Abstract
The Positive and Negative Syndrome Scale (PANSS) is the most widely used rating scale to assess psychotic symptoms in patients with schizophrenia and other primary psychoses. However, a definitive consensus regarding its dimensional structure remains elusive. The present work aims to determine the number of dimensions of the scale through a network analysis approach in a sample of individuals experiencing first-episode schizophrenia spectrum disorder (FE-SSD) with minimal or no prior exposure to antipsychotic treatment. Baseline data of 446 participants (age 25.96 ± 5.99 years, 70% males) enrolled in the OPTiMiSE trial were analysed. Exploratory Graph Analysis (EGA) was conducted to evaluate the dimensionality of the PANSS, and a bootstrap approach (bootEGA) was employed to assess model stability. The analysis was replicated, excluding unstable items with stability values below 0.75, until a stable model was achieved. The analysis of the 30 items of the PANSS revealed inadequate structural consistency, resulting in the exclusion of 9 unstable items. The final model comprised 21 symptoms distributed across four communities (Positive, Cognitive/Disorganised, Excited/Aggressive and Negative) but lacked a depressive domain. In conclusion, we propose a concise version of the PANSS, incorporating 21 items, to better assess the core symptoms of the first episode of SSD. This revised version provides clinicians with a robust psychometric tool with reduced administration time, but the complementary administration of a dedicated instrument for evaluating affective symptoms is advisable.
Similar content being viewed by others
Introduction
Primary psychoses are multifaceted conditions characterised by heterogeneous clinical entities1. Response to treatment and clinical course vary2, with schizophrenia spectrum disorders (SSD), including schizophrenia, schizophreniform disorder, or schizoaffective disorder and generally associated with less favourable outcomes3. SSD symptoms include delusions and hallucinations, but also other features like disorganised thinking, abnormal motor behaviour and negative symptoms1. None of these is pathognomonic and their severity can fluctuate among patients or in different phases of the illness, making it challenging to establish an unequivocal definition of the psychopathological domains of SSD. Historically, latent variable modelling approaches, such as factor analysis of psychometric instruments, have been employed to elucidate the structure of these symptoms4. However, the traditional descriptive and categorical approach has proven insufficient5, encouraging a paradigm shift towards a more dimensional conceptualisation of psychopathology that prioritises the diverse experiences and needs of individuals with psychosis across the illness trajectory6,7.
The Positive and Negative Syndrome Scale (PANSS)8 is the most widely used rating scale to assess psychotic symptoms in patients with schizophrenia and other psychoses, and it is considered the gold standard for randomised controlled trials (RCT). The initial model of the PANSS, consisting of 30 items, encompasses three distinct subscales: Positive (7 items), Negative (7 items) and General (16 items). Given the number and variety of symptoms included in the scale, numerous factor analytic solutions have been published since then. Most authors generally supported the presence of five different symptom dimensions: Positive, Negative, Cognitive (or Disorganised), Depressive (or Emotional) and Excitement (or Hostility). However, alternative solutions ranging from four to eight factors have also been proposed9. Still, most studies varied in how they assigned individual items to specific dimensions10 and very few models held acceptable fits11 when following conventional cutoff criteria12, leaving several questions unanswered. This could be attributed to diverse reasons, including methodological discrepancies (e.g., the estimation method chosen for factorial analysis) or the heterogeneity of the patients enrolled. Moreover, certain assumptions and methodological challenges associated with factorial techniques may pose concerns13. For example, confirmatory factor analysis (CFA), commonly used to assess the adequacy of latent models, assumes that each item loads exclusively onto one factor. This assumption may be problematic when applied to the PANSS, as schizophrenia symptoms often exhibit complex relationships with multiple psychopathological constructs11.
Considering the increasing interest in clinical staging models of schizophrenia14, the first episode of schizophrenia spectrum disorder (FE-SSD) provides a valuable opportunity to characterise its nuclear features while still unaffected by long-term treatment or chronic disease factors. However, the relatively poor statistical fit of previous factorial PANSS models observed in first-episode psychosis (FEP) suggests that a dimensional structure, rather than a categorical one, might be more appropriate for effectively describing psychopathology in these patients10.
In recent years, network analysis has emerged as a novel theoretical and statistical approach to improve the understanding of mental disorders, integrating various techniques from complex systems science into psychiatric research4. This framework offers a distinctive set of tools to explore the complexity of psychopathology and has been increasingly applied to psychosis research in both first-episode and chronic schizophrenia15. Compared to latent variable models, network theory conceptualises psychopathology as a system of interconnected symptoms and mental disorders arising from their causal and dynamic interactions rather than resulting from a common latent cause16. These connections can be graphically encoded as a model composed of nodes, representing study variables (e.g., the items of a psychometric scale) and edges linking them, reflecting significant statistical relationships. Understanding a network’s structural pattern and the significance of specific symptoms can provide valuable insights for rethinking psychopathology and intervention development. For instance, nodes within the network can be organised into communities, clusters of nodes with dense connections within the same cluster and fewer connections to items belonging to other ones, offering an alternative representation of the psychopathological dimensions of schizophrenia. From a translational perspective, networks with well-defined communities may benefit from strategies tailored to each community or targeting symptoms that act as bridges between them4.
Exploratory Graph Analysis (EGA) is a recently developed and robust tool to detect and discover the communities of a network, which have been shown to be mathematically comparable to factors17,18. Importantly, this method is exploratory and does not rely on a priori theories or assumptions nor require the researcher to interpret component loadings of individual items, making it suitable for reevaluating the theoretical structure of a construct19. Overall, EGA has been shown to perform equal or better than traditional factor analyses, especially when study samples are large20 and also offers a bootstrap procedure to test the stability and robustness of the findings21. Furthermore, an additional benefit of EGA compared to traditional factor analysis is that it enables the straightforward visualisation of connections between individual items across various dimensions, which could also aid in identifying symptoms that contribute to comorbidity in mental disorders. However, despite the advantages above, there is still limited research utilising EGA to reveal PANSS dimensions, particularly in FE-SSD.
Hence, the present work focuses on the dimensional structure of the PANSS through a network analysis approach in a sample of first-episode schizophrenia spectrum disorder with minimal or no prior exposure to antipsychotic treatment. The principal objectives of this study are: (1) to determine the number of dimensions of the scale using dedicated network techniques; (2) to assess the stability of the identified model; and (3) to test the performance of an alternative model after the exclusion of unstable items if existing.
Methods
Study design and participants
This research constitutes a secondary analysis of data from the Optimisation of Treatment and Management of Schizophrenia in Europe (OPTiMiSE) trial, conducted at 27 general hospitals and psychiatric specialty clinics in 14 European countries (Austria, Belgium, Bulgaria, Czech Republic, Denmark, France, Germany, Italy, the Netherlands, Poland, Romania, Spain, Switzerland and the UK) and Israel.
In this trial, individuals with FE-SSD, aged 18–40 years, who met the Diagnostic and Statistical Manual of Mental Disorders (4th edition) criteria for schizophrenia, schizophreniform disorder, or schizoaffective disorder were enrolled. Diagnoses were confirmed by the Mini-International Neuropsychiatric Interview-Plus22.
Exclusion criteria were: (a) a lapse of more than two years between the onset of psychosis and enrolment; (b) treatment with any antipsychotic medication for over two weeks in the preceding year or a cumulative duration of six weeks or more throughout their lifetime; (c) a previous history of intolerance to one of the study drugs; (d) meeting any of the contraindications for any of the study drugs; e) being coercively treated, represented by a legal guardian, or both, or being in legal custody; or f) being pregnant or breastfeeding at the study time.
The study adhered to the ethical principles of the Declaration of Helsinki, and each centre obtained ethics approval. Before any procedures, participants were provided with information about the purposes and protocol of the study and signed the informed consent.
For the present analysis, we utilised data gathered during phase 1 of the initial study, involving an open-label amisulpride treatment administered at a daily dosage ranging from 200 to 800 mg. A total of 446 participants were included from an initial pool of 481 subjects who underwent eligibility assessment and provided informed consent23. A more comprehensive explanation of the rationale and methodology of this clinical trial can be found in a separate publication24.
Measures
Following the initial screening visit for eligibility assessment, baseline data were collected, including sociodemographic variables, diagnoses, current treatments and rating scales.
The psychopathological assessment included the Positive and Negative Syndrome Scale (PANSS)8 to characterise nuclear symptoms of schizophrenia. All assessments were conducted by clinicians who had received a standardised training and certification in utilising the PANSS instrument. During the study, inter-rater reliability was assessed at all sites, resulting in an intraclass correlation coefficient of 0.8223. For a detailed overview of the results obtained from the other psychometric instruments utilised in the OPTiMiSE study, such as the Calgary Depression Scale for Schizophrenia (CDSS) or the Personal and Social Performance scale (PSP), readers are encouraged to consult other published works23,25.
Data analyses
First, the sociodemographic characteristics of the sample and the descriptive statistics of psychopathological measures were analysed, expressing the results with means, standard deviations (SD) and percentages.
Second, we estimated the empirical network structure of the 30 items of the PANSS using the default EGA analysis, which combines the GLASSO network estimation with EBIC model selection26 and the Walktrap algorithm27 to determine the number of communities in the network and their item composition17. In the resulting undirected network, nodes symbolise the study variables, while edges represent partial correlation coefficients between them after accounting for all other variables in the network. It is worth mentioning that this algorithm is deterministic, meaning that the number and the variable content of the communities are estimated without any input or guidance from the researcher21.
We analysed the stability of the resulting communities employing a novel bootstrap approach called Bootstrap Exploratory Graph Analysis (bootEGA), using a parametric procedure through 500 bootstrapped samples, in keeping with previous research methods21. This procedure retrieves and plots the median network structure, constructed based on the median value of each pairwise partial correlation across the bootstraps. Subsequently, it reapplies the community detection algorithm. By computing various statistics, this approach facilitates the assessment of the consistency of dimensions and the organisational pattern of items across bootstrapped networks. Moreover, it aids in identifying problematic items, such as those that might be considered multidimensional and could contribute to structural inconsistency (e.g., those frequently replicating across two or more dimensions in different bootstrapped samples)21. The frequency of dimensions across the set of bootstrapped samples was computed along with their structural consistency, which is defined as the proportion of times the original dimension is identically replicated. Afterwards, item stability was calculated, representing the number of times a node is estimated in the same dimension as the initial EGA structure in the bootstrap analysis. Instruments characterised by low item stability exhibit an unstable dimensionality structure that does not consistently replicate within bootstrapped samples28.
Furthermore, the fit of the structure suggested by EGA was verified using the confirmatory factor analysis (CFA) function from the EGAnet R package with the diagonally weighted least squares (WLSMV) estimator, calculating the Comparative Fit Index (CFI) and the Root Mean Square Error of Approximation (RMSEA).
Finally, in line with previous research suggesting that items could be considered unstable when their stability values fall below 0.7521, we replicated the analysis above after excluding these variables, aiming to identify a stable model with all items showing stability values over 0.75.
We used JASP (https://jasp-stats.org/) and RStudio (version 2023.06.1) with the EGAnet package (version 2.0.3) to perform data analyses.
Results
Participants and descriptive statistics
The sociodemographic, clinical and psychometric characteristics of the sample, along with the descriptive statistics, are presented in Table 1.
Network structure and dimensional composition of the 30-item PANSS
The network resulting from the empirical EGA for the full 30-item version of the PANSS is depicted in Fig. 1. Four dimensions emerged from this initial analysis.
a Exploratory graph analysis (EGA). b Bootstrap exploratory graph analysis. PANSS items: P1, Delusions; P2, Conceptual Disorganisation; P3, Hallucinatory Behaviour; P4, Excitement; P5, Grandiosity; P6, Suspiciousness/Persecution; P7, Hostility; N1, Blunted Affect; N2, Emotional Withdrawal; N3, Poor Rapport; N4, Passive/Apathetic Social Withdrawal; N5, Difficulty in Abstract Thinking; N6, Lack of Spontaneity and Flow of Conversation; N7, Stereotyped Thinking; G1, Somatic Concern; G2, Anxiety; G3, Guilt Feelings; G4, Tension; G5, Mannerisms and Posturing; G6, Depression; G7, Motor Retardation; G8, Uncooperativeness; G9, Unusual Thought Content; G10, Disorientation; G11, Poor Attention; G12, Lack of Judgment and Insight; G13, Disturbance of Volition; G14, Poor Impulse Control; G15, Preoccupation; G16, Active Social Avoidance.
However, the median network structure obtained with the bootstrapped EGA did not match these dimensions, retrieving a 5-cluster solution instead (median number of dimensions = 5; 95% confidence interval 3.09 - 6.91) (Fig. 1b). The analysis of the frequency of the number of communities over the 500 iterations showed that different models (ranging from 3 to 9 dimensions) were found in a substantial percentage of bootstraps, indicating instability in the structure (Table 2). Following that, the structural consistency of the empirical dimensions was assessed. Acceptable values were observed for dimensions 2 (0.718) and 4 (0.770), while dimensions 1 (0.170) and 3 (0.210) were clearly unstable.
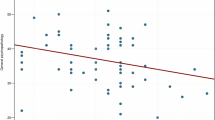
Item stability analysis (how often, across bootstraps, each variable is replicating in the same community as in the empirical structure) is shown in Fig. 2. The following nine nodes showed values below the recommended cutoff of 0.75: P4 (Excitement, 0.466), P5 (Grandiosity, 0.250), G1 (Somatic concern, 0.366), G2 (Anxiety, 0.460), G3 (Guilt feelings, 0.454), G4 (Tension, 0.454), G6 (Depression, 0.456), G12 (Lack of judgment and insight, 0.426) and G16 (Active social avoidance, 0.618).
P1, Delusions; P2, Conceptual Disorganisation; P3, Hallucinatory Behaviour; P4, Excitement; P5, Grandiosity; P6, Suspiciousness/Persecution; P7, Hostility; N1, Blunted Affect; N2, Emotional Withdrawal; N3, Poor Rapport; N4, Passive/Apathetic Social Withdrawal; N5, Difficulty in Abstract Thinking; N6, Lack of Spontaneity and Flow of Conversation; N7, Stereotyped Thinking; G1, Somatic Concern; G2, Anxiety; G3, Guilt Feelings; G4, Tension; G5, Mannerisms and Posturing; G6, Depression; G7, Motor Retardation; G8, Uncooperativeness; G9, Unusual Thought Content; G10, Disorientation; G11, Poor Attention; G12, Lack of Judgment and Insight; G13, Disturbance of Volition; G14, Poor Impulse Control; G15, Preoccupation; G16, Active Social Avoidance.
A matrix of the proportion of times these items replicated in each of the possible bootstrapped dimensions is presented in Table 3, further supporting their multidimensional properties.
Network structure and dimensional composition of the 21-item PANSS
The analysis was repeated without the lowest stability nodes, resulting in a second network model comprising the remaining 21 items of the PANSS. Once again, the model identified four communities, as illustrated in Fig. 3a.
a Exploratory graph analysis (EGA). b Bootstrap exploratory graph analysis. PANSS items: P1, Delusions; P2, Conceptual Disorganisation; P3, Hallucinatory Behaviour; P6, Suspiciousness/Persecution; P7, Hostility; N1, Blunted Affect; N2, Emotional Withdrawal; N3, Poor Rapport; N4, Passive/Apathetic Social Withdrawal; N5, Difficulty in Abstract Thinking; N6, Lack of Spontaneity and Flow of Conversation; N7, Stereotyped Thinking; G5, Mannerisms and Posturing; G7, Motor Retardation; G8, Uncooperativeness; G9, Unusual Thought Content; G10, Disorientation; G11, Poor Attention; G13, Disturbance of Volition; G14, Poor Impulse Control; G15, Preoccupation.
The first community comprised nodes representing positive symptoms of psychosis, including Delusions (P1), Hallucinatory Behaviour (P3), Suspiciousness/Persecution (P6) and Unusual Thought Content (G9). This community was designated as the Positive dimension. The second and largest group consisted of a combination of items from the three PANSS subscales and was labelled as the Cognitive / Disorganised dimension. It included Conceptual Disorganisation (P2), Abstract Thinking (N5), Stereotyped Thinking (N7), Mannerisms and Posturing (G5), Disorientation (G10), Poor Attention (G11), Disturbance of Volition (G13) and Preoccupation (G15). The third community was made up of the three variables, Hostility (P7), Uncooperativeness (G8), and Poor Impulse Control (G14) and was called the Excited/Aggressive dimension. The rest of the nodes from the negative subscale of the PANSS consistently exhibited stronger interconnections and congregated to form the fourth cluster of items. This included Blunted Affect (N1), Emotional Withdrawal (N2), Poor Rapport (N3), Passive/Apathetic Withdrawal (N4), Lack of Spontaneity, and Flow of Conversation (N6), along with the Motor retardation (G7) item from the general psychopathology subscale. This cluster was defined as the Negative dimension.
In contrast to the 30-item network, these four dimensions consistently replicated in the bootstrapped analysis (median number of dimensions = 4; 95% confidence interval 2.49–5.51), as depicted in Fig. 3b. The frequencies revealed that four dimensions were observed in 61.4% of the bootstrapped replicates, five dimensions in 22.2% and six dimensions in 12.8%. Solutions with three and seven dimensions were also observed in a minority of cases, accounting for 3.6% and 0.2%, respectively. Structural consistency was excellent for dimension 1 (1.00) and dimension 3 (0.942), and adequate for dimension 2 (0.742) and dimension 4 (0.690).
All variables showed an item stability value over 0.75 (Fig. 4), suggesting a good reliability level.
Note: P1, Delusions; P2, Conceptual Disorganisation; P3, Hallucinatory Behaviour; P6, Suspiciousness/Persecution; P7, Hostility; N1, Blunted Affect; N2, Emotional Withdrawal; N3, Poor Rapport; N4, Passive/Apathetic Social Withdrawal; N5, Difficulty in Abstract Thinking; N6, Lack of Spontaneity and Flow of Conversation; N7, Stereotyped Thinking; G5, Mannerisms and Posturing; G7, Motor Retardation; G8, Uncooperativeness; G9, Unusual Thought Content; G10, Disorientation; G11, Poor Attention; G13, Disturbance of Volition; G14, Poor Impulse Control; G15, Preoccupation.
Fit to data
Additional analyses were carried out to verify the fit of the 30-item and 21-item network communities using CFA. Thresholds for the 30-items network structure were X2(399) = 1763.319, p < 0.001, CFI = 0.856 and RMSEA = 0.088. For the 21-items model, coefficients were X2(183) = 779.048, p < 0.001, CFI = 0.925 and RMSEA = 0.086, indicating an improvement over the previous solution.
Discussion
The present study aimed to add insights into the structure of the PANSS scale in first-episode schizophrenia spectrum disorders from a network analysis perspective. To our knowledge, this analysis represents the first effort to define the core psychopathological dimensions of the initial stage of SSD using recent innovations in psychometric analysis, such as the EGA algorithm. This may facilitate the refinement of tools available to mental health clinicians, as already occurred in most medical fields, which have experienced considerable enhancements in the resources at their disposal. From a clinical standpoint, a specific instrument for the early stages of psychosis would enable them to conduct a more comprehensive and efficient assessment of patients’ psychopathological profiles and individual needs, leading to the development of tailored treatment plans.
Contrary to expectations, one of the main findings of our analysis was that, following the exclusion of items that caused instability, we obtained a 4-communities model based on a reduced number of 21 items from the PANSS, lacking the independent depressive domain found in most studies. These results are somewhat surprising given the fact that most factorial analyses, including both FEP and chronic psychosis, retrieved a 5-factor solution instead9. However, in that type of analysis, specific parameters depend on the researchers’ decision (e.g., the selection of the rotation method) and the criteria for choosing the number of factors varied from study to study, some of them only reporting forced five-factor models29.
Other reports, indeed, have shown models with a different number of factors, which may be viable or even preferable in certain stages of the illness. For example, a four-cluster structure with no affective domain has also been previously found in early-onset psychosis with no history of antipsychotic treatment, although the sample had a limited size30. Notwithstanding, it is worth noting that the first bootstrapped analysis performed in our sample also found five communities, but the structural consistency was far from optimal. Thus, we wish to draw attention to the capability of new techniques like EGA, which offers a built-in bootstrap method to enhance the reliability of the results and compare different options to find the best one.
Regarding the number of items incorporated into the model, our findings align with prior studies in FEP, demonstrating improved statistical fit when a reduced number of PANSS items were taken into account10. This may have practical implications, as a shorter version of the instrument could improve the robustness of the model11 and prove valuable in clinical routine, where time constraints present a critical barrier to routine psychometric assessments by clinicians.
The first community detected in our network included positive symptoms, which are considered the core of primary psychosis1. In the final model of our analysis, it incorporated four items: Delusions (P1), Hallucinatory Behaviour (P3), Suspiciousness/Persecution (P6) and Unusual Thought Content (G9). The excellent stability of this dimension further emphasises its nuclear significance since the very onset of the psychotic episode.
The included items exactly replicate the findings from a factor analysis in early psychosis31 and are very close to the findings from another study employing EGA in non-affective psychosis32, but the latter additionally contained the Grandiosity (P5) node. The P5 item was also included in a meta-analytical factor analysis9 and might represent a feature of more chronic stages of the illness. In a comparative study, P6 loaded in the positive factor only in the early onset schizophrenia group, whereas P5 did only in the chronic schizophrenia group33, further supporting this hypothesis. Moreover, our results agree with previous literature about the inadequacy of the PANSS positive subscale to capture these symptoms, as some of its items seem to better describe other clinical dimensions9. Future studies should explore the adoption of this alternative approach when evaluating positive symptoms using the PANSS, especially when considering its typical use as an outcome measure in clinical trials of antipsychotic medications. Furthermore, in clinical daily practice, this could help make more precise, data-driven decisions regarding changes in antipsychotic treatment.
While literature shows a certain level of consensus for positive symptoms, the Cognitive / Disorganised dimension appears to be among the least consistent across existing studies. For example, the model proposed by Wallwork and colleagues only includes three items for this factor: Conceptual Disorganisation (P2), Abstract Thinking (N5) and Poor Attention (G11), all of which are incorporated into our dimensional structure34. Our findings also align with other 5-dimension solutions, which similarly include different combinations of Stereotyped Thinking (N7), Mannerisms and Posturing (G5), Disorientation (G10), Disturbance of Volition (G13) and Preoccupation (G15)29,31,35. Medication status, including the cognitive impact of some antipsychotics and benzodiazepines, illness duration and different factorial procedures, could be considered as potential reasons for this heterogeneity. Nevertheless, it is interesting to observe that when previous research is summarised with meta-analytical methods, the items suggested for this dimension are identical to the nodes included in our network model9.
Overall, these results could have both theoretical and practical implications. Firstly, we endorse the existence of a distinct cluster comprising cognitive and disorganised symptoms, separate from the other psychopathological dimensions, even in the very early phase of the disorder, prior to significant pharmacological treatment. In this sense, the findings also align with previous research demonstrating this dimension in individuals at high risk for psychosis36,37. Furthermore, within this population, poorer cognitive function has been linked to an increased likelihood of transitioning to a full psychosis diagnosis38. Secondly, it suggests that this structural pattern may remain relatively stable from the onset of psychosis to a later chronic stage, which is also consistent with prior literature on cognitive impairment in schizophrenia39. Thirdly, it implies that the development of targeted treatments addressing this specific community (e.g., add-on strategies to complement conventional antipsychotic treatment) could potentially positively impact the entire network status, indirectly improving other clusters.
Considering the role of cognition as a critical prognostic indicator for schizophrenia, literature generally emphasises the importance of its careful evaluation39 and inclusion in network studies15. While we fully agree with these recommendations, we also support the idea that simpler yet robust psychometrics instruments (as in the case of cognitive items from the PANSS) serve as a considerably better alternative than completely neglecting cognition assessment, especially in situations where conducting a comprehensive cognitive battery is not feasible39.
Negative symptoms represent another critical dimension of psychosis, garnering increasing attention due to their association with low remission rates and poor functional outcomes1. Although the PANSS has traditionally been used to evaluate negative symptoms through its 7-item negative subscale, it is now widely acknowledged that the original item composition may not be optimal. One of the main criticisms is that this subscale incorporates items that are not relevant to the current conceptualisation of the negative domain, and no single negative symptom factor from PANSS has achieved broad consensus40,41. Another limitation of the PANSS is its inadequate assessment of avolition, a core negative symptom associated with poorer outcomes40. Our network further highlights this weakness by placing the Disturbance of Volition (G13) item, which primarily focuses on the observable behavioural indicators at the expense of experiential aspects42, in the Cognitive / Disorganised dimension instead.
Our negative solution differs from another study in FEP, which included more items, but the authors provided limited information about the treatment31. Methodological differences, as excluding affective psychoses, may account for inconsistencies with other FEP studies, as negative symptoms might exhibit diverse structures across different psychosis diagnoses, rather than forming a monolithic, transdiagnostic construct43. On the other hand, our model replicates a previous consensus34 and closely overlaps with a recent EGA analysis32. A meta-analysis of the factor structure of the PANSS also found a similar composition but also included the Active Social Avoidance (G16) item, although it was the one with the lower loading coefficient9. This item, excluded in our model as in previous studies35, has been previously identified as a bridge symptom linking the positive and negative dimensions25, suggesting a potential cross-loading issue between these dimensions. The recent EPA guidance on the assessment of negative symptoms in schizophrenia also recommends not considering G16 as a negative symptom40.
Additionally, the EPA guidance supports the exclusion of Motor Retardation (G7), which can be related to extrapyramidal side effects of pharmacological treatment40. However, the EGA procedure placed this item in the negative cluster in our sample in both bootstrap analyses with very high stability coefficients. In this context, it seems important to remember the stringent exclusion criteria applied to our sample regarding antipsychotic medication. From this perspective, our model could contribute to defining the structure of primary negative symptoms and aid in distinguishing them from secondary symptoms due to treatment side effects, which is considered a priority in current research. Nonetheless, considering the dynamic conceptualisation of psychopathology behind network theories, potential changes after treatment warrant further investigation through longitudinal studies.
As for the Excited/Aggressive dimension, it showed high stability in our sample and included three items which have been consistently found in first-episode patients29,31. On the other hand, the low values of Excitement (P4) and Grandiosity (P5) as items of this dimension in the initial bootstrap analysis might be partially attributed to the low rates of disruptive and aggressive behaviour in the current study sample44.
One primary distinction from most existing literature is that our models did not identify a stable affective dimension. These findings may be attributed to the methodology applied but could also derive from the close connection between positive and affective symptoms in FEP, as observed in prior network models45,46. Indeed, in the initial bootstrap analysis involving all 30 items of the PANSS, Anxiety (G2), Depression (G6) and Guilty Feelings (G3) were grouped in the first dimension alongside positive symptoms. However, their placement exhibited low item stability, leading to their presence in a fifth dimension in a substantial yet inconsistent manner. This tendency toward low values was also observed in another network study, where all nodes belonging to the affective domain exhibited stability coefficients below 0.7532.
Interestingly, in a previous network analysis of the sample, both Depression (G6) and Guilty Feelings (G3) were identified as bridge nodes connecting the positive dimensions of the PANSS with depressive symptoms evaluated through a specific instrument25. In the same study, Anxiety (G2), another item typically associated with the affective dimension in factor analyses, exhibited the highest bridge betweenness value. On the other hand, another work in early-onset psychosis, which also did not find a depressive dimension, integrated the Anxiety item in the disorganised factor30, further highlighting its connection with non-affective symptoms in young patients.
Once again, direct comparisons with previous factorial analyses pose challenges due to methodological differences, and further research within the network framework is warranted to evaluate the dimensional stability of affective items from the PANSS in first-episode samples. Furthermore, it is noteworthy that not all factorial analyses conducted in FEP have excluded bipolar disorders, which might exhibit a more evident depressive dimension less interconnected with positive symptoms. Additionally, affective dimensions derived from traditional factor analysis often combined depressive items (such as Guilty Feelings and Depression) with more anxious symptoms (such as Anxiety, Tension, or Somatic Concern), resulting in a conceptually weaker psychopathological construct.
However, given the elevated prevalence of depression in schizophrenia, particularly in the initial stages of the disorder47, we suggest that proper psychometric assessment should include a specific tool for depressive symptoms, such as the Calgary Depression Scale for Schizophrenia48, given the limitations of relying solely on PANSS items for their evaluation.
Regarding the other items excluded due to their low stability, Somatic Concern (G1) did not load on any dimension, in concordance with previous studies in both FEP29,31 and chronic schizophrenia34. The skewed response distribution for this variable in our study, with most responses at the lower end of the scale, may have contributed to these findings. Low loadings for G1 were also observed in a meta-analysis9. Within network analysis results, other researchers identified low stability for this item in EGA bootstrap, along with the nodes Excitement (P4) and Tension (G4), while showing variations in other PANSS items32. However, it is worth noting that their network included additional instruments besides the PANSS, enrolled chronic patients and did not reevaluate dimensions after removing unstable items from the model.
From a psychopathological perspective, one interpretation of our results is that the excluded items might reflect multiple symptom dimensions, preventing them from crystallising into a specific community within the model. For example, Active Social Avoidance, commonly regarded as a negative symptom, could stem from paranoid suspiciousness40, suggesting positive symptoms as a target to prevent social isolation in young people with SSD25. Similarly, Lack of Insight (G12) has also frequently been omitted in prior factor solutions10, likely due to the potential impact of diverse symptoms from different dimensions on determining this aspect of the disorder. On the other hand, Somatic Concern initially clustered with positive symptoms in the first empirical model but was associated with depressive-anxious symptoms in the bootstrap analysis, albeit with low consistency. While it may originate from anxious-depressive states, clinicians should remain vigilant for potential underlying hypochondriacal delusions or hallucinations related to somatic sensations.
Strength and limitations
The main distinctive features of this research derive from the use of innovative methodology within the network analysis framework. Specifically, employing dedicated metrics facilitates the objective identification of symptom communities rather than relying on visual inspection alone. Additionally, the exclusion of unstable items from the final analysis resulted in the estimation of a stable model. Other strengths lie in the characteristics of the recruited sample. While determining the suitable sample size for network analysis is a complex task, it is worth noting that our sample stands out as one of the largest among studies utilising network analysis in FE-SSD and enables the joint analysis of all the PANSS nodes. Moreover, the stringent inclusion criteria provide control over various confounding factors, and the multicenter nature of the study enhances generalisability across different settings.
However, it is important to acknowledge certain limitations inherent in the current findings. A potential concern is selection bias, given that participants were recruited for a randomised controlled trial, which could potentially diminish external validity. Conversely, excluding specific diagnoses, like affective psychosis, may restrict the generalisability of our findings to all first-episode psychosis cases, particularly when examining the stability of the depressive dimension. Also, the clinical evaluation did not include an intelligence quotient (IQ) assessment and lacked a dedicated cognitive assessment to better characterise the degree of agreement with items from the Cognitive/Disorganised dimension of the PANSS. Furthermore, it is essential to highlight that latent variable modelling and network analysis operate under distinct assumptions and implications, which can result in inaccurate direct comparisons with existing literature. Finally, the cross-sectional design of our analysis does not permit the study of potential dynamic changes in dimensions over time, an aspect that should be explored in future studies.
Conclusions
Using innovative network analysis techniques, we propose a concise version of the PANSS, incorporating 21 key items that comprehensively capture the core symptoms of initial psychosis episodes. This revised version provides clinicians with a robust psychometric tool for more precise measurement of current symptom severity with reduced administration time, although external validation in a different cohort is required. Also, while this solution may offer a sharper definition of psychotic symptoms in FE-SSD, facilitating tailored treatment plans, it is advisable to complement it with a dedicated instrument for evaluating affective symptoms.
Data availability
The data that support the findings of this study are available from the corresponding author, MPGP, upon reasonable request. Restrictions in relation to potentially identifiable personal information apply.
References
Maj, M. et al. The clinical characterization of the patient with primary psychosis aimed at personalization of management. World Psychiatry 20, 4–33 (2021).
Owen, M. J., Sawa, A. & Mortensen, P. B. Schizophrenia. Lancet 388, 86–97 (2016).
Spark, J. et al. Distinguishing schizophrenia spectrum from non-spectrum disorders among young patients with first episode psychosis and at high clinical risk: the role of basic self-disturbance and neurocognition. Schizophr. Res. 228, 19–28 (2021).
Abplanalp, S. J. & Green, M. F. Symptom structure in schizophrenia: implications of latent variable modeling vs network analysis. Schizophr. Bull. 48, 538–543 (2022).
Sandsten, K. E., Zahavi, D. & Parnas, J. Disorder of selfhood in schizophrenia: a symptom or a gestalt? Psychopathology 55, 273–281 (2022).
García-Mieres, H., Lysaker, P. & Leonhardt, B. L. A comparison of personal recovery in adults with early psychosis and prolonged schizophrenia. Psicothema 34, 35–40 (2022).
Stanghellini, G. The dynamic paradigm of illness in psychopathology. World Psychiatry 23, 163–164 (2024).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261 (1987).
Shafer, A. & Dazzi, F. Meta-analysis of the positive and Negative Syndrome Scale (PANSS) factor structure. J. Psychiatr. Res. 115, 113–120 (2019).
Langeveld, J. et al. Is there an optimal factor structure of the Positive and Negative Syndrome Scale in patients with first-episode psychosis? Scand. J. Psychol. 54, 160–165 (2013).
Higuchi, C. H. et al. Identifying strategies to improve PANSS based dimensional models in schizophrenia: accounting for multilevel structure, Bayesian model and clinical staging. Schizophr. Res. 243, 424 (2022).
Hu, L. T. & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 6, 189–194 (1999).
Goretzko, D., Siemund, K. & Sterner, P. Evaluating model fit of measurement models in confirmatory factor analysis. Educ. Psychol. Meas. 84, 123–144 (2024).
Martínez-Cao, C. et al. Is it possible to stage schizophrenia? A systematic review. Transl. Psychiatry 12, 197 (2022).
Buchwald, K. et al. Centrality statistics of symptom networks of schizophrenia: a systematic review. Psychol. Med. https://doi.org/10.1017/S003329172300363X (2024).
Borsboom, D. A network theory of mental disorders. World Psychiatry 16, 5–13 (2017).
Golino, H. F. & Epskamp, S. Exploratory graph analysis: a new approach for estimating the number of dimensions in psychological research. PLoS ONE 12, e0174035 (2017).
Christensen, A. P. & Golino, H. On the equivalency of factor and network loadings. Behav. Res. Methods 53, 1563–1580 (2021).
Christensen, A. P., Gross, G. M., Golino, H. F., Silvia, P. J. & Kwapil, T. R. Exploratory graph analysis of the multidimensional schizotypy scale. Schizophr. Res. 206, 43–51 (2019).
Golino, H. et al. Investigating the performance of Exploratory Graph Analysis and traditional techniques to identify the number of latent factors: a simulation and tutorial. Psychol. Methods 25, 292–320 (2019).
Christensen, A. P. & Golino, H. Estimating the stability of psychological dimensions via bootstrap exploratory graph analysis: a monte carlo simulation and tutorial. Psych. 2021 3, 479–500 (2021).
Sheehan, D. V. et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59, 0–0 (1998).
Kahn, R. S. et al. Amisulpride and olanzapine followed by open-label treatment with clozapine in first-episode schizophrenia and schizophreniform disorder (OPTiMiSE): a three-phase switching study. Lancet Psychiatry 5, 797–807 (2018).
Leucht, S. et al. The Optimization of Treatment and Management of Schizophrenia in Europe (OPTiMiSE) trial: rationale for its methodology and a review of the effectiveness of switching antipsychotics. Schizophr. Bull. 41, 549–558 (2015).
Dal Santo, F. et al. Searching for bridges between psychopathology and real-world functioning in first-episode psychosis: A network analysis from the OPTiMiSE trial. Eur. Psychiatry 65, e33 (2022).
Epskamp, S., Borsboom, D. & Fried, E. I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Methods https://doi.org/10.3758/s13428-017-0862-1 (2017).
Pons, P. & Latapy, M. Computing communities in large networks using random walks. Lecture Notes in Computer Science ((including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics) 3733 LNCS, p. 284–293 (2005).
Brown, G. P., Delgadillo, J. & Golino, H. Distinguishing the dimensionsof the original dysfunctional attitude scale in an archival clinical sample. Cogn. Ther. Res. 47, 69–83 (2023).
Emsley, R. et al. The factor structure for the Positive and Negative Syndrome Scale (PANSS) in recent-onset psychosis. Schizophr. Res. 61, 47–57 (2003).
Petruzzelli, M. G. et al. Early onset first episode psychosis: dimensional structure of symptoms, clinical subtypes and related neurodevelopmental markers. Eur. Child Adolesc. Psychiatry 27, 171–179 (2018).
Best, M. W., Grossman, M., Oyewumi, L. K. & Bowie, C. R. Examination of the Positive and Negative Syndrome Scale factor structure and longitudinal relationships with functioning in early psychosis. Early Inter. Psychiatry 10, 165–170 (2016).
Moura, B. M. et al. A network of psychopathological, cognitive, and motor symptoms in schizophrenia spectrum disorders. Schizophr. Bull. 47, 915–926 (2021).
Xu, K. et al. Preliminary analysis of positive and negative syndrome scale in ketamine-associated psychosis in comparison with schizophrenia. J. Psychiatr. Res. 61, 64–72 (2015).
Wallwork, R. S., Fortgang, R., Hashimoto, R., Weinberger, D. R. & Dickinson, D. Searching for a consensus five-factor model of the Positive and Negative Syndrome Scale for schizophrenia. Schizophr. Res. 137, 246–250 (2012).
White, L. et al. Empirical assessment of the factorial structure of clinical symptoms in schizophrenia: a multisite, multimodel evaluation of the factorial structure of the positive and negative syndrome scale. Psychopathology 30, 263–274 (1997).
Yang, Z., Lim, K., Lam, M., Keefe, R. & Lee, J. Factor structure of the positive and negative syndrome scale (PANSS) in people at ultra high risk (UHR) for psychosis. Schizophr. Res. 201, 85–90 (2018).
Lim, K. et al. Large-scale evaluation of the Positive and Negative Syndrome Scale (PANSS) symptom architecture in schizophrenia. Asian J. Psychiatr. 62, 102732 (2021).
Addington, J. et al. The role of cognition and social functioning as predictors in the transition to psychosis for youth with attenuated psychotic symptoms. Schizophr. Bull. 43, 57–63 (2017).
Vita, A. et al. European Psychiatric Association guidance on assessment of cognitive impairment in schizophrenia. Eur. Psychiatry 65, e58 (2022).
Galderisi, S. et al. EPA guidance on treatment of negative symptoms in schizophrenia. Eur. Psychiatry 64, e21 (2021).
Garcia-Portilla, M. P. et al. Psychometric evaluation of the negative syndrome of schizophrenia. Eur Arch Psychiatry Clin Neurosci. 265, 559–66 (2015).
Strauss, G. P., Bartolomeo, L. A. & Harvey, P. D. Avolition as the core negative symptom in schizophrenia: relevance to pharmacological treatment development. npj Schizophr. 7, 16 (2021).
Pelizza, L. et al. Negative symptom configuration within and outside schizophrenia spectrum disorders: results from the “Parma Early Psychosis” program. Psychiatry Res. 294, 113519 (2020).
Faay, M. D. M. et al. Hostility and aggressive behaviour in first episode psychosis: results from the OPTiMiSE trial. Schizophr. Res. 223, 271 (2020).
Griffiths, S. L. et al. Structure and stability of symptoms in first episode psychosis: a longitudinal network approach. Transl. Psychiatry 11, 567 (2021).
Herniman, S. E. et al. Interrelationships between depressive symptoms and positive and negative symptoms of recent onset schizophrenia spectrum disorders: A network analytical approach. J. Psychiatr. Res. 140, 373–380 (2021).
Herniman, S. E. et al. Depressive psychopathology in first-episode schizophrenia spectrum disorders: a systematic review, meta-analysis and meta-regression. Psychol. Med. 49, 2463 (2019).
Addington, D., Addington, J. & Schissel, B. A depression rating scale for schizophrenics. Schizophr. Res. 3, 247 (1990).
Acknowledgements
This study was funded by the European Commission Seventh Framework. Programme (HEALTH-F2-2010-242114).
Author information
Authors and Affiliations
Contributions
Conceptualisation: Dal Santo, Fernández-Egea, García-Portilla and Galderisi. Data curation: Dal Santo and González-Blanco. Formal analysis: Dal Santo, García-Portilla and González-Blanco. Data visualisation: Dal Santo, González-Blanco and Sáiz. Writing – original draft: Dal Santo, González-Blanco and Sáiz. Writing – review & editing: García-Portilla, Fernández-Egea, Sáiz, Giordano, Galderisi and Bobes. Study supervision: García-Portilla, Sáiz, Galderisi and Bobes. All authors gave the final approval.
Corresponding author
Ethics declarations
Competing interests
F.D.S. has received grants from the Spanish Foundation of Psychiatry and Mental Health and the European Psychiatric Association. MPGP has been a consultant to and/or has received honoraria/grants from Angelini, Alianza Otsuka-Lundbeck, Instituto de Salud Carlos III, Janssen-Cilag, Lundbeck, Otsuka, and Pfizer. EFE has received consultancy honoraria from Boehringer-Ingelheim (2022), Atheneum (2022) and Rovi (2022), speaker fees by Adamed (2022) and Otsuka (2023) and training and research material from Merz (2020). L.G.B. has been a consultant to and/or has received honoraria/grants from the Spanish Foundation of Psychiatry and Mental Health, European Psychiatric Association, Otsuka, Lundbeck, Janssen-Cilag and Pfizer. P.A.S. has been a consultant to and/or has received honoraria or grants from Adamed, CIBERSAM, European Commission, GlaxoSmithKline, Instituto de Salud Carlos III, Janssen-Cilag, Lundbeck, Otsuka, Pfizer, Plan Nacional sobre Drogas and Servier. S.G. has been a consultant to Angelini, Gedeon Richter-Recordati, Innova Pharma-Recordati Group within the last 2 years and has received honoraria/grants from Angelini, Gedeon Richter-Recordati, Janssen Pharmaceuticals, Janssen Cilag, Lundbeck and Recordati Pharmaceuticals. J.B. has received research grants and served as consultant, advisor or speaker within the last 5 years for: AB-Biotics, Acadia Pharmaceuticals, Angelini, Casen Recordati, D&A Pharma, Exeltis, Gilead, GSK, Ferrer, Indivior, Janssen-Cilag, Lundbeck, Mundipharma, Otsuka, Pfizer, Reckitt-Benckiser, Roche, Sage Therapeutics, Servier, Shire, Schwabe Farma Ibérica, research funding from the Spanish Ministry of Economy and Competiveness - Centro de Investigación Biomedica en Red area de Salud Mental (CIBERSAM) and Instituto de Salud Carlos III-, Spanish Ministry of Health, Social Services and Equality -Plan Nacional sobre Drogas- and the 7th Framework Programme of the European Union. All other authors declare that they have no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dal Santo, F., García-Portilla, M.P., Fernández-Egea, E. et al. The dimensional structure of the Positive and Negative Syndrome Scale in first-episode schizophrenia spectrum disorders: an Exploratory Graph Analysis from the OPTiMiSE trial. Schizophr 10, 81 (2024). https://doi.org/10.1038/s41537-024-00499-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41537-024-00499-5
This article is cited by
-
Morphometric similarity network-based graph convolutional networks for schizophrenia classification
Scientific Reports (2025)
-
An exploratory network analysis to investigate schizotypy’s structure using the ‘Multidimensional Schizotypy Scale’ and ‘Oxford-Liverpool Inventory’ in a healthy cohort
Schizophrenia (2025)
-
Mindfulness in Teaching: Translation, Psychometric Evaluation, and Network Estimation of the Mindfulness in Teaching Scale (MTS) for Arab Teachers
Mindfulness (2025)