Abstract
Parkinson’s disease (PD) presents with diverse symptoms, partly influenced by motor symptom asymmetry, which reflects hemispheric brain specialization. This systematic review of 80 studies explored how lateralized motor symptoms affect non-motor outcomes in PD, including cognition, emotion, and psychiatric health. Patients with right-sided motor symptoms (left-hemisphere pathology) show more global cognitive decline and higher dementia risk, while those with left-sided symptoms (right-hemisphere pathology) more often experience psychiatric issues like depression, anxiety, and impaired emotional recognition. Visuospatial deficits were consistently linked to left-sided symptoms, aligning with right-hemisphere dysfunction. Although findings vary across studies, this pattern suggests the relevance of brain lateralization in non-motor symptom assessment. Motor asymmetry may also affect treatment responses, such as deep brain stimulation outcomes. However, inconsistencies in study methods—definitions of asymmetry, motor subtypes, and comorbidities—limit meta-analytic conclusions. Overall, incorporating motor symptom asymmetry into PD diagnosis and treatment could enhance personalized care, warranting more standardized future research.
Similar content being viewed by others
Introduction
Motor symptoms in people living with Parkinson’s disease (PwPD) (including resting tremor, bradykinesia, muscle rigidity, postural instability, and gait changes) typically affect one side of the body more than the other, and may eventually affect both sides of the body as the disease advances1. These asymmetries are generally associated with contralateral neurodegenerative patterns at the level of the basal ganglia (BG), measured through different imaging methods, in particular PET and DAT-SCAN2,3, but are less obvious using MRI4. Current literature lacks consensus regarding the underlying causes of motor symptom asymmetry in Parkinson’s disease (PD), with various hypotheses proposed. These include histopathological mechanisms, genetic predispositions, motor practice, handedness, and the presence of structural lesions5. Moreover, the developmental trajectories of motor symptom (a)symmetry seem unclear, with some authors suggesting a persistence of asymmetry of motor symptoms over time, while others suggest a bilateralization of motor symptoms6,7,8.
While Braak et al. 9 model has overlooked motor symptom asymmetry as a potential variable for distinguishing distinct PD phenotypes, the recent α-Synuclein Origin and Connectome Model (SOC Model) proposed by Borghammer10 suggests the existence of two PD phenotypes based on motor symptom symmetry. Accordingly, the first so-called “Brain-first” phenotype would be characterized by disease development in subcortical regions, in particular in the olfactory bulb or amygdala, associated symptomatically to the presence of fewer autonomic symptoms, less Rapid Eye Movement (REM) sleep disorders, less hyposmia, as well as slower disease progression and cognitive decline; this phenotype is suggested to be more associated with lateralized motor symptoms and asymmetric dopaminergic denervation. The second phenotype, named “Body-first PD”, characterized by pathologic processes in the enteric nervous system, would be symptomatically characterized by greater autonomic symptoms, more rapid disease progression, and cognitive decline. This latter phenotype would be more associated with symmetrical motor symptoms and equally symmetrical dopaminergic denervation11,12. A recent post-mortem study suggested a revision of the dual-hit SOC model, in particular, the Body-first phenotype (with a symmetrical onset of disease) would be more inclined to develop dementias, especially dementia with Lewy bodies13,14. Accordingly, and therefore, links are starting to be established between (a-)symmetry of motor symptoms and major cognitive impairments in PD. One of the limitations of the SOC model is that it does not specify if different expected profiles exist based on whether the disease begins on the left or right hemi-body, as well as on the spreading of pathology from one hemisphere to the other, inducing a bilateralization of the disease as described by Hobson1. Yet, studies in various neurodegenerative pathologies, but also healthy controls (HC), have consistently pointed to a greater vulnerability of the left hemisphere for neurodegenerative processes, supported by clinical, imaging, and pathogenetic evidence of cognitive decline15. In PD, data supporting a differential impact of the side of onset/asymmetry of motor symptoms on the evolutive profile are emerging16,17,18, reinforced by the results of a recent meta-analysis18. Some authors have even suggested that patients with predominantly right motor symptoms (RPD), as compared to patients with predominantly left motor symptoms (LPD), are at a higher risk of developing dementia associated with PD19,20. This hypothesis is supported by imaging studies: Starkstein and Leiguarda21 observed an association between RPD and contralateral brain atrophy, partially supported by Claassen et al. 22 whose study revealed faster patterns of cerebral atrophy in the left hemisphere compared to the right but without a direct association with motor symptom asymmetry.
Considering motor symptom asymmetry seems of utmost importance given that this variable may not only have potential implications for the expression of motor symptoms5, non-motor symptoms5, and in fine survival rates23. That being said, the question of its impact, as well as distinct symptomatologic trajectories of right-dominant vs. left-dominant motor symptoms on non-motor symptoms in PD remains largely unanswered24,25. Three previous reviews of the literature evaluated the potential effects of motor symptom asymmetry (left vs. right) on neuropsychological performance24,25,26, showing no clear distinct patterns, although they did highlight that certain neuropsychological functions were specifically impaired in one or other of the subgroups. They suggested that this could be explained by cerebral lateralization of certain cognitive functions (e.g., verbal vs. visuo-spatial). These reviews focused mainly on neuropsychological deficits and very little on psychiatric aspects, none of them on emotional aspects (e.g., recognition and productive abilities). Moreover, none has systematically investigated the potential effects of interactions between pharmacological (e.g., dopaminergic replacement therapies [DRT]) or interventional therapies (e.g., deep brain stimulation [DBS]) and cognitive, psychiatric, and emotional symptoms. Finally, several methodological aspects of the studies included, which could have an influence on the interpretations, were not considered.
In this context, the aim of this systematic review is threefold: (i) first, to provide a systematic review and synthesis of the literature on the impact of motor (a-)symmetry on psychiatric, cognitive and emotional disorders in PwPD, (ii) second, to explore the impact of various therapies such as DBS and/or DRT on these symptoms, (iii) third and finally, to discuss the relationship between the side of onset (left or right) in PD and the risk of developing dementia.
Results
Selection and summary of the studies included in the review
The first stage of the research retrieved 11,092 articles and 50 previous citation studies. There was no time limit, and literature searches were conducted up to 3 April 2025. Two judges (PV and DG) independently evaluated the titles and abstracts, which made it possible to select 204 articles, which were then read in detail. In the end, 80 articles were selected for the review. Detailed data is shown in Fig. 1.
Impact of motor asymmetry on cognitive symptoms in PD
Composite scales
The majority of studies (65 out of 80) using global cognitive efficiency scales (e.g., Mini Mental Scale Examination—MMSE27; Montreal Cognitive Assessment— MoCA28; Mattis Dementia Rating Scale—MDRS29; Dementia Rating Scale—DRS30; National Adult Reading Test—NART31; The SCales for Outcomes in PArkinson’s disease-COGnition SCOPA-COG32) did not show significant differences between LPD and RPD patients, or between patient groups and healthy controls (HC). However, eight studies20,33,34,35,36,37,38,39 found reduced cognitive performance in RPD patients compared to LPD, while only two studies reported lower performance in LPD compared to HC37,38. These mixed results may stem from the fact that global cognitive scales are not sensitive enough to detect mild cognitive deficits within the PD spectrum40. Additionally, these tools are often used for screening in experimental protocols, leading to the exclusion of patients with pathological scores (e.g. refs. 41,42). As results, these findings may not accurately reflect the variability of neuropsychological deficits based on motor symptom asymmetry.
Comprehensive neuropsychological evaluation
A smaller number of studies carried out comprehensive evaluations, although in the majority of studies, the neuropsychological protocols were not complete nor homogeneous, with a predominance for the evaluation of executive-attention functions (49/80 studies), and to a lesser extent memory functions (28/66 studies) and visuo-perceptive functions (22/80). In line with studies reporting significant results using composite scales, reduced cognitive performance in RPD patients has been documented, most often in comparison to LPD patients, and more consistently when compared to healthy controls. Results revealed that those deficits concerned intelligence scales, especially verbal Intellectual Quotient (IQ)43,44, long-term verbal memory16,21,35,43,45,46,47, language44,47,48,49, executive functions including mental flexibility, verbal fluency and working memory16,43,47,49,50,51,52, but also dynamic motor organization53, or perceptive errors of proprioceptive information42. That said, the results were not unanimous about the presence of greater neuropsychological deficits in RPD patients as compared to LPD patients, with studies revealing an absence of differences between LPD and RPD. Other authors, but in smaller scale, suggested higher deficits in LPD for executive functions, revealing reduced performances for working memory in LPD patients, but only if associated to depressed symptoms54, as well as reduced performances for mental flexibility37,55, working memory56 and verbal fluency37. Finally, a minority of studies suggested impairments for verbal learning and episodic memory functions in LPD57,58,59, as well as for visuospatial episodic memory60. Concerning language, even if most of the studies suggested impairments in RPD patients, a minority of studies revealed more pronounced deficits in LPD patients61. This discrepancy could be explained by distinct language assessments, with Holtgraves et al. 61 assessing complex production, potentially requiring other cognitive processes. In contrast, for visuospatial functions (e.g., visual exploration, neglect, spatial relations) most of the literature suggested reduced performances in LPD patients47,57,59,60,62,63,64,65, as well as higher rates of exploration bias66 and of unilateral spatial neglect41,67,68, while one study suggested similar performances for visuospatial functions between sub-groups69. In this context, despite these heterogeneous results for some neuropsychological functions, results potentially suggest the existence of distinct neuropsychological symptom profiles as a function of motor symptom asymmetry, with a tendency for studies evaluated to reveal more neuropsychological deficits in RPD, except for visuospatial measures, which would be more reduced in LPD.
Effects of therapies on psychiatric symptoms as a function of motor symptom asymmetry
Regarding the effect on cognitive symptoms as function of motor symptom asymmetry following PD-therapies, only a very small number of studies have taken an interest in this subject, with three studies evaluating the effects of DRT and five evaluating the effects of DBS46,51,70.
Concerning DRT, Hanna-Pladdy et al. 46 have demonstrated a beneficial effect on neuropsychological performance of DRT only in LPD, while RPD did not benefit, suggesting dissociated effects of DRT as a function of motor symptom asymmetry, the results of which remain to be confirmed. Moreover, Tomer et al. 51 have also demonstrated specific relationships for cognitive performance between motor symptom asymmetry and dopaminergic medication, suggesting that relatively early in the disease progression, when dopamine depletion in the less-affected hemisphere remains mild, dopaminergic treatment optimized for motor symptoms may result in an over-medication of the less-affected hemisphere. Consequently, executive errors may reflect a hyperdopaminergic state that disrupts the functioning of the left hemisphere in LPD patients.
Concerning DBS, Hershey et al. 71 evaluated the effects of unilateral STN-DBS (timemean = 16.2; timeSD = 200 months post-DBS) on working memory depending on the hemisphere most affected, highlighting that when stimulating the hemisphere most affected (whether in LPD or RPD), there was a negative effect on performance. Of note, there was a significant difference between LPD and RPD, meaning that the effects were stronger when it was in patients with right hemisphere damage (LPD). Recently, three studies carried out by our group have explored the effects of STN-DBS (between 3 months and 60 months post-DBS) according to the asymmetry of motor symptoms on cognition20,39,52. Results revealed differential effects of DBS depending on the asymmetry of motor symptoms. Performance for executive functions was largely preserved in RPD patients, compared to the control group, at 3 months and 12 months post-DBS, with the exception of scores on the verbal executive task, where performance declined at 12 months post-DBS. On the other hand, the performance of LPD patients deteriorated post-operatively on nonverbal executive functions and on global cognitive efficiency, compared to the control group. Following this study, only one other study assessed cognitive performance one year post-DBS, but only with a global cognitive efficiency battery (in this case, the MDRS29), showing no differences between patient groups according to motor symptom asymmetry72. In the long-term (up to 60 months post-operatively), only one study has assessed the effect of the STN-DBS as function of motor symptom asymmetry20. This study, following STN-DBS surgery, specifically examined the hypothesis of more pronounced long-term cognitive decline in patients with RPD compared to those with LPD. Moreover, RPD patients had higher scores for self-reported apathy symptoms and lower scores for overall cognitive performance. Survival analyses revealed that only RPD patients exhibited subnormal performances for global cognitive efficiency.
Finally, Agosta et al. 33 demonstrated that neurorehabilitation interventions can have dissociable effects on cognitive performance depending on motor symptom asymmetry. These findings suggest that different types of interventions may influence cognitive outcomes in Parkinson’s disease, but in a subgroup-specific manner. In the same context, DeGutis et al. 73 highlighted the effects of attentional training on motor functions, with particularly pronounced benefits observed in LPD patients, suggesting the involvement of specific underlying factors for rehabilitation. Replication studies are needed, whether in the context of dopaminergic treatment, DBS, or behavioral interventions.
Impact of motor asymmetry on psychiatric symptoms in PD
In terms of psychiatric symptoms, most studies relied on self-assessment questionnaires, primarily evaluating depression (50 studies), anxiety (25 studies), and to a lesser extent, apathy (9 studies) and sleep disorders (11 studies), with psychosis assessed only once. Results indicated that patients with left predominant symptoms (LPD) exhibited more psychiatric symptoms compared to those with right predominant symptoms (RPD), who appeared less affected. Specifically, LPD patients showed increased depressive symptoms16,45,54,74,75,76,77, anxiety45,56,69,75,76, sleep disorders (including nocturnal hallucinations, disturbing dreams, and sleepiness)78,79,80, and psychosis35. A minority of studies reported higher rates of depression and anxiety in RPD patients51,79,81,82.
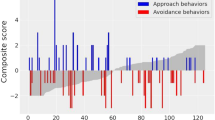
In contrast, RPD patients exhibited increased apathy19,52, magical ideation (i.e., belief that unrelated events are causally connected)56, sleep disorders83, hallucinations83, stress level19,79, and pathological gambling84. This suggests dissociated cerebral pathways for psychiatric symptoms, with anxio-depressive and sleep disturbance patterns prevalent in LPD patients, while apathy and gambling tendencies were more pronounced in RPD. Additionally, a recent study noted differing patterns of approach behavior, with LPD patients showing increased approach behavior, whereas avoidance behavior showed no differences between groups78. Some studies found no significant differences between LPD and RPD for various psychiatric symptoms42,44,48,53,57,72,73,85,86,87,88,89,90,91, while some studies revealed higher levels of symptoms (e.g., sleep disorders) in symmetric patients92. Most of these studies (70/80) were not cohort studies but involved selected patients with exclusion criteria for psychiatric symptoms, potentially introducing bias. In contrast, cohort studies, which include all patients, suggested significant differences16,35.
Effects of therapies on psychiatric symptoms as a function of motor symptom asymmetry
As in the case of cognitive symptoms, only a few studies have assessed the effects of PD therapies on psychiatric symptoms (e.g., depression, anxiety, apathy). Interestingly, both short- and long-term studies have shown an impact of STN-DBS on depressive symptoms, anxiety, and apathy, with effects dissociated according to asymmetry20,39,52. In detail, these few studies seem to suggest a reduction in apathy and anxiety in RPD, while in LPD, a reduction in depression was observed. On the other hand, Bove et al. 72 found no effect on depression. Long-term data suggest that patient groups tend to return to pre-DBS levels of psychiatric symptoms. As before, it is also important to bear in mind that psychiatric symptoms are part of the exclusion criteria for STN-DBS-type operations, thus inducing a recruitment bias for these studies.
Impact of motor asymmetry on emotional abilities in PD
Emotional processing as a function of motor symptom asymmetry
In terms of emotion abilities, the majority of studies have focused on emotion recognition abilities, in particular on the ability to recognize facial74,81,93,94 or vocal37,39,50,93,95 emotions. These studies highlighted reduced performance for emotion recognition abilities in LPD37,38,39,50,81,91,95,96, regardless of the valence of the emotions, with deficits for negative emotions (disgust50; anger50; sadness95), positive emotions (happiness)37,38,50, but also for the recognition of neutral stimuli39. Some studies showed no effects48,82,97, and others showed reduced performances at the same level in both groups as compared to healthy controls74,93,94, while only one study showed reduced abilities in RPD, but on measures of emotional valence of artworks55, not on stimuli with human characteristics. Concerning emotional production abilities, to date, only one study has assessed emotion production in facial modality, demonstrating, as in the case of recognition, alterations in LPD, in particular for the production of happiness and anger on patient’s faces90.
Effects of therapies on emotional processing as a function of motor symptom asymmetry
Regarding emotion recognition abilities, only one study39 assessed changes following STN-DBS, finding that patients with LPD showed normalization in emotional prosody recognition three months postoperatively. This normalization was evident in ratings for neutral, happy, and angry stimuli39. In contrast, RPD patients exhibited a postoperative decline in recognizing emotional prosody, despite comparable preoperative performance to the control group. Notably, significant differences were observed postoperatively for the Fear recognition. As emotional deficits are not typically included in the exclusion criteria for STN-DBS, these results suggest that they could serve as a crucial metric for evaluating asymmetry effects on non-motor symptoms in pre- and post-DBS scenarios, free from selection bias. However, the limited number of studies necessitates further confirmation.
Methodological limitations of the reviewed studies
The systematic literature review highlights five main groups of limitations across the included studies: (i) heterogeneity in experimental designs and assessment tools, (ii) variability in patient socio-demographic and clinical characteristics, (iii) inconsistency in methods used to calculate motor symptom asymmetry, (iv) insufficient control of confounding variables such as gender, medication status, and motor symptom subtypes, and (v) lack of standardization in the reporting and interpretation of concomitant treatments. These limitations often overlap and compound one another, making it difficult to compare results across studies and draw robust, generalizable conclusions regarding non-motor symptom expression in PD. Addressing these issues will require more harmonized research protocols and more systematic consideration of clinically relevant variables.
Experimental design and choices of tools
Most studies employed a cross-sectional experimental design, with only a minority conducting longitudinal evaluations. As a result, observations are limited to group-level characteristics, whereas longitudinal studies allow for both group and individual-level analyses, revealing changes or developments over time. Additionally, assessment tools varied, with different tests/questionnaires used to measure similar functions, often lacking comparability in psychometric properties. Furthermore, most studies focused on comparing raw scores, rather than examining the prevalence of deficient performance, which may offer a more sensitive measure of group differences.
Patient characteristics
Most studies involved highly heterogeneous patient samples, particularly in terms of disease duration, which varied from diagnosis to several decades post-diagnosis. This variability was seen both between and within study samples, often with wide ranges or large standard deviations. Another key factor distinguishing studies is the presence of a control group. Studies that included a control group tended to show more sensitive results, with some detecting reduced performance in one subgroup compared to healthy controls, which wasn’t apparent in patient-only comparisons. Additionally, certain studies considered other discriminant variables beyond asymmetry, such as motor symptom type58 or gender17.
Asymmetry calculation
One significant limitation of these studies, both methodologically and conceptually, is the calculation of asymmetry. One common method uses the asymmetry index based on part III of the Unified Parkinson’s Disease Rating Scale (UPDRS) motor items, subtracting left-side scores from right-side scores items16,20,37,38,39,52,72,78,98. Others use a standardized index [(Left UPDRS III symptoms—Right UPDRS III symptoms)/(Left UPDRS III symptoms + Right UPDRS III symptoms)]2,50,81. Some studies add thresholds (e.g., ±2) to define asymmetrical profiles, while others rely solely on the patient’s reported side of onset51,59. This inconsistency leads to variability in results, with some studies focusing on objectively measured asymmetry, while others consider the magnitude or subjective perception of asymmetry. Recently, some researchers have assessed asymmetry using DAT-SCAN, a neuroimaging technique that measures basal ganglia (BG) denervation. They applied an asymmetry index for the striatum using the formula (asymmetry index = (right putamen – left putamen specific binding ratio (SBR))/(right putamen + left putamen specific binding ratio (SBR))), setting a 20% asymmetry threshold2,99,100. This suggests that patients with less than 20% asymmetry may have symmetrical pathology, a method not yet applied to motor symptoms. Kaasinen2 explored the link between BG asymmetry and motor symptoms, finding that 8.1% of patients showed motor symptoms on the same side as BG denervation. DAT-SCAN-based asymmetry calculations focus on extreme asymmetry, facilitating the creation of a symmetrical group, while motor asymmetry using UPDRS lacks such thresholds. No study has established a motor-level cut-off for distinguishing symmetrical and asymmetrical groups. For instance, applying a 20% cut-off to UPDRS III could classify scores between +6 and −6 as symmetrical. Future studies comparing motor symmetry based on UPDRS-III with putamen dopaminergic asymmetry measured by DAT-SCAN are needed to address ongoing methodological debates.
Confounding biological and clinical moderators (e.g., gender, symptom subtype, medication effects)
Another limitation of the presently reviewed studies is the high heterogeneity across samples and methodologies. This variability arises from several confounding factors that are often insufficiently controlled or inconsistently reported. Gender differences, for instance, have been shown to influence both the clinical presentation and progression of PD101, with men typically showing greater executive dysfunction and women more emotional dysregulation. Moreover, gender and motor symptom asymmetry may interact17. Similarly, dopaminergic medication status critically modulates cognitive and affective performance102,103, and the effects can vary depending on baseline dopamine levels in different brain regions, potentially leading to both improvements and impairments in function. Additionally, motor symptom subtypes, such as tremor-dominant versus akinetic-rigid presentations, are rarely analyzed as separate subgroups, despite evidence that they are associated with distinct cognitive and psychiatric profiles104.
Inconsistent reporting of concomitant treatments and interacting pharmacological variables
Concomitant medications, particularly antidepressants and anxiolytics, which are frequently prescribed in PD populations, can significantly alter cognitive and emotional processing105, yet their influence is rarely accounted for in study designs or statistical models. As a result, these methodological inconsistencies limit the comparability of findings and hinder the identification of robust, generalizable patterns in the cognitive, psychiatric, and emotional domains of PD as a function of motor symptom asymmetry. Future research would benefit from adopting more standardized assessment protocols and controlling for these key variables to clarify the true nature of non-motor symptom expression in PD.
Discussion
The objective of this article was to systematically review the literature on how motor symptom asymmetry in PD impacts non-motor symptoms. From diagnosis and possibly from the prodromal phase, distinct cognitive and psychiatric trajectories emerge based on motor symptom asymmetry. Patients with left-predominant motor symptoms (LPD), indicative of right-hemisphere dysfunction, are more likely to exhibit psychiatric symptoms such as anxiety, depression, emotional recognition deficits, and visuospatial impairments. In contrast, patients with right-predominant motor symptoms (RPD), reflecting left-hemisphere pathology, show a greater propensity for global cognitive decline, particularly in memory and executive functions, which may increase their risk of developing dementia over time. These lateralized patterns underscore the importance of considering hemispheric involvement when assessing non-motor symptoms in Parkinson’s disease19,20.
Asymmetry in motor symptoms not only influences the progression of PD but also interacts with therapies like DRT and DBS. The cognitive outcomes of DBS appear vary based on motor symptom asymmetry20,39,52,71. Patients with LPD may be more vulnerable to neuropsychological decline following DBS. However, they often exhibit improvements in psychiatric symptoms and emotional recognition39,98. Conversely, patients with RPD may be less prone to cognitive side effects but could experience a worsening of affective symptoms post-treatment20,52. Recent machine learning studies, offering a complementary approach to clinical data, have reinforced the hypothesis that in the context of DBS, motor symptom asymmetry is an important factor to consider106.
Recent interest has grown in the relationship between motor symptom asymmetry and non-motor symptoms, revealing distinct patient phenotypes based on disease duration and treatment. RPD patients show pronounced deficits in memory, executive function, and language, likely linked to left hemisphere involvement in these cognitive tasks15. This hemispheric specialization may explain the variability observed in cognitive outcomes, particularly when patients are considered as a single group without being stratified based on asymmetry side or the symmetrical/asymmetrical nature of their pathology24,26. Conversely, LPD patients appear more susceptible to emotional and visuo-spatial processing deficits, aligning with the idea of right hemisphere lateralization for these functions. Moreover, LPD patients commonly report higher levels of anxiety and depressive symptoms, potentially indicating disruption of right hemisphere networks107,108. RPD patients seem more vulnerable to apathy, suggesting a link to long-term dementia risk19,20. Moreover, neuroimaging studies have identified distinct patterns of left hemispheric atrophy, either associated with motor symptom asymmetry109 or occurring independently of it22. These findings suggest that left hemisphere atrophy in patients with PD may be linked to dementia, thereby supporting the hypothesis of a greater vulnerability to cognitive decline in patients with right-sided motor symptoms (RPD). Complementary evidence from biomarker studies has also shown higher concentrations of dementia-related biomarkers in RPD patients16,99. Another, non-mutually exclusive, hypothesis posits that the presence of bilateral motor symptoms may also act as a risk factor for cognitive deterioration10,14,110, without necessarily contradicting the specific contribution of left hemispheric vulnerability.
The systematic review also highlights the emerging interest in how motor symptom asymmetry influences therapeutic management in PD, particularly concerning DBS. The findings suggest that the effects of STN-DBS on neuropsychological performance, psychiatric symptoms, and emotional processing vary based on motor symptom asymmetry20,39,52. Past studies on unilateral DBS may provide insights into these observations, revealing improved outcomes in the more affected hemisphere71. For instance, Hershey et al. 71 found that unilateral stimulation of the most affected brain region yielded significant effects on working memory tasks, particularly for LPD patients, suggesting greater right hemisphere involvement. Similar findings regarding DRT indicate that LPD patients often show more significant improvements in cognitive functions compared to RPD patients46. This underscores the need for nuanced approaches to therapy based on the asymmetry of motor symptoms. However, this area of research remains in its infancy, necessitating further validation through longitudinal studies with larger cohorts.
To integrate the observed differences into a cohesive framework, we propose a theoretical model outlining the evolution of cognitive, psychiatric, and emotional symptoms based on motor symptom asymmetry (see Fig. 2). This model visually synthesizes current evidence and illustrates two distinct trajectories emerging from the asymmetrical onset of motor symptoms. It also includes a schematic representation of cognitive symptom progression over time, highlighting the differing risks and profiles associated with right-versus left-sided motor onset. Importantly, the model emphasizes underexplored aspects, such as the role and evolution of symptomatology in patients with symmetrical motor presentations. By offering a comprehensive, asymmetry-informed perspective, this model complements traditional motor-focused frameworks and supports the development of more personalized clinical care strategies.
As extensively exposed in the Results section, significant methodological limitations exist in the studies reviewed, including heterogeneity in PD stages, socio-demographical characteristics, type of motor symptoms, medication, or psychometric tools. A lack of longitudinal evaluations, as well as epidemiological naturalistic follow-up (e.g., studies evaluating the evolution of symptoms, without exclusion/inclusion criteria’s), further complicates our understanding of the relationship between non-motor symptoms and motor (a)symmetry. While motor symptom asymmetry likely contributes to performance variability, additional factors like gender may also play a crucial role in the manifestation of non-motor symptoms in PD17,111,112. In addition, although we analyzed cognitive, psychiatric, and emotional symptoms separately, it is not possible to rule out potential interactions among them, interactions that may reveal a much more complex clinical picture. While some of the referenced studies report elevated levels of depression and anxiety in patient populations, they often lack detailed information on medication use, which limits our ability to assess its impact on cognitive outcomes. Future research would benefit from incorporating standardized assessments of mood symptoms and medication to better disentangle the respective contributions of depression and neurodegenerative processes to cognitive decline.
To conclude, from diagnosis and possibly even in the prodromal phase, two distinct cognitive, psychiatric, and emotional trajectories are observed based on motor symptom asymmetry in PD, potentially affecting patients’ daily quality of life. Patients with predominantly right motor symptoms (left brain alteration) tend to develop cognitive-apathetic non-motor symptoms and are at higher risk of long-term dementia. Conversely, patients with left motor symptoms (right brain alteration) are more likely to experience anxio-depressive symptoms, visuo-spatial disorders, and have a lower risk of developing dementia over time. These divergent profiles suggest a need to move beyond motor symptom classifications alone and consider asymmetry when tailoring interventions. Although the proposed model offers a promising structure for this purpose, further empirical validation is needed to refine and generalize its clinical relevance.
Methods
A literature review (not registrated) on published and reviewed articles was carried out until December 2023, using Web of Science (webofknowledge.com), based on PRISMA criteria with the following search items: ((((((((((((((ALL = (Parkinson’s disease)) OR ALL = (PD)) AND ALL = (motor asymmetry)) OR ALL = (lateralization)) OR ALL = (side of onset)) OR ALL = (hemi-park*)) OR ALL = (disconnect*)) AND ALL = (non-motor)) OR ALL = (NMS))))))). Additional studies were subsequently extracted from the lists of references. The following exclusion criteria were applied during the data extraction process: (i) non-relevant topic; (ii) non-human studies; (iii) no mention of asymmetry/lateralization/side of onset/hemi-parkinsonism/disconnectivity; (iv) absence of non-motor assessment (cognition, psychiatry and/or emotion disorders); (v) not an original article (exclusion of reviews and meta-analysis). The objective was to extract from the studies the clinical data and socio-demographic characteristics of the evaluated patients (e.g., disease duration, asymmetry assessment, type of motor symptoms such as tremor, bradykinesia, or akinesia, specific anti-Parkinsonian medications, and other concomitant treatments, gender), the methodological characteristics of the studies (e.g., longitudinal or translational design), information on implemented therapies (e.g., DBS), as well as data on assessed non-motor symptoms (e.g., neuropsychological tests, psychiatric questionnaires or assessments). Tables 1–3.
References
Hobson, D. E. Asymmetry in parkinsonism, spreading pathogens and the nose. Parkinsonism Relat. Disord. 18, 1–9 (2012).
Kaasinen, V. Ipsilateral deficits of dopaminergic neurotransmission in Parkinson’s disease. Ann. Clin. Transl. Neurol. 3, 21–26 (2016).
Kumakura, Y., Gjedde, A., Danielsen, E. H., Christensen, S. & Cumming, P. Dopamine storage capacity in caudate and putamen of patients with early Parkinson’s disease: correlation with asymmetry of motor symptoms. J. Cereb. Blood Flow. Metab. 26, 358–370 (2006).
Gorell, J. et al. Increased iron-related MRI contrast in the substantia nigra in Parkinson’s disease. Neurology 45, 1138–1143 (1995).
Djaldetti, R., Ziv, I. & Melamed, E. The mystery of motor asymmetry in Parkinson’s disease. Lancet Neurol. 5, 796–802 (2006).
Lee, C. et al. Patterns of asymmetry do not change over the course of idiopathic parkinsonism: implications for pathogenesis. Neurology 45, 435–439 (1995).
Morrish, P., Sawle, G. & Brooks, D. Clinical and [18F] dopa PET findings in early Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 59, 597–600 (1995).
Tatsch, K. et al. Relationship between clinical features of Parkinson’s disease and presynaptic dopamine transporter binding assessed with [123 I] IPT and single-photon emission tomography. Eur. J. Nucl. Med. 24, 415–421 (1997).
Braak, H., Rub, U. & Del Tredici, K. Involvement of precerebellar nuclei in multiple system atrophy. Neuropathol. Appl. Neurobiol. 29, 60–76 (2003).
Borghammer, P. The α-synuclein origin and connectome model (SOC Model) of Parkinson’s disease: explaining motor asymmetry, non-motor phenotypes, and cognitive decline. J. Parkinson’s Dis. 11, 455–474 (2021).
Knudsen, K. et al. Asymmetric dopaminergic dysfunction in brain-first versus body-first Parkinson’s disease subtypes. J. Parkinson’s Dis. 11, 1677–1687 (2021).
Borghammer, P. The α-synuclein origin and connectome model (SOC Model) of parkinson’s disease: explaining motor asymmetry, non-motor phenotypes, and cognitive decline. J. Parkinson’s Dis. 11, 455 (2021).
Borghammer, P. The brain-first vs. body-first model of Parkinson’s disease with comparison to alternative models. J. Neural Trans. 130, 1-17 (2023).
Borghammer, P. et al. A postmortem study suggests a revision of the dual-hit hypothesis of Parkinson’s disease. npj Parkinson’s Dis. 8, 166 (2022).
Lubben, N., Ensink, E., Coetzee, G. A. & Labrie, V. The enigma and implications of brain hemispheric asymmetry in neurodegenerative diseases. Brain Commun. 3, fcab211 (2021).
Voruz, P., Constantin, I. M. & Péron, J. A. Biomarkers and non-motor symptoms as a function of motor symptom asymmetry in early Parkinson’s disease. Neuropsychologia 177, 108419 (2022).
Constantin, I. M., Voruz, P. & Péron, J. A. Moderating effects of uric acid and sex on cognition and psychiatric symptoms in asymmetric Parkinson’s disease. Biol. Sex. Differ. 14, 1–11 (2023).
Coundouris, S. P. et al. A meta-analytic review of prospection deficits in Parkinson’s disease. Neurosci. Biobehav. Rev. 108, 34–47 (2020).
Harris, E., McNamara, P. & Durso, R. Apathy in patients with Parkinson disease as a function of side of onset. J. Geriatr. Psychiatry Neurol. 26, 95–104 (2013).
Voruz, P. et al. Motor symptom asymmetry predicts cognitive and neuropsychiatric profile following deep brain stimulation of the subthalamic nucleus in Parkinson’s disease: a 5-year longitudinal study. Arch. Clin. Neuropsychol. 38, 904–912 (2023).
Starkstein, S. E. & Leiguarda, R. Neuropsychological correlates of brain atrophy in Parkinson’s disease: a CT-scan study. Mov. Disord. 8, 51–55 (1993).
Claassen, D. O. et al. Cortical asymmetry in Parkinson’s disease: early susceptibility of the left hemisphere. Brain Behav. 6, e00573 (2016).
Elbaz, A. et al. Survival study of Parkinson disease in Olmsted County, Minnesota. Arch. Neurol. 60, 91–96 (2003).
Riederer, P. et al. Lateralisation in Parkinson disease. Cell tissue Res. 373, 297–312 (2018).
Steinbach, M. J., Campbell, R. W., DeVore, B. B. & Harrison, D. W. Laterality in Parkinson’s disease: a neuropsychological review. Appl. Neuropsychol. Adult 30, 126–140 (2023).
Verreyt, N., Nys, G. M., Santens, P. & Vingerhoets, G. Cognitive differences between patients with left-sided and right-sided Parkinson’s disease. A review. Neuropsychol. Rev. 21, 405–424 (2011).
Tombaugh, T., McDowell, I., Kristjansson, B. & Hubley, A. Mini-Mental State Examination (MMSE) and the Modified MMSE (3MS): a psychometric comparison and normative data. Psychol. Assess. 8, 48 (1996).
Nasreddine, Z. S. et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatrics Soc. 53, 695–699 (2005).
Lucas, J. A. et al. Normative data for the Mattis dementia rating scale. J. Clin. Exp. Neuropsychol. 20, 536–547 (1998).
Brown, G. G. et al. Validity of the Dementia Rating Scale in assessing cognitive function in Parkinson’s disease. J. Geriatr. Psychiatry Neurol. 12, 180–188 (1999).
Nelson, H. & Willison, J. National adult reading test (NART) manual. Windsor, Berkshire, UK: NFER-Nelson (1982).
Serrano-Dueñas, M., Calero, B., Serrano, S., Serrano, M. & Coronel, P. Metric properties of the mini-mental Parkinson and SCOPA-COG scales for rating cognitive deterioration in Parkinson’s disease. Mov. Disord. 25, 2555–2562 (2010).
Agosta, S. et al. Lateralized cognitive functions in Parkinson’s patients: a behavioral approach for the early detection of sustained attention deficits. Brain Res. 1726, 146486 (2020).
Cooper, C. et al. Does laterality of motor impairment tell us something about cognition in Parkinson disease?. Parkinsonism Relat. Disord. 15, 315–317 (2009).
Cubo, E. et al. Motor laterality asymmetry and nonmotor symptoms in Parkinson’s disease. Mov. Disord. 25, 70–75 (2010).
Harris, E., McNamara, P. & Durso, R. Novelty seeking in patients with right-versus left-onset Parkinson disease. Cogn. Behav. Neurol. 28, 11–16 (2015).
Stirnimann, N. et al. Hemispheric specialization of the basal ganglia during vocal emotion decoding: Evidence from asymmetric Parkinson’s disease and 18FDG PET. Neuropsychologia 119, 1–11 (2018).
Thomasson, M. et al. Crossed functional specialization between the basal ganglia and cerebellum during vocal emotion decoding: insights from stroke and Parkinson’s disease. Cogn. Affect. Behav. Neurosci. 22, 1030–1043 (2022).
Voruz, P. et al. Motor symptom asymmetry in Parkinson’s disease predicts emotional outcome following subthalamic nucleus deep brain stimulation. Neuropsychologia 144, 107494 (2020).
Skorvanek, M. et al. Global scales for cognitive screening in Parkinson’s disease: critique and recommendations. Mov. Disord. 33, 208–218 (2018).
Nys, G. M., Santens, P. & Vingerhoets, G. Horizontal and vertical attentional orienting in Parkinson’s disease. Brain Cogn. 74, 179–185 (2010).
Smith, J. et al. Motor asymmetry and estimation of body-scaled aperture width in Parkinson’s disease. Neuropsychologia 49, 3002–3010 (2011).
Huber, S. J., Miller, H., Bohaska, L., Christy, J. A. & Bornstein, R. A. Asymmetrical cognitive differences associated with hemiparkinsonism. Arch. Clin. Neuropsychol. 7, 471–480 (1992).
Mohr, E. et al. Neuropsychological and glucose metabolic profiles in asymmetric Parkinson’s disease. Can. J. Neurol. Sci. 19, 163–169 (1992).
Foster, P. S. et al. Anxiety affects working memory only in left hemibody onset Parkinson disease patients. Cogn. Behav. Neurol. 23, 14–18 (2010).
Hanna-Pladdy, B., Pahwa, R. & Lyons, K. E. Paradoxical effect of dopamine medication on cognition in Parkinson’s disease: relationship to side of motor onset. J. Int. Neuropsychol. Soc. 21, 259–270 (2015).
Starkstein, S., Leiguarda, R., Gershanik, O. & Berthier, M. Neuropsychological disturbances in hemiparkinson’s disease. Neurology 37, 1762–1762 (1987).
Blonder, L. X., Gur, R. E. & Gur, R. C. The effects of right and left hemiparkinsonism on prosody. Brain Lang. 36, 193–207 (1989).
Spicer, K. B., Roberts, R. J. & LeWitt, P. A. Neuropsychological performance in lateralized parkinsonism. Arch. Neurol. 45, 429–432 (1988).
Garrido-Vásquez, P. et al. An ERP study of vocal emotion processing in asymmetric Parkinson’s disease. Soc. Cogn. Affect. Neurosci. 8, 918–927 (2013).
Tomer, R., Aharon-Peretz, J. & Tsitrinbaum, Z. Dopamine asymmetry interacts with medication to affect cognition in Parkinson’s disease. Neuropsychologia 45, 357–367 (2007).
Voruz, P. et al. Motor symptom asymmetry predicts non-motor outcome and quality of life following STN DBS in Parkinson’s disease. Sci. Rep. 12, 3007 (2022).
Finali, G., Piccirilli, M. & Rizzuto, S. Neuropsychological characteristics of parkinsonian patients with lateralized motor impairment. J. Neural. Transm. 9, 165–176 (1995).
Foster, P. S., Yung, R. C., Drago, V., Crucian, G. P. & Heilman, K. M. Working memory in Parkinson’s disease: the effects of depression and side of onset of motor symptoms. Neuropsychology 27, 303 (2013).
Ciccarelli, N. et al. Emotional valence may influence memory performance for visual artworks in Parkinson’s disease. Neurol. Sci. 40, 2175–2178 (2019).
Modestino, E. J., Amenechi, C., Reinhofer, A. & O’Toole, P. Side-of-onset of Parkinson’s disease in relation to neuropsychological measures. Brain Behav. 7, e00590 (2017).
Karádi, K. et al. Visuospatial impairment in Parkinson’s disease: the role of laterality. Laterality Asymmetries Body Brain Cogn. 20, 112–127 (2015).
Katzen, H. L., Levin, B. E. & Weiner, W. Side and type of motor symptom influence cognition in Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 21, 1947–1953 (2006).
Tomer, R., Levin, B. E. & Weiner, W. J. Side of onset of motor symptoms influences cognition in Parkinson’s disease. Ann. Neurol. Off. J. Am. Neurol. Assoc. Child Neurol. Soc. 34, 579–584 (1993).
Amick, M., Grace, J. & Chou, K. Body side of motor symptom onset in Parkinson’s disease is associated with memory performance. J. Int. Neuropsychol. Soc. 12, 736–740 (2006).
Holtgraves, T., McNamara, P., Cappaert, K. & Durso, R. Linguistic correlates of asymmetric motor symptom severity in Parkinson’s disease. Brain Cogn. 72, 189–196 (2010).
Agniel, A. et al. Cognition and cerebral blood flow in lateralised Parkinsonism: lack of functional lateral asymmetries. J. Neurol. Neurosurg. Psychiatry 54, 783–786 (1991).
Davidsdottir, S., Cronin-Golomb, A. & Lee, A. Visual and spatial symptoms in Parkinson’s disease. Vis. Res. 45, 1285–1296 (2005).
Ren, X. et al. Veering in hemi-Parkinson’s disease: primacy of visual over motor contributions. Vis. Res. 115, 119–127 (2015).
Schendan, H. E., Amick, M. M. & Cronin-Golomb, A. Role of a lateralized parietal-basal ganglia circuit in hierarchical pattern perception: evidence from Parkinson’s disease. Behav. Neurosci. 123, 125 (2009).
Ebersbach, G. et al. Directional bias of initial visual exploration: a symptom of neglect in Parkinson’s disease. Brain 119, 79–87 (1996).
Lee, A., Harris, J., Atkinson, E. & Fowler, M. Evidence from a line bisection task for visuospatial neglect in left hemiparkinson’s disease. Vis. Res. 41, 2677–2686 (2001).
Villardita, C., Smirni, P. & Zappalà, G. Visual neglect in Parkinson’s disease. Arch. Neurol. 40, 737–739 (1983).
Kurlawala, Z., Shadowen, P. H., McMillan, J. D., Beverly, L. J. & Friedland, R. P. Progression of nonmotor symptoms in Parkinson’s disease by sex and motor laterality. Parkinson’s Dis. 2021, 8898887 (2021).
Voruz, P. et al. Differential effects of disease duration and dopaminergic replacement therapy on vocal emotion recognition in asymmetric Parkinson’s disease. Neurodegener. Dis. 24, 129–140 (2025).
Hershey, T. et al. Unilateral vs. bilateral STN DBS effects on working memory and motor function in Parkinson disease. Exp. Neurol. 210, 402–408 (2008).
Bove, F. et al. Does motor symptoms asymmetry predict motor outcome of subthalamic deep brain stimulation in Parkinson’s disease patients?. Front. Hum. Neurosci. 16, 931858 (2022).
DeGutis, J. et al. Side of motor symptom onset predicts sustained attention deficits and motor improvements after attention training in Parkinson’s disease. Neuropsychologia 190, 108698 (2023).
Clark, U. S., Neargarder, S. & Cronin-Golomb, A. Specific impairments in the recognition of emotional facial expressions in Parkinson’s disease. Neuropsychologia 46, 2300–2309 (2008).
Fleminger, S. Left-sided Parkinson’s disease is associated with greater anxiety and depression. Psychol. Med. 21, 629–638 (1991).
Foster, P. S. et al. Anxiety and depression severity are related to right but not left onset Parkinson’s disease duration. J. Neurol. Sci. 305, 131–135 (2011).
Pellicano, C. et al. Neuropsychiatric and cognitive symptoms and body side of onset of Parkinsonism in unmedicated Parkinson’s disease patients. Parkinsonism Relat. Disord. 21, 1096–1100 (2015).
Béreau, M. et al. Imbalanced motivated behaviors according to motor sign asymmetry in drug-naïve Parkinson’s disease. Sci. Rep. 13, 21234 (2023).
Stavitsky, K. et al. Hallucinations, dreaming and frequent dozing in Parkinson’s disease: Impact of right-hemisphere neural networks. Cogn. Behav. Neurol. Off. J. Soc. Behav. Cogn. Neurol. 21, 143 (2008).
Zhu, S. et al. The association between clinical characteristics and motor symptom laterality in patients with Parkinson’s disease. Front. Neurol. 12, 663232 (2021).
Garrido-Vásquez, P., Pell, M. D., Paulmann, S., Sehm, B. & Kotz, S. A. Impaired neural processing of dynamic faces in left-onset Parkinson’s disease. Neuropsychologia 82, 123–133 (2016).
St. Clair, J., Borod, J. C., Sliwinski, M., Cote, L. J. & Stern, Y. Cognitive and affective functioning in Parkinson’s disease patients with lateralized motor signs. J. Clin. Exp. Neuropsychol. 20, 320–327 (1998).
Rodríguez-Violante, M., Cervantes-Arriaga, A., Villar-Velarde, A. & Corona, T. Relationship between the type and side of motor symptoms with the prevalence of non-motor symptoms in Parkinson’s disease. Neurología 26, 319–324 (2011).
Voon, V. et al. Factors associated with dopaminergic drug–related pathological gambling in Parkinson disease. Arch. Neurol. 64, 212–216 (2007).
Adwani, S., Yadav, R., Kumar, K., Chandra, S. & Pal, P. K. Neuropsychological profile in early Parkinson’s disease: Comparison between patients with right side onset versus left side onset of motor symptoms. Ann. Indian Acad. Neurol. 19, 74 (2016).
Barber, J., Tomer, R., Sroka, H. & Myslobodsky, M. S. Does unilateral dopamine deficit contribute to depression?. Psychiatry Res. 15, 17–24 (1985).
Direnfeld, L. K. et al. Parkinson’s disease: the possible relationship of laterality to dementia and neurochemical findings. Arch. Neurol. 41, 935–941 (1984).
Elkurd, M., Wang, J. & Dewey, R. B. Jr Lateralization of motor signs affects symptom progression in Parkinson disease. Front. Neurol. 12, 711045 (2021).
Poletti, M. et al. The relationship between motor symptom lateralization and cognitive performance in newly diagnosed drug-naïve patients with Parkinson’s disease. J. Clin. Exp. Neuropsychol. 35, 124–131 (2013).
Ratajska, A. M. et al. Laterality of motor symptom onset and facial expressivity in Parkinson disease using face digitization. Laterality 27, 57–70 (2022).
Yuvaraj, R. & Murugappan, M. Hemispheric asymmetry non-linear analysis of EEG during emotional responses from idiopathic Parkinson’s disease patients. Cogn. Neurodyn. 10, 225–234 (2016).
Hansen, F. O. et al. Non-motor asymmetry and dopamine degeneration in Parkinson’s disease. Brain Commun. 7, fcaf002 (2025).
Buxton, S. L., MacDonald, L. & Tippett, L. J. Impaired recognition of prosody and subtle emotional facial expressions in Parkinson’s disease. Behav. Neurosci. 127, 193 (2013).
Clark, U. S., Neargarder, S. & Cronin-Golomb, A. Visual exploration of emotional facial expressions in Parkinson’s disease. Neuropsychologia 48, 1901–1913 (2010).
Ventura, M. I. et al. Hemispheric asymmetries and prosodic emotion recognition deficits in Parkinson’s disease. Neuropsychologia 50, 1936–1945 (2012).
Yuvaraj, R., Murugappan, M. & Palaniappan, R. The effect of lateralization of motor onset and emotional recognition in PD patients using EEG. Brain Topogr. 30, 333–342 (2017).
Kalampokini, S. et al. Facial emotion recognition in Parkinson’s disease: association with age and olfaction. J. Clin. Exp. Neuropsychol. 40, 274–284 (2018).
Benis, D. et al. Subthalamic nucleus oscillations during vocal emotion processing are dependent of the motor asymmetry of Parkinson’s disease. NeuroImage 222, 117215 (2020).
Fiorenzato, E., Antonini, A., Bisiacchi, P., Weis, L. & Biundo, R. Asymmetric dopamine transporter loss affects cognitive and motor progression in Parkinson’s disease. Mov. Disord. 36, 2303–2313 (2021).
Scherfler, C. et al. Left hemispheric predominance of nigrostriatal dysfunction in Parkinson’s disease. Brain 135, 3348–3354 (2012).
Miller, I. N. & Cronin-Golomb, A. Gender differences in Parkinson’s disease: clinical characteristics and cognition. Mov. Disord. 25, 2695–2703 (2010).
Cools, R. et al. Role of dopamine and clinical heterogeneity in cognitive dysfunction in Parkinson’s disease. Prog. Brain Res. 269, 309–343 (2022).
Aarsland, D. et al. Parkinson disease-associated cognitive impairment. Nat. Rev. Dis. Prim. 7, 47 (2021).
Burn, D. et al. Motor subtype and cognitive decline in Parkinson’s disease, Parkinson’s disease with dementia, and dementia with Lewy bodies. J. Neurol. Neurosurg. Psychiatry 77, 585–589 (2006).
Marsh, L. Depression and Parkinson’s disease: current knowledge. Curr. Neurol. Neurosci. Rep. 13, 1–9 (2013).
Ferrea, E., Negahbani, F., Cebi, I., Weiss, D. & Gharabaghi, A. Machine learning explains response variability of deep brain stimulation on Parkinson’s disease quality of life. npj Digital Med. 7, 269 (2024).
Rotenberg, V. S. The peculiarity of the right-hemisphere function in depression: solving the paradoxes. Prog. Neuro Psychopharmacol. Biol. Psychiatry 28, 1–13 (2004).
Wang, Q. et al. Alterations of regional spontaneous brain activities in anxiety disorders: a meta-analysis. J. Affect. Disord. 296, 233–240 (2022).
Danti, S. et al. Cortical thickness in de novo patients with Parkinson disease and mild cognitive impairment with consideration of clinical phenotype and motor laterality. Eur. J. Neurol. 22, 1564–1572 (2015).
Borghammer, P. et al. Neuropathological evidence of body-first vs. brain-first Lewy body disease. Neurobiol. Dis. 161, 105557 (2021).
Kang, K. W., Choi, S.-M. & Kim, B. C. Gender differences in motor and non-motor symptoms in early Parkinson disease. Medicine 101, e28643 (2022).
Martinez-Martin, P. et al. Gender-related differences in the burden of non-motor symptoms in Parkinson’s disease. J. Neurol. 259, 1639–1647 (2012).
Bowen, F. P., Hoehn, M. M. & Yahr, M. D. Cerebral dominance in relation to tracking and tapping performance in patients with Parkinsonism. Neurology 22, 32–9 (1972).
Cicero, C. E. et al. Exploring the relation between REM sleep behavior disorder onset and striatal dopaminergic dysfunction in Parkinson’s Disease. J. Neurol. 272, 1–8 (2025).
Cubo, E. et al. Effects of motor symptom laterality on clinical manifestations and quality of life in Parkinson’s disease. J. Parkinson’s Dis. 10, 1611–1620 (2020).
Di Caprio, V., Modugno, N., Mancini, C., Olivola, E. & Mirabella, G. Early-stage Parkinson’s patients show selective impairment in reactive but not proactive inhibition. Mov. Disord. 35, 409–418 (2020).
Dominey, P., Decety, J., Broussolle, E., Chazot, G. & Jeannerod, M. Motor imagery of a lateralized sequential task is asymmetrically slowed in hemi-Parkinson’s patients. Neuropsychologia 33, 727–741 (1995).
Erro, R. et al. Side of onset does not influence cognition in newly diagnosed untreated Parkinson’s disease patients. Parkinsonism Relat. Disord. 19, 256–259 (2013).
McNamara, P., Stavitsky, K., Harris, E., Szent-Imrey, O. & Durso, R. Mood, side of motor symptom onset and pain complaints in Parkinson’s disease. Int. J. Geriatr. Psychiatry. 25, 519–524 (2010).
Mirabella, G., Fragola, M., Giannini, G., Modugno, N. & Lakens, D. Inhibitory control is not lateralized in Parkinson’s patients. Neuropsychologia 102, 177–189 (2017).
Nuber-Champier, A., Voruz, P., Constantin, I., Cionca, A. & Péron, J. A. Cerebrospinal ceramides and cognition as a function of striatal asymmetry in early stage of Parkinson’s disease. J. Parkinson’s Dis. 1877718X251319242 (2024).
Smith, J. G. et al. Perceptual bias for affective and nonaffective information in asymmetric Parkinson’s disease. Neuropsychology 24, 443 (2010).
Viitanen, M., Mortimer, J. & Webster, D. Association between presenting motor symptoms and the risk of cognitive impairment in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 57, 1203–1207 (1994).
Wright, W. G., Gurfinkel, V., King, L. & Horak, F. Parkinson’s disease shows perceptuomotor asymmetry unrelated to motor symptoms. Neurosci. Lett. 417, 10–15 (2007).
Zhang, L. et al. Aberrant changes in cortical complexity in right-onset versus left-onset parkinson’s disease in early-stage. Front. Aging Neurosci. 13, 749606 (2021).
Noone, P. Addenbrooke’s cognitive examination-III. Occup. Med. 65, 418–420 (2015).
Barbizet, J. & Cany, E. A psychometric study of various memory deficits associated with cerebral lesions. Pathol. Memory 49-64 (1969).
Fong, M. W., Van Patten, R. & Fucetola, R. P. The factor structure of the Boston diagnostic aphasia examination. J. Int. Neuropsychol. Soc. 25, 772–776 (2019).
Riccio, C. A. & Hynd, G. W. Validity of Benton’s judgement of line orientation test. J. Psychoeduc. Assess. 10, 210–218 (1992).
Welsh, K. A. et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part V. A normative study of the neuropsychological battery. Neurology 44, 609–609 (1994).
Benton, A., Hamsher, D. S. & Sivan, A. Controlled oral word association test. Arch. Clin. Neuropsychol. (1994).
Norman, M. A., Evans, J. D., Miller, W. S. & Heaton, R. K. Demographically corrected norms for the California verbal learning test. J. Clin. Exp. Neuropsychol. 22, 80–94 (2000).
Homack, S., Lee, D. & Riccio, C. A. Test review: Delis-Kaplan executive function system. J. Clin. Exp. Neuropsychol. 27, 599–609 (2005).
Dubois, B., Slachevsky, A., Litvan, I. & Pillon, B. The FAB: a frontal assessment battery at bedside. Neurology 55, 1621–1626 (2000).
Benedict, R. H., Schretlen, D., Groninger, L. & Brandt, J. Hopkins Verbal Learning Test–Revised: Normative data and analysis of inter-form and test-retest reliability. Clin. Neuropsychol. 12, 43–55 (1998).
Kawas, C., Karagiozis, H., Resau, L., Corrada, M. & Brookmeyer, R. Reliability of the Blessed Telephone Information-Memory-Concentration Test. J. Geriatr. Psychiatry Neurol. 8, 238–242 (1995).
Pennebaker, J. W., Francis, M. E. & Booth, R. J. Linguistic inquiry and word count: LIWC 2001. Mahway Lawrence Erlbaum Assoc. 71, 2001 (2001).
Marra, C. et al. The Multiple Features Target Cancellation (MFTC): an attentional visual conjunction search test. Normative values for the Italian population. Neurol. Sci. 34, 173–180 (2013).
Blair, J. R. & Spreen, O. Predicting premorbid IQ: a revision of the National Adult Reading Test. Clin. Neuropsychol. 3, 129–136 (1989).
Rey, A. L’examen clinique en psychologie (Presses Universitaries De France, 1958).
Randolph, C. Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) (Psychological Corporation, 1998).
Shin, M.-S., Park, S.-Y., Park, S.-R., Seol, S.-H. & Kwon, J. S. Clinical and empirical applications of the Rey–Osterrieth complex figure test. Nat. Protoc. 1, 892–899 (2006).
Jensen, A. R. & Rohwer, W. D. Jr The Stroop color-word test: a review. Acta Psychol. 25, 36–93 (1966).
Kortte, K. B., Horner, M. D. & Windham, W. K. The trail making test, part B: cognitive flexibility or ability to maintain set? Appl. Neuropsychol. 9, 106–109 (2002).
Langdon, D. W. & Warrington, E. K. VESPAR: Verbal and Spatial Reasoning Test (Psychology Press, 1995).
Hartman, D. E. Wechsler Adult Intelligence Scale IV (WAIS IV): return of the gold standard. Appl. Neuropsychol. 16, 85–87 (2009).
Mountain, M. A. & Snow, W. G. Wisconsin Card Sorting Test as a measure of frontal pathology: a review. Clin. Neuropsychol. 7, 108–118 (1993).
Elwood, R. W. The wechsler memory scale—revised: psychometric characteristics and clinical application. Neuropsychol. Rev. 2, 179–201 (1991).
Ginsberg, J. Review of wechsler test of adult reading. J. Psychoeduc. Assess. 29, 581–586 (2003).
Marin, R. S., Biedrzycki, R. C. & Firinciogullari, S. Reliability and validity of the Apathy Evaluation Scale. Psychiatry Res. 38, 143–162 (1991).
Rieu, I. et al. International validation of a behavioral scale in Parkinson’s disease without dementia. Mov. Disord. 30, 705–713 (2015).
Vasconcelos, A. G., Malloy-Diniz, L. & Correa, H. Systematic review of psychometric proprieties of Barratt Impulsiveness Scale Version 11 (BIS-11). Clin. Neuropsychiatry 9, 61–74 (2012).
Beck, A. T., Epstein, N., Brown, G. & Steer, R. Beck anxiety inventory. Journal of consulting and clinical psychology (1993).
Beck, A. T., Steer, R. A. & Brown, G. K. Beck depression inventory (Harcourt Brace Jovanovich, 1987).
Gioia, G. A., Isquith, P. K., Guy, S. C. & Kenworthy, L. Test review behavior rating inventory of executive function. Child Neuropsychol. 6, 235–238 (2000).
Parkitny, L. & McAuley, J. The depression anxiety stress scale (DASS). J. Physiother. 56, 204 (2010).
Kent, L., Vostanis, P. & Feehan, C. Detection of major and minor depression in children and adolescents: evaluation of the Mood and Feelings Questionnaire. J. Child Psychol. Psychiatry 38, 565–573 (1997).
Montorio, I. & Izal, M. The Geriatric Depression Scale: a review of its development and utility. Int. Psychogeriatr. 8, 103–112 (1996).
Thompson, E. Hamilton rating scale for anxiety (HAM-A). Occup. Med. 65, 601–601 (2015).
Sharp, R. The Hamilton rating scale for depression. Occup. Med. 65, 340–340 (2015).
Davidson, J., Turnbull, C. D., Strickland, R., Miller, R. & Graves, K. The montgomery-åsberg depression scale: reliability and validity. Acta Psychiatr. Scandinavica 73, 544–548 (1986).
Jenkinson, C., Fitzpatrick, R., Peto, V., Greenhall, R. & Hyman, N. The Parkinson’s Disease Questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Age Ageing 26, 353–357 (1997).
Trenkwalder, C. et al. Parkinson’s disease sleep scale—validation of the revised version PDSS-2. Mov. Disord. 26, 644–652 (2011).
Wing, J. K., Mann, S. A., Leff, J. P. & Nixon, J. M. The concept of a ‘case’ in psychiatric population surveys. Psychol. Med. 8, 203–217 (1978).
Buysse, D. J., Reynolds, C. F. III, Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213 (1989).
Jenkins, R., Mann, A. & Belsey, E. The background, design and use of a short interview to assess social stress and support in research and clinical settings. Soc. Sci. Med. Part E Med. Psychol. 15, 195–203 (1981).
Spielberger, C. D. State-Trait Anxiety Inventory For Adults (Consulting Psychologists Press, 1983).
Biggs, J. T., Wylie, L. T. & Ziegler, V. E. Validity of the Zung self-rating depression scale. Br. J. Psychiatry 132, 381–385 (1978).
Acknowledgements
The present study was performed at the Clinical and Experimental Neuropsychology Laboratory (CENLab) within the Faculty of Psychology and Educational Sciences (FPSE) of the University of Geneva (UNIGE). The first author was funded by Institutional Funds of the State of Geneva (PI: Péron) and by Swiss National Science Foundation (SNSF) Project grant to J.A.P. (PI) (grant no. 105314_215015). The funders had no role in data collection, discussion of content, preparation of the manuscript, or decision to publish.
Author information
Authors and Affiliations
Contributions
P.V.: writing—original draft preparation; data curation; formal analysis D.G.: data curation; review and editing J.A.P.: formal analysis; data curation; resources; investigation; project administration; writing—review and editing; funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Voruz, P., Guérin, D. & Péron, J.A. Impact of motor symptom asymmetry on non-motor outcomes in Parkinson’s disease: a systematic review. npj Parkinsons Dis. 11, 188 (2025). https://doi.org/10.1038/s41531-025-01046-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-01046-4
This article is cited by
-
Striatal (a-)symmetry reveals sex-specific autonomic vulnerabilities in early Parkinson’s disease
npj Women's Health (2026)
-
Is motor asymmetry a predictor of non-motor outcomes in Parkinson’s disease?
Journal of Neural Transmission (2026)