Abstract
Despite great advancements in the treatment of chronic airway diseases, improvements in morbidity and mortality have stalled in recent years. Asthma and chronic obstructive pulmonary disease are complex and heterogeneous diseases that require tailored management based on individual patient characteristics and needs. The Treatable Traits (TTs) approach aims to personalise and improve patient care through the identification and targeting of clinically relevant and modifiable pulmonary, extra-pulmonary and behavioural traits. In this article, we outline the rationale for TTs-based management and provide practical guidance for its application in primary care. To aid implementation, seven potential ‘prime’ traits are proposed: airflow obstruction, eosinophilic inflammation, adherence, inhaler technique, smoking, low body mass index/obesity and anxiety and depression—selected for their prevalence, recognisability and feasibility of use. Some of the key questions among healthcare professionals, that may be roadblocks to widespread application of a TTs model of care, are also addressed.
Similar content being viewed by others
Introduction
Asthma and chronic obstructive pulmonary disease (COPD) are two prevalent, complex and heterogeneous airway diseases with clinical features that may overlap1,2. In recent years, a management paradigm based on the identification of so-called ‘treatable traits’ (TTs) has been proposed to personalise and improve patient care. The TTs strategy targets clinically relevant, measurable and modifiable characteristics (traits) in each patient in the pulmonary, extra-pulmonary and behavioural and psychosocial domains3. The TTs approach is agnostic to traditional disease labels and applicable to all patients with chronic airway diseases4. By recognising the complexity and variability in clinical and biological characteristics among individual patients with chronic airway diseases, treatment is more rational, precise and effective.
Although the concepts underpinning the TTs approach are now well established, some areas of uncertainty remain among healthcare professionals (HCPs), particularly in the primary care setting. Below, we discuss (1) the rationale for introducing a TTs approach in clinical practice; and, (2) the hurdles and challenges of its implementation.
Rationale for implementing a Treatable Traits approach in clinical practice
Conceptual advantages
Asthma and COPD guidelines have traditionally advocated a stepwise approach to adjusting treatment based on symptom control and reducing the risk of exacerbations1,2. This has been instrumental in improving outcomes for patients, as shown by reductions in hospital admission and mortality in the 1990s to early 2000s5. However, progress has stalled with no overall improvements to asthma and COPD mortality observed between 2001 and 20175,6. This slowed progress may be attributed to the fact that guidelines are largely informed by evidence derived from grouped mean data from randomised controlled trials (RCTs). This may result in treatment algorithms biased towards the greatest efficacy for the majority, but not necessarily the most appropriate treatment for each individual patient5. Further, the stepwise approach assumes that (1) symptoms are driven by the same mechanisms in individual patients, and (2) symptom control is achieved by following the ‘one-size-fits-all’ treatment algorithm, although this is not always the case7. In fact, in many patients, elimination of symptoms and restoration of normal lung function cannot be achieved8,9 and pursuing this unattainable goal by progressively increasing treatment may lead to patient and clinician frustration, as well as adverse effects from high-dose treatment. This is particularly pertinent for inhaled corticosteroids (ICS), where 80–90% of the maximal therapeutic effect may be achieved at low doses in most patients10. Escalation to higher doses of ICS should be preceded by both confirmation of adherence to treatment and the presence of the relevant biological processes targeted by corticosteroids (elevated blood eosinophils or fractional exhaled nitric oxide [FeNO]). In addition, current asthma guidelines advocate stepping down treatment when asthma symptoms are controlled. While stepping down treatment may be appropriate in certain circumstances, a universal step-down model risks the false assumption that treatment targets and disease characteristics are homogenous in all patients7. It also assumes that a short-term increase in treatment can, in some way, change the underlying disease pathophysiology to reduce future requirement for treatment. By contrast, in COPD, the Global Initiative for Chronic Lung Disease (GOLD) recommends assessing two key TTs (dyspnoea and exacerbations) to manage patients during follow-up and rarely recommends stepping down treatment, with the exception of patients on ICS who suffer from, or are at risk of, pneumonia, in whom stopping ICS is an option for consideration2.
The heterogeneity, complexity and multi-morbidity in each patient needs to be considered on an individual basis11. The TTs approach offers a practical method of designing personalised treatment strategies that account for patient heterogeneity. This is not a revolutionary concept, nor is it inherently complex; rather, it reinforces many existing elements of good clinical practice—identifying and treating clinical features presented in an individual patient. Analogous approaches have been implemented in other areas with great success, such as cardiovascular disease. During the 1990s, heart attack risk factors, such as blood pressure, cholesterol and smoking, were stratified into a theragnostic tool for predicting and preventing future events and this vastly improved clinical outcomes12.
Real-life examples of the Treatable Traits approach in clinical practice
Use of oral corticosteroids in asthma and COPD
Rescue oral corticosteroids (OCS) play an important role in the acute management of exacerbations of asthma and COPD1,13,14. However, it is well established that long-term use of OCS is associated with side effects1,15,16,17,18. It was found that patients with severe asthma who received frequent prednisolone (≥4 prescriptions per year) had an increased risk of many conditions associated with OCS exposure, with the highest risk observed with maintenance daily prednisolone19. Additional studies have shown that OCS-induced morbidity emerged at low levels of exposure and validate that episodic rescue prednisolone is not a benign intervention15,16. However, OCS prescription remains widespread and use in the treatment of poorly controlled mild–moderate disease is particularly concerning18. Doses of OCS can be minimised through the identification of biomarkers and TTs within a structured management approach, to optimise treatment and reduce the risk of exacerbations18. Following this approach, there is an initial assessment of disease severity, after which comorbidities and risk factors contributing to difficult-to-treat asthma are identified and treated. If this proves ineffective, referral to a specialist is advised before consideration of prescribing OCS at the minimum dose18.
Measuring eosinophilic airway inflammation
Type 2 (T2) airway inflammation has been identified as a TT in some patients with asthma or COPD, and can be assessed by measurement of blood eosinophil counts and/or FeNO (if available) (Table 1). Eosinophilic airway inflammation is associated with an increased exacerbation risk and more severe disease in patients with chronic airway diseases1,2. In asthma, eosinophilic airway inflammation is mediated by allergic sensitisation and T2 lymphocytes, although eosinophilic inflammation can occur independently of an allergic response. The eosinophilic phenotype is common, although not universal, with ~50–70% of patients having T2-high asthma20,21,22 and this estimate is higher in a severe asthma population (>80%)23. In contrast, airway inflammation in COPD is typically associated with a neutrophilic response (Type 1) and 20–40% of patients with COPD also present with an eosinophilic phenotype22,24. Therefore, the presence of T2 inflammation requires assessment as part of phenotype and risk determination22.
Sputum eosinophil count is an effective indicator of eosinophilic airway inflammation, but it is not broadly used in clinical practice due to duration of the analysis and required expertise and facilities1,25,26. Alternatively, blood eosinophil count is an effective and more practical marker of eosinophilic inflammation26,27. Measuring blood eosinophils is a simple, inexpensive and quick method that is frequently performed in primary care27. FeNO testing can also be used to assess the presence of eosinophilic airway inflammation, although its accessibility is generally confined to the specialist domain26,28. Furthermore, controversy persists within treatment guidelines as to the role of FeNO in the management of asthma in primary care. The British Thoracic Society and European Respiratory Society guidelines have recently advised that FeNO may have a role in asthma diagnosis and clinical decision-making29,30. A recently updated systematic review has demonstrated that FeNO-guided treatment may reduce exacerbation frequency in patients with asthma, though the clinical relevance of these effects could not be determined31. FeNO suppression testing with monitored ICS treatment is useful in distinguishing patients who require escalation to biologic therapy from those in which improved adherence to ICS is likely to achieve disease control32,33,34, and has been shown to be cost effective35. It is not yet clear whether routine FeNO testing in all patients with asthma is clinically effective or cost effective, this may be elucidated by a large UK programme currently exploring its suitability in primary care36.
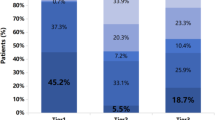
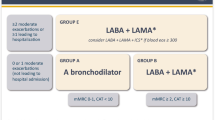
By contrast, there is a growing volume of evidence that indicates blood eosinophils are a predictive biomarker for responsiveness to ICS in patients with asthma and COPD. Studies have demonstrated a continuous beneficial effect in reduction of exacerbation rate from ICS treatment in correlation with increasing blood eosinophil count in patients with COPD37. This evidence has led to inclusion of eosinophil measurement in international guidelines as a clinical decision-making factor. The GOLD strategy report recommend using a blood eosinophil count of ≥300 cells/μL as an indication for escalation of treatment from a long-acting muscarinic antagonist (LAMA) + long-acting β2-agonist (LABA) combination to triple therapy treatment (ICS + LAMA + LABA)2. Similar utility of the biomarker is found in asthma; greater treatment benefits are observed in patients with eosinophilic asthma treated with ICS versus patients with lower blood eosinophil count, with regard to exacerbation rate, lung function and health-related quality of life38,39. However, utilisation of blood eosinophil count as a predictive marker for targeting ICS use in patients with asthma is not yet recommended by the Global Initiative for Asthma (GINA)1. In cases of severe asthma which remain uncontrolled despite optimised therapy, patients should be referred to a specialist for further investigation. Severe eosinophilic asthma can be effectively treated in the specialist domain with add-on T2-targeting biologic therapy, to which blood eosinophil count is a well-documented and reliable predictor of responsiveness1. GINA recommendations advocate a blood eosinophil level threshold of ≥150 cells/μL for consideration of add-on T2-targeting biologic therapy in patients with exacerbations or poor symptoms control1. In summary, eosinophilic inflammation is an important TT to address; its widespread measurement in primary care may inform rational treatment decisions and facilitate timely, appropriate referrals for specialist assessment40,41.
Patient engagement, education and empowerment
Some common frustrations among patients with asthma and COPD regarding the current treatment paradigm include a feeling that their own beliefs and concerns are not recognised and a perception that the treatment is neither patient-centric nor tailored to their personal needs and goals42. Together, these frustrations may erode the patient–clinician partnership, diminish engagement and contribute to non-adherence to treatment42. The TTs approach, however, empowers prescribers to avoid inappropriate treatment when specific traits have been ruled out. It provides patients with a demonstrable common-sense fit between their understanding of the problem (drivers of disease) and the proposed solution (treatment plan)4,12. In the same way that patients with cardiovascular disease may know their blood pressure or cholesterol numbers and patients with type 2 diabetes may know their haemoglobin A1c, the TTs model of care, helps patients with asthma or COPD understand their disease and make better-informed decisions about their medication use. This targeted approach enables collaborative decision-making with patients, with rationally agreed treatment goals12. In summary, by avoiding patient frustration due to misaligned treatment expectations, this could in turn promote good self-management and adherence. Finally, there is a perception that the TTs approach is complicated and may be overwhelming for patients12. By contrast, studies have shown that patients desire increased objective assessment, more individualised approaches and involvement in shared decision-making12,42.
Practical implementation questions
There remains some uncertainty and hesitancy around the feasibility of implementing a TTs approach within current healthcare systems12; some common questions are discussed below.
Are there a few ‘prime’ treatable traits that should be considered for the initial management of patients with chronic obstructive airways diseases?
There are many potential traits to consider in patients with airways diseases4. Simplification of the approach, to ease implementation in primary care, could have a substantial impact on early care and timely referrals. Therefore, we propose seven potential ‘prime traits’ (Table 1), selected for their prevalence, recognisability and feasibility of implementation in primary care. We also acknowledge that, in clinical practice, other TTs may deserve attention and treatment if identified in individual patients, such as rhinitis, gastroesophageal reflux, poor indoor and outdoor air quality (e.g. damp walls and/or presence of moulds), cardiovascular diseases and diabetes1,12,43,44,45,46.
-
(1)
Airflow limitation measurement is essential for the diagnosis and assessment of severity of chronic airway diseases1,47,48. With resources available to support training and equipment, quality-assured spirometry tests can be accurately performed in primary care1,2,4,49.
-
(2)
Eosinophilic, or T2, inflammation which, as previously discussed, may be measured by blood eosinophil count, is highly associated with exacerbation risk and is predictive of response to ICS and biologic therapy in COPD and asthma1,2,39,40,50. In addition, FeNO is a simple point-of-care breath test that could potentially be measured in primary care and is prognostic for exacerbation risk in asthma, particularly when combined with blood eosinophil count31,41,51. FeNO is also predictive of response to ICS and a useful tool for identifying poor ICS adherence in uncontrolled disease28,52,53. Although the utility of FeNO testing in primary care remains under investigation, if available, it is potentially valuable in implementing a TTs strategy for asthma36,54.
-
(3)
Treatment adherence is an essential driver of improved outcomes for both asthma and COPD55,56 and can be evaluated in a primary care setting through open discussions and review of the prescription refill rate1,4.
-
(4)
Incorrect inhaler technique is a common problem that reduces the effective delivery of drug(s) to the lung, with a detrimental impact on symptoms and exacerbation risk1,57. Outcomes may be improved through education and training on correct inhaler technique1.
-
(5)
Smoking should be assessed in each patient, with support and advice offered to encourage cessation1,2,58,59.
-
(6)
Obesity is a major contributor to poor asthma control; thus, body mass index (BMI) should be evaluated, and lifestyle and dietary interventions introduced where necessary1. In patients with COPD, low BMI is associated with worse outcomes and nutritional supplementation may be beneficial in those who are malnourished2.
-
(7)
Patients with chronic airway diseases are at increased risk of anxiety and depression, which are associated with reduced symptom control and an increased risk of exacerbations1,2,60. Mood disorder substantially impacts symptom burden, particularly in females61.
Importantly, many TTs are dynamic and their expression and relevance to the clinical situation may change—both with time and with effective treatment. Monitoring of traits is therefore needed, the frequency of which should be tailored to the individual patient depending on the cumulative effect of their particular traits. Furthermore, TTs do not always exist independently of one another; a change in one trait can, in some cases, effect change in another. For example, treating eosinophilic inflammation can reduce the frequency of exacerbations39,62. In fact, several factors, including exacerbations and dyspnoea, may be regarded as both traits and outcomes. This is important to consider when conducting routine observation of traits to enable effective management of clinically relevant changes over time.
Implementation of a Treatable Traits approach can be done irrespective of the disease label
Disease labels are not required for identifying key traits or underlying drivers of disease. However, prescribing practices and healthcare pathways are generally reliant on the presence of a disease label. These labels certainly have value as the first step in diagnosis, but not the last, as we believe this should be augmented by a subsequent TTs assessment. For example, in the case of a patient presenting with the traditional disease label of ‘asthma’, who has a high level of blood eosinophilia, low forced expiratory volume in 1 second (FEV1) and an inconsistent prescription refill rate, under the TTs model a clinician could provide a more detailed diagnosis of ‘eosinophilic asthma with airflow obstruction and low adherence’. In this way, the diagnostic process is refined to provide a nuanced label for the individual patient, which is more meaningful for the patient and clinician alike. Another example relates to a patient with a diagnosis of asthma who is currently prescribed low doses of ICS without long-acting bronchodilators. In this case, the persistence of inadequate disease control plus a raised Th2 biomarker (e.g. FeNO) may indicate that increasing anti-inflammatory treatment, or addressing inadequate adherence/inhaler technique in the current ICS regime, could be effective management options. Finally, a high symptom report despite good lung function and normal biomarkers may indicate other factors, such as undiagnosed anxiety or depression, as more important targets than physiological or inflammatory factors for gaining control and improving wellbeing in a particular patient. These examples show that a TTs strategy would lead to more comprehensive treatment of the patient’s overall condition than if the clinician had focused solely on the traditional disease label. We believe an important evolution in respiratory care will be the interpretation of labels as the basis for further disease investigation, rather than a signpost towards a blanket one-size-fits-all approach to treatment.
Is a controlled or real-world effectiveness trial needed to demonstrate the clinical benefit of the Treatable Traits approach?
A common question is around whether a RCT is needed to demonstrate the efficacy of the TTs model of care as a whole. It is notable that, historically, our treatment paradigms across airways diseases have not been based on any singular overarching study of the whole framework, but on individual controlled studies that demonstrate the efficacy of each component on managing an element of disease. Our guidelines have evolved iteratively as individual pieces of evidence became available. With this in mind, there are several reasons why a controlled efficacy trial for the TTs model of care may not be necessary. Firstly, the clinical impact of managing each individual trait is well supported by high-quality evidence, often from RCTs (see Table 1). For example, large studies have shown that eosinophilic inflammation in patients with asthma or COPD can be effectively treated with ICS and the level of inflammation is predictive of treatment response, with reductions in exacerbation rates increasing in proportion with blood eosinophil count38,39,63. Likewise, there is clear evidence that bronchodilators can be used to treat airflow obstruction; treatment with formoterol and salmeterol has demonstrated significant improvements in FEV1 in patients with COPD49. Secondly, an efficacy trial for the TTs approach may not be feasible logistically—to assess the efficacy of all prime traits simultaneously in a controlled setting, while comparing TTs to a standard model of care, in a sufficiently large patient population, would be prohibitively complex and time-consuming. Due to the inherent heterogeneity of airways diseases, controlling for multiple factors would also be an enormous challenge.
On the other hand, effectiveness trials have been performed in specific settings to investigate the relative benefits of the TTs approach compared with traditional stepwise treatment. McDonald et al. carried out a study to determine the effectiveness of a TTs approach for severe asthma in comparison with a stepwise approach to treatment. Eligible patients (n = 55) were randomised to receive either usual care or a targeted intervention based on a TTs approach, over a 16-week treatment period. The targeted intervention consisted of individualised biomarker-informed treatment and a multidisciplinary treatment plan guided by the identified TTs in each patient. The primary outcome was health-related quality of life, as assessed by the Asthma Quality of Life Questionnaire (AQLQ). The results of this study demonstrated a statistically and clinically significant improvement in health-related quality of life in the targeted intervention group, with a mean increase in AQLQ score of 0.86 from baseline (p < 0.001), compared with a mean value of −0.004 in the usual care group, which represented no significant change64.
A possible methodology to compare different types of individualised care could comprise a study in which a stacked approach—in which all seven prime traits are evaluated and treated in parallel—is compared with sequential assessment and treatment of traits to determine which leads to quicker disease control. Further studies could investigate prime traits versus a wider array of traits, and a specialist TTs service versus a solo practitioner aided by a practice nurse, as well as comparing different funding models. Findings of such studies could help to facilitate widespread acceptance and implementation of a TTs approach.
When should treatable traits be assessed in clinical practice
We believe that a strategy based on TTs can and should be applied from the first visit and continued during follow-up. Of course, some TTs (e.g. adherence and inhaler technique) can only be applied during follow-up, after the patient has initiated therapy, but others can be assessed from the very first visit (e.g. symptoms, smoking, exacerbations and comorbidities).
Cost of implementation
Finally, another persistent concern relates to potential costs associated with implementation of the TTs approach. We anticipate that, after an initial investment into clinical investigations, lifetime costs will likely be reduced due to potential improvement in exacerbation rate and clinical outcomes12, and from the improved cost-effectiveness of rationally targeted interventions rather than ‘trials of treatment’.
Challenges in implementation in low-middle income countries
We recognise that there may be specific challenges for implementation of a TTs strategy in low-middle income countries (LMICs)65, including: (1) limited access to spirometry66. Hence, evaluation of airflow limitation is challenging; (2) although not exclusive to LMICs, clinicians in these settings may not have sufficient time with patients at consultations, which can negatively impact communication67. Hence, patient engagement, education and empowerment may be perceived as challenging; (3) access to FeNO testing is currently very limited68; (4) obtaining blood tests, such as eosinophil counts, may have financial implications for patients as, in many settings, healthcare is privatised and government resources are limited66. Further, the eosinophil count cut of 300 cells/μL may not be applicable to some LMICs69. Using this cutoff may lead to a higher proportion of patients being on ICS and may increase the risk of pneumonia in this population70. Despite these challenges, we believe that a basic TTs approach is feasible, even in such settings and that the improved targeting of treatment options is likely to prove clinically effective and cost effective in the wider perspective.
Conclusions
The burden of disease for asthma and COPD remains high because of the complexity and heterogeneity of these diseases. It is time to advance towards the identification and targeting of TTs in order to treat the individual patient and look beyond the disease label they have been assigned.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
References
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. https://ginasthma.org/wp-content/uploads/2023/05/GINA-2023-Full-Report-2023-WMS.pdf (2023).
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2023 Report). https://goldcopd.org/wp-content/uploads/2023/01/GOLD-2023-ver-1.2-7Jan2023_WMV.pdf (2023).
McDonald, V. M. & Gibson, P. G. Treatable traits and their application in high-, middle- and low-income countries. Respirology 24, 942–943 (2019).
Agusti, A. et al. Treatable traits: toward precision medicine of chronic airway diseases. Eur. Respir. J. 47, 410–419 (2016).
Pavord, I. D. et al. After asthma: redefining airways diseases. Lancet 391, 350–400 (2018).
Shaw, D. E., Gaynor, C. M. & Fogarty, A. W. Changes in asthma mortality in England and Wales since 2001. Thorax 74, 1174–1175, https://doi.org/10.1136/thoraxjnl-2019-213350 (2019).
Shaw, D. E. et al. Balancing the needs of the many and the few: where next for adult asthma guidelines? Lancet Respir. Med. 9, 786–794 (2021).
Beasley, R. et al. Optimal asthma control: time for a new target. Am. J. Respir. Crit. Care Med. 201, 1480–1487 (2020).
Bateman, E. D. et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am. J. Respir. Crit. Care Med. 170, 836–844 (2004).
Beasley, R. et al. Inhaled corticosteroid therapy in adult asthma. Time for a new therapeutic dose terminology. Am. J. Respir. Crit. Care Med. 199, 1471–1477 (2019).
Fabbri, L. M. et al. COPD and multimorbidity: recognising and addressing a syndemic occurrence. Lancet Respir. Med. https://doi.org/10.1016/s2213-2600(23)00261-8 (2023).
Agusti, A., Gibson, P. G. & McDonald, V. M. Treatable traits in airway disease: from theory to practice. J. Allergy Clin. Immunol. Pract. 11, 713–723 (2023).
Kirkland, S. W., Cross, E., Campbell, S., Villa-Roel, C. & Rowe, B. H. Intramuscular versus oral corticosteroids to reduce relapses following discharge from the emergency department for acute asthma. Cochrane Database Syst. Rev. 6, CD012629 (2018).
Rowe, B. H., Spooner, C. H., Ducharme, F. M., Bretzlaff, J. A. & Bota, G. W. Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst. Rev. 18, CD000195 (2007).
Bloechliger, M. et al. Adverse events profile of oral corticosteroids among asthma patients in the UK: cohort study with a nested case-control analysis. Respir. Res. 19, 75 (2018).
Price, D. B. et al. Adverse outcomes from initiation of systemic corticosteroids for asthma: long-term observational study. J. Asthma Allergy 11, 193–204 (2018).
Barry, L. E., Sweeney, J., O’Neill, C., Price, D. & Heaney, L. G. The cost of systemic corticosteroid-induced morbidity in severe asthma: a health economic analysis. Respir. Res. 18, 129 (2017).
Blakey, J. et al. Oral corticosteroids stewardship for asthma in adults and adolescents: a position paper from the Thoracic Society of Australia and New Zealand. Respirology 26, 1112–1130 https://doi.org/10.1111/resp.14147.
Sweeney, J. et al. Comorbidity in severe asthma requiring systemic corticosteroid therapy: cross-sectional data from the Optimum Patient Care Research Database and the British Thoracic Difficult Asthma Registry. Thorax 71, 339–346 (2016).
Seys, S. F. et al. Cluster analysis of sputum cytokine-high profiles reveals diversity in T(h)2-high asthma patients. Respir. Res. 18, 39 (2017).
Peters, M. C. et al. Measures of gene expression in sputum cells can identify TH2-high and TH2-low subtypes of asthma. J. Allergy Clin. Immunol. 133, 388–394 (2014).
George, L. & Brightling, C. E. Eosinophilic airway inflammation: role in asthma and chronic obstructive pulmonary disease. Ther. Adv. Chronic Dis. 7, 34–51 (2016).
Heaney, L. G. et al. Eosinophilic and noneosinophilic asthma: an expert consensus framework to characterize phenotypes in a global real-life severe asthma cohort. Chest 160, 814–830 (2021).
David, B., Bafadhel, M., Koenderman, L. & De Soyza, A. Eosinophilic inflammation in COPD: from an inflammatory marker to a treatable trait. Thorax 76, 188 (2021).
Hastie, A. T. et al. Association of sputum and blood eosinophil concentrations with clinical measures of COPD severity: an analysis of the SPIROMICS cohort. Lancet Respir. Med. 5, 956–967 (2017).
Wagener, A. H. et al. External validation of blood eosinophils, FE(NO) and serum periostin as surrogates for sputum eosinophils in asthma. Thorax 70, 115–120 (2015).
Yancey, S. W. et al. Biomarkers for severe eosinophilic asthma. J. Allergy Clin. Immunol. 140, 1509–1518 (2017).
Price, D. et al. Using fractional exhaled nitric oxide (FeNO) to diagnose steroid-responsive disease and guide asthma management in routine care. Clin. Transl. Allergy 3, 37 (2013).
British Thoracic Society and Scottish Intercollegiate Guidelines Network. British Guideline on the Management of Asthma. https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/ (2019).
Louis, R. et al. European Respiratory Society guidelines for the diagnosis of asthma in adults. Eur. Respir. J 15, 21015852101585, https://www.ncbi.nlm.nih.gov/pubmed/35169025 (2022).
Korevaar, D. A. et al. Effectiveness of FeNO-guided treatment in adult asthma patients: a systematic review and meta-analysis. Clin. Exp. Allergy 53, 798–808 (2023).
Boddy, C. E. et al. Clinical outcomes in people with difficult-to-control asthma using electronic monitoring to support medication adherence. J. Allergy Clin. Immunol. Pract. 9, 1529–1538.e1522 (2021).
Faruqi, S. et al. Suppression of F (ENO) with observed inhaled corticosteroid therapy in severe asthma: is it a useful test in clinical practice? ERJ Open Res. 5, https://doi.org/10.1183/23120541.00123-2019 (2019).
Butler, C. A. et al. Utility of fractional exhaled nitric oxide suppression as a prediction tool for progression to biologic therapy. ERJ Open Res. 00273–02021. https://doi.org/10.1183/23120541.00273-2021 (2021).
Barry, L. E., O’Neill, C., Butler, C., Chaudhuri, R. & Heaney, L. G. Cost-effectiveness of fractional exhaled nitric oxide suppression testing as an adherence screening tool among patients with difficult-to-control asthma. J. Allergy Clin. Immunol. Pract. 11, 1796–1804.e1793, https://doi.org/10.1016/j.jaip.2023.03.008 (2023).
University of Southampton. Research project: DEFINE: Development and Evaluation of a FeNO-Guided Asthma Management Intervention in Primary Care. https://www.southampton.ac.uk/research/projects/m-thomas-nihr-pgfar-via-oxford-development-evaluation-of-an-online-feno-guided (2022).
Singh, D. et al. Blood eosinophils and chronic obstructive pulmonary disease: a global initiative for chronic obstructive lung disease science committee 2022 review. Am. J. Respir. Crit. Care Med. 206, 17–24 (2022).
Lee, L. A. et al. Efficacy and safety of once-daily single-inhaler triple therapy (FF/UMEC/VI) versus FF/VI in patients with inadequately controlled asthma (CAPTAIN): a double-blind, randomised, phase 3A trial. Lancet Respir. Med. 9, 69–84 (2021).
Demarche, S. F. et al. Effectiveness of inhaled corticosteroids in real life on clinical outcomes, sputum cells and systemic inflammation in asthmatics: a retrospective cohort study in a secondary care centre. BMJ Open 7, e018186 (2017).
Price, D. B. et al. Blood eosinophil count and prospective annual asthma disease burden: a UK cohort study. Lancet Respir. Med. 3, 849–858 (2015).
Couillard, S. et al. Derivation of a prototype asthma attack risk scale centred on blood eosinophils and exhaled nitric oxide. Thorax 77, 199–202 (2021).
McDonald, V. M., Higgins, I. & Gibson, P. G. Insight into older peoples’ healthcare experiences with managing COPD, asthma, and asthma-COPD overlap. J. Asthma 50, 497–504 (2013).
Reddel, H. K. et al. Heterogeneity within and between physician-diagnosed asthma and/or COPD: NOVELTY cohort. Eur. Respir. J. 58, https://doi.org/10.1183/13993003.03927-2020 (2021).
Jaakkola, M. S., Hyrkäs-Palmu, H. & Jaakkola, J. J. K. Residential exposure to dampness is related to reduced level of asthma control among adults. Int. J. Environ. Res. Public Health 19, https://doi.org/10.3390/ijerph191811338 (2022).
Simpson, A. J. et al. Treatable traits in the European U-BIOPRED adult asthma cohorts. Allergy 74, 406–411 (2019).
McDonald, V. M. et al. Treatable traits can be identified in a severe asthma registry and predict future exacerbations. Respirology 24, 37–47 (2019).
Contoli, M. et al. Fixed airflow obstruction due to asthma or chronic obstructive pulmonary disease: 5-year follow-up. J. Allergy Clin. Immunol. 125, 830–837 (2010).
O’Donnell, D. E. & Gebke, K. B. Activity restriction in mild COPD: a challenging clinical problem. Int. J. Chron. Obstruct. Pulmon. Dis. 9, 577–588 (2014).
Kew, K. M., Mavergames, C. & Walters, J. A. Long-acting beta2-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 15, CD010177 (2013).
Bhatt, S. P. et al. Dupilumab for COPD with type 2 inflammation indicated by eosinophil counts. N. Engl. J. Med. 389, 205–214 (2023).
Gruffydd-Jones, K., Ward, S., Stonham, C., Macfarlane, T. V. & Thomas, M. The use of exhaled nitric oxide monitoring in primary care asthma clinics: a pilot study. Prim. Care Respir. J. 16, 349–356 (2007).
Heaney, L. G. et al. Remotely monitored therapy and nitric oxide suppression identifies nonadherence in severe asthma. Am. J. Respir. Crit. Care Med. 199, 454–464 (2019).
McNicholl, D. M., Stevenson, M., McGarvey, L. P. & Heaney, L. G. The utility of fractional exhaled nitric oxide suppression in the identification of nonadherence in difficult asthma. Am. J. Respir. Crit. Care Med. 186, 1102–1108 (2012).
Santillo, M. et al. Qualitative study on perceptions of use of Fractional Exhaled Nitric Oxide (FeNO) in asthma reviews. npj Prim. Care Respir. Med. 32, 13 (2022).
Bårnes, C. B. & Ulrik, C. S. Asthma and adherence to inhaled corticosteroids: current status and future perspectives. Respir. Care 60, 455–468 (2015).
Humenberger, M. et al. Adherence to inhaled therapy and its impact on chronic obstructive pulmonary disease (COPD). BMC Pulm. Med. 18, 163 (2018).
Kocks, J. W. H. et al. Systematic review of association between critical errors in inhalation and health outcomes in asthma and COPD. npj Prim. Care Respir. Med. 28, 43 (2018).
Chaudhuri, R. et al. Effects of smoking cessation on lung function and airway inflammation in smokers with asthma. Am. J. Respir. Crit. Care Med. 174, 127–133 (2006).
van Eerd, E. A., van der Meer, R. M., van Schayck, O. C. & Kotz, D. Smoking cessation for people with chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 8, CD010744 (2016).
Parry, G. D. et al. Cognitive behavioural intervention for adults with anxiety complications of asthma: prospective randomised trial. Respir. Med. 106, 802–810 (2012).
Eastwood, M. C. et al. A randomized trial of a composite T2-biomarker strategy adjusting corticosteroid treatment in severe asthma: a post hoc analysis by sex. J. Allergy Clin. Immunol. Pract. 11, 1233–1242.e1235 (2023).
O’Byrne, P. M. et al. Inhaled combined budesonide-formoterol as needed in mild asthma. N. Engl. J. Med. 378, 1865–1876 (2018).
Pascoe, S. et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir. Med. 7, 745–756 (2019).
McDonald, V. M. et al. Targeting treatable traits in severe asthma: a randomised controlled trial. Eur. Respir. J. 55, 1901509 (2020).
Barne, M. Gaps in asthma diagnosis and treatment in low- and middle-income countries. Front. Allergy 4, 1240259 (2023).
Masekela, R., Zurba, L. & Gray, D. Dealing with access to spirometry in Africa: a commentary on challenges and solutions. Int. J. Environ. Res. Public Health 16, https://doi.org/10.3390/ijerph16010062 (2018).
Irving, G. et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open 7, e017902 (2017).
Loewenthal, L. & Menzies-Gow, A. FeNO in asthma. Semin. Respir. Crit. Care Med. 43, 635–645 (2022).
Dhumal, P. Absolute blood eosinophil counts among 3,763 healthy, asthmatic, and COPD subjects across India. Eur. Respir. J. 62, PA3602 (2023).
Zhang, Q. et al. Risk of pneumonia with different inhaled corticosteroids in COPD patients: a meta-analysis. Copd 17, 462–469 (2020).
Acknowledgements
Medical writing support under the direction of the authors, including assisting authors with the development of the manuscript drafts, incorporation of comments, fact checking and referencing was provided by Jasmine Bensilum, MSc, and editorial support, including formatting, proofreading and submission, was provided by Sarah Christopher, PhD all of Prime (Knutsford, UK), supported by GSK according to Good Publication Practice guidelines (https://www.acpjournals.org/doi/10.7326/M22-1460). This work was funded by GSK through the Treatable Traits Initiative. The 2021 Treatable Traits in Airways Diseases International Symposium was a scientific meeting organised by GSK for HCPs with a documented interest in airways diseases. Delegates were not paid for their participation.
Author information
Authors and Affiliations
Contributions
The authors were jointly responsible for developing the outline and for input into subsequent drafts, including critical review and revisions of the paper. All authors have read and approved the final draft for publication. The sponsor and authors were jointly involved in conceptualisation; however, the ultimate responsibility for opinions and conclusions presented lies with the authors.
Corresponding author
Ethics declarations
Competing interests
AA has research grants from AstraZeneca, GSK and Menarini; is a lector for AstraZeneca, Chiesi, Cipla, GSK, Menarini, Sanofi and Zambon; and is a member of scientific boards for AstraZeneca, Chiesi, GSK, Menarini and Sanofi. PGG has research grants from AstraZeneca and GSK; consulting lecturing and advisory board honoraria from AstraZeneca, Chiesi, GSK, Novartis and Sanofi; and is a respiratory physician at John Hunter Hospital, New South Wales, Australia. LGH has research grants from Aerocrine, Amgen, AstraZeneca, Genentech (Roche), GSK, MedImmune, Novartis and Vitalograph; consulting lecturing and advisory board honoraria from AstraZeneca, Boehringer Ingelheim, Chiesi, Circassia, Evelo Biosciences, GSK, Napp Pharmaceuticals, Novartis, Roche, Teva and Theravance; and is a clinical professor a Queens University and Belfast City Hospital, Belfast, UK. MT has consulting lecturing honoraria from GSK and is an Emeritus Professor of Primary Care Research at the University of Southampton, UK. All authors have no non-financial competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Agusti, A., Gibson, P.G., Heaney, L.G. et al. Change is in the air: key questions on the ‘Treatable Traits’ model for chronic airway diseases in primary care. npj Prim. Care Respir. Med. 34, 21 (2024). https://doi.org/10.1038/s41533-024-00381-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-024-00381-y
This article is cited by
-
Qualitative insights into planning implementation of FeNO-guided asthma management in primary care
npj Primary Care Respiratory Medicine (2025)
-
Emerging Therapeutics in COPD: Mapping Innovation to Treatable Traits
Lung (2025)