Abstract
Idiopathic REM sleep behavior disorder (iRBD) is a prodromal stage of α-synucleinopathies including Parkinson’s disease (PD), yet its clinical heterogeneity remains underexplored. This study aimed to identify novel brain-clinical biotypes in iRBD by integrating structural MRI and clinical assessments. We included 172 patients with video-polysomnography-confirmed iRBD and 126 controls who underwent multimodal MRI and clinical evaluation. Similarity Network Fusion was used to integrate cortical thickness, surface area, subcortical volume, and clinical data, followed by spectral clustering to identify iRBD biotypes. Two distinct biotypes were identified: Biotype 1 showed widespread cortical-subcortical-cerebellar atrophy, functional hypoconnectivity, more motor and cognitive deficits with higher prodromal PD risk; Biotype 2 demonstrated increased surface area in limbic and parietal regions, cortical-cerebellar hyperconnectivity, and preserved neurocognitive function. These findings underscore the presence of distinct neurobiological subtypes in iRBD, highlighting the need for longitudinal monitoring to clarify their trajectories and implications for disease progression.
Similar content being viewed by others
Introduction
Idiopathic/isolated REM sleep behavior disorder (iRBD) is a distinct parasomnia characterized by the enactment of dreams and excessive electromyographic activity during REM sleep (REM sleep without atonia, RSWA)1. Recent evidence indicates that iRBD serves as a specific prodromal stage of α-synucleinopathies, such as Parkinson’s disease (PD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA), with over 90% of iRBD patients converting to α-synucleinopathies within 15 years2. Therefore, recognizing iRBD and its associated neurodegenerative biomarkers is crucial for identifying the prodromal stage of α-synucleinopathies and predicting disease progression3. Several biomarkers have been identified in iRBD that may potentially forecast a faster disease progression, including autonomic dysfunction, olfactory loss, color vision impairment, neurocognitive impairment, dopamine dysfunction, excessive daytime sleepiness, depression, and motor function abnormalities4.
Meanwhile, increasing evidence underscores PD, DLB, and MSA as heterogeneous conditions, with potential subtypes exhibiting distinct clinical features and underlying mechanisms5,6. For example, previous endeavors have aimed at delineating different subtypes of PD and DLB via clinical7,8 and imaging biomarkers9,10. However, the heterogeneity of α-synucleinopathies might manifest not only at disease onset but also during its prodromal stage, characterized by the initial neuroanatomical spread of α-synuclein aggregates11. Thus, identifying different biotypes of iRBD will be helpful for facilitating understanding of iRBD heterogeneity and, as well as optimizing the efficacy of neuroprotective interventions.
A recent study has identified two subtypes of iRBD based on clinical symptoms, with subtype 1 characterized by higher non-motor symptom burden and widespread reduction of cortical gray matter volume than subtype 212. However, the accuracy and reproducibility of these classification systems, grounded solely on clinical data, may have been limited13. An alternative and potentially more robust approach to categorizing patients with iRBD is to implement data integration techniques beyond using neuroimaging or behavioral/clinical features alone to identify brain-clinical biotypes14,15. This method offers the advantage of objectively capturing a diverse aspect of patient characteristics and exploring biological heterogeneity in vivo. By employing data-driven methods, researchers can achieve an unbiased detection of patient groups with similar brain-behavior profiles13.
In this study, we aim to integrate brain structural measures, including cortical thickness, surface area, and subcortical volume, and clinical assessments to identify subtypes in patients with iRBD, and to discover whether these biotypes will elucidate heterogeneities in brain structures and clinical characteristics in iRBD. To achieve this, we leveraged a novel multimodal data integration framework, similarity network fusion (SNF)16, which allows us to integrate structural brain features and clinical characteristics simultaneously in clustering, thus unveiling differential biotypes that are more readily interpretable in both clinical and neurobiological domains17. We hypothesized that there exist distinct iRBD biotypes that will be characterized by distinct neuroanatomic patterns and clinical profiles.
Results
Demographic characteristics of participants
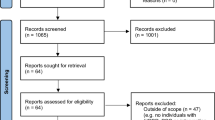
In this study, a total of 300 subjects were initially recruited. Two subjects were excluded due to poor image quality, resulting in a final cohort of 172 patients with iRBD and 126 control subjects. There is no significant difference (p = 0.62) in age between the RBD group (mean age: 67.86 ± 6.94 years) and controls (mean age: 66.07 ± 6.92 years). Additionally, the RBD group exhibited a higher proportion (p < 0.05) of male participants (77.3%) compared to the control group (55.6%).
Biotyping based on SNF
Based on the area under the curve for a cumulative distribution function (CDF) of consensus values (Fig. 1B), we focused on the subtyping results at clustering numbers C = 2, given that these Cs made the largest increases (ΔCDF > 0) of consensus degree. For this optimal solution, high stability of between-subject subgroups across bootstrapped samples was observed in the consensus matrices (Fig. 1A).
A consensus matrix of clustering results. 1000 iterations of bootstrapping (random sampling of 90% of participants) constructed a consensus matrix for a spectral clustering solution, which indicates how many times a pair of participants is clustered into the same group among 1000 iterations. B Determination of the optimal clustering solution. The optimal number of clusters was determined as C = 2, based on the largest Δ in the cumulative consensus distribution.
The number of participants classified into each of these two biotypes was Biotype 1: n = 86 and Biotype 2: n = 86. Tables 1 and S2 show the detailed demographic, clinical characteristics, and neurodegenerative markers of the two iRBD biotypes and controls. There was no significant difference in age, education, RBD onset age or symptom duration between the two biotypes. However, Biotype 1 had a significantly higher UPDRS-III score, lower HK-MoCA score, and higher prodromal PD risk score than Biotype 2, indicating more pronounced motor dysfunction, poorer cognitive functioning, and higher neurodegenerative risk in Biotype 1 relative to Biotype 2.
Neuroanatomic pattern of the 2 iRBD biotypes
Compared to controls, iRBD patients from both biotypes showed no significant differences in cortical thickness. Additionally, no significant differences were observed between Biotype 1 and Biotype 2 (Table S3).
In terms of cortical surface area, Biotype 1 patients demonstrated significantly smaller surface areas in 17 of 34 left-hemisphere regions of interest (ROIs) and 14 of 34 right-hemisphere ROIs, spanning frontal, temporal, and occipital regions. Conversely, Biotype 2 patients exhibited significantly larger surface areas in 7 of 34 left-hemisphere ROIs and 4 of 34 right-hemisphere ROIs, including limbic and occipital regions (Fig. 2 and Table S4). Additionally, Biotype 1 patients demonstrated more extensive surface area reductions than Biotype 2 patients across the limbic, frontal, temporal, and occipital regions (Fig. S1 and Table S4).
A Group difference in subcortical volume, cortical surface area and cortical volume between Biotype 1 patients and controls. B Group difference in cortical surface area and cortical volume between Biotype 2 patients and controls. The color bar represents t-statistics, with red indicating increase and blue indicating decrease. L/RH, left/right hemisphere.
Cortical and subcortical volume analyses revealed that Biotype 1 patients had significantly smaller volumes in 19 of 24 subcortical ROIs, whereas no differences in subcortical volume were observed in Biotype 2 patients. Additionally, patients with Biotype 1 exhibited significantly smaller cortical volumes in 5 of 34 left-hemisphere ROIs and 8 of 34 right-hemisphere ROIs, encompassing frontal, temporal, and parietal regions relative to controls. In contrast, Biotype 2 patients demonstrated increased volume solely in the right inferior parietal cortex (Fig. 2 and Table S5–S6). Furthermore, Biotype 1 patients showed more extensive volume reductions than Biotype 2 patients across the subcortical nuclei, as well as the limbic, frontal, temporal, and occipital regions (Fig. S1 and Table S5–S6).
All the above results survived further Bonferroni multiple testing correction. In patients with Biotype 1, the relationship between cortical/subcortical matrices and clinical symptoms is intricate. The interplay is highlighted by the association of decreased surface area and volume with various clinical scores, indicating a multifaceted impact on symptomatology (Fig. 3). While Biotype 2 patients exhibit a clearer trend, as increased surface area and volume were mainly associated with better cognitive function (Fig. 3).
Only significant results are displayed, with the color indicating the corresponding r-values. lh left hemisphere, rh right hemisphere, CC cingulate cortex. RBDQ RBD questionnaire, MoCA Montreal Cognitive Assessment, SCOPA-AUT Scales for Outcomes in Parkinson’s Disease-Autonomic, HADS Hospital Anxiety and Depression Scale, OIT Olfactory Identification Test, PPD prodromal Parkinson’s disease, LR Likelihood ratio.
Functional connectivity of the 2 biotypes
When compared to controls, iRBD patients with Biotype 1 predominantly exhibited extensive cortical-subcortical-cerebellar hypoconnectivity, along with hyperconnectivity between the cerebellum and sensorimotor cortex. In contrast, Biotype 2 patients primarily demonstrated cerebellar-cortical hyperconnectivity, accompanied by scattered cortical-cerebellar hypoconnectivity (Fig. 4). Additionally, Biotype 1 patients also demonstrated pronounced cortical-subcortical-cerebellar hypoconnectivity compared to Biotype 2 patients (Fig. S1). Furthermore, the additional supplementary FC analysis using the DK cortical and aseg subcortical atlases reaffirmed the original findings of Biotype 1, demonstrating widespread cortical-subcortical hypoconnectivity (Fig. S2). However, no statistically significant FC changes were observed in Biotype 2.
Discussion
In this study, we identified two distinct biotypes in patients with iRBD through a comprehensive SNF approach that integrated multiple structural imaging phenotypes and clinical measures. Our findings were supportive of two distinct neuroanatomic phenotypes within iRBD patients, each exhibiting unique characteristics compared to control subjects. Notably, patients classified under Biotype 1 displayed cortical and subcortical atrophy and cortical-subcortical-cerebellar hypoconnectivity, while those in Biotype 2 exhibited relative cortical volume increase and mainly cortical-cerebellar hyperconnectivity. The most notable discrepancies in symptomologies between the two biotypes were the significantly more prominent motor dysfunction and lower cognitive functioning in Biotype 1.
Subcortical volume reductions are also observed in Biotype 1 patients with iRBD compared to controls. Consistent findings across previous studies highlight reduced volumes in key subcortical regions such as the putamen, pallidum, and caudate in individuals with iRBD18,19,20. These findings correspond with observations of presynaptic dopaminergic dysfunction in dopamine transporter single-photon emission computed tomography studies21. Brainstem volume reduction has been identified, suggesting an underlying dysfunction in the nuclei that modulate REM sleep muscle tone22. Furthermore, patients in Biotype 1 also exhibit cortical atrophy, evidenced by decreased surface area and volume reduction across various cortical regions, especially limbic, temporal, and parietal areas. Previous studies support these findings, showing volume decreases in frontal20,23,24, cingulate23,25, occipital and parietal20, and temporal regions20,25 in patients with iRBD. Cortical atrophy likely reflects a loss of neuronal integrity, which is typical of neurodegeneration.
On the other hand, our study found that Biotype 2 patients did not have significant differences in subcortical volume compared to controls. Furthermore, Biotype 2 patients show cortical volume increase, with increased surface area in limbic regions and volume in the right inferior parietal gyrus. A multicenter study previously identified increased surface area in the inferior temporal and parahippocampal regions in iRBD patient population26, albeit there was no further elaboration on this intriguing phenomenon. Strictly speaking, cortical volume increase does not reflect neurogenesis, a rare event in adult brains outside specific areas like the hippocampus, subventricular zone, and olfactory bulb, but it is more likely part of a complex reactive process27. Increased gray matter volume may represent adaptive plasticity, such as cerebral edema, reactive gliosis, and increased neuronal branching, serving to temporarily compensate or mask underlying pathology28. Some studies discussed brain compensation during the early stages of neurodegenerative conditions like Alzheimer’s disease (AD) and Huntington’s disease29,30,31, such that a greater gray matter volume was protective against clinical deterioration, supporting the role of brain reserve. Prior research also highlights the association between brain volume and functional reserve markers in PD and other neurodegenerative diseases32. The positive association between increased surface area and cognitive functioning in Biotype 2 also suggests that structural variations may aid functional maintenance despite underlying pathology. Thus, enhancing brain reserve might potentially alleviate symptoms and slow the progression of synucleinopathies. The neuronal mechanisms underlying potential compensation are complex, necessitating further longitudinal data and intervention studies to validate the compensation hypothesis29.
In this study, no significant differences in cortical thickness were observed between the two biotypes, as well as between iRBD and the control group. It is proposed that the mechanisms governing the horizontal and vertical development of the cerebral cortex might operate independently, influencing cortical surface area and thickness separately33. Gray matter volume is a composite of these indices, thus reflecting both traits34. Previous research indicated cortical thinning in several regions among patients with iRBD compared to healthy controls, such as the lingual gyrus18, fusiform gyrus18,24, lateral occipital cortex18,35, orbitofrontal, dorsolateral frontal, and cingulate cortex19. Cortical and subcortical atrophy in iRBD is more severe and extensive in patients who also have mild cognitive impairment36,37. Though reduced surface area is suggested to be a major factor contributing to volume reduction38, few studies have investigated surface area changes in individuals with iRBD or cognitive decline39. Future longitudinal studies are warranted to explore whether surface area alterations precede cortical thickness changes in RBD.
Both biotypes exhibit mixed patterns of functional connectivity alterations compared to controls. Biotype 1 patients primarily demonstrate widespread cortical-subcortical-cerebellar hypoconnectivity with limited cerebellar-sensorimotor hyperconnectivity. In contrast, Biotype 2 patients display cortical-cerebellar hyperconnectivity with minimal cortical and cerebellar hypoconnectivity. Similarly, distinct neurodegenerative diseases manifest different FC patterns. For instance, AD consistently exhibits reduced connectivity in the default mode network, correlating with dementia severity40. Our previous meta-analysis of FC studies in α-synucleinopathies revealed widespread abnormal crosstalk across brain networks with both hypo- and hyperconnectivity41. Hypoconnectivity, indicative of internetwork disruption, may underlie functional disconnection and pathology spread across interconnected networks. Hyperconnectivity (that is, increased synchrony of spontaneous BOLD fluctuations) is also a common finding in resting-state fMRI studies across a range of neurodegenerative diseases42. The exact mechanism of hyperconnectivity remains unclear, with some activation of existing network regions was proposed as a compensatory strategy. Notably, both biotypes exhibit some possibly functional compensation, with Biotype 2 showing predominance. This aligns with the scaffolding theory of aging, suggesting increased activation as an adaptive response using compensatory scaffolding to counteract neural decline by utilizing alternative neural circuits for cognitive function maintenance43. Other compensation models propose augmented activation within existing networks as contributory factors44.
Pathologically, DLB and PD are thought to arise from the propagation and accumulation of misfolded α-synuclein in the brain45. Braak et al.‘s hypothesis suggests that pathological α-synuclein aggregates and dysfunction initiate in the lower brainstem and ascend to the midbrain and cerebral cortex, potentially leading to iRBD and subsequent phenoconversion to PD or DLB46,47. While there are two proposed subtypes of α-synuclein pathology progression in PD: “brain-first” (starting in the brain and spreading to the peripheral system) and “body-first” (originating in the enteric or peripheral autonomic nervous system and spreading to the brain), with iRBD being suggested as an early indicator of the “body-first” subtype48. In addition, an emerging concept redefines PD and DLB from a biological definition based on the detection of pathological α-synuclein49. Our findings introduce a novel biotyping framework for iRBD based on neuroimaging-clinical integration via SNF analysis. Specifically, Biotype 1 aligns with typical neurodegeneration patterns, while Biotype 2 exhibits an ‘atypical’ pattern characterized by relative brain volume preservation or even increases, suggestive of a potential compensatory reserve. The observed gradient in prodromal PD risk (Biotype 1 > Biotype 2 > Controls) further supports the validity of this biotypic stratification and underscores its potential for refining prognostic models. These findings also raise an important question: Could distinct biotypes reflect differential responses to α-synuclein pathology or represent divergent disease progression phenotypes? Addressing this question through longitudinal studies will be essential to further elucidate the clinical and biological significance of these biotypes.
This study has some limitations. First, the absence of a validation dataset underscores the need for future research with larger cohorts to validate current findings. Second, the cross-sectional study inherently limits our ability to predict the phenoconversion to Parkinsonism-first or dementia-first trajectories, so longitudinal studies are warranted to address this gap50. In addition, not all participants were definitively clustered into specific biotypes, which is reasonable given the inherent complexity of the population under study. Therefore, the identified biotypes may serve as an initial step in addressing disease heterogeneity, based on neuroanatomic and clinical characteristics. Future investigations should expand input features to include clinical, genetic, environmental, and additional neuroimaging factors for a more comprehensive understanding. Extensive research on clinical heterogeneity, coupled with advances in biological markers, will guide the path towards precision medicine, enabling targeted and effective interventions.
In conclusion, we identified two distinct biotypes of iRBD, each with unique clinical, neuroanatomic, and functional connectivity features, which suggest distinct neurobiological subtypes in iRBD. Longitudinal monitoring of these biotypes and integrating with other omics data will be essential to elucidate their trajectories and implications for disease progression. Our biotyping framework provides a testable model for future research to investigate differential progression trajectories and potentially inform more targeted therapeutic development for iRBD patients.
Methods
Study design and participants
This is a cross-sectional study employing data-driven clustering to identify biotypes within an iRBD cohort, with secondary comparisons to controls. Patients with iRBD were recruited from our ongoing RBD cohort in the Li Chiu Kong Family Sleep Assessment Unit at Shatin Hospital, Shatin, Hong Kong51,52,53, from September 2021 to November 2023. Control participants, comprised of neurologically healthy individuals, were recruited from both local community and the Sleep Assessment Unit.
Diagnosis of iRBD among patients was confirmed via video-polysomnography assessment, adhering to the diagnostic criteria of the International Classification of Sleep Disorders, 3rd edition1. The exclusion criteria for all subjects included: RBD features related to narcolepsy and other pre-existing neurodegenerative disorders; and presence of MRI contraindications (e.g., metal implants or claustrophobia). Ethical approval was obtained from the Clinical Research Ethics Committee of the Joint Chinese University of Hong Kong and New Territories East Cluster, with a reference number of 2021.277. All individuals provided written informed consent.
Questionnaires and clinical assessments
A comprehensive questionnaire was administered to all participants.
-
1.
General questionnaire: A structured questionnaire captured socio-demographic information, lifestyle habits (e.g., tea, coffee, alcohol consumption, smoking status), sleep-wake patterns, and common sleep symptoms such as insomnia.
-
2.
Excessive daytime sleepiness: The Epworth Sleepiness Scale (ESS) was utilized to quantify excessive daytime sleepiness.
-
3.
Insomnia severity: Severity of insomnia symptoms was assessed using the Insomnia Severity Index (ISI).
-
4.
Anxiety and depression symptoms: The Hospital Anxiety and Depression Scale (HADS) was employed to evaluate the severity of depressive and anxiety symptoms.
-
5.
Autonomic dysfunction symptoms: Symptoms such as constipation, erectile dysfunction, urinary dysfunction, and symptomatic hypotension were evaluated using the Scales for Outcomes in Parkinson’s Disease-Autonomic (SCOPA-AUT).
-
6.
Severity of RBD symptoms: the clinical aspects and severity of RBD features were assessed by RBD questionnaire–Hong Kong (RBDQ-HK), a locally designed and validated questionnaire comprising 13 questions54. It contains two components: (1) dream-related factors (factor 1) and (2) behavioral factors (factor 2).
In addition, participants underwent a series of clinical, neuropsychiatric, neurocognitive, and autonomic function assessments:
-
1.
Motor function: The Unified Parkinson’s Disease Rating Scale part III (UPDRS-III)55 measured motor function.
-
2.
Cognitive function: The Hong Kong version of the Montreal Cognitive Assessment (HK-MoCA)56 was used to assess global cognitive function.
-
3.
Psychiatric disorders: Lifetime psychiatric disorders were evaluated via structured interviews based on DSM-IV criteria and supplemented by clinical records.
-
4.
Sleep disorders: Diagnostic Interview for Sleep Patterns and Disorders (DISP)57, a structured diagnostic interview, was used to further evaluate RBD symptoms, sleep patterns, and other sleep disorders.
-
5.
Olfactory function: The Olfactory Identification Test (OIT)58 was used to assess olfactory function.
-
6.
Color vision discrimination: The Farmsworth-Munsell 100 hue test was conducted to assess color vision discrimination59.
-
7.
Prodromal PD likelihood: The 2019 version of Movement Disorder Society (MDS) criteria for prodromal PD60 was used to determine the overall likelihood ratio (LR) for prodromal PD, with the likelihood ratio being transformed using Log base 10.
MRI acquisition and processing
MRI examinations were performed using a whole-body 3.0 T MRI scanner (MAGNETOM Prisma; Siemens AG, Munich, Germany) equipped with a 64-channel head coil at the Prince of Wales Hospital, Hong Kong. Participants were comfortably positioned in the coil and provided with soft earplugs to mitigate external noise interference. Additional stabilization of the head was ensured using foam pads to minimize potential motion artifacts of the participant. High-resolution sagittal T1-weighted anatomical images were acquired utilizing a sagittal 3D T1-weighted Magnetization Prepared Rapid Gradient Echo (MPRAGE) sequence with the following parameters: repetition time (TR) = 2300 ms, echo time (TE) = 3.06 ms, flip angle = 9°, and voxel size = 1 mm³ isotropic. Resting-state functional MRI (rsfMRI) images were obtained using a Gradient-Recalled Echo-Planar Imaging pulse sequence with TR = 1500 ms, TE = 30 ms, flip angle = 70°, and voxel size = 2 × 2 × 3 mm³. During rsfMRI scanning, participants were instructed to relax with their eyes closed, ensuring that they remained awake and motionless throughout the procedure.
T1-weighted images were processed using FreeSurfer software (version 7.1.0) on the same workstation, employing its fully automatic pipeline61. For each subject, FreeSurfer parcellated 34 cortical ROIs per hemisphere based on the Desikan-Killiany atlas62 and 24 subcortical ROIs. Regional cortical thickness, cortical surface area, and cortical/subcortical volume were extracted.
Resting-state fMRI data analyses were conducted using Statistical Parametric Mapping (SPM, https://www.fil.ion.ucl.ac.uk/spm/) version 12 and the CONN toolbox63. These software packages offer methods to mitigate head motion artifacts and accurately identify correlated and anti-correlated networks. To address potential spurious correlations in resting-state networks, preprocessing and cleaning of the fMRI signal were performed. The Artifact Detection Toolbox in CONN was employed to identify problematic time points characterized by head displacement exceeding 0.5 mm or global mean intensity deviating more than 3 standard deviations from the mean image intensity. Runs with over 30% outlier images were excluded from analysis, although no participants were excluded due to excessive motion. The first-level general linear model (GLM) incorporated participant motion parameters, including rotation and translation parameters and their derivatives, as well as artifactual covariates. Anatomical volumes were segmented into gray matter, white matter, and cerebrospinal fluid areas, with resulting masks eroded to minimize partial volume effects. Noise-signal for anatomical CompCor correction was extracted from the union of eroded white matter and ventricle masks, transformed to native functional space. Six CompCor parameters, Friston-24 motion parameters, and linear trend were regressed from the timeseries data using a GLM. The resulting residual blood-oxygen-level-dependent (BOLD) timeseries underwent band-pass filtering (0.008 Hz < f < 0.09 Hz). We predefined 132 ROIs in the CONN toolbox based on the Harvard–Oxford cortical & subcortical structural atlases (https://neurovault.org/collections/262/) and AAL atlas cerebellar areas64. Additionally, we conducted a supplementary functional connectivity analysis using the same atlas for the structural analyses, i.e., Desikan-Killiany cortical atlas and the aseg subcortical atlas.
Pearson’s correlation coefficients were calculated to determine the correlation between the timeseries of each pair of regions. Subsequently, Fisher’s r-to-z transformation was applied to correlation coefficients.
Similarity network fusion and spectral clustering
Biotyping was performed using similarity network fusion (SNF), a method for integrating multiple data sources into one comprehensive graph16. This graph captures the relationship between samples by combining independent similarity networks generated from each data source using a K-nearest neighbors weighted kernel. Through an iterative process of combining these networks via a non-linear message passing protocol, SNF creates a final network that incorporates information from all data sources. This integrated network can then be used for various analytical techniques, such as clustering or graph analysis, for further exploration and interpretation. SNF has demonstrated effectiveness in unraveling heterogeneity within neuropsychiatric populations14,65. SNF was used to integrate structural imaging (cortical thickness, surface area, and subcortical volume) and clinical data types (see Table S1 listing all SNF input features). The SNF algorithm was conducted in Matlab_R2023a, which has been previously described16 (http://compbio.cs.toronto.edu/SNF/).
Before applying SNF, imaging features were preprocessed by regressing out age, sex, and handedness (and total intracranial volume for surface area and volume) to account for potential confounders. Specifically, for each imaging feature Y (e.g., volume and surface area), the following regression model was applied:
The adjusted feature values used in subsequent analyses were the residuals (ϵ) from this model. Additionally, each input feature for SNF was normalized using z-scoring. Biotyping using SNF involved the following steps:
-
1.
Calculation of a sample similarity network for each data type: Four between-subjects distance matrices were computed for cortical thickness, surface area, subcortical volume, and clinical symptoms separately. The distance matrix was calculated consistently using the ‘cosine similarity’ kernel to generate between-subjects affinity matrices, with each cell representing the similarity of distance profiles between two participants. The scaled exponential similarity kernel was used for this calculation.
-
2.
Integration of these networks into a SNF-combined similarity network: The resulting four affinity matrices were input to SNF to create a single fused affinity matrix. Parameters such as the number of nearest neighbors (k), the number of iterations (T), and hyperparameters related to feature scaling (μ) were set as recommended in the original paper (k = 30, T = 20, μ = 0.5)16 to ensure reproducibility of biotype findings.
-
3.
Identification of homogeneous biotypes: Spectral clustering was used to identify biotypes by inputting the single fused affinity matrix into a spectral clustering algorithm. Following the methodology outlined in the original work of SNF16, we utilized a traditional spectral method that combines MinCut and equipartitioning to minimize the objective function using a normalized Laplacian matrix66. To ensure more reproducible and outlier-robust biotype findings, we iteratively performed the SNF process 1000 times based on bootstrapped samples (resampling 90% of cases without replacement) and created a consensus matrix with varying clustering numbers (C) from 2 to 20. Each cell in the consensus matrix indicates the consistency of grouping a pair of participants together across 1000 iterations at a specific clustering number (2–20).
-
4.
Clustering solution evaluation: The SNF process was iterated 1000 times based on bootstrapped samples to construct a consensus matrix. By varying the clustering number (C) from 2 to 20, the degree of consensus for each clustering solution was evaluated using the cumulative consensus distribution approach. The clustering solution with the highest stability across different sampled cases was selected.
The illustrative example of SNF steps was shown in Fig. 5.
A Example representation of cortical thickness, surface area, subcortical volume, and clinical datasets for the same cohort of patients. B Patient-by-patient similarity networks, equivalent to the patient-by-patient data. Patients are represented by nodes, and patients’ pairwise similarities are represented by edges. C The iterative network fusion results in convergence to the final fused network. Edge color indicates which data type has contributed to the given similarity.
Statistical analysis
All acquired demographic and clinical data were processed and analyzed using standard statistical analysis methods with SPSS 27.0 (Chicago, IL, USA) and R project Version 4.3.2. Descriptive data will be presented as means ± SD or frequencies (%). Categorical data will be analyzed using chi-square or Fisher’s exact probability test. Continuous data will be compared among groups using Analysis of covariance (ANCOVA; age and sex as covariates) and Kruskal-Wallis tests. For post-hoc analysis, the Bonferroni test will be used to account for the multiple comparison effect. A p < 0.05 is considered statistically significant for all analyses.
To illustrate the neuroanatomic pattern in different biotypes, the cortical thickness, surface area, cortical/subcortical volume were compared among the 2 biotypes and controls using ANCOVA tests (age, sex, and handedness as covariates for all measurements and total intracranial volume as extra covariate for surface area and volume measurement). We applied region-specific corrections based on the number of comparisons within each anatomical domain67. For cortical measurements, a p ≤ 0.001 is considered statistical significance to correct multiple comparisons of 34 regions on each hemisphere, aligns with Bonferroni correction for 34 comparisons (0.05/34 ≈ 0.001). For subcortical volume, a p < 0.005 is considered statistical significance to correct multiple comparisons of 10 subcortical regions (0.05/10 = 0.005) on each hemisphere. For post-hoc between-group analysis, the Bonferroni test will be used to account for the multiple comparison effect. Functional connectivity analyses were thresholded at a connection-level p < 0.001, with multiple comparisons corrected by false discovery rate at p < 0.05.
Pearson correlation or Spearman rank correlation analyses were conducted separately for each biotype to identify neuroanatomic alterations (regions with significant changes in biotype vs. controls) that were significantly correlated (p < 0.05) with clinical symptomatology. The imaging features consisted of aforementioned processed data from regions showing significant differences between biotypes and controls. Clinical scores encompassed various measures, including RBDQ-HK (factor 1, factor 2, and total scores), UPDRS-III total score, HK-MoCA total score, HADS (depression, anxiety, and total scores), SCOPA-AUT total score, Color Hue Test score, OIT score, and MDS- prodromal PD total LR.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Abbreviations
- AD:
-
Alzeimer’s disease
- ANCOVA:
-
Analysis of covariance
- BOLD:
-
Blood-oxygen-level-dependent
- CDF:
-
Cumulative distribution function
- DISP:
-
Diagnostic Interview for Sleep Patterns and Disorders
- DLB:
-
Dementia with Lewy bodies
- DSM-IV:
-
Diagnostic and Statistical Manual of Mental Disorders, fourth edition
- ESS:
-
Epworth Sleepiness Scale
- FC:
-
Functional connectivity
- FDR:
-
False discovery rate
- GLM:
-
General linear model
- HADS:
-
Hospital Anxiety and Depression Scale
- HK-MoCA:
-
The Hong Kong version of the Montreal Cognitive Assessment
- iRBD:
-
idiopathic/isolated REM sleep behavior disorder
- ISI:
-
Insomnia Severity Index
- LR:
-
Likelihood ratio
- MDS:
-
Movement Disorder Criteria
- MPRAGE:
-
Magnetization Prepared Rapid Gradient Echo
- MRI:
-
Magnetic Resonance Imaging
- MSA:
-
Multiple system atrophy
- OIT:
-
Olfactory Identification Test
- PD:
-
Parkinson’s disease
- RBDQ-HK:
-
RBD questionnaire-Hong Kong
- ROIs:
-
Regions of interest
- rsfMRI:
-
Resting-state functional MRI
- RSWA:
-
REM sleep without atonia
- SNF:
-
Similarity network fusion
- SCOPA-AUT:
-
Scales for Outcomes in Parkinson’s Disease-Autonomic
- SPM:
-
Statistical Parametric Mapping
- TIV:
-
Total intracranial volume
- TR:
-
Repetition time
- TE:
-
Echo time
- UPDRS-III:
-
The Unified Parkinson’s Disease Rating Scale part III
- v-PSG:
-
video-Polysomnography
References
American Academy of Sleep Medicine. International Classification of Sleep Disorders, third edition, text revision (ICSD-3-TR). Am. Acad. Sleep Med. (2023).
Iranzo, A. et al. Neurodegenerative disorder risk in idiopathic REM sleep behavior disorder: study in 174 patients. PLoS ONE 9, e89741 (2014).
Miglis, M. G. et al. Biomarkers of conversion to α-synucleinopathy in isolated rapid-eye-movement sleep behaviour disorder. Lancet Neurol. 20, 671–684 (2021).
Postuma, R. B. et al. Risk and predictors of dementia and parkinsonism in idiopathic REM sleep behaviour disorder: a multicentre study. Brain 142, 744–759 (2019).
Greenland, J. C., Williams-Gray, C. H. & Barker, R. A. The clinical heterogeneity of Parkinson’s disease and its therapeutic implications. Eur. J. Neurosci. 49, 328–338 (2019).
Ferman, T. J. et al. Subtypes of dementia with Lewy bodies are associated with α-synuclein and tau distribution. Neurology 95, e155–e165 (2020).
Fereshtehnejad, S. M. et al. New clinical subtypes of parkinson disease and their longitudinal progression: a prospective cohort comparison with other phenotypes. JAMA Neurol. 72, 863–873 (2015).
Morenas-Rodríguez, E. et al. Clinical subtypes of dementia with lewy bodies based on the initial clinical presentation. J. Alzheimer’s Dis. 64, 505–513 (2018).
Wang, L. et al. Association of specific biotypes in patients with Parkinson disease and disease progression. Neurology 95, e1445–e1460 (2020).
Inguanzo, A. et al. MRI data-driven clustering reveals different subtypes of Dementia with Lewy bodies. npj Parkinson’s Dis. 9, 5 (2023).
Berg, D. et al. Prodromal Parkinson disease subtypes - key to understanding heterogeneity. Nat. Rev. Neurol. 17, 349–361 (2021).
Seger, A. et al. Clinical subtypes in patients with isolated REM sleep behaviour disorder. npj Parkinson’s Dis. 9, 155 (2023).
Feczko, E. et al. The heterogeneity problem: approaches to identify psychiatric subtypes. Trends Cogn. Sci. 23, 584–601 (2019).
Stefanik, L. et al. Brain-behavior participant similarity networks among youth and emerging adults with schizophrenia spectrum, autism spectrum, or bipolar disorder and matched controls. Neuropsychopharmacology 43, 1180–1188 (2018).
Jacobs, G. R. et al. Integration of brain and behavior measures for identification of data-driven groups cutting across children with ASD, ADHD, or OCD. Neuropsychopharmacology 46, 643–653 (2021).
Wang, B. et al. Similarity network fusion for aggregating data types on a genomic scale. Nat. methods 11, 333–337 (2014).
Hong, S.-J. et al. Decomposing complex links between the childhood environment and brain structure in school-aged youth. Dev. Cogn. Neurosci. 48, 100919 (2021).
Ellmore, T. M. et al. Reduced volume of the putamen in REM sleep behavior disorder patients. Parkinsonism Relat. Disord. 16, 645–649 (2010).
Rahayel, S. et al. Abnormal gray matter shape, thickness, and volume in the motor cortico-subcortical loop in idiopathic rapid eye movement sleep behavior disorder: association with clinical and motor features. Cereb. Cortex. 28, 658–671 (2018).
Chen, M. et al. Structural and functional brain alterations in patients with idiopathic rapid eye movement sleep behavior disorder. J. Neuroradiol. 49, 66–72 (2022).
Iranzo, A. et al. Dopamine transporter imaging deficit predicts early transition to synucleinopathy in idiopathic rapid eye movement sleep behavior disorder. Ann. Neurol. 82, 419–428 (2017).
Iranzo, A. The REM sleep circuit and how its impairment leads to REM sleep behavior disorder. Cell tissue Res. 373, 245–266 (2018).
Park, K. M., Lee, H.-J., Lee, B. I. & Kim, S. E. Alterations of the brain network in idiopathic rapid eye movement sleep behavior disorder: structural connectivity analysis. Sleep. Breath. 23, 587–593 (2019).
Rahayel, S. et al. Patterns of cortical thinning in idiopathic rapid eye movement sleep behavior disorder. Mov. Disord. 30, 680–687 (2015).
Li, G. et al. Altered structure and functional connectivity of the central autonomic network in idiopathic rapid eye movement sleep behaviour disorder. J. Sleep. Res. 30, e13136 (2021).
Rahayel, S. et al. Brain atrophy in prodromal synucleinopathy is shaped by structural connectivity and gene expression. Brain 145, 3162–3178 (2022).
Riddle D. R. Brain Aging: Models, Methods, and Mechanisms (Taylor & Francis, 2007).
Baril, A. A. et al. Gray matter hypertrophy and thickening with obstructive sleep apnea in middle-aged and older adults. Am. J. Respir. Crit. Care Med. 195, 1509–1518 (2017).
Gregory, S. et al. Operationalizing compensation over time in neurodegenerative disease. Brain 140, 1158–1165 (2017).
Gregory, S. et al. Testing a longitudinal compensation model in premanifest Huntington’s disease. Brain 141, 2156–2166 (2018).
Guo, L. H., Alexopoulos, P., Wagenpfeil, S., Kurz, A. & Perneczky, R. Brain size and the compensation of Alzheimer’s disease symptoms: a longitudinal cohort study. Alzheimers Dement. 9, 580–586 (2013).
Gregory, S., Long, J. D., Tabrizi, S. J. & Rees, G. Measuring compensation in neurodegeneration using MRI. Curr. Opin. Neurol. 30, 380–387 (2017).
Geschwind, D. H. & Rakic, P. Cortical evolution: judge the brain by its cover. Neuron 80, 633–647 (2013).
Winkler, A. M. et al. Joint analysis of cortical area and thickness as a replacement for the analysis of the volume of the cerebral cortex. Cereb. Cortex. 28, 738–749 (2017).
Pereira, J. B. et al. Cortical thinning in patients with REM sleep behavior disorder is associated with clinical progression. NPJ Parkinsons Dis. 5, 7 (2019).
Rahayel, S. et al. Cortical and subcortical gray matter bases of cognitive deficits in REM sleep behavior disorder. Neurology 90, e1759–e1770 (2018).
Rémillard-Pelchat, D. et al. Comprehensive analysis of brain volume in REM sleep behavior disorder with mild cognitive impairment. J. Parkinsons Dis. 12, 229–241 (2022).
Risacher, S. L. et al. Alzheimer disease brain atrophy subtypes are associated with cognition and rate of decline. Neurology 89, 2176–2186 (2017).
Hogstrom, L. J., Westlye, L. T., Walhovd, K. B. & Fjell, A. M. The structure of the cerebral cortex across adult life: age-related patterns of surface area, thickness, and gyrification. Cereb. cortex. 23, 2521–2530 (2013).
Brier, M. R. et al. Loss of intranetwork and internetwork resting state functional connections with Alzheimer’s disease progression. J. Neurosci. 32, 8890–8899 (2012).
Tang, S. et al. Large-scale network dysfunction in α-Synucleinopathy: a meta-analysis of resting-state functional connectivity. EBioMedicine 77, 103915 (2022).
Pievani, M., Filippini, N., van den Heuvel, M. P., Cappa, S. F. & Frisoni, G. B. Brain connectivity in neurodegenerative diseases–from phenotype to proteinopathy. Nat. Rev. Neurol. 10, 620–633 (2014).
Park, D. C. & Reuter-Lorenz, P. The adaptive brain: aging and neurocognitive scaffolding. Annu Rev. Psychol. 60, 173–196 (2009).
Barulli, D. & Stern, Y. Efficiency, capacity, compensation, maintenance, plasticity: emerging concepts in cognitive reserve. Trends Cogn. Sci. 17, 502–509 (2013).
Peng, C., Gathagan, R. J. & Lee, V. M. Distinct α-Synuclein strains and implications for heterogeneity among α-Synucleinopathies. Neurobiol. Dis. 109, 209–218 (2018).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 24, 197–211 (2003).
Braak, H., Ghebremedhin, E., Rüb, U., Bratzke, H. & Del Tredici, K. Stages in the development of Parkinson’s disease-related pathology. Cell Tissue Res. 318, 121–134 (2004).
Horsager, J. et al. Brain-first versus body-first Parkinson’s disease: a multimodal imaging case-control study. Brain 143, 3077–3088 (2020).
Simuni, T. et al. A biological definition of neuronal α-synuclein disease: towards an integrated staging system for research. Lancet Neurol. 23, 178–190 (2024).
Wang, J. et al. Visuospatial dysfunction predicts dementia-first phenoconversion in isolated REM sleep behaviour disorder. J Neurol. Neurosurg. Psychiatry. 96, 76–84 (2024).
Liu, Y. et al. A case-control-family study of idiopathic rapid eye movement sleep behavior disorder. Ann. Neurol. 85, 582–592 (2019).
Wang, J. et al. Familial α-synucleinopathy spectrum features in patients with psychiatric REM sleep behaviour disorder. J. Neurol. Neurosurg. Psychiatry 94, 893–903 (2023).
Huang, B. et al. Gut microbiome dysbiosis across early Parkinson’s disease, REM sleep behavior disorder and their first-degree relatives. Nat. Commun. 14, 2501 (2023).
Li, S. X. et al. Validation of a new REM sleep behavior disorder questionnaire (RBDQ-HK). Sleep. Med. 11, 43–48 (2010).
Movement Disorder Society Task Force on Rating Scales for Parkinson's Disease. The Unified Parkinson’s disease rating scale (UPDRS): status and recommendations. Mov Disord. 18, 738–750 (2003).
Wong, A. et al. The validity, reliability and clinical utility of the Hong Kong Montreal Cognitive Assessment (HK-MoCA) in patients with cerebral small vessel disease. Dement Geriatr. Cogn. Disord. 28, 81–87 (2009).
Merikangas, K. R. et al. The structured diagnostic interview for sleep patterns and disorders: rationale and initial evaluation. Sleep. Med. 15, 530–535 (2014).
Chan, A., Tam, J., Murphy, C., Chiu, H. & Lam, L. Utility of olfactory identification test for diagnosing Chinese patients with Alzheimer’s disease. J. Clin. Exp. Neuropsychol. 24, 251–259 (2002).
Farnsworth, D. B. The Farnsworth-Munsell 100-hue and dichotomous tests for color vision*. J. Optical Soc. Am. 33, 568–578 (1943).
Heinzel, S. et al. Update of the MDS research criteria for prodromal Parkinson’s disease. Mov. Disord. 34, 1464–1470 (2019).
Fischl, B. et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33, 341–355 (2002).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31, 968–980 (2006).
Whitfield-Gabrieli, S. & Nieto-Castanon, A. Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect. 2, 125–141 (2012).
Tzourio-Mazoyer, N. et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. NeuroImage 15, 273–289 (2002).
Markello, R. D. et al. Multimodal phenotypic axes of Parkinson’s disease. NPJ Parkinsons Dis. 7, 6 (2021).
Ng, A. Y., Jordan, M. I. & Weiss, Y. On spectral clustering: analysis and an algorithm. In Proc. of the 14th International Conference on Neural Information Processing Systems: Natural and Synthetic, 849–856 (ACM, 2001).
Laansma, M. A. et al. International multicenter analysis of brain structure across clinical stages of Parkinson’s disease. Mov. Disord. 36, 2583–2594 (2021).
Acknowledgements
This study was supported by the Health and Medical Research Fund (10210686) of the Food and Health Bureau of Hong Kong. The authors would like to thank all the participants, research staff, and colleagues from the Li Chiu Kong Family Sleep Assessment Unit and The Gerald Choa Neuroscience Centre MRI Core Facility for the study.
Author information
Authors and Affiliations
Contributions
S.T. and Y.K.W. contributed to the conception and design of the study. S.T., B.H., Y.L.W., J.W., L.Z., S.Y.G., and Y.H.Y. contributed to the acquisition and analysis of data. S.T. drafted the manuscript, B.H., Y.L.W., Y.P.L., J.W., L.Z., S.Y.G., Y.H.Y., J.W.Y.C., S.W.H.C., W.C.W.C., J.A., J.F.G. and Y.K.W. reviewed the manuscript and provided comments. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Prof. Yun Kwok Wing received personal fees from Eisai Co., Ltd, for delivering a lecture, and sponsorship from Lundbeck HK Ltd and Aculys Pharma, Inc. Dr. Joey Wing Yan Chan received personal fee from Eisai Co., Ltd, and travel support from Lundbeck HK limited for overseas conference. The remaining authors declare that the study was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tang, S., Huang, B., Wang, Y. et al. Brain-clinical biotyping in patients with idiopathic REM sleep behavior disorder. npj Parkinsons Dis. 11, 156 (2025). https://doi.org/10.1038/s41531-025-01012-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-01012-0