Abstract
Altered neural excitation/inhibition (E/I) balance has long been suspected as a potential underlying cause for clinical symptoms in schizophrenia (SZ). Recent methodological advancements linking the spectral slope (β) of neurophysiological recordings – such as them electroencephalogram (EEG) – to E/I ratio provided much-needed tools to better understand this plausible relationship. Importantly, most approaches treat E/I ratio as a stationary feature in a single scaling range. On the other hand, previous research indicates that this property might change over time, as well as it can express different characteristics in low- and high-frequency regimes. In line, in this study we analyzed resting-state EEG recordings from 30 patients with SZ and 31 healthy controls (HC) and characterized E/I ratio via β separately for low- (1–4 Hz) and high- (20–45 Hz) frequency regimes in a time-resolved manner. Results from this analysis confirmed the bimodal nature of power spectra in both HC and SZ, with steeper spectral slopes in the high- compared to low-frequency ranges. We did not observe any between-group differences in stationary (i.e., time-averaged) neural signatures, however, the temporal variance of β in the 20–45 Hz regime was significantly reduced in SZ patients when compared to HC, predominantly over regions corresponding to the dorsal attention network. Furthermore, this alteration was found correlated to positive clinical symptom scores. Our study indicates that altered E/I ratio dynamics are a characteristic trait of SZ that reflect pathophysiological processes involving the parietal and occipital cortices, potentially responsible for some of the clinical features of the disorder.
Similar content being viewed by others
Introduction
Schizophrenia (SZ) is one of the most common psychiatric disorders with a lifetime prevalence of about 1%1 and an increasing trend of incidence over the past 30 years2. The precise pathophysiology of SZ is yet unknown and thus SZ management (including diagnosis) mostly relies on assessment of clinical presentation3,4. The vast phenotypic heterogeneity5 observed in SZ, however, renders it immensely difficult to untangle the possible etiologies behind its various symptoms, and thus research focusing on identifying biomarkers that might help in better understanding its multifactorial pathomechanisms, progression monitoring or prognosis estimation is of central importance.
Power spectral abnormalities in the electroencephalogram (EEG) are extensively studied in SZ6; however, traditional research mostly focused on deviations in band limited power (BLP). Typically, BLP analyses assess neural activity in characteristic frequency regimes (e.g., 8–13 Hz for alpha) by integrating spectral power in the given regime. These approaches, however, most often disregard that neural power spectra are arguably composed of broadband fractal (\(1/{f}^{\beta }\)) ‘background activity’ with superimposed oscillatory peaks, and these components might represent different neural processes7,8 and thus should be treated separately. Indeed, separating fractal and oscillatory components of EEG power spectra appears to be relevant in SZ, too9. Furthermore, it has been proposed lately that the spectral slope (β) of the broadband component—i.e., the slope of the linear regression line fitted on log-transformed power over log-transformed frequency—can characterize the proportion of incoming excitatory and inhibitory activity, with flatter spectra indicating higher E/I ratio and vice versa10. This advancement might prove to be immensely relevant in SZ research, as altered excitatory NMDA11,12 and inhibitory GABA13,14 brain signaling has been consistently reported in SZ (for recent reviews, see e.g., refs. 15,16). Accordingly, abnormal excitation/inhibition (E/I) balance has been proposed as one of the underlying mechanisms of affected perceptual and cognitive functions in SZ17,18,19,20. Supporting this theory, by utilizing the concept outlined in ref. 10 Molina et al. 21 analyzed EEG recordings of SZ patients and revealed stronger inhibitory tone (i.e., steeper spectra) in contrast to healthy controls (HC), which was also correlated to attention and vigilance in a memantine stress test. Increased β was also identified in SZ during a self-referential task, and it was also found associated with negative symptom scores22.
Even though β is a promising novel biomarker in SZ given the apparent presence of aberrant E/I signaling, previous findings in the literature warrant further considerations. It has been shown that the power spectra of electrophysiological recordings can be characterized with different slopes in various frequency regimes, i.e., β can change with the frequency band8,23,24,25. This phenomenon is often referred to as bi- or multimodality9,24,26,27. Moreover, even though the relationship between E/I ratio and β proposed by Gao et al.10 was supported by multiple independent studies28,29, literature also indicates that this relationship is reversed for slow (<5 Hz) brain rhythms30,31. This aspect might be especially important in SZ; while in21 a single slope estimate was obtained from the 4–50 Hz domain, it was also shown recently that EEG spectra are bimodal in SZ with a flatter low-range and steeper high-range domain9. Finally, previous evidence suggests that neural activity can express multifractal characteristics in healthy population32 as well as in SZ33. The presence of multifractality indicates that the fractal scaling exponent of the dynamic process—that is equivalent to its spectral slope β34,35 – changes over time36. Accordingly, a single, global estimate might be insufficient to properly characterize the dynamics of neural E/I ratio in SZ and instead a time-resolved analysis characterizing both the mean and variance of β over time appears as a more reasonable approach.
Disentangling how E/I balance is affected and plausibly related to clinical symptoms in SZ is crucial for better understanding its pathophysiology and thus could open new venues in its diagnosis and management. Therefore, in line with the aforementioned notions, we analyzed EEG recordings of 30 patients with SZ and contrasted findings with those from 31 HC individuals in this cross-sectional, case-controlled study. We hypothesized that the power spectra of EEG recordings in SZ patients will be (i) bimodal and thus characterized with different scaling exponents in low- and high-frequency regimes, and that (ii) this property fluctuates over short time scales. We also expected to find (iii) steeper spectra (within-subject mean in time, μ) and altered temporal variability (within-subject standard deviation in time, σ) of β in SZ when compared to HC, indicating disrupted E/I balance. Finally, although there is indication on the role of E/I balance in SZ pathology, there is no clear consensus yet on how E/I ratio as captured via β might relate to the clinical appearance of SZ. Our goal was therefore also to (iv) gain novel insights on this aspect.
Materials and methods
Participants and clinical measures
A total of 38 patients with SZ and 39 HC individuals were enrolled in this study, of which 8-8 individuals were excluded from analysis due to low data quality (see below). Demographic and clinical information of the final study sample are presented in Table 1. There were no statistical differences between the two groups in terms of age, proportion of female/male individuals or years spent in education. The study was reviewed and approved by the Semmelweis University Regional and Institutional Committee of Science and Research Ethics (registration number: 197/2015, date: 10/05/2015). All participants provided written informed consent before enrollment in line with the Declaration of Helsinki.
Patients with SZ were recruited from the Department of Psychiatry and Psychotherapy (DPP), Semmelweis University, Budapest, Hungary, while HC participants were recruited from the general population of Budapest, Hungary. All patients met the criteria for SZ based on the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5)4. Psychiatric symptoms on the Positive and Negative Syndrome Scale (PANSS)37 were evaluated by trained psychiatrists. All data collection were carried out at the DPP between May 2016 and July 2018. Patients did not go through a medication washout period at the time of recordings and PANSS evaluation; detailed information on medication is shown in Table 1. No follow-up data was analyzed in this study.
Selection criteria for all participants included the following: no history of stroke, intellectual disability, epileptic seizure, substance dependence or abuse in the past three months, and no history of head injury with loss of consciousness for more than ten minutes. Furthermore, an exclusion criterion for patients was presence of any other mental disorder (according to DSM-5), and for healthy controls, presence of any mental disorder.
EEG recording, quality control and pre-processing
EEG in both cohorts was collected at 1000 Hz sampling rate using a 64-channel Neuroscan amplifier from standard 10-10 locations referenced to linked mastoids (M1/M2). Measurements were carried out in a dimly lit, sound-attenuated room. Participants were seated in an armchair and were instructed to remain idle but awake (resting state) with their eyes closed (EC) for two minutes. After collection, raw EEG recordings were visually inspected by two investigators independently. During the screening procedure, investigators were unaware of the data group label (HC or SZ) and they only contrasted outcomes once all steps were completed. Channels identified as noisy/bad (e.g., amplitude values consistently spanning outside ±100 µV range, flatline signal, aberrant power spectrum) in over 10 participants (channels AF7, AF8, AFz, F1, F2, TP7, TP8), as well as M1/M2 electrodes were removed from all recordings. Artifact free segments i.e., those absent of overt spikes or distributed high frequency or large amplitude noise were isolated in all recordings if they were marked as ‘clean’ by both experimenters independently, and a 30-s-long, continuous epoch from these was selected randomly for further analysis. This epoch length was decided upon as a reasonable compromise among the study sample, as being long enough for meaningful analysis of dynamics, yet it could be obtained in most study participants. In turn, those participants where such a segment could not be identified were excluded from further analysis, yielding a final sample of 31 HC and 30 SZ participants, with 55 channels each.
Data was preprocessed using Matlab (MathWorks, Nattick, MA) and the EEGLAB toolbox38. EEG was first downsampled to 256 Hz, then bandpass filtered between 0.5 and 100 Hz using a 4th order zero-phase Butterworth filter, with additional notch filters at 50, 100 and 150 Hz. Components of non-neural origin—such as muscle and heart activity—were removed using independent component analysis and the multiple artefact rejection algorithm (MARA) technique39,40 with default parameter settings. MARA is an automated, machine learning-based software plugin to EEGLAB that classifies independent components as artifacts (e.g., line noise, muscle activity or eye movements) or neural activity based on six temporal, spectral or spatial features41 and is widely utilized in the scientific literature. For more details on MARA, the reader is referred to the original publications39,40 or41. In the total study cohort, the average number of removed components was 26.55 ± 10.16 (~48.27%), while 24.94 ± 10.78 for the HC and 28.37 ± 9.25 for the SZ groups individually. These proportions of neuronal vs. artifactual components are in line with those expected39,40. There was no statistical difference between the number of rejected components between the HC and SZ groups (p = 0.1804, two-sample t-test). Finally, data was re-referenced to the common average reference.
Data analysis
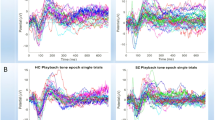
For characterizing neural E/I ratio, the spectral slopes were estimated using the irregular-resampling auto-spectral analysis (IRASA) technique42. IRASA decomposes the power spectrum into broadband fractal and superimposed oscillatory components, so that β can be estimated from the fractal component without the biasing effects of oscillatory (such as alpha) peaks42. It is important to note that despite the spectral slope being negative (\(1/{f}^{\beta }\)), according to convention43 we will use its absolute value throughout this manuscript, and therefore an increase in β will denote a steeper spectrum, and vice versa. In this work we employed a bimodal analysis approach, in that spectral slopes were estimated separately for low- and high-frequency regimes (see below); the process is illustrated on Fig. 1 from two representative regions in the HC (upper panels) and SZ (lower panels) groups. For details of the IRASA method and its theoretical background, please see the Supplementary Material and the original publications42,44.
In every panel, gray lines indicate the mixed (i.e., raw), while black lines the isolated fractal power spectra, respectively, with gray shaded areas denoting the standard error of the mean. Inset plots show corresponding isolated oscillatory spectra, obtained by subtracting the fractal from the raw (mixed) spectra. Boundaries of the two frequency regimes of interest (1–4 Hz and 20–45 Hz) are indicated with black dashed lines, while the range excluded from slope estimation (4–20 Hz) is marked in yellow. Blue and red dashed lines are illustrative and depict the power-law functions fitted on the fractal spectra in the low- and high-frequency regimes, respectively, with their corresponding slopes presented in matching colors. The panels illustrate that IRASA is effective in separating the fractal from the mixed power spectrum with minimal residual effect, and the utilized parameter settings and employed frequency regimes allow for unbiased estimates. In both groups low- and high-range slopes are roughly equal over F5 region, while the spectrum appears steeper in high- compared to low-range over P3. HC healthy control, SZ schizophrenia, IRASA irregular resampling auto-spectral analysis.
In the time-resolved analysis, the 30-s EEG segments were first divided into 8-second-long epochs with 75% overlap (yielding 12 windows). The window size was defined following previous recommendations as at this time scale EEG still can be treated as stationary yet providing ideal frequency resolution6, while a 75% window overlap—i.e., 25% step size – in dynamic fractal analysis has been proven effective in picking up changes in fractal scaling exponent despite introducing redundancy45,46. Then, IRASA was applied to each 8-s epoch to reconstruct the spectrum and separate fractal and oscillatory spectral components in the 1–45 Hz regime for all channels. Frequency resolution was set to 0.0625 Hz, and the rescaling factor h ranged from 1.1 to 2.6 in 0.1 increments, to avoid potential ‘smearing’ effects around the alpha peak (see Supplementary Material in ref. 9). Spectral slopes were estimated in the 1–4 Hz (\({\beta }_{{lo}}\)) and 20–45 Hz (\({\beta }_{{hi}}\)) ranges independently via ordinary least squares (OLS) linear regression of log-transformed fractal power on log-transformed frequency (see Fig. 1). These frequency regimes were selected in line with previous studies29,30 and considering the filtering effects introduced by up- and downsampling during IRASA analysis (see9 and its Supplementary Material). For control purposes, slope estimates were obtained from the broadband 1–45 Hz spectra, too (\({\beta }_{{bb}}\)).
To reduce dimensionality and improve physiological interpretability, channels were grouped according to established resting-state networks (RSNs) of the brain47. In line with our previous approaches9,48, channels were assigned to the RSN whose activity they most likely register based on the work of Giacometti and colleagues49. Out of the 7 RSNs proposed by Yeo and coworkers47, we isolated the visual network (VN), the somatomotor network (SM), the dorsal attention network (DA), the frontoparietal network (FP) and the default mode network (DMN), while channels corresponding to the ventral attention and limbic networks were pooled (VAL) due to limitations in spatial resolution. The 55-channel montage and RSN-channel assignment is illustrated on Fig. 2 using the BrainNet Viewer software50; spectral slope estimates were averaged over channels belonging to RSNs for each time window. Finally, for every participant, neural indices (RSN-wise) were characterized by their mean and standard deviation over time. These will be indicated by \(\mu (\cdot )\) and \(\sigma (\cdot )\), respectively, e.g., the temporal standard deviation of high-range spectral slope will be denoted as \(\sigma ({\beta }_{{hi}})\).
The six RSNs include the visual network (VN, 12 channels), the somatomotor network (SM, 10 channels), the dorsal attention network (DA, 9 channels), the combined ventral attention- and limbic networks (VAL, 12 channels), the frontoparietal network (6 channels) and the default mode network (6 channels). Channels correspondence to different RSNs are indicated with various colors (VN: purple; SM: blue; DA: green; VAL: gray; FP: orange and DMN: red).
Statistical analysis and relationships with clinical scores
The obtained neurophysiological indices were first tested for normality using the Lilliefors test, then between group differences were assessed via two-sample t-tests in case of normal distributions, while Mann-Whitney U tests otherwise. The bimodal nature of the spectra was assessed in the SZ and HC groups independently by contrasting \(\mu ({\beta }_{{lo}})\) and \(\mu ({\beta }_{{hi}})\) values with paired t-tests or Wilcoxon signed rank tests, depending on data normality. Note that this analysis was carried out for each channel individually. For all variables, outcomes were adjusted for multiple comparisons using the false discovery rate (FDR) method of Benjamini and Hochberg51 at a statistical significance level of 0.05. Finally, neural indices of the SZ group that indicated significant between-group difference were contrasted with general (GEN), negative (NEG), positive (POS) and summed (SUM) PANSS symptom scores. In that, first the confounding effects of age, sex, years in education, disease duration and CPZ were regressed out from all variables using multiple linear regression. Then, the Pearson or Spearman correlation coefficient (depending on data normality) was computed between the neural indices and symptom scores. Notably, correlational analyses were performed only for those neural indices where significant between-group difference was found. Given the exploratory nature of this analysis, outcomes were not adjusted for multiple comparisons.
Results
Bimodality of power spectra
In both study groups, EEG spectra were steeper in the high- compared to the low-frequency regime over the majority of channels (Fig. 3). Precisely, \({\mu (\beta }_{{hi}})\) was higher than \(\mu ({\beta }_{{lo}})\) over 36 and 35 out of 55 cortical locations in the HC and SZ groups, respectively. This bimodality could be observed most prominently over parieto-occipital and central regions, while EEG spectra over temporal-frontal brain regions were found rather unimodal (Fig. 3, right). These results – in accordance with9—confirm that EEG spectra should be treated as bimodal in the 1–45 Hz range with steeper slopes characteristic of high- compared to low-frequency regimes, and this property appears to be mostly preserved in SZ when compared to HC.
Lower \(\mu ({\beta }_{{lo}})\) values (left column) compared to \(\mu ({\beta }_{{hi}})\) (middle column) are apparent in both study groups. The right column shows the difference (\(\mu \left({\beta }_{{hi}}\right)-\mu ({\beta }_{{lo}})\), with asterisk symbols denoting statistically significant bimodality (p < 0.05, adjusted) over most of the cortex with a parieto-occipital dominance.
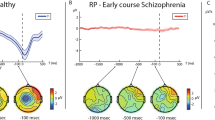
Reduced temporal variance of high-range spectral slope in Schizophrenia
We did not find any differences between HC and SZ in the mean spectral slopes in either frequency regimes following FDR-adjustment (see also Fig. 3). However, in terms of temporal variability, \(\sigma ({\beta }_{{hi}})\) was found generally reduced in the SZ population (Fig. 4). This difference was most apparent over the parieto-occipital cortex, with another cluster over the left frontal lobe. RSN-wise statistical analysis confirmed significantly lower \(\sigma ({\beta }_{{hi}})\) in SZ in the DA network (mean 0.1264 vs. 0.0955, t59 = 2.7353, p = 0.0082), while this difference was exhibited as a tendency for VN (mean 0.1299 vs. 0.1004, t59 = 2.3317, p = 0.0232, non-significant after FDR-adjustment) and SM(median 0.0947 vs. 0.0728, Z = 2.0557, p = 0.0398, non-significant after FDR-adjustment). The same pattern was also exhibited by the rest of the RSNs, namely, VAL (median 0.1047 vs. 0.0864, Z = 1.5797, p = 0.1142, non-significant), FP (mean 0.1297 vs. 0.1064, t59 = 1.6672, p = 0.1008, non-significant) and DMN (mean 0.1398 vs. 0.1134, t59 = 1.9373, p = 0.0575, non-significant), although not reaching statistical significance. In comparison, no significant between-group differences were identified for \({\beta }_{{lo}}\) either in terms of mean or temporal variability (see Supplementary Fig. S1 for the latter). Note that also no significant between-group differences were found for \({\beta }_{{bb}}\) at all. Accordingly, these results imply that E/I ratio has similar baseline level in SZ, while its temporal variability is reduced compared to what is observed in the HC population.
The upper left and right panels show the topology of \(\sigma ({\beta }_{{hi}})\) in HC and SZ, respectively. The lower panel shows resting-state network (RSN)-wise analysis of \(\sigma ({\beta }_{{hi}})\), with black, straight horizontal line and asterisk indicating significant between-group difference (p < 0.05, adjusted). In all box plots, continuous and dotted lines indicate the mean and median, respectively, the rectangular area denotes the inter-quartile range, horizontal whiskers indicate 5th and 95th percentile, and circles show the individual samples. Note that black, horizontal dotted lines indicate between group differences that were rendered non-significant by multiple comparisons adjustment. \({\beta }_{{hi}}\): high-range (20–45 Hz) spectral exponent; \(\sigma ({\beta }_{{hi}})\): standard deviation of \({\beta }_{{hi}}\) over time.
Correlations with clinical symptom scores
Finally, we computed if the observed between-group difference—in \(\sigma ({\beta }_{{hi}})\) over the DA network – were associated with PANSS scores in the SZ group. An anticorrelated relationship between \(\sigma ({\beta }_{{hi}})\) of DA and positive PANSS scores could be identified; however, assumptions of OLS regression were not satisfied (normality of the residuals in particular) and thus we characterized this relationship via Spearman correlation coefficient (r = –0.3989, p = 0.0298) after adjusting for confounding variables (Fig. 5).
Both variables were adjusted for the plausible confounding effects of age, sex, years of education, disease duration and chlorpromazine daily equivalent dose. The straight red line denotes the ordinary least squares regression line, which only serves illustrative purposes. \(\sigma ({\beta }_{{hi}})\): standard deviation of high-range (20–45 Hz) spectral exponent over time; PANSS positive and negative syndrome scale.
Discussion
Neural markers of SZ derived from EEG data have been a subject of research interest for decades6,52. Previous analyses revealed mostly consistent abnormalities in SZ in terms of resting-state EEG, such as increased delta (1–4 Hz) and/or theta (4–7 Hz) BLP over frontal regions53,54, globally reduced alpha (8–13 Hz) BLP53 or abnormalities in gamma (30–80 Hz) synchronization55. However, most of these efforts did not take into consideration of the broadband spectral characteristics and \(1/{f}^{\beta }\) nature of neural activity. Our presented results provide important novel insights on these aspects.
Altered neural E/I ratio has long been hypothesized as one of the key etiological factors of SZ3,15, supported by both molecular12,56, electrophysiological21 or transcranial magnetic stimulation20 evidence. The proposal of β as a non-invasive marker for E/I ratio10 and simultaneously developed novel analysis strategies42,57,58 led to a rapid upsurge of interest in E/I phenomena recently; however, such studies investigating SZ are yet scarce21,59. Our goal was to address this knowledge gap with notable key considerations in mind. The hypothesis that an increased (decreased) E/I ratio results in the reduction (increase) of β has been confirmed empirically by multiple independent studies using pharmaceutical interventions21,29,31, optogenetic manipulation28, computer simulations60 or a priori hypotheses based on histological structure10. Nonetheless, while the model of Gao and coworkers indicated that this result holds mainly in the ~20–50 Hz frequency regime, the range of estimation in practice varies broadly among studies. This may be concerning according to the results of Becker and colleagues30, which implied that the relationship between β and inhibitory tone is reversed in the low-frequency (<5 Hz) regime. Even though that study used spontaneous resting alpha BLP as a proxy for inhibition61,62, Muthukumarshawamy and Lilley31 showed that increased GABA-ergic tone via administering the GABA reuptake inhibitor Tiagabine resulted in simultaneous decrease in low- (<2.5 Hz) and increase in high-range (>20 Hz) spectral slopes. This taken together with previous reports on bimodal nature of EEG spectra8,9,23,24 warrants the low- and high-frequency regimes of the power spectrum to be treated separately. Our results support this notion: the bimodal analysis not only confirmed significant difference of \({\beta }_{{lo}}\) and \({\beta }_{{hi}}\) but also indicated that dynamics governing only the latter appear to be affected in SZ. In contrast, when we characterized spectra with a single broadband slope estimate, no group-level differences were identified. We also did not observe the steeper grand-averaged EEG spectrum in SZ as reported in ref. 21; however, in that study the authors analyzed data collected during an auditory oddball paradigm and slopes were estimated from the 4–50 Hz range, which might explain this discrepancy63.
In accordance with our previous findings9 on an independent HC and SZ-patient cohort64, the extent of bimodality was stronger over parieto-occipital regions, while less prominent or non-existent over frontal areas. As these regions are also normally expected to exhibit stronger resting alpha power in eyes-closed state65, this might raise the possibility that the presence of a prominent alpha peak confounded the results via spectral leakage. Our analysis pipeline was designed to counter this possibility in IRASA employing Hanning windowing to reduce leakage as well as we increased the set of rescaling factors to 1.1:0.1:2.6 from the recommended standard 1.1:0.05:1.9 range42. While Fig. 1 indicates that with these parameter settings the isolated fractal spectra were not compromised in the employed frequency regimes, we cannot rule out the possibility of an interplay between resting alpha power and the slope of the fractal spectrum. In fact, it is important to emphasize that such a pattern is likely to emerge along physiological—instead of methodological – principles. Namely, it is argued that alpha power is a proxy for inhibitory tone61,62, which also served as the theoretical foundation for the analysis conducted by Becker and colleagues30. In this context, larger alpha power and steeper slope in the higher frequency regime would confluently indicate stronger inhibitory tone, and therefore our findings regarding \(\sigma ({\beta }_{{hi}})\) coinciding with areas with more prominent alpha activity might very well reflect the same neural phenomenon through different means. A more elaborate investigation of this question is possible by a detailed analysis of ‘traditional’ spectral measures (such as BLP), which we believe is beyond the scope of this paper; however, our plan is to publish those outcomes shortly in a companion article.
The lack of between-group difference in \(\mu ({\beta }_{{lo}})\) and \(\mu ({\beta }_{{hi}})\) values implies that overall E/I balance is maintained in SZ on longer time scales. As noted, this might appear to be in contrast with previous, similar literature21,22; however, these studies analyzed EEG collected during task performance and not in resting-state. Indeed, our previous bimodal analysis of an independent resting-state EEG dataset also indicated no difference in \(\mu ({\beta }_{{lo}})\) and \(\mu ({\beta }_{{hi}})\) between HC and SZ groups9. Our central result presented here shows that this breaks down on shorter time scales: SZ patients expressed reduced temporal fluctuations in \({\beta }_{{hi}}\) when compared to HC individuals. Precisely, reduced \(\sigma ({\beta }_{{hi}})\) was most prominent over the parieto-occipital cortices (see Fig. 4), regions likely representing the activity of the DA network49. Even though SZ-related EEG abnormalities are more commonly found over the frontal and temporal lobes52, the importance of the parietal cortex regarding attention, working memory and other cognitive domain deficits in SZ has been emphasized66,67. Our results are in line with the latter notion, especially with21 linking E/I ratio to attentional and vigilance deficits in SZ. Therefore, investigating variability of EEG spectral power and E/I ratio measures in attentional and working memory tasks in SZ appears as an important future research direction, for which our presented analytical approach could prove valuable. Additionally, reduced \(\sigma ({\beta }_{{hi}})\) may also imply loss of multifractality in neural dynamics. Multifractality often emerges in physiological systems as a result of antagonistic feedback mechanisms68 and its loss can indicate the involvement of either, or both components36,69. In terms of neural circuits, this might reflect the disruption of large-scale excitatory-inhibitory feedback loops70, which can be expected in SZ. Better understanding of this phenomenon can bring novel insights on the pathophysiology of SZ and its symptoms, and therefore it is one of our key goals in the future.
Our analysis revealed an association between the investigated neural indices and clinical symptoms; however, given the exploratory nature of these results—as outcomes were not adjusted for multiple comparisons—we must exercise caution regarding their interpretation. Precisely, E/I dynamics were negatively correlated with positive PANSS scores in the DA network (Fig. 5). The pathophysiology of positive symptoms in SZ is not yet fully understood and thus is a subject of intense research71,72. As indicated previously, the parietal cortex was rather associated with cognitive deficits in SZ66,67, in line with the plausible affectedness of the DA network. Neural E/I ratio have been linked to multiple cognitive domains recently in various conditions such as aging or multiple sclerosis29,73,74,75, which tentatively projects that β-based E/I analysis could be helpful in better understanding its cognitive disfunction in SZ. On the other hand, positive symptoms can be well-managed with antidopaminergic medication in roughly two-thirds of cases76, which raises the possibility that \({\beta }_{{hi}}\) fluctuations in the DA network might be related to the activity of dopaminergic system. On the other hand, it is important to note that patients were on medication during the time of the assessments, and therefore it is possible that outcomes are confounded by the variability in therapy response to different pharmaceuticals. While we cannot confirm or rule out this possibility based on the current study sample, this is an important future direction that might yield valuable novel insights on the neurobiology of SZ, but also on identifying neural features that can be utilized to estimate therapy response. Nevertheless, our current dataset and experimental design could not allow us to provide further explanations for these associations, however, we consider it as an important direction to pursue in the future, such as investigating how the spectral slope is modulated by antipsychotic medication77 or how it is related to performance in cognitive tasks requiring spatial attention and goal-directed behavior78 in patients with SZ.
While our study provides novel insights into affected neural dynamics in SZ, it also has certain limitations. Analyses were performed on resting-state data, and thus the relevance of the identified alterations in terms of cognitive deficits could not be investigated and requires future research. This issue is even more relevant in light of recent reports suggesting that the mean spectral slope might indicate alterations in task-response rather than resting activity in SZ21,22. It is important to note that our characterization of EEG spectral dynamics is likely incomplete given that it was obtained from 30 s of continuous activity. This was a technical limitation of our dataset, as longer continuous segments could only have been obtained from a sufficiently smaller number of participants, thus reducing statistical robustness. On the other hand, the known scale invariant property of neural activity suggests relevant dynamic patterns on time scales beyond 30 s27,33, which warrants further research. Also, EEG data was evaluated in the sensor space and thus we cannot draw exact conclusions on the role of well-defined brain regions. Although the RSN-level analysis might provide more robust insights on large-scale brain regional activity, our reported results will need to be confirmed with more appropriate analytical approaches such as source activity reconstruction by utilizing neuroimaging with precise anatomical localization (e.g., functional magnetic resonance imaging). The specificity of the identified neural correlates remains another open question in terms of SZ subtypes or neuropsychiatric conditions with an overlapping symptom profile (e.g., bipolar disorder or autism spectrum disorder). Even though during the correlation analyses we regressed out CPZ, our SZ population was heterogenous in terms of medication. Different pharmaceuticals commonly used in SZ treatment can affect EEG spectral properties in varying ways79,80,81, which in turn might had have an influence on the outcomes. According to recent synthesis, it is yet largely unknown how antipsychotic treatment might affect spectral characteristics linked to the E/I ratio81, and therefore while we cannot completely rule out that pharmacotherapy had an influence on the observed EEG alterations in SZ, this is an important research question that we intend to pursue in the future. Also, SZ disease duration varied in a broad range (from 0 to 28 years). It has been shown that early-stage and chronic SZ can exhibit different EEG signatures82, which likely introduced additional variability in our results. From the cross-sectional, resting-state design of this study it also follows that our biological understanding of EEG-symptom correlations remains elusive. Even though \(\sigma ({\beta }_{{hi}})\) was meaningful in revealing between-group differences, we did not test explicitly if this truly indicates the presence – or in case of SZ, the loss of – multifractal dynamics in neural activity (e.g., as in refs. 48,83,84). This remains an open question but appears as a research avenue worth exploring in the future. Finally, results regarding the E/I ratio are commonly linked to glutamatergic/GABA-ergic activity, however altered functioning of the dopaminergic system is also evident in SZ85. In fact, recent notions imply the joint affectedness of dopamine-, GABA- and glutamatergic systems resulting in E/I imbalance in SZ86. Previous literature also reported on the effects of dopaminergic activity and medication on \(1/{f}^{\beta }\) brain dynamics87 and thus sfuture efforts should make an attempt in synthesizing similar analysis outcomes with the dopamine hypothesis in SZ16.
In summary, we identified diminished fluctuations in high-frequency spectral in SZ when compared to HC, demonstrating that short-term temporal variability of neural E/I ratio can be distinctive and associated with clinical symptoms even if the baseline of E/I balance is maintained over longer time scales. Additionally, we addressed key methodological issues when inferring E/I ratio from the slope of EEG power spectra, confirming the relevance of assessing the power spectrum in a bimodal manner. Even though the work presented here can be considered first of its kind and thus exploratory in some regards, it provides novel and valuable insights into the neural signatures of SZ and raises questions hopefully facilitating future research in the field.
Data availability
Anonymized data (including raw EEG recordings, demographic and clinical information) generated throughout this study is available in a public Zenodo repository titled “Resting-state EEG, clinical, and demographics data from schizophrenia patients and age-matched healthy controls” at https://zenodo.org/records/14808296 (https://doi.org/10.5281/zenodo.14808295).
Code availability
All data analyses were carried out via Matlab (version 2023b) utilizing the EEGLAB toolbox38 (version 2020.0) along with custom analysis codes. Matlab codes developed and used for analyzing the data and visualizing outcomes (along with pre-processed EEG) are provided in a public GitHub repository at https://github.com/samuelracz/schizophrenia_EI_variability.
References
McGrath, J. et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol. Rev. 30, 67–76 (2008).
Solmi, M. et al. Incidence, prevalence, and global burden of schizophrenia - data, with critical appraisal, from the Global Burden of Disease (GBD) 2019. Mol. Psychiatry 28, 5319–5327 (2023).
McCutcheon, R. A., Reis Marques, T. & Howes, O. D. Schizophrenia-an overview. JAMA Psychiatry 77, 201–210 (2020).
American Psychiatric Association, D. and A.P. Association, Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Vol. 5 (American Psychiatric Association Washington, DC, 2023).
Habtewold, T. D. et al. A systematic review and narrative synthesis of data-driven studies in schizophrenia symptoms and cognitive deficits. Transl. Psychiatry 10, 244 (2020).
Boutros, N. N. et al. The status of spectral EEG abnormality as a diagnostic test for schizophrenia. Schizophr. Res. 99, 225–237 (2008).
He, B. Y. J. Scale-free brain activity: past, present, and future. Trends Cogn. Sci. 18, 480–487 (2014).
He, B. J. et al. The temporal structures and functional significance of scale-free brain activity. Neuron 66, 353–369 (2010).
Racz, F. S. et al. Separating scale-free and oscillatory components of neural activity in schizophrenia. Brain Behav. 11, e02047 (2021).
Gao, R., Peterson, E. J. & Voytek, B. Inferring synaptic excitation/inhibition balance from field potentials. NeuroImage 158, 70–78 (2017).
Braun, U. et al. Dynamic brain network reconfiguration as a potential schizophrenia genetic risk mechanism modulated by NMDA receptor function. Proc. Natl Acad. Sci. 113, 12568–12573 (2016).
Yang, G. J. et al. Functional hierarchy underlies preferential connectivity disturbances in schizophrenia. Proc. Natl Acad. Sci. 113, E219–E228 (2016).
Hyde, T. M. et al. Expression of GABA signaling molecules KCC2, NKCC1, and GAD1 in cortical development and schizophrenia. J. Neurosci. 31, 11088–11095 (2011).
Curley, A. A. et al. Cortical deficits of glutamic acid decarboxylase 67 expression in schizophrenia: clinical, protein, and cell type-specific features. Am. J. Psychiatry 168, 921–929 (2011).
Liu, Y. et al. A selective review of the excitatory-inhibitory imbalance in schizophrenia: underlying biology, genetics, microcircuits, and symptoms. Front. Cell Dev. Biol. 9, 664535 (2021).
Howes, O. D. & Shatalina, E. Integrating the neurodevelopmental and dopamine hypotheses of schizophrenia and the role of cortical excitation-inhibition balance. Biol. Psychiatry 92, 501–513 (2022).
Lisman, J. Excitation, inhibition, local oscillations, or large-scale loops: what causes the symptoms of schizophrenia? Curr. Opin. Neurobiol. 22, 537–544 (2012).
Starc, M. et al. Schizophrenia is associated with a pattern of spatial working memory deficits consistent with cortical disinhibition. Schizophr. Res. 181, 107–116 (2017).
Anticevic, A. & Lisman, J. How can global alteration of excitation/inhibition balance lead to the local dysfunctions that underlie schizophrenia? Biol. Psychiatry 81, 818–820 (2017).
Lányi, O. et al. Excitation/inhibition imbalance in schizophrenia: a meta-analysis of inhibitory and excitatory TMS-EMG paradigms. Schizophrenia 10, 56 (2024).
Molina, J. L. et al. Memantine effects on electroencephalographic measures of putative excitatory/inhibitory balance in schizophrenia. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 5, 562–568 (2020).
Northoff, G. et al. The self and its prolonged intrinsic neural timescale in schizophrenia. Schizophr. Bull. 47, 170–179 (2021).
Miller, K. J. et al. Power-law scaling in the brain surface electric potential. PLoS Comput. Biol. 5, e1000609 (2009).
Nagy, Z. et al. Decomposing multifractal crossovers. Front. Physiol. 8, 533 (2017).
Racz, F. S. et al. Alternative EEG pre-processing pipelines can lead to conflicting conclusions regarding cortical excitation/inhibition ratio. Preprint at bioRxiv https://www.biorxiv.org/content/10.1101/2024.11.08.622698v1 (2024).
Eke, A., Herman, P. & Hajnal, M. Fractal and noisy CBV dynamics in humans: influence of age and gender. J. Cereb. Blood Flow. Metab. 26, 891–898 (2006).
Mukli, P. et al. Impact of healthy aging on multifractal hemodynamic fluctuations in the human prefrontal cortex. Front. Physiol. 9, 1072 (2018).
Chini, M. et al. An increase of inhibition drives the developmental decorrelation of neural activity. eLife 11, e78811 (2022).
Akbarian, F. et al. The spectral slope as a marker of excitation/inhibition ratio and cognitive functioning in multiple sclerosis. Hum. Brain Map. 44, 5784–5794 (2023).
Becker, R., Van de Ville, D. & Kleinschmidt, A. Alpha oscillations reduce temporal long-range dependence in spontaneous human brain activity. J. Neurosci. 38, 755–764 (2018).
Muthukumaraswamy, S. D. & Liley, D. T. J. 1/f electrophysiological spectra in resting and drug-induced states can be explained by the dynamics of multiple oscillatory relaxation processes. NeuroImage 179, 582–595 (2018).
Dutta, S. et al. Multifractal parameters as an indication of different physiological and pathological states of the human brain. Phys. A 396, 155–163 (2014).
Racz, F. S. et al. Multifractal and entropy-based analysis of delta band neural activity reveals altered functional connectivity dynamics in schizophrenia. Front. Syst. Neurosci. 14, 49 (2020).
Eke, A. et al. Physiological time series: distinguishing fractal noises from motions. Pflug. Arch. Eur. J. Physiol. 439, 403–415 (2000).
Mandelbrot, B. B. & Van Ness, J. W. Fractional Brownian motions, fractional noises and applications. SIAM Rev. 10, 422–437 (1968).
Ivanov, P. C. et al. Multifractality in human heartbeat dynamics. Nature 399, 461–465 (1999).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
Delorme, A. & Makeig, S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods 134, 9–21 (2004).
Winkler, I., Haufe, S. & Tangermann, M. Automatic classification of artifactual ICA-components for artifact removal in EEG signals. Behav. Brain Funct. 7, 30 (2011).
Winkler, I. et al. Robust artifactual independent component classification for BCI practitioners. J. Neural Eng. 11, 035013 (2014).
Gabard-Durnam, L. J. et al. The Harvard Automated Processing Pipeline for Electroencephalography (HAPPE): standardized processing software for developmental and high-artifact data. Front. Neurosci. 12, 97 (2018).
Wen, H. G. & Liu, Z. M. Separating fractal and oscillatory components in the power spectrum of neurophysiological signal. Brain Topogr. 29, 13–26 (2016).
Eke, A. et al. Fractal characterization of complexity in temporal physiological signals. Physiol. Meas. 23, 1–38 (2002).
Racz, F. S. et al. Multiple-resampling cross-spectral analysis: an unbiased tool for estimating fractal connectivity with an application to neurophysiological signals. Front. Physiol. 13, 817239 (2022).
Hartmann, A. et al. Real-time fractal signal processing in the time domain. Phys. A 392, 89–102 (2013).
Kaposzta, Z. et al. Real-time algorithm for detrended cross-correlation analysis of long-range coupled processes. Front. Physiol. 13, 817268 (2022).
Yeo, B. T. T. et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J. Neurophysiol. 106, 1125–1165 (2011).
Racz, F. S. et al. Multifractal and entropy analysis of resting-state electroencephalography reveals spatial organization in local dynamic functional connectivity. Sci. Rep. 9, 13474 (2019).
Giacometti, P., Perdue, K. L. & Diamond, S. G. Algorithm to find high density EEG scalp coordinates and analysis of their correspondence to structural and functional regions of the brain. J. Neurosci. Methods 229, 84–96 (2014).
Xia, M. R., Wang, J. H. & He, Y. BrainNet viewer: a network visualization tool for human brain connectomics. PLoS ONE 8, e68910 (2013).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate - a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B-Stat. Methodol. 57, 289–300 (1995).
Perrottelli, A. et al. EEG-based measures in at-risk mental state and early stages of schizophrenia: a systematic review. Front. Psychiatry 12, 653642 (2021).
Clementz, B. A. et al. Resting Eeg in first-episode schizophrenia-patients, bipolar psychosis patients, and their first-degree relatives. Psychophysiology 31, 486–494 (1994).
Begic, D. et al. Quantitative electroencephalography in schizophrenia and depression. Psychiatr. Danub 23, 355–362 (2011).
Reilly, T. J. et al. Gamma band oscillations in the early phase of psychosis: a systematic review. Neurosci. Biobehav. Rev. 90, 381–399 (2018).
Lewis, D. A. et al. Cortical parvalbumin interneurons and cognitive dysfunction in schizophrenia. Trends Neurosci. 35, 57–67 (2012).
Donoghue, T. et al. Parameterizing neural power spectra into periodic and aperiodic components. Nat. Neurosci. 23, 1655–U288 (2020).
Bruining, H. et al. Measurement of excitation-inhibition ratio in autism spectrum disorder using critical brain dynamics. Sci. Rep. 10, 9195 (2020).
Abbasi, S. et al. Increased noise relates to abnormal excitation-inhibition balance in schizophrenia: a combined empirical and computational study. Cereb. Cortex 33, 10477–10491 (2023).
Martinez-Canada, P. et al. Combining aperiodic 1/f slopes and brain simulation: an EEG/MEG proxy marker of excitation/inhibition imbalance in Alzheimer’s disease. Alzheimers Dement. 15, e12477 (2023).
Klimesch, W., Sauseng, P. & Hanslmayr, S. EEG alpha oscillations: the inhibition-timing hypothesis. Brain Res. Rev. 53, 63–88 (2007).
Jensen, O. & Mazaheri, A. Shaping functional architecture by oscillatory alpha activity: gating by inhibition. Front. Hum. Neurosci. 4, 186 (2010).
Gyurkovics, M. et al. Stimulus-induced changes in 1/f-like background activity in EEG. J. Neurosci. 42, 7144–7151 (2022).
Olejarczyk, E. & Jernajczyk, W. Graph-based analysis of brain connectivity in schizophrenia. PLoS ONE 12, e0188629 (2017).
Barry, R. J. et al. EEG differences between eyes-closed and eyes-open resting conditions. Clin. Neurophysiol. 118, 2765–2773 (2007).
Danckert, J., Saoud, M. & Maruff, P. Attention, motor control and motor imagery in schizophrenia: implications for the role of the parietal cortex. Schizophr. Res. 70, 241–261 (2004).
Hahn, B. et al. Posterior parietal cortex dysfunction is central to working memory storage and broad cognitive deficits in schizophrenia. J. Neurosci. 38, 8378–8387 (2018).
Ivanov, P. et al. Stochastic feedback and the regulation of biological rhythms. Europhys. Lett. 43, 363–368 (1998).
Amaral, L. A. N. et al. Behavioral-independent features of complex heartbeat dynamics. Phys. Rev. Lett. 86, 6026–6029 (2001).
Poil, S. S. et al. Critical-state dynamics of avalanches and oscillations jointly emerge from balanced excitation/inhibition in neuronal networks. J. Neurosci. 32, 9817–9823 (2012).
Begue, I., Kaiser, S. & Kirschner, M. Pathophysiology of negative symptom dimensions of schizophrenia - Current developments and implications for treatment. Neurosci. Biobehav. Rev. 116, 74–88 (2020).
Marzouk, T. et al. Transcranial magnetic stimulation for positive symptoms in schizophrenia: a systematic review. Neuropsychobiology 79, 384–396 (2020).
Dave, S., Brothers, T. A. & Swaab, T. Y. 1/f neural noise and electrophysiological indices of contextual prediction in aging. Brain Res. 1691, 34–43 (2018).
Czoch, A. et al. Resting-state fractal brain connectivity is associated with impaired cognitive performance in healthy aging. Geroscience 46, 473–489 (2023).
Kaposzta, Z. et al. Fingerprints of decreased cognitive performance on fractal connectivity dynamics in healthy aging. Geroscience 46, 713–736 (2023).
Conley, R. R. & Kelly, D. L. Management of treatment resistance in schizophrenia. Biol. Psychiatry 50, 898–911 (2001).
Jackson, A. & Seneviratne, U. EEG changes in patients on antipsychotic therapy: a systematic review. Epilepsy Behav. 95, 1–9 (2019).
Machner, B. et al. Resting-state functional connectivity in the dorsal attention network relates to behavioral performance in spatial attention tasks and may show task-related adaptation. Front. Hum. Neurosci. 15, 757128 (2021).
Hyun, J., Baik, M. J. & Kang, U. G. Effects of psychotropic drugs on quantitative EEG among patients with schizophrenia-spectrum disorders. Clin. Psychopharmacol. Neurosci. 9, 78 (2011).
Aiyer, R., Novakovic, V. & Barkin, R. L. A systematic review on the impact of psychotropic drugs on electroencephalogram waveforms in psychiatry. Postgrad. Med. 128, 656–664 (2016).
De Pieri, M. et al. Pharmaco-EEG of antipsychotic treatment response: a systematic review. Schizophrenia 9, 85 (2023).
Sponheim, S. R. et al. Resting EEG in first-episode and chronic schizophrenia. Psychophysiology 31, 37–43 (1994).
Racz, F. S. et al. Multifractal dynamics of resting-state functional connectivity in the prefrontal cortex. Physiol. Meas. 39, 024003 (2018).
Racz, F. S. et al. Multifractal dynamic functional connectivity in the resting-state brain. Front. Physiol. 9, 1704 (2018).
Goto, Y. & Grace, A. A. The dopamine system and the pathophysiology of schizophrenia: a basic science perspective. Int. Rev. Neurobiol. 78, 41–68 (2007).
Wada, M. et al. Dopaminergic dysfunction and excitatory/inhibitory imbalance in treatment-resistant schizophrenia and novel neuromodulatory treatment. Mol. Psychiatry 27, 2950–2967 (2022).
Stylianou, O. et al. Scale-free functional brain networks exhibit increased connectivity, are more integrated and less segregated in patients with Parkinson’s disease following dopaminergic treatment. Fractal Fract. 6, 737 (2022).
Acknowledgements
This research was supported by the National Research, Development and Innovation Office (OTKA FK 138385 and OTKA PD 146424), as well as the Ministry of Innovation and Technology of Hungary from the National Research, Development and Innovation Fund, financed under the TKP2021-EGA-25 funding scheme.
Funding
Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Contributions
F.S.R. designed the analytical pipeline, performed data screening, pre-processing and analysis, results interpretation, and wrote the initial draft of the manuscript. K.F., H.M., and Z.F. contributed to electrophysiological and clinical data collection and study conceptualization. M.B. contributed to data collection, screening and pre-processing. P.M. contributed to developing the analytical pipeline and interpreting results. G.C. conceptualized the study and provided oversight and guidance over data collection, analysis and all other study aspects. All authors contributed to manuscript development and revisions, and all authors have read and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Racz, F.S., Farkas, K., Becske, M. et al. Reduced temporal variability of cortical excitation/inhibition ratio in schizophrenia. Schizophr 11, 20 (2025). https://doi.org/10.1038/s41537-025-00568-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41537-025-00568-3