Abstract
Electrodes underpin electrophysiological signals recording, requiring stable skin contact and low impedance for high-quality, long-term acquisition. Dry microneedle electrodes penetrate the stratum corneum and bypass hair to ensure robust contact, but conventional rigid designs lack tissue conformity, risking discomfort and injury. This work introduces a modulus-adjustable, mechanically adaptive dry microneedle electrode (MDME) constructed from PEDOT: PSS and shape memory polymer. Submillimeter MDME penetrates skin barriers and, upon body temperature activation, softens to match tissue mechanics, minimizing invasiveness. The MDME exhibits low, stable interface impedance and enables high-quality electromyography, electrocardiography, electroencephalography, and electrocorticography recordings. After one month of usage, the electrophysiological root mean square noise increased by only 6 μV, compared to 63 μV of Ag/AgCl gel electrodes. Electroencephalogram signal-to-noise reached 8.12 dB versus 7.26 dB for the cranial screw electrodes. This work represents a notable advancement in MDME-based electrophysiological recording, expanding its potential applications in personalized healthcare and human-machine interaction.
Similar content being viewed by others
Introduction
Electrophysiological (EP) signals are electrical signals generated by the body’s physiological activity1,2, including the electrical activity of muscles (electromyogram, EMG)3, heart (electrocardiogram, ECG)4, and brain (electroencephalogram, EEG)5. Recording and analyzing EP signals are increasingly crucial in enhancing human-machine collaboration across diverse applications, including motor rehabilitation6, disorder diagnosis7, disease treatment8, and intelligent interaction systems9,10. For example, EMG signals can be decoded to control robotic prosthetics or exoskeletons for individuals with motor impairments, ECG monitoring enables the detection of cardiovascular abnormalities such as arrhythmias and atrial fibrillation, and EEG signals are used in brain-computer interfaces for intention recognition and cognitive monitoring11,12. The successful acquisition of high-quality EP signals critically depends on the performance of the EP electrodes, which serve as the primary interface between biological tissues and electronic systems13,14. EP electrodes are primarily categorized as wet or dry, and low-impedance electrodes are essential for effective EP detection and signal transmission. Wet electrodes, utilizing conductive gels or pastes, are widely used in clinical and research settings to maintain low electrode-skin impedance15. However, their performance deteriorates over time due to gel dehydration, leading to increased impedance and reduced signal-to-noise ratio (SNR) and root mean square (RMS) values during prolonged use16. Dry electrodes were developed to address the limitations of long-term EP acquisition17. Unfortunately, they often suffer from higher electrode-skin impedance caused by barriers such as the stratum corneum, hair, and grease, resulting in impedance mismatch18. This mismatch diminishes common-mode rejection and SNR, complicating high-quality, long-term EP signal recording19,20.
Dry microneedle electrodes present a promising minimally invasive alternative for EP recording. These electrodes establish direct electrical contact with the epidermis by penetrating the stratum corneum and circumventing the hair barrier, achieving lower interface impedance and improved signal quality21,22. This approach eliminates the need for skin abrasion, shaving, or conductive gels to ensure consistent electrode-skin contact, minimizing motion artifacts and susceptibility to environmental noise23. However, conventional microneedle electrodes, typically fabricated from high-modulus metals, exhibit significant limitations. Their inherent rigidity prevents them from conforming to soft tissue’s complex and dynamic topography24,25. This mechanical mismatch can induce localized stress concentrations, increasing the risk of pain, inflammation, and even infection, especially in vulnerable populations such as neonates and elderly individuals with fragile skin26. While flexible dry microneedle electrodes, comprising a high-modulus metal layer deposited onto a flexible polymer substrate, represent an improvement, they still suffer from inherent drawbacks27. The stark contrast in Young’s modulus between the rigid metal and the compliant polymer complicates the fabrication process, potentially leading to delamination, cracking, and diminished mechanical integrity under repeated deformation28. Furthermore, the relatively rigid metal component continues to exert localized pressure on the underlying tissue29. Exploring organic conductive films, such as PEDOT: PSS or graphene-based materials, offers a compelling alternative for realizing fully flexible microneedle electrodes30,31. However, achieving sufficient mechanical strength for consistent stratum corneum penetration remains a significant challenge32,33. While high-aspect-ratio microneedle designs can partially address this issue, the fundamental mismatch between the mechanical properties of even flexible conductive films and those of biological tissues persists34. Even with optimized designs, prolonged use of these electrodes may still induce subtle tissue damage, inflammation, or discomfort due to sustained mechanical stress35,36.
This work presents a flexible and mechanically adaptive dry microneedle electrode (MDME) composed of a modulus-adjustable shape memory polymer (SMP) microneedle substrate and a doped-PEDOT: PSS conductive film. The submillimeter (~ 800 μm) MDME effectively penetrates skin barriers to directly contact the epidermis, exhibiting lower electrode-skin impedance than commercial Ag/AgCl gel electrodes. Triggered by body temperature, the MDME’s modulus decreases to match that of soft tissue, ensuring seamless attachment to irregular tissue surfaces while minimizing invasiveness. Upon temperature activation (~ 60 °C), the microneedle array restores its original shape, ensuring reusability. The flexible, biocompatible, and recoverable MDME demonstrates an RMS noise of 37 μV, lower than Ag/AgCl (40 μV). After one month of use, the RMS noise increased by only 6 μV, compared to a 63 μV increase in Ag/AgCl electrodes, demonstrating its superior capability in EMG, ECG, and EEG acquisition. Additionally, the high quality and spatial resolution of the MDME were validated in electrocorticogram (ECoG) recordings, where it achieved a higher SNR (8.12 dB) than the cranial screw electrodes (7.26 dB), allowing precise detection of steady-state visually evoked potentials (SSVEPs) at frequencies of 8 Hz, 13 Hz, and 40 Hz. This work represents a significant advancement in MDME-based EP recording, offering promising applications in personalized health management, rehabilitation training, and human-machine interaction.
Results
Design and characterization of the MDME
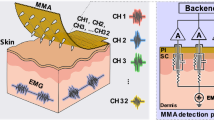
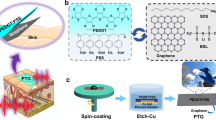
The MDME-based EP recording system was designed according to the diagram illustrated in Fig. 1a. The MDME comprises a modulus-adjustable SMP microneedle substrate coupled with a doped-PEDOT: PSS conductive film. The microneedle array was fabricated using a 40 mm × 40 mm inverse mold, enabling the creation of precisely defined microneedle structures. A key feature of the MDME is the ability to tune the Young’s modulus of the SMP substrate. This was achieved by manipulating the compound ratio of the epoxy monomer E44 (molecular weight ~ 450 g/mol) and the curing agent polyether amine D230 (molecular weight ~ 230 g/mol). Alternatively, the substrate could be immersed in anhydrous ethanol to adjust the mechanical properties. These methods provide a versatile means to tailor the MDME’s stiffness to match the target tissue. The PEDOT: PSS film, functioning as the conductive layer for EP signal acquisition, was deposited onto the microneedle substrate via spin-coating. To enhance the electrical performance and uniformity of the PEDOT: PSS film, high-boiling-point dimethyl sulfoxide (DMSO) and low-boiling-point isopropanol (IPA) were sequentially introduced into the PEDOT: PSS solution37. This approach effectively mitigated the “coffee ring effect”, which negatively impacts thin films’ morphology and electrical properties38. Additionally, Tween-20 and (3-glycidoxypropyl) trimethoxysilane were incorporated as surfactant and crosslinking agents to reduce surface tension and enhance the adhesion of the PEDOT: PSS film to the SMP microneedles. Detailed fabrication steps for the MDME are provided in Figure S1. Furthermore, to evaluate batch‐to‐batch reproducibility, we measured the impedance at 500 Hz for four MDME formulations across three independent manufacturing batches (Figure S2). The results demonstrated minimal variability between batches, indicating consistent manufacturing quality. The overall dimensions of an MDME were approximately 40 × 40 × 1 mm3 (L × W × T). The adjustable modulus and optimized microneedle geometry enhance mechanical adaptability and minimize constraints during EP recording. As a result, optimized MDMEs can be comfortably applied to irregular and even hairy surfaces, such as the skin over a fully flexed elbow joint (Fig. 1b). Leveraging these unique properties, the MDME demonstrates superior capabilities for non-invasive EEG and high-resolution ECoG recording, alongside conventional EMG and ECG acquisition. Fig. 1c shows the experimental setup for EEG recording, where the MDME is mounted on a standard EEG cap. This allows for convenient, gel-free EEG recording, improving patient comfort and reducing preparation time. Fig. 1d depicts the low-invasive ECoG recording setup, where the arrayed MDME is surgically implanted in a rat, enhancing the spatiotemporal resolution while maintaining high-precision SNR.
a The MDME consists of a modulus-adjustable SMP microneedle substrate and a doped-PEDOT: PSS conductive film. b Optical images showing a prepared MDME attached to an elbow joint (left) and with good deformability (right). c Experimental setup for MDME-based EEG recording. d MDME-based ECoG recording in a rat model. e Microscope image showing uniform distribution of microneedle arrays. f The height profile along the top line of the microneedles, demonstrates good height uniformity. g Working principle of conductive microneedle structures for EP acquisition. h H&E and Masson’s staining of normal rat skin and skin after 7 days of wearing the MDME.
The precise geometry and uniformity of the microneedle structures fabricated on the SMP substrate were meticulously characterized using scanning electron microscopy (SEM) and super-depth-of-field microscopy. Representative top-view and side-view images, presented in Fig. 1e, Figure S3, and Figure S4, reveal a highly consistent microneedle array with well-defined features. The microneedles feature a uniform square base (400 × 400 μm²) with sharp, pointed tips spaced 400 μm apart. A quantitative analysis of the microneedle geometry was performed using cross-sectional height profiling. The measured height profile, obtained along a scanning line across the microneedle array, demonstrates a consistent microneedle height of approximately 800 μm, with only minimal variation (± 50 μm) (Fig. 1f). Furthermore, the side-bottom surface angle of approximately 70° further confirms the uniformity and sharpness of the microneedle structure, which is designed to facilitate smooth and minimally invasive skin penetration, contributing to the overall performance and user comfort of the MDME. Human skin thickness exhibits considerable variability, influenced by anatomical location, age, gender, and individual differences. This results in a typical skin thickness range of 0.5–4.0 mm39. To confirm microneedle penetration, we conducted experiments on chicken and pig skin (Fig. S5). Under applied pressure, the microneedles effectively penetrate the skin’s outer barriers (stratum corneum, hair, and grease), establishing a reliable conductive pathway and significantly reducing impedance at the MDME-skin interface (Fig. 1g). Simultaneously, body temperature triggers the deformation of the microneedles, which assists in the penetration process and ensures stable and consistent contact, while minimizing invasiveness and reducing the potential for discomfort. Upon reaching ~ 60 °C, the deformed microneedles return to their original shape, with negligible degradation in performance even after 500 times of use. Long-term biocompatibility studies were conducted to confirm the safety of MDME. Fig. 1h presents histological examinations from Hematoxylin-eosin (H&E) and Masson’s trichrome staining of rat skin after seven days of continuous MDME application, demonstrating that the epidermal structure remains intact, with well-arranged cells and no signs of pathological changes. These findings reveal that the MDME is non-cytotoxic and biocompatible, supporting its potential for safe and prolonged use in EP recording applications.
Modulus adjustment and electrical characteristics of the MDME
The MDME comprises a microneedle substrate fabricated from an SMP with tunable mechanical properties and a conductive thin film of doped-PEDOT: PSS conductive film. To optimize the SMP’s Young’s modulus for effective skin penetration and conformability, we investigated two distinct methods: varying the compound ratios of the SMP constituents and controlled immersion in anhydrous ethanol (Fig. 2a). Under both processing approaches, the temperature-dependent behavior of the SMP’s modulus was systematically characterized and evaluated to determine optimal performance at physiological temperature (37 °C) (Fig. 2b and c). Initially, the compound ratio of the epoxy monomer E44 to the curing agent polyether amine D230 was designed to be 1:1, 1:1.1, 1:1.2, and 1:1.3. Notably, the tensile Young’s modulus at body temperature (37 °C) exhibited a clear trend of decreasing tensile Young’s modulus with increasing D230 content, measuring 88.2 MPa, 61.6 MPa, 10.9 MPa, and 1.98 MPa for the 1:1, 1:1.1, 1:1.2, and 1:1.3 ratios, respectively (Fig. 2b). This tunability allows for precise control over the mechanical behavior of the SMP substrate. Subsequently, we explored the impact of anhydrous ethanol immersion on the SMP’s mechanical properties. Specifically, we investigated the effect of varying immersion times and temperatures on the elastic modulus of SMP films with a compound ratio of 1:1. Consistent with the compound ratio experiments, Young’s modulus exhibited a monotonic decrease with increasing immersion time. At 37 °C, the tensile Young’s modulus values were 32.76 MPa, 27.62 MPa, 22.14 MPa, 12.7 MPa, and 1.49 MPa for immersion durations of 5, 10, 15, 20, and 40 h, respectively (Fig. 2c). This indicates that ethanol immersion effectively plasticizes the SMP film. Furthermore, the SMP exhibits excellent shape memory capabilities. The deformed SMP structure can be reliably recovered to its original shape through a simple heating process, enabling potential reusability. This characteristic was verified through both microscopic and macroscopic demonstrations (Figure S6). Specifically, SMP samples cast into the shape of the ‘UESTC’ logo and long strips were successfully deformed and subsequently restored to their original configuration upon heating (Figure S7), demonstrating the material’s robust shape memory effect. Video S1 demonstrates the shape memory process of the ‘UESTC’ logo.
a Two ways of regulating the Young’s modulus of the SMP: compound ratios and anhydrous ethanol immersion. b Distribution of the effect of different components and temperature on the elastic modulus of MDME. c Distribution of the effect of different treatment times and temperatures on the elastic modulus of MDME. d Impedance spectra of commercial Ag/AgCl gel electrode, Cu electrode, and MDME on skin. e The corresponding impedances are at 1, 10, 100, and 1000 Hz. f Variations of the resistance of MDME with the strains. g Resistance variation of MDME in repeated stretching-releasing cycles. h Resistance variation of MDME in the 400th-430th stretching-releasing cycles. i Variations of the resistance of different components MDME in repeated stretching-releasing cycles.
To fabricate the MDMEs, a layer of PEDOT: PSS conductive thin film was spin-coated onto SMP microneedle substrates with the four different compound ratios (1:1, 1:1.1, 1:1.2, and 1:1.3). We employed commercially available Ag/AgCl gel electrodes and copper film electrodes as compared electrodes to evaluate the performance of the MDME in EP recordings. The impedance of the electrode is inversely proportional to the effective electrochemical surface area (Fig. S8). Therefore, we used samples of the same size(1 cm2) to conduct test electrode-skin impedance measurements within the frequency range of 1–105 Hz, as depicted in Fig. 2d. All impedance spectra exhibited smooth curves, monotonically decreasing with increasing frequency, as expected for a capacitive interface. Notably, the MDME incorporating the 1:1.3 SMP substrate demonstrated the lowest interfacial impedance across the entire frequency range. Quantitative impedance values extracted from Fig. 2d, specifically at 1, 10, 100, and 1000 Hz, are presented in Fig. 2e. The corresponding impedance values for the 1:1.3 MDME were (97.7, 42.9, 10.4, 1.7 kΩ cm2), significantly lower than those observed for the 1:1 MDME (376, 138, 36, 7.19 kΩ cm2), 1:1.1 MDME (345, 123, 29.7, 6.26 kΩ cm2), 1:1.2 MDME (271, 102, 28, 5.73 kΩ cm2), Ag/AgCl gel (1130, 393, 67, 8.62 kΩ cm2), and copper film (203, 97.7, 26.3, 5.03 kΩ cm2). The substantially lower impedance values achieved by the MDMEs can be attributed to the microneedles effectively penetrating the stratum corneum, creating additional conductive pathways, and establishing more direct electrical contact with the underlying epidermis (Fig. S9). Furthermore, the 1:1.3 MDME benefits from its enhanced mechanical adaptation to the skin surface at body temperature, facilitating seamless and continuous attachment and achieving optimal impedance performance (Fig. S10). To assess the MDME’s robustness under physiological conditions, we evaluated its electrical stability under strain. We investigated the resistance changes of MDMEs composed of PEDOT: PSS conductive film and four types of SMP substrates during tensile loading through fracture. Fig. S11 shows the stress-strain curves. Within the elastic deformation region, the resistance changes for all samples remained below 15%, indicating acceptable stability under typical operating conditions(Fig. 2f). During cyclic stretching and release testing, Resistance variations remained below 12.5% even after 500 cycles (Fig. 2g and h). Under the 10% strain regime, the 1:1.3 sample demonstrated the smallest resistance change after 1000 stretch-release cycles, indicating superior performance compared to the other tested ratios, and these changes remained below 20% (Fig. 2i). Considering the reported range of elastic modulus for human skin (0.5–1.95 MPa) (Fig. S12) and the need for long-term stability, the SMP with a 1:1.3 compound ratio or a 40-h ethanol immersion treatment was selected as the optimal substrate for further MDME integration and in vivo EP recording.
ECG and EMG recording using MDME
To verify the EP recording capabilities of the MDME, we systematically evaluated signal acquisition during ECG and EMG measurements. The ECG signal originates from fluctuations in the surface potential of cardiomyocytes, which are triggered by the depolarization and repolarization events within the heart’s ventricles, atria, and pacemaker cells. For EMG and ECG measurements, the MDME was connected to the external recording system via low-loss transmission lines. The MDME surface is uniformly coated with PEDOT: PSS by spin‑coating, covering the entire microneedle array from tip to base. During SMP synthesis, the MDME is securely bonded to a low‑loss transmission line via edge through‑holes, providing electrical interconnection with the PEDOT: PSS film and enabling interfacing with a commercial amplifier. To assess mechanical stability, we suspended weights of 20, 50, 100, and 200 g from the wiring and measured MDME’s impedance. The results exhibited minimal impedance variation, indicating robust mechanical and electrical stability under load (Fig. S13). A three-electrode configuration was employed for ECG acquisition. Two MDMEs were positioned on the volar (inner) aspect of the left and right forearms to serve as active (recording) electrodes, while a third MDME was placed on the ankle as a ground electrode (Fig. 3a). Figure 3b presents a comparative analysis of ECG signals acquired using the MDMEs and conventional Ag/AgCl gel electrodes. Both electrode types successfully captured high-quality ECG signals, exhibiting peak voltages of approximately 1.3 mV. An enlarged view of a representative ECG waveform (green dashed box, Fig. 3c) reveals distinct characteristic peaks (P, Q, R, S, and T), demonstrating the MDME’s ability to capture diagnostically relevant information. RMS analysis was further conducted to quantify signal fluctuation and baseline noise over time.
a Schematic illustration of the ECG detection. b ECG signals were recorded from MDME and Ag/AgCl gel electrodes. c Corresponding ECG characteristic peaks of P, Q, R, S, and T. d The RMS noises were recorded by Ag/AgCl gel electrodes and MDME during ECG recording over the 30-day observation period. e The spectrogram of the ECG pulse was recorded using the MDME. f The spectrogram of the ECG pulse was recorded using the Ag/AgCl gel electrodes. g Schematic illustration of the EMG detection. h Comparison of EMG signals using MDME, and Ag/AgCl gel electrodes. i The SNR for the signal detected by MDME and Ag/AgCl gel electrodes. j The spectrogram of the EMG pulse was recorded using the MDME. k EMG signals were generated by the flexion or extension of different fingers. l EMG signal potential was generated by the five fingers.
The RMS noise level for the MDME was approximately 37 μV, lower than that of the Ag/AgCl gel electrodes (40 μV) (Figs. 3d and S14). Notably, the RMS noise of the MDME increased by only 6 μV after one month, remaining within the margin of error. In contrast, the RMS noise of the Ag/AgCl electrodes increased by 63 μV over the same period, likely due to drying of the gel and degradation of the electrode-skin interface. These results highlight the enhanced long-term stability of the MDME compared to conventional gel electrodes. Furthermore, frequency spectrum analysis of the ECG signals within the 0–1000 Hz range was performed using Fourier transformation (Fig. 3e and f). The signal power associated with the PQRST complex, spanning the 50–250 dB range, was distinguishable in the spectrum obtained with the MDME, exhibiting superior signal clarity compared to the Ag/AgCl gel electrodes. These results indicated that the MDME could act as a comparable alternative for ECG recording, promising for long-term ECG monitoring.
EMG is an essential technique for evaluating neuromuscular activity, reflecting the electrical activity generated by the excitation and contraction of muscle fibers at the body surface. The experimental setup for EMG recording using MDMEs is illustrated in Fig. 3g. Two MDMEs were positioned on the volar aspect of the forearm, separated by a distance of 5 cm, to function as the active and reference electrodes. A third MDME was placed on the elbow as a ground electrode to minimize the influence of movement artifacts during muscle activity. Upon clenching the fist, resulting in contraction of the wrist flexor muscles, a distinct muscle electrical signal was immediately observed, which returned to baseline upon relaxation of the hand (Fig. 3h). The EMG signals recorded by the MDME were comparable in amplitude and morphology to those recorded by commercial Ag/AgCl gel electrodes. During repeated clenching and relaxation of the fist, the EMG signal baseline remained remarkably stable, which we attribute to the stable electrode-skin interface contact facilitated by the microneedle microstructure and the adhesive properties of the SMP substrate. Quantification of the EMG signal quality via SNR analysis revealed that the MDME exhibited a higher SNR than the Ag/AgCl gel electrode (Fig. 3i). The SNRs obtained using the MDMEs and Ag/AgCl gel electrodes were 35.7 and 27, respectively, indicating a superior signal quality with the MDME. Moreover, the frequency spectrum of the muscle electrical signals within the 0–400 Hz range, obtained via Fourier transformation (Fig. 3j), demonstrated higher amplitudes in the 100–250 Hz band, a frequency range associated with muscle fiber action potentials. Additionally, MDMEs can detect EMG signals generated by individual fingers’ bending, as shown in Fig. 3k and l. By differentiating the amplitude variations of low-amplitude muscle electrical signals produced by different finger flexion or extension movements, the movement of each finger could be distinguished. In summary, through a comparative evaluation against Ag/AgCl gel electrodes in ECG and EMG applications, the MDME demonstrates superior recording performance in electrophysiological measurements.
EEG and ECoG recording using MDME
EEG signals, which reflect the brain’s electrical activity, are typically measured in the microvolt (μV) range. Compared to ECG and EMG, EEG signals are significantly weaker, rendering their measurement more challenging and susceptible to noise contamination. Furthermore, the presence of hair on the scalp can introduce significant impedance, obstructing traditional dry electrodes and substantially degrading signal quality. To address these limitations and further validate the effectiveness of the MDME in EEG recording, we developed a portable MDME-based EEG system (Fig. 4a). This system comprises a wearable EEG cap equipped with MDMEs and a battery-powered signal processing unit. Real-time EEG data is wirelessly aggregated and transmitted to a laptop via Wi-Fi, enabling continuous and remote EEG monitoring. The MDME-based EEG cap was displayed in Fig. 4b. with two MDMEs placed at the O1 and O2 sites on the occipital lobe, and another two MDMEs were placed on the forehead and behind the ear, serving as reference electrodes40. Adhering to the International 10–20 system for electrode placement (Fig. 4c), the MDME-based EEG cap was applied to the hairy scalp of volunteers within a quiet, controlled environment for eye-state triggered EEG acquisition. The biopotential difference between (O1, O2) and the reference electrode BIAS represents the EEG signals, and the biopotential difference between electrode EYE and the reference electrode BIAS represents the eye movement signals. GND is the Ground electrode that sits above the earlobe. With open- and closed-eye state transitions, the alpha wave could be effectively triggered. At the same time, closing the eyes will cause the eye movement signal to drop significantly (Fig. 4d). A Fourier transformation of the alpha wave and the eye movement extracted from Fig. 4d is presented in Fig. 4e. This analysis revealed a prominent spectral peak in the frequency range of 8–13 Hz within the EEG signal, consistent with the presence of alpha waves41. Video S2 demonstrates the alpha wave and eye movement recording using MDME. This indicates that the dominant component of the EEG signal during the closed-eye state was the alpha rhythm, which is typically associated with relaxed wakefulness and internal cognitive processing. To further evaluate the performance benefits of MDME electrodes, we also assessed the performance of traditional Ag/AgCl gel electrodes on hairy skin (Fig. 4f and g). The Ag/AgCl gel electrodes exhibited lower signal quality characterized by higher noise levels, baseline drift, and inconsistent contact. These results revealed that the microneedle structures in MDME electrodes play a crucial role in penetrating hair, establishing a more stable and low-impedance contact with the scalp.
a Schematic diagram of portable EEG acquisition system. b Photograph depicting the assembly of the MDME device onto an EEG cap. c Schematic diagram of MDME placement d Time domain waveforms of EOG and EEG signals recorded by MDME. e Frequency domain waveforms of eye movement and alpha wave recorded by MDME. f Time domain waveforms of eye movement and alpha wave signals recorded by Ag/AgCl gel electrodes. g Frequency domain waveforms of EOG and EEG signals recorded by Ag/AgCl gel electrodes. h EOG during open and close eyes. i EEG during wake and rest states.
The MDME-based EEG cap was further utilized to acquire EEG signals during awake and restful states. Figure 4h shows the eye movement signal recorded during alternating periods of open and closed eyes. A series of eight eye blinks was used as a clear marker to delineate the transitions between these two distinct brain states, as illustrated in Fig. 4i. During the awake state, the EEG signals acquired via the MDME system exhibited high-frequency, low-amplitude electrical activity, a pattern characteristic of an alert and actively processing brain. Conversely, during the restful state, the EEG signals from the MDME displayed a low-frequency, high-amplitude electrical activity pattern. The recorded EEG signals were notably free of artifacts and exhibited optimal stability, suggesting the MDME provided robust and reliable signal acquisition. These attributes facilitate the efficient collection of high-quality bioelectrical signals while significantly enhancing user comfort and signal fidelity, both of which are paramount for continuous long-term monitoring and accurate interpretation of underlying physiological states.
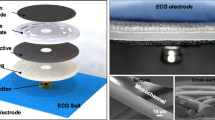
ECoG recording is a widely adopted and minimally invasive technique for diagnosing brain diseases, owing to its superior spatial resolution and SNR compared to EEG. Building upon the promising data collection capabilities observed in EEG recordings, we developed an ECoG recording system for a rat model (Fig. 5a). This system comprised a stereotactic instrument positioned within a darkened room and a set of precisely controlled flashing lights. To optimize signal acquisition from the rat brain, a matching sandwich-structured MDME (4.5 × 4.5 mm2) was meticulously designed. Specifically, four symmetrically distributed microneedle regions were pre-fabricated on an SMP substrate. An Au/polyimide (Au/PI) film was transferred onto a polydimethylsiloxane (PDMS) substrate, establishing electrical interconnections with the four microneedle regions (Fig. 5b). Detailed fabrication procedures and characterization data for the sandwich-structured MDME electrode are presented in Fig. S15. To monitor ECoG signals in vivo, the MDME electrode was carefully positioned to conform to the dura mater overlying the primary visual cortex of the left hemisphere of a rat brain42. As a control, four cranial screw electrodes, each with a diameter of 500 µm, were implanted into the symmetric visual cortex regions of the right hemisphere. The modulus-adjustable and mechanically adaptive properties of the MDME allowed it to achieve a low-invasive, conformal attachment to the cerebral cortex surface, minimizing tissue disruption (Fig. 5c). ECoG signals acquired using both the MDME and the cranial screw electrodes were compared (Fig. 5d). The Pearson correlation coefficient between the signals obtained from the two electrode types reached an impressive 0.9, indicating strong signal coherence. Moreover, the average SNRs were 8.12 and 7.26 dB for the MDME and the cranial screw electrodes, respectively (Figs. 5e, S16), demonstrating the superior signal quality achieved with the MDME. Local Field Potentials (LFPs), reflecting the synchronous activity of neuronal populations, are crucial indicators for probing brain activity in neuroscience research. The MDME can potentially record thousands of LFPs within brain tissue simultaneously (Fig. S17), providing rich data on the dynamic changes occurring within neural networks.
a Schematic diagram of MDME and rat experimental setup. b Diagram of MDME structure. c The surgical operation and SSVEP experimental setup of MDME and the cranial screw electrodes. d The representative ECoG signals were recorded by the MDME and the cranial screw electrodes. e The SNR of ECoG signals was recorded by the MDME and the cranial screw electrodes. f The power spectrum of 8 Hz SSVEP. g The power spectrum of 13 Hz SSVEP. h The power spectrum of 40 Hz SSVEP.
Further investigation involved a SSVEP experiment designed to collect and analyze the sustained responses elicited in the visual cortex by fixed-frequency visual stimuli (Fig. S18). Video S3 shows the SSVEP experiment. We employed three distinct visual stimulation frequencies (8, 13, and 40 Hz) as the primary experimental conditions. These frequencies represent commonly used paradigms in SSVEP research, as detailed in Supplementary Table 1. Power spectral analysis of the recorded signals revealed prominent spectral components at the stimulation frequencies of 8 Hz (Fig. 5f), 13 Hz (Fig. 5g), and 40 Hz (Fig. 5h) in the ECoG power spectrum. Notably, the ECoG power spectrum exhibited peaks at the fundamental stimulation frequencies and their corresponding harmonic frequencies, such as 16 Hz, 24 Hz, and 32 Hz for the 8 Hz stimulus, and 26 Hz and 39 Hz for the 13 Hz stimulus. These SSVEP experimental results provide compelling evidence that the MDME is highly effective in capturing SSVEPs, which has significant implications for the subsequent development of brain-computer interface technologies and human-machine interaction systems.
Discussion
This work introduces a modulus-adjustable, mechanically adaptive dry microneedle electrode that addresses the limitations of conventional rigid electrodes. The submillimeter-scale MDME (~ 800 μm) effectively penetrated the stratum corneum and bypassed hair, ensuring direct epidermal contact and achieving an electrode-skin impedance of 1.2 kΩ at 10 Hz—significantly lower than that of commercial Ag/AgCl gel electrodes (2.5 kΩ). Upon body temperature activation (~ 37 °C), the SMP substrate’s modulus decreased to 1.98 MPa, matching soft tissue stiffness and improving long-term comfort and biocompatibility. EP recordings demonstrated stable performance across various modalities. For ECG signals, the MDME maintained a low RMS noise of 37 μV, with only a 6 μV increase after one month of continuous use, whereas Ag/AgCl electrodes showed a 63 μV increase under identical conditions. For EMG signals, the MDME demonstrated a higher SNR of 35.7 dB, compared to 8 dB obtained using the Ag/AgCl gel electrodes. For EEG signals, the MDME achieved an SNR of 8.12 dB, outperforming cranial screw electrodes (7.26 dB), and accurately captured SSVEPs at 8, 13, and 40 Hz. Additionally, ECoG recordings revealed high spatial resolution and signal fidelity, supporting precise cortical mapping. The MDME’s reusability, mechanical adaptability, and biocompatibility make it a promising candidate for long-term, high-quality electrophysiological monitoring in personalized healthcare, neurorehabilitation, and human-machine interfaces. Future work will explore integration with wireless systems and closed-loop feedback mechanisms, advancing its clinical and wearable applications.
Methods
Preparation of PEDOT: PSS film
The PEDOT: PSS solution was composed of PEDOT: PSS (CLEVIOS™ PH 1000), 10% w/w dimethyl sulfoxide (DMSO), 5% w/w isopropanol (IPA), 1% w/w (3-glycidoxypropyl)trimethoxysilane (GOPS), and 0.5% w/w TWEEN 20. Before application, the solution was stirred at room temperature for 10 mins. It was subsequently spin-coated onto the substrate and dried in an oven at 60 °C for 1 h.
Fabrication of MDME composites
The detailed preparation process is depicted in Fig. S1. The MDME primarily consists of a microneedle-structured shape memory polymer substrate combined with a PEDOT: PSS conductive film layer. The fabrication process begins with the addition of a fixed ratio of D230 to E44, followed by thorough stirring to achieve a homogeneous mixture, which is then poured into a mold. The mixture is degassed under vacuum to eliminate any trapped air bubbles. The mold is subsequently cured in an oven at 100 °C for 1 h. After heating, it is allowed to cool naturally to room temperature. The resulting microneedle-structured shape memory polymer substrate is then de-molded. The prepared PEDOT: PSS solution is spin-coated onto the substrate and dried to form a conductive film, completing the fabrication process.
Materials characterization
The shape memory properties of the microneedle structures in the MDME devices were characterized using a Zeiss Sigma 300 Scanning Electron Microscope (SEM). A Keyence VHX-7000 digital microscope was used to examine the overall morphology, surface, and cross-sectional features of the MDME devices. Impedance between the skin and the device was measured using an electrochemical workstation (CHI 660E, CH Instruments Inc.). Mechanical properties were evaluated using a tensile testing machine (CARE IBTC-300SL).
Skin-electrode impedance measurement
Skin-electrode impedance was measured using electrochemical impedance spectroscopy (EIS) with an electrochemical workstation. The scanning range of the electrochemical workstation was set between 1 Hz and 100 kHz. Before assembling the bioelectrodes on the skin, the forearm skin surface was cleaned with 75% medical alcohol followed by deionized water. Additionally, the skin-electrode impedance of the MDME was measured in an area similar to that of the gel electrode to minimize sample variation. Each device was measured at least three times.
Ethics approval
All experiments involving animals and human participants were conducted following a standard protocol (1061420210617007) approved by the Ethics Committee of the Animal Experiment Center at the University of Electronic Science and Technology of China.
Biocompatibility validation in rats
A 4 × 4 cm² area of dorsal skin of the rats was shaved, and histopathological examinations, including Hematoxylin-eosin (H&E) staining and Masson’s trichrome staining, were conducted following device application for seven days. The H&E and Masson’s trichrome staining results revealed an intact and well-defined epidermal structure, with neatly arranged and closely packed cells. These findings demonstrated the absence of pathological changes following long-term device application, confirming its non-toxicity and biocompatibility.
Human Research Participants
We recruited five volunteers aged 23–27 years to participate in ECG, EMG, and EEG recordings. Before the experiment, the subjects reviewed the relevant research materials and received comprehensive explanations, with satisfactory answers provided to their queries. The participants demonstrated a clear understanding of the relevant medical research materials, including the potential risks and benefits associated with the study. The subjects were informed that participation in the study was entirely voluntary, and they retained the right to withdraw at any time. They explicitly expressed their willingness to undergo scrutiny of the research materials by the drug regulatory department, ethics committee, or the applicant. Additionally, the participants agreed to the potential publication of research results in scientific journals or presentations at scientific conferences. It is important to note that all experiments involving human participants adhered to a standardized protocol (1061420210617007), approved by the Ethics Committee of the Animal Experiment Center at the University of Electronic Science and Technology of China. This ethical oversight ensures the responsible conduct of the research involving human participants.
Detection of epidermal electrophysiologic signals
ECG signals were acquired by placing two MDME devices on the inner side of the wrist and one MDME device on the ankle. The MDMEs were connected to a commercial ECG acquisition module. To detect EMG signals, two MDMEs were placed on the inner side of the forearm and one MDME on the outer side, forming a total of three electrode sets. These electrodes were connected to an EMG signal module with signal amplification and filtering capabilities for EMG signal monitoring. For comparison purposes, Ag/AgCl gel electrodes were also used. The EEG acquisition system primarily uses an Open-BCI module for collecting and transmitting EEG data. During testing, the data are wirelessly transmitted to a computer via Wi-Fi.
ECoG signals measurement
Four male Sprague-Dawley rats (approximately 270 g in body weight and 6 weeks old) were used in the study. All rats were anesthetized using isoflurane gas. Stereotactic coordinates were referenced to bregma, with the skull surface flat, following the method outlined by Paxinos and Watson. Four small holes were drilled into the skull over the primary (and secondary) visual cortex, regions potentially involved in SSVEP generation, with the drills positioned vertically to maintain the flatness of the skull surface. A small hole was drilled in the cerebellum. The cranial screw electrodes (500 µm in diameter) were implanted into the drill holes, with the reference electrode positioned at the cerebellum, a region exhibiting lower activity compared to other brain sites. The experiments were conducted in a well-lit, shielded room. Before the circular stimulus, a 5-min control period was recorded for each rat. Subsequently, the rats were sequentially exposed to an 8 Hz low-frequency stimulus. ECoG signals were recorded using a Cerebus Multi-Channel Neural Signal Acquisition System (sampling rate of 20,000 Hz) and filtered with an online bandpass filter (0.1–120 Hz) and a 50 Hz notch filter to eliminate line frequency interference.
Statistical analysis
The SNR was calculated using the equation SNR (dB) = 20log10(Asignal / Anoise), where Asignal is the peak-to-peak voltage of the ECG signal and Anoise is the peak-to-peak voltage of the noise. All experiments discussed in the manuscript were conducted with at least three replicates. The data are presented as mean and standard deviation of error propagated from replicates. Statistical details of experiments can be found in figure legends where applicable.
Data availability
The authors declare that all data supporting the findings of this study are available within the Article and its Supporting Information.
References
Wu, H. et al. Materials, devices, and systems of on‐skin electrodes for electrophysiological monitoring and human–machine interfaces. Adv. Sci. 8, 2001938 (2021).
Cheng, L., Li, J., Guo, A. & Zhang, J. Recent advances in flexible noninvasive electrodes for surface electromyography acquisition. npj Flex. Electron. 7, 39 (2023).
Sadikoglu, F., Kavalcioglu, C. & Dagman, B. Electromyogram (EMG) signal detection, classification of EMG signals and diagnosis of neuropathy muscle disease. Procedia Comput. Sci. 120, 422–429 (2017).
Pereira, T. M. C., Sebastiao, R., Conceição, R. C. & Sencadas, V. A review on intelligent systems for ecg analysis: from flexible sensing technology to machine learning. IEEE J. Biomed. Heal. Informatics. 29, 3398–3413 (2024).
Harati, A. & Jahanshahi, A. A reliable stretchable dry electrode for monitoring of EEG signals. Sens. Actuators A Phys. 326, 112727 (2021).
Al-Ayyad, M., Owida, H. A., De Fazio, R., Al-Naami, B. & Visconti, P. Electromyography monitoring systems in rehabilitation: a review of clinical applications, wearable devices and signal acquisition methodologies. Electronics 12, 1520 (2023).
Balzekas, I. et al. Invasive electrophysiology for circuit discovery and study of comorbid psychiatric disorders in patients with epilepsy: Challenges, opportunities, and novel technologies. Front. Hum. Neurosci. 15, 702605 (2021).
Piccini, J. P. et al. Advances in cardiac electrophysiology. Circ. Arrhythmia Electrophysiol. 15, e009911 (2022).
Wang, H. et al. High‐performance hydrogel sensors enabled multimodal and accurate human–machine interaction system for active rehabilitation. Adv. Mater. 36, 2309868 (2024).
Yao, G., Li, P., Liu, M., Liao, F. & Lin, Y. Smart contact lenses: catalysts for science fiction becoming reality. Innov. Cambridge 5, 100710 (2024).
Gordleeva, S. Y. et al. Real-time EEG–EMG human–machine interface-based control system for a lower-limb exoskeleton. Ieee Access 8, 84070–84081 (2020).
Gu, X. et al. EEG-based brain-computer interfaces (BCIs): A survey of recent studies on signal sensing technologies and computational intelligence approaches and their applications. IEEE/ACM Trans. Comput. Biol. Bioinforma. 18, 1645–1666 (2021).
Song, E., Li, J., Won, S. M., Bai, W. & Rogers, J. A. Materials for flexible bioelectronic systems as chronic neural interfaces. Nat. Mater. 19, 590–603 (2020).
Gan, X. Y. et al. Closed-eye intraocular pressure and eye movement monitoring via a stretchable bimodal contact lens. MICROSYSTEMS Nanoeng. 11, 83 (2025).
Sayyad, P. W., Al-Nashash, H., Al-Othman, A. & Al-Sayah, M. H. Emerging trends in system-integrated wearable epidermal and flexible electrodes: Material design and applications in physiological monitoring. IEEE Trans. Components, Packag. Manuf. Technol 15, 905–937 (2025).
Huang, J. et al. Physiological sensing system integrated with vibration sensor and frequency gel dampers inspired by spider. Mater. Horizons 11, 822–834 (2024).
Ershad, F., Patel, S. & Yu, C. Wearable bioelectronics fabricated in situ on skins. npj Flex. Electron. 7, 32 (2023).
Yang, L. et al. Materials for dry electrodes for the electroencephalography: advances, challenges, perspectives. Adv. Mater. Technol. 7, 2100612 (2022).
Xie, R. et al. Strenuous exercise-tolerance stretchable dry electrodes for continuous multi-channel electrophysiological monitoring. NPJ Flex. Electron. 6, 75 (2022).
Tian, Q. et al. Hairy‐skin‐adaptive viscoelastic dry electrodes for long‐term electrophysiological monitoring. Adv. Mater. 35, 2211236 (2023).
Singh, O. P., El-Badawy, I. M., Sundaram, S. & O’Mahony, C. Microneedle electrodes: materials, fabrication methods, and electrophysiological signal monitoring-narrative review. Biomed. Microdevices 27, 9 (2025).
Singh, O. P. et al. Flexible, conductive fabric‐backed, microneedle electrodes for electrophysiological monitoring. Adv. Mater. Technol. 9, 2301606 (2024).
Ji, H. et al. Skin-integrated, biocompatible, and stretchable silicon microneedle electrode for long-term EMG monitoring in motion scenario. npj Flex. Electron. 7, 46 (2023).
Lim, K. et al. Material and structural considerations for high-performance electrodes for wearable skin devices. Commun. Mater. 5, 49 (2024).
Gong, S., Lu, Y., Yin, J., Levin, A. & Cheng, W. Materials-driven soft wearable bioelectronics for connected healthcare. Chem. Rev. 124, 455–553 (2024).
Blume‐Peytavi, U. et al. Fragility of epidermis in newborns, children and adolescents. J. Eur. Acad. Dermatology Venereol. 30, 3–56 (2016).
Chen, Y. et al. Flexible inorganic bioelectronics. npj Flex. Electron. 4, 2 (2020).
Li, G. & Wen, D. Wearable biochemical sensors for human health monitoring: sensing materials and manufacturing technologies. J. Mater. Chem. B 8, 3423–3436 (2020).
Im, C. & Seo, J.-M. A review of electrodes for the electrical brain signal recording. Biomed. Eng. Lett. 6, 104–112 (2016).
Wen, Y. & Xu, J. Scientific importance of water‐processable PEDOT–PSS and preparation, challenge and new application in sensors of its film electrode: a review. J. Polym. Sci. Part A Polym. Chem. 55, 1121–1150 (2017).
Huang, H. et al. Graphene-based sensors for human health monitoring. Front. Chem. 7, 399 (2019).
Lu, F. et al. Review of stratum corneum impedance measurement in non-invasive penetration application. Biosensors 8, 31 (2018).
Uehara, O., Kusuhara, T., Matsuzaki, K., Yamamoto, Y. & Nakamura, T. Skin electrical impedance model for evaluation of the thickness and water content of the stratum corneum. Adv. Biomed. Eng. 11, 98–108 (2022).
Wang, B. & Facchetti, A. Mechanically flexible conductors for stretchable and wearable e‐skin and e‐textile devices. Adv. Mater. 31, 1901408 (2019).
Campbell, A. & Wu, C. Chronically implanted intracranial electrodes: tissue reaction and electrical changes. Micromachines 9, 430 (2018).
Gori, M., Vadalà, G., Giannitelli, S. M., Denaro, V. & Di Pino, G. Biomedical and tissue engineering strategies to control foreign body reaction to invasive neural electrodes. Front. Bioeng. Biotechnol. 9, 659033 (2021).
Shahrim, N. A., Ahmad, Z., Azman, A. W., Buys, Y. F. & Sarifuddin, N. Mechanisms for doped PEDOT: PSS electrical conductivity improvement. Mater. Adv. 2, 7118–7138 (2021).
Xing, R. et al. Inkjet printed polystyrene sulfuric acid-doped poly (3, 4-ethylenedioxythiophene)(PEDOT) uniform thickness films in confined grooves through decreasing the surface tension of PEDOT inks. Rsc Adv 7, 7725–7733 (2017).
Krackowizer, P. & Brenner, E. Thickness of the human skin. Phlebologie 37, 83–92 (2008).
Mahmud, M., Bertoldo, A. & Vassanelli, S. EEG Based Brain-Machine Interfacing: Navigation of Mobile Robotic Device. in Mobile Robots - Control Architectures, Bio-Interfacing, Navigation, Multi Robot Motion Planning and Operator Training (ed. Bedkowski, J.) 129–144 (IntechOpen, 2011).
Clayton, M. S., Yeung, N. & Cohen Kadosh, R. The many characters of visual alpha oscillations. Eur. J. Neurosci. 48, 2498–2508 (2018).
Zhu, M. et al. Flexible electrodes for in vivo and in vitro electrophysiological signal recording. Adv. Healthc. Mater. 10, 2100646 (2021).
Acknowledgements
This work was supported by the National Natural Science Foundation of China under grant numbers 62422104 (G.Y.), U21A20460 (Y.L.), 62371115 (G.Y.), 52021001 (Y.L.); Science and Technology Major Project of Tibetan Autonomous Region of China under grant no. XZ202201ZD0001G (G.Y.); Science and Technology Department of Sichuan Province under grant no. 2024NSFSC0234 (G.Y.); and the Medico-Engineering Cooperation Funds, Fundamental Research Funds for the Central Universities, UESTC under grant nos. ZYGX2020ZB041 (G.Y.), ZYGX2021YGLH002 (G.Y.).
Author information
Authors and Affiliations
Contributions
G.Y. conceived the concept. Y.L., K.C., and D.Y. provided lab assistance. G.Y., Y.L., and K.C. discussed and finalized the project plan. G.Y., Y.L., T.P., and M.G. supervised the project. G.Y. and C.Z. designed the device. C.Z., X.G., K.C., P.L., and J.P. performed the experiments and generated data in all figures. C.Z., K.C., G.Y., and K.C. participated in vivo experiments. C.Z., G.Y., T.P., M.G., Z.H., B.J., Z.Y., K.Z., D.Y., K.C., and Y.L. analyzed the data. C.Z., G.Y., K.C., and Y.L. wrote the manuscript. All authors reviewed and commended on the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, C., Yao, G., Gan, X. et al. Modulus-adjustable and mechanically adaptive dry microneedle electrodes for personalized electrophysiological recording. npj Flex Electron 9, 77 (2025). https://doi.org/10.1038/s41528-025-00458-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41528-025-00458-9