Abstract
The asthma diagnosis jigsaw puzzle is a clinical practice and teaching concept conceived in clinical practice and refined through an expert multidisciplinary consensus process by academics and clinicians with an interest in primary respiratory care. The concept incorporates guidance to facilitate the effective diagnosis of adults or children with asthma in primary care where misdiagnosis is common. The jigsaw puzzle metaphor teaches a problem-solving approach to diagnosis, introducing the concept of diagnosis over time and in no particular sequence. Puzzle pieces can be collected from the domains of presentation, history, symptoms and physical examination, as well as objective tests. The clinician’s challenge is to complete the diagnostic jigsaw puzzle testing the likelihood of a picture which can be recognised as asthma. This approach aligns with symptom-based pattern-recognition approaches taught to primary care clinicians which gets easier and more reliable with experience. Relational continuity, or informational continuity through the patient record, is integral to the process of puzzle completion. Where non-fitting puzzle pieces are encountered, alternative or additional diagnoses should be considered and/or referral to secondary care pursued. As a metaphor, ‘puzzle completion’ may be used within clinical communication encounters, addressing the importance of partnership working (‘completing the puzzle together’), uncertainty (deciding ‘which pieces fit’) and changes in symptoms over time (enabling the ‘puzzle picture to become clearer’). Adaptation of this teaching concept has started through translation of educational resources, including puzzle pieces. Supporting case vignettes developed locally will contextualise the jigsaw puzzle teaching concept. The Asthma Diagnosis Jigsaw Puzzle teaching concept has been piloted in North Macedonia and is also developed for educational workshops by primary care health educators in Malaysia, India and Uganda.
Similar content being viewed by others
Introduction: what is the need for improved diagnosis of asthma in primary care given the availability of national and international guidelines?
Asthma is one of the most common chronic diseases encountered in primary care. The reported prevalence of asthma varies across countries, ranging from 1%–18%1, although high rates of misdiagnosis are also well documented2,3,4. Evidence-based guidelines and consensus recommendations exist to support clinicians with asthma diagnosis5,6,7,8. For example, treatment pathways provided by the Global Initiative for Asthma (GINA), start from diagnosis based on symptoms and a demonstration of variable airflow obstruction (and/or reversibility) using peak flow and/or spirometry9. Where available, bronchodilator responsiveness (reversibility) testing is recommended for adults and children from 5 years, when they are symptomatic. However, in practice, this can be difficult as lung function is often normal when the patient is asymptomatic or has received treatment. There are currently no tests recommended for children <5 years, typically diagnosis is based on history, observation and context, often over a period of time. In this group, asthma should be suspected if there are recurring episodes of cough, breathlessness and/or wheeze occurring with or between viral infections, that respond to bronchodilators or a trial of inhaled corticosteroids, and where there is a patient or family history of atopy10.
Current guidelines and consensus statements are typically generated by respiratory specialists using data from research studies. Such guidelines are weighted towards specialist or secondary care settings and tend to be linear or algorithmic in approach. As such they do not capture or incorporate the expertise and flexibility used by expert practitioners in primary care in guideline implementation. Here, first contact presentations with multi-morbidity are increasingly common necessitating the use of multiple, sometimes overlapping, protocols, and information is often gathered in an iterative rather than linear manner11. Additionally, access to diagnostic investigations (such as routine availability of peak flow meters or spirometry) and continuity of care is either limited or absent in many countries.
Methods: how was the asthma diagnosis jigsaw puzzle teaching concept developed?
The concept of the jigsaw puzzle emerged from discussions between a small group of family physicians with an interest in respiratory care. To test and refine it as a diagnostic clinical practice and teaching concept, a multidisciplinary group of 20 primary care asthma experts from 14 countries was convened. The group included family physicians, a nurse, two pharmacists and adult and paediatric asthma specialists (Table 1). An in-person facilitated workshop was held over 2 days during the world conference of the International Primary Care Respiratory Group, followed by online consultations.
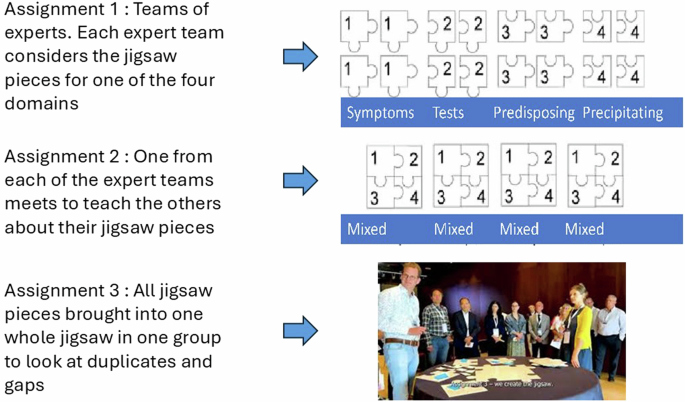
A three-round modified nominal group technique was used during the workshops12, conducted in English. This used an adapted teaching method also known as the jigsaw teaching method (Fig. 1)13 to facilitate collaboration and consensus building. Drawing on international expertise enabled content to reflect asthma diagnosis in a variety of settings, envisaging adaptation of the teaching concept across different language and resource contexts.
Prior to the workshop, the faculty categorised the asthma diagnostic process into four domains: presenting symptoms, physical examination and investigations, predisposing factors and precipitating factors, informed by case formulation used in biopsychosocial approaches14. Participants were advised that the goal was to build an asthma jigsaw puzzle. For Assignment 1, participants were allocated to one of the domain groups based on role, country and area of expertise. Each domain group was invited by the facilitators to discuss and agree on the most important factors—jigsaw pieces—in their domain which were described using the ‘why/how/when/who’ framework to justify inclusion (Box 1).
During the workshop, the original terms “predisposing factors” and “precipitating factors” (i.e. what prompted the presentation) were revised following vigorous debate. The final categorisation of domains was clarified as follows: Presentation, history, symptoms and physical examination and objective tests, to ease understanding of the multi-national primary care audience.
In Assignment 2, participants were each asked to move to a different table so that all four domains were represented at each table. Participants advocated for their jigsaw pieces, duplicates were prioritised and by consensus placed in the most relevant domain.
For Assignment 3, participants came together as a whole group, presenting and agreeing the final puzzle pieces required to construct a complete jigsaw puzzle. This final stage was led by two facilitators, one ensuring that all groups had the opportunity to speak, the other ensuring clarity and accuracy of language for each item of content and related descriptors.
A video summary of these stages can be seen here.
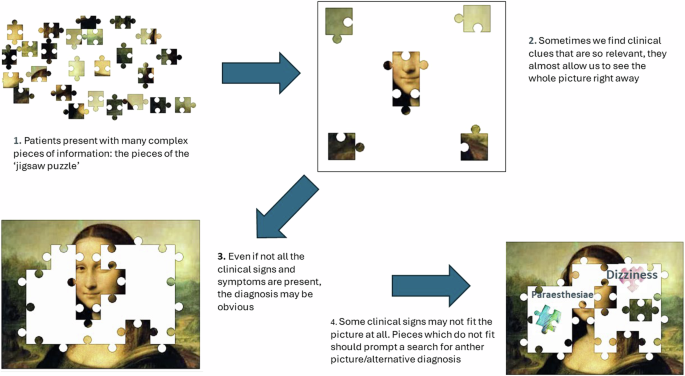
Following the in-person workshops, expert participants were invited to form a writing group. This group met three times. There was consensus that the metaphor of a jigsaw puzzle would be a helpful educational and teaching concept. The group decided that key outputs from the workshop should be a desktop helper, a practical two-page guide for global primary care and at least one peer-reviewed publication that explained the process. A sub-group finalised the desktop helper and, after trial and error, chose a famous image to illustrate the jigsaw puzzle metaphor as shown in Fig. 2.
Discussion: how does the asthma diagnosis jigsaw puzzle teaching concept add value to the challenge of asthma diagnosis?
The Asthma Diagnosis Jigsaw Puzzle is a practical and adaptable teaching concept which aims to improve confidence and competence in the diagnosis of asthma for adults and children, irrespective of resource setting. There are different ways to complete a jigsaw puzzle. A primary care clinician starts by finding the four corners, which, in the jigsaw puzzle metaphor could represent either the cardinal symptoms of asthma, (wheeze, cough, breathlessness and tight chest) or the domains (presentation, symptoms and physical examination, history and objective tests). At least some of these would point the clinician towards a diagnosis of asthma. Additional jigsaw pieces are then required to build the picture, systematically collected from the (adult) patient or, in the case of children, from the caregiver, within categories of history, physical examination and objective tests. Where puzzle pieces do not fit, they can be considered as belonging to a different picture, prompting a reformulation of diagnostic hypotheses (Fig. 2). Over time, through gathering information the picture becomes clearer, but it is only fully complete when the central pieces (in our image, the nose and mouth) are added. These are the objective test results. Where such objective tests are not available, the final puzzle picture can often still be defined, though not as clearly as when tests are utilised. It is not intended as an exhaustive list of differential diagnoses or to provide an overview of all the complexities of making a diagnosis.
The jigsaw puzzle metaphor fits intuitive, problem-solving and pattern mapping approaches mastered by expert primary care clinicians. The process of combining pieces becomes easier over time and with experience, as patterns are recognised more reliably. Just like a jigsaw puzzle, the final picture of the diagnosis gradually takes shape, as patient and clinician identify new puzzle pieces. Adaptation of the teaching concept includes both translation of key puzzle pieces across language groups, with adjustment of content to reflect commonly encountered symptoms, history, and objective tests e.g. haemoptysis - as a non-fitting piece - in settings where TB is highly prevalent.
Communication approaches using the language of puzzle completion during clinical encounters opens the possibility for patients and families to participate in the diagnostic process. Patients and caregivers are invited to gain an understanding of the complex and changing nature of symptoms and of their disease. By responding to the idea of working together with their clinician to complete ‘the puzzle’ of diagnosis, this also enables uncertainty to be visualised within the diagnostic process rather than understood as a lack of competence on the part of their healthcare provider. In some countries ‘doctor shopping’15 is common for patients in primary care, and continuity of care is particularly challenging. The value of follow up can be emphasised using a puzzle metaphor, patients and caregivers can be reassured, guided and educated by the process of working together with the clinician to achieve the diagnosis over time.
Future plans: adaptation and roll-out of teaching resources
The launch of the asthma diagnostic jigsaw puzzle teaching concept has yielded positive responses internationally, at the WONCA World 2023 Conference, the European Respiratory Society 2023 Congress, the International Primary Care Respiratory Group’s World Conference 2024, European Academy of Allergy and Clinical Immunology (EAACI) 2024 Conference and WONCA Europe conference 2024.
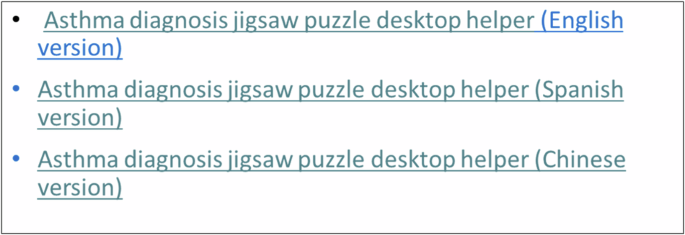
A new clinical practice and teaching resource, the ‘Desktop Helper no.15: the jigsaw puzzle approach to building a diagnostic picture of asthma in primary care over time’ has been translated from English and received positive feedback when used for teaching health professionals in North Macedonia. It is available online in a variety of languages (Fig. 3) and includes details of puzzle pieces in each domain which do not fit, where an alternative diagnosis may be relevant.
The development of additional resources to support teaching, learning and local adaptation of the asthma diagnosis jigsaw puzzle teaching concept is underway. These include locally developed case vignettes. The fidelity of the jigsaw puzzle metaphor as an adaptable teaching concept will be tested through evaluation of upcoming workshops in Uganda, Malaysia and India.
Conclusion
The variability of asthma symptoms over time and the absence of any single objective diagnostic test poses a problem for diagnosis of asthma internationally. Achieving the correct diagnosis is essential to ensure adults and children receive the right care including pharmacological treatment with inhaled medications and non-pharmacological interventions. The asthma diagnosis jigsaw puzzle teaching concept is a succinct, adaptable symptom-based approach relevant for first contact and follow-up clinical encounters in primary care. It has the potential to support more effective diagnosis of asthma and improved clinical outcomes, along with the delivery of patient-centred care. Teaching resources have been developed and are being disseminated internationally.
Data availability
No datasets were generated or analysed during the current study.
References
Porsbjerg, C., Melén, E., Lehtimäki, L. & Shaw, D. Asthma. Lancet 401, 858–873 (2023).
Gillis, R. M. E., van Litsenburg, W., van Balkom, R. H., Muris, J. W. & Smeenk, F. W. The contribution of an asthma diagnostic consultation service in obtaining an accurate asthma diagnosis for primary care patients: results of a real-life study. NPJ Prim. Care Respir. Med. 27, 35 (2017).
Starren, E. S. et al. A centralised respiratory diagnostic service for primary care: a 4-year audit. Prim. Care Respir. J. 21, 180–186 (2012).
Aaron, S. D., Boulet, L. P., Reddel, H. K. & Gershon, A. S. Underdiagnosis and overdiagnosis of Asthma. Am. J. Respir. Crit. Care Med. 198, 1012–1020 (2018).
Gaillard, E. A. et al. European respiratory society clinical practice guidelines for the diagnosis of asthma in children aged 5–16 years. Eur. Respir. J. 58, 2004173 (2021).
Louis R. et al. European respiratory society guidelines for the diagnosis of asthma in adults. Eur. Respir. J. 15, 2101585. (2022).
Venkatesan, P. 2023 GINA report for asthma. Lancet Respir. Med. 11, 589 (2023).
Excellence; NIfHaC. Asthma: Diagnosis, Monitoring and Chronic Asthma Management: NICE 2024. https://www.nice.org.uk/guidance/ng80/resources/asthma-diagnosis-monitoring-and-chronic-asthma-management-pdf-1837687975621 (2021).
Levy, M. L. et al. Key recommendations for primary care from the 2022 Global Initiative for Asthma (GINA) update. npj Prim. Care Respir. Med. 33, 7 (2023).
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. www.ginasthma.org (2024).
Wieringa, S. & Greenhalgh, T. 10 years of mindlines: a systematic review and commentary. Implement. Sci. 10, 45 (2015).
Jünger, S. & Payne, S. The crossover artist: consensus methods in health research. In Handbook of Theory and Methods in Applied Health Research (ed. Junger, S.) 188–213 (Elgaronline, 2020).
Nalls, A. J. & Wickerd, G. The jigsaw method: reviving a powerful positive intervention. J. Appl. Sch. Psychol. 39, 201–217 (2023).
Borrell-Carrió, F., Suchman, A. L. & Epstein, R. M. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann. Fam. Med. 2, 576–582 (2004).
Sansone, R. A. & Sansone, L. A. Doctor shopping: a phenomenon of many themes. Innov. Clin. Neurosci. 9, 42–46 (2012).
Barber, C. M. et al. British thoracic society clinical statement on occupational asthma. Thorax 77, 433–442 (2022).
Acknowledgements
The Asthma Jigsaw Project was jointly funded by the IPCRG, GlaxoSmithKline, AstraZeneca and Vitalograph.
Author information
Authors and Affiliations
Contributions
D.R. and J.W.H.K. conceived the jigsaw puzzle metaphor; S.W. designed the workshop; D.R., J.W.H.K., S.W. and J.C.d.S. developed the desktop helper. The other authors (M.B., M.J.B., I.B., L.D., E.G., V.M., A.O., A.B.) commented on the desktop helper and contributed to the drafting, review and editing of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Figure 1 (image): all identifiable individuals have given their written consent for publication of their image.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Consent for Publication Fig. 1 (image): all identifiable individuals have given their written consent for publication of their image
The Asthma Jigsaw Project was jointly funded by the IPCRG, GlaxoSmithKline, AstraZeneca and Vitalograph. Industry sponsors took no part in the development process or in the drafting of the Desktop Helper or this manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ryan, D., Kocks, J.W.H., Williams, S. et al. The asthma diagnosis jigsaw puzzle: an adaptable teaching concept to facilitate the diagnosis of asthma in adults and children presenting to primary care. npj Prim. Care Respir. Med. 35, 14 (2025). https://doi.org/10.1038/s41533-024-00410-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-024-00410-w
This article is cited by
-
BTS/NICE/SIGN guideline for asthma 2024: Diagnosis, monitoring and chronic asthma management. How does this compare to GINA 2024?
npj Primary Care Respiratory Medicine (2025)