Abstract
Underdiagnosis and overdiagnosis commonly occur in Chronic Obstructive Pulmonary Disease (COPD) patients. We assessed diagnostic accuracy, clinical characteristics, healthcare utilization, and care plan registration for patients undergoing primary care. We conducted a cross-sectional, population-based study using a health record registry from four primary healthcare centers in Catalonia (Spain) for patients aged ≥15 years. The variables included sociodemographic characteristics, dyspnea, comorbidities, spirometry results, treatments, and healthcare use. Logistic regression models were used to analyze differences between patients with and without airflow limitation, and ordinal logistic regression models were used to examine the association between disease severity and healthcare use. Among the 2610 patients, 54% had spirometry data, 29.5% had confirmed airflow obstruction, and 24% were overdiagnosed according to the GOLD criteria. Patients without airflow obstruction were younger (OR: 0.98, 95% CI: 0.96–0.99) and more likely to be current smokers (OR: 1.44, 95% CI: 1.13–1.84). Airflow obstruction severity was significantly associated with increased use of emergency home ambulance use (OR: 1.7, 95% CI: 1.23–2.35), emergency department visits (OR: 1.48, 95% CI: 1.11–1.99), and hospital admission (OR: 1.8, 95% CI: 1.32–2.47), but not primary care visits and follow-up frequency. COPD is frequently overdiagnosed in primary healthcare settings. The severity of airflow obstruction is associated with increased healthcare utilization, including hospital admissions. Improved diagnostic accuracy and management may enhance COPD care and reduce healthcare costs.
Similar content being viewed by others
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is the third leading cause of death globally1. COPD is associated with significant morbi-mortality2,3, with avoidable hospitalizations and increased healthcare utilization4. According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD), diagnosing COPD requires both clinical assessment and lung function testing, with forced spirometry showing post-bronchodilator (post-BD) airflow obstruction, defined by a post-BD forced expiratory volume in 1 s (FEV1) / Forced Vital Capacity (FVC) ratio < 0.75. COPD diagnoses are frequently made in family medicine and Primary Healthcare (PHC) consultations when patients report symptoms such as fatigue, dyspnea, and long-term smoking6. Despite patients being labeled with a diagnosis of COPD, confirmatory spirometry is frequently delayed or omitted entirely, resulting in a significant risk of over- or misdiagnosis7, with only 31% of patients with a COPD diagnosis having documented spirometry results8.
COPD management and follow-up are based on assessing symptoms and risk of exacerbation5; it includes non-pharmacological interventions, such as smoking cessation, immune protection with vaccinations (i.e., COVID-19, influenza, pneumococcal, and RSV), pulmonary rehabilitation during the stable phase and after an exacerbation, self-management education, and exercise training. Pharmacological treatments should be individualized, with regular evaluations of inhaler techniques. International guidelines recommend interdisciplinary and integrated care approaches that encompass family medicine specialists, GPs, nurses, and other healthcare professionals5. However, the availability of the healthcare workforce varies across healthcare systems, limiting healthcare delivery. In Spain, there are approximately 0.77 GPs per 1000 inhabitants in the primary healthcare setting9, while the distribution of pulmonologists is 0.4 per 1000 inhabitants10. However, despite the existing recommendations, there is a lack of evaluations on how COPD care is implemented in clinical practice11,12.
Studies have focused on assessing diagnostic accuracy13, drug treatment pathways14, comorbidity3, patient severity characteristics15, and the potential for avoidable hospitalizations11,12. However, limited research has examined all these factors alongside specific care plans for patients with COPD and other non-pharmacological interventions in the PHC. Additionally, epidemiological estimates for COPD prevalence are often derived from survey data or non-representative samples, such as patients linked with hospitals13, complicating efforts to assess the COPD burden accurately in family medicine consultations and the broader PHC setting13,16. Therefore, this study aimed to estimate the prevalence of COPD in the PHC, examine under and over-diagnosed COPD, and assess the clinical characteristics, healthcare utilization, implementation of specific care plans, and healthcare services associated with the severity of airflow obstruction in patients with COPD.
Material and methods
Study design and context
This population-based study used the PHC Electronic Health Record (EHR) registries of four PHC centers in Catalonia, Spain. In the Spanish healthcare system, all citizens are assigned to a PHC facility to receive comprehensive care for the most prevalent diseases by family medicine specialists and PHC nurses. The EHR system encompasses a wide array of clinical data, including diagnoses, health problems, and clinical indicators, as documented by family medicine physicians and PHC nurses during routine clinical follow-up appointments.
Population and participants
The study population comprised 114,303 individuals aged 15 years and older assigned to the PHC centers. Patients aged ≥15 years were included because this is when individuals transition from pediatric care to adult PHC. We included all patients with a recorded diagnosis of COPD according to the International Classification of Diseases, 10th Revision (ICD-10) codes J43.0-2, J43.8-9, J44.0-1, and J44.8-9. We excluded patients residing in institutional settings (e.g. nursing homes) and those of COPD who had died before the study initiation date.
Study variables
We retrieved the following variables from the EHR database: Spirometry data from the most recent spirometry data stored in the designated EHR fields, excluding free-text entries. In cases where no spirometry data were available in these fields, this absence does not confirm that a spirometry assessment was not conducted but rather indicates that it was not registered in the format of the EHR: The FVC, the FEV1, and the FEV1/FVC ratio, both pre-and post-bronchodilation. Sociodemographic variables: age, sex, Body Mass Index (BMI), modified Medical Research Council scale (mMRC) score for dyspnea17, and active drug prescribed treatment for COPD. We also retrieved the next grouped diseases and disorders: Cardiovascular, gastrointestinal, endocrine, musculoskeletal, neurological, respiratory (other than COPD), mental disorders, dementia, anxiety/depression, and kidney failure; detailed disease classifications within each group are provided in the web appendix. The total number of diagnosed chronic diseases is registered in the EHR. An index of comorbidity and complexity using the Adjusted Morbidity Groups Index (AMG): it is a weighted summary of morbidity of patients’ chronic diseases and acute diagnostic codes and complexity; we used the indicator ≥85th percentile, which identifies moderate to high-risk morbidity patients18 and vaccination status (seasonal flu, pneumococcus, herpes zoster, and COVID-19). We also retrieved patients’ active COPD care plans, identifying whether PHC nurses perform specific COPD clinical follow-up and secondary prevention activities, as well as smoking habits (current smoker, cigarettes/day, packs/year consumed), registered inhaler compliance, and alcohol consumption (yes/no). Healthcare use data for the previous year were collected, including family physicians’ and PHC nurses’ consultations and hospital and emergency use services: Home ambulance calls, emergency department visits, and hospital admissions.
Data extraction and analysis
On March 15, 2024, data were extracted from the EHR system using a Structured Query Language (SQL) query to retrieve all study variables. We characterized patients with a registered COPD diagnosis using descriptive statistics. Continuous variables were summarized with means and standard deviations, whereas categorical variables were presented as frequencies and percentages. The overall prevalence of COPD diagnoses was calculated using the number of patients with a documented COPD diagnosis as the numerator and the total number of patients registered as the denominator. Additionally, we computed the prevalence of confirmed COPD cases according to the GOLD criteria, defined as patients with a registered COPD diagnosis and demonstrable airflow obstruction based on their most recent FEV1/FVC post-BD ratio. Prevalence was stratified across three age groups: 15–50, >50–75, and ≥75 years old.
Differences between patients with and without airflow obstruction were analyzed using logistic regression models, as defined by the FEV1/FVC post-BD ratio (<0.7 and ≥0.7). In these models, the presence or absence of airflow obstruction was the outcome variable. The explanatory variables included sociodemographic characteristics, risk factors, comorbidities, and current drug treatments.
The severity of airflow obstruction was analyzed using the GOLD grades when postbronchodilator FEV1 data were available. We used an ordinal logistic regression model with GOLD classification as the response variable and patient characteristics and risk factors as explanatory. The models were adjusted for potential confounders, including sex, age, and AMG index. All results are reported as adjusted odds ratios (ORs) with 95% confidence intervals (CIs) and P-values, using a confidence level of 95% (p < 0.05). All statistical analyses were conducted using R software19.
Ethics and data access
The study was conducted following the 1975 Declaration of Helsinki. The institutional ethics committee approved the protocol for human research (HCB/2023/1053). Informed consent was waived, given that the data were anonymized, ensuring patient confidentiality and preventing researchers from identifying them.
Results
Of the total population assigned to the PHC centers, 95% (n = 109,008) had a health record, and we identified a total of 2,610 patients with a COPD registry in the EHR, yielding a prevalence of 2.39% (95% CI: 2.3–2.5%). Of these, 61.7% were male, with a mean age of 73 years, and an average COPD diagnosis duration of 8.9 years (SD: 7.2). A history of smoking was recorded in 44.9% of smokers as current or former, and 25.5% reported experiencing moderate to severe dyspnea. A high comorbidity burden (AMG ≥ P85) was observed in 86.3% of patients, with cardiovascular diseases (65.9%) and musculoskeletal conditions (44.1%) being the most prevalent comorbidities. Anxiety and depression were noted in 47.3% of participants. Other respiratory diseases were registered in 6.8% of patients, and asthma was recorded in 6.4% (95% CI: 5.2%;7.8%). The most prescribed drug was SAMA (36.4%), followed by LABA–LAMA combinations (13.9%); all characteristics are presented in Table 1.
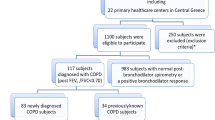
The post-BD FEV1/FVC ratio was either not recorded or unavailable in the EHR for 1,201 patients (46%, 95% CI: 44.1–47.9%). In patients who underwent spirometry, 24% (95% CI: 22.81–26.14%) had no evidence of airflow obstruction (post-BD FEV1/FVC ratio ≥ 0.7). The prevalence of COPD (based on the confirmation of post-BD airflow obstruction) decreased to 0.7% (95% CI: 0.66–0.76%). The flow chart in Fig. 1 shows the prevalence of COPD in the study population and among individuals with and without airflow obstruction.
Patients with and without airflow obstruction showed that overdiagnosed patients were younger (mean age: 71.96 vs. 74.54 years old; OR: 0.98, 95% CI: 0.96–0.99) and more likely to have a registry of current smoking (50.32% vs. 41.30%; OR: 1.44, 95% CI: 1.13–1.84). Patients were also more treated than patients without airflow obstruction, but 38.1% had an active prescription of SAMA and 11.6% had an active prescription of SABA. All other clinical characteristics, including dyspnea symptoms and primary care service utilization, showed no statistically significant differences. The results of the association study are presented in Table 2.
The airflow obstruction severity according to the GOLD grades based on patient characteristics, risk factors, assigned care plans, non-pharmacological follow-up activities, and PHC service utilization showed no significant associations with the frequency of consultations with PHC physicians or nurses over the past 12 months. Furthermore, no association was found between GOLD grades and the assignment of specific COPD care plans, typically including clinical activities, such as patient education, guidance, and secondary prevention, primarily administered by PHC nurses. Preventive vaccination rates for seasonal influenza and COVID-19 were not associated with GOLD grades. However, we found a significant association between higher GOLD grades and increased use of emergency home ambulance services (OR: 1.7, 95% CI: 1.23–2.35), more frequent hospital emergency department visits (OR: 1.48, 95% CI: 1.11–1.99), and higher hospital admission rates (OR: 1.8, 95% CI: 1.32–2.47). The results are presented in Table 3.
Discussion
Results of this study show that the registered prevalence of COPD is affected by a substantial proportion of overdiagnoses and that half of all patients with a COPD registry in the EHR lack evidence of airflow obstruction due to unavailable or absent spirometry. Despite the absence of post-BD airflow obstruction data, patients with over-diagnosed COPD had a record of clinical symptoms of dyspnea, with no differences having been observed compared with those with confirmed COPD. Healthcare utilization, including consultations, specific care plans, and nonpharmacological interventions, did not vary significantly across GOLD grades. However, higher airflow obstruction was associated with increased hospital admissions, emergency department visits, and ambulance use in 2019.
Nearly half (46%) of patients diagnosed with COPD lacked spirometry data, and 24% were overdiagnosed without airflow obstruction. This resulted in almost 75% of COPD diagnoses not fulfilling or proving the COPD criteria. The over-diagnosis proportion (i.e., patients diagnosed without airflow obstruction) was in line with a recent meta-analysis of the literature, which reported 14–26% of patients diagnosed with COPD without spirometry results not proving the airflow obstruction and 25–50% of clinician-registered patients having COPD without a spirometry13. The absence of spirometry data in the EHR does not necessarily indicate that spirometry was not performed to diagnose COPD. It is possible that spirometry was conducted but was not recorded in the corresponding EHR fields or linked to the patient’s digital records. However, a persistent issue remains regarding clinicians’ inconsistent use and interpretation of spirometry results despite scientific societies advocating that COPD diagnoses and treatment should only be initiated following objective testing5,20. The spirometry approach may require modifications to enhance the COPD screening process, particularly in family medicine facilities. Expanding the use and interpretation of spirometry to other PHC healthcare professionals or supporting physicians in implementing new applications and algorithms could optimize patient management21,22. This approach would also facilitate patient-clinician communication, potentially adding clinical value beyond the confirmatory role that spirometry currently plays in COPD diagnosis23,24.
Patients clinically diagnosed with COPD but without airflow obstruction showed respiratory symptoms comparable to confirmed COPD cases25. These individuals were generally younger, had higher rates of overweight and obesity, and were more likely to have a history of current smoking. This subgroup may include patients with COPD overdiagnoses or pre-COPD characteristics. Similarly, a population-based study in Spain found that patients with pre-COPD were younger, had a higher proportion of females, had a greater body mass index, and experienced similar symptoms of dyspnea26. However, the clinical presentation, defining characteristics, and associated risks of pre-COPD require further scientific investigation. Given that clinicians treat these patients as if they have COPD, clinical guidance and recommendations to ensure appropriate treatment strategies within these two groups are needed.
Patients with higher airflow obstruction showed similar frequencies of assigned care plans, nonpharmacological follow-up activities, and PHC service use as those with lower disease severity. However, they were associated with significantly higher use of emergency services and higher hospitalization rates. A Study in the Northern-Central region of Spain found no association in influenza vaccination rates across COPD severity groups, which ranged from 65.3–52%, compared with 59.48–61.9% in our study. Similarly, 73–75% of patients had received the pneumococcal vaccine, compared with 64–70.9% in our cohort27. Active care plans documented in the EHR suggest a decline in secondary prevention activities for COPD, consistent with reports indicating that only 32% of patients with COPD had self-management plans incorporating dietary advice, exercise, and exacerbation management15. Preventive interventions were associated with reduced emergency department visits (OR 0.53, 95% CI: 0.32–0.87) and decreased hospital admissions (OR 0.75, 95% CI: 0.57–0.98)28. However, our findings revealed that patients with severe COPD received similar care from family physicians and PHC nurses as those with milder forms of the disease. This uniformity in care provision persisted despite the observed association between increased COPD severity and higher utilization of emergency services, including home ambulance calls, emergency department visits, and hospital admissions. This discrepancy between disease severity and intervention intensity suggests a potential gap in the tailoring of care plans to the specific needs of patients with more severe COPD who might benefit from more intensive monitoring and management at the primary care level to potentially mitigate their higher utilization of acute care services, including avoidable hospitalizations.
Practical implications
This study emphasizes significant concerns regarding the limited clinical application of spirometry and the inadequate follow-up of pharmacological and non-pharmacological interventions for patients with COPD in the PHC setting. COPD diagnosis and management may benefit from a multifaceted, interdisciplinary approach within PHC. Integration of PHC physicians, nurses, and physiotherapists might be crucial to generalizing the use of spirometry and ensuring that patients with COPD receive not only reactive care during exacerbations but also proactive management aimed at preventing exacerbations and promoting lung health and patients’ best quality of life.
The high rates of hospitalizations and emergency service use among patients with COPD highlight the urgent need for enhanced coordination between hospitals and PHC settings. Strengthening communication and collaboration between healthcare settings is crucial for preventing recurrent hospital admissions and ensuring continuous, proactive management of COPD in an integrated care environment29.
Limitations
Data were obtained from four PHC centers, covering the entire population assigned to each center. Due to technical limitations, we could not retrieve the text registered in the EHR. Data on the number of exacerbations per year, including those requiring antibiotics or corticosteroids and hospitalizations linked to COPD (we could only extract the number of hospitalizations per patient), were unavailable in the EHR using the data extraction methodology. A high proportion of spirometry data was not recorded or was unavailable because PHC clinicians did not complete the corresponding EHR fields when the spirometer EHR links were not used. While this limits the accuracy, it also reflects the low-value placed on spirometry in routine clinical practice. Furthermore, we could not extract Alpha-1 antitrypsin deficiency because this is typically examined in hospitals. We did not exclude patients with an asthma registry because we did not assess its validity; however, the proportion of patients with this registry was only 6.4%. Additionally, the study’s cross-sectional design limits the ability of the researchers to establish causal relationships between variables.
Conclusions
A substantial proportion of COPD diagnoses in primary healthcare are false positives, with limited use of spirometry for diagnostic confirmation. Overdiagnosed patients showed dyspnea symptoms similar to those with confirmed COPD, leading to the need for pharmacological treatment and management. Although higher airflow obstruction was associated with increased hospital admissions, emergency department visits, and ambulance use, follow-up care and secondary prevention measures remained similar across all severity stages. Effective coordination across multiple healthcare settings among patients with higher airflow obstruction might ensure integrated care that addresses the multifaceted needs of this patient population.
Data availability
The authors will make the raw data supporting this article’s conclusions available upon reasonable request without undue reservation.
References
World Health Organization. Chronic obstructive pulmonary disease. https://www.who.int/ (2023). (accessed 09 March 2025).
Halpin, D. M. G. et al. The GOLD summit on chronic obstructive pulmonary disease in low- and middle-income countries. Int. J. Tuberc. Lung Dis. 23, 1131–1141 (2019).
Pace, W. D. et al. COPD population in US primary care: data from the optimum patient care DARTNet research database and the advancing the patient experience in COPD registry. Ann. Fam. Med. 20, 319–327 (2022).
Miravitlles, M. & Ribera, A. Understanding the impact of symptoms on the burden of COPD. Respir. Res. 18, 1–11 (2017).
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for prevention, diagnosis and management of COPD: 2024. 2024. (accessed 16 Aug 2024). https://goldcopd.org/2024-gold-report/.
Price, D., Freeman, D., Cleland, J., Kaplan, A. & Cerasoli, F. Earlier diagnosis and earlier treatment of COPD in primary care. Prim. Care Respir. J. 20, 15–22 (2011).
De Miguel Díez, J. et al. Fiabilidad del diagnóstico de la EPOC en atención primaria y neumología en Espana. Factores predictivos. Arch. Bronconeumol. 39, 203–208 (2003).
Patel, K. et al. Exploring the causes of COPD misdiagnosis in primary care: a mixed methods study. PLoS One 19, 1–12 (2024).
Spanish Ministry of Health. Informe Anual del Sistema Nacional de Salud 2023. 2023 (accessed 14 Jan 2025); https://www.sanidad.gob.es/estadEstudios/estadisticas/sisInfSanSNS/tablasEstadisticas/InfAnualSNS2023/INFORME_ANUAL_2023.pdf.
Spanish Ministry of Health; 2010–2023. Specialized care information system (SIAE) (accessed 14 Jan 2025); https://pestadistico.inteligenciadegestion.sanidad.gob.es/publicoSNS/C/siae/siae/hospitales/personal-y-formacion/areas-profesionales-y-especialidades.
Fisk, M. et al. Inaccurate diagnosis of COPD: The Welsh national COPD audit. Br. J. Gen. Pract. 69, E1–E7 (2019).
Josephs, L., Culliford, D., Johnson, M. & Thomas, M. COPD overdiagnosis in primary care: a UK observational study of consistency of airflow obstruction. NPJ Prim. Care Respir. Med. 29, 33 (2019).
Perret, J. et al. Undiagnosed and ‘overdiagnosed’ COPD using postbronchodilator spirometry in primary healthcare settings: a systematic review and meta-analysis. BMJ Open. Respir. Res. 10, 1–16 (2023).
Soriano, J. B. et al. Prevalence and determinants of COPD in Spain: EPISCAN II. Arch. Bronconeumol. 57, 61–69 (2021).
Ragaišiene, G. et al. Diagnosing COPD in primary care: what has real life practice got to do with guidelines? Multidiscip. Respir. Med. 14, 28 (2019).
Diab, N. et al. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 198, 1130–1139 (2018).
Bestall, J. C. et al. Usefulness of the medical research council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 54, 581–586 (1999).
Monterde, D., Vela, E. & Clèries, M. Adjusted morbidity groups: a new multiple morbidity measurement of use in primary care. Aten. Primaria 48, 674–682 (2016).
R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2024.
Gupta, S., Goodridge, D., Pakhalé, S., McIntyre, K. & Pendharkar, S. R. Choosing wisely: the canadian thoracic society’s list of six things that physicians and patients should question. Can. J. Respir. Crit. Care Sleep. Med. 1, 54–61 (2017).
Yamada, J. et al. Barriers and enablers to objective testing for asthma and COPD in primary care: a systematic review using the theoretical domains framework. Chest 161, 888–905 (2022).
Savic-Pesic, D. et al. Validity of the espiro mobile application in the interpretation of spirometric patterns: an app accuracy study. Diagnostics 14, 29 (2023).
Martín-Luján, F. et al. Effectiveness of the spirometry-based motivational intervention to quit smoking: RESET randomised trial. Eur. J. Gen. Pract. 29, 2276764 (2023).
Clair, C. et al. Biomedical risk assessment as an aid for smoking cessation. Cochrane Database Syst. Rev. 3, CD004705 (2019).
Agustí, A. et al. The many faces of COPD in real life: a longitudinal analysis of the NOVELTY cohort. ERJ Open. Res. 10, 00895–02023 (2024).
Cosío, B. G. et al. Unravelling young COPD and pre-COPD in the general population. ERJ Open. Res. 9, 00334–02022 (2023).
Garrastazu, R. et al. Prevalence of influenza vaccination in chronic obstructive pulmonary disease patients and impact on the risk of severe exacerbations. Arch. Bronconeumol. 52, 88–95 (2016).
Schrijver, J. et al. Self-management interventions for people with chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 1, CD002990 (2022).
World Health Organization. Continuity and coordination of care: a practice brief to support implementation of the WHO Framework on integrated people-centred health services. Geneva: World Health Organization; 2018.
Acknowledgements
The Instituto de Salud Carlos III (ISCIII) funded this study through the PMP21/00090 project, which was co-funded by the European Union’s Resilience and Recovery Facility.
Author information
Authors and Affiliations
Contributions
L.G.P., M.V., and A.B.S. conceived and planned the study. LG.P. and M.V. extracted the data. L.G.P. conducted the formal analysis. L.G.P., M.V., and A.B.S. took the lead in writing the initial draft, and A.A. provided critical feedback. R.F. and A.A. provided the resources. L.G.P., M.V., A.B.S., R.F., A.A., and A.S.A. contributed to the interpretation of the results. L.G.P., M.V., A.B.S., R.F., A.A., A.S.A., and A.O. reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
A.A. reports consulting fees, lectures, and research grants from GSK, AZ, Chiesi, Menarini, Zambon, MSD, and Sanofi. All authors declare that the research was conducted without commercial or financial relationships that could cause a conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Vila, M., Sisó-Almirall, A., Ocaña, A. et al. Prevalence, diagnostic accuracy, and healthcare utilization patterns in patients with COPD in primary healthcare: a population-based study. npj Prim. Care Respir. Med. 35, 17 (2025). https://doi.org/10.1038/s41533-025-00419-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41533-025-00419-9
This article is cited by
-
Assessment of risk factors in the development of chronic obstructive pulmonary diseases in several districts of Albania
Discover Public Health (2026)