Abstract
Chronic Obstructive Pulmonary Disease (COPD) is a global health concern, primarily linked to cigarette smoking. The potential role of electronic cigarettes (e-cigarettes) in COPD development remains unclear. Despite growing popularity as a smoking alternative, evidence suggests e-cigarettes may have harmful respiratory effects. This systematic review and meta-analysis assess the relationship between e-cigarette use and odds of having COPD. A comprehensive search of Web of Science, Embase, and PubMed was conducted to identify observational studies that assessed the association between e-cigarette use and the risk of COPD, providing risk estimates (hazard ratios, risk ratios, or odds ratios) for current, former, and ever e-cigarette users. Random-effects meta-analysis was performed using R software (V 4.4), and heterogeneity was assessed with the I2 statistic. Sensitivity analyses were conducted to test the robustness of the findings. Publication bias was evaluated using Egger’s test and funnel plots. Seventeen studies (1087 records screened) were included. E-cigarette use was associated with significantly higher odds of COPD compared to non-use. The pooled odds ratios were 1.48 (95% CI: 1.36–1.61) for current users, 1.84 (95% CI: 1.51–2.23) for former users, and 1.79 (95% CI: 1.42–2.25) for ever users. Sensitivity analysis confirmed the robustness of the findings. E-cigarette use is associated with higher odds of having COPD. Public health efforts should consider raising awareness of the potential respiratory risks associated with e-cigarette use.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a debilitating respiratory condition marked by persistent lung inflammation and restricted airflow, progressively worsening over time and often leading to significant impairment1. With 391.9 million people impacted, it is one of the major causes of illness and mortality worldwide, placing a heavy strain on healthcare systems and general quality of life2. The prevalence of COPD, however, is not uniform across populations. The global prevalence of COPD varies by region and risk factor exposure. In the general population, COPD affects approximately 10–12% of adults over 40 years old, though prevalence increases significantly among high-risk groups, such as current and former smokers, as well as individuals with occupational or environmental exposures3. These variations highlight the importance of assessing emerging potential risk factors, including e-cigarette use, which may contribute to COPD risk beyond traditional smoking. COPD is a heterogeneous disease characterized by persistent respiratory symptoms and airflow limitation due to airway inflammation and lung tissue destruction. While chronic bronchitis (excessive mucus production and cough) and emphysema (alveolar damage leading to reduced gas exchange) are commonly described phenotypes, many patients exhibit features of both, reflecting a combined disease presentation rather than distinct subtypes4,5. The primary risk factor for COPD has traditionally been identified as cigarette smoking, which damages lung tissue over time through the inhalation of harmful chemicals6,7. However, COPD development is influenced by a range of additional risk factors beyond smoking. The cumulative exposure to smoking, often quantified in pack-years, significantly impacts risk, but non-smoking factors are increasingly recognized, especially in low- and middle-income countries. These include advanced age, a history of pulmonary tuberculosis, lower socioeconomic status, indoor biomass exposure from cooking or heating with wood or charcoal, and occupational exposure to dust, fumes, and chemicals8,9. Identifying these diverse risk factors is essential for understanding regional variations in COPD prevalence and for assessing the potential role of emerging exposures such as e-cigarette use. Although smoking rates have declined in many countries due to public health initiatives, some regions continue to experience stagnant or increasing rates. Consequently, focus has turned to other possible risk factors for respiratory illnesses, such as the rising use of e-cigarettes.
Over the past 20 years, e-cigarettes, which were first developed as a substitute for traditional tobacco use, have quickly become more and more popular10. These devices function by heating a liquid, typically composed of nicotine, flavourings, and various chemicals, to create an aerosol that the user inhales11. Unlike traditional cigarettes, e-cigarettes do not produce harmful tar or combustion products associated with conventional tobacco smoke12. As a result, e-cigarettes may lower the risk of certain smoking-related diseases, such as lung cancer and cardiovascular disease, when used as a complete substitute for smoking. However, despite this potential benefit, e-cigarettes are not without risks and may still contribute to respiratory diseases, including COPD. As a result, they have been marketed as a potentially safer alternative for smokers and as a tool for smoking cessation. Despite these claims, e-cigarette aerosols still contain substances that may harm the respiratory system, such as ultrafine particles, volatile organic compounds, and toxic chemicals that are known to irritate the airways13. Globally, it is estimated that around 35 million of adults are current e-cigarette users14. Concerns over vaping’s long-term effects on health, especially on the lungs and respiratory system, have grown as a result15,16.
As e-cigarette use has become more widespread, particularly among younger populations, research into their potential health risks has intensified. Recent studies have suggested a potential link between e-cigarette use and poor respiratory outcomes, including COPD. While some research has explored the role of e-cigarettes in COPD exacerbations17, our research focuses specifically on the risk of having COPD rather than disease progression. Additionally, previous studies have primarily investigated vaping-associated lung injury (EVALI), asthma, and lung carcinogenesis, with only a brief mention of COPD, highlighting the need for more COPD-specific research18. Although the exact mechanism by which e-cigarettes may cause COPD is yet unknown, it is thought that long-term exposure to the chemicals in e-cigarette aerosols may cause inflammation and lung tissue damage19, similar to the effects of traditional cigarette smoking. However, despite these concerns, the current evidence on the association between e-cigarette use and COPD is inconsistent. While some studies suggest that vaping may expose users to fewer toxic substances than traditional smoking, evidence indicates that e-cigarette aerosols still contain harmful chemicals, including formaldehyde and ultrafine particles, which can cause airway inflammation, oxidative stress, and lung tissue damage factors that contribute to respiratory disease progression, including COPD20. Additionally, e-cigarette aerosols contain other toxic chemicals such as acrolein, acetaldehyde, and reactive oxygen species, which have been linked to increased airway resistance, impaired lung function, and long-term respiratory health risks similar to cigarette smoking, potentially contributing to COPD development21. However, some studies argue that e-cigarettes may cause only mild, short-term respiratory irritation and do not provide strong evidence that vaping leads to serious lung diseases. Instead, they propose that e-cigarettes could be a less harmful alternative to smoking, while emphasizing the need for long-term studies to confirm their safety22.
Given the chronic and progressive nature of COPD, early identification of risk factors is crucial for prevention and management. Although e-cigarettes are commonly viewed as a less dangerous option to smoking, it is still unknown what their long-term effects will be, especially for those who have never smoked. This highlights the need for a thorough investigation into whether e-cigarette use could serve as a risk factor for having COPD or contribute to the progression of the disease.
To gather the present knowledge of the relationship between using e-cigarettes and the risk of getting COPD, a systematic review and meta-analysis are required. This review aimed to identify gaps in the existing literature and comprehensively examining the association between e-cigarette use and the risk of having COPD.
Methods
Study design
In order to gather and evaluate the literature on the association between e-cigarette use and the risk of having COPD, a systematic review and meta-analysis were carried out. The review compiled with the guidelines set by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)23 (Table S1). The protocol for this study was also registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42024600164).
Data sources and search strategy
We systematically searched PubMed, Embase, and Web of Science from database inception to February 15, 2024. No start date restrictions were applied, ensuring that all relevant studies available up to the search date were considered. The search strategy utilized a combination of free text terms related to (“E-cigarettes” OR “Electronic nicotine delivery systems” OR “Vaping”) AND (“Chronic Obstructive Pulmonary Disease” OR “Emphysema” OR “Bronchitis”). No language or type of article restriction was imposed in the search. The full search strategy, including all keywords and filters used, is presented in Table S2.
Eligibility criteria
The following criteria were required for studies to be included: (1) they investigated the association between e-cigarette use and the risk of COPD; (2) participants were 18 years of age or older, including current, former, or ever e-cigarette users, where ever e-cigarette users refers to individuals who have used e-cigarettes at least once in their life time; (3) studies providing quantitative risk estimates such as odds ratios (OR), risk ratios (RR), hazard ratios (HR), or sufficient data to calculate these metrics; (4) they were published in peer-reviewed journals. COPD diagnosis was accepted based on self-reports, physician-confirmed diagnoses, and pulmonary function testing (e.g., spirometry). While self-reported COPD diagnosis may introduce some variability, they were included to ensure a comprehensive analysis, given the limited number of available studies. The primary exposure of interest was e-cigarette use, with the outcome being the risk of COPD. Studies examining COPD exacerbations (worsening of pre-existing COPD) or disease progression were excluded, as our focus was on new COPD diagnoses rather than changes in severity. The exclusion criteria included case reports, conference abstracts, editorials, and review articles. Studies that focused solely on other respiratory conditions without specific data on COPD were excluded.
Study selection
To ascertain eligibility, two reviewers independently examined the abstracts and titles of every study that was retrieved. The same reviewers then obtained and reviewed full-text articles of studies identified as potentially relevant. Discussions or, if necessary, the involvement of a third reviewer were used to resolve any disputes over the inclusion of the study. To enhance efficiency and reduce manual errors, we used Nested-Knowledge, a semi-automated software designed for systematic reviews. This tool facilitated duplicate removal, study screening, tagging, and data extraction, improving workflow consistency. The use of semi-automated tools like Nested-Knowledge is becoming more common in systematic reviews due to their ability to streamline processes and enhance accuracy24,25,26. No additional software was used.
Data extraction and quality assessment
Data were gathered using a structured extraction form. The collected data included important study details such as author, year of publication, country of origin, sample size, study design, participant characteristics (e.g., age, gender), along with effect sizes and their corresponding 95% confidence intervals (CIs) and diagnostic criteria for the COPD. The data extraction procedure was carried out by two independent reviewers, and any disputes were settled by discussion or, if required, by consulting a third reviewer. The semi-automated Nested-Knowledge software’s “tagging” feature made the data extraction procedure much easier.
Utilizing the Newcastle-Ottawa Scale (NOS), two assessors independently assessed the listed studies’ quality. The studies were evaluated based on participant selection, study group comparability, and the technique for identifying the association between e-cigarette exposure and COPD outcomes (Table S3). All studies assessing ever e-cigarette users in this meta-analysis adjusted for age in their analyses, ensuring that the observed associations between ever e-cigarette use and COPD risk were independent of age-related effects.
Data synthesis and statistical analysis
Data analysis was conducted using R software version 4.4, to investigate the association between e-cigarette use and the onset of COPD. A random-effects meta-analysis was applied to account for variations across studies. The outcomes were presented as combined OR along with 95% CIs. While ORs were the primary summary measure used in the meta-analysis, some included studies also reported RR or HR. Although related, these measures differ in interpretation: ORs describe the odds of an outcome occurring, RRs indicate the relative probability, and HRs reflect the rate of occurrence over time.
Heterogeneity was assessed across the studies using the I2 statistic, with 25, 50, and 75% denoting low, moderate, and high heterogeneity, respectively27. The robustness of the findings was evaluated using a leave-one-out sensitivity analysis28. Additionally, two sensitivity analyses were conducted: one assessing the impact of including only studies with objective COPD diagnoses (e.g., spirometry) while excluding self-reported cases, and another including only studies with a NOS score ≥7 to evaluate the effect of study quality on the results. For every analysis, a p-value of less than 0.05 was considered statistically significant.
Results
Literature search
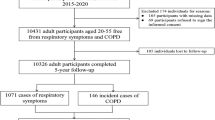
A total of 1087 entries were found through the database search, including 761 from Embase, 200 from PubMed and 126 from Web of Science. Only 808 distinct records left for screening after 279 duplicates were eliminated. This method left 54 full-text publications for in-depth evaluation after 754 records were eliminated because, according to their titles and abstracts, they did not match the inclusion requirements. After thorough analysis, 37 publications were not eligible for inclusion due to reasons such as being case reports7, review papers8, irrelevant6, and failure to address the outcomes of interest16. Finally, 1729,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45 study were chosen to be part of the systematic review (Fig. 1).
Characteristics of included studies
The included studies were conducted in the USA (15 studies), China (1 study), and South Korea (1 study), and consisted of 12 cross-sectional studies and 5 cohort studies (Table 1). The study populations ranged from general adult populations to specific subgroups, such as women of childbearing age and non-institutionalized civilians. Participants ages varied widely, from 18 years to over 50 years, with female representation ranging from 34–100%. Of the included studies, 15 relied on self-reported COPD diagnoses, while 02 used spirometry-based measures such as the FEV1/FVC ratio to confirm COPD. Effect sizes for current, former, and ever e-cigarette users were primarily reported as OR or HR or incidence rate ratios (IRR). Sample sizes varied considerably among the studies, ranging from smaller cohorts of approximately 8087 participants to large-scale studies with over 705,159 individuals.
Quality assessment of included studies
The included studies were assessed for quality using the NOS, with scores ranging from 5–9 for cohort studies and up to 6 for cross-sectional studies (Table S3). Studies with higher scores (≥8) demonstrated robust methodologies, including comprehensive follow-up, strong comparability adjustments, and adequate outcome assessments, making them less prone to bias and more reliable. In contrast, studies with lower scores (≤5) had limitations in selection representativeness, comparability, and follow-up adequacy, potentially introducing bias, particularly in those relying on self-reported COPD diagnosis rather than objective measures.
Association between current e-cigarettes users and risk of COPD
The meta-analysis demonstrated a statistically significant association between current e-cigarette use and the odds of having COPD, with a pooled OR of 1.473 (95% CI: 1.260–1.723). Compared to never users, current e-cigarette users had 47.3% greater odds of having COPD. Low heterogeneity (I2 = 0%) among the selected studies suggests that the findings were consistent across the included datasets. Our meta-analysis supports a positive association between e-cigarette use and the odds of having COPD (Fig. 2).
Association between former e-cigarettes users and risk of COPD
The meta-analysis found a significant association between former e-cigarette use and odds of COPD, with a pooled OR of 1.766 (95% CI: 1.418–2.200). According to this, those who have ever used e-cigarettes have 76.6% greater odds of having COPD than people who have never used them. There was some variation in the outcomes among the included research, as seen by the moderate to high heterogeneity among the studies (I2 = 55.7%). The pooled effect estimates are shown in Fig. 3.
Association between ever e-cigarettes users and risk of COPD
The meta-analysis found a substantial association between the odds of having COPD and ever using e-cigarettes, with a pooled OR of 1.388 (95% CI: 1.070–2.458). The findings suggest that compared to those who have never used e-cigarettes, those who have ever used them have 38.8% greater odds of having COPD. The absence of heterogeneity among studies (I2 = 0%) indicates that the findings were highly consistent across all included studies. Ever using e-cigarettes is positively associated with the risk of COPD, according to the pooled effect estimates in Fig. 4.
Subgroup analysis of association between current e-cigarettes users and risk of COPD
Subgroup analyses were performed based on study design (cross-sectional and cohort) to explore potential sources of heterogeneity in the association between current e-cigarette use and the odds of having COPD. The pooled OR for cross-sectional studies was 1.592 (95% CI: 1.349–1.879), indicating a statistically significant association. In contrast, the pooled OR for cohort studies was 1.145 (95% CI: 0.842–1.557), and the confidence interval included 1, suggesting that the association was not statistically significant in longitudinal data. Heterogeneity was absent across both subgroups (I2 = 0%), and the test for subgroup differences was not statistically significant (p = 0.0642), indicating no substantial variation between study designs (Fig. 5).
Sensitivity analysis
A leave-one-out sensitivity analysis was conducted to evaluate the robustness of pooled estimates for current, former, and ever e-cigarette users. For current users, pooled ORs ranged from 1.441–1.532, for former users from 1.460–3.000, and for ever users from 1.430–2.330. In all cases, excluding any single study did not significantly change the overall effect size, confirming the stability of the correlation between e-cigarette use (in all groups) and odds of having COPD (Figs. 6–8). Additionally, a sensitivity analysis including only studies with spirometry-based COPD diagnoses yielded a pooled OR of 1.14 (95% CI: 0.82–1.58) (Fig. S1), which was not statistically significant. Furthermore, a sensitivity analysis including only studies with a NOS score ≥7 was conducted for current and former e-cigarette users. For current users, the pooled OR was 1.56 (95% CI: 1.07–2.25), with moderate heterogeneity (I2 = 42%) (Fig. S2). For former users, the pooled OR was 2.57 (95% CI: 1.91–3.46), with low heterogeneity (I2 = 0%) (Fig. S3).
Publication bias
Using an Egger’s test and a funnel plot, publication bias was evaluated. Visual examination of the funnel plot (Fig. 9) revealed no discernible asymmetry, indicating that considerable publication bias is unlikely in the studies evaluating the association between the greater odds of having COPD and current e-cigarette use. With a p-value of 0.1449, Egger’s test further confirmed this conclusion, indicating that small-study effects are unlikely to have affected the findings.
Discussion
The results from this systematic review and meta-analysis suggest an association between e-cigarette use and greater odds of having COPD. Specifically, the pooled ORs for current, former, and ever e-cigarette users were 1.473 (95% CI: 1.260–1.723), 1.766 (95% CI: 1.418–2.200), and 1.388 (95% CI: 1.070–2.458), respectively, indicating that individuals who use or have used e-cigarettes face significantly greater odds of having COPD. The odds were particularly notable for former users (76.6% greater odds), followed by current users (47.3% greater odds) and ever users (38.8% greater odds). Given that COPD already affects a notable portion of the adult population, even moderate increases in risk among e-cigarette users may carry important public health implications. Additionally, a prospective cohort study reported a HR of 1.17 (95% CI: 0.83–1.66), while a separate cohort study identified an IRR of 1.57 (95% CI: 1.15–2.13), further supporting the association between e-cigarette use and COPD risk. Moreover, a longitudinal cohort study found a RR of 1.36 (95% CI: 0.55–3.39) for current e-cigarette users, further corroborating the link between vaping and COPD risk. The low heterogeneity observed in studies on current users (I2 = 0%) suggests consistent results, while the moderate heterogeneity for former and ever users emphasizes the need for further research to explore the complexities of e-cigarette exposure and its role in COPD development.
The meta-analysis revealed that current e-cigarette users had 47.3% higher odds of having COPD compared to non-users. This estimate, derived from 17 studies with a total sample size of over 4.3 million participants, suggests a significant association between e-cigarette use and greater odds of having COPD. However, since most of the included studies did not report the duration of e-cigarette use, these findings should not be interpreted as evidence of long-term risk.
A sensitivity analysis limited to spirometry-based COPD diagnoses did not yield statistically significant results, suggesting that self-reported diagnoses may have influenced the overall association. These findings emphasize the need for high-quality studies using objective diagnostic measures to better assess the link between e-cigarette use and the odds of having COPD. Previous research has consistently shown that traditional smoking is a major risk factor for COPD31, but these findings suggest that e-cigarettes may also pose serious risks to respiratory health. This elevated risk among e-cigarette users is in line with earlier studies that recognized the harmful effects of vaping on lung function and inflammation, even in individuals who have never smoked traditional cigarettes46.
While our study focused on the association between e-cigarette use and odds of having COPD, previous research has well established that traditional cigarette smoking is a major risk factor for COPD. A systematic review and meta-analysis found that ever smokers had an OR of 2.89 (95% CI: 2.63–3.17), and current smokers had an OR of 3.51 (95% CI: 3.08–3.99) for COPD risk, compared to non-smokers47. Similarly, prior48 reported that persistent smokers had a significantly higher 10-year cumulative incidence of COPD compared to nonsmokers, with an OR of 5.37 (95% CI: 2.75–10.48) using BTS criteria and OR of 4.56 (95% CI: 2.58–8.07) using GOLD criteria. In contrast, the pooled OR for current e-cigarette users in our meta-analysis was 1.485 (95% CI: 1.364–1.617), suggesting that while the relative risk of COPD is lower in e-cigarette users compared to smokers, the risk remains significant. Although e-cigarettes expose users to fewer toxic combustion products than cigarettes, they still contain harmful chemicals that contribute to airway inflammation, oxidative stress, and lung function decline all of which are key mechanisms in COPD development. Given these findings, while e-cigarettes may pose a lower relative risk of COPD than traditional smoking, they are not risk-free, and their long-term effects remain uncertain49. More direct comparative studies are needed to assess the relative risk of e-cigarette use vs. smoking in COPD development. While e-cigarettes may expose users to fewer toxic combustion products than traditional cigarettes, their role in smoking cessation remains debated. Public health guidelines suggest that e-cigarettes may serve as a harm reduction tool for smokers who are unable to quit using conventional cessation methods. However, the long-term health effects of e-cigarette use remain uncertain, and their impact on COPD risk warrants further investigation50. Future research should focus on evaluating the effectiveness of e-cigarettes in smoking cessation and their potential consequences for respiratory health.
The meta-analysis also demonstrated greater odds of having COPD among former e-cigarette users, suggesting that these findings have negative impact of e-cigarette use on lung health may persist even after cessation, raising concerns about the long-term consequences of vaping51. Given that ever-users who may have only used e-cigarettes occasionally also show an increased risk, the results highlight the potential for even intermittent exposure to harmful aerosols and chemicals to contribute to COPD50. One possible concern is whether this increased risk is due to older age among ever users, as COPD is a progressive disease that develops over time. However, all studies included in our meta-analysis that assessed ever e-cigarette users adjusted for age, ensuring that the observed association is independent of age-related effects. This strengthens the validity of our findings and suggests that the increased odds of COPD among ever e-cigarette users is not merely a result of aging but may be directly linked to vaping history. This aligns with rising evidence points to e-cigarettes being more harmful than previously thought, particularly concerning long-term respiratory health52.
In comparison to previous meta-analyses, our study provides important insights into the association between e-cigarette usage and the odds of COPD. Earlier analyses reported that traditional cigarette smokers have a significantly higher risk of having COPD53, our findings suggest an elevated odds associated with current e-cigarette use, although the magnitude of this association appears lower compared to that observed for traditional smoking. This highlights the growing concerns about the long-term respiratory health effects of e-cigarettes, especially as their usage increases among younger populations. Although e-cigarettes may seem like a safer alternative to traditional smoking, they still pose significant health risks, emphasizing the need for further research and public health initiatives to address these issues.
The substantial heterogeneity observed in studies of former (I2 = 70%) and ever e-cigarette users (I2 = 46%) reflects variations in study populations, definitions of e-cigarette use, and diagnostic criteria for COPD. Current e-cigarette users also exhibited considerable variability, contributing to the complexity of the findings. Differences in exposure duration, intensity of use, and the presence of co-existing respiratory conditions could further influence the variability in results. Comorbid conditions such as asthma or previous smoking habits may compound the likelihood of COPD among e-cigarette users, although these factors were not consistently controlled for across studies54. According to the subgroup analysis, current e-cigarette users had significantly higher odds of COPD compared to non-users, with a pooled OR of 1.473 (95% CI: 1.260–1.723). Compared to cross-sectional studies, which indicated a pooled OR of 1.592 (95% CI: 1.349–1.879), cohort studies showed a reduced pooled OR of 1.145 (95% CI: 0.842–1.557). The p-value of 0.06 suggests that the methodological techniques employed may have an effect on the association between e-cigarette use and odds of having COPD, even though the changes between research designs may not be statistically significant. This highlights the need for more study to ascertain how personal and environmental variables affect how using e-cigarettes affects lung health. Importantly, the funnel plot and Egger’s test results revealed no obvious publication bias, ensuring the validity of the findings.
The overall quality of the included studies varied. Most studies received moderate to high scores on the NOS, indicating reliable methodological rigor. Studies that utilized spirometry-based COPD diagnoses were generally more robust than those relying on self-reported diagnoses, which may introduce misclassification bias. Additionally, while several studies included large, population-based samples, others were limited by cross-sectional designs, restricting causal inference. To further evaluate the impact of study quality, a sensitivity analysis including only studies with a NOS score ≥7 was conducted. The results remained consistent for both current and former e-cigarette users, indicating that the association between e-cigarette use and COPD risk remains significant even when limited to high-quality studies, reinforcing the robustness of our conclusions. However, future research should prioritize longitudinal designs with objective diagnostic measures to strengthen causal assessments of the association between e-cigarette use and COPD risk.
Several mechanisms have been proposed to explain the increased odds of COPD in e-cigarette users. A key factor is the presence of harmful chemicals in e-cigarette aerosols, such as ultrafine particles, volatile organic compounds, and toxic metals13. Chronic inhalation of these substances can lead to inflammation and damage to lung tissue, mirroring the pathophysiological processes seen in traditional cigarette smokers55,56. In addition, nicotine itself, while not a direct carcinogen, has been shown to promote oxidative stress and inflammation, which can contribute to respiratory dysfunction and airway remodelling57. These processes are key contributors to the development and progression of COPD.
The results of this meta-analysis carry significant clinical implications. First, they emphasize the need for healthcare professionals to be vigilant in monitoring the respiratory health of individuals who use or have used e-cigarettes, particularly given the heightened odds of COPD associated with e-cigarette use. Incorporating routine lung function assessments into clinical care for e-cigarette users could aid in the early detection and prevention of COPD. Clinicians should approach the recommendation of e-cigarettes for smoking cessation with caution and ensure these products are not initiated by individuals without a prior history of smoking. While our findings suggest respiratory risks associated with e-cigarette use, it is important to acknowledge that e-cigarettes generally reduce exposure to many of the carcinogens and cardiovascular toxins found in combustible cigarettes. Therefore, Public education initiatives should communicate that e-cigarette use is not without health risks. While some evidence suggests that the harms may be lower than those associated with combustible tobacco products, e-cigarettes are not risk-free — particularly with respect to respiratory health.
Despite offering insightful information about the relationship between e-cigarette usage and the risk of COPD, this meta-analysis has a number of limitations that should be noted. The included studies varied considerably in their design, and while random-effects models were used to account for this heterogeneity, significant moderating factors such as differences in e-cigarette products, usage patterns, and population characteristics remain unexplored. Most studies relied on self-reported diagnoses, which may introduce bias and affect the accuracy of the findings. Additionally, limited data were available on the duration of e-cigarette use (time of exposure) and dose-response relationships (e.g., daily vs. occasional use, nicotine concentration), making it difficult to assess the cumulative effects of vaping on COPD risk. Given that age is associated with both COPD risk and e-cigarette use, it may act as a collider variable. Adjustment for age alone may not fully address this complexity, and the lack of individual-level data limited our ability to explore these interactions. Another important limitation involves the smoking history of participants. Many included studies did not clearly differentiate between never smokers and former smokers among e-cigarette users. Additionally, dual-use (the simultaneous use of both e-cigarettes and combustible cigarettes) was not consistently addressed. Dual-use may increase cumulative exposure to inhaled toxicants, complicating the interpretation of the independent association between e-cigarette use and COPD risk. As a result, the observed relationship might partially reflect the effects of prior or concurrent smoking rather than vaping alone. Furthermore, all the studies included in this meta-analysis were conducted in the United States, South Korea, and China, which would restrict the findings’ generalizability to other areas with different e-cigarette usage patterns and healthcare systems58. Additionally, limited data were available on the duration of e-cigarette use (time of exposure) and dose-response relationships (e.g., daily vs. occasional use, nicotine concentration), making it difficult to assess the cumulative effects of vaping on COPD risk. Most included studies categorized participants simply as ‘current’, ‘former’, or ‘never’ users, without considering the intensity or duration of use. As a result, potential dose-response effects could not be evaluated, possibly obscuring important exposure-risk relationships. Although most studies attempted to adjust for major confounders, the possibility of residual confounding remains. Inconsistencies in confounder adjustment across studies could bias the pooled estimates, limiting the causal interpretation of the findings. Subsequent studies ought to concentrate on examining the effects of characteristics including the length and severity of e-cigarette use, the existence of underlying respiratory disorders, and concurrent exposure to other risk factors such environmental contaminants59. It is important to note that, due to the observational design of most included studies, causal relationships between e-cigarette use and COPD cannot be established. In order to determine the temporal association between e-cigarette use and the development of COPD and to identify potential causative pathways, longitudinal studies are very important. To provide a more thorough knowledge of the worldwide effects of vaping on respiratory health, research must be expanded to incorporate studies from other cultural and geographic contexts.
Conclusion
This meta-analysis found a statistically significant increased odds of having COPD in current, former, and ever e-cigarette users. These findings emphasize the need for healthcare professionals to monitor respiratory health in e-cigarette users, particularly those with pre-existing conditions. Additionally, public health initiatives are essential to raise awareness about the respiratory hazards of e-cigarette use and to promote safer consumption practices, ultimately improving respiratory health outcomes.
Data availability
The data is with the authors and available on request.
References
Schwalk, A. J., Patel, N. M. & Madisi, N. Y. Developing interventions for chronic obstructive pulmonary disease. Semin. Respir. Crit. Care Med. 45, 582–592 (2024).
Adeloye, D. et al. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir. Med. 10, 447–458 (2022).
Goel, S., Shabil, M., Kaur, J., Chauhan, A. & Rinkoo, A. V. Safety, efficacy and health impact of electronic nicotine delivery systems (ENDS): an umbrella review protocol. BMJ Open. 14, e080274 (2024).
Sharma, S., Rai, G., Devtalla, H., Gauba, P. & Dang, S. Combating chronic obstructive pulmonary disease (COPD) using nanocarriers. Nanocarrier Drug Delivery Systems: Therapeutic Diagnostic Med. 57, https://www.degruyterbrill.com/document/doi/10.1515/9783111320847-003/pdf?licenseType=restricted (2024).
Kim, W.-D. Phenotype of chronic obstructive pulmonary disease based on computed tomography–defined underlying pathology. Tuberc. Respir. Dis. 85, 302 (2022).
Wei, K., Zhang, X., Yang, J. & Chen, J. Tobacco introduced Perilla frutescens and Ocimum basilicum genes attenuates neutrophilic inflammation in lung tissues of COPD rats. Ecotoxicol. Env. Saf. 271, 115956 (2024).
Zhang, Y. et al. Effects of web-based acceptance and commitment therapy on health-related outcomes among patients with lung cancer: a feasibility randomized controlled trial. PsychoOncol 33, e70045 (2024).
Makanza, E. Risk factors for chronic obstructive pulmonary disease among patients visiting chris hani baragwanath academic hospital, medical outpatient department, 2015–2020 (University of Johannesburg, South Africa, 2021).
Woolley, K. E. et al. Investigating the association between wood and charcoal domestic cooking, respiratory symptoms and acute respiratory infections among children aged under 5 years in Uganda: a cross-sectional analysis of the 2016 demographic and health survey. Int. J. Env. Res. Public. Health 17, 3974 (2020).
Tahniyath, U., Begum, S. S. & Unnisa, M. Vaping trends among adoloscents: understanding the rise of E cigarettes in youth culture. J. Adv. Med. Pharm. Sci. 26, 48–63 (2024).
Reilly, S. M., Cheng, T., Feng, C. & Walters, M. J. Harmful and potentially harmful constituents in e-liquids and aerosols from electronic nicotine delivery systems (ENDS). Chem. Res. Toxicol. 37, 1155–1170 (2024).
Berenguer, C., Pereira, J. A. & Câmara, J. S. Fingerprinting the volatile profile of traditional tobacco and e-cigarettes: a comparative study. Microchem. J. 166, 106196 (2021).
Marques, P., Piqueras, L. & Sanz, M.-J. An updated overview of e-cigarette impact on human health. Respir. Res. 22, 151 (2021).
Besaratinia, A. & Tommasi, S. Vaping: a growing global health concern. EClinicalMedicine 17, 100208 (2019).
Awad, A. A. et al. Association of electronic cigarette use and suicidal behaviors: a systematic review and meta-analysis. BMC Psychiatry 24, 608 (2024).
Shabil, M. et al. The impact of electronic cigarette use on periodontitis and periodontal outcomes: a systematic review and meta-analysis. BMC Oral. Health 24, 1197 (2024).
Polosa, R. et al. COPD smokers who switched to e-cigarettes: health outcomes at 5-year follow up. Ther. Adv. Chronic Dis. 11, 2040622320961617 (2020).
Petrella, F. et al. Clinical impact of vaping on cardiopulmonary function and lung cancer development: an update. Eur. J. Cancer Prev. 32, 584–589 (2023).
Ali, N., Xavier, J., Engur, M., Pv, M. & Bernardino de la Serna, J. The impact of e-cigarette exposure on different organ systems: A review of recent evidence and future perspectives. J. Hazard. Mater. 457, 131828 (2023).
Sapru, S. et al. E-cigarettes use in the United States: reasons for use, perceptions, and effects on health. BMC Public. Health 20, 1–10 (2020).
Darabseh, M. Z., Selfe, J., Morse, C. I. & Degens, H. Is vaping better than smoking for cardiorespiratory and muscle function?. Multidiscip. Respir. Med. 15, 674 (2020).
Polosa, R., Rodu, B., Caponnetto, P., Maglia, M. & Raciti, C. A fresh look at tobacco harm reduction: the case for the electronic cigarette. Harm Reduct. J. 10, 19 (2013).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71 (2021).
Sharma, N. et al. Association of celiac disease and myocardial infarction: a systematic review and meta-analysis. BMC Cardiovasc. Disord. 24, 655 (2024).
Malvi, A. et al. Cannabis consumption and risk of asthma: a systematic review and meta-analysis. BMC Pulm. Med. 25, 1–11 (2025).
Tiwari, S. et al. Prevalence of dengue and leptospirosis coinfection and associated mortality rates: a systematic review and meta-analysis. BMC Infect. Dis. 25, 111 (2025).
Shabil, M., Bushi, G. & Khatib, M. N. A commentary on “Psychological health among healthcare professionals during COVID-19 pandemic: an updated meta-analysis. Indian. J. Psychiatry 66, 763–764 (2024).
Meng, Z., Wang, J., Lin, L. & Wu, C. Sensitivity analysis with iterative outlier detection for systematic reviews and meta-analyses. Stat. Med. 43, 1549–1563 (2024).
Wills, T. A., Choi, K., Pokhrel, P. & Pagano, I. Tests for confounding with cigarette smoking in the association of E-cigarette use with respiratory disorder: 2020 national-sample data. Prev. Med. 161, 107137 (2022).
Barrameda, R. et al. Use of e-cigarettes and self-reported lung disease among US adults. Public. Health Rep. 135, 785–795 (2020).
Bircan, E., Bezirhan, U., Porter, A., Fagan, P. & Orloff, M. S. Electronic cigarette use and its association with asthma, chronic obstructive pulmonary disease (COPD) and asthma-COPD overlap syndrome among never cigarette smokers. Tob. Induc. Dis. 19, 75 (2021).
Cook, S. F. et al. Cigarettes, ENDS Use, and Chronic Obstructive Pulmonary Disease incidence: a prospective longitudinal study. Am. J. Prev. Med. 65, 173–181 (2023).
Cordova, J. et al. Tobacco use profiles by respiratory disorder status for adults in the wave 1-wave 4 population assessment of tobacco and health (PATH) study. Prev. Med. Rep. 30, 102016 (2022).
Osei, A. D. et al. Association between e-cigarette use and chronic obstructive pulmonary disease by smoking status: behavioral risk factor surveillance system 2016 and 2017. Am. J. Prev. Med. 58, 336–342 (2020).
Goldberg Scott, S. et al. Demographic, clinical, and behavioral factors associated with electronic nicotine delivery systems use in a large cohort in the united states. Tob. Use Insights 16, 1179173X221134855 (2023).
Paulin, L. M. et al. Association of tobacco product use with chronic obstructive pulmonary disease (COPD) prevalence and incidence in Waves 1 through 5 (2013–2019) of the Population Assessment of Tobacco and Health (PATH) study. Respir. Res. 23, 273 (2022).
Bhatta, D. N. & Glantz, S. A. Association of e-cigarette use with respiratory disease among adults: a longitudinal analysis. Am. J. Prev. Med. 58, 182–190 (2020).
Antwi, G. O. & Rhodes, D. L. Association between E-cigarette use and chronic obstructive pulmonary disease in non-asthmatic adults in the USA. J. Public. Health 44, 158–164 (2022).
Parekh, T., Owens, C., Fay, K., Phillips, J. & Kitsantas, P. Use of e-cigarettes and development of respiratory conditions in women of childbearing age. South. Med. J. 113, 488–494 (2020).
Perez, M. F., Atuegwu, N. C., Mead, E. L., Oncken, C. & Mortensen, E. M. Adult e-cigarettes use associated with a self-reported diagnosis of COPD. Int. J. Env. Res. Public. Health 16, 3938 (2019).
Song, B., Li, H., Zhang, H., Jiao, L. & Wu, S. Impact of electronic cigarette usage on the onset of respiratory symptoms and COPD among Chinese adults. Sci. Rep. 14, 5598 (2024).
Wills, T. A., Pagano, I., Williams, R. J. & Tam, E. K. E-cigarette use and respiratory disorder in an adult sample. Drug. Alcohol. Depend. 194, 363–370 (2019).
Xie, Z., Ossip, D. J., Rahman, I. & Li, D. Use of electronic cigarettes and self-reported chronic obstructive pulmonary disease diagnosis in adults. Nicotine Tob. Res. 22, 1155–1161 (2020).
Xie, W. et al. Association of electronic cigarette use with incident respiratory conditions among US adults from 2013 to 2018. JAMA Netw. Open. 3, e2020816 (2020).
Kim, C. Y. et al. Factors associated with electronic cigarette use and pulmonary function outcomes: a cross-sectional analysis of Korean National Health and Nutrition Examination Survey Data from 2013 to 2019. https://www.researchsquare.com/article/rs-4352866/v1 (2024).
Keith, R. & Bhatnagar, A. Cardiorespiratory and immunologic effects of electronic cigarettes. Curr. Addict. Rep. 8, 336–346 (2021).
Forey, B. A., Thornton, A. J. & Lee, P. N. Systematic review with meta-analysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema. BMC Pulm. Med. 11, 1–61 (2011).
Lindberg, A. et al. Ten-year cumulative incidence of COPD and risk factors for incident disease in a symptomatic cohort. Chest 127, 1544–1552 (2005).
Liu, B. et al. Developing a new sepsis screening tool based on lymphocyte count, international normalized ratio and procalcitonin (LIP score). Sci. Rep. 12, 20002 (2022).
Fang, M., Xia, Z., Rong, X. & Xiao, J. The association of smoking on the increased risk of osteoporotic fracture: results from a cross-sectional study and two-sample Mendelian randomization. Tob. Induc. Dis. 22. https://doi.org/10.18332/tid/189485 (2024).
Davis, L. C., Sapey, E., Thickett, D. R. & Scott, A. Predicting the pulmonary effects of long-term e-cigarette use: are the clouds clearing?. Eur. Respir. Rev. 31, 210121 (2022).
Wang, L., Wang, Y., Chen, J., Liu, P. & Li, M. A review of toxicity mechanism studies of electronic cigarettes on respiratory system. Int. J. Mol. Sci. 23, 5030 (2022).
Glantz, S. A., Nguyen, N. & Oliveira da Silva, A. L. Population-based disease odds for e-cigarettes and dual use versus cigarettes. NEJM Evid. 3, EVIDoa2300229 (2024).
Liu, R., Wang, S., Tian, F. & Yi, L. SIR-3DCNN: a framework of multivariate time series classification for lung cancer detection. IEEE Trans. Instrum. Meas. 74, https://doi.org/10.1109/TIM.2025.3563000 (2025).
Tsai, M., Byun, M. K., Shin, J. & Crotty Alexander, L. E. Effects of e-cigarettes and vaping devices on cardiac and pulmonary physiology. J. Physiol. 598, 5039–5062 (2020).
Huang, C. et al. Causal associations of self-reported walking pace with respiratory diseases: a mendelian randomization analysis. Medicine 104, e41746 (2025).
Li, L., Yang, D. C. & Chen, C.-H. Metabolic reprogramming: a driver of cigarette smoke-induced inflammatory lung diseases. Free. Radic. Biol. Med. 163, 392–401 (2021).
Liu, T. et al. Relationship between vascular aging and left ventricular geometry in patients with obstructive sleep apnea hypopnea syndrome-related hypertension. Sci. Rep. 15, 6191 (2025).
Chen, Z. et al. Geriatric nutritional risk index as a predictor of mortality in women with chronic inflammatory airway disease: evidence from NHANES 1999–2018. Front. Nutr. 12, 1547952 (2025).
Acknowledgements
The authors acknowledge the Nested-Knowledge, MN, USA for providing the access to the software.
Author information
Authors and Affiliations
Contributions
Muhammed Shabil: Conceptualization, Methodology, Writing - Original Draft, Project Administration. Ajay Malvi: Conceptualization, Methodology, Writing - Original Draft. Mahalaqua Nazli Khatib: Data Curation, Writing - Review & Editing. Subbulakshmi Ganesan: Formal Analysis, Investigation. Mandeep Kaur: Resources, Data Curation. Manish Srivastava: Supervision, Project Administration. G. V. Siva Prasad: Methodology, Validation. Pranchal Rajput: Software, Formal Analysis. Brijendra Mohan: Validation, Writing - Review & Editing. Diptismitha Jena: Investigation, Writing - Original Draft. Ganesh Bushi: Visualization, Supervision. Sanjit Sah: Data Curation, Methodology. Prakasini Satapathya: Conceptualization, Supervision. Shailesh Kumar Samal: Formal Analysis, Investigation. Edward Mawejje: Writing - Review & Editing, Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shabil, M., Malvi, A., Khatib, M.N. et al. Association of electronic cigarette use and risk of COPD: a systematic review and meta-analysis. npj Prim. Care Respir. Med. 35, 31 (2025). https://doi.org/10.1038/s41533-025-00438-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41533-025-00438-6
This article is cited by
-
Reassessing the link between e-cigarette use and COPD: addressing critical methodological and conceptual flaws
npj Primary Care Respiratory Medicine (2025)