616; 1:500), CD8 (Leica, Cat# PA0183; 1:2), FoxP3 (Abcam, Cat# ab20034; 1:200); Panel 2: CD68 (Biogenex, Cat# AM416-5M; 1), Vimentin (Leica, Cat# PA0640; 1:2), CD163 (Leica, Cat# CD163-L-CE; 1:125), HLA-DR (Abcam, Cat# ab20181; 1:6000), PanCK, and CD20 (Leica, Cat# NCL-L-CD20-L26; 1:4) with the Opal 7-Color Automation IHC Kit (Akoya Biosciences) on a Leica Bond RX automated stainer (Leica Biosystems). FFPE tissue sections (4 μm) were baked for 2 h at 60 °C, followed by automatic deparaffinization, rehydration, and The Heat Induced Epitope Retrieval (HIER) in BOND Epitope Retrieval Solution 2, pH 9 (Leica Biosystems) for 30 min at 95 °C. Primary antibodies against each marker were diluted using Akoya 1× Antibody Diluent Block (Akoya, Cat# ARD1001EA) sequentially applied, with optimized dilutions and orders (Supplementary Table 2) for 30 min per marker at room temperature. Signal amplification was achieved using tyramide signal amplification (TSA) reagents performed in six cycles. In each cycle, the tissue was incubated sequentially with a primary antibody for 30 min at room temperature, the secondary antibody conjugated to polymeric horseradish peroxidase (HRP), an Opal fluorophore in TSA buffer, and BOND Epitope Retrieval Solution 1, pH 6 (Leica Biosystems) for 20 min at 95 °C to strip the tissue-bound primary–secondary antibody complexes before the next staining cycle. After nuclear counterstaining with DAPI, slides were coverslipped with Vectashield HardSet Antifade mounting medium (Vector Laboratories). Whole slide scans (WSS) were captured at 10× magnification using the Vectra Polaris automated multispectral microscope (Akoya/PerkinElmer) with Vectra Polaris 1.0.13 software. Regions of interest were chosen for multispectral imaging (MSI) at 20× magnification using the Phenochart 1.1.0 software (Akoya). Spectral unmixing and image exportation were performed using the InForm v2.5.1 software (Akoya).
Images were analyzed using HALO AI software (Indica Labs). Whole-slide scans (WSS) were first preprocessed for image alignment and quality assurance to ensure accurate segmentation of tissue regions and fluorescence channels. Tissue segmentation was performed by selecting regions of interest (ROIs) based on morphological features and fluorescence intensity patterns. Tissue classification and single-cell analysis were conducted using the integrated AI-driven tissue classifier (DenseNet V2) and cell phenotyping modules (HighPlex FL v4.0.4) to identify and quantify cells expressing specific markers, including CD56, Granzyme B, CD4, CD8, FoxP3, CD68, Vimentin, CD163, HLA-DR, and CD20. The pathologist’s annotations on H&E-stained slides served as a reference for confirming ROI selection and cell phenotype. Fluorescence intensities were adjusted and normalized across slides to reduce inter-sample variability. The data output included marker co-expression profiles, cell density maps, and spatial distributions of immune and tumor cell populations for further statistical analysis.
Statistical analysis
Mann-Whitney statistical tests were used to compare responders and non-responders in the analysis of sTILs and multiplex immunofluorescence derived populations. Correlation between computational and pathologist sTILs was performed with Spearman’s rank correlation test.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to the confidential nature of the clinical data, but are available from the corresponding author in patient ID-redacted form upon reasonable request.
Code availability
The code used for the data analysis presented in this manuscript utilizes publicly available software packages with no customization.
References
Li, C. H. et al. Current treatment landscape for patients with locally recurrent inoperable or metastatic triple-negative breast cancer: a systematic literature review. Breast Cancer Res. 21, 143 (2019).
Cortes, J. et al. Eribulin monotherapy versus treatment of physician’s choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomised study. Lancet 377, 914–923 (2011).
Twelves, C. et al. Subgroup analyses from a phase 3, open-label, randomized study of eribulin mesylate versus capecitabine in pretreated patients with advanced or metastatic breast cancer. Breast Cancer (Auckl.) 10, 77–84 (2016).
Adams, S. et al. Pembrolizumab monotherapy for previously treated metastatic triple-negative breast cancer: cohort A of the phase II KEYNOTE-086 study. Ann. Oncol. 30, 397–404 (2019).
Cortes, J. et al. Pembrolizumab plus chemotherapy in advanced triple-negative breast cancer. N. Engl. J. Med. 387, 217–226 (2022).
Schmid, P. et al. Pembrolizumab for early triple-negative breast cancer. N. Engl. J. Med. 382, 810–821 (2020).
Bardia, A. et al. Sacituzumab Govitecan in metastatic triple-negative breast cancer. N. Engl. J. Med. 384, 1529–1541 (2021).
Tolaney, S. M. et al. 276TiP ASCENT-04/KEYNOTE-D19: Phase III study of sacituzumab govitecan (SG) plus pembrolizumab (pembro) vs treatment of physician’s choice (TPC) plus pembro in first-line (1L) programmed death-ligand 1-positive (PD-L1+) metastatic triple-negative breast cancer (mTNBC). Ann. Oncol. 33, S664–S665 (2022).
Tolaney, S. M. et al. Eribulin plus pembrolizumab in patients with metastatic triple-negative breast cancer (ENHANCE 1): a Phase Ib/II study. Clin. Cancer Res. 27, 3061–3068 (2021).
Wei, S. C., Duffy, C. R. & Allison, J. P. Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov. 8, 1069–1086 (2018).
Sanmamed, M. F. & Chen, L. A paradigm shift in cancer immunotherapy: from enhancement to normalization. Cell 175, 313–326 (2018).
Gong, J. et al. Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: a comprehensive review of registration trials and future considerations. J. Immunother. Cancer 6, 8 (2018).
Garrone, O. et al. Exploratory analysis of circulating cytokines in patients with metastatic breast cancer treated with eribulin: the TRANSERI-GONO (Gruppo Oncologico del Nord Ovest) study. ESMO Open, 5. (2020).
Shimizu, T. et al. Eribulin promotes proliferation of CD8+ T cells and potentiates T cell-mediated anti-tumor activity against triple-negative breast cancer cells. Breast Cancer Res. Treat. 203, 57–71 (2024).
El Bairi, K. et al. The tale of TILs in breast cancer: a report from The International Immuno-Oncology Biomarker Working Group. NPJ Breast Cancer 7, 150 (2021).
Salgado, R. et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann. Oncol. 26, 259–271 (2015).
Adams, S. et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J. Clin. Oncol. 32, 2959–2966 (2014).
Leon-Ferre, R. A. et al. Tumor-infiltrating lymphocytes in triple-negative breast cancer. JAMA 331, 1135–1144 (2024).
Liu, S. et al. A panoptic segmentation dataset and deep-learning approach for explainable scoring of tumor-infiltrating lymphocytes. NPJ Breast Cancer 10, 52 (2024).
Andreou, C., Weissleder, R. & Kircher, M. F. Multiplexed imaging in oncology. Nat. Biomed. Eng. 6, 527–540 (2022).
Gao, G. et al. Prognostic value of tumor-infiltrating lymphocytes in patients with triple-negative breast cancer: a systematic review and meta-analysis. BMC Cancer 20, 179 (2020).
Huertas-Caro, C. A. et al. Tumor infiltrating lymphocytes (TILs) are a prognosis biomarker in Colombian patients with triple negative breast cancer. Sci. Rep. 13, 21324 (2023).
Mathias, C. et al. PD-1/PD-L1 inhibitors response in triple-negative breast cancer: can long noncoding RNAs be associated?. Cancers 15, 4682 (2023).
Zheng, H. et al. Tumor microenvironment: key players in triple negative breast cancer immunomodulation. Cancers 13, 3357 (2021).
Ruffell, B. & Coussens, L. M. Macrophages and therapeutic resistance in cancer. Cancer Cell 27, 462–472 (2015).
Omilian, A. R. et al. CD163+ macrophages in the triple-negative breast tumor microenvironment are associated with improved survival in the Women’s circle of health study and the Women’s circle of health follow-up study. Breast Cancer Res. 26, 75 (2024).
Stavrou, M. & Constantinidou, A. Tumor associated macrophages in breast cancer progression: implications and clinical relevance. Front. Immunol. 15, 1441820 (2024).
Tan, Q. et al. Potential predictive and prognostic value of biomarkers related to immune checkpoint inhibitor therapy of triple-negative breast cancer. Front. Oncol. 12, 779786 (2022).
Loibl, S. et al. A randomised phase II study investigating durvalumab in addition to an anthracycline taxane-based neoadjuvant therapy in early triple-negative breast cancer: clinical results and biomarker analysis of GeparNuevo study. Ann. Oncol. 30, 1279–1288 (2019).
Overgaard, N. H. et al. CD4+/CD8+ double-positive T cells: more than just a developmental stage?. J. Leukoc. Biol. 97, 31–38 (2015).
Desfrancois, J. et al. Increased frequency of nonconventional double positive CD4CD8 alphabeta T cells in human breast pleural effusions. Int J. Cancer 125, 374–380 (2009).
Desfrancois, J. et al. Double positive CD4CD8 alphabeta T cells: a new tumor-reactive population in human melanomas. PLoS ONE 5, e8437 (2010).
Rahemtullah, A. et al. A double-positive CD4+CD8+ T-cell population is commonly found in nodular lymphocyte predominant Hodgkin lymphoma. Am. J. Clin. Pathol. 126, 805–814 (2006).
Bohner, P. et al. Double positive CD4(+)CD8(+) T cells are enriched in urological cancers and favor T helper-2 polarization. Front Immunol. 10, 622 (2019).
Menard, L. C. et al. Renal cell carcinoma (RCC) tumors display large expansion of double positive (DP) CD4+CD8+ T cells with expression of exhaustion markers. Front Immunol. 9, 2728 (2018).
Parrot, T. et al. Transcriptomic features of tumour-infiltrating CD4(low)CD8(high) double positive alphabeta T cells in melanoma. Sci. Rep. 10, 5900 (2020).
Thacker, G. et al. Immature natural killer cells promote progression of triple-negative breast cancer. Sci. Transl. Med. 15, eabl4414 (2023).
Liu, X. et al. NK and NKT cells have distinct properties and functions in cancer. Oncogene 40, 4521–4537 (2021).
Mamessier, E. et al. Human breast cancer cells enhance self tolerance by promoting evasion from NK cell antitumor immunity. J. Clin. Invest. 121, 3609–3622 (2011).
Deng, J. et al. Serial single-cell profiling analysis of metastatic TNBC during Nab-paclitaxel and pembrolizumab treatment. Breast Cancer Res. Treat. 185, 85–94 (2021).
Carter, J. M. et al. Distinct spatial immune microlandscapes are independently associated with outcomes in triple-negative breast cancer. Nat. Commun. 14, 2215 (2023).
Gonzalez-Ericsson, P. I. et al. Tumor-specific major histocompatibility-II expression predicts benefit to anti–PD-1/L1 therapy in patients with HER2-negative primary breast cancer. Clin. Cancer Res. 27, 5299–5306 (2021).
Yoshida, T. et al. Eribulin mesilate suppresses experimental metastasis of breast cancer cells by reversing phenotype from epithelial-mesenchymal transition (EMT) to mesenchymal-epithelial transition (MET) states. Br. J. Cancer 110, 1497–1505 (2014).
Hayashi, T. et al. Effect of eribulin on epithelial-mesenchymal transition plasticity in metastatic breast cancer: an exploratory, prospective study. Genes Cells 28, 364–373 (2023).
Niwa, Y. et al. Liposome-encapsulated eribulin shows enhanced antitumor activity over eribulin for combination therapy with anti-PD-1 antibody. Mol. Cancer Ther. 22, 499–510 (2023).
Mor-Vaknin, N. et al. Vimentin is secreted by activated macrophages. Nat. Cell Biol. 5, 59–63 (2003).
Thalla, D. G. et al. Extracellular vimentin is expressed at the rear of activated macrophage-like cells: potential role in enhancement of migration and phagocytosis. Front Cell Dev. Biol. 10, 891281 (2022).
Zhang, H. et al. Roles of tumor-associated macrophages in anti-PD-1/PD-L1 immunotherapy for solid cancers. Mol. Cancer 22, 58 (2023).
Bullock, K. K. & Richmond, A. Beyond Anti-PD-1/PD-L1: improving immune checkpoint inhibitor responses in triple-negative breast cancer. Cancers 16, 2189 (2024).
Acknowledgements
This study was supported financially by Eisai. The study was also supported by the Molecular Pathology Shared Resource, Digital and Computational Pathology Laboratory and the Human Immune Monitoring Core at Columbia University Irving Medical Center.
Author information
Authors and Affiliations
Contributions
Y.H.F., Q.W., H.L., H.G., D.C., R.V. and E.C. analyzed data, generated the figures and contributed to the manuscript text. Q.W. generated and analyzed the multiplexed imaging data. M.K., K.K., R.V. and E.C. reviewed and annotated clinical data. H.G., D.C., M.G.P., C.F.C. reviewed pathology material. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Foong, Y.H., Wang, Q., Kearney, M. et al. Spatial biomarkers of response to eribulin plus pembrolizumab in patients with metastatic triple negative breast cancer in the ENHANCE-1 trial. npj Breast Cancer 11, 72 (2025). https://doi.org/10.1038/s41523-025-00791-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41523-025-00791-2