Abstract
Positive symptoms are a prominent feature of schizophrenia. Despite antipsychotic treatment, ~30% of patients develop refractory positive symptoms (RPSs). Current research fails to elucidate the potential neurophysiological mechanisms underlying RPSs, thereby hindering the development of additional treatments. This study, which included 37 patients with RPSs and 40 with non-refractory positive symptoms (NRPSs), aimed to explore their underlying neural mechanisms. Outcome measures were relative power spectrum density and interregional synchronization across frequency bands and theta-gamma phase-amplitude coupling (θ-γ PAC). The single-frequency analysis indicated that RPSs exhibited elevated theta power and reduced lateralization in the left temporal lobe and temporo-parietal junction, along with enhanced functional connectivity in the left frontocentral region. The cross-frequency analysis revealed that RPSs exhibited slightly higher θ-γ coupling at the left temporo-parietal junction compared to NRPSs. Correlation analysis revealed significant associations among theta power, the lateralization index, functional connectivity, and the severity of positive symptoms. The aberrant activation of the theta rhythm in the left temporo-parietal region may lead to increased functional asymmetry in the brain, impeding interregional and inter-frequency information transmission and thus significantly impairing the normal processing of auditory information. These findings offer potential insights into the neurophysiological basis of positive symptoms in schizophrenia and may inform future clinical interventions.
Similar content being viewed by others
Introduction
Schizophrenia is a chronic, multifactorial psychotic disorder affecting millions worldwide and is characterized by functional decline. The diagnosis requires at least two of the following five symptoms, with at least one being (1), (2), or (3): (1) delusions, (2) hallucinations, (3) disorganized speech, (4) grossly disorganized or catatonic behavior, and (5) negative symptoms. Positive symptoms, including hallucinations, delusions, and disorganized thinking, are central to the diagnosis of schizophrenia and are often the most distressing for patients. Among these positive symptoms, auditory hallucinations are particularly common, affecting approximately 60–75% of individuals with the disorder1. Given the significant distress caused by positive symptoms, identifying effective treatment options for individuals with treatment-resistant positive symptoms would be of considerable clinical value.
For clinical treatment, the first treatment option for positive symptoms in schizophrenia is antipsychotic medication, which can induce a rapid decrease in severity2. Despite adequate pharmacological therapy, up to 30% of schizophrenia patients suffer from treatment-refractory positive symptoms (RPS)3. In addition, noninvasive brain stimulation techniques offer immense potential as an add-on treatment for persistent symptoms of schizophrenia4. The comprehensive parameterization of brain stimulation necessitates a close association with the underlying neurophysiological mechanisms governing the symptoms. Thus, understanding the pathogenesis of positive symptoms is instrumental in developing more effective treatments.
The electroencephalogram (EEG) possesses the capability to capture electrical signals emanating from neuronal clusters with high temporal resolution5. Numerous EEG studies have elucidated a spectrum of electrophysiological alterations linked to positive symptoms6. The current studies consistently report that patients present abnormal auditory gamma responses7,8,9 and that phase-locked values in the gamma band were positively associated with auditory hallucinations10. Patients with schizophrenia exhibited reduced gamma activity in the left frontal lobe and bilateral frontal activation during language processing tasks, and the left frontal hypoactivation was significantly associated with the severity of delusions and hallucinations. Beyond task-related EEG abnormalities, resting-state EEG alterations also warrant investigation. When the brain is at rest, the spontaneous activity may reflect the potential of the brain to efficiently process task information11,12.
Indeed, the resting-state neural activity in individuals diagnosed with schizophrenia and hallucinations exhibits various alterations13. Current research can be broadly categorized into two approaches: the “trait” perspective and the “state” perspective. Arora et al. found that delta and theta activity were similar in hallucinators and non-hallucinators, but non-hallucinators had more alpha activity than hallucinators (trait)14. Dynamic connectivity analysis revealed that patients experiencing hallucinations had weaker connectivity between speech and auditory areas than healthy controls15. Koutsoukos et al. found that the θ-γ phase amplitude coupling (PAC) value increased in the left fronto-temporal region during hallucination (state)16. Thus, resting-state brain activity provides a valuable window into the pathophysiological mechanisms underlying refractory positive symptoms in schizophrenia.
In order to understand the neurophysiological mechanisms of positive symptoms more intuitively and clearly, the present study was conducted from the perspective of trait. RPSs and schizophrenia patients with non-refractory positive symptoms (NRPS) were recruited for a comparative analysis of spontaneous neural oscillations, initiated with resting-state EEG. The study encompasses the characterization of neural oscillatory activity across diverse frequency bands, interregional synchronization, and modulation of high-frequency oscillations by low-frequency oscillations, particularly focusing on θ-γ PAC. Additionally, the study explores the relationships between identified EEG biomarkers and symptoms associated with positive symptoms. A thorough exploration of the neurophysiological mechanisms underlying refractory positive symptoms can establish a robust theoretical foundation for subsequent clinical interventions.
Results
Demographics of NRPSs and RPSs
The demographic and clinical characteristics of the participants are shown in Table 1. No statistically significant group disparities were observed in terms of gender (\({\chi }^{2}\)(1) = 0.59, p = 0.44), age (t (71.5) = 0.62, p = 0.54), education level (t(70.0) = 0.28, p = 0.78), or onset age of the disease (t(67.7) = 1.89, p = 0.06) between the NRPSs and RPSs groups. A statistically significant group difference was observed in the duration of the disease (t (39.1) = −10.36, p < 0.001). The outcomes derived from the PANSS scale assessments indicated a statistically significant elevation in positive symptoms (t(58.7) = −12.09, p < 0.001), general psychopathology scores (t(67.3) = −4.77, p < 0.001), and total scores (t(63.3) = −4.23, p < 0.001) within the group characterized as RPSs compared to the corresponding scores in NRPSs. Nevertheless, no statistically significant distinction was observed in relation to negative symptoms (t(73.9) = −0.93, p = 0.35) between the two groups. These findings suggest that negative symptoms have persisted since the onset of the illness and have not improved substantially with treatment. In contrast, positive symptoms exhibited a progressive exacerbation throughout the course of the illness.
Relative power and lateralization
The ANCOVA results indicated that only the group factor showed a significant effect (see Supplementary Material for detailed results). As illustrated in Fig. 1A, comparisons between the two groups revealed distinct regional variations across the six frequency bands. There were no significant differences between the two groups in other frequency bands. In the theta band, the relative power in the RPSs group was significantly higher than that in the NRPSs group, particularly in the left temporo-parietal region (FT7: t(75) = 2.97, p = 0.04; C5: t(75) = 3.01, p = 0.04; C3: t(75) = 2.85, p = 0.04; TP7: t(75) = 2.79, p = 0.04; CP5: t(75) = 2.97, p = 0.04; CP3: t(75) = 3.18, p = 0.04; P7: t(75) = 3.06, p = 0.04; P5: t(75) = 2.90, p = 0.04) and right temporo-parietal region (TP8: t(75) = 2.93, p = 0.04; P8: t(75) = 2.72, p = 0.04). This implies that the persistently elevated theta relative power observed at the left temporo-parietal junction in RPSs, following a full course of medication, may be associated with the persistence of positive symptoms.
A Topographic distribution of significant differences in relative power in the NRPS group compared with the RPS group. Each subplot represents the t values of independent sample t-test. The orange color represents higher relative power in the NRPS group compared to the RPS group, while the green color represents lower relative power in the NRPS group compared to the RPS group. White stars represent electrodes that exhibited statistically significant differences (p < 0.05) with FDR correction. B Relative power results for regions of interest for lateralization. (From left to right, first figure) Delineation of regions of interest in the brain based on relative power results, including the left/right temporal lobes (blue) and the left/right temporo-parietal junction (orange). (From left to right, second and third panels) Comparison of the two sets of relative power results for lateralization at the temporal lobe and temporo-parietal junction.
Further, based on the previous significant difference in electrode distribution, we classified them into the left temporal lobe, left temporo-parietal junction, right temporal lobe, and right temporo-parietal junction, as shown on the left in Fig. 1B. We calculated the lateralization index of two groups at the temporal lobe and temporo-parietal junction and tested it statistically. The results of the analysis of ANCOVA showed that only the group factor was significant in both groups. We found that the RPS group exhibited a significant decrease in temporo-parietal lateralization index (t(73.5) = 2.36, p = 0.02) and a trend toward decrease in temporal lateralization index (t(68.6) = 1.93, p = 0.06) compared to the NRPS group. This implies that observed lateralized distinctions in neural activity within the temporo-parietal region of the brain may signify neurophysiological irregularities linked to the manifestation of refractory positive symptoms.
Functional connectivity
In order to investigate disorders pertaining to oscillatory synchronization and enhance our comprehension of functional connectivity in RPSs, we computed the wPLI values in the six frequency bands between the two groups for statistical analysis. The results of the analysis of ANCOVA showed that only the group factor was significant in both groups. T-test results showed that there is no significant difference between the two groups in the delta, alpha, beta, low gamma, and high gamma bands. The first and second images (from left to right) in Supplementary Fig. 1 represent the phase synchronization of theta bands between the 60 electrodes two by two in the NRPS and RPS groups, respectively. Statistically significant findings revealed a heightened strength of functional connectivity between the left frontal lobe and central regions, i.e., FC5 and C1, in RPS compared to NRPS. This implies that the aberrant augmentation of functional connectivity between the left frontal and central regions may represent a plausible neurophysiological mechanism contributing to the refractory positive symptoms.
Theta-gamma phase amplitude coupling
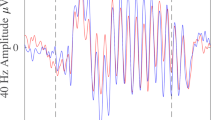
Recent studies have demonstrated that neural oscillation dynamics are governed by a complex hierarchical organization, i.e., gamma oscillations are modulated by the phase of theta waves17. Based on our findings that RPS patients showed power and phase abnormalities at the temporal lobe and temporo-partial junction in the theta band, theta-gamma PAC was further performed according to the brain regions in Fig. 1B. Figure 2 presents the grand-average PAC in theta-gamma frequency range, computed using the KL-MI method, for NRPSs, RPSs, and the contrast between RPSs and NRPSs in each region. RPSs exhibited elevated theta-gamma coupling values in the left temporal lobe and left temporo-parietal junction in comparison to NRPSs. Conversely, minimal disparities in theta-gamma coupling values were observed in the right temporal lobe and right temporo-parietal junction between the two groups. Subsequent statistical analysis revealed that PAC values between theta-high gamma frequencies at the left temporo-parietal junction demonstrated a trend toward elevation in RPSs compared to NRPSs (t(75) = 1.91, p = 0.06). Meanwhile, no significant difference in theta-gamma PAC was found between the two cohorts in other regions. This suggests that the abnormally increased theta power at the left temporo-parietal junction in RPS patients had an effect on high-frequency oscillations, i.e., gamma oscillations.
From left to right, the first column is the average PAC value within the four ROIs for the NRPS group, the second column is the average ROI value within the four ROIs for the RPS group, and the third column is the difference between RPS minus NRPS (orange means that the RPS group is larger than the NRPS group, and green means that the RPS group is smaller than the NRPS group). The blue boxes represent the theta-high γ (50–100 Hz) coupling values, which were stacked and averaged and then statistically analyzed between the two groups.
Correlation with positive symptoms
To investigate the specific neurophysiological correlates of positive symptoms, we performed correlation analyses between the significant EEG features identified in the preceding sections and positive symptom scores derived from the PANSS scale (see Fig. 3). We found significant positive associations between the positive symptom scores and the relative power of theta (r = 0.29, p = 0.01) and connectivity value between FC5 and C1 under theta band (r = 0.37, p = 0.001). These results suggest that higher theta oscillatory activity and frontal-central connectivity are associated with more severe positive symptoms, including auditory hallucinations. However, this cross-sectional association does not imply causation and may reflect shared neuropathological mechanisms. In addition, we found significant negative associations between the positive symptom score and the lateralization index at the temporo-parietal junction (r = −0.25, p = 0.03), suggesting that patients with right lateralization at the temporo-parietal junction in the theta frequency band have fewer positive symptoms. The observed associations, although statistically significant, were weak in magnitude.
First from left to right, a significant positive correlation between the relative power spectrum density of left temporo-parietal junction and positive symptoms (r = 0.29, p = 0.012). Second, a significant negative correlation between the lateralization index of left temporo-parietal junction and positive symptoms (r = −0.25, p = 0.028). Third, a significant positive correlation between the wPLI between FC5 and C1 and positive symptoms (r = 0.37, p = 0.001).
We conducted additional partial correlation analyses using illness duration as a covariate, since this was the only available potential confounding variable we could include (antipsychotic dosage data were unfortunately unavailable for the NRPS group and could therefore not be incorporated). These analyses showed that the previously significant associations did not remain significant after controlling for illness duration. While this suggests that illness duration may contribute to the observed associations, it is also possible that the reduced statistical power due to covariate inclusion may have impacted the results.
Discussion
In this study, we conducted an analysis of rsEEG in RPSs and NRPSs. We systematically compared differences in relative power and functional connectivity across six frequency bands between the two groups. Further, we compared differences in θ-γ PAC, specifically within the temporal lobe and temporo-parietal junction between the two groups. Our study revealed that : (1) compared to NRPSs, RPS patients exhibited a significant elevation in theta relative power in the left temporal lobe and the left temporo-parietal junction, with a less pronounced lateralization of theta relative power between hemispheres; (2) enhanced functional connectivity was observed in the left frontal-central region in RPSs patients; (3) the theta relative power at the left temporo-parietal joint and the functional connectivity in the left frontal-central region were significantly and positively correlated with positive symptoms; additionally, the lateralization index of theta power at the temporo-parietal joint demonstrated a significant negative correlation with positive symptoms. Thus, refractory positive symptoms in schizophrenia are associated with aberrant enhancements in theta oscillations. Longitudinal or interventional studies are required to determine causal relationships. These findings provide a promising avenue for understanding the neurophysiological mechanisms of refractory positive symptoms, which may guide subsequent clinical treatments.
Our findings, indicating an abnormal elevation in theta oscillations at the temporal lobe and temporo-parietal junction in RPS patients, align with Ishii et al.‘s discovery of increased theta rhythms in the left superior temporal cortex during auditory hallucinations in patients with similar symptoms18. Simultaneously, research has demonstrated the engagement of the superior temporal cortex in the left hemisphere in phonological processing, while the left temporo-parietal junction has been implicated in the manifestation of positive symptoms of schizophrenia, particularly auditory verbal hallucinations19. Theta oscillations, the most widely studied low-frequency oscillations, are notably prominent in the hippocampus and arise from the interaction between glutamatergic and gamma-aminobutyric acidergic neurons20. Given the pivotal role of the hippocampus in situational and declarative memory formation and retrieval21, theta oscillations are associated with memory processes22,23. Studies have shown that a significant increase in theta power during information encoding predicts subsequent recall24. In this context, the abnormally elevated theta power observed in RPS patients might reflect an aberrant engagement of memory-related processes, such as prolonged encoding or rehearsal of past acoustic information. This speculative interpretation may help explain the persistence of positive symptoms, although further investigation is needed to validate this hypothesis.
Normal brain function relies on effective communication among distributed neuronal networks to coordinate ongoing information processing25,26. A prominent hypothesis posits that the fundamental pathology of schizophrenia results from abnormal functional connectivity within and between brain regions27. Our findings align with this hypothesis, revealing abnormal enhancement of functional connectivity in the left frontal-central region within the theta band in patients with refractory positive symptoms. Theta oscillations are implicated in top-down control of various cognitive and executive processes28, with the prefrontal cortex playing a key role in top-down executive control29. Therefore, this aberrant top-down control may be a significant contributor to the manifestation of auditory hallucinations.
We acknowledge that without a healthy control group, our findings must be interpreted in the context of prior work showing robust theta‑band abnormalities in schizophrenia. Multiple studies have reported elevated resting‑state theta power (4–7 Hz) in patients versus controls18,30. Complementing this, Griskova‑Bulanova et al. demonstrated that patients exhibit reduced ASSR power across the theta–beta range (4–18 Hz), which correlates inversely with positive symptom severity31. At the network level, theta‑band functional connectivity is also disrupted: excessive local frontal synchrony has been linked to impaired goal‑directed cognition and positive symptoms32,33, whereas weakened long‑range coupling between prefrontal and temporo‑parietal regions underlies contextual integration deficits and may foster delusional beliefs19,34. Furthermore, alterations in lateralization—such as reduced left‑hemispheric frontal theta dominance—have been associated with the neurobiology of verbal hallucinations, albeit with notable variability across tasks and symptom subtypes18,35. These converging lines of evidence both contextualize our observations and underscore the need for future studies that directly include healthy controls.
We should also seriously consider the limitations of this study. Firstly, our study encountered limitations due to the absence of detailed P3 item scores specifically related to auditory hallucinations within the PANSS scale section for patients. Consequently, our correlation analyses were constrained to examining the association between total positive symptom scores and EEG features. Nevertheless, it is crucial to note that during subject recruitment, stringent criteria were applied to ensure minimal divergence between the two groups, focusing solely on one positive symptom. In addition to PANSS positive scale score, duration, and PANSS general psychopathology severity were different between the two groups. These might be confounding factors for EEG results. However, the covariance results showed that only the group factor was significant, so our findings are still relevant.
Secondly, it is well established that antipsychotic drugs can have an effect on the theta band activity of the patient’s brain36,37. The experiment faced a limitation due to the absence of recorded medication information for the patients, thereby preventing the complete exclusion of potential drug-related influences on the experimental outcomes. Thus, our cohort limit the ability to fully disentangle antipsychotic effects from symptom-related neurophysiology. Future studies should integrate detailed drug monitoring or enroll drug-naïve patients to clarify medication-specific effects. Thirdly, we acknowledge the absence of immediate self-report data following EEG recordings to capture state-dependent effects, which limits our ability to analyze transient symptom fluctuations; this limitation should be addressed in future research. Fourthly, we recognize that the long-term effects of chronic illness on the brain—such as structural changes like brain atrophy or prolonged exposure to antipsychotic medication—may be more profound and complex. These effects cannot be completely ruled out in the present study. Finally, there was a trend toward a difference in θ-γ PAC between the two groups (p = 0.06), although this did not reach statistical significance and showed no significant correlation with positive symptoms. Currently, a clear explanation for this result remains elusive. Consequently, in subsequent analyses, we plan to augment the subject cohort and conduct a more comprehensive exploration to elucidate the underlying factors contributing to this observation.
Methods
Participants
Seventy-seven hospitalized patients, including 40 NRPSs (24 females, age 46.85 ± 10.63) and 37 RPSs (18 females, age 48.49 ± 12.29), participated in this study. During the initial clinical interview with the physician, participants underwent an assessment based on inclusion and exclusion criteria. This study was approved by the Tianjin Anding Hospital Ethics Committee (2020-30). All participants received details about the experiment and were required to read and sign their names on written informed consents before participating.
Inclusion criteria
All participants satisfied the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5)38 diagnostic criteria for “schizophrenia or schizophrenia-like disorder.” The participants ranged in age from 18 to 70 years, encompassing both genders. The educational attainment of participants was at least at the junior high school level.
NRPSs
The patient was assessed by the supervising physician as having auditory hallucinations or positive symptoms as the main clinical feature at the time of admission; a Clinical General Impression Severity (CGI-S) score of ≤3; and a score of ≤3 on all positive symptom items of the Positive and Negative Syndrome Scale (PANSS), and all patients had no symptomatic recurrence in the past 3 months without drug treatment.
RPSs
The duration of symptoms over the course of this treatment was greater than or equal to 12 weeks; the patients were treated with greater than or equal to 2 different antipsychotic medications (chlorpromazine equivalent dose≥600 mg), and the final dose of medication lasted for greater than or equal to 6 weeks, with poor efficacy (CGI ≥ 4 or less than a 20% reduction in PANSS scores since the current treatment); and the patient was assessed by the supervising physician as displaying stable and pronounced refractory auditory hallucinations within the last two weeks prior to the patient’s admission, with a sustained score of greater than or equal to 4 on the PANSS hallucination (P3) item or with a change of ≤20% in the Psychotic Symptom Rating Scales (PSYRATS) scores.
Exclusion criteria
Participants were excluded if they met any of the following criteria: Participants were excluded if they met criteria for any psychiatric disorder other than schizophrenia, as diagnosed by DSM-5; severe physical or neurological illness; electroconvulsive therapy or other physical therapy within the last 4 weeks; any brain device or implant, including cochlear implants and aneurysm clips; previous autoimmune disease or family history of immune disorders; use of antibiotics or immunosuppressive drugs within the past four weeks.
8-min resting-state EEG experimental procedures
All participants engaged in an 8-min resting-state session. The resting-state session comprised eight 1-min trials, each involving either the open eyes (EO) or closed eyes (EC) condition. The sequence of open and closed eyes alternated for this study39,40. Participants were instructed to relax with their EO and EC in one of two alternating orders of eight 1-min intervals (occocooc). The experimental protocol took place within an acoustically isolated chamber featuring conventional overhead illumination. Before the experiments, all patients were seated comfortably, stayed relaxed, and were required to control their body movements and eye blinks during the experiments. The session was initiated by the participant pressing the spacebar, which triggered a computerized auditory cue: “Please open your eyes.” Participants subsequently adjusted to comply with the instruction to open their eyes, marking the onset of the EO trial. Following a one-minute interval, another auditory cue, “Please close your eyes,” was presented, prompting participants to close their eyes, thereby initiating the EC trial. The chronological arrangement of these auditory cues is depicted in supplementary material.
EEG data acquisition
Resting-state EEG signals were recorded using the SynAmps2 system (Neuroscan, USA) and a 64-channel Ag/AgCl electrode cap. All electrodes were positioned in compliance with the 10–20 international electrode placement system41. Data recording was referenced to a linked left mastoid electrode (“M1”) with the ground electrode located at “AFz”. EEG signals were sampled at 1000 Hz, and the online bandpass was filtered at 0.1–200 Hz. During recording, the impedance of all electrodes was kept below 10 kΩ.
EEG signals analysis
EEG preprocessing
EEG signal analyses were conducted utilizing the EEGLAB (version 2023.0) toolbox in MATLAB (version R2020b; The MathWorks, Inc., USA), complemented by a suite of custom MATLAB scripts. Initially, electrodes deemed inactive, including CB1, CB2, HEO, VEO, EKG, and EMG, were excluded from the experimental setup. The offline signals were re-referenced to the mean of bilateral mastoid electrodes ([“M1” + “M2”]/2) and subsequently down-sampled to a frequency of 250 Hz. The function pop_eegfiltnew.m was employed to implement a 0.5–120 Hz bandpass filter (finite impulse response filter, cutoff frequency (−6 dB): [0.25 Hz, 120.25 Hz], zero-phase, non-causal). Notch filtering at 50 and 100 Hz was applied to mitigate industrial frequency interference. The plugin clean_rawdata()42 within EEGLAB was utilized for automatic rejection of high-amplitude artifacts through artifact subspace reconstruction. Channels rejected during this step were spatially interpolated using spherical interpolation. For detailed parameter settings, please refer to our previous article43.
Artifacts arising from eyeblinks, eye movements, and muscle activity were corrected via independent component analysis employing the ICLabel toolbox44. Components classified as “ocular” (eyeblinks/eye movements) or “muscle” with a probability threshold >90% were manually rejected. Residual artifacts (e.g., transient muscle spikes) were further excluded using amplitude thresholding (±100 μV). Following this preprocessing, clean EEG data were obtained for each participant. To standardize analysis duration and minimize temporal bias, 3-min sections were randomly selected from clean EO data using a MATLAB script (seed = participant ID; randperm function). If multiple artifact-free intervals existed, the longest contiguous segment was prioritized. In this study, EEG oscillations were defined within the frequency range of 0.5 to 100 Hz, encompassing δ (1–4 Hz), θ (4–8 Hz), α (8–13 Hz), β (13–30 Hz), and γ (30–100 Hz). Notably, the γ band was further stratified into low γ (30–50 Hz) and high γ (50–100 Hz)45.
Spectral analysis
Welch’s FFT method46 was employed to compute the absolute power spectral density (PSD) within the δ, θ, α, β, low γ, and high γ frequency bands. MATLAB offers an intrinsic command known as the pwelch.m function for the acquisition of PSD. In this study, 3-min open-eye EEG signals were split into 4s segments with 0% overlap47, resulting in 45 equal segments. The Hamming window was applied to individual segments, and the PSD estimate was determined through the averaging of the resultant periodograms. To mitigate absolute power discrepancies arising from factors such as varied scalp signal conductivity and facilitate the comparative analysis of EEG signals across diverse individuals, this study opted to compute relative power. Precisely, the relative power for each subject and electrode was determined as the ratio of the cumulative raw PSDs within specific frequency ranges to the total power (sum of raw PSDs in the 1–100 Hz frequency range).
Lateralization analysis
For the evaluation of laterality effects, electrodes were categorized into left temporal lobe (FT7, T7), left temporo-parietal junction (C5, C3, TP7, CP5, CP3, P7, P5), right temporal lobe (FT8, T8) and right temporo-parietal junction (C6, C4, TP8, CP6, CP4, P8, P6) according to the distribution of relative power across significant electrodes. The lateralization index (LI) was calculated according to the formula:
where R indicated the mean value for the right brain hemisphere and L indicated the mean value for the left brain hemisphere. The lateralization index values span from −1 to 1, where proximity to 1 suggests a greater lateralization of neuronal activity towards the right hemisphere, values nearing −1 indicate a stronger lateralization towards the left hemisphere, and 0 indicates no laterality.
Connectivity analysis
The weighted phase lag index (wPLI) was extracted to calculate functional connectivity. This denotes a metric of phase-based connectivity computed at a particular frequency, encompassing solely non-zero phase lag/lead associations between two time series signals48. Specifically, it quantifies the degree to which phase angle disparities between two time series, denoted as x(t) and y(t), are distributed towards the positive or negative sectors of the imaginary axis within the complex plane:
Here \({S}_{{xy},t}\) signifies the complex cross-spectral density of the time series x(t) and y(t) at the time point t, while || denotes the absolute value. The wPLI mitigates the likelihood of identifying spurious connectivity in scenarios involving volume-conducted noise sources with minimal phase lag, thereby enhancing the sensitivity of detecting phase synchronization. The wPLI values are confined within the range of 0 (indicating no phase synchronization) to 1 (indicating perfect phase synchronization)49. We calculated the wPLI value for each pair of electrodes per 4s epoch in each trial, and the final phase synchronizations within each subject were averaged across trials.
Phase amplitude coupling
The Kullback-Leibler-based modulation index (KL-MI) was applied to quantify the degree of phase amplitude coupling (PAC)50. First, we filtered the raw signals to extract the phase (signals ranging from 1 to 29 Hz, with a 1 Hz bandwidth) and amplitude (signals ranging from 30 to 100 Hz, with a 2 Hz bandwidth) using the Hilbert transform. For each phase-amplitude pair, the low-frequency phases (\({\phi }_{{f}_{P}}(t)\)), ranging from −\(\pi\) to \(\pi\), were discretized into 18 bins (each 20° wide), and the mean amplitude of the corresponding high-frequency (\({A}_{{f}_{A}}(t)\)) within each bin was computed51. Following this, entropy (H) was utilized to assess the distribution of (\({A}_{{f}_{A}}(t)\)) across 18 bins, as defined by:
Where M = 18 (representing the number of bins) and \({p}_{i}\) was determined by:
Where \({\left\langle {A}_{{f}_{A}}\right\rangle }_{{\phi }_{{f}_{P}}}(i)\) is the mean \({A}_{{f}_{A}}\) value at phase bin I, and the MI was determined by:
Where \({H}_{\max }\) was obtained for the uniform distribution \({p}_{i}=1/M\)(\({H}_{\max }=\,\log M\)). Consequently, the KL-MI served as a metric ranging from 0 (indicating absence of phase-amplitude modulation) to 1 (representing maximal phase-amplitude modulation). Given the extended data length, a heightened level of reliability in the MI measurement could be ensured. The above steps are illustrated in articles by Liu et al.52. The 3 min signal was analyzed for PAC calculations rather than the 4s epoch.
Statistical analysis
Demographic and scale score statistical procedures were performed using R packages. Independent sample t-tests were employed for group comparisons, with the exception of gender, which was evaluated using a Chi-square test. Statistical significance was defined as p < 0.05. Values slightly above this threshold (e.g., p ≈ 0.06) were interpreted as indicating a statistical trend. To account for the duration of the disease, as well as differences in total PANSS scores and general psychiatric scores on the PANSS scale between the two groups, we conducted an analysis of covariance (ANCOVA) prior to comparing the groups. Further, all EEG features were compared between the two groups using an independent sample t-test with a false discovery rate (FDR) correction for multiple comparisons53.
To explore the relationship between EEG findings and clinical positive symptoms, correlations were computed between positive symptom scores on the PANSS scale and rsEEG theta relative power, functional connectivity values within the theta band, and differences in theta-gamma coupling. Relative power, functional connectivity, and PAC differences were obtained through statistical analyses comparing the two groups. For correlation assessment, a two-tailed Pearson correlation coefficient was employed54, and significance was established at a priori values ≤0.05.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request. All code used to analyze the presented results was available upon request.
Code availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request. All code used to analyze the presented results was available upon request.
References
McCarthy-Jones, S. et al. Better than mermaids and stray dogs? Subtyping auditory verbal hallucinations and its implications for research and practice. Schizophr. Bull. 40, S275–S284 (2014).
Sommer, I. E. et al. The treatment of hallucinations in schizophrenia spectrum disorders. Schizophr. Bull. 38, 704–714 (2012).
Shergill, S. S., Murray, R. M. & McGuire, P. K. Auditory hallucinations: a review of psychological treatments. Schizophr. Res. 32, 137–150 (1998).
Koops, S., van den Brink, H. & Sommer, I. E. Transcranial direct current stimulation as a treatment for auditory hallucinations. Front. Psychol. 6, 244 (2015).
Müller-Putz, G. R. Electroencephalography. Handb. Clin. Neurol. 168, 249–262 (2020).
Ford, J. M. et al. Neurophysiological studies of auditory verbal hallucinations. Schizophr. Bull. 38, 715–723 (2012).
Tada, M. et al. Alterations of auditory-evoked gamma oscillations are more pronounced than alterations of spontaneous power of gamma oscillation in early stages of schizophrenia. Transl. Psychiatry 13, 1–8 (2023).
O’Donnell, B. F. et al. The auditory steady-state response (ASSR): a translational biomarker for schizophrenia. Suppl. Clin. Neurophysiol. 62, 101–112 (2013).
Thuné, H., Recasens, M. & Uhlhaas, P. J. The 40-Hz auditory steady-state response in patients with schizophrenia: a meta-analysis. JAMA psychiatry 73, 1145–1153 (2016).
Mulert, C., Kirsch, V., Pascual-Marqui, R., McCarley, R. W. & Spencer, K. M. Long-range synchrony of gamma oscillations and auditory hallucination symptoms in schizophrenia. Int. J. Psychophysiol. 79, 55–63 (2011).
Zhang, R. et al. Efficient resting-state EEG network facilitates motor imagery performance. J. neural Eng. 12, 066024 (2015).
Li, F. et al. Differentiation of schizophrenia by combining the spatial EEG brain network patterns of rest and task P300. IEEE Trans. Neural Syst. Rehabil. Eng. 27, 594–602 (2019).
Alderson-Day, B. et al. Auditory hallucinations and the brain’s resting-state networks: findings and methodological observations. Schizophr. Bull. 42, 1110–1123 (2016).
Arora, M., Knott, V. J., Labelle, A. & Fisher, D. J. Alterations of resting EEG in hallucinating and nonhallucinating schizophrenia patients. Clin. EEG Neurosci. 52, 159–167 (2021).
Zhang, W. et al. Abnormal dynamic functional connectivity between speech and auditory areas in schizophrenia patients with auditory hallucinations. NeuroImage: Clin. 19, 918–924 (2018).
Koutsoukos, E., Angelopoulos, E., Maillis, A., Papadimitriou, G. N. & Stefanis, C. Indication of increased phase coupling between theta and gamma EEG rhythms associated with the experience of auditory verbal hallucinations. Neurosci. Lett. 534, 242–245 (2013).
Kirihara, K., Rissling, A. J., Swerdlow, N. R., Braff, D. L. & Light, G. A. Hierarchical organization of gamma and theta oscillatory dynamics in schizophrenia. Biol. Psychiatry 71, 873–880 (2012).
Ishii, R. et al. Theta rhythm increases in left superior temporal cortex during auditory hallucinations in schizophrenia: a case report. Neuroreport 11, 3283–3287 (2000).
Vercammen, A., Knegtering, H., den Boer, J. A., Liemburg, E. J. & Aleman, A. Auditory hallucinations in schizophrenia are associated with reduced functional connectivity of the temporo-parietal area. Biol. Psychiatry 67, 912–918 (2010).
Leung, L. S. & Shen, B. GABAB receptor blockade enhances theta and gamma rhythms in the hippocampus of behaving rats. Hippocampus 17, 281–291 (2007).
Eichenbaum, H. Hippocampus: cognitive processes and neural representations that underlie declarative memory. Neuron 44, 109–120 (2004).
Vertes, R. P. Hippocampal theta rhythm: a tag for short-term memory. Hippocampus 15, 923–935 (2005).
Uhlhaas, P. J., Haenschel, C., Nikolić, D. & Singer, W. The role of oscillations and synchrony in cortical networks and their putative relevance for the pathophysiology of schizophrenia. Schizophr. Bull. 34, 927–943 (2008).
Sederberg, P. B., Kahana, M. J., Howard, M. W., Donner, E. J. & Madsen, J. R. Theta and gamma oscillations during encoding predict subsequent recall. J. Neurosci. 23, 10809–10814 (2003).
Engel, A. K., Fries, P. & Singer, W. Dynamic predictions: oscillations and synchrony in top–down processing. Nat. Rev. Neurosci. 2, 704–716 (2001).
Singer, W. Distributed processing and temporal codes in neuronal networks. Cogn. Neurodyn. 3, 189–196 (2009).
Andrew, M. & Heim, G. Eugen Bleuler's dementia praecox or the group of schizophrenias. Cogn. Neurodyn. 37, 471–479 (1950).
Buschman, T. J. & Miller, E. K. Top-down versus bottom-up control of attention in the prefrontal and posterior parietal cortices. Science 315, 1860–1862 (2007).
Hugdahl, K., Løberg, E.-M. & Nygård, M. Left temporal lobe structural and functional abnormality underlying auditory hallucinations. Front. Neurosci. 3, 401 (2009).
Amico, F., Keane, M. & McCarthy-Jones, S. Resting-state EEG and MEG correlates of auditory hallucinations in adults with schizophrenia: a systematic review. NeuroRegulation 9, 174–174 (2022).
Griskova-Bulanova, I. et al. Envelope following response to 440 Hz carrier chirp-modulated tones show clinically relevant changes in schizophrenia. Brain Sci. 11, 22 (2020).
Spencer, K. M. et al. Abnormal neural synchrony in schizophrenia. J. Neurosci. 23, 7407–7411 (2003).
Narayanan, B. et al. Resting state electroencephalogram oscillatory abnormalities in schizophrenia and psychotic bipolar patients and their relatives from the bipolar and schizophrenia network on intermediate phenotypes study. Biol. Psychiatry 76, 456–465 (2014).
Ford, J. M., Roach, B. J., Faustman, W. O. & Mathalon, D. H. Synch before you speak: auditory hallucinations in schizophrenia. Am. J. Psychiatry 164, 458–466 (2007).
Hugdahl, K. et al. Auditory verbal hallucinations in schizophrenia as aberrant lateralized speech perception: evidence from dichotic listening. Schizophr. Res. 140, 59–64 (2012).
Ozaki, T., Toyomaki, A., Hashimoto, N. & Kusumi, I. Quantitative resting state electroencephalography in patients with schizophrenia spectrum disorders treated with strict monotherapy using atypical antipsychotics. Clin. Psychopharmacol. Neurosci. 19, 313 (2021).
Saletu, B., Grünberger, J., Linzmayer, L. & Anderer, P. Comparative placebo-controlled pharmacodynamic studies with zotepine and clozapine utilizing pharmaco-EEG and psychometry. Pharmacopsychiatry 20, 12–27 (1987).
Regier, D. A., Kuhl, E. A. & Kupfer, D. J. The DSM-5: Classification and criteria changes. World psychiatry 12, 92–98 (2013).
Wang, X. et al. Resting-state electroencephalographic signatures predict treatment efficacy of tACS for refractory auditory hallucinations in schizophrenic patients. IEEE J. Biomed. Health Inform. 29, 1886–1896 (2024).
Babiloni, C. et al. International Federation of Clinical Neurophysiology (IFCN)–EEG research workgroup: recommendations on frequency and topographic analysis of resting state EEG rhythms. Part 1: applications in clinical research studies. Clin. Neurophysiol. 131, 285–307 (2020).
Jurcak, V., Tsuzuki, D. & Dan, I. 10/20, 10/10, and 10/5 systems revisited: their validity as relative head-surface-based positioning systems. Neuroimage 34, 1600–1611 (2007).
Blum, S., Jacobsen, N. S., Bleichner, M. G. & Debener, S. A Riemannian modification of artifact subspace reconstruction for EEG artifact handling. Front. Hum. Neurosci. 13, 141 (2019).
Wang, X. et al. Double-blind, randomized, placebo-controlled pilot clinical trial with gamma-band transcranial alternating current stimulation for the treatment of schizophrenia refractory auditory hallucinations. Transl. Psychiatry 15, 36 (2025).
Pion-Tonachini, L., Kreutz-Delgado, K. & Makeig, S. ICLabel: an automated electroencephalographic independent component classifier, dataset, and website. Neuroimage 198, 181–197 (2019).
Ahmadi, A., Khorasani, A., Shalchyan, V. & Daliri, M. R. State-based decoding of force signals from multi-channel local field potentials. IEEE Access 8, 159089–159099 (2020).
Welch, P. The use of fast Fourier transform for the estimation of power spectra: a method based on time averaging over short, modified periodograms. IEEE Trans. Audio Electroacoust. 15, 70–73 (1967).
Albrecht, M. A. et al. The effects of dexamphetamine on the resting-state electroencephalogram and functional connectivity. Hum. Brain Mapp. 37, 570–588 (2016).
Vinck, M., Oostenveld, R., Van Wingerden, M., Battaglia, F. & Pennartz, C. M. An improved index of phase-synchronization for electrophysiological data in the presence of volume-conduction, noise and sample-size bias. Neuroimage 55, 1548–1565 (2011).
Ahn, S. et al. Interbrain phase synchronization during turn-taking verbal interaction—a hyperscanning study using simultaneous EEG/MEG. Hum. Brain Mapp. 39, 171–188 (2018).
Tort, A. B. et al. Dynamic cross-frequency couplings of local field potential oscillations in rat striatum and hippocampus during performance of a T-maze task. Proc. Natl. Acad. Sci. USA 105, 20517–20522 (2008).
Wang, S. et al. Features of beta-gamma phase-amplitude coupling in cochlear implant users derived from EEG. Hear. Res. 428, 108668 (2023).
Liu, X. et al. Altered gamma oscillations and beta–gamma coupling in drug-naive first-episode major depressive disorder: association with sleep and cognitive disturbance. J. Affect. Disord. 316, 99–108 (2022).
Genovese, C. R., Lazar, N. A. & Nichols, T. Thresholding of statistical maps in functional neuroimaging using the false discovery rate. Neuroimage 15, 870–878 (2002).
Afyouni, S., Smith, S. M. & Nichols, T. E. Effective degrees of freedom of the Pearson’s correlation coefficient under autocorrelation. Neuroimage 199, 609–625 (2019).
Acknowledgements
This research reported in this publication was supported by the National Natural Science Foundation of China (Grant Nos. 81925020) and the National Key Research and Development Program of China (2023YFF1203700). We thank the doctors of Tianjin Anding Hospital for their help with participant recruitment and assessment for this study.
Author information
Authors and Affiliations
Contributions
Xiaojuan Wang and Shuang Liu designed the study and wrote the protocol. Shuang Liu, Jie Li, and Dong Ming supervised data collection. Meijuan Li, Ying Gao, Xiaojuan Wang and Shaobing Li collected the data. Xiaojuan Wang, and Shuang Liu analyzed data and undertook the statistical analysis. Xiaojuan Wang wrote the first draft of the manuscript. Sitong Chen and Shuang Liu critically reviewed the results and provided substantial input to the manuscript. All authors contributed to and have approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, X., Chen, S., Li, J. et al. Enhanced theta oscillations in the left temporoparietal region associated with refractory positive symptoms in schizophrenia. Schizophr 11, 104 (2025). https://doi.org/10.1038/s41537-025-00652-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41537-025-00652-8