Abstract
Mycoplasma gallisepticum (MG) is an avian respiratory pathogen causing significant global economic losses to the poultry industries. Current live-attenuated and bacterin vaccines provide some measures of protective immunity but exhibit suboptimal efficacy, utility, or safety. To address these shortcomings, we utilized knowledge of MG biology and virulence to develop a subunit vaccine containing recombinantly produced primary adhesin GapA, cytadhesin-related molecule CrmA, and four early-phase-expressed variable lipoprotein hemagglutinins (VlhAs) (3.03, 3.06, 4.07, 5.05) of the virulent strain Rlow. The vaccine was tested in chickens using a subcutaneous dose of 50 µg per protein, a prime-boost schedule, and strain Rlow challenge in multiple studies to compare adjuvant formulations. While different adjuvants resulted in variable levels of protection, only CpG oligodeoxynucleotide (CpG ODN 2007) resulted in significant reductions of both MG recovery and tracheal pathology. These results demonstrate that a rationally designed and safe subunit vaccine is efficacious against MG disease.
Similar content being viewed by others
Introduction
Mycoplasma gallisepticum is the primary etiologic agent of avian mycoplasmosis, which predisposes infected poultry to subsequent co-infections with other pathogens. This co-infection can lead to a pathological condition known as chronic respiratory disease (CRD), which substantially compromises the integrity and function of the respiratory tract. Significant economic losses from chronic MG infection occur due to reduced egg production and hatchability, as well as downgrading of carcasses1. Losses to the broiler chicken industry alone are estimated at $588 million annually in the United States. Additionally, an estimated 37% of the commercial egg laying birds in the United States (262 million birds) are infected with MG resulting in a $132 million annual loss to that industry1,2,3,4,5,6. These issues have made MG a priority pathogen for discovery of enhanced control measures in the USDA’s National Poultry Improvement Plan7.
MG is transmitted by inhalation of aerosolized respiratory secretions, indirect contact, and by egg transmission8. Currently, MG control strategies include strict biosecurity to maintain MG-free breeder flocks and vaccination programs on large-scale poultry farms. The two types of commercially available vaccines for MG include live-attenuated vaccine (LAV) strains and bacterins, which are an inactivated suspension of whole bacteria. There are multiple commercially available LAVs including: F strain, K strain, Vaxsafe MG (ts-11), Vaxsafe MG304 (ts-304),and 6/852,9,10,11,12. Certain MG LAVs can negatively impact poultry production, suffer from issues of virulence in different host species or in young birds, and demonstrate varying levels of protective efficacy13,14,15. Both live-attenuated vaccines and bacterins present issues in distinguishing vaccinated from naturally animals16. Because no vaccines to date have been found to fully prevent infection with MG, they are not sufficient to meet the National Poultry Improvement Plan Standard of using uninfected chickens7,17,18,19. In addition, possible reversion to virulence has been reported, as evidenced by recovery of vaccine-like isolates from unvaccinated birds16,20,21,22,23. However, another recent paper has suggested that some highly genetically similar strains may actually be from the original parent strain used to derive the vaccine rather than having been from the vaccine strain itself24. Finally, the molecular nature of attenuating mutations is not defined for current LAVs which is concerning because a lack of defined mutations increases the risk of unintended consequences and makes the ability to identify and confirm strains that have reverted to virulence more challenging. Given these shortcomings (inadequate protection as defined by infection of a vaccinated chicken that still results in reduced egg laying, reduced feed conversion/weight gain, and/or gross pathology at time of necropsy, residual virulence, the potential for reversion to wild-type virulence, and undefined attenuation), the poultry industry continues to lack a suitable, safe, and effective vaccine to prevent avian respiratory mycoplasmosis.
Lack of bacterin efficacy may be the result of many factors, but likely stems from inadequate presentation of key protective antigens in a non-replicating formulation. An MG subunit vaccine that retained the safety profile of a bacterin and targeted key protective antigens formulated to present them in a non-replicating vaccine would be desirable. Here, we aimed to use prior knowledge of key MG proteins, including those dynamically expressed by MG and likely not available in standard bacterins, to rationally design an efficacious and flexible MG subunit vaccine.
Our previous work demonstrated that both of the primary cytadhesin molecules, gallisepticum adhesion protein A (GapA) and the cytadhesin-related molecule A (CrmA) are required for MG cytadherence25. Others have independently confirmed the importance of these two proteins26. Lack of GapA reduces cytadherence to host cells in vitro by approximately 80%25. It has also been shown that antibodies against GapA can reduce cytadherence to host cells in vitro by approximately 64%27. Notably, GapA expression is essential for the increased efficacy of LAV strain ts-304 relative to strain ts-1111. Both GapA and CrmA are conserved across all the naturally occurring MG strains sequenced to date, making the inclusion of both proteins in a subunit vaccine essential.
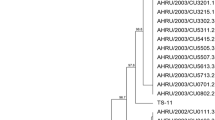
Previous literature has described in MG a large vlhA (variable lipoprotein and hemagglutinin) multigene family encoding the hemagglutinins28. MG VlhAs are phase-variably expressed, antigenically heterogeneous, and immunodominant antigens in infected birds29,30. We detailed the phase-variable expression of the vlhAs in vivo, where the pattern of dominant vlhA expression in the first week of infection is dynamic, nonrandom, and regulated by previously unrecognized mechanism(s). The first four days of in vivo vlhA expression is dominated by vlhA 3.03, with accessory expression from vlhAs 4.07/4.07.6 and vlhA 5.05. Expression of vlhAs 3.03 and 5.05 begin declining after day one, whereas vlhA 4.07/4.07.6 expression begins declining after day two. vlhA 4.07.1/4.08 expression steadily increases after day two, is roughly equal with vlhA 3.03 expression on day five and is dominant on days six and seven. vlhA 3.06 expression follows the same trend as vlhA 4.07.1/4.08, but at a lower level31. Thus, this subset of MG VlhAs are likely critical for pathogen-host interaction during infection of natural target tissues.
Although the exact function is unconfirmed, VlhA proteins are believed to be important for MG-host interaction, pathogenesis, and immune evasion32,33,34. We postulate that early VlhA phase variation is driven, in part, by the alterations in the cellular architecture of the trachea during infection. As the infection progresses, host cells experience denuding of cilia, squamous cell metaplasia, and eventual destruction of the host cell membranes1. We hypothesize that MG vlhA expression is changing in response to these alterations and MG expresses a specific set of vlhA genes to best persist in the changing environments. Thus, if this ordered switching was disrupted, we may be able to halt disease progression (Fig. 1).
A The current working model of ordered VlhA switching of MG in response to the changing respiratory epithelial phenotype during infection. Loose attachment to ciliary cells with VlhA proteins transitions to tight attachment on the cell membrane with both VlhA proteins and the cytadhesins GapA and CrmA, utilizing gliding motility mechanisms. As epithelial phenotypes change, so do their surface molecules, and vlhA gene expression in the bacterium changes to allow for continued adhesion to host cells. B In the presence of a vaccine that contains all the VlhA antigens that are expressed early in MG infection, phase variation is not allowed to progress. Even the rare bacterial cell that manages to evade antibodies and attach to host cells will be targeted when VlhA switching occurs, as antibodies are present against these subsequent VlhA proteins as well. The addition of GapA and CrmA antigens further helps to ensure that attachment of MG bacteria to host respiratory epithelium is minimized.
Inclusion of key phase-variable proteins into a subunit vaccine presents a broader range of protective antigens than a bacterin, conceivably providing the enhanced protective efficacy of a LAV but without risks associated with LAV reversion to virulence. VlhA proteins of MG have indeed been shown to be protective antigens, with anti-serum against a 29 kDa VlhA peptide inhibiting growth of MG in vitro and providing chickens with partial protection against challenge with MG35. Based on their early-phase switched expression in vivo, their potential role in early-phase host-interaction, and their potential to be protective antigens, we included VlhAs 3.03, 4.07, 5.05, and 3.06 in our subunit vaccine.
Given the experimental nature of the vaccine formulation and because different adjuvants can induce highly varied immune responses, we evaluated several adjuvants. We investigated adjuvants with different mechanisms of action including: depot formation causing slow release of antigen (water in oil adjuvants – Montanide ISA 78 VG), speculated activation of inflammatory dendritic cells (Alum), enhancing antigen presentation (oil in water adjuvants – Addavax), and TLR agonists (MPLA, CpG ODNs, Pam2CSK4, Pam3CSK4)36,37,38,39,40,41,42,43,44. No chicken studies have directly compared whether diacylated and triacylated lipoproteins induce meaningfully different responses or outcomes in a vaccine context. Data presented in this study will shed light on this uncertainty. This is especially relevant to MG, which has been reported to have both diacylated and triacylated lipoproteins45.
The hypothesis for our vaccine design is that Chickens vaccinated with our vaccine generate anti-attachment and anti-VlhA antibodies to specific VlhAs dominantly expressed during the initial phase of infection. In the face of such a repertoire of preformed anti-GapA, anti-CrmA and anti-VlhA antibodies, MG attempting to infect the host will be bound by specific antibodies that will minimize their ability to attach. MG that do manage to attach will be met with additional anti-VlhA antibodies each time they attempt to switch to a successive VlhA (Fig. 1). We designed our MG subunit vaccine based on our knowledge of critical attachment proteins and phase-variable surface proteins expressed early during infection in chickens. The impetus for this approach is grounded in our knowledge of genes biologically critical for interaction of MG with the respiratory tract during infection, combined with the need for vaccines of increased safety and efficacy.
Results
Recombinant Proteins had 65–95% Purity
Proteins were made recombinantly to allow for mass production and efficient purification. Recombinant proteins (GapA, CrmA, VlhA 3.03, VlhA 3.06, VlhA 4.07, VlhA 5.05) were produced in E. coli and purified by nickel column affinity chromatography. The presence of the intended recombinant protein was confirmed by LC-MS proteomics run on purified samples. Recombinant proteins achieved purities of 65–95% as determined by densitometry on SDS-PAGE gels depending on the individual subunit and individual preparation (Fig. 2).
Individual purified recombinant proteins. 1, Precision Protein Plus Unstained Standards protein ladder; 2, truncated rGapA (predicted 106 kDa); 3, truncated rCrmA (predicted 102 kDa); 4, rVlhA 3.03 (predicted 71.6 kDa); 5, rVlhA 3.06 (predicted 76.3 kDa); 6, rVlhA 4.07 (predicted 74 kDa); 7, rVlhA 5.05 (predicted 71.5 kDa); 8, negative control (water).
Chicken serum did not recognize MG proteins prior to vaccination
ELISAs evaluating serum reactivity against individual recombinant proteins and MG lysate were performed to confirm a lack of MG exposure prior to the vaccinations and challenges. Pre-vaccination sera from the chickens had minimal observable IgY reactivity against MG lysate or individual subunits (Supplementary Fig. 2).
All recombinant proteins were immunogenic
Chickens were evaluated for serum antibody responses against all individual recombinant proteins and MG lysate to confirm the immunogenicity of the subunit vaccine and to evaluate in later correlations if these antibody responses could predict outcome after infection. All post-vaccination, pre-challenge sera from chickens vaccinated with a subunit formulation showed statistically significant (p ≤ 0.05) increases in IgY against Mg lysate and all individual vaccine subunits as compared to saline-vaccinated control chickens (Fig. 3A–U). The Montanide ISA 78 VG-adjuvanted-vaccine induced the highest serum IgY titers against MG lysate and all VlhAs (Fig. 3A, D–G). The CpG ODN-adjuvanted-vaccine induced the highest serum IgY titers against GapA and CrmA (Fig. 3I, J).
Serum IgY responses from chickens vaccinated with physiologic saline, or with subunits adjuvanted by Montanide ISA 78 VG, Addavax, or Alum (a–g). Serum IgY responses from chickens vaccinated with physiologic saline, or with subunits adjuvanted by MPLA or CpG ODNs (h–n). Serum IgY responses from chickens vaccinated with physiologic saline, or with subunits adjuvanted by Pam2CSK4 or Pam3CSK4 (o-u). Error bars display median group values with 95% confidence intervals. Only statistically significant (p ≤ 0.05) results are shown (*p ≤ 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001). Data points represent individual animals.
No gross lesions were found at necropsy in vaccine groups that showed efficacy
Air sacs were evaluated grossly for pathologic signs of infection. Vaccine injection sites were examined to check for sustained local reactions to vaccine injection. Air sacs were evaluated for gross lesions, indicated by a change from clear to cloudy air sac membranes, and the presence of caseous exudate. In the first study (saline-vaccinated control, Montanide ISA 78 VG, Addavax, Alum), gross air sac lesions were seen in one saline-vaccinated control chicken and in one chicken vaccinated with the Montanide ISA 78VG-adjuvanted vaccine. Both chickens had a caseous exudate in the thoracic air sacs. Neither study two (saline-vaccinated control, MPLA, CpG ODN 2007) nor study three (saline-vaccinated control, Pam2CSK4, Pam3CSK4) had any chickens with gross air sac lesions. Any discoloration identified at the vaccination injection sites was evaluated by histological examination. All chickens receiving the vaccine adjuvanted with Montanide ISA 78 VG had injection-site granulomas. No injection-site granulomas were seen with any other vaccine formulation.
Alum-, MPLA-, CpG ODN-, and Pam2CSK4-adjuvanted-vaccines reduced bacterial recovery
Bacteria was recovered from chicken tracheas to determine how effectively the chickens cleared the MG infection. Three sections of the trachea, from the proximal, middle, and distal regions were placed together into Hayflick’s broth, processed, and the broth was serially diluted to test for the titer of living MG recovered from the vaccinated and challenged chickens.
In the first study, vaccination with the Alum-adjuvanted vaccine resulted in reductions in bacterial recovery (p = 0.0448) compared to saline-vaccinated control chickens (Fig. 4a). In the second study, vaccination with the MPLA- and CpG ODN-adjuvanted-vaccines resulted in significant reductions in bacterial recovery (p = 0.0021, p = 0.0076, respectively) compared to saline-vaccinated control chickens (Fig. 4b). In the third study, vaccination with the Pam2CSK4-adjuvanted vaccine resulted in significant reductions in bacterial recovery (p = 0.0134) as compared to saline-vaccinated control chickens (Fig. 4c).
M. gallisepticum recoveries in color changing units (CCUs) from chickens vaccinated with physiologic saline, or with subunits adjuvanted by Montanide ISA 78 VG, Addavax, or Alum (a). M. gallisepticum CCU recoveries from chickens vaccinated with physiologic saline, or with subunits adjuvanted by MPLA or CpG ODNs (b). M. gallisepticum CCU recoveries from chickens vaccinated with physiologic saline, or with subunits adjuvanted by Pam2CSK4 or Pam3CSK4 (c). Error bars display median group values with 95% confidence intervals. Only comparisons with p < 0.15 are shown. Data points represent individual animals.
CpG ODN-Adjuvanted-Vaccine Reduced Average Tracheal Thickness
Average tracheal thickness of the mucosa and submucosa was evaluated to determine pathology caused by the MG infection. Three sections of the trachea, from the proximal, middle, and distal regions were examined for tracheal mucosal thickening to detect typical lesions induced by the infection. In the first study, no vaccine resulted in significant reductions in average tracheal thickness compared to saline-vaccinated control chickens (Fig. 5a). In the second study, vaccination with the CpG ODN-adjuvanted vaccine resulted in significant reductions in average tracheal thickness (p = 0.0002) compared to saline-vaccinated control chickens (Fig. 5b). In the third study, vaccination with the Pam2CSK4-adjuvanted vaccine trended toward reducing average tracheal thickness (p = 0.1396) compared to saline-vaccinated control chickens (Fig. 5c).
Average tracheal thickness from chickens vaccinated with physiologic saline, or with vaccine adjuvanted by Montanide ISA 78 VG, Addavax, or Alum (a). Average tracheal thickness from chickens vaccinated with physiologic saline, or with vaccine adjuvanted by MPLA or CpG ODNs (b). Average tracheal thickness from chickens vaccinated with physiologic saline, or with vaccine adjuvanted by Pam2CSK4 or Pam3CSK4 (c). Error bars display mean group values with 95% confidence intervals. Only comparisons with p < 0.15 are shown. Data points represent individual animals.
MPLA- and CpG ODN-adjuvanted-vaccines reduced thickest tracheal section
Three sections of the trachea, from the proximal, middle, and distal regions were examined for tracheal mucosal thickening to determine the most extreme example of pathology induced by the MG infection in each chicken. In the first study, the Alum-adjuvanted vaccine trended toward reducing the thickest tracheal section (p = 0.0790) compared to saline-vaccinated control chickens (Fig. 6a). In the second study, vaccination with the MPLA- and CpG ODN-adjuvanted vaccines resulted in significant reductions in the thickest tracheal section (p = 0.0049, p = 0.0050, respectively) compared to saline-vaccinated control chickens (Fig. 6b). In the third study, vaccination with the Pam2CSK4-adjuvanted vaccine trended toward reducing the thickest tracheal section (p = 0.0672) compared to saline-vaccinated control chickens (Fig. 6c).
Thickest tracheal section from chickens vaccinated with physiologic saline, or with vaccine adjuvanted by Montanide ISA 78 VG, Addavax, or Alum (a). Thickest tracheal section from chickens vaccinated with physiologic saline, or with vaccine adjuvanted by MPLA or CpG ODNs (b). Thickest tracheal section from chickens vaccinated with physiologic saline, or with vaccine adjuvanted by Pam2CSK4 or Pam3CSK4 (c). Error bars display mean group values with 95% confidence intervals. Only comparisons with p < 0.15 are shown. Data points represent individual animals.
Montanide ISA 78 VG-Adjuvanted-Vaccine Resulted in Increased Tracheal Wash IgY Responses
Tracheal wash endpoint ELISAs were performed to evaluate both IgY and IgA mucosal antibody responses at the time of necropsy. The group vaccinated with the Montanide ISA 78 VG-adjuvanted vaccine was the only one with significantly different tracheal wash IgY results. It had elevated tracheal wash IgY against the Mg lysate (p ≤ 0.05) compared to all other groups in the study (saline-vaccinated control, Addavax, Alum) (Fig. 7). No groups had significantly different tracheal wash IgA results (Supplementary Fig. 1).
Tracheal wash IgY vs MG Lysate endpoint titers from chickens vaccinated with physiologic saline, or with vaccine adjuvanted by Montanide ISA 78 VG, Addavax, or Alum (a). Tracheal wash IgY endpoint titers from chickens vaccinated with physiologic saline, or with vaccine adjuvanted by MPLA or CpG ODNs (b). Tracheal wash IgY endpoint titers from chickens vaccinated with physiologic saline, or with vaccine adjuvanted by Pam2CSK4 or Pam3CSK4 (c). Error bars display geometric mean titer with 95% confidence intervals. Dashed line indicates the limit of detection. Only statistically significant (p ≤ 0.05) results are shown (*p ≤ 0.05, **p < 0.01, ***p < 0.001). Data points represent individual animals.
Montanide ISA 78 VG-, Alum-, and Pam2CSK4-Adjuvanted-Vaccines had ELISA Data Correlate to Bacterial Recovery
Simple linear regressions were performed to evaluate if ELISA results correlated with bacterial recovery and could thus predict outcome (Supplementary Table 1). For chickens vaccinated with the Montanide ISA 78 VG-adjuvanted-vaccine, post-vaccination serum IgY against GapA (r2 = 0.3045), VlhA 3.03 (r2 = 0.3354), tracheal wash IgY against Mg lysate (r2 = 0.5084), and tracheal wash IgA against Mg lysate (r2 = 0.3652) were all positively correlated with recovery of MG. For chickens vaccinated with the Alum-adjuvanted vaccine, post-vaccination serum IgY against GapA (r2 = 0.5970) and CrmA (r2 = 0.8153) was negatively correlated with recovery of MG. For chickens vaccinated with the Pam2CSK4-adjuvanted vaccine, tracheal wash IgA against Mg lysate (r2 = 0.2644) was positively correlated with recovery of MG. No ELISA results were significantly correlated with recovery of MG for chickens vaccinated with vaccine adjuvanted with Addavax, MPLA, CpG ODNs, or Pam3CSK4.
Montanide ISA 78 VG-, Alum-, MPLA-, CpG ODN-, and Pam3CSK4-adjuvanted-vaccines had ELISA data correlate to average tracheal thickness
Simple linear regressions were performed to evaluate if ELISA results correlated with average tracheal thickness and could thus predict outcome (Supplementary Table 2). For chickens vaccinated with Montanide ISA 78 VG-adjuvanted vaccine, tracheal wash IgY against Mg lysate (r2 = 0.4499) and tracheal wash IgA against Mg lysate (r2 = 0.6845) were positively correlated with average tracheal thickness. For chickens vaccinated with Alum-adjuvanted vaccine, post-vaccination serum IgY against CrmA (r2 = 0.2842) and VlhA 5.05 (r2 = 0.2642) were negatively correlated with average tracheal thickness. For chickens vaccinated with MPLA-adjuvanted vaccine, tracheal wash IgY against Mg lysate (r2 = 0.4519) and tracheal wash IgA against Mg lysate (r2 = 0.7241) were positively correlated with average tracheal thickness. For chickens vaccinated with CpG ODN-adjuvanted vaccine, tracheal wash IgA against Mg lysate (r2 = 0.4473) was positively correlated with average tracheal thickness. For chickens vaccinated with Pam3CSK4-adjuvanted vaccine, post-vaccination serum IgY against Mg lysate (r2 = 0.3161), VlhA 3.03 (r2 = 0.3440), and VlhA 5.05 (r2 = 0.3106) were negatively correlated with average tracheal thickness, whereas tracheal wash IgA against Mg lysate (r2 = 0.4637) was positively correlated with average tracheal thickness. No ELISA resulted were significantly correlated with average tracheal thickness for chickens vaccinated with vaccine adjuvanted by Addavax or Pam2CSK4.
Montanide ISA 78 VG-, Alum-, Addavax-, MPLA-, and CpG ODN-adjuvanted-vaccines had ELISA data correlate to thickest tracheal section
Simple linear regressions were performed to evaluate if ELISA results correlated with thickest tracheal section and could thus predict outcome (Supplementary Table 3). For chickens vaccinated with Montanide ISA 78 VG-adjuvanted vaccine, post-vaccination serum IgY against VlhA 3.03 (r2 = 0.3013), VlhA 5.05 (r2 = 0.3021), tracheal wash IgY against Mg lysate (r2 = 0.4671), and tracheal wash IgA against Mg lysate (r2 = 0.5756) were all positively correlated with thickest tracheal section. For chickens vaccinated with Addavax-adjuvanted vaccine, post-vaccination serum IgY against CrmA (r2 = 0.2863) and VlhA 4.07 (r2 = 0.3191) were negatively correlated with thickest tracheal section. For chickens vaccinated with Alum-adjuvanted vaccine, post-vaccination serum IgY against GapA (r2 = 0.2807) and CrmA (r2 = 0.5330) were negatively correlated with thickest tracheal section, whereas tracheal wash IgA against Mg lysate (r2 = 0.4397) was positively correlated with thickest tracheal section. For chickens vaccinated with MPLA-adjuvanted vaccine, tracheal wash IgA against Mg lysate (r2 = 0.6633) was positively correlated with thickest tracheal section. For chickens vaccinated with CpG ODN-adjuvanted vaccine, post-vaccination serum IgY against VlhA 3.06 (r2 = 0.2939) and VlhA 4.07 (r2 = 0.2912) were positively correlated with thickest tracheal section. No ELISA results were significantly correlated with thickest tracheal section for chickens vaccinated with vaccine adjuvanted by Pam2CSK4 or Pam3CSK4.
Discussion
We have demonstrated that our subunit vaccine formulation containing the CpG ODN 2007 adjuvant provides protection against Mg disease in chickens as determined by significant decreases in recoverable MG load from the trachea and significant decreases in both average tracheal thickness and thickest tracheal section. Average tracheal thickness has been the standard measure for assessing MG disease due to its objective nature, lack of advanced skills needed to take it, experimental reproducibility, correlation with lesion severity, and translatability across researchers46,47. Thickest tracheal section is a non-standard measure we have taken to improve the sensitivity of the tracheal thickness assessment. This measurement provides resolution that can discern between a chicken with very few, sparse tracheal lesions, and a chicken with no lesions at all.
Although vlhA 3.03, 4.07/4.07.6, 5.05, 4.07.1/4.08, and 3.06 are the vlhAs predominantly expressed in-vivo during the first seven days of infection with Rlow, we only included VlhAs 3.03, 3.06, 4.07, and 5.05 in our vaccine. VlhA 4.07 differs from its tandem repeat VlhA 4.07.6 by two amino acids, and they share 99.85% identity. VlhA 3.06 differs from VlhA 4.07.1 and its tandem repeat VlhA 4.08 by 27 and 12 amino acids, sharing 98.69% and 99.27% identity, respectively. Although VlhAs 4.07.6, 4.07.1, and 4.08 were not included within the vaccine, the VlhAs that were included cover the breadth of early phase-expressed in-vivo vlhAs. This had the additional advantage of reducing the subunits required within the vaccine, making it easier to produce.
The vaccine subunits proved immunogenic when paired with any of the adjuvants tested. The Montanide ISA 78 VG and CpG ODN adjuvants resulted in the strongest immunogenicity, as determined by post-vaccination serum IgY antibody titers. The low serum IgY responses to Mg lysate relative to the purified subunits were expected. The subunit protein targets are only a fraction of the total proteome of Mg. Furthermore, data have shown that Mg strain Rlow predominantly expresses vlhA 3.03, and comparatively, has very low expression of all other vlhAs when grown in broth31. Because the MG used to make the MG lysate was grown in broth, antibodies specific for VlhAs 3.06, 4.07, or 5.05 likely lacked abundant specific targets in the lysate. Furthermore, even the proteins likely to be represented in the lysate (GapA, CrmA, and VlhA 3.03) were present at far lower concentrations than were used when testing the individual immunogenicity of the recombinant proteins. Taken together, this explains the low immunogenicity of the subunit vaccine when assessed using MG lysate. All subunit proteins appear to have similar levels of immunogenicity with slight differences based on adjuvant used.
It is believed protection against disease caused by MG is primarily antibody mediated. An experimental live-attenuated strain (TS 100) was found to induce protection in hosts lacking a thymus, but not in those lacking the bursa of Fabricius48. An assessment of the LAV strain GT5 found that vaccinated chickens had higher levels of IgY and IgY secreting plasma cells in the tracheal lamina propria compared with sham vaccinated chickens49. GT5 vaccinated chickens also had lower numbers of CD4+ and CD8+ cells infiltrating the tracheal mucosa compared with sham vaccinated chickens50. Vaccine strain ts-11 is believed to drive protection primarily through memory B cells in the mucosa51. Previous work identified that T-cells were found to make up the bulk of the lymphocytes initially infiltrating into the trachea following challenge with pathogenic Mg. Another study demonstrated that B-cells were detected around week 3 post-vaccination and were seen in tandem with a drop in tracheal mycoplasma DNA52. It has also been shown for vaccine strain ts-304 that vaccinated chickens have almost no T-cell infiltration into the mucosa at 14 days post challenge, whereas there is some B-cell infiltration. This is in stark contrast to the unvaccinated chickens in that study which showed considerable T-cell infiltration51.
In the studies described here, correlations between tracheal IgY or IgA and outcome measures were either not significant, or they were positively correlated with worse outcome measures. It should be noted that proliferation of B cells in the tracheal mucosa and mucosal antibody production are different measures, and thus this does not conclude that B-cells in the tracheal mucosa are a maladaptive response induced by the different formulations of the subunit vaccine. Neither tracheal IgY nor IgA was ever negatively correlated with worse outcome measures in our studies. This shows that a detectable tracheal IgY or IgA response at our necropsy timepoint may be indicative that the chickens were still struggling with infection rather than that they were protected. This is supported by previously published work showing that sham vaccinated chickens had higher tracheal wash anti-Mg IgA than chickens that were vaccinated with GT549.
When correlating serum IgY titers with outcome measures, the results differed between the vaccines. This indicates protection may be driven by different mechanisms when using different adjuvants. Serum IgY titers against the Mg lysate or individual subunits were typically negatively correlated with the outcome measures. The two exceptions were for Montanide ISA 78 VG, which curiously induced serum IgY titers positively correlated with numerous outcome measures, and CpG ODNs which induced anti-VlhA 3.06 and anti-VlhA 4.07 titers positively correlated with the thickest tracheal section. It could be that serum IgY titers were a proxy for how strongly the chickens responded to some of the vaccines, rather than having a causative relationship to protection. A serum passive transfer study would help determine the role of anti-Mg serum IgY responses. Serum IgY titers were most predictive of outcome measures for Alum-vaccinated chickens. The strikingly high negative correlation between serum anti-CrmA IgY titers and bacterial recovery (Supplementary Table 1) indicates that these antibodies are a good predicter of bacterial clearance in chickens vaccinated with our Alum-adjuvanted subunit vaccine.
When compared with saline-vaccinated control chickens, our subunit vaccine resulted in reduced bacterial burdens in the trachea with every formulation used with median reductions ranging from 5-fold to 125-fold (Fig. 4). This drop in bacterial burden shows that the subunit vaccine was either preventing bacterial attachment at the time of infection, substantially reducing the time it takes to clear the infection, or both. Should a vaccinated chicken become infected, this suggests that they may decrease the risk of transmission because the chickens have fewer bacteria present that can be shed and potentially infect other chickens.
Compared to saline-vaccinated control chickens, all formulations except the formulation adjuvanted with Montanide ISA 78VG resulted in a mean reduction in average tracheal thickness, and all formulations resulted in mean reductions in the thickest tracheal sections (Figs. 5 and 6). This indicates that the vaccine either led to reduced pathology during infection, a faster resolution of pathology after infection, or both. The striking 125-fold median reduction in bacterial recovery in conjunction with significantly reduced average tracheal thickness and thickest tracheal section seen with the CpG ODN-adjuvanted vaccine suggests that this adjuvant is the best of our tested adjuvants to include in our subunit vaccine (Figs. 4–6).
T-cell involvement was not investigated in these studies but may be responsible for many of the differences seen. Unvaccinated chickens have been shown to have initially infiltrating natural killer cells with infiltration of CD8+ T-cells and CD4 + T-cells increasing over the following weeks. Although this occurs, its unknown if this response contributes to protection52.
Given that dysregulation of Th1/Th2 responses has been associated with chronic infection, it is plausible that certain adjuvants in tandem with our subunit formulation commit to T-cell subsets with different levels of impact53. Given that Th polarization also affects the outcome of other mycoplasma infections, it is logical that whichever Th response is pushed, will also greatly affect vaccine efficacy54. Our data suggest that TH2 skewing adjuvants tend to perform well, given that Alum, TLR2 agonists, and class B CpG ODNs all tend to push TH2 responses39,55. However, this does not seem to be an absolute requirement given the efficacy of the TLR-4 agonist adjuvant, which is known to skew toward TH1 responses56. Unvaccinated chickens challenged with MG strain AP3AS have responses that tended to skew away from TH2 polarization51. These heightened anti-TH2 responses were not seen in Ts-304 vaccinated and AP3AS challenged chickens during the same study. This further supports the notion that TH2 responses may be the more helpful immune responses against M. gallisepticum infection.
The dose of adjuvant may have influenced results considerably. Montanide ISA 78VG, Addavax, and Alum are all dosed based on injection volume. Outcomes of these adjuvants may change with differing vaccination volume as a result. MPLA, CpG ODNs, Pam2CSK4 and Pam3CSK4 were all dosed based on gram amounts. MPLA and CpG ODNs were used at a 5,000 times higher dose than Pam2CSK or Pam3CSK4. It is conceivable that at a higher dose, Pam2CSK4 or Pam3CSK may result in significant improvements in all three main outcome measures. This is more likely for Pam2CSK4 which was significant or trending toward significant results in all three main outcome measures.
Because the VlhAs were expressed recombinantly in E. coli with a lipoprotein signal sequence, it is possible that these proteins contain triacylated lipid domains57. This means that the recombinant VlhAs alone may be driving activation of the TLR2A/TLR1LB and TLR2B/TLR1LA heterodimers. Thus, the Pam3CSK4 adjuvanted group could be experiencing a more TLR-specific immune response compared to the mixed-TLR response likely seen with the other adjuvants. Our data demonstrate that if a meaningful difference exists between using diacylated or triacylated lipoproteins in a vaccine context for chicken, it was not discernable at this dosage.
Our work highlights the value of our biologically informed and rational approach to developing a vaccine to combat MG disease.
Methods
Studies Performed
Data were generated across three vaccination-challenge studies. Control groups were solely injected with saline and are referred to as saline-vaccinated controls. The first study compared a saline-vaccinated control to vaccine adjuvanted with Montanide ISA 78 VG, Addavax, or Alum. The second study compared a saline-vaccinated control to vaccine adjuvanted with either MPLA or CpG ODN 2007. The third study compared a saline-vaccinated control to vaccine adjuvanted with either Pam2CSK4 or Pam3CSK4. For all experiments, n = 15 chickens were used per group. Rarely, chickens were euthanized prior to the end of the study for reasons unrelated to the study and were thus not included in the analysis.
Plasmid design and protein production
All gene sequences were taken from the Mycoplasma gallisepticum Rlow genome. GapA and CrmA were designed as truncated proteins to improve expression and water solubility. Truncation of GapA and CrmA was performed by removing non-extracellular domains as predicted by DeepTMHMM. Both truncated GapA and truncated CrmA were designed in pET-27b(+) plasmids with a 10x HIS-tag on the C-terminal ends of the proteins. All VlhAs were designed in pET-28b(+) plasmids with an E. coli lipoprotein signal sequence (Biomatik, Wilmington DE). A 6x HIS-tag was added on the C-terminal ends of the proteins. Plasmids were used to transform BL21(DE3) E. coli for expression. Transformed E. coli were grown in Expression Medium (19 g Bacto-tryptone, 24 g yeast extract, 10 g 5 × M9 minimal salts, 4 mL 100% glycerol, topped to 1 L with distilled water, with the pH adjusted to 7.1 with sodium hydroxide) at 37 °C, with shaking at 200 rpm until OD600 > 1 at which point expression was induced with 0.5 mM IPTG and they were incubated at 16 °C, with shaking at 200 rpm, overnight. The culture was then aliquoted, pelleted, and the pellets were frozen at −20 °C. Protein was extracted using Bacterial Protein Extract Reagent (ThermoFisher, Waltham MA) as per the manufacturer’s protocol.
Expressed recombinant proteins were purified using HisPurTM Ni-NTA Spin Columns (ThermoFisher, Waltham MA) as per the manufacturer’s protocol. The presence of recombinant proteins was confirmed by LC-MS proteomics. Protein purity was determined by densitometry using Image Lab (Bio-Rad software) run on images taken by a Chemidoc imager (Bio-Rad, Hercules CA) obtained from SDS-PAGE gels using Mini-PROTEAN TGX Stain-Free Gels (Bio-Rad, Hercules CA). Protein concentration was determined by Qubit 2.0 Fluorometer. Proteins were flash frozen in liquid nitrogen and placed at -80 °C for future use.
Vaccine formulations and preparations
500 µL of sterile physiologic saline (.9% NaCl) was given to saline-vaccinated control groups. Vaccines were formulated to contain 50 µg each of GapA, CrmA, VlhA 3.03, VlhA 3.06, VlhA 4.07, and VlhA 5.05 for a total dose of 300 µg. All vaccines were formulated to be given in 500 µL volumes. Sterile physiologic saline was added if needed to attain necessary volume prior to adjuvant mixing. The Montanide ISA 78 VG-adjuvanted formulation was prepared by mixing the full protein formulation with Montanide ISA 78 VG (Seppic, Fairfield NJ) in a v/v ratio of 3:7, respectively. This was combined in an apparatus containing an MX494 double female leur lock (Smiths Medical, Dublin OH) with two NORM-JECT© Leur Lock Solo 2 mL syringes attached on either end (Air-Tite Products Co., Virginia Beach VA). The mixture was then injected back and forth for 20 cycles at a speed of 8 seconds per cycle (back and forth is 1 cycle). Then the mixture was injected back and forth for 60 cycles as fast as possible. Successful preparation was confirmed by performing a drop test in water and viewing a lack of mixing with the water. The Addavax-adjuvanted formulation was prepared by mixing the full protein formulation with Addavax (Invivogen, San Diego CA) in a v/v ratio of 1:1 and mixing by pipetting as per the manufacturer’s protocol. The Alum-adjuvanted formulation was prepared by mixing the full protein formulation with Alhydrogel 2% (Invivogen, San Diego CA) in a v/v ratio of 1:1 and mixing by pipetting as per the manufacturer’s protocol. The MPLA-adjuvanted formulation was prepared by mixing the full protein formulation with 25 µg of MPLA-SM* (Invivogen, San Diego CA) per dose and mixing by pipetting as per the manufacturers protocol. The CpG ODN-adjuvanted formulation was prepared by mixing the full protein formulation with 25 µg of CpG ODN 2007 (Invivogen, San Diego CA) per dose and mixing by pipetting as per the manufacturers protocol. The Pam2CSK4-adjuvanted formulation was prepared by mixing the full protein formulation with 5 ng of Pam2CSK4 (Invivogen, San Diego CA) per dose and mixing by pipetting as per the manufacturers protocol. The Pam3CSK4-adjuvanted formulation was prepared by mixing the full protein formulation with 5 ng of Pam3CSK4 (Invivogen, San Diego CA) per dose and mixing by pipetting as per the manufacturers protocol. Doses were selected based on published research, manufacturer recommendations, or a combination of the two. Protein formulations within each study were prepared prior to aliquotting for combination with various adjuvants to help prevent within-study dose differences.
Adjuvants
Montanide ISA78 VG is a water in oil adjuvant. Water in oil adjuvants work by associating the antigen with the water phase. These water and antigen droplets are surrounded by oil. When injected, this mixture forms a depot at the injection site that allows for slow, continuous release of antigen. These adjuvants may also recruit immune cells to their location36,37. Water in oil adjuvants commonly polarize toward TH1 responses58. They tend to cause significant inflammatory reactions at injection sites that cause strong immune responses but are also notorious for causing granulomas38.
Addavax is an oil in water adjuvant. It is similar to MF59 and is a squalene-based nano emulsion. Addavax tends to cause a mixed TH1/TH2 response59,60. Squalene based oil in water adjuvants work by rapidly priming the immune system via non-degradative endocytosis. This presents intact antigen and transports it quickly to draining lymph nodes40. Squalene-based oil in water adjuvants have been found to both activate CD8+ T-cells by a RIPK3-dependent pathway and activate B-cells by a RIPK3-indepdent pathway61.
Alhydrogel 2% is an alum-based adjuvant. Alum tends to polarize toward TH2 responses. The exact mechanism of action of Alum is not known. It is believed to activate inflammatory dendritic cells by inducing the formation of uric acid39. Alum adjuvants may form depots, but these are dispensable for the induced immune response62. Alum may also assist in stabilizing the structure of antigens that adsorb to it63.
Chickens have different toll-like receptors than other species. The chicken TLR repertoire includes TLR1LA, TLR1LB, TLR2A, TLR2B, TLR3, TLR4, TLR5, TLR7, TLR15, and TLR2164. Monophosphoryl lipid A (MPLA) is similar in structure to lipopolysaccharide except that it has one fewer phosphate groups in the Lipid A region. This change limits its inflammatory toxicity while retaining its TLR4 agonist ability41. This is recognized by chicken TLR465. CpG ODN 2007 is a class B (also known as “K” type) CpG ODN. This type of CpG ODN is a potent B-cell stimulator66,67. CpG ODNs are TLR9 agonists, but in chickens these compounds are recognized by TLR2142. Pam2CSK4 is a synthetic diacylated lipopeptide. It is a TLR2/6 agonist. In chickens, diacylated lipopeptides are recognized by the TLR2A/TLR1LB heterodimer, the TLR2B/TLR1LA heterodimer, and TLR1543. However, the TLR2A/TLR1LB heterodimer cannot recognize all diacylated lipopeptides, as evidenced by its inability to respond to the diacylated lipopeptide macrophage-activating lipopeptide (Malp-2)44. The extent to which TLR15 recognizes diacylated lipopeptides is unknown. Pam3CSK4 is a synthetic triacylated lipopeptide. It is a TLR2/1 agonist. In chickens, triacylated lipopeptides are recognized by the TLR2A/TLR1LB heterodimer and the TLR2B/TLR1LA heterodimer44.
Infection studies
All animal studies were approved and performed in accordance with our Institutional Animal Care and Use Committee (IACUC) Protocol (#A22-008). Four-week-old specific pathogen free female white leghorn chickens (Charles River, Willimantic CT) were randomly allocated into HEPA-filtered isolators in groups of 15 upon arrival. They were acclimated for one week. Water and non-medicated feed were provided ad libitum. Chickens were identified by leg banding and then blood was collected from the wing vein or jugular vein. The next day, chickens were prime-vaccinated. Chickens were vaccinated subcutaneously between the back and right wing with 500 µL of physiologic saline or of the specified vaccine formulation. Three weeks later, chickens were boost-vaccinated with the same vaccine dose and route. Blood was collected from chickens 20 days later from the wing vein or jugular vein. At three weeks post-boost vaccination, chickens were challenged intratracheally on D0 with estimated counts of 1* 108 CFU of Mycoplasma gallisepticum as determined by the optical density at 620 nm. Strain Rlow was used and given in 200 µL of Hayflick’s media delivered by a P200 pipette with a gel loading tip. Chickens were challenged a second time using the same dose and route on D2. Chickens were infected in sets of five chickens per group, cycling between the different groups. Chickens were euthanized on D14. Chickens were euthanized in sets of five chickens cycling between the different groups. Euthanasia was carried out by the injection of Telazol (Covetrus, Portland ME) into the breast muscle at a dose of 10 mg/kg followed by cervical dislocation upon full anesthetization, as determined by lack of a palpebral reflex. Chickens were necropsied and the gross lesions in the air-sacs were evaluated. Tracheas were harvested and separated into sections.
Preparation of Inoculum
Frozen tubes containing 1 mL of passage 14 Mycoplasma gallisepticum strain Rlow were thawed and inoculated into 19 mL of Hayflick’s medium (10% horse serum and 5% yeast extract). Cultures were grown for 24 hours at 37 °C until mid-log phase was reached as determined by a color shift from red to orange. Tubes were then centrifuged at 10,000 × g for 10 minutes. The bacterial pellets were resuspended in 10 mL of fresh Hayflick’s medium per tube grown. 400 µL of inoculum was used to determine OD620 blanked with 400 µL of fresh Hayflick’s medium. This process was then repeated and averaged. The tube containing Rlow was then centrifuged at 10000xg for 10 minutes. The bacterial pellet was resuspended with fresh Hayflick’s medium to a concentration of 5.0* 108 CFU/mL. The inoculum was then divided amongst 1.5 mL tubes with repeated mixing by pipetting to prevent dose differences caused by bacterial settling. The unused and remaining used stocks of inoculum post-infection were serially diluted in a 96 well plate and incubated at 37 °C for 28 days to confirm that the inoculum dose was viable.
Preparation of heat-inactivated chicken serum
Blood samples that were collected from the chickens pre-vaccination (D-1 of prime vaccination) and post-boost vaccination/pre-challenge (D-1 of infection) were processed identically. Blood was incubated at room temperature for >1 hour to allow for clotting. Clots were then rimmed with a P200 pipette tip. Tubes containing blood were centrifuged at 1000 × g for 10 minutes. The serum was carefully pipetted off and separated into another tube. The serum was then heat inactivated. Heat-inactivated serum was then stored at −20 °C for future use in ELISAs determining systemic immunoglobulin responses.
Indirect enzyme-linked immunosorbent assays (ELISAs)
Serum and tracheal wash antibody responses were evaluated by ELISA. Nunclon Maxisorp plates (Thermo Fisher Scientific, Waltham MA) were used for serum IgY ELISAs and tracheal wash IgY endpoint titers. Immulon 2HB plates were used for tracheal wash IgA endpoint titers (Thermo Fisher Scientific, Waltham MA). Plates were coated for 1 hour at 37 °C with 100 µL carb/bicarb buffer containing. 5 µg/mL desired antigen per well. Plates were then washed 3 × with PBST containing 0.05% Tween-20 and blocked for 1 hour at room temperature with 100 µL of 3% (w/v) bovine serum albumin diluted in PBST. Plates were washed 3x with PBST. Serum samples were diluted 1:1000 in PBST and tracheal wash samples were diluted 1:250 in PBST. Samples were loaded into wells as 100 µL volumes and incubated for 1 hour at room temperature. Plates were then washed 3x with PBST. The secondary antibody, HRP-conjugated goat anti-chicken IgY (Sigma-Aldrich, Saint Louis MO) or HRP-conjugated goat anti-chicken IgA (Invitrogen, Carlsbad CA), was diluted in PBST as per manufacturer’s instructions, loaded at 100 µL per well, and incubated for 1 hour at room temperature. Plates were then washed 3x with PBST. 100 µL TMB Substrate Solution was added to each well and plates were incubated for 3:30 min (serum IgY ELISAs), 2:35 min (tracheal wash IgY ELISAs), 3:00 min (tracheal wash IgA ELISAs), or 15:00 min (tracheal wash IgY and IgA endpoint ELISAs), at which point the development was stopped with 100 µL TMB-STOP Solution per well. The plate was then immediately read at 450 nm on a Cytation 5 plate reader (Biotek, Winooski VT).
Bacterial Recoveries
Three sections of 1 cm in length each were removed from the proximal, middle, and distal portions of the trachea (three total sections per trachea) and placed together into tubes containing 3 mL of Hayflick’s media. The tube was then placed on ice. Upon completion of the necropsies, tubes were vortexed 4 × for 30 seconds each time and incubated at 37 °C for 3 hours. Samples were then filtered through. 45 µM WhatmanTM UniflowTM disposable sterile syringe filters (Cytiva, Marlborough MA). 200 µL of sample was loaded in duplicate into a 96 well plate. Fivefold serial dilutions were performed into fresh Hayflick’s medium. The plate was sealed, wrapped in Parafilm, and incubated at 37 °C for 28 days. The tubes were also incubated at 37 °C for 28 days. Growth was determined by a medium color shift from red to yellow. The duplicate wells were averaged to determine color changing units.
Histology and Tracheal Measurements
Three sections of 0.5 cm in length each were taken from the proximal, middle, and distal portions of the trachea (three total sections per trachea) and placed together into tubes containing 5 mL of 10% neutral buffered formalin for histology. Tissues fixed at room temperature with shaking at 100 rpm for 24–48 hours. Tissues were then trimmed and submitted for hematoxylin and eosin staining. Upon receiving the stained slides, they were blinded by someone other than the measurer. The thickness of the mucosa and submucosa of the tracheal rings was measured using a microscope with a gradation bar. Measurements were taken at 12 o’ clock, 3 o’ clock, 6 o’ clock, and 9 o’ clock. In the event of an artifact, the closest measurable section was used. These twelve measurements were converted to micrometers and averaged to determine average tracheal thickness. The single thickest mucosal section found anywhere amongst any of the three tracheal rings was measured, converted to micrometers, and reported as the thickest tracheal section.
Tracheal PBS washes
The remaining tracheal sections not used for recoveries or histopathological examination were flushed with the same 1 mL of sterile phosphate buffered saline through the lumen four times. These samples were frozen at –20 °C for future ELISAs evaluating tracheal antibody responses.
Statistical analyses
All statistical analyses were performed using GraphPad Prism 9. Statistical analyses on average tracheal thickness, thickest tracheal section, bacterial recoveries, serum IgY titers, and tracheal wash endpoint titers were performed using a non-parametric One-Way ANOVA on ranks (Kruskal-Wallis) with a Dunn’s post-hoc test for multiple comparisons. Correlations between ELISA results, average tracheal thickness, thickest tracheal section, and bacterial recoveries were performed using simple linear regressions. MG recoveries and tracheal wash endpoint titers were log10 transformed for correlation analyses.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Ley, D. H. Diseases of Poultry, 12th ed. in Diseases of Poultry (eds. Saif, Y. et al.) 807–834 (Blackwell Publishing Press, Ames, IA, 2008).
Carpenter, T. E., Mallinson, E. T., Miller, K. F., Gentry, R. F. & Schwartz, L. D. Vaccination with F-strain Mycoplasma gallisepticum to reduce production losses in layer chickens. Avian Dis. 25, 404–409 (1981).
Johnson, D. C., Emory, W. H., Kleven, S. H. & Stallknecht, D. E. A Mycoplasma gallisepticum epornitic in turkeys: its epidemiology and eradication. Avian Dis. 25, 1047–1052 (1981).
Mohammed, H. O., Carpenter, T. E. & Yamamoto, R. Evaluation of factors associated with infection of commercial layers with Mycoplasma gallisepticum and M. synoviae. Avian Dis. 31, 470–476 (1987).
Mohammed, H. O., Carpenter, T. E. & Yamamoto, R. Economic impact of Mycoplasma gallisepticum and M. synoviae in commercial layer flocks. Avian Dis. 31, 477–482 (1987).
Stipkovits, L. & Kempf, I. Mycoplasmoses in poultry. Rev. Sci. Tech. Int. Epizoot. 15, 1495–1525 (1996).
USDA. National Poultry Improvement Plan Program Standards. (2019).
Yoder, H. W. Avian Mycoplasmas. in Diagnostic Procedure in Veterinary Bacteriology and Mycology 333–341 https://doi.org/10.1016/B978-0-12-161775-2.50030-X (Elsevier, 1990).
Ferguson-Noel, N. M. & Williams, S. M. The efficacy of Mycoplasma gallisepticum K-strain live vaccine in broiler and layer chickens. Avian Pathol. 44, 75–80 (2015).
Whithear, K. G., Soeripto, Harringan, K. E. & Ghiocas, E. Safety of temperature sensitive mutant Mycoplasma gallisepticum vaccine. Aust. Vet. J. 67, 159–165 (1990).
Kanci Condello, A. et al. Mycoplasma gallisepticum strain ts-304 is a safe and effective live attenuated vaccine for use in chickens. Vet. Microbiol. 244, 108654 (2020).
Evans, R. D. & Hafez, Y. S. Evaluation of a Mycoplasma gallisepticum strain exhibiting reduced virulence for prevention and control of poultry mycoplasmosis. Avian Dis. 36, 197–201 (1992).
Burnham, M. R., Branton, S. L., Peebles, E. D., Lott, B. D. & Gerard, P. D. Effects of F-strain Mycoplasma gallisepticum inoculation at twelve weeks of age on performance and egg characteristics of commercial egg-laying hens. Poult. Sci. 81, 1478–1485 (2002).
Lin, M. Y. & Kleven, S. H. Cross-immunity and antigenic relationships among five strains of Mycoplasma gallisepticum in young Leghorn chickens. Avian Dis. 26, 496–507 (1982).
Lin, M. Y. & Kleven, S. H. Correlation of titer, preservation method, and storage of Mycoplasma gallisepticum F strain and the immune response in chickens. Avian Dis. 28, 273–277 (1984).
Ricketts, C. et al. Identification of strain-specific sequences that distinguish a mycoplasma gallisepticum vaccine strain from field isolates. J. Clin. Microbiol. 55, 244–252 (2017).
Talkington, F. D. & Kleven, S. H. Evaluation of protection against colonization of the chicken trachea following administration of Mycoplasma gallisepticum bacterin. Avian Dis. 29, 998–1003 (1985).
Abdelwhab, E. M. et al. Detection and molecular characterization of Mycoplasma gallisepticum field infection in TS-11-vaccinated broiler breeders. J. Appl. Poult. Res. 20, 390–396 (2011).
Bwala, D. G., Solomon, P., Duncan, N., Wandrag, D. B. R. & Abolnik, C. Assessment of Mycoplasma gallisepticum vaccine efficacy in a co-infection challenge model with QX-like infectious bronchitis virus. Avian Pathol. 47, 261–270 (2018).
Ley, D. H. et al. Transmissibility of live Mycoplasma gallisepticum vaccine strains ts-11 and 6/85 from vaccinated layer pullets to sentinel poultry. Avian Dis. 41, 187–194 (1997).
Steinlage, S. J. T. et al. Isolation and characterization of a 6/85-like mycoplasma gallisepticum from commercial laying hens. Avian Dis. 47, 499–505 (2003).
El Gazzar, M., Laibinis, V. A. & Ferguson-Noel, N. Characterization of a ts-11–like Mycoplasma gallisepticum isolate from commercial broiler chickens. Avian Dis. 55, 569–574 (2011).
Armour, N. K. & Ferguson-Noel, N. Evaluation of the egg transmission and pathogenicity of Mycoplasma gallisepticum isolates genotyped as ts-11. Avian Pathol. 44, 296–304 (2015).
Leigh, S. A. & Evans, J. D. Genetic comparison of the Mycoplasma gallisepticum 6/85 vaccine strain and 6/85-like field isolates. Vet. Microbiol. 291, 110008 (2024).
Papazisi, L. et al. GapA and CrmA coexpression is essential for Mycoplasma gallisepticum cytadherence and virulence. Infect. Immun. 70, 6839–6845 (2002).
Indiková, I. et al. Role of the GapA and CrmA Cytadhesins of Mycoplasma gallisepticum in promoting virulence and host colonization. Infect. Immun. 81, 1618–1624 (2013).
Goh, M. S., Gorton, T. S., Forsyth, M. H., Troy, K. E. & Geary, S. J. Molecular and biochemical analysis of a 105 kDa Mycoplasma gallisepticum cytadhesin(GapA). Microbiology 144, 2971–2978 (1998).
Noormohammadi, A. H., Markham, P. F., Duffy, M. F., Whithear, K. G. & Browning, G. F. Multigene families encoding the major Hemagglutinins in phylogenetically distinct mycoplasmas. Infect. Immun. 66, 3470–3475 (1998).
Noormohammadi, A. H. et al. Mycoplasma synoviae has two distinct phase-variable major membrane antigens, one of which is a putative hemagglutinin. Infect. Immun. 65, 2542–2547 (1997).
Markham, P. F., Glew, M. D., Browning, G. F., Whithear, K. G. & Walker, I. D. Expression of Two Members of the pMGA Gene Family of Mycoplasma gallisepticum Oscillates and Is Influenced by pMGA-Specific Antibodies. Infect. Immun. 66, 2845–2853 (1998).
Pflaum, K., Tulman, E. R., Beaudet, J., Liao, X. & Geary, S. J. Global changes in mycoplasma gallisepticum phase-variable Lipoprotein gene vlhA expression during in vivo infection of the natural chicken host. Infect. Immun. 84, 351–355 (2016).
Pflaum, K. et al. The influence of host tissue on M. gallisepticum vlhA gene expression. Vet. Microbiol. 251, 108891 (2020).
Noormohammadi, A. H. Role of phenotypic diversity in pathogenesis of avian mycoplasmosis. Avian Pathol. 36, 439–444 (2007).
Tulman, E. R. et al. Extensive variation in surface lipoprotein gene content and genomic changes associated with virulence during evolution of a novel North American house finch epizootic strain of Mycoplasma gallisepticum. Microbiology 158, 2073–2088 (2012).
Saito, S. et al. Cloning and DNA sequence of a 29 kilodalton polypeptide gene of Mycoplasma gallisepticum as a possible protective antigen. Vaccine 11, 1061–1066 (1993).
Awate, S., Babiuk, L. A. & Mutwiri, G. Mechanisms of action of adjuvants. Front. Immunol. 4, 1–10 (2013).
Jansen, T., Hofmans, M. P. M., Theelen, M. J. G. & Schijns, V. E. J. C. Structure–activity relations of water-in-oil vaccine formulations and induced antigen-specific antibody responses. Vaccine 23, 1053–1060 (2005).
Tizard, I. R. Adjuvants and adjuvanticity. in Vaccines for Veterinarians 75-86.e1 https://doi.org/10.1016/B978-0-323-68299-2.00016-2 (Elsevier, 2021).
Kool, M. et al. Alum adjuvant boosts adaptive immunity by inducing uric acid and activating inflammatory dendritic cells. J. Exp. Med. 205, 869–882 (2008).
Nguyen-Contant, P., Sangster, M. Y. & Topham, D. J. Squalene-based influenza vaccine adjuvants and their impact on the hemagglutinin-specific B cell response. Pathogens 10, 355 (2021).
Fensterheim, B. A. et al. The TLR4 agonist Monophosphoryl Lipid A drives broad resistance to infection via dynamic reprogramming of macrophage metabolism. J. Immunol. 200, 3777–3789 (2018).
Brownlie, R. et al. Chicken TLR21 acts as a functional homologue to mammalian TLR9 in the recognition of CpG oligodeoxynucleotides. Mol. Immunol. 46, 3163–3170 (2009).
Oven, I. et al. Diacylated lipopeptide from Mycoplasma synoviae mediates TLR15 induced innate immune responses. Vet. Res. 44, 99 (2013).
Higuchi, M. et al. Combinational recognition of bacterial lipoproteins and peptidoglycan by chicken Toll-like receptor 2 subfamily. Dev. Comp. Immunol. 32, 147–155 (2008).
Jan, G., Fontenelle, C., Le Hénaff, M. & Wróblewski, H. Acylation and immunological properties of Mycoplasma gallisepticum membrane proteins. Res. Microbiol. 146, 739–750 (1995).
Kulappu Arachchige, S. N. et al. Measures of tracheal lesions are more discriminatory and reproducible indications of chronic respiratory disease caused by Mycoplasma gallisepticum in poultry. Avian Pathol. 51, 550–560 (2022).
Nunoya, T., Tajima, M., Yagihashi, T. & Sannai, S. Evaluation of respiratory lesions in chickens induced by Mycoplasma gallisepticum. Jpn. J. Vet. Sci. 49, 621–629 (1987).
Lam, K. M. & Lin, W. Resistance of chickens immunized against Mycoplasma gallisepticum is mediated by bursal dependent lymphoid cells. Vet. Microbiol. 9, 509–514 (1984).
Papazisi, L. et al. A modified live Mycoplasma gallisepticum vaccine to protect chickens from respiratory disease. Vaccine 20, 3709–3719 (2002).
Javed, M. A. et al. Correlates of immune protection in chickens vaccinated with Mycoplasma gallisepticum Strain GT5 following challenge with pathogenic M. gallisepticum Strain R low. Infect. Immun. 73, 5410–5419 (2005).
Kulappu Arachchige, S. N. et al. Mucosal immune responses in the trachea after chronic infection with Mycoplasma gallisepticum in unvaccinated and vaccinated mature chickens. Cell. Microbiol. 23, 1–17 (2021).
Gaunson, J. E., Philip, C. J., Whithear, K. G. & Browning, G. F. The cellular immune response in the tracheal mucosa to Mycoplasma gallisepticum in vaccinated and unvaccinated chickens in the acute and chronic stages of disease. Vaccine 24, 2627–2633 (2006).
Miao, Y. et al. Mycoplasma gallisepticum induced inflammation-mediated Th1/Th2 immune imbalance via JAK/STAT signaling pathway in chicken trachea: Involvement of respiratory microbiota. Vet. Microbiol. 265, 109330 (2022).
Zhao, J., Wang, X. & Wang, Y. Relationships between Th1/Th2 cytokine profiles and chest radiographic manifestations in childhood Mycoplasma pneumoniae pneumonia. Ther. Clin. Risk Manag. 12, 1683–1692 (2016).
Martinson, J. A. et al. Impact of class A, B and C CpG‐oligodeoxynucleotides on in vitro activation of innate immune cells in human immunodeficiency virus‐1 infected individuals. Immunology 120, 526–535 (2007).
Netea, M. G., Van Der Meer, J. W. M., Sutmuller, R. P., Adema, G. J. & Kullberg, B.-J. From the Th1/Th2 Paradigm towards a Toll-Like Receptor/T-Helper Bias. Antimicrob. Agents Chemother. 49, 3991–3996 (2005).
Braun, V. & Hantke, K. Lipoproteins: Structure, Function, Biosynthesis. in Bacterial Cell Walls and Membranes (ed. Kuhn, A.) vol. 92 39–77 (Springer International Publishing, Cham, 2019).
Riteau, N. et al. Water-in-oil–only adjuvants selectively promote T follicular helper cell polarization through a Type I IFN and IL-6–dependent pathway. J. Immunol. 197, 3884–3893 (2016).
Calabro, S. et al. The adjuvant effect of MF59 is due to the oil-in-water emulsion formulation, none of the individual components induce a comparable adjuvant effect. Vaccine 31, 3363–3369 (2013).
Ott, G. et al. MF59 design and evaluation of a safe and potent adjuvant for human vaccines. in Vaccine Design (eds. Powell, M. F. & Newman, M. J.) vol. 6 277–296 (Springer US, Boston, MA, 1995).
Kim, E. H. et al. Squalene emulsion-based vaccine adjuvants stimulate CD8 T cell, but not antibody responses, through a RIPK3-dependent pathway. eLife 9, e52687 (2020).
Hutchison, S. et al. Antigen depot is not required for alum adjuvanticity. FASEB J. 26, 1272–1279 (2012).
Colaprico, A. et al. Adsorption onto aluminum hydroxide adjuvant protects antigens from degradation. Vaccine 38, 3600–3609 (2020).
Temperley, N. D., Berlin, S., Paton, I. R., Griffin, D. K. & Burt, D. W. Evolution of the chicken Toll-like receptor gene family: A story of gene gain and gene loss. BMC Genomics 9, 62 (2008).
Nawab, A. et al. Chicken toll-like receptors and their significance in immune response and disease resistance. Int. Rev. Immunol. 38, 284–306 (2019).
Gürsel, M., Verthelyi, D., Gürsel, I., Ishii, K. J. & Klinman, D. M. Differential and competitive activation of human immune cells by distinct classes of CpG oligodeoxynucleotide. J. Leukoc. Biol. 71, 813–820 (2002).
Hartmann, G. et al. Delineation of a CpG Phosphorothioate Oligodeoxynucleotide for activating primate immune responses in vitro and in vivo. J. Immunol. 164, 1617–1624 (2000).
Acknowledgements
We thank Dr. Lawrence Silbart for helpful discussions. We would like to acknowledge Dr. Jeremy Balsbaugh and Dr. Jennifer Liddle from the UConn Proteomics and Metabolomics Core for running the LC-MS Proteomics on recombinantly expressed proteins, Dr. Emily Reinhardt for help with necropsies and histologic identification of granulomas, Denise Long from the Connecticut Veterinary Medical Diagnostic Laboratory for processing tracheas and suspected granuloma samples, James Brennan and Cassandra Leone from UConn Animal Care Services for assistance drawing blood from chickens, and UConn Animal Care Services for help with animal husbandry. This work was supported by USDA-NIFA grant #2022-67016-37222 and the Center of Excellence for Vaccine Research (CEVR).
Author information
Authors and Affiliations
Contributions
J.M.M., J.B.M., A.B.M, E.R.T., S.M.S., and S.J.G. conceptualized the project. J.M.M designed experiments and R.G.O., J.B.M., E.R.T., S.M.S., and S.J.G. contributed to experimental design. J.M.M., P.L.P., E.F.H., M.E.D., and A.Q.K. produced and purified recombinant proteins. J.M.M., R.G.O., P.L.P., E.F.H., M.E.D., A.Q.K, and J.B.M. performed animal experiments. J.M.M., P.L.P., E.F.H., M.E.D., and A.Q.K. performed ELISAs. J.M.M. measured tracheal thicknesses. J.M.M. analyzed data and wrote the manuscript. All authors contributed edits/comments to the manuscript.
Corresponding author
Ethics declarations
Competing interests
Edan R. Tulman, Steven M. Szczepanek, and Steve J. Geary are inventors on a patent applied for by the University of Connecticut. Patent application 63/390,756 pertains to all aspects of the subunit vaccine. It is still pending and has not been issued. All other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Miller, J.M., Ozyck, R.G., Pagano, P.L. et al. Rationally designed Mycoplasma gallisepticum vaccine using a recombinant subunit approach. npj Vaccines 9, 178 (2024). https://doi.org/10.1038/s41541-024-00978-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41541-024-00978-x