Abstract
Intervention for social cognition could be key to improving social functioning in patients with schizophrenia. A first step towards its clinical implementation involves interviewing patients about their subjective difficulties with social cognition as they experience them in the real world. The present study focused on the clinical subtypes classified by the discrepancies between the subjective difficulties in social cognition and actual cognitive impairment. A total of 131 outpatients with schizophrenia and 68 healthy controls were included. Objective measurement of social cognition was performed using a test battery covering four representative domains, and subjective difficulties were determined by a questionnaire covering the same domains. A two-step cluster analysis explored the potential classification of social cognition in patients with schizophrenia. There was little correlation between the objective performance on social cognition tasks and subjective difficulties in social cognition. The analysis yielded three clusters: the low-impact group (low objective impairment and low subjective difficulties), the unaware group (high objective impairment but low subjective difficulties), and the perceptive group (moderate objective impairment and high subjective difficulties). Positive, negative, and general symptoms were more severe in the two groups that showed impaired performance on the social cognition tasks (i.e., the unaware and perceptive groups) than those in the low-impact group. Neurocognition and functional capacity were the lowest in the unaware group, and social functioning was the lowest in the perceptive group. Awareness about the clinical subtypes of social cognition could serve as a guidepost for providing individualized, targeted interventions.
Similar content being viewed by others
Introduction
Impaired social cognition is widely observed in patients with schizophrenia and contributes strongly to a decline in social functioning as a mediator between neurocognition and social functioning1,2. Therefore, improvement of social cognition is an essential therapeutic target in the treatment of schizophrenia and could represent the key to clinical recovery in these patients3,4. Social cognition refers to “mental operations that underlie social interactions, including perceiving, interpreting, and generating responses to the intentions, dispositions, and behaviors of others” and has a critical role in social interaction and participation5. Four core domains of social cognition have been identified: theory of mind, social perception and knowledge, attributional style/bias, and emotion processing6. Measures of and interventions for social cognition have been developed mainly based on these core domains. Reliable and validated measures have been developed, also taking into account cultural and linguistic differences7,8,9,10. Interventions have been divided into pharmacotherapy and psychosocial therapy. In regard to pharmacotherapy, mainly the efficacy of oxytocin has been examined, and further evidence is expected to be accumulated11,12,13,14. In regard to psychosocial therapy, several programs have been developed, for example, Social Cognition and Interaction Training15. Many studies regarding those programs have been accumulated on improving social cognition and even social functioning16,17,18.
However, according to a previous online survey, only a few patients with schizophrenia actually received examinations or treatment related to social cognition19; the survey revealed that only 3.9% of patients with schizophrenia received treatments to improve social cognition, and a large proportion of the patients were still unfamiliar with the term or concept of social cognition in the first place. Given these findings, it would be very unlikely for patients with schizophrenia to voluntarily request treatment for social cognition in the current clinical settings. Thus, it could be said that there is an unmet need in relation to treatment of patients with schizophrenia in that while effective interventions have been developed, they have not been provided to the patients. A first step towards clinical implementation of intervention for social cognition is for the medical workers to interview the patient to determine the presence and degree of difficulties the patients experience in their real lives in relation to social cognition, i.e., the subjective difficulties20,21,22. In the previous study referred to above, patients with schizophrenia, while not being aware of the term social cognition, perceived strong subjective difficulties when presented with specific situations in their lives that required social cognition19; this was the case for all four domains of social cognition. Furthermore, the degree of subjective difficulties itself was related to the level of social functioning23. These findings suggest that measures of subjective difficulties can be important indicators that could be efficiently utilized and provide much information in clinical settings.
While subjective difficulties could have an important clinical role, it remains under question if they simply reflect the actual level of impairments of cognitive performance as measured objectively. In general, patients with schizophrenia have impaired insight24,25. One cause is impaired metacognition, and it is not uncommon to find a discrepancy between a patient’s subjective perceptions and the results of objective assessments of their symptoms26. Such discrepancy is often observed not only in psychopathological symptoms but also in cognitive functions27. In particular, the degree of discrepancy between subjective perception of one’s own cognitive function and objective assessment of cognitive performance has been defined as “introspective accuracy”28. Introspective accuracy has often been assessed by measuring the confidence in a cognitive task29. In patients with schizophrenia, diverse patterns have been noted, such as underestimation, agreement, or overestimation30. In general, patients with schizophrenia tend to be overconfident as compared with healthy controls in regard to their performance and functioning, which was associated with various clinical variables, such as higher interpersonal difficulties and delusional symptoms31,32,33. In addition, there are also several reports of schizophrenia patients exhibiting overconfidence about their social cognition. Overconfidence regarding social cognition affected the performance in patients with schizophrenia34,35. Similar to the diverse patterns of introspective accuracy in patients with schizophrenia, a variety of patterns would also be expected in the discrepancies/agreements between subjective difficulties and objective assessment of social cognition, and their clarification could have clinical implications. In fact, a study indicated that the subjective difficulties with social cognition measured by the Observable Social Cognition Rating Scale were not strongly correlated with the objective performance in patients with schizophrenia as a whole, and further detailed examination of this discrepancy is warranted22.
This study was aimed at determining the degree of agreement between objective performance in tasks of social cognition and subjective difficulties in social cognition in patients with schizophrenia, measured for four representative domains. Based on the results, patients with schizophrenia were exploratively classified into groups according to their objective performance and subjective difficulties in social cognition, and the clinical characteristics of these groups were comparatively assessed.
Methods
Study design and participants
This study had a cross-sectional design, and outpatients with schizophrenia and healthy controls were recruited from the National Center of Neurology and Psychiatry, Hokkaido University Hospital and Toho University Omori Medical Center. A total of 131 patients with schizophrenia and 68 healthy controls were included in the study. Participants were aged between 20 and 59 years. The diagnosis of schizophrenia or absence of psychiatric disorders was confirmed using the Mini-International Neuropsychiatric Interview, for use of which we had obtained a license36,37. The patients with schizophrenia had not undergone hospitalization in the previous two months, their prescriptions had not changed in the previous six weeks, and there had been no changes in the prescribed dosages in the previous two weeks. The participants were from a part of our previous study, the Evaluation Study for Social Cognition Measures in Japan, and the detailed study protocol and primary outcome of which have been described elsewhere38,39.
Written informed consent was obtained from the participants prior to the start of the survey, and the participants were informed that they could opt out of the survey at any point. This study was conducted with the approval of the Ethics Committee of the National Center of Neurology and Psychiatry (B2020-107) and the Independent Clinical Research Review Committee of Hokkaido University Hospital (022-0137). The protocol is registered in the UMIN-Clinical Trials Registry (UMIN000043777). This study was performed in accordance with the principles in the latest version of the Declaration of Helsinki.
Measures
Each of the four representative domains of social cognition was assessed using the corresponding task. Specifically, emotion processing was assessed by the Facial Emotion Selection Test (FEST)40, theory of mind by the Hinting41, attributional bias by the Ambiguous Intentions and Hostility Questionnaire (AIHQ)42,43, and social perception and knowledge by the Social Attribution Task-Multiple Choice44. Higher scores indicated higher levels of functioning, except in the AIHQ. For the AIHQ, a reversed score was used to adapt to the other scales. The total score on each of the scales was used. The psychometric properties of the four scales have been examined in the Social Cognition and Psychometric study6,45,46. In addition, they have been recommended for use considering their reliability and validity in Japanese39. Subjective difficulties in social cognition were evaluated using the Self-Assessment of Social Cognition Impairment questionnaire (ACSo)19,20. The ACSo is a self-administered 12-item questionnaire to determine the patients’ subjective difficulties with the four domains of social cognition mentioned above. Higher scores indicated higher degrees of subjective difficulties.
The scores for the four domains were standardized using data from the healthy controls, and composite Z-scores for subjective difficulties and objective performance were calculated, respectively.
The other variables assessed in the present study were psychopathology, assessed by the Positive and Negative Syndrome Scale (PANSS)47,48, neurocognition, assessed by the Brief Assessment of Cognition for Schizophrenia, Japanese Version49,50, functional capacity, assessed by the University of California, San Diego Performance-based Skill Assessment-Brief (UPSA-B)51,52, and social functioning, assessed by the Specific Levels of Functioning Scale (SLOF) with interviewer ratings53,54. Except for the case of PANSS, the total score on each scale was used.
Data analysis
First, the demographics, objective performance in tasks of social cognition, and subjective difficulties in social cognition were compared between the patients with schizophrenia and healthy controls. The t-test was used for comparing continuous variables, and the chi-squared test for comparing categorical variables. Next, using the data from healthy controls, the objective performance and subjective difficulties in the four domains of the patients with schizophrenia were standardized, and the composite Z-scores for objective performance and subjective difficulties were calculated, respectively. To assess the relationship between objective performance and subjective difficulties in patients with schizophrenia, as well as their relationships with other clinical characteristics, correlation analyses were performed. Then, to identify potential clusters of patients with schizophrenia based on agreement or discrepancy between the levels of objective performance and subjective difficulties in social cognition, the two-step cluster analysis was performed using the Z-scores for objective performance and subjective difficulties by the log-likelihood method and Bayesian Information Criterion (BIC). The two-step cluster analysis is an approach for exploring empirical groups of individuals with similar characteristics and has the advantage of allowing automatic calculation of the optimal number of clusters55. This is a hybrid approach that first uses a distance measure (the log-likelihood method in the present study) to separate groups and then a probabilistic approach to choose the optimal subgroup model56. The number of clusters is determined by selecting the best-fitting (i.e., the lowest BIC value) model among the clustering candidates. Furthermore, the silhouette coefficient, calculated from degrees of internal cohesion and external separation, is checked, and a value of 0.5 or greater is considered as being indicative good clustering.
Finally, the clinical characteristics of the identified clusters were assessed by analysis of variance and Tukey’s post hoc test.
Patients with missing values were excluded from each analysis. In all the analyses, the proportions of those with missing values were less than 5%, suggesting that their exclusion had negligible effects on the results57. Statistical differences were determined using two-tailed tests and the significance level was set at p < 0.05. Data analyses were performed using SPSS, version 26.0.
Results
Demographics and objective and subjective social cognition performance in patients with schizophrenia and healthy controls
As shown in Table 1, there were no significant differences in the age or sex distribution between the patients with schizophrenia and healthy controls. The scores on all four domains of social cognition in the objective assessment were significantly lower in the patients with schizophrenia. The scores in all four domains of social cognition in the subjective assessment by the patients were significantly higher in the patients with schizophrenia.
Correlations between objective measures and subjective perception of social cognition
The composite Z-scores of the objective performance and subjective difficulties were −1.60 (standard deviation 1.76) and 0.74 (standard deviation 1.51), respectively. As shown in Table 2, there was a small, but significant correlation between the Z-scores of objective performance and subjective difficulties. There were significant/some degrees of correlations of the objective performance scores with the psychiatric symptoms (PANSS), neurocognition (BACS), functional capacity (UPSA-B), and social functioning (SLOF). There were also significant and weak correlations between the subjective difficulty scores and each of the aforementioned variables, except for negative symptoms and neurocognition.
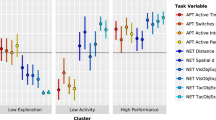
Clusters by objective and subjective social cognition in patients with schizophrenia
The two-step cluster analysis yielded three clusters that fit well with the silhouette coefficient. The BIC values for one, two, three, and four clusters were 200.1, 170.5, 155.6, and 160.3, respectively. The value was the lowest for three clusters, i.e., it was the optimal model. As shown in Fig. 1, Cluster 1 (the low-impact group) comprised 65 patients (49.6%) who showed very little impairment of objective performance in the social cognition tasks and also very few subjective difficulties. Cluster 2 (the unaware group) comprised 43 patients (32.8%) who showed severely impaired objective performance on the social cognition tasks, but scarce subjective difficulties. Cluster 3 (the perceptive group) comprised 23 patients (17.6%) who showed moderately impaired objective performance and reported the highest level of subjective difficulties.
As shown in Table 3, there were no differences in the age, sex distribution, or duration of illness among the three groups. As for the psychiatric symptoms, the scores for positive, negative, and general symptoms were higher in the two groups showing impaired performance on the social cognition tasks (i.e., the unaware and perceptive groups) as compared with those in the low-impact group. Neurocognition and functional capacity were lowest in the unaware group, and social functioning was the lowest in the perceptive group. The results of the post hoc analysis are shown in Table 4.
Discussion
In the present study, we investigated the discrepancies between the objective performance on tasks of social cognition and subjective difficulties in social cognition across the four representative domains of social cognition in patients with schizophrenia. We exploratively classified the patients, based on the agreements and discrepancies between the two. The participants in the present study were patients with stable and chronic schizophrenia. Overall, the patients with schizophrenia showed poorer objective performance on the tasks of social cognition and higher subjective difficulties in social cognition than the healthy controls, consistent with previous reports1,2. Consistent results were obtained across all four domains of social cognition58. Next, there was only a small correlation between the objective performance on social cognition tasks and subjective difficulties in social cognition, indicating that interpreting subjective difficulties as representing the actual level of social cognition should be done cautiously. On the other hand, the results of the cluster analysis, with three clusters classified according to the objective performance on social cognition tasks and subjective difficulties in social cognition, provided clinically helpful insights. The three groups consisted of those with no impairment in objective performance and no subjective difficulties, those with impaired objective performance, but no perceived difficulties, and those with impaired objective performance as well as perceived difficulties in social cognition. About half of the patients from a previous study which classified schizophrenia patients into subgroups based on the results of performance on the tasks of emotion processing and theory of mind were classified into the unimpaired group in this study55. Similar to the proportion in this previous study, the low-impact group, with little impairment in objective performance on social cognitive tasks, accounted for 49.6% of all the participants in the present study. The fact that there were no demographic differences among the groups but differences in the clinical characteristics suggests that the present classification might be reasonable and valid as a classification of clinical subtypes based on the social cognition in patients with schizophrenia.
The three groups in this study had some interesting clinical features. First, the low-impact group showed fewer subjective difficulties in social cognition, higher objective performance on the social cognition tasks, and the highest level of social functioning. It is worth noting that nearly half of the participants had very little cognitive impairment and showed the highest level of social functioning. This is consistent with the numerous reports suggesting that cognition is a strong contributor to social functioning in patients with schizophrenia59,60,61. This group of patients could evaluate themselves reasonably accurately. These results were consistent with previous reports suggesting that a high introspective accuracy contributes to a high level of social functioning62,63. This group also had the mildest positive, negative, and general psychopathological symptoms and would be one group with a relatively good prognosis among patients with schizophrenia with a diverse course. Next, the unaware group showed impaired objective performance on the tasks of social cognition but reported few subjective difficulties in social cognition. The unaware group showed the most impaired social cognition, as well as the most impaired neurocognition and functional capacity. In addition, these patients showed more severe positive, negative, and general psychopathological symptoms than the low-impact group. This group of patients may be unaware of their impaired social cognition due to impairment of other aspects of cognition, such as metacognition, which causes a lack of insight of these patients into their symptoms and illness. It could also be considered as overestimation of the actual level of social cognition by these patients. The characteristics of the unaware group are consistent with those of patients exhibiting overconfidence, with poor functioning and worse psychiatric symptoms34,64,65. Finally, the perceptive group exhibited impaired objective performance on social cognition tasks, had serious subjective difficulties in social cognition, and had severe positive, negative, and general psychopathological symptoms. Furthermore, the perceptive group showed poorer social functioning than the unaware group, which showed the most severe cognitive impairment. As discussed so far, cognitive impairment and low introspective accuracy, such as overconfidence, have been noted as strong contributors to low functioning, which would be a contradictory result for the perceptive group. In this type of high introspective accuracy group, i.e., patients with both high impairments and difficulties, social functioning may be more likely to be influenced by other factors not determined solely by cognitive impairments. For example, depressive symptoms can increase subjective difficulties in social cognition and decrease social functioning2,66. Although the duration of illness was not significantly different among the present groups, the stage of illness could have had an impact. Impairments of social cognition are found in first-episode psychosis and further at-risk states67,68, but the proportion of people who perceive that social cognition is related to their social life increases as the duration of illness increases19. This may be due in part to the fact that the longer the disease duration, the more difficulties the patients face in interpersonal situations related to social cognition and the greater negative attitudes they experience from others. Other psychosocial factors, such as internal stigma or lack of service engagement with social services, could have similar effects61,69. The social factors may have particularly influenced the clustering in the present study, since difficulties perceived in social life were used for the analyses rather than the degree of confidence in performing the task.
The findings of the present study have significant implications, especially in clinical settings. Interviewing patients to determine their subjective difficulties in social cognition is simple to do in clinical settings. It should also be an essential conversation among patients, families, and healthcare providers when implementing examinations and treatments for social cognition. If a patient expresses serious difficulties in social cognition during the interview, he/she may be assumed to belong to the perceptive group and his/her objective performance could be declining. This group is characterized by the lowest social functioning. Thus, these patients should be actively encouraged to receive treatments to improve their social cognition and, consequently, their social functioning, although providing motivation for treatment to these patients is often a challenge70,71. On the other hand, careful observation is required in patients who report fewer difficulties. While some of these patients may actually have little impairment of social cognition, there is also a certain subset of these patients who belong to the unaware groups, i.e., those with a high degree of impairment in objective performance. These patients may be better served by provision of metacognitive training to improve their insight into their own disease before they receive treatment for social cognition72,73. Examination of the level of social cognition using objective measures is also helpful in this group, as that would contribute to confirming the patient’s actual degree of functional impairment and defining the treatment goals. In addition to the questionnaire for measuring the subjective difficulties used in the present study, obtaining information from the patient’s relatives who are close to the patient is also essential22. As an example, a scale for disability caused by cognitive impairments has been developed, including the perspectives of patients’ relatives74, and further research in this area is warranted. Furthermore, it has been suggested that cognitive impairments may be an endophenotype that extends across a variety of psychiatric illnesses, including depression and bipolar disorder75,76. Therefore, the clinical subtypes identified in the present study may not be specific to patients with schizophrenia alone.
The present study had some limitations. Although we used a recommended test battery covering all four representative domains of social cognition in this study, it was difficult to collect a large sample size. While this sample size was considered acceptable for cluster analysis, a larger sample size would be desirable for more detailed analyses, such as investigations pertaining to each domain of social cognition. The characteristics were only compared among the groups, and no intra-group variations in the characteristics were investigated. In addition, in the present cluster analysis, only objective performance on social cognition tasks and subjective difficulties in social cognition were entered as variables, and other factors that could potentially be used for classification of the patients into clusters were not examined. Depressive symptoms and comorbidities were not adequately assessed in the present study. In particular, the presence of very few depressive symptoms leads to an overestimation in self-assessment, while moderate depressive symptoms could lead to an accurate assessment77,78. Furthermore, severe depressive symptoms could worsen subjective difficulties in social cognition, although they may have little impact on the performance66. Therefore, these may affect the results of cluster analysis, and the results of the present study should be interpreted with caution. An additional limitation was the asymmetry between the measures of subjective difficulties and objective performance that were entered in the cluster analysis. Indeed, the objective performance in some patients with schizophrenia was better than that of healthy controls, but the subjective difficulties measure did not adequately detect this superiority over the healthy controls. This could have affected the results of the cluster analysis.
Conclusion
As in previous studies, a certain number of patients with low cognitive impairment exhibited high social functioning in the present study, reinforcing the importance of focusing on cognitive impairment in the treatment of schizophrenia. The present study also revealed clinical subtypes derived by measuring subjective and objective cognition simultaneously. As in previous studies, the group with a discrepancy, i.e., overestimation, showed worse symptoms and levels of functioning. On the other hand, the group with no discrepancies, but with both high impairments and difficulties showed the lowest levels of functioning. Focusing on these subtypes classified on the basis of such clinical discrepancies could allow rational approaches to be adopted to resolve some unmet needs in the treatment of schizophrenia in the real world79,80,81. Future studies should include a detailed examination of patients with different clinical subtypes of schizophrenia rather than schizophrenia patients as a whole. The present results could contribute to a more precise assessment of the actual impairments of social cognition and could serve as a guidepost for providing individualized, targeted interventions. Intervention in social cognition can be a key to achieving functional recovery in patients with schizophrenia, and the first step in implementing this would be to listen to the patient.
Data availability
The data that support the findings of this study are available upon reasonable request to the corresponding author.
References
Green, M. F., Horan, W. P. & Lee, J. Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry 18, 146–161 (2019).
Kharawala, S. et al. The relationship between cognition and functioning in schizophrenia: a semi-systematic review. Schizophr. Res. Cogn. 27, 100217 (2022).
Horan, W. P. & Green, M. F. Treatment of social cognition in schizophrenia: current status and future directions. Schizophr. Res. 203, 3–11 (2019).
Nahum, M. et al. Online social cognition training in schizophrenia: a double-blind, randomized, controlled multi-site clinical trial. Schizophr. Bull. 47, 108–117 (2021).
Green, M. F. et al. Social cognition in schizophrenia: an NIMH workshop on definitions, assessment, and research opportunities. Schizophr. Bull. 34, 1211–1220 (2008).
Pinkham, A. E. et al. The social cognition psychometric evaluation study: results of the expert survey and RAND panel. Schizophr. Bull. 40, 813–823 (2014).
Weinreb, S., Li, F. & Kurtz, M. M. A meta-analysis of social cognitive deficits in schizophrenia: does world region matter? Schizophr. Res. 243, 206–213 (2022).
Hajdúk, M., Achim, A. M., Brunet Gouet, E., Mehta, U. M. & Pinkham, A. E. How to move forward in social cognition research? Put it into an international perspective. Schizophr. Res. 215, 463–464 (2020).
Lim, K., Lee, S.-A., Pinkham, A. E., Lam, M. & Lee, J. Evaluation of social cognitive measures in an Asian schizophrenia sample. Schizophr. Res. Cogn. 20, 100169 (2020).
Okano, H. et al. Evaluation of social cognition measures for Japanese patients with schizophrenia using an expert panel and modified Delphi method. J. Pers. Med. 11, 275 (2021).
Goh, K. K. & Lu, M.-L. Relationship between the domains of theory of mind, social dysfunction, and oxytocin in schizophrenia. J Psychiatr. Res. 155, 420–429 (2022).
Guastella, A. J. et al. A single dose of oxytocin nasal spray improves higher-order social cognition in schizophrenia. Schizophr. Res. 168, 628–633 (2015).
Strauss, G. P. et al. The effects of combined oxytocin and cognitive behavioral social skills training on social cognition in schizophrenia. Psychol. Med. 49, 1731–1739 (2019).
Yamada, Y. et al. Social cognition deficits as a target of early intervention for psychoses: a systematic review. Front. Psychiatry 10, 333 (2019).
Penn, D. L., Roberts, D. L., Combs, D. & Sterne, A. Best practices: the development of the Social Cognition and Interaction Training program for schizophrenia spectrum disorders. Psychiatr. Serv. 58, 449–451 (2007).
Lahera, G. et al. Social Cognition and Interaction Training (SCIT) versus Training in Affect Recognition (TAR) in patients with schizophrenia: a randomized controlled trial. J. Psychiatr. Res. 142, 101–109 (2021).
Dark, F. et al. Randomized controlled trial of social cognition and interaction training compared to befriending group. Br. J. Clin. Psychol. 59, 384–402 (2020).
Kanie, A. et al. The feasibility and efficacy of social cognition and interaction training for outpatients with schizophrenia in Japan: a multicenter randomized clinical trial. Front. Psychiatry 10, 589 (2019).
Uchino, T. et al. Perceptions of and subjective difficulties with social cognition in schizophrenia from an internet survey: knowledge, clinical experiences, and awareness of association with social functioning. Psychiatry Clin. Neurosci. 76, 429–436 (2022).
Graux, J. et al. A transnosographic self-assessment of social cognitive impairments (ACSO): first data. Front. Psychiatry 10, 847 (2019).
Haddad, C. et al. Self-assessment of social cognition in a sample of Lebanese in-patients with schizophrenia. Schizophr. Res. Cogn. 26, 100207 (2021).
Halverson, T. F. et al. Psychometric properties of the Observable Social Cognition Rating Scale (OSCARS): self-report and informant-rated social cognitive abilities in schizophrenia. Psychiatry Res. 286, 112891 (2020).
Uchino, T. et al. Mediation effects of social cognition on the relationship between neurocognition and social functioning in major depressive disorder and schizophrenia spectrum disorders. J. Pers. Med. 13, 683 (2023).
Aleman, A., Agrawal, N., Morgan, K. D. & David, A. S. Insight in psychosis and neuropsychological function: meta-analysis. Br. J. Psychiatry 189, 204–212 (2006).
Lincoln, T. M., Lüllmann, E. & Rief, W. Correlates and long-term consequences of poor insight in patients with schizophrenia. A systematic review. Schizophr. Bull. 33, 1324–1342 (2007).
Lopez-Morinigo, J.-D. et al. Can metacognitive interventions improve insight in schizophrenia spectrum disorders? A systematic review and meta-analysis. Psychol. Med. 50, 2289–2301 (2020).
Cella, M., Swan, S., Medin, E., Reeder, C. & Wykes, T. Metacognitive awareness of cognitive problems in schizophrenia: exploring the role of symptoms and self-esteem. Psychol. Med. 44, 469–476 (2014).
Silberstein, J. & Harvey, P. D. Impaired introspective accuracy in schizophrenia: an independent predictor of functional outcomes. Cogn. Neuropsychiatry 24, 28–39 (2019).
Pinkham, A. E., Klein, H. S., Hardaway, G. B., Kemp, K. C. & Harvey, P. D. Neural correlates of social cognitive introspective accuracy in schizophrenia. Schizophr. Res. 202, 166–172 (2018).
Mervis, J. E., Vohs, J. L. & Lysaker, P. H. An update on clinical insight, cognitive insight, and introspective accuracy in schizophrenia-spectrum disorders: symptoms, cognition, and treatment. Expert Rev. Neurother. 22, 245–255 (2022).
Moritz, S., Woodward, T. S. & Chen, E. Investigation of metamemory dysfunctions in first-episode schizophrenia. Schizophr. Res. 81, 247–252 (2006).
Köther, U. et al. Don’t give me that look”—Overconfidence in false mental state perception in schizophrenia. Psychiatry Res. 196, 1–8 (2012).
Moritz, S. et al. Overconfidence in incorrect perceptual judgments in patients with schizophrenia. Schizophr. Res. Cogn. 1, 165–170 (2014).
Jones, M. T. et al. Confidence, performance, and accuracy of self-assessment of social cognition: a comparison of schizophrenia patients and healthy controls. Schizophr. Res. Cogn. 19, 100133 (2020).
Perez, M. M., Tercero, B. A., Penn, D. L., Pinkham, A. E. & Harvey, P. D. Overconfidence in social cognitive decision making: correlations with social cognitive and neurocognitive performance in participants with schizophrenia and healthy individuals. Schizophr. Res. 224, 51–57 (2020).
Otsubo, T. et al. Reliability and validity of Japanese version of the Mini‐International Neuropsychiatric Interview. Psychiatry Clin. Neurosci. 59, 517–526 (2005).
Sheehan, D. V. et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59, 34–57 (1998).
Kubota, R. et al. Study protocol: the Evaluation Study for Social Cognition Measures in Japan (ESCoM). J. Pers. Med. 11, 667 (2021).
Akiyama, H. et al. The evaluation study for social cognition measures in Japan: psychometric properties, relationships with social function, and recommendations. Asian J. Psychiatr. 95, 104003 (2024).
Hagiya, K. et al. Facial expression perception correlates with verbal working memory function in schizophrenia. Psychiatry Clin. Neurosci. 69, 773–781 (2015).
Corcoran, R., Mercer, G. & Frith, C. D. Schizophrenia, symptomatology and social inference: investigating ‘theory of mind’ in people with schizophrenia. Schizophr. Res. 17, 5–13 (1995).
Buck, B. et al. Improving measurement of attributional style in schizophrenia; a psychometric evaluation of the Ambiguous Intentions Hostility Questionnaire (AIHQ). J. Psychiatr. Res. 89, 48–54 (2017).
Kanie, A. et al. New instrument for measuring multiple domains of social cognition: construct validity of the Social Cognition Screening Questionnaire (Japanese version). Psychiatry Clin. Neurosci. 68, 701–711 (2014).
Bell, M. D., Fiszdon, J. M., Greig, T. C. & Wexler, B. E. Social attribution test-multiple choice (SAT-MC) in schizophrenia: comparison with community sample and relationship to neurocognitive, social cognitive and symptom measures. Schizophr. Res. 122, 164–171 (2010).
Pinkham, A. E., Harvey, P. D. & Penn, D. L. Social cognition psychometric evaluation: results of the final validation study. Schizophr. Bull. 44, 737–748 (2018).
Pinkham, A. E., Penn, D. L., Green, M. F. & Harvey, P. D. Social cognition psychometric evaluation: results of the initial psychometric study. Schizophr. Bull. 42, 494–504 (2016).
Hashimoto, N. et al. A pilot validation study of the Japanese translation of the Positive and Negative Syndrome Scale (PANSS). Asian J. Psychiatr. 54, 102210 (2020).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
Kaneda, Y. et al. Brief assessment of cognition in schizophrenia: validation of the Japanese version. Psychiatry Clin. Neurosci. 61, 602–609 (2007).
Keefe, R. S. E. et al. Norms and standardization of the Brief Assessment of Cognition in Schizophrenia (BACS). Schizophr. Res. 102, 108–115 (2008).
Mausbach, B. T. et al. Usefulness of the UCSD performance-based skills assessment (UPSA) for predicting residential independence in patients with chronic schizophrenia. J. Psychiatr. Res. 42, 320–327 (2008).
Sumiyoshi, C. et al. Utility of the UCSD Performance-based Skills Assessment-Brief Japanese version: discriminative ability and relation to neurocognition. Schizophr. Res. Cogn. 1, 137–143 (2014).
Schneider, L. C. & Struening, E. L. SLOF: a behavioral rating scale for assessing the mentally ill. Soc. Work. Res. Abstr. 19, 9–21 (1983).
Sumiyoshi, T. et al. Cognitive insight and functional outcome in schizophrenia; a multi-center collaborative study with the specific level of functioning scale-Japanese version. Schizophr. Res. Cogn. 6, 9–14 (2016).
Rocca, P. et al. Social cognition in people with schizophrenia: a cluster-analytic approach. Psychol. Med. 46, 2717–2729 (2016).
Benassi, M. et al. Using two-step cluster analysis and latent class cluster analysis to classify the cognitive heterogeneity of cross-diagnostic psychiatric inpatients. Front. Psychol. 11, (2020).
Schafer, J. L. Multiple imputation: a primer. Stat. Methods Med. Res. 8, 3–15 (1999).
Savla, G. N., Vella, L., Armstrong, C. C., Penn, D. L. & Twamley, E. W. Deficits in domains of social cognition in schizophrenia: a meta-analysis of the empirical evidence. Schizophr. Bull. 39, 979–992 (2013).
Green, M. F. & Nuechterlein, K. H. Should schizophrenia be treated as a neurocognitive disorder? Schizophr. Bull. 25, 309–319 (1999).
Halverson, T. F. et al. Pathways to functional outcomes in schizophrenia spectrum disorders: meta-analysis of social cognitive and neurocognitive predictors. Neurosci. Biobehav. Rev. 105, 212–219 (2019).
Galderisi, S. et al. Interplay among psychopathologic variables, personal resources, context-related factors, and real-life functioning in individuals with schizophrenia a network analysis. JAMA Psychiatry 75, 396–404 (2018).
Gould, F. et al. Self-assessment in schizophrenia: accuracy of evaluation of cognition and everyday functioning. Neuropsychology 29, 675–682 (2015).
Silberstein, J. M., Pinkham, A. E., Penn, D. L. & Harvey, P. D. Self-assessment of social cognitive ability in schizophrenia: association with social cognitive test performance, informant assessments of social cognitive ability, and everyday outcomes. Schizophr. Res. 199, 75–82 (2018).
Olsson, A.-K., Hjärthag, F. & Helldin, L. Overestimated function in patients with schizophrenia: a possible risk factor for inadequate support? Schizophr. Res. 206, 194–199 (2019).
Harris, M. T. & Rempfer, M. V. Profiles of self-evaluation as a metacognitive skill: an indicator of rehabilitation potential among people with schizophrenia. Psychiatr. Rehabil. J. 43, 308–317 (2020).
Harvey, P. D., Twamley, E. W., Pinkham, A. E., Depp, C. A. & Patterson, T. L. Depression in schizophrenia: associations with cognition, functional capacity, everyday functioning, and self-assessment. Schizophr. Bull. 43, 575–582 (2017).
Healey, K. M., Bartholomeusz, C. F. & Penn, D. L. Deficits in social cognition in first episode psychosis: a review of the literature. Clin. Psychol. Rev. 50, 108–137 (2016).
Shakeel, M. K. et al. Longitudinal changes in social cognition in individuals at clinical high risk for psychosis: an outcome based analysis. Schizophr. Res. 204, 334–336 (2019).
Mucci, A. et al. Factors associated with real-life functioning in persons with schizophrenia in a 4-year follow-up study of the Italian network for research on psychoses. JAMA Psychiatry 78, 550–559 (2021).
Tobe, M. et al. Characteristics of motivation and their impacts on the functional outcomes in patients with schizophrenia. Compr. Psychiatry 65, 103–109 (2016).
Saperstein, A. M. & Medalia, A. The role of motivation in cognitive remediation for people with schizophrenia. Curr. Top. Behav. Neurosci. 27, 533–546 (2016).
Lysaker, P. H. et al. Metacognitive function and fragmentation in schizophrenia: relationship to cognition, self-experience and developing treatments. Schizophr. Res. Cogn. 19, 100142 (2020).
Hotte-Meunier, A. et al. Effects of metacognitive training (MCT) on social cognition for schizophrenia spectrum and related psychotic disorders: a systematic review and meta-analysis. Psychol. Med. 54, 914–920 (2024).
Passerieux, C., Bulot, V., Hardy-Baylé, M.-C. & Roux, P. Assessing cognitive-related disability in schizophrenia: reliability, validity and underlying factors of the evaluation of cognitive processes involved in disability in schizophrenia scale. Disabil. Rehabil. 40, 1953–1959 (2018).
Bora, E., Yucel, M. & Pantelis, C. Cognitive endophenotypes of bipolar disorder: a meta-analysis of neuropsychological deficits in euthymic patients and their first-degree relatives. J. Affect. Disord. 113, 1–20 (2009).
Weightman, M. J., Air, T. M. & Baune, B. T. A review of the role of social cognition in major depressive disorder. Front. Psychiatry 5, 179 (2014).
Harvey, P. D. et al. Autism symptoms, depression, and active social avoidance in schizophrenia: association with self-reports and informant assessments of everyday functioning. J. Psychiatr. Res. 115, 36–42 (2019).
Durand, D. et al. Factors influencing self-assessment of cognition and functioning in schizophrenia: implications for treatment studies. Eur. Neuropsychopharmacol. 25, 185–191 (2015).
Gupta, M., Bassett, E., Iftene, F. & Bowie, C. R. Functional outcomes in schizophrenia: understanding the competence-performance discrepancy. J. Psychiatr. Res. 46, 205–211 (2012).
Uchino, T. et al. Associations of personality traits with the capacity-performance discrepancy of functional outcome in patients with schizophrenia. Neuropsychiatr. Dis. Treat. 15, 2869–2877 (2019).
Nemoto, T. et al. Social anxiety and negative symptoms as the characteristics of patients with schizophrenia who show competence–performance discrepancy in social functioning. Psychiatry Clin. Neurosci. 73, 394–399 (2019).
Acknowledgements
The present study was supported by a grant from the Japan Agency for Medical Research and Development (AMED) (grant number JP20dk0307092) to R.O., N.H., S.I., and T.N. This funding source had no role in the study design, data collection or analyses, in the decision to publish, or in the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
T.U., R.O., N.H., and T.N. designed the study and wrote the protocol. H.A., I.W., A.A., M.N., H.O., R.K., Y.Y., A.T., and S.I. were involved in the conceptualization of the study. T.U., H.A., A.A., and I.W. collected the data. T.U. undertook the statistical analysis and wrote the first draft of the manuscript. All the authors contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
T.U. and T.N. belong to the Department of Psychiatry and Implementation Science, Toho University Faculty of Medicine, and received funds from Nippon Life Insurance Company. Other authors have no known competing financial interests or personal relationships that could have influenced the work reported in this paper.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Uchino, T., Akiyama, H., Okubo, R. et al. Clinical subtypes of schizophrenia based on the discrepancies between objective performance on social cognition tasks and subjective difficulties in social cognition. Schizophr 10, 94 (2024). https://doi.org/10.1038/s41537-024-00515-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-024-00515-8