Abstract
Increasing evidence supported a link between peripheral inflammation and Parkinson’s disease (PD). However, the role of peripheral inflammation in the progression of PD clinical symptoms remained unclear. This study evaluates peripheral inflammation using serum differential leukocyte counts and their derived ratios. A total of 170 PD patients were retrospectively enrolled from Guangdong Provincial People’s Hospital (GDPH) and 68 from PPMI. Partial correlation analysis showed that neutrophil-to-lymphocyte ratio (NLR) negatively correlated with MoCA in GDPH but not in PPMI. Moreover, peripheral inflammation was shown to correlate with white matter integrity. The result of the longitudinal analysis showed that higher baseline NLR predicted worsening in letter number sequencing (LNS) score. Path analysis indicated that white matter integrity significantly mediated the relationship between NLR and cognitive change in the LNS score from Year 5 to baseline. Peripheral inflammation is associated with global cognition and white matter integrity in PD and predicts cognitive decline.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is a common neurodegenerative movement disorder pathologically characterized by abnormal aggregation of α-synuclein (α-Syn), the loss of dopaminergic neurons in substantial nigra, and chronic neuroinflammation1. Mounting evidence supported that excessive neuroinflammation could damage neurons and aggravate α-Syn deposition2. However, the etiology of neuroinflammation in PD was inclusive. Recently, in addition to resident immune cells, such as microglia and astrocytes, the peripheral immune cells have also gained widespread attention3. Indeed, bidirectional communication between central and peripheral inflammation was identified and demonstrated to be essential for maintaining brain homeostasis2. In particular, the cycling immune cells activated in peripheral system could infiltrate into central nervous system through the blood-CSF, blood-pia mater, blood-brain barrier (BBB), and meningeal lymphatic vessels4, secret various inflammatory cytokines, and subsequently induce neuroinflammation5. Despite this, the exact role of peripheral inflammation in PD remained unclear.
Peripheral inflammation involves dysfunction in innate and adaptive immune systems, which are mainly composed of various cycling immune cells, including monocytes, macrophages, neutrophils, dendritic cells, natural killer cells, T cells, and B cells. In this regard, the differential peripheral white blood cell (WBC) counts and their ratios, such as neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), system immune-inflammation Index (SII), and lymphocyte-to-monocyte ratio (LMR) are considered sensitive biomarkers assessing the degree of peripheral inflammation6. Moreover, serum albumin and platelet count were closely related to peripheral inflammation, and their ratio, platelet-to-albumin ratio (PAR), is recognized as a potential marker reflecting peripheral inflammatory state7.
Our previous cross-sectional study found that SII was negatively correlated with activity of daily living score8. Considering that PD was a muti-system disorder, and α-Syn deposition appeared outside of central nervous system in prodromal period1, peripheral inflammation was therefore postulated to be involved in PD initiation. A prospective cohort study including 161,968 participants with a median follow-up of 9.66 years showed that baseline serum lymphocytes, monocytes, platelets and LMR were inversely correlated with the risk of PD development, while elevated NLR and SII increased PD risk6. However, whether peripheral inflammation participates in PD disease progression and how much influence it could exert remained unknown. Previous studies found that baseline CXCL1 is associated with PD motor progression9, and a composite marker mainly based on interleukin (IL)-2 and IL-6 could predict progression of non-motor symptoms10. Nevertheless, most of them focused on immune mediators and global cognition, instead of immune cells and specific cognitive domains. Moreover, another study investigating the longitudinal association between serum C-reactive protein (CRP) and PD symptoms progression reported negative result11, suggesting there existed high inconsistency regarding longitudinal follow-up associations between peripheral inflammation markers and progression of clinical symptoms.
While infiltrating into central nervous system, peripheral inflammatory cells were shown to exert detrimental effect on BBB, which may trigger white matter damage12. Of note, severe white matter injury could increase the risk of long-term Parkinsonism13 and PD cognitive impairment14, which was also associated with PD motor and nonmotor dysfunction15. Based on these, we speculated that white matter integrity may be involved in the effect of peripheral inflammation on PD clinical symptoms progression. In particular, the white matter integrity was evaluated by diffusion tensor imaging (DTI) measures, such as fractional anisotropy (FA) and mean diffusivity (MD).
In this study, we extended our prior work by investigating (1) whether baseline periphery markers based on serum leukocyte are associated with clinical symptoms progression; and (2) whether white matter integrity measured by neuroimaging mediates the effect of peripheral inflammation on clinical progression. To test these, we retrospectively analyzed cross-sectional data from Guangdong Provincial People’s Hospital (GDPH) and baseline data from Parkinson’s Progression Marker Initiative (PPMI). Meanwhile, the longitudinal data from PPMI was also analyzed using linear mixed model.
Results
The demographics and clinical features of enrolled patients
A total of 170 patients with PD were included in the cross-sectional study, and their clinical features were summarized in Supplementary Table 1. Except for MDS-UPDRS III and CRP, the proportion of missing value was less than 15% for other variables. Some patients with PD only underwent clinical assessment in either “ON” or “OFF” stage. Moreover, the detection method of CRP varied from immune-turbidimetry assay, dry chemistry method and immunochromatographic assay. To avoid potential bias, we unified the measurement method using immune-turbidimetry assay. As for the longitudinal study, 68 participants were eligible, and their demographic information and clinical features were summarized in Supplementary Table 2. In brief, the mean age at baseline was 60.79 (8.74) years old. The median disease duration and education were 3.00 (2.00, 5.00) months and 16.00 (14.00, 18.00) years respectively. Most patients were male (66.18%). The LEDD was 0 at baseline and incrementally increased as time went by.
Partial correlation between clinical symptoms and peripheral inflammation markers
In the GDPH cohort, partial correlation analysis showed that NLR appeared to be negatively correlated with MoCA (P < 0.05), PLR positively with HAMD (P < 0.05), SII positively with HAMA, while inversely with MoCA (P < 0.05) (Fig. 1a). In PPMI, only serum monocyte at baseline was found to positively correlate with baseline GDS (P < 0.05) (Fig. 1b).
a GDPH database. b PPMI cohort. The color of square box corresponded to partial correlation coefficient. MDS-UPDRS MDS Unified Parkinson’s Disease Rating Score, MoCA Montreal Cognitive Assessment, HAMD The Hamilton Depression Rating Scale for Depression, HAMA Hamilton Anxiety Rating Scale, ADL Activities of Daily Living, GDS Geriatric Depression Scale Score, STAI State-Trait Anxiety Inventory, NLR Neutrophil-to-lymphocyte Ratio, PLR Platelet-to-lymphocyte Ratio, SII System Immune-inflammation Index, LMR Lymphocyte-to-monocyte Ratio; ·, 0.1 < P ≤ 0.05; *, 0.05 < P ≤ 0.01; **, 0.01 < P ≤ 0.001; ***, 0.001 < P ≤ 0.0001. The analysis was adjusted by age, sex, education, disease duration and LEDD.
Partial correlation between white matter integrity and peripheral inflammation markers
Regarding the correlation between MD and peripheral inflammation markers, serum lymphocytes count appeared to negatively correlate with MD of left corticospinal tract and left sagittal stratum; NLR positively with mean white matter, middle cerebellar peduncle, body of corpus callosum, right retrolenticular part of internal capsule, left sagittal stratum, right external capsule, and left cingulum around hippocampus; PLR positively with right superior cerebellar peduncle; SII positively with right retrolenticular part of internal capsule in both cohort (Fig. 2).
a GDPH database. b PPMI cohort. The color of square box corresponded to partial correlation coefficient. FA Fractional Anisotropy, MD Mean Diffusivity, NLR Neutrophil-to-lymphocyte Ratio, PLR Platelet-to-lymphocyte Ratio, SII System Immune-inflammation Index, LMR Lymphocyte-to-monocyte Ratio, ·, 0.1 < P ≤ 0.05; *, 0.05 < P ≤ 0.01; **, 0.01 < P ≤ 0.001; ***, 0.001 < P ≤ 0.0001. The analysis was adjusted by age, sex, education, disease duration and LEDD.
As for the correlation between FA and peripheral inflammation markers, serum neutrophil count negatively correlated with FA of genu of corpus callosum, body of corpus callosum, and fornix; NLR negatively with mean white matter, genu of corpus callosum, body of corpus callosum, splenium of corpus callosum, bilateral superior cerebellar peduncle, right anterior limb of internal capsule and left superior longitudinal fasciculus; SII inversely correlated with mean white matter, body of corpus callosum, right medial lemniscus, bilateral superior cerebellar peduncle and left superior longitudinal fasciculus; LMR positively correlated with left superior cerebellar peduncle in both cohort.
Linear mixed model for clinical symptoms progression with 5-year follow-up
The results of linear mixed effect model showed a significant main effect of baseline NLR on SCOPA-AUT (β = -0.227, P = 0.047) and LNS (β = 0.274, P = 0.010), baseline PLR on LNS (β = 0.297, P = 0.028), baseline SII on LNS (β = 0.241, P = 0.020) and SDMT (β = 0.204, P = 0.037) (Table 1).
Significant baseline peripheral inflammation markers × Time interaction effect was shown in the Model 1. The value of the interaction effect indicates the average change of estimated effect taken on dependent variable over follow-up time. Here, after adjustment of age, sex, disease duration, education and LEDD, the higher serum lymphocytes count at baseline was predictive of improvement in LNS (β = 0.035, P = 0.043) but faster deterioration in SFT (β = −0.031, P = 0.042); the higher NLR predictive of more rapid deterioration in SCOPA-AUT (β = 0.036, P = 0.040) and LNS (β = 0.046, P = 0.008), but improvement in RBDSQ (β = −0.035, P = 0.045); the higher SII predictive of improvement in STAI, but faster deterioration in LNS; higher LMR predictive of more rapid deterioration in HVLT immediate recall (β = −0.036, P = 0.021) and HVLT delayed recall (β = −0.046, P = 0.003) (Table 1).
Sub-group analysis of linear mixed model by gender for Clinical Symptoms Progression
Considering sex-based differences in peripheral inflammation in patients with PD, we conducted a sub-group analysis. In male patients with PD, the results showed significant main effect of baseline serum lymphocytes count on MDS-UPDRS III (β = 0.276, P = 0.031) and GDS (β = 0.243, P = 0.042), baseline NLR on LNS (β = 0.273, P = 0.033) and SDMT (β = 0.255, P = 0.027), baseline SII on LNS (β = 0.245, P = 0.035) and SDMT (β = 0.262, P = 0.013), as well as baseline LMR on SDMT (β = −0.305, P = 0.009). As for interaction effect between baseline peripheral inflammation and time, we found higher baseline serum lymphocytes count as predictive of improvement in MoCA (β = 0.051, P = 0.014) and LNS (β = 0.043, P = 0.030), higher NLR as predictive of improvement in RBDSQ (β = −0.044, P = 0.044) but faster deterioration in LNS (β = −0.053, P = 0.010), higher PLR as predictive of more rapid deterioration in LNS (β = −0.060, P = 0.029), and higher LMR as predictive of faster deterioration in HVLT Delayed Recall (β = −0.042, P = 0.043) (Table 2).
Regarding female patients with PD, the results indicated significant main effects of baseline lymphocyte count on LNS (β = −0.471, P = 0.023) and HVLT Delayed Recall (β = −0.316, P = 0.036). Moreover, higher baseline serum lymphocyte count appeared to be predictive of faster deterioration in MDS-UPDRS III (β = 0.081, P = 0.032), SFT (β = −0.064, P = 0.048); higher NLR predictive of improvement in SFT (β = 0.074, P = 0.029); higher PLR predictive of improvement in MDS-UPDRS III (β = −0.133, P = 0.010) and STAI (β = −0.065, P = 0.043); higher SII predictive of improvement in STAI (β = −0.082, P = 0.028); higher LMR predictive of faster deterioration in SFT (β = −0.120, P = 0.003) and HVLT Delayed Recall (β = −0.064, P = 0.045) (Table 2).
The role of baseline peripheral inflammatory markers on PD progression at every time point
The results of Model 2 were summarized in Supplementary Table 3. In PD patients, we found that higher NLR was predictive of faster deterioration of sleep disturbance measured by RBDSQ at year-5 (β = 0.228, P = 0.030) follow-up visit and attention and working memory measured by LNS in year-3 (β = −0.249, P = 0.016), year-4 (β = −0.283, P = 0.007) and year-5 (β = −0.212, P = 0.039) follow-up visits. Likewise, higher PLR was also predictive of faster deterioration on LNS at year-2 (β = −0.301, P = 0.042) and year-3 (β = −0.377, P = 0.012) following-up visits, and higher LMR predictive of faster deterioration on memory measured by HVLT Delayed Recall (β = −0.247, P = 0.008) at year-5 follow-up visit.
In male PD patients, higher baseline lymphocyte count was predictive of improvement in global cognition measured by MoCA at year-5 (β = 0.289, P = 0.018) follow-up visit; higher NLR was predictive of faster deterioration on LNS at year-4 (β = −0.344, P = 0.006) and year-5 (β = −0.247, P = 0.040) follow-up visit; Likewise, higher PLR was predictive of faster deterioration on LNS at each following time point.
In female patients with PD, higher baseline lymphocytes count predict faster deterioration of motor symptoms measured by MDS-UPDRS III at each time point; higher NLR predicts faster deterioration on LNS at year-3 (β = −0.473, P = 0.039) but improvement on SFT at year-4 (β = 0.393, P = 0.043); higher PLR predict improvement on MDS-UPDRS III at year-3 (β = −0.649, P = 0.028) and year-5 (β = −0.817, P = 0.011) follow-up time points; higher LMR predict faster deterioration on SFT at year-4 (β = −0.577, P = 0.013) and year-5 (β = −0.521, P = 0.032) follow-up points.
The VIFs of all linear mixed models were shown in Supplementary Table 4.
Path analysis
Based on the above research results, we conducted path analysis to explore further whether baseline white matter integrity is involved in the impairment of baseline peripheral inflammation on cognition. The results of Path analysis showed that FA of body of corpus callosum [total effect = 0.361; direct effect = 0.317; indirect effect = 0.043], mean white matter MD [total effect = −0.286; direct effect = −0.241; indirect effect = −0.045], MD of left sagittal stratum [total effect = −0.387; direct effect = −0.349; indirect effect = −0.038] at baseline were significant mediators of the relationship between baseline NLR and change in LNS score over five years (Fig. 3b, c, e) in PD patients. Especially, only MD of left cingulum around hippocampus at baseline was shown to partly mediate the causative effect of baseline NLR on the change in LNS scale over five years in male PD patients [total effect = −0.390; direct effect = −0.325; indirect effect = −0.065] (Fig. 3h).
a The FA of right cingulum mediated the relationship between baseline lymphocytes and change in MoCA score over five years in male patients with PD. b–e The white matter integrity index mediated the relationship between baseline NLR and LNS score over five years in all PD patients. f–i The white matter integrity index mediated the relationship between baseline NLR and LNS score over five years in male PD patients. FA Fractional Anisotropy, MD Mean Diffusivity, NLR Neutrophil-to-lymphocyte Ratio, MoCA Montreal Cognitive Assessment, LNS Letter number sequencing score.
Discussion
Increasing evidence supports the involvement of peripheral inflammation in the progression of PD symptoms. However, clinical evidence regarding peripheral immune cells in this context remains limited. In this study, we assessed peripheral inflammation using differential WBC counts and their ratio, which are accessible in routine blood tests, and thoroughly investigated their association with PD progression through cross-sectional and longitudinal analyses.
We found that those peripheral inflammation markers were associated with cognitive function, mood and white matter integrity in partial correlation analysis. Moreover, after adjustment of age, sex, disease duration, education, and LEDD, the baseline lymphocytes appeared to be associated with the improvement of attention and working memory but with the progression of executive function. Moreover, higher NLR and SII at baseline were shown to be correlated with faster deterioration in attention and working memory, and higher LMR at baseline was shown to be predictive of deterioration in memory over time. In particular, gender difference on effect of peripheral inflammation was identified in subgroup analysis. Furthermore, decreased white matter integrity may partly mediate the detrimental effect of NLR on longitudinal changes in the cognitive domains of attention and working memory. Taken together, our study underscored the prognosis significance of the peripheral inflammation markers of lymphocytes, NLR, PLR SII, and LMR, which may be reliable and easily accessible biomarkers for predicting and monitoring PD progression, especially in cognitive impairment. Moreover, our study further provides clinical evidence for the involvement of the peripheral inflammation in PD progression. This information may provide a theoretical basis for applying anti-inflammation drug to treat PD and contribute to developing more appropriate timing for clinical intervention.
Consistent with previous study16, NLR was negatively correlated with MoCA in GDPH database. Another cross-sectional study17 also found that the peripheral cytokine levels could affect regional gray matter volume in patients with PD, which may contribute to the correlation between peripheral inflammation and cognition. However, this correlation was nonsignificant in PPMI. The reason for this may be the permeability of BBB, a cellular barrier separating the delicate neuronal environment from the peripheral blood. The patients enrolled in PPMI were early-staged, whose BBB integrity was found18 to be relatively intact. Moreover, the influence of peripheral inflammation exerted on central nervous system was indirect and sample size was relatively small due to the strict exclusion criteria applied, which may contribute to relatively low partial correlation coefficients between peripheral inflammation markers and cognition.
The index of SII, NLR, and PLR are well-established indicators of the overall inflammatory status of the organism. In particular, NLR integrates two leukocyte subpopulations, among which neutrophil represents chronic inflammation and lymphocyte might indicate the regulatory processes19. Higher NLR was observed in PD compared with healthy control in two studies at the same time20,21. Moreover, a study conducted by Muñoz-Delgado et al. observed that NLR was significantly and negatively correlated with striatal dopamine transporter density levels in the caudate and the putamen19, which may explain why NLR non-significantly correlated with MDS-UPDRS III during OFF state in current cross-sectional study. Moreover, the index of NLR was shown to have an acceptable discrimination power of PD with mild cognitive impairment (PD-MCI) from PD with normal cognition22, suggesting participation of NLR on PD cognitive function.
With respect to the correlation between longitudinal association between NLR and cognition, baseline NLR could not predict the change of MoCA over time, which was consistent with a previous study21. Nevertheless, we found that the baseline NLR was associated with faster deterioration in attention and working memory assessed by LNS. The underlying mechanism may be attributed to the Alzheimer’s disease (AD) pathology, which has been identified as an essential contributor to PD cognitive impairment23. Previous studies had observed that serum NLR was positively correlated with levels of CSF beta-amyloid (Aβ), total Tau, phosphorylated Tau24, and cortical beta-amyloid deposition evaluated by 18F-florbetapir positron emission tomography (PET)25.
In addition to decreased gray matter volume and pathological protein deposits, the decrease of white matter integrity may also be investigated in progression of PD cognitive decline. White matter hyperintensity burden was demonstrated to have great prognosis significance on cognitive function in patients with PD26. We herein extended the research and found that NLR was positively associated with widespread impairment of white matter integrity across the whole white matter skeleton, mainly on corpus callosum, cingulum and sagittal stratum. More importantly, path analysis showed that FA of body of corpus callosum and MD of mean white matter skeleton and sagittal stratum partly mediate the detrimental effect of NLR on attention and working memory in PD patients. Moreover, in male PD patients, FA of mean white matter skeleton and Genus of corpus callosum, and MD of cingulum around the hippocampus were involved in the progression of attention and working memory. In addition to vascular mechanism, decreased white matter integrity also denoted myelin damage in the axon27, which could impair neuronal signaling. Moreover, some evidence indicates that impairment of white matter is also correlated with synaptic density loss in white matter impairment-connected cortex28 and glymphatic dysfunction29, both of which were proposed to be involved in PD cognitive deficit30,31.
Regarding regional white matter impairment, Goldman and his colleagues found that reduced central volumes in corpus callosum32 and white matter abnormalities in most anterior callosal segments33 were associated with decline in attention and working memory in PD patients. Given anterior callosal-prefrontal cortical connection, impairment of white matter integrity in Genus of corpus callosum may give rise to “frontal–striatal” cognitive deficit33. The frontoparietal network and ventral attention network (VA) were inter-connected by the body of the corpus callosum34, impairment of which may also be involved in progression of cognitive decline. Meanwhile, increasing evidence supports involvement of cingulum in attention, working memory and executive function because of its close link with prefrontal cortex35.
Interestingly, we also discovered sex differences in effect of peripheral inflammation. In male patients, higher baseline lymphocyte count could predict improvement of global cognition and attention and working memory, while NLR and PLR were correlated with progression of attention and working memory. Regarding female patients, higher lymphocyte at baseline predicted deterioration of motor symptoms, while PLR did the opposite. Higher lymphocytes and LMR were shown to predict the progression of executive function, as opposed to NLR. Moreover, only higher baseline LMR exerted a consistently detrimental effect on memory in both sexes. Indeed, sex differences in peripheral inflammation had been identified previously. Recent research revealed inflammatory activation on peripheral monocytes with enrichment of gene sets associated with interferon-gamma stimulation in females with PD, while more heterogeneous activation patterns in males36. Moreover, male patients with PD were shown to have higher response to α-synuclein in T lymphocytes in blood37. There also existed different profiles of serum immune markers between sex37. However, the sex-based differences in peripheral lymphocytes, neutrophils and platelets were rarely explored, and their mechanisms need further study.
There are some limitations in this study. First of all, the limited sample size and follow-up period may generate bias in our conclusion. Next, although the rigorous exclusion criteria (i.e., inflammatory diseases or cancer) were applied and multivariate regression analysis was conducted, the confounding factors, such as drugs, exercise and nutritional status affecting peripheral immune cells, could not be entirely ruled out. Thus, the exact relationship between peripheral immune cells and clinical characteristics separated by sex requires further assessment and validation in patients with PD. Then, the information of other inflammatory markers, including cytokines and chemokine, was unavailable in PPMI, so we could not further validate the effect of peripheral inflammation on PD symptoms in other ways. Moreover, numerous evidence had supported the association between systemic immune-inflammation index and cognitive decline in elderly people38,39,40, while this study only included PD patients and whether the effect of peripheral inflammation on cognition and other symptomatic outcomes is PD-specific needed further exploration in the future. Last, considering that our longitudinal study only enrolled PD patients at early stage, the conclusion on predictive significance of peripheral inflammation markers might not be suitable to the patients at other stages.
In summary, our study revealed that peripheral inflammation markers are associated with motor symptoms and cognitive function in PD. More importantly, baseline serum inflammatory markers predicted cognitive decline, particularly cognitive sub-domains such as executive function, memory, and attention and working memory. Furthermore, decreased white matter integrity may partly mediate the peripheral inflammation-induced cognitive decline over a 5–year period. Moreover, there may exist sex-based differences in the effect of peripheral inflammation on PD symptom progression.
Our findings not only provided clinical evidence on the involvement of peripheral immune cells in PD progression but also proposed a reliable and easily accessible blood marker of NLR to predict PD cognitive decline. Of note, our study also underscored the sex difference in this process. However, as potential confounders influencing peripheral immune cells were not entirely excluded, our findings warrant further validation by well-designed clinical trials with large sample sizes and extended follow-up periods.
Methods
Participants
The patients with PD were diagnosed by at least two skilled neurologists according to the UK PD Society Brain Bank Clinical Diagnostic Criteria41 from the Department of Neurology, Guangdong Provincial People’s Hospital (Guangzhou, China) between 2013 and 2020. All participants underwent brain magnetic resonance imaging (MRI) and provided written informed consent. The cross-sectional study component of this research protocol was approved by the Medical Ethics Committee of Guangdong Provincial People’s Hospital (No. KY2020-544-01). Meanwhile, in order to validate our analysis in a larger population and explore longitudinal change of PD symptoms, we also collected data from PPMI (https://www.ppmi-info.org) on April 28, 2022. The PPMI, an ongoing, multicenter and observational study, has recruited approximately 4000 participants across all stages of PD to explore PD progression biomarkers and accelerate disease-modifying therapeutic trials42. The PD participants in the PPMI cohort were untreated, in the early stages of the disease, and had dopamine deficits detected by dopamine transporter (DAT) SPECT imaging. Each participating site in the PPMI database obtained Institutional Review Board approval, and adhered fully to the principles outlined in the Declaration of Helsinki. Before the study began, all subjects provided written informed consent. Only PD patients with accessible diffusion tensor images at baseline and 5-year follow-up in PPMI were included in the current study.
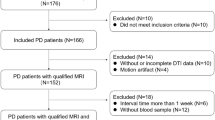
To mitigate potential influences on peripheral inflammation, patients who were exposed to conditions potentially influencing the immune response at the time of clinical evaluation were excluded in both cohorts. These conditions included current infections or acute inflammatory diseases, tumor, history of traumatic brain injury, blood and immune system disease, and the use of any immunosuppressive agents. Specially, to exclude the effect of genetic status, the participants whose age of disease onset below 50 years old were excluded in GDPH cohort. Moreover, we also excluded participants using any drugs affecting platelet numbers in platelet-related analysis in both cohorts. The flowchart of patients’ enrollment was presented in Supplementary Fig. 1.
Clinical evaluation
In GDPH cohort, motor function was evaluated using the Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III during ON and OFF state of patients. Disease severity was assessed by the Hoehn and Yahr (HY) stage. The Mini-mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) were used to evaluate global cognition. Hamilton depression rating scale (HAMD) and Hamilton anxiety rating scale (HAMA) were used to assess depression and anxiety separately. Moreover, the England Activity of Daily Living Scale (ADL) was used to evaluate daily living ability.
In PPMI, MDS-UPDRS part III was used to assess motor symptoms during ON state, and MDS-UPDRS part II was used to measure motor aspects of daily living experiences. With respect to cognitive assessment, the MoCA was used to evaluate global cognition, both the Letter Number Sequencing (LNS) Score and Symbol Digit Modalities Test (SDMT) for attention and working memory, the Semantic Fluency Total Score (SFT) for executive function, the Hopkins Verbal Learning Test (HVLT) for memory, and Benton Judgment of the Line Orientation Scores (JoLO) for visuospatial function. Other non-motor symptoms were evaluated using a series of scales as follows: the MDS-UPDRS part I for the overall non-motor symptoms, the Geriatric Depression Scale Score (GDS) for depression, the State-Trait Anxiety Inventory (STAI) for anxiety, the Epworth Sleepiness Scale (ESS) and REM Sleep Behavior Disorder Screening Questionnaire (RBDSQ) for sleep disturbance, the ADL for daily living ability, and the Parkinson’s Disease-Autonomic Dysfunction (SCOPA-AUT) score for autonomic system function. We also collected demographic characteristics, including age, gender, duration from diagnosis to enrollment, years of education. and total levodopa equivalent daily dose (LEDD).
Serum inflammatory markers
2 mL fasting venous blood samples were collected into ethylenediaminetetraacetic acid (EDTA) coated tubes. We applied an XN-9000 automated blood analyzer (Sysmex Corporation, Kobe, Japan) in the hematology lab to calculate the inflammatory markers, such as neutrophil, lymphocyte, monocyte, and platelet counts on blood samples. Moreover, the composite metrics like SII, NLR, PLR, and LMR were also measured. In particular, SII was calculated according to the following formulas43.
MRI data collection and processing
In GDPH database, we obtained DTI data from all the participants. The MRI scans were performed using a SIGNA EXCITE 3.0 T MRI scanner (General Electric Company, USA) with the following parameters: TE = 76 ms; TR = 8000 ms; flip angle = 90°; FOV = 256 × 256 mm2; slice thickness = 2.5 mm; voxel size = 2 × 2 × 3 mm3; and NEX = 1. Images of 25 different nonlinear diffusion-weighted gradient directions (b = 1000 s/ mm2) and one non-diffusion-weighted gradient direction (b = 0) were collected. Each gradient was scanned for 60 layers, and a total of 1560 files were obtained.
With regard to PPMI cohort, the neuroimaging scan was conducted at baseline. The DTI data obtained followed the standardized imaging protocol on Tim Trio 3 Tesla Siemens scanners (Siemens, Erlangen, Germany). The MRI parameters were as follows: 72 axial slices, echo time (TE) = 88 ms, repetition time (TR) = 550–1000 ms, flip angle = 90°, voxel size: 2.0 × 2.0 × 2.0 mm3, acquisition matrix = 1044 × 1044; and 64 diffusion-sensitive gradient directions at b = 1000 s/mm2. One diffusion-unweighted (b0) image was also included. More details can be found in the MRI technical operation manual on the PPMI consortium website.
For MRI processing, we calculated the FA and MD values of white matter using the FMRIB Software Library (FSL) v6.044 according to a previously published method30. The pre-procession steps included skull stripping, eddy current correction, tensor fitting, and reorientation. Then, each FA and MD image was aligned to a 1 × 1 × 1 mm standard space through the nonlinear registration, and the FA and MD of all anatomical white matter regions identified with the John Hopkins University WM atlas (ICBM-DTI-81) were calculated.
Statistical analysis
R software (version 4.4.0; The R Foundation for Statistical Computing, Vienna, Austria) was used to perform all statistical analyses in this study. Continuous data with a normal distribution were expressed as mean ± standard deviation and analyzed using either independent sample t-tests to compare two different groups or one-way analysis of variance (ANOVA) for multi-group comparisons. Nonnormally distributed data were expressed as median ± interquartile range (IQR) and analyzed using the rank sum test for two groups or the Kruskal-Wallis test for multiple groups. The differences in proportions of categorical variables were compared using a chi-squared test. Missing values were listed in the table. A two-sided p-value less than 0.05 indicated statistically significant test results for all statistical tests.
Partial correlation analysis was performed to investigate the relationships between clinical symptoms, white matter integrity and serum inflammatory markers in cross-sectional study, with adjustment of age, sex, disease duration, education and LEDD. Concerning data from a longitudinal study, we conducted a linear mixed effects model (LMM) with the R packages lme445 and lmerTest46 to investigate the potential effect of peripheral inflammatory markers on PD symptoms.
To evaluate the effects of time and baseline serum inflammatory markers, we introduced follow-up time, baseline serum inflammatory markers and their interaction (baseline serum inflammatory markers *follow-up time) as fixed factors in the model. Of note, the serum inflammatory markers were log-transformed and standardized to Z scores (Z = (value − mean)/SD). For random effects, the patient number (PATNO) was entered as a random factor to consider possible inter-individual variability. The characteristic of follow-up time was treated as a continuous variable in Model 1. When there existed a significant interaction effect in Model 1, we additionally constructed a model (Model 2) including follow-up time as categorical variable to specify the interaction effect in each time point. Moreover, since the random slope model is more susceptible to convergence failure and we had a limited sample size, we selected the random intercept model for our LMM instead47. The models were further adjusted for age, sex, disease duration, education, and LEDD, which were each centered (demeaned) prior to estimation. The multicollinearity of variables was evaluated using the variance inflation factor (VIF), which is considered48 to be severe when it exceeds 10. The outliers measured by the “outlierTest” function49 from R package of “car” were eliminated. Moreover, the normality assumptions of the residuals were confirmed by the Shapiro–Wilk test and graphical inspection of histograms and normality plots. Furthermore, considering that sex-dependent change in immune system have been identified in PD36,50, we conducted sub-group analysis by gender to explore sex-based differences in the effect of peripheral inflammation.
To explore the mediating role of white matter integrity between peripheral inflammatory markers and progression of PD symptoms, we also conducted a path analysis that included total, direct, and indirect effects. Path analysis is a statistical technique to measure mediating effects in causative sequence that can provide insights about the relative contribution among causative relationships and the directions of causative paths51.
Data availability
The data was publicly available on PPMI website (https://www.ppmi-info.org/access-data-specimens/). And the anonymized data from GDPH dataset are available from the corresponding author upon reasonable request.
References
Kalia, L. V. & Lang, A. E. Parkinson’s disease. Lancet 386, 896–912 (2015).
Tansey, M. G. et al. Inflammation and immune dysfunction in Parkinson disease. Nat. Rev. Immunol. 22, 657–673 (2022).
Roodveldt, C. et al. The immune system in Parkinson’s disease: what we know so far. Brain 147, 3306–3324 (2024).
Zou, K., Deng, Q., Zhang, H. & Huang, C. Glymphatic system: a gateway for neuroinflammation. Neural Regen. Res. 19, 2661–2672 (2023).
Morris, H. R., Spillantini, M. G., Sue, C. M. & Williams-Gray, C. H. The pathogenesis of Parkinson’s disease. Lancet 403, 293–304 (2024).
Zhong, X. et al. Peripheral immunity and risk of incident brain disorders: a prospective cohort study of 161,968 participants. Transl. Psychiatry 13, 382 (2023).
Stidham, R. W. et al. Intestinal dilation and platelet:albumin ratio are predictors of surgery in stricturing small bowel Crohn’s disease. Clin. Gastroenterol. Hepatol. 14, 1112–1119.e1112 (2016).
Li, S. et al. Serum Folate, Vitamin B12 Levels, and systemic immune-inflammation index correlate with motor performance in Parkinson’s disease: a cross-sectional study. Front. Neurol. 12, 665075 (2021).
Li, Y. et al. Parkinson’s disease peripheral immune biomarker profile: a multicentre, cross-sectional and longitudinal study. J. Neuroinflamm. 19, 116 (2022).
Kim, R. et al. Serum inflammatory markers and progression of nonmotor symptoms in early Parkinson’s disease. Mov. Disord. 37, 1535–1541 (2022).
Lawton, M. et al. Blood biomarkers with Parkinson’s disease clusters and prognosis: the oxford discovery cohort. Mov. Disord. 35, 279–287 (2019).
Huang, X., Hussain, B. & Chang, J. Peripheral inflammation and blood–brain barrier disruption: effects and mechanisms. CNS Neurosci. Ther. 27, 36–47 (2020).
Jacob, M. A. et al. Cerebral small vessel disease progression increases risk of incident Parkinsonism. Ann. Neurol. 93, 1130–1141 (2023).
Nicoletti, A. et al. Vascular risk factors, white matter lesions and cognitive impairment in Parkinson’s disease: the PACOS longitudinal study. J. Neurol. 268, 549–558 (2021).
Chen, H. et al. Cerebral small vessel disease may worsen motor function, cognition, and mood in Parkinson’s disease. Park. Relat. Disord. 83, 86–92 (2021).
Lucero, J., Gurnani, A., Weinberg, J. & Shih, L. C. Neutrophil-to-lymphocyte ratio and longitudinal cognitive performance in Parkinson’s disease. Ann. Clin. Transl. Neurol. 11, 2301–2313 (2024).
Chen, B. et al. Correlations of gray matter volume with peripheral cytokines in Parkinson’s disease. Neurobiol. Dis. 201, 106693 (2024).
Lau, K., Kotzur, R. & Richter, F. Blood–brain barrier alterations and their impact on Parkinson’s disease pathogenesis and therapy. Transl. Neurodegen. 13, 37 (2024).
Muñoz-Delgado, L. et al. Peripheral inflammation is associated with dopaminergic degeneration in Parkinson’s disease. Mov. Disord. 38, 755–763 (2023).
Muñoz-Delgado, L. et al. Peripheral immune profile and neutrophil-to-lymphocyte ratio in Parkinson’s disease. Mov. Disord. 36, 2426–2430 (2021).
Kim, R., Kang, N., Byun, K., Park, K. & Jun, J.-S. Prognostic significance of peripheral neutrophils and lymphocytes in early untreated Parkinson’s disease: an 8-year follow-up study. J. Neurol. Neurosurg. Psychiatry 94, 1040–1046 (2023).
Contaldi, E., Magistrelli, L., Cosentino, M., Marino, F. & Comi, C. Lymphocyte count and neutrophil-to-lymphocyte ratio are associated with mild cognitive impairment in Parkinson’s disease: a single-center longitudinal study. J. Clin. Med. 11, 5543 (2022).
Aarsland, D. et al. Parkinson disease-associated cognitive impairment. Nat. Rev. Dis. Prim. 7, 47 (2021).
Jacobs, T. et al. The neutrophil to lymphocyte ratio associates with markers of Alzheimer’s disease pathology in cognitively unimpaired elderly people. Immun. Ageing 21, 32 (2024).
Mehta, N. H. et al. Peripheral immune cell imbalance is associated with cortical beta-amyloid deposition and longitudinal cognitive decline. Sci. Rep. 13, 8847 (2023).
Carvalho de Abreu, D. C. et al. White matter hyperintensity burden predicts cognitive but not motor decline in Parkinson’s disease: results from the Ontario Neurodegenerative diseases research initiative. Eur. J. Neurol. 30, 920–933 (2023).
Yang, K. et al. White matter changes in Parkinson’s disease. npj Park. Dis. 9, 150 (2023).
Zhang, J. et al. Linking white matter hyperintensities to regional cortical thinning, amyloid deposition, and synaptic density loss in Alzheimer’s disease. Alzheimer’s Dement. 20, 3931–3942 (2024).
Zhou, Y. et al. Impaired meningeal lymphatics and glymphatic pathway in patients with white matter hyperintensity. Adv. Sci. 11, e2402059 (2024).
He, P. et al. The association of the glymphatic function with Parkinson’s disease symptoms: neuroimaging evidence from longitudinal and cross-sectional studies. Ann. Neurol. 94, 672–683 (2023).
Frigerio, I. et al. Regional differences in synaptic degeneration are linked to alpha-synuclein burden and axonal damage in Parkinson’s disease and dementia with Lewy bodies. Acta Neuropathol. Commun. 12, 4 (2024).
Goldman, J. G. et al. Corpus callosal atrophy and associations with cognitive impairment in Parkinson disease. Neurology 88, 1265–1272 (2017).
Bledsoe, I. O., Stebbins, G. T., Merkitch, D. & Goldman, J. G. White matter abnormalities in the corpus callosum with cognitive impairment in Parkinson disease. Neurology 91, e2244–e2255 (2018).
Liu, Y. et al. Connectivity-based topographical changes of the corpus callosum during aging. Front. Aging Neurosci. 13, 753236 (2021).
Bubb, E. J., Metzler-Baddeley, C. & Aggleton, J. P. The cingulum bundle: anatomy, function, and dysfunction. Neurosci. Biobehav. Rev. 92, 104–127 (2018).
Carlisle, S. M. et al. Sex-based differences in the activation of peripheral blood monocytes in early Parkinson disease. npj Park. Dis. 7, 36 (2021).
Bourque, M., Morissette, M., Soulet, D. & Di Paolo, T. Impact of sex on neuroimmune contributions to Parkinson’s disease. Brain Res. Bull. 199, 110668 (2023).
Lu, W., Zhang, K., Chang, X., Yu, X. & Bian, J. The association between systemic immune-inflammation index and postoperative cognitive decline in elderly patients. Clin. Interven. Aging ume 17, 699–705 (2022).
Hung, K.-C. et al. Association between the neutrophil-to-lymphocyte ratio and cognitive impairment: a meta-analysis of observational studies. Front. Endocrinol. 14, 1265637 (2023).
Li, S. et al. The neutrophil-to-lymphocyte ratio is associated with mild cognitive impairment in community-dwelling older women aged over 70 years: a population-based cross-sectional study. Front. Aging Neurosci. 15, 1261026 (2023).
Gelb, D. J., Oliver, E. & Gilman, S. Diagnostic criteria for Parkinson disease. Arch. Neurol. 56, 33 (1999).
Marek, K. et al. The Parkinson’s progression markers initiative (PPMI) – establishing a PD biomarker cohort. Ann. Clin. Transl. Neurol. 5, 1460–1477 (2018).
Dziedzic, E. A. et al. Investigation of the Associations of Novel Inflammatory Biomarkers—Systemic Inflammatory Index (SII) and Systemic Inflammatory Response Index (SIRI)—with the severity of coronary artery disease and acute coronary syndrome occurrence. Int. J. Mol. Sci. 23, 9553 (2022).
Jenkinson, M., Beckmann, C. F., Behrens, T. E. J., Woolrich, M. W. & Smith, S. M. Fsl NeuroImage 62, 782–790 (2012).
Luke, S. G. Evaluating significance in linear mixed-effects models in R. Behav. Res. Methods 49, 1494–1502 (2017).
Hatsukawa, H. & Ishikawa, M. Clinical potential of pupillary light reflex parameters as objective indicators reflecting chronic rhinosinusitis-specific quality of life: a 12-month prospective longitudinal study. Sci. Rep. 11, 21586 (2021).
Harrison, X. A. et al. A brief introduction to mixed effects modelling and multi-model inference in ecology. PeerJ 6, e4794 (2018).
Lei, Z. et al. Changes in soil organic carbon and its influencing factors in the growth of Pinus sylvestris var. mongolica plantation in Horqin Sandy Land, Northeast China. Sci. Rep. 9, 16453 (2019).
Pretis, F., Reade, J. J. & Sucarrat, G. Automated General-to-Specific (GETS) regression modeling and indicator saturation for outliers and structural breaks. J. Stat. Softw.86, 1–44 (2018).
Nissen, S. K. et al. Alterations in blood monocyte functions in Parkinson’s Disease. Mov. Disord. 34, 1711–1721 (2019).
Hsu, J. L. et al. Magnetic resonance images implicate that glymphatic alterations mediate cognitive dysfunction in Alzheimer Disease. Ann. Neurol. 93, 164–174 (2022).
Acknowledgements
The PPMI is supported by the Michael J. Fox Foundation for Parkinson’s Research and its funding partners, including Abbott, Avid, Biogen, Bristol-Myers Squibb, Covance, Elan, GE Healthcare, Genentech, GSK, Lilly, MERCK, MSD, Pfizer, Roche, and UCB (details of the PPMI funding partners can be found at https://www.ppmi-info.org/about-ppmi/who-we-are /study-sponsors). In addition, this study was supported by the National Natural Science Foundation of China (No. 82471257, 82371249, 82101377, 82071419), the Science and Technology Planning Project of Guangzhou (No.202201000005).
Author information
Authors and Affiliations
Contributions
P.K.H., Y.Y.L. and Z.H.H.: conception, methodology, data acquisition, analysis, interpretation of the results, writing of the original draft; Y.Y.G. and Q.R.D.: methodology, interpretation of the results, revision of the manuscript for intellectual content; Y.H.Q., S.J.F., R.Y.H., and L.X.G.: methodology, interpretation of the results; G.X.M. and Y.H.Z.: data acquisition, analysis; L.S., L.J.W., and K.N.: conception, methodology, interpretation of the results, supervision, revision of the manuscript for intellectual content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
He, P., Li, Y., Huang, Z. et al. Peripheral inflammation’s variable impact on cognitive and symptomatic outcomes in Parkinson’s disease: a longitudinal and cross-sectional analysis. npj Parkinsons Dis. 11, 155 (2025). https://doi.org/10.1038/s41531-025-01019-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41531-025-01019-7