Abstract
To assist patients in maintaining oral health in patients with Parkinson’s disease (PD), this review aims to search the literature on aspects related to oral health in PD patients. In contrast to other research, we included the involvement of microbes in PD patients’ poor oral health. Finally, we conclude that, in comparison to healthy individuals, PD patients have poorer oral health and a higher incidence of oral ailments.
Similar content being viewed by others
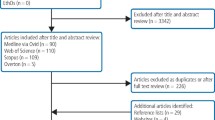
Introduction
Oral health is a critical component of overall health, over 3.5 billion individuals worldwide are in the oral unhealthy or sub-healthy state. So, global oral health challenges are vast1.
Parkinson’s disease (PD) is a progressive neurodegenerative disorder characterized by bradykinesia, muscle rigidity, resting tremor, and postural instability, affecting multiple body systems and with increasing prevalence in older people. The global burden of Parkinson’s disease is escalating due to the rapidly aging population worldwide2. Statistically, PD predominantly affects the older people, and patients with Parkinson’s disease are more likely to have oral health issues compared to healthy individuals, underscoring the importance of studying oral health in this patient population3. This review addresses three key areas: oral health challenges in PD patients, strategies for maintaining oral health, and approaches to treating oral disorders in individuals with Parkinson’s disease. The review also explores the links between PD and oral health disorders, the challenges faced by patients in accessing dental care, the complexities encountered in dental practice, medication considerations, and provides treatment recommendations for patients, caregivers, and dental professionals.
This paper first examines how PD affects oral health (e.g., dry mouth, periodontal disease, masticatory muscle dysfunction, etc.), but it also reverse-analyzes how oral health issues (e.g., microbiota dysbiosis, systemic inflammation) affect the progression of PD. A more thorough viewpoint for comprehending the intricate relationships between the two is offered by this investigation of the reciprocal relationship. Secondly, this article delves further into the connection between PD and the gut and oral microbiota, pointing out that microbiota dysbiosis may impact the development of PD via the gut-brain axis in addition to causing oral disease. Third, we suggest that rather than merely using generic oral medicines, PD patients’ oral health issues require individualized treatment programs.
Parkinson’s disease affects oral health
Numerous studies have demonstrated a bidirectional relationship between Parkinson’s disease and oral health4,5,6,7. The impact of Parkinson’s disease on oral health, as well as oral health disorders can influence the progression of PD. Generally, the primary oral health issues in Parkinson’s patients can be categorized into salivary problems (such as xerostomia and drooling), periodontal disease, oral complications arising from cognitive impairment or depression (such as oral dysfunction8, Periodontal Disease9) and temporomandibular disorders.
Xerostomia and drooling
Saliva plays a critical role in maintaining oral health10. Saliva contains proteins that help maintain the balance of the oral microbiome. A reduction in saliva disrupts this balance, increasing the risk of Candida infections. Saliva also plays a crucial role in attenuating and removing dietary sugars, acids, oral bacteria, and other harmful substances from the mouth, a process known as salivary self-cleaning. Additionally, saliva has significant acid-buffering capacity11. In summary, saliva protects teeth from decay through four key mechanisms: removing sugars and other debris, buffering acids, maintaining the balance between demineralization and remineralization, and exerting bacteriostatic effects10. Reduced saliva volume allows more food residues, especially sugars, to remain in the mouth, providing nutrients for dental plaque. Exposure to high-sucrose environments enables plaque bacteria to ferment sugars, producing acids that lower oral pH, thereby accelerating the onset or progression of dental caries. Simultaneously, the reduced capacity to balance demineralization and remineralization, coupled with diminished bacteriostatic activity, exacerbates the situation.
Parkinson’s disease often leads to abnormal salivation, primarily manifested as xerostomia and drooling. The prevalence of dry mouth among Parkinson’s patients ranges from 49% to 77%, while drooling occurs in 5–80% of cases12. Several factors contribute to dry mouth in Parkinson’s patients: increased acetylcholinesterase (AChE) activity in saliva compared to controls13, reduced cholinergic stimulation resulting in decreased saliva production, and the use of dopaminergic or anticholinergic medications that exacerbate xerostomia14. Additionally, dry mouth often leads to reduced food intake, which further diminishes salivary flow and worsens the condition15. Drooling in Parkinson’s patients can be attributed to several factors. As a progressive neurodegenerative disorder, Parkinson’s disease is characterized by tremors and slowed movements16. Patients often experience dysphagia (difficulty swallowing) and muscular dysfunction. The primary cause of drooling is not excessive saliva production but rather reduced swallowing efficiency. Additionally, oral conditions like periodontitis and dental caries, which are more prevalent in Parkinson’s patients, contribute to poor oral health and excessive salivation. Moreover, xerostomia can worsen dysphagia, potentially leading to further drooling17. Common medications for Parkinson’s disease, including levodopa and clozapine, are known contributors to hypersalivation. Studies report that 30–80% of patients treated with clozapine experience excessive salivation (sialorrhea)18.
Periodontitis
Periodontitis is a chronic, multifactorial inflammatory disease primarily driven by dental plaque accumulation, characterized by the progressive destruction of supporting tissues of the teeth, including the gingiva and alveolar bone19. Parkinson’s disease is closely associated with increased periodontal inflammation20. Due to symptoms such as tremors, bradykinesia (slowed movements), and rigidity21, Parkinson’s patients often struggle with maintaining daily and thorough oral hygiene. These motor impairments significantly limit their ability to perform effective oral cleaning routines. Studies have shown that the reduced motor function associated with Parkinson’s disease increases the vulnerability to periodontitis4,22. A key factor contributing to oral diseases such as caries and periodontitis is the disruption of the oral microbiota balance, often caused by a decline in microbial diversity (ecological disturbance)23. Abnormal salivation associated with Parkinson’s disease can lead to dysbiosis of the oral microbiota24.
Cognitive impairment
Cognitive impairment is a common non-motor symptom of Parkinson’s disease that affects a significant proportion of patients. At diagnosis, approximately 25% of Parkinson’s patients exhibit mild cognitive decline or mild cognitive impairment (MCI). Mild Cognitive Decline is a general term describing a noticeable decline in cognitive abilities, such as memory, attention, or problem-solving, that is greater than what is expected with normal aging. MCI is defined as the symptomatic predementia stage on the continuous sign of cognitive decline25, and up to 83% may develop severe cognitive impairment after 20 years26. Clinicians can diagnose the syndromes of dementia and MCI based on disease history, inspection result, and suitable objective assessments, using standard criteria27. Cognitive impairment in Parkinson’s disease commonly manifests as memory loss, disorganized thinking, impaired reasoning, paraphasia, and other cognitive disturbances, all of which significantly impact daily functioning. Compared to other neurodegenerative diseases, such as Alzheimer’s Disease, PD-MCI takes longer to convert into dementia than AD-MCI28, and the obvious characteristics which distinguishes Dementia with Lewy bodies (DLB) and Parkinson’s disease dementia (PDD) is early cognitive impairment in DLB and later onset following that of motor symptoms in PDD29.
Temporomandibular disorders
Temporomandibular disorders (TMD) encompass a diverse group of musculoskeletal and neurological conditions affecting the temporomandibular joint complex, as well as surrounding muscular and osseous structures30. TMD is characterized by intra-articular (within the joint) or extra-articular (outside the joint) issues, commonly presenting with jaw dysfunction and pain in the head, neck, and maxillofacial regions31,32. PD characterized by symptoms such as bradykinesia (slowed movement), muscle rigidity, postural instability, and resting tremors, which can affect the head, neck, and maxillofacial regions33. Parkinson’s patients frequently experience rigidity and tremors, which can exert abnormal forces on the teeth and jaw, potentially exacerbating symptoms of temporomandibular disorders (TMD)34. Studies have shown that individuals with Parkinson’s disease have a significantly higher risk of developing temporomandibular disorders compared to control groups35.
Depressive disorder
Depression and anxiety are among the most common mental health symptoms at the onset of Parkinson’s disease (PD)36. These conditions are significantly more prevalent in PD patients than in the general population, affecting 30–35% of newly diagnosed patients and up to 60% of those with advanced disease37. Clinically, depression in PD presents with symptoms such as depressed mood, feelings of vulnerability, anhedonia (loss of interest), communication difficulties, and disturbances in sleep and recreational activities38. The primary contributing factors may include progressive degeneration of the nigrostriatal dopaminergic pathway, abnormal neurotransmitter secretion, imbalance in the noradrenaline system, dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, neuroinflammation, and disruptions in nutritional supply39. Patients with depression or anxiety have a higher risk of developing oral diseases. Medications commonly used to treat depressive disorders, such as antipsychotics, antidepressants, and mood stabilizers, often have side effects like xerostomia (dry mouth), creating a bidirectional relationship between affective disorders and poor oral health40.
Burning mouth syndrome
Among middle-aged and elderly, anxiety disorders are the most prevalent psychiatric conditions associated with burning mouth syndrome (BMS), affecting 63.7% of cases, followed by depressive disorders, which affect 36.3%41. BMS is a chronic neuropathic pain condition characterized primarily by a burning sensation or pain in the absence of an identifiable cause. The exact etiology of BMS remains unclear, but recent studies suggest it may involve a combination of neuropathic, endocrine, and psychological factors42. The following table (Table 1) summarizes key findings from the literature, highlighting connections between oral health issues and Parkinson’s disease.
Decreased ability to maintain oral hygiene
Current studies suggest that as Parkinson’s disease progresses, patients’ ability to manage their oral hygiene declines. Those impacts are all-around. Cognitive impairment diminishes the ability to maintain proper oral hygiene and reduces the likelihood of seeking dental care. A lack of oral hygiene practices in individuals with cognitive impairment often results in a severely compromised oral environment9. Autonomic dysfunction and anti-Parkinson medications can lead to dysphagia, chewing difficulties, oral dyskinesia, salivary overflow, and xerostomia. These issues disrupt the self-cleaning mechanisms of the oral cavity and compromise oral hygiene, with swallowing problems potentially leading to aspiration pneumonia, a life-threatening condition43. In addition, PD patients may have difficulty in the aspect of using dental cleaning tools. A retrospective study found that over two-thirds of individuals with Parkinson’s disease did not replace their brush heads for eight weeks, and most brushed for less than two minutes44. The tremors in the hands, head, and face of PD patients, which make using interdental brushes and dental floss challenging and can easily cause pain or gum damage. Additionally, swallowing dysfunction increases the risk of choking and asphyxia when using mouthwash45.
Oral health affects Parkinson’s disease
Oral diseases can further aggravate the progression of PD, with the role of the oral microbiota being particularly significant. The brain-gut axis has been implicated in the pathogenesis of PD, highlighting the interconnectedness between oral health, gut health, and neurological conditions. Systemic inflammation resulting from oral infections can exacerbate PD, contributing to the overall inflammatory burden in the body. Additionally, many oral diseases cause eating discomfort, for example, periodontal disease causes the destruction of oral tissue and inflammation46, and temporomandibular disorders cause masticatory dysfunction and myalgia47, which can result in malnutrition—a common complication that further deteriorates the health of PD patients. Oral diseases can also worsen cognitive dysfunction, as inflammation and poor oral health are linked to the progression of neurological symptoms in PD.
Microbiota
Increasing research evidence suggests a direct link between Parkinson’s disease (PD) and the oral and gastrointestinal microbiota of patients48. The oral cavity and gastrointestinal tract host diverse and complex microbial populations that exist in symbiosis with the host and play a crucial role in overall health. Under normal conditions, these microbial communities support health maintenance, but imbalances can trigger various health issues, including dental caries, periodontal disease, bloating, and constipation. The oral cavity can serve as a reservoir of harmful microbes, and their migration to the gut may contribute to the pathogenesis of systemic diseases49.
Changes in gut flora are strongly associated with several symptoms of PD. Alterations in microbial composition and metabolism contribute to constipation, and symptoms similar to irritable bowel syndrome are linked to reduced Prevotella abundance in PD patients. The PD-associated microbiota favors protein hydrolysis metabolism, and studies in PD mouse models have shown that germ-free mice exhibit milder motility symptoms and reduced constipation compared to specific pathogen-free mice50. Additionally, the oral microbiota plays a critical role in the interplay between health and systemic diseases. Differences in the oral microbiota between PD patients and healthy individuals have been documented. The study found distinct beta diversity in the oral microbiota of PD patients compared to controls, with increased abundance of Prevotella, Prevotellaceae, Veillonella, Solobacterium, Veillonellaceae, Lactobacillaceae, and Corynebacteriaceae, and decreased levels of Capnocytophaga, Rothia, Kingella, Leptotrichia, Actinobacteria, and Leptobacteriaceae51. The increased presence of Prevotella and other opportunistic oral pathogens in PD patients may be linked to reduced oral hygiene, such as less frequent brushing, fewer professional dental visits, and increased rates of dental caries, periodontal disease, and tooth loss.
The gut-brain axis, through dysregulation of oral and intestinal microbiota, plays a crucial role in PD pathogenesis and progression, linking oral health directly to systemic inflammation and neurodegeneration. Research has demonstrated a strong link between the gut microbiota, neurodevelopment, and neurological disorders, with the gut-brain axis (GBA) serving as a critical connection52,53,54. The GBA illustrates the bidirectional communication between the nervous system and the gut, where gut-derived metabolites can influence neural function, and the gut is modulated by neural inputs50. Various intestinal conditions have been implicated in the increased risk of Parkinson’s disease (PD). For example, inflammatory bowel diseases, including ulcerative colitis and Crohn’s disease, are associated with a 22–35% increased risk of developing PD55. The GBA is a complex and dynamic system that connects the gut and the brain. In 2003, Braak hypothesized that gastrointestinal factors could contribute to the pathogenesis of PD. Key PD symptoms, such as GBA dysfunction, neural system infection, and dopaminergic system impairment, are associated with alterations in gut bacterial species56. Variations in gut bacteria are considered environmental factors that may drive the progression of PD. Additionally, the metabolism of levodopa, a primary treatment for PD, can be influenced by gut bacteria, leading to altered drug efficacy. The gut microbiota has also been linked to PD symptoms, including disease onset, muscle rigidity, tremors, cognitive impairment, and the variability in drug requirements among patients. In summary, the pathogenesis and clinical symptoms of Parkinson’s disease may be linked to disruptions in the gut-brain axis. Although these findings suggest a critical role of the gut microbiota in PD progression, conclusive evidence that gut microbial variations are the primary drivers of PD onset is still lacking57. The interrelationship between gut microbiota, oral diseases, and Parkinson’s disease is illustrated in the diagram below (Fig. 1). Normally, gut microbiota is stable, but it can become imbalanced due to environmental and host factors, leading to changes in microbial species and composition—a state known as ecological imbalance58. Evidence indicates that the gut microbiota in PD patients differs significantly from that of healthy individuals and is often imbalanced. While variations exist across populations, most reports highlight an increase in the relative abundance of Akkermansia and Bifidobacterium and a decrease in Faecalibacterium and Lachnospiraceae59,60. Although PD patients generally have lower gut bacterial diversity compared to healthy individuals, absolute bacterial counts are often not reported, and bacterial levels tend to decline as PD progresses61.
In summary, the oral and gut microbiota of PD patients are often dysregulated, differing significantly in composition and abundance compared to healthy individuals. Research indicates that the oral and gut microbiota interact with PD pathogenesis, with changes in gut microbiota contributing to PD progression, and PD, in turn, altering the microbiota52. Understanding these interactions is crucial for informing strategies for the prevention and management of Parkinson’s disease.
Systemic inflammation
Numerous studies in the field of nosography have previously confirmed the definitive association between systemic inflammation and the risk of Parkinson’s disease62,63. Findings from two independent studies corroborate that systemic inflammation is linked to decreased dopamine levels in Parkinson’s disease patients. While Parkinson’s disease is a complex, multifactorial neurological disorder, the primary pathogenic factor for its symptoms is the degeneration of the dopaminergic system64.
Malnutrition
Parkinson’s disease, a complex neurological disorder, is influenced by various factors, including nutrient intake and quality of life65. Nutrient intake, a latent and multifaceted environmental factor, plays a critical role in the progression of Parkinson’s disease and has recently garnered significant attention66. A study on induced Parkinson’s disease in mouse models demonstrated that zinc deficiency could be a driving factor in dyskinesia and dopaminergic system dysfunction. The study concluded that zinc deficiency can cause misexpression of hundreds of genes, including those related to Parkinson’s disease. In summary, zinc deficiency exacerbates the symptoms of Parkinson’s disease. It has been demonstrated that maintaining natural teeth positively impacts cognitive function. This is primarily because a complete dentition reduces the risk of systemic inflammation, preserves normal chewing function, and ensures adequate nutritional intake67. It is evident that various oral diseases, such as xerostomia, drooling, periodontitis, burning mouth syndrome, and temporomandibular disorders, can contribute to eating difficulties or loss of appetite, leading to malnutrition. Malnutrition and Parkinson’s disease can exacerbate each other68,69.
Cognitive disorder
Cognitive impairment is a common symptom of Parkinson’s disease, often leading to unfavorable clinical outcomes. The primary pathogenic factors are dysfunction in the dopaminergic system and cholinergic neuron disruption. The main symptoms of cognitive impairment in Parkinson’s disease include reduced attention, diminished thinking ability, and sensory decline. As the condition progresses, memory abilities and other cognitive functions further deteriorate70. The role of systemic inflammation, triggered by oral infection and malnutrition, has been discussed earlier in this article. Research has established a positive correlation between chewing ability and cognitive function71. Furthermore, a poor oral environment can significantly impair cognitive function. In summary, it has been demonstrated that oral health and cognitive function influence each other, with a direct proportional relationship between the two72.
Maintenance of oral health in PD patients
A significant knowledge gap exists regarding the utilization of dental care among patients with Parkinson’s disease35,73,74,75. To date, research on patients’ knowledge of dental care has revealed substantial variations in knowledge of oral health care and access to dental care systems among different groups of Parkinson’s disease patients75,76,77. To determine whether dental care needs are being met and if the Parkinson’s disease population receives less treatment than other groups, extensive epidemiological studies are necessary.
Oral hygiene maintenance
There are significant differences in tooth brushing frequency between individuals with Parkinson’s disease (PD) and the general population. Some studies indicate that the majority of PD patients brush their teeth more than twice daily78, a higher frequency than the general population, while other studies suggest that some PD patients brush less frequently79. Factors such as disease severity, the care environment, and oral hygiene awareness may all contribute to these differing outcomes. A retrospective study found that over two-thirds of individuals with Parkinson’s disease did not replace their brush heads for eight weeks, and most brushed for less than two minutes44. This finding suggests that PD patients may have deficiencies in maintaining oral hygiene. In terms of brushing tools, PD patients are more likely to use electric toothbrushes than traditional ones44. Although several studies have found no significant difference in plaque control between electric and manual toothbrushes80, electric toothbrushes offer PD patients a more effective way to clean their mouths with less effort, reducing the difficulty and improving the effectiveness of oral hygiene. Besides brushing, tools like dental floss, interdental brushes, and mouthwash are effective for plaque removal and oral hygiene maintenance, but PD patients use these tools significantly less often than the general population. The primary reason is the tremors in the hands, head, and face of PD patients, which make using interdental brushes and dental floss challenging and can easily cause pain or gum damage. Additionally, swallowing dysfunction increases the risk of choking and asphyxia when using mouthwash45. Some findings from current studies suggest that as Parkinson’s disease progresses, patients’ ability to maintain oral hygiene continues to deteriorate. At some unpredictable stage of Parkinson’s disease, patients may become dependent on others for routine oral hygiene care. PD patients also require specialized dental visits, including chairside prophylactic, conservative, prosthetic, surgical, and periodontal treatments44. However, patients with advanced oral health issues, such as tooth decay requiring extraction, often cannot receive conservative or prosthetic treatment during these typically outcome-oriented visits. In summary, PD patients face numerous challenges in both daily oral care and professional dental treatment. The key points are summarized in the figure below (Fig. 2).
Nursing for Parkinson’s patients
Research indicates that most individuals with Parkinson’s disease are cared for by caregivers, as the condition primarily affects older people and leads to various cognitive and behavioral impairments81,82. These caregivers may include family members, personal carers, or nursing home professionals. Unfortunately, a literature review revealed that oral hygiene care is often not prioritized by either professional caregivers or the patients themselves83. Inger et al. surveyed employees of assisted living facilities and found that while 89% of participants believed dental care was essential to quality care, 35% reported having no formal training in the field. The lack of adequate training for caregivers directly contributes to their low willingness to provide oral health care84. Even when caregivers were provided with guidelines and their implementation was monitored, there was no overall improvement in the oral health of nursing home residents44,85. Significant improvements and shifts in staff attitudes toward oral hygiene practices could occur if dental hygienists provided training to caregivers, performed monthly professional cleanings, and offered personal hygiene education86.
Difficulties in oral health care for PD patients
Barriers to oral health care in Parkinson’s disease (PD) patients arise primarily from two main factors. The first is the physical pathology of Parkinson’s disease, characterized by four key symptoms: tremor (trembling in hands, arms, legs, and face), postural instability (poor balance and coordination), rigidity (stiffness of the limbs and trunk), and bradykinesia (slowness of movement)87,88. The second factor involves socio-economic aspects, including the patient’s family economic status, the accessibility of oral health services, and the relevant policies in the patient’s region. Daily oral self-care for healthy individuals typically involves the use of toothbrushes, dental floss, and interdental brushes, all requiring fine hand control. However, PD patients often experience worse self-perceived hand function, reduced grip strength, and impaired fine motor skills, making it difficult to hold a toothbrush and perform precise cleaning tasks89. Additionally, Parkinson’s disease usually manifests asymmetrically, with varying levels of impairment in each hand90. If the dominant hand is more affected, maintaining oral hygiene becomes even more challenging. Cognitive impairment, which some patients develop, further complicates hand dexterity and adherence to oral care routines91. Obeso et al. observed that patients with advanced Parkinson’s disease may struggle to avoid falling forward, increasing their risk of dental trauma92. They also noted that these patients exhibit a specific gait disorder characterized by an inability to step backward to a deliberate height, reduced step length, and, at times, the need to run to maintain balance93. Mobility limitations often lead patients to prefer home-based oral care, but this model is not widely accessible. Additionally, autonomic dysfunction and anti-Parkinson medications can lead to dysphagia, chewing difficulties, oral dyskinesia, salivary overflow, and xerostomia. These issues disrupt the self-cleaning mechanisms of the oral cavity and compromise oral hygiene, with swallowing problems potentially leading to aspiration pneumonia, a life-threatening condition43.
The plight of the professional dental practice
Oral illnesses are deeply rooted in social factors and tend to be chronic94. Access to dental care services largely depends on factors such as distance, transportation, mobility, and affordability through healthcare system, dental insurance, and socio-economic status. For patients with Parkinson’s disease, accessing dental care poses significant challenges. The difficulties faced by PD patients in accessing dental care can be categorized into the following types:
Parkinson’s disease (PD) alters the oral and gut microbiota, leading to unique lesions in the oral environment that render standard therapies ineffective when directly applied95. Similarly, treatment methods for dysphagia developed for stroke or similar conditions cannot be indiscriminately applied to individuals with PD96. Additionally, dyskinesia and cognitive impairments associated with PD hinder standard diagnostic procedures and treatment5. These challenges indicate that oral therapies for PD patients lack universality. Therefore, healthcare professionals need interdisciplinary expertise. However, fostering collaboration and communication among multidisciplinary healthcare professionals is challenging. Currently, there is a shortage of healthcare professionals with the necessary interdisciplinary skills, leading to most PD patients not receiving targeted oral care97.
Some clinicians may harbor biases against PD patients, leading to less compassionate care. Treatments lacking in empathy further complicate the ability of PD patients to receive adequate oral care12. If a person has a frightening or embarrassing dental experience, they may tend to avoid subsequent dental treatment, leading to increased anxiety, a condition known as “dental anxiety”98. Due to inadequate oral care, many PD patients have had negative dental experiences. These experiences can heighten anxiety and fear, leading to dental anxiety and hindering further treatment. Some PD patients with neuropsychiatric symptoms, such as depression, fatigue, cognitive decline, and dementia, may struggle to express their need for dental care, resist treatment, and have difficulty attending dental appointments. Parkinson’s disease medications are known to have psychological side effects, such as disorientation and memory loss99, which can complicate patients’ ability to maintain proper dental hygiene and schedule regular checkups. A Swedish study showed a significant decline in dental care visits following a dementia diagnosis77. The decline was more pronounced in individuals with mixed dementia, dementia with Parkinson’s syndrome, and those with severe and rapid cognitive impairment100. After a dementia diagnosis, 19% of individuals had no documented dental appointments, with those living alone being the most likely to stop seeing a dentist. To provide appropriate support and oral care for people with Parkinson’s disease (PD), patients, dental and healthcare professionals, and family members must be aware of the risk factors affecting oral health. A study found that patients with mild symptoms and the strongest effects of their medication benefited most from short dental appointments (no more than 45 min) scheduled in the early morning, 90 min after taking their Parkinson’s medication101. Patients can use this guideline to schedule their dental appointments at the most effective time. Additionally, PD patients may face communication challenges with their dentists due to conditions like apathy, anxiety, and depression75. More critically, dental treatment may be impossible if the dentist lacks relevant experience.
Orofacial lesions in PD patients present significant challenges for dentists102. Parkinson’s patients have a high prevalence of temporomandibular joint disorders (TMD), with approximately 20% exhibiting signs and symptoms103. These patients often have limited maximum unassisted jaw opening, lateral movement, and protrusion35. Additionally, disease-related facial and oral muscle pain may cause patients to resist or limit mouth opening, reducing the dentist’s ability to operate effectively. The risk of aspiration and ingestion of dental instruments increases when PD patients are supine during dental procedures. Operating the dental chair at 45-degree tilt, using occlusal props, rubber dams, and high-volume oral evacuation has been shown to enhance airway protection and reduce this risk101. Additionally, Parkinson’s-related head tremors, muscle spasms, and ankylosis make it difficult for patients to remain still or stable, and uncontrollable tremors can complicate dental procedures. In some cases, symptom exacerbation may even necessitate stopping the treatment104. Due to these tremors, the risk of injuring soft tissues in the mouth is heightened when sharp instruments are used during examination. When administering anesthesia to PD patients, it is crucial to be aware of potential adverse drug interactions. Adrenaline-containing drugs should be avoided in local anesthesia, as they can interact with COMT inhibitors to cause high blood pressure105. If general anesthesia is required, potential interactions must be considered; for example, combining pethidine and selegiline can cause heat, muscle rigidity, and restlessness106. Doctors should also avoid medications that can induce or worsen Parkinson’s symptoms, such as phenothiazines, butyrophenones, and metoclopramide107.
Treatment of oral diseases in patients with PD
Parkinson’s patients experience more oral health issues, and the pharmacological, psychological, and physical effects of Parkinson’s disease on the individual must be carefully considered in treating their oral conditions.
Medication for Parkinson’s
Parkinson’s disease is characterized by the degeneration and death of nigrostriatal dopaminergic neurons, resulting in dopamine deficiency and elevated acetylcholine levels in the body. Levodopa, a dopamine precursor, is a potent treatment for PD and is often combined with other medications in clinical practice108. For instance, combining levodopa with a peripheral decarboxylase inhibitor like carbidopa significantly reduces nausea and vomiting post-administration and increases the amount of levodopa reaching the brain. Levodopa has a short half-life and is rapidly metabolized when used alone. Co-administration with a catechol-O-methyltransferase (COMT) inhibitor extends the half-life of both levodopa and dopamine, enhancing their therapeutic effects. Monoamine oxidase type B inhibitors, such as selegiline, inhibit endogenous dopamine catabolism and are often potentiated when combined with levodopa.
The complexity and variety of medications used in treating Parkinson’s patients necessitate that dentists be fully aware of the patient’s medication history before diagnosis and treatment to avoid adverse drug interactions. The interaction between epinephrine and COMT inhibitors can result in dangerously high blood pressure, so epinephrine-containing medications should be avoided. Co-administration of pethidine and selegiline can induce agitation, muscle rigidity, and hyperthermia in patients107. Additionally, avoid medications like metoclopramide, phenothiazines, and butyrophenones (such as haloperidol) that may cause or exacerbate Parkinson’s symptoms. Due to the pharmacokinetics of levodopa and the variability of the patient’s symptoms, early morning appointments are often preferred for dental visits. Some Parkinson’s patients may experience urinary incontinence, making it necessary to assist them with restroom use before the dental visit101.
The interdisciplinary cooperation of medical workers
Despite the close proximity of the central nervous system to the oral cavity, research on the treatment of PD patients with oral diseases is limited. Healthcare providers should prioritize the pathological features of PD and apply therapies specifically tailored to PD patients. This necessitates that medical professionals possess interdisciplinary knowledge and engage in transdisciplinary collaboration. The medical field should cultivate professionals with interdisciplinary knowledge and promote interdisciplinary cooperation. Healthcare professionals should develop dental treatments specifically tailored to the needs of PD patients109.
Popularizing regular home visit nursing
Parkinson’s symptoms make adequate dental care and treatment challenging. According to surveys, PD patients with oral diseases are less likely to receive regular dental care76. Therefore, it is essential to promote regular home visit nursing. Home visit nursing ensures that PD patients’ oral diseases are detected in a timely manner and helps guarantee the prevention of further oral health issues.
Paying attention to prevention
Studies have shown that PD patients with oral diseases tend to seek dental treatment rather than focus on prevention76. However, it is widely recognized in the medical field that the most effective treatment is often prevention110. PD patients should receive regular dental care and examinations to help reduce the risk of oral diseases, and to detect and treat them early. The best approach to managing oral health in PD patients is prevention. Effective prevention requires ensuring that patients receive regular examinations and dental care. Due to the physical symptoms of PD, home visit nursing is a more suitable approach. Eliminating biases against PD patients is equally important, as it improves their medical experience and increases the likelihood of them seeking dental treatment proactively. PD patients should also maintain healthy living habits that contribute to the management and potential remission of Parkinson’s disease.
Exploring the correlation feature between PD and oral diseases
There is a bidirectional relationship between Parkinson’s disease (PD) and oral diseases. Certain changes in the oral cavity can be early indicators of PD78. For example, PD patients often exhibit a distinctive oral microbiota111. These features can be used for the early diagnosis of Parkinson’s disease. Similarly, when a PD patient requires dental treatment, these PD-specific features should be taken into account to ensure more effective and targeted care. Some patients exhibit increased salivation and swallowing difficulties, necessitating special positioning during consultations. DeBowes et al. recommend a semi-tilted position (45-degree angle) during consultations to prevent choking and aspiration, effectively reducing excessive saliva accumulation in the oral cavity112. For patients with involuntary movements and tremors, an assistant is needed to help stabilize the patient’s body and head, and to ensure effective aspiration of oral fluids. Additionally, bite blocks and other oral tools can be employed to assist patients who have difficulty opening their mouths due to muscle rigidity. Local anesthesia should be used cautiously, as the resulting loss of sensation may exacerbate swallowing difficulties, increasing the risk of choking and aspiration. Due to the prevalence of orthostatic hypotension, it is crucial to gradually raise the dental chair at the end of the consultation and allow the patient time to adjust before standing to avoid fainting or falling.
Improving patients’ living habits
Favorable living habits can help attenuate symptoms caused by PD, thereby reducing treatment difficulty. For example, maintaining regular exercise leads to better clinical outcomes, and different types of exercise produce varying positive effects113. A sensible diet, such as the protein-restricted diet (PRD), ketogenic diet (KD), Mediterranean diet (MD), or the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet, can reduce the severity of Parkinson’s disease65. Good sleep quality can slow the progression of Parkinson’s disease114. Positive social relationships promote healthy behavior115. An environment free from harmful chemicals such as pesticides and metal ions can decrease the risk of developing PD and slow the progression of the disease116. Current studies suggest that as Parkinson’s disease progresses, patients’ ability to manage their oral hygiene declines. At some point, they may become dependent on others for routine oral care. However, they still wish to care for themselves as independently as possible. If they can no longer manage their daily brushing routine, they may consider accepting additional care assistance117. It is clear that healthcare providers often fail to prioritize oral health and care due to factors such as lack of knowledge, time constraints, unclear responsibilities, patient resistance, and low priority. Large-scale epidemiological studies are needed to determine whether the dental care needs of the Parkinson’s population are being met and if there is an imbalance in services compared to the general population. Statistical findings will provide clinicians and policymakers with the necessary data to ensure that optimal dental care is provided to Parkinson’s patients and to improve their oral health status.
Limitation
Despite our efforts to provide a comprehensive narrative review, this study has certain limitations. First, the selection of literature was based on relevance and the authors’ expertise, which may have led to an underrepresentation of certain areas of research. This inherent selection bias may limit the generalizability of our conclusions. Second, narrative reviews, by nature, lack a standardized methodology for data synthesis, increasing the potential for subjectivity in analysis and interpretation. To mitigate this, we have incorporated multiple perspectives by citing diverse studies and discussing contrasting viewpoints where applicable. Additionally, this review does not include a systematic quality assessment of the included studies, which could influence the strength of the conclusions drawn.
Conclusion
In general, there is a reciprocal relationship between Parkinson’s disease and dental health: Parkinson’s can lead to dry mouth, periodontitis, TMD, and other oral health issues, while gut microbiota, inflammatory responses, and other factors can also influence both dental health and Parkinson’s disease. The oral health of Parkinson’s patients is crucial and should not be overlooked. Both patients and their relatives or caregivers must recognize the importance of oral health and learn proper oral care practices. Currently, there are numerous barriers to maintaining oral health for PD patients, including their mobility and mental challenges, as well as the special preparations needed for professional dental consultations and the complexity of oral disease treatment. However, there remains a lack of specialized treatments for the oral diseases that occur in PD patients. Therefore, we recommend that individuals with Parkinson’s disease (PD) focus on preventing oral disorders, adopting healthier lifestyles, and collaborating with healthcare professionals across disciplines to preserve oral health, improve overall well-being, and achieve a higher quality of life.
Data availability
No datasets were generated or analyzed during the current study.
References
Watt, R. G. et al. Ending the neglect of global oral health: time for radical action. Lancet 394, 261–272 (2019).
Dorsey, E. R. et al. The Emerging Evidence of the Parkinson Pandemic. J. Parkinsons Dis. 8, S3–s8 (2018).
Verhoeff, M. C. et al. Parkinson’s disease and oral health: A systematic review. Arch. Oral. Biol. 151, 105712 (2023).
Bian, M., Chen, L. & Lei, L. Research progress on the relationship between chronic periodontitis and Parkinson’s disease. Zhejiang da xue xue bao Yi xue ban. J. Zhejiang Univ. Med. Sci. 51, 108–114 (2022).
Auffret, M. et al. Oral Health Disorders in Parkinson’s Disease: More than Meets the Eye. J. Parkinsons Dis. 11, 1507–1535 (2021).
Wang, B. et al. Mechanisms of oral microflora in Parkinson’s disease. Behav. Brain Res. 474, 115200 (2024).
Wang, Z. Z. et al. Risk of dementia or Parkinson’s disease in the presence of Sjögren’s syndrome: A systematic review and meta-analysis. Front. Integr. Neurosci. 16, 1027044 (2022).
Nakamura, T. et al. Oral dysfunctions and cognitive impairment/dementia. J. Neurosci. Res. 99, 518–528 (2021).
Said-Sadier N., et al. Association between Periodontal Disease and Cognitive Impairment in Adults. Int. J. Environ. Res. Public Health, 20, 4707 (2023).
Llena-Puy, C. The rôle of saliva in maintaining oral health and as an aid to diagnosis. Med. Oral. Patologia Oral. Y. Cirugia Bucal 11, E449–E455 (2006).
Pedersen, A. et al. Salivary functions in mastication, taste and textural perception, swallowing and initial digestion. Oral. Dis. 24, 1399–1416 (2018).
Verhoeff, M. C. et al. Salivation in Parkinson’s disease: A scoping review. Gerodontology 40, 26–38 (2023).
Fedorova, T. et al. Salivary acetylcholinesterase activity is increased in Parkinson’s disease: a potential marker of parasympathetic dysfunction. Parkinsons Dis. 2015, 156479 (2015).
Špiljak, B. et al. Sialorrhea and xerostomia in Parkinson’s disease patients. Acta Clin. Croatica 61, 320–326 (2022).
Barbe, A. G. et al. Circadian rhythms and influencing factors of xerostomia among Parkinson’s disease patients. Oral. Dis. 25, 282–289 (2019).
Zafar, S., Yaddanapudi, S. S. Parkinson Disease. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2025, StatPearls Publishing LLC; 2025.
Arnao, V. et al. In patient’s with Parkinson disease, autonomic symptoms are frequent and associated with other non-motor symptoms. Clin. Autonomic Res. 25, 301–307 (2015).
Bird, A. M., Smith, T. L. & Walton, A. E. Current treatment strategies for clozapine-induced sialorrhea. Ann. Pharmacother. 45, 667–675 (2011).
Kwon, T., Lamster, I. B. & Levin, L. Current Concepts in the Management of Periodontitis. Int. Dent. J. 71, 462–476 (2021).
Yilmaz, M. et al. Parkinson’s disease is positively associated with periodontal inflammation. J. Periodontol. 94, 1425–1435 (2023).
Abusrair, A. H., Elsekaily, W. & Bohlega, S. Tremor in Parkinson’s Disease: From Pathophysiology to Advanced Therapies. Tremor Other Hyperkinetic Mov. 12, 29 (2022).
Kaur, T., Uppoor, A. & Naik, D. Parkinson’s disease and periodontitis - the missing link? A review. Gerodontology 33, 434–438 (2016).
Minty, M. et al. Oral microbiota-induced periodontitis: a new risk factor of metabolic diseases. Rev. Endocr. Metab. Disord. 20, 449–459 (2019).
Berthouzoz, E. et al. Oral and intestinal dysbiosis in Parkinson’s disease. Rev. Neurologique 179, 937–946 (2023).
Langa, K. M. & Levine, D. A. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA 312, 2551–2561 (2014).
Jellinger, K. A. Pathobiology of Cognitive Impairment in Parkinson Disease: Challenges and Outlooks. Int. J. Mol. Sci. 25, 498 (2023).
Hugo, J. & Ganguli, M. Dementia and cognitive impairment: epidemiology, diagnosis, and treatment. Clin. Geriatr. Med. 30, 421–442 (2014).
Besser, L. M. et al. Mild cognitive impairment in Parkinson’s disease versus Alzheimer’s disease. Parkinsonism Relat. Disord. 27, 54–60 (2016).
Jellinger, K. A. & Korczyn, A. D. Are dementia with Lewy bodies and Parkinson’s disease dementia the same disease?. BMC Med. 16, 34 (2018).
Ohrbach, R. et al. Clinical orofacial characteristics associated with risk of first-onset TMD: the OPPERA prospective cohort study. J. Pain. 14, T33–T50 (2013).
Gauer, R. L. & Semidey, M. J. Diagnosis and treatment of temporomandibular disorders. Am. Fam. Physician 91, 378–386 (2015).
Romero-Reyes, M. & Bassiur, J. P. Temporomandibular Disorders, Bruxism and Headaches. Neurologic Clin. 42, 573–584 (2024).
Beaumont, S. et al. Temporomandibular Disorder: a practical guide for dental practitioners in diagnosis and management. Aust. Dent. J. 65, 172–180 (2020).
Minervini, G. et al. Prevalence of temporomandibular disorders in subjects affected by Parkinson disease: A systematic review and metanalysis. J. Oral. Rehabilit. 50, 877–885 (2023).
Baram, S. et al. Orofacial function and temporomandibular disorders in Parkinson’s Disease: a case-controlled study. BMC Oral. Health 23, 381 (2023).
Weintraub, D. et al. The neuropsychiatry of Parkinson’s disease: advances and challenges. Lancet Neurol. 21, 89–102 (2022).
Weintraub, D. et al. Neuropsychiatric symptoms and cognitive abilities over the initial quinquennium of Parkinson disease. Ann. Clin. Transl. Neurol. 7, 449–461 (2020).
Mendonça, I. P. et al. Neurobiological findings underlying depressive behavior in Parkinson’s disease: A review. Int. Immunopharmacol. 83, 106434 (2020).
Ahmad, M. H. et al. Neurobiology of depression in Parkinson’s disease: Insights into epidemiology, molecular mechanisms and treatment strategies. Ageing Res. Rev. 85, 101840 (2023).
Kisely, S. et al. The oral health of people with anxiety and depressive disorders - a systematic review and meta-analysis. J. Affect. Disord. 200, 119–132 (2016).
Dibello, V., et al. Exploring the Association of Burning Mouth Syndrome with Depressive and Anxiety Disorders in Middle-Aged and Older Adults: A Systematic Review. J. Personalized Med., 13, 1014 (2023)
Khawaja, S. N., Alaswaiti, O. F. & Scrivani, S. J. Burning Mouth Syndrome. Dent. Clin. North Am. 67, 49–60 (2023).
Pradeep, A. R. et al. Clinical evaluation of the periodontal health condition and oral health awareness in Parkinson’s disease patients. Gerodontology 32, 100–106 (2015).
Auerbacher, M. et al. Oral health in patients with neurodegenerative and cerebrovascular disease: a retrospective study. Disabil. Rehabilit. 45, 2316–2324 (2023).
Patel, B. et al. A comprehensive review of the diagnosis and treatment of Parkinson’s disease dysphagia and aspiration. Expert Rev. Gastroenterol. Hepatol. 14, 411–424 (2020).
Sedghi, L. M., Bacino, M. & Kapila, Y. L. Periodontal Disease: The Good, The Bad, and The Unknown. Front. Cell. Infect. Microbiol. 11, 766944 (2021).
Liu, F. & Steinkeler, A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent. Clin. North Am. 57, 465–479 (2013).
Yemula, N. et al. Parkinson’s Disease and the Gut: Symptoms, Nutrition, and Microbiota. J. Parkinsons Dis. 11, 1491–1505 (2021).
Kitamoto, S. et al. The Bacterial Connection between the Oral Cavity and the Gut Diseases. J. Dent. Res. 99, 1021–1029 (2020).
Sampson, T. R. et al. Gut Microbiota Regulate Motor Deficits and Neuroinflammation in a Model of Parkinson’s Disease. Cell 167, 1469–80.e12 (2016).
Pereira, P. A. B. et al. Oral and nasal microbiota in Parkinson’s disease. Parkinsonism Relat. Disord. 38, 61–67 (2017).
Cryan, J. F. et al. The Microbiota-Gut-Brain Axis. Physiological Rev. 99, 1877–2013 (2019).
Wang, Q., Yang, Q. & Liu, X. The microbiota-gut-brain axis and neurodevelopmental disorders. Protein Cell 14, 762–775 (2023).
Loh, J. S. et al. Microbiota-gut-brain axis and its therapeutic applications in neurodegenerative diseases. Sig. Transduct. Target. Ther. 9, 37 (2024).
Lin, J. C. et al. Association Between Parkinson’s Disease and Inflammatory Bowel Disease: a Nationwide Taiwanese Retrospective Cohort Study. Inflamm. Bowel Dis. 22, 1049–1055 (2016).
Claudino, D. O. S. et al. Role of enteric glia and microbiota-gut-brain axis in parkinson disease pathogenesis. Ageing Res. Rev. 84, 101812 (2023).
Dong, S. et al. Brain-gut-microbiota axis in Parkinson’s disease: A historical review and future perspective. Brain Res. Bull. 183, 84–93 (2022).
Keightley, P. C., Koloski, N. A. & Talley, N. J. Pathways in gut-brain communication: evidence for distinct gut-to-brain and brain-to-gut syndromes. Aust. N.Z. J. Psychiatry 49, 207–214 (2015).
Cirstea, M. S. et al. Microbiota Composition and Metabolism Are Associated With Gut Function in Parkinson’s Disease. Mov. Disord. 35, 1208–1217 (2020).
Wallen, Z. D. et al. Characterizing dysbiosis of gut microbiome in PD: evidence for overabundance of opportunistic pathogens. NPJ Parkinsons Dis. 6, 11 (2020).
Minato, T. et al. Progression of Parkinson’s disease is associated with gut dysbiosis: Two-year follow-up study. PloS One 12, e0187307 (2017).
Li, C. et al. Systemic inflammation and risk of Parkinson’s disease: A prospective cohort study and genetic analysis. Brain Behav. Immun. 117, 447–455 (2024).
Mou, Y. et al. Gut Microbiota Interact With the Brain Through Systemic Chronic Inflammation: Implications on Neuroinflammation, Neurodegeneration, and Aging. Front. Immunol. 13, 796288 (2022).
Muñoz-Delgado, L. et al. Peripheral Inflammation Is Associated with Dopaminergic Degeneration in Parkinson’s Disease. Movement disorders : official journal of the Movement Disorder. Society 38, 755–763 (2023).
Knight, E. et al. The Role of Diet and Dietary Patterns in Parkinson’s Disease. Nutrients 14, 4472 (2022).
Bianchi, V. E., Rizzi, L. & Somaa, F. The role of nutrition on Parkinson’s disease: a systematic review. Nutritional Neurosci. 26, 605–628 (2023).
Galindo-Moreno, P. et al. The impact of tooth loss on cognitive function. Clin. Oral. Investig. 26, 3493–3500 (2022).
Burgos, R. et al. ESPEN guideline clinical nutrition in neurology. Clin. Nutr. 37, 354–396 (2018).
Bianchi, V. E., Herrera, P. F. & Laura, R. Effect of nutrition on neurodegenerative diseases. A systematic review. Nutritional Neurosci. 24, 810–834 (2021).
Zhang, Q. et al. Approach to Cognitive Impairment in Parkinson’s Disease. Neurotherapeutics : the journal of the American Society for Experimental. NeuroTherapeutics 17, 1495–1510 (2020).
Weijenberg, R. A., Scherder, E. J. & Lobbezoo, F. Mastication for the mind–the relationship between mastication and cognition in ageing and dementia. Neurosci. Biobehav. Rev. 35, 483–497 (2011).
Wei, T. et al. Association between adverse oral conditions and cognitive impairment: A literature review. Front. Public Health 11, 1147026 (2023).
Clifford, T. & Finnerty, J. The dental awareness and needs of a Parkinson’s disease population. Gerodontology 12, 99–103 (1995).
Nakayama, Y., Washio, M. & Mori, M. Oral health conditions in patients with Parkinson’s disease. J. Epidemiol. 14, 143–150 (2004).
Barbe, A. G. et al. Self-assessment of oral health, dental health care and oral health-related quality of life among Parkinson’s disease patients. Gerodontology 34, 135–143 (2017).
Baram, S. et al. Dental care utilization among persons with Parkinson’s disease in Denmark. Community Dent. Oral. Epidemiol. 51, 527–534 (2023).
Lexomboon, D. et al. Discontinued dental care attendance among people with dementia: A register-based longitudinal study. Gerodontology 38, 57–65 (2021).
García-De-La-Fuente, A. M. et al. Facts and controversies regarding oral health in Parkinson’s disease: A case-control study in Spanish patients. Med. Oral. Patologia Oral. Y. Cirugia Bucal 27, e419–e425 (2022).
John, T. K. et al. Does parkinsonism affect periodontal health? A cross-sectional study in a tertiary hospital. J. Indian Soc. Periodontol. 25, 538–543 (2021).
Conway, F. Powered or manual toothbrushes for people with disabilities - which is better?. Evid. Based Dent. 25, 45–46 (2024).
Meng, D. et al. Prevalence of Parkinson’s disease among adults aged 45 years and older in China: a cross-sectional study based on the China health and retirement longitudinal study. BMC Public Health 24, 1218 (2024).
Chen, Z., Li, G. & Liu, J. Autonomic dysfunction in Parkinson’s disease: Implications for pathophysiology, diagnosis, and treatment. Neurobiol. Dis. 134, 104700 (2020).
Zenthöfer, A. et al. Poor dental hygiene and periodontal health in nursing home residents with dementia: an observational study. Odontology 105, 208–213 (2017).
Wårdh, I., Jonsson, M. & Wikström, M. Attitudes to and knowledge about oral health care among nursing home personnel–an area in need of improvement. Gerodontology 29, e787–e792 (2012).
Lauritano, D., et al. Aging and Oral Care: An Observational Study of Characteristics and Prevalence of Oral Diseases in an Italian Cohort. Int. J. Environ. Res. Public Health, 16, 3763 (2019).
Girestam Croonquist, C. et al. Effects of Domiciliary Professional Oral Care for Care-Dependent Elderly in Nursing Homes - Oral Hygiene, Gingival Bleeding, Root Caries and Nursing Staff’s Oral Health Knowledge and Attitudes. Clin. Interventions Aging 15, 1305–1315 (2020).
Bloem, B. R., Okun, M. S. & Klein, C. Parkinson’s disease. Lancet 397, 2284–2303 (2021).
Li, Z. et al. Shigella evades pyroptosis by arginine ADP-riboxanation of caspase-11. Nature 599, 290–295 (2021).
Toktas, H. et al. FPL tendon thickness, tremor and hand functions in Parkinson’s disease. Open Med. 11, 16–20 (2016).
Wong-Yu, I. S. K., Ren, L. & Mak, M. K. Y. Impaired Hand Function and Its Association With Self-Perceived Hand Functional Ability and Quality of Life in Parkinson Disease. Am. J. Phys. Med. Rehabilit. 101, 843–849 (2022).
Kobayashi-Cuya, K. E. et al. Observational Evidence of the Association Between Handgrip Strength, Hand Dexterity, and Cognitive Performance in Community-Dwelling Older Adults: A Systematic Review. J. Epidemiol. 28, 373–381 (2018).
Obeso, J. A. et al. Past, present, and future of Parkinson’s disease: A special essay on the 200th Anniversary of the Shaking Palsy. Mov. Disord. 32, 1264–1310 (2017).
Khan, I. Falls: considerations for the dental surgeon. Br. Dent. J. 228, 509–514 (2020).
Peres, M. A. et al. Oral diseases: a global public health challenge. Lancet 394, 249–260 (2019).
Li, Z. et al. Oral, Nasal, and Gut Microbiota in Parkinson’s Disease. Neuroscience 480, 65–78 (2022).
Umemoto, G. & Furuya, H. Management of Dysphagia in Patients with Parkinson’s Disease and Related Disorders. Intern. Med. 59, 7–14 (2020).
Rozas, N. S. et al. Incorporating oral health into interprofessional care teams for patients with Parkinson’s disease. Parkinsonism Relat. Disord. 43, 9–14 (2017).
Liddell, A. & Locker, D. Changes in levels of dental anxiety as a function of dental experience. Behav. Modif. 24, 57–68 (2000).
Connolly, B. S. & Lang, A. E. Pharmacological treatment of Parkinson disease: a review. JAMA 311, 1670–1683 (2014).
Fereshtehnejad, S. M. et al. Dental care utilization in patients with different types of dementia: A longitudinal nationwide study of 58,037 individuals. Alzheimers Dement. 14, 10–19 (2018).
Friedlander, A. H. et al. Parkinson disease: systemic and orofacial manifestations, medical and dental management. J. Am. Dent. Assoc. 140, 658–669 (2009).
Lobbezoo, F. & Naeije, M. Dental implications of some common movement disorders: a concise review. Arch. Oral. Biol. 52, 395–398 (2007).
Martimbianco, A. L. C. et al. Evidence-Based Recommendations for the Oral Health of Patients with Parkinson’s Disease. Neurol. Ther. 10, 391–400 (2021).
Gosnell, R. et al. Development of guidelines for improving oral health in individuals with Parkinson’s disease. Gerodontology 36, 229–235 (2019).
Morimoto, Y. et al. Management for the patients with severe Parkinson’s disease during dental treatments and tooth extractions: A retrospective observational study. J. Dent. Sci. 19, 261–267 (2024).
Starr, C. Interaction between pethidine and selegiline. Lancet 337, 554 (1991).
Nicholson, G., Pereira, A. C. & Hall, G. M. Parkinson’s disease and anaesthesia. Br. J. Anaesth. 89, 904–916 (2002).
Cotzias, G. C., Papavasiliou, P. S. & Gellene, R. Modification of Parkinsonism–chronic treatment with L-dopa. N. Engl. J. Med. 280, 337–345 (1969).
Verhoeff, M. C., Raphael, K. G. & Lobbezoo, F. A personal exploration of oral health in Parkinson’s disease through the eyes of a multifaceted authority. J. Oral. Rehabilit 51, 1645–1652 (2024).
Verhoeff, M. C. et al. Clinicians’ view on the management of oral health in Parkinson’s disease patients: a qualitative study. BDJ open 9, 20 (2023).
Yay, E. et al. Oral and gut microbial profiling in periodontitis and Parkinson’s disease. J. Oral. Microbiol. 16, 2331264 (2024).
Debowes, S. L., Tolle, S. L. & Bruhn, A. M. Parkinson’s disease: considerations for dental hygienists. Int. J. Dent. Hyg. 11, 15–21 (2013).
Tsukita, K., Sakamaki-Tsukita, H. & Takahashi, R. Long-term Effect of Regular Physical Activity and Exercise Habits in Patients With Early Parkinson Disease. Neurology 98, e859–e871 (2022).
Xu, Z., Anderson, K. N. & Pavese, N. Longitudinal Studies of Sleep Disturbances in Parkinson’s Disease. Curr. Neurol. Neurosci. Rep. 22, 635–655 (2022).
Mavandadi, S. et al. Social Control and Health Behaviors Among Individuals Living with Parkinson’s Disease: A Pilot Study. Int. J. Behav. Med. 31, 799–805 (2024).
Reichmann, H. et al. Life style and Parkinson’s disease. J. Neural Transm. 129, 1235–1245 (2022).
Holmberg, B. et al. Assenting to exposedness - meanings of receiving assisted bodily care in a nursing home as narrated by older persons. Scand. J. Caring Sci. 33, 868–877 (2019).
Zhang, X. et al. Zinc Deficiency Exacerbates Behavioral Impediments and Dopaminergic Neuron Degeneration in a Mouse Model of Parkinson Disease. J. Nutr. 153, 167–175 (2023).
Acknowledgements
This study was supported by Natural Science Foundation of Liaoning Province of China (Grant No. 2023-MS-190).
Author information
Authors and Affiliations
Contributions
Xiaohui Qiu: Conceptualization, Writing-Original Draft Ran Zhang: Conceptualization, Supervision, Writing-Review & Editing Yi Cheng: Writing-Original Draft Chengde Jin: Writing-Review & Editing Yushi Zhang: Writing-Review & Editing Ziqi Zhang: Conceptualization, Supervision, Writing-Review & Editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qiu, X., Zhang, R., Cheng, Y. et al. Oral health implications in Parkinson’s disease. npj Parkinsons Dis. 11, 73 (2025). https://doi.org/10.1038/s41531-025-00927-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-00927-y