Abstract
While bilateral high-frequency subthalamic nucleus stimulation (Bi-HFS) frequently worsens speech in Parkinson’s disease (PD), low-frequency stimulation (LFS) may alleviate gait deficits but lacks robust evidence for speech benefits. This randomized trial compared Bi-LFS (60 Hz) and Bi-HFS (130 Hz) in 33 PD patients with postural instability/gait difficulty (PIGD), and evaluated asymmetric frequency stimulation (AFS) in 20 patients. Bi-LFS significantly improved dysphonia severity index (DSI, FDR-p = 0.024), maximum phonation time (MPT, FDR- p = 0.025), and subjective speech ratings compared to Bi-HFS. Left-LFS/right-HFS (L-LFS/R-HFS) matched Bi-LFS efficacy and surpassed Bi-HFS in objective measures (FDR-p ≤ 0.021). Speech improvements correlated with motor/gait gains, independent of tremor. Findings suggest Bi-LFS mitigates speech dysfunction in PIGD-PD, with left-sided LFS potentially driving benefits, while AFS provides comparable outcomes. These data support tailored stimulation protocols to optimize speech in PD. The National Medical Research Registration and Information System of China (MR-31-23-036810).
Similar content being viewed by others
Introduction
Beyond the cardinal motor impairments, patients with Parkinson’s disease (PwPD) suffer from progressive voice and speech function deterioration, manifesting as dysphonia and hypokinetic dysarthria. These impairments are primarily characterized by a breathy and harsh voice, reduced vocal intensity, monotonic pitch, variable speech rate and rhythm, and imprecise articulation1,2. The neuropathological mechanisms underlying the voice and speech abnormalities of PD have not been well characterized. In early-stage PD, the affected brainstem impairs glossopharyngeal and vagus nerves that control laryngeal/pharyngeal muscles and respiratory-articulatory coordination, causing initial abnormalities in speech and voice3. Subsequent nigrostriatal degeneration exacerbates bradykinesia and rigidity in relevant musculature (parallel to limb symptoms), while sensorimotor, affective, and cognitive deficits further compound speech impairments4,5. The multifactorial and incompletely elucidated pathogenesis renders limited therapeutic efficacy and high interindividual variability with conventional treatments.
Subthalamic nucleus (STN) deep brain stimulation (DBS) is a well-established neuromodulation therapy for advanced PD. However, its effects on dysarthria and dysphonia remain controversial, but are generally considered detrimental6. The effects of STN DBS on speech and voice functions are influenced by multiple factors, including stimulating frequency, intensity, and laterality2,6,7. High-frequency and high-intensity stimulation, as well as left-sided stimulation (compared to right-sided) has been reported to be associated with speech and voice worsening6. Furthermore, similar to the asymmetric progression of motor symptoms in PD, the control of speech and voice functions may also be hemisphere-specific8. These characteristics highlight a potential clinical need for individualized programming strategies to optimize DBS for speech and voice functions: selectively using asymmetric, frequency-specific stimulation parameter titration based on symptom lateralization and the lateralized effects of DBS. Moreover, lateralized effects are also evident in other axial symptoms like gait, while limb symptoms inherently require lateralized adjustments7,9,10. Therefore, these lateralized frequency-specific programming strategies should also consider other axial and motor symptoms.
In this study, we aimed at: (1) validating the differential effects of high- versus low-frequency STN DBS on speech and voice outcomes reported in previous studies; (2) evaluating the effects of asymmetric frequency stimulation (AFS) and the role of frequency-based stimulation laterality on speech and voice performance; and (3) investigating the consistency of these effects across speech, voice, and other symptoms, such as gait, under various frequency-specific programming strategies.
Results
Demographics and clinical characteristics
Thirty-four right-handed PwPDs were enrolled, and one dropped out due to intolerance to the off-stimulation (Stim-off) condition and phase transitions. Finally, 33 participants completed Experiment Part I and 20 (60.6%) completed Experiment Part II (Fig. 1). Overall, the mean age of the patients was 64.9 (SD 8.9) years (range: 34–78 years), and the mean duration of disease was 11.7 (SD 4.5) years, with a mean post-STN DBS duration of 16.7 (SD 6.2) months. The patients had a mean levodopa equivalent daily dose (LEDD) of 416.7 (SD 253.3) mg/day. The clinical characteristics of patients enrolled in AFS trial were comparable to the overall sample (Table 1).
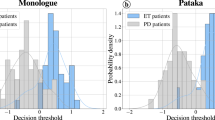
Experiment Part I: Bi-HFS vs. Bi-LFS
Overall voice quality, measured by the dysphonia severity index (DSI), showed no significant difference between the Stim-off and bilateral high frequency stimulation (Bi-HFS) condition (-2.6 ± 2.1 vs. -2.1 ± 2.0, Cohen’s d = 0.27, p = 0.449). In contrast, bilateral low frequency stimulation (Bi-LFS) significantly improved the DSI score (-1.6 ± 2.3) compared to the Stim-off (d = 0.53, p = 0.024) and Bi-HFS (d = 0.54, p = 0.012) condition. Similarly, Bi-LFS improved the maximum phonation time (MPT) with statistical significance compared to the Stim-off condition (14.2 ± 9.5 s vs 12.2 ± 8.2 s, Wilcoxon r = 0.39, p = 0.035) and Bi-HFS (13.1 ± 9.8 s, r = 0.47, p = 0.025). For the diadochokinetic rate (DDK rate), both Bi-HFS (3.9 ± 1.5 syllables/s) and Bi-LFS (4.0 ± 1.4 syllables/s) showed a trend toward improvement compared to the Stim-off state (3.5 ± 1.5 syllables/s; d1 = 0.31, p1 = 0.091; d2 = 0.33, p2 = 0.079), with no significant difference observed between Bi-HFS and Bi-LFS (d = -0.12, p = 1.000) (Fig. 2). No significant differences were observed in the remaining objective acoustic parameters (sound pressure level (SPL), harmonic noise ratio (HNR), vowel articulation index (VAI), fundamental frequency (F0) and its standard deviation (F0SD)) across the three states (Supplementary Fig. 1).
For perceptual ratings, Bi-HFS showed no significant changes in GRBAS-Grade, intelligibility, or naturalness compared to the Stim-off state (GRBAS-G: 1.0 ± 0.8 vs. 1.0 ± 0.8, r = 0.04, p = 1.000; intelligibility: 3.2 ± 1.1 vs. 3.2 ± 1.1, r = 0.12, p = 1.000; naturalness: 3.4 ± 1.0 vs. 3.5 ± 1.0, r = 0.24, p = 0.563). In contrast, Bi-LFS significantly improved these parameters compared to both Stim-off and Bi-HFS (GRBAS-G: 0.8 ± 0.7, r1 = 0.39, p1 = 0.034; r2 = 0.46, p2 = 0.027; intelligibility: 3.0 ± 1.1, r1 = 0.58, p1 = 0.005; d2 = 0.42, p2 = 0.022; naturalness: 3.3 ± 1.0, r1 = 0.60, p1 = 0.003; d2 = 0.37, p2 = 0.044) (Fig. 2). The scores for GRBAS subparts are provided in Supplementary Fig. 1.
Experiment Part II: Bi-HFS vs. Bi-LFS vs. AFS
The DSI demonstrated significant improvement in the left-sided LFS/right-sided HFS (L-LFS/R-HFS) state (-1.2 ± 2.2) compared to Bi-HFS (-2.2 ± 2.1, r = 0.59, p = 0.033) and showed no notable difference compared to Bi-LFS (-1.1 ± 2.2, d = -0.03, p = 0.880). In contrast, the deterioration in DSI score was observed in left-sided HFS/right-sided LFS (L-HFS/R-LFS) condition (-2.1 ± 2.2) compared to both L-LFS/R-HFS (d = 0.54, p = 0.024) and Bi-LFS condition (d = 0.61, p = 0.012). For MPT, both L-LFS/R-HFS (16.1 ± 11.4 s) and L-HFS/R-LFS (16.3 ± 11.4 s) significantly outperformed Bi-HFS (13.7 ± 9.2 s, r1 = 0.71, p1 = 0.006; r2 = 0.67, p2 = 0.011), but was comparable to Bi-LFS (15.4 ± 11.1 s, both p = 1.000). Regarding SPL, L-LFS/R-HFS (65.1 ± 9.6 dB) showed a significant increase over Bi-HFS (62.7 ± 10.9 dB, d = 0.75, p = 0.013) and a trend toward higher values compared to Bi-LFS (63.7 ± 10.7 dB, d = 0.40, p = 0.088) and L-HFS/R-LFS (64.0 ± 9.8 dB, d = 0.42, p = 0.077). In comparison, L-HFS/R-LFS did not significantly differ from Bi-HFS (d = 0.34, p = 0.588). For the DDK rate, both L-LFS/R-HFS (4.4 ± 1.4 syllables/s) and L-HFS/R-LFS (4.2 ± 1.7 syllables/s) showed significant improvement compared to Bi-HFS (3.9 ± 1.8 syllables/s; d1 = 0.60, p1 = 0.021; d2 = 0.47, p2 = 0.050) (Fig. 3).
Despite these objective parameter differences, no significant changes were observed in perceptual ratings, including GRBAS-Grade, intelligibility, and naturalness, across the states (all p > 0.05; see Fig. 3 and Supplementary Fig. 2).
Correlation between motor and acoustic parameter changes
The improvement trends in voice outcomes across different frequency DBS strategies were closely corresponded with the improvement in overall motor symptoms and gait performance. Specifically, all voice parameters exhibited a significant correlation with the MDS Parkinson’s disease rating scale (MDS UPDRS) part III total score (e.g., MPT: r = 0.54, p < 0.0001), as well as with the subscales for axial symptoms (r = 0.49, p < 0.0001), rigidity (r = 0.39, p < 0.0001), and bradykinesia (r = 0.49, p < 0.0001). However, no significant correlation was observed with tremor improvement (r = 0.16, p = 0.08). Furthermore, the improvements in voice outcomes were significantly associated with gait parameters. Notably, MPT and DDK rate correlated significantly with gait measures such as stride length (e.g., MPT: r = 0.28, p = 0.001), gait speed (r = 0.29, p < 0.001), arm swing range (r = 0.20, p = 0.018) and duration of turning (r = 0.26, p = 0.002). Additionally, perceptual evaluations of intelligibility and naturalness were found to be significantly correlated with all these gait parameters, further reinforcing the capacity of these measures as indicators of both motor and voice function improvements (Fig. 4).
Discussion
In this study, we first confirmed the superiority of Bi-LFS over Bi-HFS in improving dysarthria and dysphonia in PwPD suffering from treatment-resistant gait disturbances. We further demonstrated that the L-LFS/R-HFS may provide greater benefits in acoustic parameters compared to L-HFS/R-LFS and Bi-HFS. Lastly, changes in objective acoustic performance following lateralized, asymmetrical frequency stimulation were in line with changes in overall motor symptoms and gait.
Bi-LFS has been introduced to manage speech and voice impairment11,12,13,14 as well as gait disorders resistant to Bi-HFS11,15,16,17,18. These benefits may stem from the reduced current spread to surrounding brain regions (e.g., pedunculopontine nucleus) and fiber tracts (e.g., corticobulbar fibers) compared to high-frequency stimulation2,15. However, the use of Bi-LFS was limited by the exacerbation of appendicular symptoms such as tremor5,6, and by the gradual decline in its axial benefits over time19,20. Consequently, Bi-LFS was only tolerable in a subset of patients19,20. Hopefully, the L-LFS/R-HFS strategy, which retains high-frequency stimulation on the right while reducing the frequency on the left, appears to offer a balanced approach. Side effects on speech due to left-sided STN HFS may be in part related to the dominance of the left hemisphere8. Previous studies have provided evidence that left-sided HFS may be inferior to right-sided HFS in terms of verbal and cognition aspects7. Notably, one recent study reported that computer-based acoustic analyses favored right- over left-sided HFS, and the subjective improvement were only observed with right-sided HFS2. Another study found that 130 Hz stimulation of the left STN worsened verbal fluency, while right-sided stimulation improved it8. Beyond this lateralized effect of subthalamic HFS on voice and speech in PD, the current study demonstrated that the stimulating frequency also plays a crucial role in the lateralized effects of DBS. Explicitly, L-LFS/R-HFS was superior to L-HFS/R-LFS and Bi-HFS in objective voice and speech improvement.
Optimizing stimulating parameters can be challenging in some cases to account for all motor symptoms and side effects. While L-LFS/R-HFS is preferred for addressing speech and voice issues, our published data21 suggested tremor laterality influenced the choice of stimulation frequency laterality. Specifically, patients may benefit more from lateralized HFS to the STN contralateral to the limb with predominant tremor. Therefore, for PwPD suffering from severe right limb tremor along with speech impairment, careful consideration is needed when selecting stimulating frequency laterality.
Here we propose a lateralized frequency-based programming strategy for STN-DBS targeting axial-predominant PIGD subtype patients. For patients exhibiting inadequate or exacerbated axial symptoms under Bi-HFS, Bi-LFS should be initiated. When unilateral tremor-predominant limb symptom exacerbation drives LFS intolerance, contralateral HFS should be reactivated, while other causes of intolerance warrant trial of lateralized stimulation (L-LFS/R-HFS first). When managing the therapeutic dilemma of utilizing L-HFS to address exacerbated right-limb symptoms while mitigating potential speech deterioration, implement comprehensive parameter optimization including reduced pulse width (30-40 μs), frequency titration to 80-100 Hz, voltage threshold monitoring. Further clinical trials are necessary to validate this hypothesis.
This study has several limitations that warrant discussion. Firstly, our cohort consisted of patients predominantly affected by postural and gait disorders rather than those specifically selected for voice and speech impairment. Secondly, the stimulating contacts remained unchanged across different conditions. Given prior evidence suggesting superior speech outcomes with ventral STN LFS15 and potential speech deterioration with dorsal STN HFS22, the interaction between stimulation frequency and anatomical localization within the STN, while not addressed in our study, warrants further investigation. Additionally, we used 1.5 h as the washout time between each stimulation condition, and its adequacy for the study of speech and voice remains uncertain. However, we believe that 1.5-h washout period should generally be sufficient as impacts of DBS on speech and voice is perceivable during the monopolar review. Future research on AFS requires further investigation in larger cohorts to confirm its efficacy and broaden its clinical applicability.
Methods
Participants
This study was part of a randomized clinical trial investigating the frequency-specific effect of STN DBS on gait kinematic parameters in PwPD with treatment-resistant postural and gait disorders after STN DBS surgery21. The treatment-resistant postural and gait disturbances were defined as TD/PIGD score ratio ≤ 0.9 according to the MDS UPDRS23, and the PIGD sub-score of the MDS UPDRS (i.e., item 2.11, 2.13, 3.9‒3.13) ≥ 6 points despite optimal anti-parkinsonian medication and stimulation parameter adjustment. The study protocol was approved by Ethics Committee of the Ruijin Hospital Shanghai Jiao Tong University School of Medicine (approval number: 2023-239). Written informed consent was obtained from each participant before enrollment. The trial was registered in the National Medical Research Registration and Information System of China (MR-31-23-036810) on August 3, 2023.
Sample size estimation
The sample size was estimated based on Experiment Part II. Due to the lack of prior research on AFS, and based on our preliminary study results, we anticipated detecting an estimated mean difference of 1.4 points in improvement of MDS UPDRS-III axial sub-score between AFS and Bi-HFS, with a standard deviation (SD) of 2 points for the paired differences, achieving 80% power at a 0.05 significance level. This calculation resulted in a required sample size of 19 participants. Ultimately, 33 patients completed the study for the comparison between Bi-LFS and Bi-HFS, and 20 participants completed the Experiment Part II.
Surgical procedure and DBS devices
The surgical procedure was described in detail in our previous work24. Postoperative CT imaging was performed to confirm the satisfactory placement of DBS leads. All patients received 4-contact electrodes implants and constant voltage stimulation. Among the 33 patients included, 8 received Medtronic DBS (lead 3387 and model Activa, Medtronic, USA), 2 received PINS DBS (lead L302 and model G102R, PINS, China), and 23 received SceneRay DBS device (lead 1210 and model SR1101, SceneRay, China). Since asymmetric frequency feature of the SceneRay device was a unique feature among existing stimulators in China at the time of study, AFS was only conducted in patients with SceneRay device. Of these 23 patients, 20 consented to undergo AFS testing.
Experiment procedures and clinical evaluations
The study was conducted during hospitalization in one day or two consecutive days depending on whether the AFS parameters would be evaluated or not. All assessments were carried out in the defined off-medication condition, namely a discontinuation of antiparkinsonian medications for at least 12 h. All participants received acoustic and motor evaluations in the Stim-off, Bi-HFS (130 Hz), and Bi-LFS (60 Hz) conditions on the first day (Experiment Part I) and for participants enrolled in the AFS trial, they further received motor assessments in two extra stimulating conditions, i.e., L-HFS/R-LFS and L-LFS/R-HFS, on the second day (Experiment Part II). For Experiment Part I, the Stim-off condition was defined as the stimulator being switched off for at least 1.5 h and was always evaluated first to minimize the duration of discomfort and its potential perception by the participants25. The order of the Bi-HFS and Bi-LFS conditions was randomized, and assessment was conducted after the stimulator being switched on for 1.5 h. Similarly, for Experiment Part II, the order of L-HFS/R-LFS and L-LFS/R-HFS was also randomized.
The total electrical energy delivered (TEED), active contacts, and pulse width were controlled across different conditions18. The TEED was calculated as follows:
The most recent optimal stimulation parameter tuned by an experienced neurologist prior to the study was used as a reference to define parameters for each experiment condition26. If intolerance occurred (e.g., dizziness, paresthesia and muscle contraction), the voltage was fine-tuned to the individual’s maximum tolerance level.
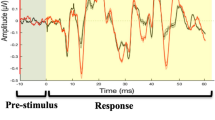
Acoustic Data acquisition and preprocessing
Acoustic data was acquired by a recording microphone (ATMOS, Germany) using 22.4kHz mono mode and analyzed on the lingWAVES platform (version 2.6; Wevosys, Germany)16. Voice recordings were conducted in a room with an ambient noise level of less than 45 dB. The patient was seated in a relaxed posture, with the microphone positioned approximately 30 cm from the mouth to maintain consistent recording conditions. The following tasks were completed: (1) Sustained phonation of the vowels /a/, /i/, and /u/ for as long and as smoothly as possible; (2) Soft phonation of the vowel /a/ in the lightest possible tone at a comfortable loudness; (3) Sustained pitch glide of the vowel /a/, starting at the lowest pitch, ascending to the highest achievable pitch, and descending back to the lowest; (4) Rapid and clear repetition of /pataka/ at least six times; (5) Reading the Chinese standard text, “The North Wind and the Sun”, at a comfortable pitch and loudness. These tasks were selected to provide comprehensive and objective data for analyzing and describing dysphonia and dysarthria in PD27,28. To ensure consistency and comparability, all recordings were performed by the same experimenter in the same controlled environment. Following data collection, all samples were anonymized, and a blinded analysis was conducted by an independent evaluator using Praat software. The following parameters were retrieved from voice and speech samples for voice quantification: DSI, MPT, SPL, DDK rate, HNR, VAI, F0, and F0SD. The definitions of the parameters, the corresponding tasks, and their pathophysiological interpretation in PD are summarized in Supplementary Table 1.
GRBAS assessment and evaluation of speech intelligibility and naturalness
The GRBAS scale was used for subjective perceptual evaluation of voice quality, by the reading Chinese version text of ‘The North Wind and the Sun’, which includes assessments of Grade of dysphonia (G), roughness (R), breathiness (B), asthenia (A), and strain (S)29. Each of these parameters is rated on a four-point scale: 0 = normal; 1 = mild; 2 = moderate; 3 = severe. To ensure the accuracy and objectivity of the assessments, three experienced speech-language pathologists independently and blindly rated the recorded voice samples, and the average score of the three raters was used.
For the evaluation of speech intelligibility and naturalness, a total of 10 raters with no background in linguistics were recruited. The raters met the following criteria: (1) native Mandarin speakers with no history of auditory deficits; (2) unfamiliar with the speech characteristics of neurodegenerative diseases; (3) unaware of the study’s purpose. Among the raters, there were 6 females and 4 males, with an average age of 21.62 ± 8.02 years. Prior to rating, all raters underwent standardized training to ensure they understood the rating criteria and procedures30. The recorded speech samples were played back in random order, and each sample was played only once. The overall intelligibility rating of speech was as follows: 1 = very easy to understand; 2 = mostly understandable but with some difficulty; 3 = understandable if the listener knows the context; 4 = partially understandable; 5 = completely unintelligible. The overall naturalness rating of speech was as follows: 1 = normal; 2 = mild; 3 = moderate; 4 = severe; 5 = very severe.
Evaluations of movement symptoms and gait kinematics
The primary outcome of movement symptoms was the change in MDS UPDRS-III axial sub-score (3.1, 3.9‒3.13) between different stimulation conditions. Secondary outcomes included: (1) MDS UDPRS-III total score and other sub-scores, including rigidity (3.3), bradykinesia (3.2, 3.4‒3.8, 3.14) and tremor (3.15‒3.18); (2) Berg balance scale; (3) gait parameters measured by sensors.
The MDS UPDRS-III was assessed and videotaped by an experienced assessor for each condition. A second experienced assessor scored from the videotape except for the rigidity sub-score. Both patients and assessors were blinded to the stimulation condition. We also employed a sensor- and deep vision-based analysis system (GYENNO MATRIX, GYENNO China) to analyze the gait and balance performance objectively and quantitatively. Subjects wore ten inertial sensors secured by elastic Velcro straps on bilateral wrists, ankles, knees, and feet, the sternum, and the back at the L5 level. Patients were asked to perform the 5-meter timed-up-and-go (TUG) test six times. Spatiotemporal parameters on test duration, pace (cadence, stride length and gait speed), arm and trunk movement, dynamic stability, turning and freezing of gait (FoG) were collected. The detailed description of parameters was in Supplementary Table 2.
Statistical analysis and outcomes
Based on the normality of the data (Shapiro-Wilk test), a repeated-measure one-way ANOVA with Geisser-Greenhouse sphericity correction, or a repeated-measure nonparametric test (Friedman test), was applied to compare the Stim-off, Bi-LFS, and Bi-HFS conditions. The paired t-test (for normally distributed data) and the Wilcoxon Signed-Rank Test (for non-normally distributed data) were employed for post hoc analysis, with False Discovery Rate (FDR) correction applied to multiple comparisons. Cohen’s d and Wilcoxon r were used to describe effect sizes.
For the AFS analysis, the same statistical methods were applied, with the following primary predefined comparisons: (1) L-HFS/R-LFS vs. L-LFS/R-HFS, (2) L-HFS/R-LFS vs. Bi-HFS, (3) L-HFS/R-LFS vs. Bi-LFS, (4) L-LFS/R-HFS vs. Bi-HFS, and (5) L-LFS/R-HFS vs. Bi-LFS. The FDR method was used to correct for multiple comparisons following these five tests.
To explore the relationship between symptom improvement under different DBS frequency combinations, data from all patient states (n=139) were compiled, and pairwise Spearman correlation analyses were conducted between MDS-UPDRS Part III scores, dynamic gait parameters, and voice metrics that showed statistically significant differences. Spearman correlation results were also corrected for multiple comparisons using the FDR method, with patients treated as covariate to account for inter-patient variability. For clarity, positive correlations reflect consistent trends in clinical improvement or worsening, while negative correlations reflect opposing trends. A FDR corrected p-value of < 0.05 was considered statistically significant. Statistical analyses and graphical representation were performed using R (version 4.1.3).
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Rusz, J. et al. Defining speech subtypes in De Novo Parkinson disease: response to long-term levodopa therapy. Neurology 97, e2124–e2135 (2021).
Bobin, M. et al. Direct subthalamic nucleus stimulation influences speech and voice quality in Parkinson’s disease patients. Brain Stimulation 17, 112–124 (2024).
Cao, F. et al. Speech and language biomarkers for Parkinson’s disease prediction, early diagnosis and progression. npj Parkinsons Dis. 11, 57 (2025).
Ma, A., Lau, K. K. & Thyagarajan, D. Voice changes in Parkinson’s disease: What are they telling us?. J. Clin. Neurosci. 72, 1–7 (2020).
Mu, L. et al. Mechanisms of swallowing, speech and voice disorders in Parkinson’s disease: literature review with our first evidence for the periperal nervous system involvement. Dysphagia 39, 1001–1012 (2024).
Tabari, F. et al. Speech, voice, and language outcomes following deep brain stimulation: A systematic review. PLoS ONE 19, e0302739 (2024).
Lin, Z., Zhang, C., Li, D. & Sun, B. Lateralized effects of deep brain stimulation in Parkinson’s disease: evidence and controversies. npj Parkinsons Dis. 7, 64 (2021).
Del Bene, V. A. et al. Differential Cognitive Effects of Unilateral Subthalamic Nucleus Deep Brain Stimulation for Parkinson’s Disease. Ann. Neurol. 95, 1205–1219 (2024).
Lizárraga, K. J. et al. Lateralized Subthalamic Stimulation for Axial Dysfunction in Parkinson’s Disease: A Randomized Trial. Mov. Disord. 37, 1079–1087 (2022).
Lizarraga, K. et al. Asymmetric neuromodulation of motor circuits in Parkinson’s disease: The role of subthalamic deep brain stimulation. Surg. Neurol. Int. 8, 261 (2017).
Xie, T., Kang, U. J. & Warnke, P. Effect of stimulation frequency on immediate freezing of gait in newly activated STN DBS in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 83, 1015–1017 (2012).
Moreau, C. et al. Modulation of dysarthropneumophonia by low-frequency STN DBS in advanced Parkinson’s disease. Mov. Disord. 26, 659–663 (2011).
Fabbri, M. et al. Is lowering stimulation frequency a feasible option for subthalamic deep brain stimulation in Parkinson’s disease patients with dysarthria. Parkinsonism Relat. Disord. 64, 242–248 (2019).
Phokaewvarangkul, O., Boonpang, K. & Bhidayasiri, R. Subthalamic deep brain stimulation aggravates speech problems in Parkinson’s disease: Objective and subjective analysis of the influence of stimulation frequency and electrode contact location. Parkinsonism Relat. Disord. 66, 110–116 (2019).
Xie, T. et al. Effect of low versus high frequency stimulation on freezing of gait and other axial symptoms in Parkinson patients with bilateral STN DBS: a mini-review. Transl. Neurodegener. 6, 13 (2017).
Xie, T. et al. Low-frequency stimulation of STN-DBS reduces aspiration and freezing of gait in patients with PD. Neurology 84, 415–420 (2015).
Xie, T. et al. Long-term effect of low frequency stimulation of STN on dysphagia, freezing of gait and other motor symptoms in PD. J. Neurol. Neurosurg. Psychiatry 89, 989–994 (2018).
Moreau, C. et al. STN-DBS frequency effects on freezing of gait in advanced Parkinson disease. Neurology 71, 80–84 (2008).
Ricchi, V. et al. Transient effects of 80 Hz stimulation on gait in STN DBS treated PD patients: a 15 months follow-up study. Brain Stimul. 5, 388–392 (2012).
Zibetti, M. et al. Low-frequency Subthalamic Stimulation in Parkinson’s Disease: Long-term Outcome and Predictors. Brain Stimul. 9, 774–779 (2016).
Zeng, Z., Lin, Z., Huang, P., Pan, Y. & Li, D. Effect of High, Low, and Asymmetric Frequency Stimulation of the Subthalamic Nucleus in Parkinson’s Disease: A Randomized Trial. In: Asian and Oceanian Parkinson’s Disease and Movement Disorders Congress. Late-Breaking Abstracts. LBA-5 (2025).
John, K. D. et al. Deep brain stimulation effects on verbal fluency dissociated by target and active contact location. Ann. Clin. Transl. Neurol. 8, 613–622 (2021).
Stebbins, G. T. et al. How to identify tremor dominant and postural instability/gait difficulty groups with the movement disorder society unified Parkinson’s disease rating scale: comparison with the unified Parkinson’s disease rating scale. Mov. Disord. 28, 668–670 (2013).
Lin, Z. et al. Revisiting the L-Dopa response as a predictor of motor outcomes after deep brain stimulation in Parkinson’s disease. Front Hum. Neurosci. 15, 604433 (2021).
Vallabhajosula, S. et al. Low-frequency versus high-frequency subthalamic nucleus deep brain stimulation on postural control and gait in Parkinson’s disease: a quantitative study. Brain Stimul. 8, 64–75 (2015).
Picillo, M., Lozano, A. M., Kou, N., Puppi Munhoz, R. & Fasano, A. Programming deep brain stimulation for Parkinson’s disease: the Toronto Western Hospital Algorithms. Brain Stimul. 9, 425–437 (2016).
Rusz, J., Tykalova, T., Ramig, L. O. & Tripoliti, E. Guidelines for speech recording and acoustic analyses in dysarthrias of movement disorders. Mov. Disord. 36, 803–814 (2021).
Wuyts, F. L. et al. The dysphonia severity index: an objective measure of vocal quality based on a multiparameter approach. J. Speech Lang. Hear Res. 43, 796–809 (2000).
Baird, L., Evans, N. & Greenhill, S. J. Blowing in the wind: Using ‘North Wind and the Sun’ texts to sample phoneme inventories. J. Int. Phonetic Assoc. 52, 453–494 (2022).
Darley, F. L., Aronson, A. E. & Brown, J. R. Differential diagnostic patterns of dysarthria. J. Speech Hearing Res. 12, 246–269 (1969).
Acknowledgements
This study was funded by the Shanghai Municipal Health Commission (202140181 to D.L.), the Shanghai Science and Technology Commission (22Y11903900 to D.L.) and Ruijin Hospital Guangci Innovative Technology Launch Program (GCQH202205 to D.L.). This study was also supported by the Shanghai Youth Science and Technology Talents Sailing projects (23YF1424000 to Z.L.) and the Youth Project of National Science Foundation of China (82301664 to Z.L.).
Author information
Authors and Affiliations
Contributions
Z.Z., D.L., B.S. and C.Z. contributed to the conception and design of the study; Z.Z., M.Y., Z.L., P.H. and Y.P. contributed to the acquisition and analysis of data; Z.Z., Z.L. and D.L. contributed to drafting the text or preparing the figures.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zeng, Z., Yang, M., Lin, Z. et al. Effect of high, low, and asymmetric frequency subthalamic stimulation on speech and voice in Parkinson’s disease: a randomized trial. npj Parkinsons Dis. 11, 223 (2025). https://doi.org/10.1038/s41531-025-01090-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-01090-0