Abstract
The absence of validated correlates of protection (CoPs) hampers the rational design and clinical development of new tuberculosis vaccines. In this review, we provide an overview of the potential CoPs in tuberculosis vaccine research. Major hindrances and potential opportunities are then discussed. Based on recent progress, it is reasonable to anticipate that success in the ongoing efforts to identify CoPs would be a game-changer in tuberculosis vaccine development.
Similar content being viewed by others
Introduction
As one of the most prevalent communicable diseases, tuberculosis (TB) remains the leading cause of death from a single infectious agent, only being surpassed by COVID-19 during the 2019–2021 pandemic. There were an estimated 10.6 million new active TB cases and 1.3 million deaths in 2022, according to the latest World Health Organization (WHO) global tuberculosis report1. It is also estimated that one-quarter of the world’s population has been infected with Mycobacterium tuberculosis (Mtb), the causative agent of TB, and has a 5–10% lifetime risk of progressing into active TB disease2,3. Thus, the global control of TB remains challenging. The 1-century-old Mycobacterium bovis Bacille Calmette-Guérin (BCG) is the only licensed vaccine against TB. Although BCG offers protection against the aggressive forms of the disease, including meningeal and miliary TB in children, its protective efficacy ranges from 0% to 80% in adolescents and adults4. Considering that vaccines are one of the most effective ways of controlling infectious diseases, developing better vaccines is a crucial objective in TB research.
The development of a more effective TB vaccine faces obvious challenges, among which, the absence of validated correlates of protection (CoPs) is a crucial knowledge gap that significantly hampers progress5,6. CoPs are defined as biological parameters that predict the degree of protection against infectious disease; reliable CoPs could facilitate the development of new vaccines by assessing protective efficacy without exposing clinical trial participants to the infectious agent that the vaccine aims to protect against7,8. Currently, TB vaccine testing is entirely empirical. Since Mtb is a slow-growing bacterium and it takes months to years to progress into active TB diseases post-exposure in humans9,10, the lengthy TB vaccine clinical trials to measure differences in clinical endpoints require tremendous costs and resources. Hence, robust, generalizable, and vaccine-induced CoPs that serve as an intermediate outcome to infer efficacy are desperately needed.
In this review, we provide an overview of potential CoPs for TB vaccines and summarize the usage of different samples in TB vaccine CoPs research. The current major hurdles and potential opportunities for finding reliable CoPs are then discussed in some detail.
The identification of different immune cell populations in TB vaccine CoP research
Th1 immune responses
The most protective antigens and corresponding CoPs have often not been identified in complex diseases that depend heavily on T cell immune responses for protection. The genome of Mtb encodes ~4000 individual proteins that are dynamically produced during different infection stages, and this hinders the identification of the most protective antigens and the corresponding CoPs, which will be discussed in Section “The major hurdles of TB vaccine CoPs identification”. CD4+ T cells are crucial effector cells in the host’s response to Mtb infection, and the helper type 1 CD4+ T cells (Th1) that secrete cytokines IFN-γ, IL-2, and TNF-α are prominent in the immune response against Mtb11. Typically, in TB vaccine development, the effect of a vaccine on the number of bacteria in the lungs and spleens of mice was correlated with the numbers and proportions of multifunctional CD4+ T cells expressing IFN-γ, IL-2, and TNF-α (Fig. 1). Consequently, the Th1 cytokine profiles in antigen-specific T cell responses have been routinely used as biomarkers and assessed as predictors of protection in the evaluation of TB vaccines12,13. IFN-γ was found crucial for the expression of protective immunity, and IFN-γ deficiency causes a high susceptibility to mycobacterial infections14,15. However, excessive IFN-γ production can accelerate death in infected mice16, and current TB vaccine screening criteria that favor vaccines with robust antigen-specific Th1 memory immune responses may over-emphasize IFN-γ production. The MVA85A vaccine could induce high levels of Th1 immune responses in several animal models, such as mice17, guinea pigs18, cattle19, and non-human primates (NHPs)20, as well as in human clinical trials21,22, however, this vaccine failed to show protection in BCG-immunized infants in a phase IIb clinical trial23. Thus, although Th1 cells are considered central mediators of protection, accumulating evidence suggests that current Th1 cell measurements do not reliably indicate the establishment and recall of host resistance against Mtb infection.
Protective immunity is dependent on the crosstalk between innate and adaptive immune systems. The summaries of the multi-faceted protective immune responses are collected from several research models and reflect the main features overall. Some components are still understudied as endpoints. Abbreviations: AMs alveolar macrophages, Breg regulatory B cells, DCs dendritic cells, IFN interferon, Ig immunoglobulin, IL interleukin, ILCs innate lymphoid cells, Mø macrophage, MAIT mucosal-associated invariant T cells, Mtb Mycobacterium tuberculosis, NK natural killer cells, TNF tumor necrosis factor, TCM central memory T cells, TEM effector memory T cells, TRM tissue-resident memory T cells, Treg regulatory T cells. Created with bioRender.com.
Th17 immune responses
Several studies have shown that IL-17-secreting T cells are involved in immune protection against Mtb infection at early stages of infection24,25,26. Th17 cells could recruit neutrophils, monocytes, and Th1 cells to the infection site and granuloma formation and inhibit Mtb replication and dissemination24,27,28,29. Mice lacking IL-17 receptors were also defective in exerting long-term control of Mtb infection30. We and others showed that Th17-inducing TB vaccines gave high levels of immune protection against Mtb challenge in animal models31,32,33,34,35,36. However, similar to IFN-γ-producing Th1 cells, the overexpression of Th17 cells could also enhance susceptibility to infection by exaggerating the influx of neutrophils and inflammatory monocytes to the site of infection, causing lung tissue damage37,38,39. In addition, repeated antigenic exposure led to increased IL-17 expression and immune-mediated pathology40. Thus, current findings suggest a critical role for IL-17-producing Th17 cells in protective immunity via an early but transient burst of IL-17 production, whereas long-lasting Th17 cell activation might contribute to tissue pathology.
CD8+ T cell immune responses
Antigenic peptides from intracellular pathogens such as Mtb can enter the cytosol and associate with major histocompatibility complex class I molecules, resulting in antigen presentation to CD8+ T cells. Upon antigen recognition, CD8+ T cells differentiate into immune effector cells, which can lyse infected target cells and kill the intracellular bacteria through a range of mechanisms41,42. Although less prominent than CD4+ T cells, CD8+ T cells also show a protective role in Mtb infection animal models such as mice43,44, cattle45, and NHPs46. Immune protection induced by several TB vaccines is mediated by robust Mtb-specific CD8+ T cell responses47,48,49,50,51. However, high-frequency vaccine-induced CD8+ T cell responses might contribute to the limited protection against Mtb infection52,53. Thus, further profiling of cytotoxic T cell sub-types that employ different mechanisms of cytotoxicity is likely to be rewarding. State-of-the-art technologies such as single-cell multi-omics might help define the heterogeneity among immune cells, including CD8+ T cells, and provide additional opportunities to find CoPs. This will be discussed in Section “The opportunities for identification of TB vaccine CoPs”.
Humoral responses/B-cell mediated responses
For many approved vaccines against extracellular pathogens, the titer of neutralizing antibodies has served as a reliable CoP and an admittance criterion. However, humoral responses fill a minor part of the literature on the host responses to Mtb, primarily due to the paradigm that humoral immune responses play little role in the protection against intracellular pathogens. We and others showed that T cell immune response-inducing TB vaccines could confer protection against Mtb infection without inducing detectable antigen-specific humoral immunity, and some humoral response-inducing vaccines failed to enhance protection54,55. Nevertheless, antibodies are a major arm of adaptive immunity and have the potential to modulate immune protection against Mtb. In 2019, a cohort study showed that “TB resisters”, who were defined as the Mtb-exposed individuals who kept healthy and were persistently negative in IFN-γ release assay (IGRA) and tuberculin skin tests (TST), possessed IgM and class-switched IgG antibody responses56. Evidently, exposure resulted in the presence of sufficient antigen to generate an immune response in at least the antibody arm of the immune system, either directly by antigen deposition or through initial bacterial proliferation. Thus, the definition of the “TB resisters” population suggests IFN-γ T cell-independent mechanisms exist, which provides a new avenue for identifying CoPs, which will be discussed in detail in Section “The opportunities for identification of TB vaccine CoPs”. Recently, distinct features of antibody responses in individuals progressing to active TB from non-progressing TB were profiled. A multivariate antibody score differentially associated with progression could identify progressors up to 2 years before TB diagnosis57. Furthermore, mucosal and systemic Mtb-specific antibody responses were correlated with protection in NHP models and human beings58,59. Thus, a series of studies has now elucidated the contribution of humoral responses/B cells to the modulation of immune responses to Mtb. For example, it was shown that Mtb-specific IgG purified from LTBI individuals enhanced macrophage activation and intracellular Mtb killing60. Besides producing antibodies, B cells are also competent antigen-presenting cells and produce a wide range of cytokines, which can further influence the function of other immune cells61,62. In addition, B cells are an important component of protective granulomas, which contribute to the control of Mtb infection and prevention of reactivation through various mechanisms63,64. The role of humoral responses/B-cell-mediated responses in TB infection was well reviewed elsewhere65,66,67,68. The uncovering of antibody-dependent protection against Mtb infection in the last decade might have opened a new avenue for finding CoPs in TB vaccine design.
Tissue-resident memory T cells (TRM)
TRM represents a distinct subset of memory lymphocyte lineage that colonizes tissues independently of new recruitment of T cells from the blood and provides a rapid response against reencountered infections69,70. One of the major mechanisms by which Mtb escapes from adaptive immunity is by delaying the initiation of the cellular immune responses and the recruitment of activated circulating T cells to the lung mucosa, the site of primary infection9,71,72. Thus, the lung TRM cells participate in the first line of defense, helping to control the replication and dissemination of Mtb at the early stage of infection by immediately sensing infection and inducing recall immune memory responses73. In 2014, Daniel Barber et al. reported the protection afforded by lung parenchyma cells for the first time in Mtb-infected mice: they showed that the Mtb-specific memory CD4+ T cells in the lung could be divided into two subsets, namely, a population of protective cells colonizing the lung parenchyma, and another population which is less protective circulating in the blood vasculature, The populations were distinguished with surface markers as KLRG1−CXCR3+ and KLRG1+CX3CR1+cells, respectively74. Adoptive transfer experiments indicated the lung parenchyma cells (KLRG1−CXCR3+) to be highly protective against Mtb infection16,74,75. Based on these findings, we studied the properties of circulating CD4+ T cells in patients with active TB and found that high expression levels of KLRG1 were associated with disease progression and lower levels associated with protective responses in immunotherapeutics76. However, the definition of TRM cells in Mtb infection is complicated. In general, memory T cells do not develop when an antigen is still present, and actual memory only forms when the antigens disappear. Thus, it is still controversial whether actual memory can form in the murine models of TB since the host cannot eliminate the invading bacilli in this model. In addition, in Daniel Barber’s report, not all lung parenchyma cells are tissue-resident memory cells. Thus, the role of TRM in Mtb infection still needed to be further defined by using other animal models, such as low-dose NHP infection models, in which some of the animals could entirely clear the invading Mtb. Nevertheless, several studies indicated the protective roles of TB vaccine-induced TRM in Mtb infection, and a better understanding of vaccine-induced lung TRM could facilitate the identification of CoPs. In 2016, Stefan H. E. Kaufmann et al. reported that mucosal delivery of BCG-induced TRM mediated immune protection against Mtb infection in a murine model77. However, confirmation was not sought by intravascular staining for definitive identification of TRM. In 2017, we reported the use of a comprehensive intravascular staining technique and a surface markers staining assay to show that a novel recombinant virus-vectored TB vaccine induced high levels of lung CD8+ TRM49. Several TB vaccines were also reported to be able to induce lung TRM, determined by intravascular staining in murine models78,79,80,81. In an NHP model, intravenous (i.v.) immunization with BCG induced more lung parenchymal CD4+ T cells compared with intradermal inoculation and led to a sterilizing immunity against Mtb infection in 202082; this model provided a unique opportunity to define CoPs of TB vaccines, which will be discussed in detail in Section “The opportunities for identification of TB vaccine CoPs”.
Trained immunity/innate immune memory
Immune memory has been regarded as an exclusive characteristic of adaptive immunity. However, a growing body of evidence suggesting that innate immune cells also show memory responses has challenged this dogma. Innate immune memory also termed trained immunity, was defined as the long-term functional reprogramming of innate immune cells that is evoked by exogenous/endogenous stimulation, with the cells returning to the non-activated state yet showing altered inflammatory immune responses (such as IL-1β, IL-6, and TNF-α) and immune protection against the secondary homologous/heterologous infection83,84,85. The TB vaccine BCG was one of the first agonizts found to induce trained immunity in seminal studies of BCG vaccination of school children86,87. More recently, monocytes derived from BCG-immunized healthy volunteers showed enhanced release of inflammatory cytokines in response to heterologous bacterial and fungal pathogens infection; in addition, BCG could enhance lymphocyte-independent protection in immunodeficient SCID mice against disseminated candidiasis88. These non-specific protective effects remained for at least one year after vaccination89 and were mediated by glycolysis and epigenetic regulation90. Importantly, i.v. BCG vaccination-trained hematopoietic stem cells generated epigenetically modified macrophages/monocytes that provided protection against Mtb infection91, and a randomized clinical trial of BCG vaccination showed that BCG enhanced protection against heterologous infections and improved survival in the elderly92. We recently showed that intrinsic factors in different BCG strains contributed to different stimulating abilities in trained immunity and antimicrobial functions93. These studies suggest that TB vaccine-induced trained immunity might provide CoPs. However, a major challenge is the heterogeneity of individuals, such as in the history of heterologous infections, genetic polymorphisms, and microbiota, which might confound the determination of vaccine-induced trained immunity. A better understanding of trained immunity, especially Mtb protection-associated innate immune memory, is warranted to accompany the derivation of an accurate CoP for TB vaccination.
Tissue-resident alveolar macrophages (AMs)
AMs, resident macrophages of the airway lumen, provide innate immunity in the first line of defense against respiratory pathogens and infections. Mtb is transmitted from persons with active pulmonary TB via respiratory droplets, which are inhaled and deposited in the lung alveoli of close contacts. The deposited Mtb is actively engulfed by the resident AMs via phagocytosis. The early productive Mtb infection occurs almost exclusively within resident AMs for up to 10 days after infection94,95, suggesting that the immune responses induced by Mtb-infected AMs are delayed and/or weakened in the early phase of infection and specifically-acquired immune protection is slow to emerge96.
Studies in mice showed that highly transmissible Mtb strains induced rapid IL-1 receptor-dependent AMs migration and, subsequently, Th1 responses, whereas poorly transmissible strains delayed this process and developed a Th17 response, suggesting flexibility in the development of acquired immunity dependent upon the heterogeneity of innate immune AMs97. Prior exposure to mycobacteria, either by BCG vaccination or by a contained Mtb infection, impacted the initial response of AMs against infection through both AM-intrinsic changes and signals that depend on the altered lung environment98. Thus, the plasticity of AMs suggests that early innate responses could be targeted through vaccination to fine-tune the host response against Mtb infection. Recently, Zhou Xing et al. showed that respiratory adenovirus infection could induce immune memory in AMs, and this was associated with increased glycolytic metabolism and enhanced generation of neutrophil chemokines upon restimulation; the response protected against secondary bacterial infection, and the protection was independent of circulating monocytes99. The evidence suggests that AMs might be targeted by novel TB vaccines to impede the development of Mtb infection. Zhou Xing et al. further showed that a recombinant adenovirus-vectored vaccine, AdAg85A, induced an innate immune memory in AMs that contributed to anti-Mtb protection in mice100. Others have shown that the adenovirus-based TB vaccine and BCG vaccination also drove a long-term activation of AMs that restrained the growth of Mtb and disrupted early bacterial dissemination after the Mtb challenge101,102. Together, these studies indicate that differences in responsivity among lung resident AMs influence the outcome of Mtb infection and might contribute to the definition of TB vaccine CoPs.
Other immune cells
In addition to AMs, other innate and adaptive immune cells can also dictate the course of infection after encountering respiratory pathogens. Immune cells such as neutrophils, monocytes, dendritic cells (DCs), natural killer (NK) cells, γδ T cells, regulatory T cells (Treg), regulatory B cells (Breg), innate lymphoid cells (ILCs), and mucosal-associated invariant T cells (MAIT) have also been shown to tune innate immunity and activate antigen-specific adaptive immune responses (Fig. 1). The relevance of these cells to the efficacy of TB vaccines has been well-reviewed elsewhere103,104,105,106,107 and is not a focus of this review. A major hurdle for deriving innate immune cell-based vaccine CoPs is that innate immunity is non-specific. Thus, infection by non-tuberculous pathogens, allergy, or even sterile inflammation would confound the determination of Mtb-induced innate immune responses in naturally complicated conditions prevailing in clinical trials. Thus, although innate immune responses play important roles in host immunity against TB infection, our opinion is that an innate phenotype is unlikely to be used as a definitive CoP of TB vaccines in the coming years, primarily due to their complex, multilayered, and non-specific characteristics.
The available samples For Tb vaccine CoP discovery
The identification of CoPs relies on the knowledge of the immunological processes of the host after infection or vaccination. There are several limitations in seeking this knowledge, such as technical feasibility, financial costs, and ethical requirements. Given such restrictions, whole blood samples are always the main source of biological samples for studying CoPs. Whole blood is one of the most accessible samples in humans/animals. It can be separated into peripheral blood mononuclear cells (PBMCs), plasma, or serum to study circulating cells, soluble cytokines, and antibodies. Recently, the use of blood in mycobacterial growth inhibition assays (MGIA) has provided unbiased measures of ability to control mycobacterial growth in vitro108. These assays offer the opportunity to determine the contributions of multiple components of the immune responses, either in whole blood or cell samples. Thus, MGIA is used to down-select candidate TB vaccines at an early stage of their development109,110,111. In addition to whole blood, cells obtained by bronchoalveolar lavage (BAL) and lung and spleen cells from animal models are also widely used to determine adaptive antigen-specific T-cell immune responses. However, tissue samples are not readily accessible without invasive procedures in human clinical trials. Lymph nodes are another valuable and feasible source of samples to study CoPs, particularly in experimental animals. There is increasing interest in how Mtb is controlled in the lymph node in the NHP model82,112 and the contained Mtb infection murine model61,113 (Fig. 2).
The samples that are typically obtained from mice, NHPs, and human beings in clinical trials are summarized. Abbreviations: BAL bronchoalveolar lavage, CoPs correlates of protection, TB tuberculosis, PBMCs peripheral blood mononuclear cells, PET-CT positron emission tomography-computed tomography, VOCs volatile organic compounds. Created with bioRender.com.
The distribution of immune cells in the lung tissues is crucial, and new methods such as advanced imaging techniques, for example, positron emission tomography-computed tomography (PET-CT), can reflect the protective and pathological changes within the lung tissues and lesions after Mtb infection. Urine samples also offer some advantages over whole blood in terms of convenience of collection and safety. The potential of using urine samples as a source of CoPs in TB is inferred from the use of urine analysis to indicate TB disease progression. Among the potential CoPs, lipoarabinomannan, a cell wall component of Mtb detected in urine, shows promise in detecting patients with disseminated TB among human immunodeficiency virus-infected populations114,115. In addition, invasive sampling, for example, to obtain puncture biopsy samples116 or surgically resected human tissue samples117,118, offers valuable opportunities to study the local immune responses. Moreover, there have been studies using breath-detected volatile organic compounds (VOCs) in the diagnosis of TB119,120 (Fig. 2).
Considered together, analyses of the various types of biological samples could build a picture of the host immune responses against Mtb infection observed from different perspectives; a comprehensive analysis of such samples is needed to better characterize vaccine-induced protective responses.
The major hurdles of Tb vaccine CoPs identification
The quest for definitive CoPs for TB vaccines has encountered multiple obstacles. Firstly, the slow and intermittent growth characteristics of Mtb results in different disease states of TB infection, which hinders the definition of protective immunity against TB. According to the WHO’s annual TB reports, it is estimated that one-quarter of the world’s population has been infected with Mtb, and there is a 5–10% lifetime risk of developing active TB diseases1. Although individuals with asymptomatic latent TB infection (LTBI) fail to completely eradicate invading Mtb, an immune system that is persistently or intermittently responding against Mtb antigens might contribute to the absence of clinically manifest TB disease progression. Thus, immune profiles induced by latency-associated antigens might guide finding CoPs against LTBI. However, the recent recognition of the “TB resister” population has added a layer of complexity to defining protective immunity; this population might induce anti-TB immunity that is different from the typical CD4 Th1 responses. Thus, the search for TB CoPs should comprehensively consider the differences in protection against primary infection, persistent latent infection, reactivation, progression from latent infection to active disease, and reinfection. Recently, considering the lack of consistency in conceptual and diagnostic definitions of different TB states, with definitions that failed to reflect the spectrum of TB diseases, an International Consensus for Early TB classification framework was established to comprehensively consider macroscopic pathology, infectiousness, symptoms, and signs121. The new international consensus classification and novel diagnostics might solve this problem, improve cross-study data comparisons, and assist with future study design. Secondly, the protective recall antigen-specific immune responses induced by vaccines might not be identical to the protective immunity induced by natural infection. Therefore, a reliable CoP induced by natural Mtb infection might not be suitable to be used as a CoP induced by TB vaccination. Although cytokines are necessary for controlling intracellular infection with agents such as Mtb, excessive cytokine production induced by a vaccine might also cause cell necrosis and tissue damage. Thus, the optimal “cut-off” value for natural and vaccine-induced immune responses might differ. A phase III randomized controlled TB vaccine clinical trial is needed to solve this problem. Fortunately, the clinical trials of the M72/AS01E vaccine provide valuable guidance to finding CoPs by profiling vaccine-induced protective immunity in human beings, which will be discussed in the next section. Thirdly, vector-specific immune responses induced by different types of recombinant-vectored vaccines might confound the identification of CoPs. Subunit protein vaccines and nucleic acid vaccines, such as mRNA vaccines, could solve this problem. Fourthly, the biomarker dynamics and time of sampling will further influence the outcome of CoPs prediction. Thus, a rigorous and comprehensive study design is needed to precisely define the immune CoPs. Finally, the host genetics, such as species differences and polymorphisms in genes encoding proteins involved in intercellular cytokine signaling, are other confounding factors in identifying CoPs. Clinical trials that enroll large numbers of participants in different regions could solve this problem, but such a trial is expected to be prohibitively expensive. Alternatively, genetically diverse mice strains could represent an appropriate range of genotypes. This, too, will be discussed in the next section.
The opportunities for identification of Tb vaccine CoPs
In principle, key opportunities for finding vaccine CoPs arise when the vaccine induces protection in some but not all vaccines. Then, comparisons of the two groups, protected vs unprotected vaccines, could provide a solid basis for the definition of a robust CoP. Recently, several TB vaccines and vaccination strategies, such as the M72/AS01E protein subunit vaccine and BCG i.v. inoculation, have shown promise in providing substantial immune protection or even sterilizing immunity against Mtb infection in clinical trials and pre-clinical models. Moreover, new experimental models such as the controlled human infection model and the ultra-low-dose infection murine model, are available for clinical and pre-clinical vaccine evaluation, and the discovery of the TB resisters population in close contacts of active TB patients gives another opportunity. Conventional high-throughput technologies and novel state-of-the-art technological approaches such as omics and artificial intelligence are increasingly being adopted and will further facilitate the discovery of TB vaccine CoPs. These new opportunities suggest that the identification of reliable CoPs to determine the efficacy of TB vaccine candidates might be feasible shortly (Fig. 3).
The available experimental approach, research models, and resources that might facilitate TB vaccine CoPs determination are summarized based on current knowledge. Abbreviations: BCG Bacille Calmette–Guérin, CC collaborative cross, CoPs correlates of protection, DO diversity outbred, i.v. intravenous immunization, TB tuberculosis, Mtb Mycobacterium tuberculosis, ULD ultra-low-dose. Created with bioRender.com.
Controlled human infection model
A controlled human infection model can substantially accelerate the development of new vaccines since the size of volunteer groups can be significantly smaller, the experiment duration can be shorter, and the expenses can be far less compared with traditional clinical trials. In a controlled human infection model study, a well-characterized strain of an infectious agent is administered at a controlled dose and by a specific route to carefully selected volunteers; volunteers are closely monitored for evidence of infection under medical supervision for diagnosis and management of early symptoms of diseases122. This model is a great tool for vaccine development and has contributed to the development of vaccines for other disease agents, including influenza, shigella, enteric fever, malaria, campylobacter, cholera, and respiratory syncytial virus122. It is particularly attractive for TB vaccine assessment since the low rates of natural exposure to infection, the slow growth characteristic of Mtb, and the slow speed of TB disease progression render the conventional assessments of protective efficacy extraordinarily time-consuming and costly. Thus, the controlled human infection model of mycobacterial challenge could substantially accelerate the development of TB vaccines towards clinical trials.
Methods of using either BCG or a conditionally replicating Mtb strain are being developed in studies of controlled human mycobacterial infection, and intradermal or respiratory/mucosal routes of infection have been used. Initially, because deliberately infecting healthy volunteers with virulent Mtb is not ethical in the absence of a reliable method of anti-TB treatment that could completely eradicate infection, the group of Dr. Helen McShane, in 2012, used an attenuated M. bovis BCG vaccine strain that does not cause disease or latency in healthy humans; intradermal “infection” allowed straightforward quantification of mycobacteria from punch biopsies by PCR and bacterial culture123. This model was then used to evaluate TB vaccines in human beings124,125. Subsequently, the intradermal route was changed into the aerosol route to more closely mimic the natural route of Mtb infection and was used to evaluate TB vaccines in several clinical trials (NCT03912207 and NCT04777721)126. Live BCG has also been directly instilled into the lung lobes via bronchoscopy and was well-tolerated in healthy volunteers127. In addition to optimization of the vaccination route, other modifications, such as the incorporation of an auto-luminescent fluorophore reporter gene or detection of exhaled volatile compounds by mass spectrometry, can be proposed to avoid invasive sampling for mycobacterial recovery and quantification128,129. Currently, a conditionally replicating Mtb strain with a genetically inserted suicide mechanism is being developed for controlled infection in man. In this approach, the survival of Mtb is dependent on two exogenous compounds so that the invading bacteria are killed if the compounds are withdrawn130. The proof-of-concept of using the conditionally replicating Mtb strains has been obtained in mice and NHPs models; next, the strains will be reconstructed to meet, at a minimum, compliance with good manufacturing practice before usage in a human challenge study131.
These controlled human infection models could not only be used to provide early proof-of-concept of the protective efficacy of TB vaccine candidates but could also sharply facilitate the interrogation of immunity for the identification and validation of CoPs at defined time points after infection.
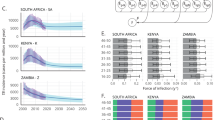
Ultra-low-dose aerosol infection and genetically diverse mouse model
In general, in the pre-clinical evaluation of TB vaccine protective efficacy, mice are aerosol-infected with a “conventional” (50–200 colony-forming units [CFU]) or a “high” (>250 CFU) dose of Mtb; however, in natural infection, most people are infected by one or two bacilli that successfully implant after inhalation of low doses132. This divergence between laboratory models and clinical scenarios hinders the discovery of CoPs. To solve this problem, a model of ultra-low-dose (ULD) aerosol Mtb infection in mice was established in 2021, in which infection was initiated by only 1–3 CFU133 and induced well-circumscribed granulomas that shared features with human granulomas and more closely replicated human TB disease. The model revealed a blood transcriptional signature that correlated with the wide range of lung bacterial burdens and might predict Mtb infection outcomes in both NHPs and human infections. It has been used to evaluate the protective efficacy of several TB vaccines134,135,136 and showed that the elevated serum levels of IFN-γ, IL-17A, IL-6, CCL2, CXCL1, and CXCL2 were associated with vaccine-induced protection134. The observation that vaccine-induced Th1/Th17 cytokines secretion enhancement correlates with protection is consistent with murine models that used conventional infection doses; however, whether an excessive production of these cytokines leads to exacerbated lung lesions, as suggested by conventional infection doses16,38, remains to be defined in ULD models. The model provides a unique experimental system for studying the host immunology and pathogenesis of Mtb infection, which will accelerate the discovery of a reliable TB vaccine CoP.
Genetic diversity plays a significant role in individual variation in vaccine-induced immune responses. However, classical inbred mouse strains, in which all individuals are genetically identical, were routinely used in vaccine studies, including those for TB. Collaborative cross (CC) and diversity outbred (DO) mouse strains are new mammalian animal resources that more accurately represent the genetic and phenotypic heterogeneity observed in naturally outbred populations. They were recently used to evaluate TB vaccines. It was shown that CC strains varied dramatically in primary susceptibility to Mtb infection and produced qualitatively distinct immune states137. BCG protected only half of the CC strains against TB, and this was correlated with heterogeneity in several inflammatory mediators in the lung microenvironment138. Similarly, DO mice were used to study immune correlates of TB disease and risk translation across species139; BCG-vaccinated DO mouse populations exhibited a wide range of disease outcomes. Sixteen chromosomal loci were found to be associated with complex infection traits and cytokine production140,141. Thus, these genetically diverse murine models can be used to facilitate precise definitions of vaccine-induced CoPs during the development of vaccines that protect a range of genotypes that mimic the heterogeneity in human populations.
The clinical trials of the M72/AS01E vaccine
The novel TB vaccine M72/AS01E is composed of the M72 antigen, which is a recombinant fusion protein based on two immunodominant antigens Mtb32A (Rv0125/PepA) and Mtb39A (Rv1196/PPE18), and a liposome-based adjuvant AS01E, which contains monophosphoryl lipid A and the saponin QS21142. In 2019, a proof-of-concept Phase IIb trial showed that the M72/AS01E vaccine provided 49.7% (95% confidence interval [CI], 2.1-74.2) protection against microbiologically-confirmed pulmonary TB disease in Mtb-infected IGRA-positive adults who did not have active TB143. The T cell and antibody responses were evaluated in according-to-protocol subgroups totaling 244 participants (120 in the vaccine group and 124 in the placebo group) to test the immunogenicity. Among participants in the M72/AS01E group, the frequencies of multifunctional M72-specific CD4+ T cells (IFN-γ/IL-2/TNF-α-secreting cells) were substantially increased after immunization, and increases persisted for at least 36 months, with no evidence of waning. Robust M72-specific IgG responses were also observed. In light of this finding, this cohort was believed to offer a unique opportunity to identify CoPs against TB disease progression.
A “TB Immune Correlates Program” was launched for TB vaccine M72/AS01E-induced CoPs in 2020144, which aims to provide the strategy and governance framework to facilitate finding CoPs through an international consortium of investigators. These projects were planned to (1) define candidate biomarkers and assays to be performed for the discovery of TB vaccine CoPs; (2) develop the statistical framework to evaluate the pre-specified hypotheses; (3) pursue additional hypothesis-generating exploratory efforts; (4) ensure rigorous, efficient and streamlined usage of the cryopreserved samples from these two trials144. The priority is informed by existing knowledge and recent findings from animal studies and clinical trials, including antigen-specific T cell responses (functional/activated/memory profiles, recognized epitopes, TCR repertoire/gene expression, and secretion of immunomodulatory factors), humoral responses (the titers/sub-classes/avidity/specificity of antibodies, Fc-mediated function, and mucosal antibody responses), donor-unrestricted T cells, innate immunity, etc.144.
The sterilizing immunity induced by RhCMV/TB and BCG i.v. in the NHP model
Recently, two promising pre-clinical studies showed that TB vaccines could induce sterilizing immunity against Mtb infection in the NHPs model. Firstly, in 2018, RhCMV/TB, a cytomegalovirus-vectored vaccine encoding 9 Mtb antigens (ESAT-6, Ag85A, Ag85B, Rv3407, Rv1733, Rv2626, Rpf A, Rpf C, and Rpf D), reduced the overall extent of pulmonary and extra-pulmonary Mtb infection and disease by 68% compared to unvaccinated controls in rhesus macaques145. Notably, 14 out of 34 RhCMV/TB-vaccinated rhesus macaques showed no detectable TB disease by computed tomography (CT) scan and necropsy, compared with 0 out of 17 unvaccinated controls. This is the first demonstration of sterilizing immunity against highly pathogenic Mtb infection in the NHP model. Analysis showed that multifunctional CD4+ and CD8+ T cell immune responses were induced by RhCMV/TB145.
In 2020, a study compared different vaccination routes of BCG in the NHP model and found that BCG i.v. immunization protected 9 out of 10 rhesus macaques against Mtb challenge, which contrasted to limited protection afforded by other routes at the same dose; notably, 6 out of 9 protected macaques had no detectable infection, as determined by PET-CT, mycobacterial growth, pathology, and granuloma formation82. This encouraging result was confirmed by another study in 2023, which showed i.v. BCG protected 9 out of 12 SIV-infected animals; no culturable bacteria were detectable in tissues146. Ironically, the high level of protection made it challenging to detect cellular or humoral CoPs since 90% of animals were protected. In several studies, the i.v. BCG vaccination was “optimized” to achieve a lower (~50%) protective efficacy and facilitate correlates analysis. Multivariate analysis incorporating longitudinal cellular and humoral immune parameters of cells in BAL showed that, at 2–12 weeks post-i.v. BCG vaccination, the numbers of NK cells and CD4+ T cells producing TNF-α/IFN-γ or TNF-α/IL-17 (Th1/Th17 cells) were correlated with protection147. In another study, single-cell RNA sequencing was used to transcriptionally profile the responses to PPD among BAL cells that were collected 13/25 weeks, or 14–15 weeks (2 batches) after vaccination. High-dose i.v. BCG vaccination drove a local influx of AMs into the airways, and the cells exhibited a basal activation phenotype up to 25 weeks post-immunization; in addition, after PPD stimulation, intercellular immune signaling pathways between myeloid and T cells were enhanced, with robust Th1/Th17 transcriptional phenotypes in T cells, and augmented IFN-γ response in AMs148. The humoral immune responses in the BAL 4 weeks after immunization were correlated with the Mtb burden post-challenge149. Recently, it was shown that depletion of CD4+ T cells and CD8α-expressing lymphocytes (both innate and adaptive), but not CD8αβ+ T cells, before Mtb challenge of BCG i.v.-vaccinated NHPs resulted in the loss of protection150. These studies indicate that the cross-talk between myeloid cells and lymphocytes in the local infection sites is crucial and long-lasting during Mtb infection, and corresponding parameters might be used as CoPs.
Peripheral blood samples are far more convenient than BAL samples for COP analysis. In analyses of blood immune features, the early innate transcriptional response on day 2 after BCG i.v. immunization, especially an innate response module enriched for type I interferon and RIG-I-like receptor signaling pathways, was highly correlated with antigen-responsive lung CD4+ T cells at week eight and with Mtb burden following challenge in the NHPs model151. In addition, the antibody responses induced by i.v. BCG was also correlated with protection against Mtb infection149. These studies suggest that analysis of peripheral blood signatures early post-vaccination holds promise for predicting vaccine-induced anti-TB protection.
TB resisters and latent infection
Resisters (people) and persisters (bacteria) deserve further consideration. These appear at first to be relatively defined states compared to the spectrum of immunological and pathological conditions found in tuberculosis disease. After initial Mtb exposure in human beings, 30% will develop a primary infection, among which 85–90% of immune-competent people develop asymptomatic LTBI, in which there is a state of persistent immune response against Mtb stimulation (IGRA or TST positive) but the bacillary replication is controlled without clinical evidence of active TB disease152,153. Once asymptomatic LTBI is established after initial exposure, there is only a 5–10% lifetime risk of developing into active TB disease2,3. Thus, the majority of the LTBI population is “resistant” to active TB diseases. However, the bacteria are not fully dormant and undergo periods of growth, so the immune response to the antigens may fluctuate between suppressive and facilitatory states throughout the lengthy latency period, rendering the identification of CoPs a challenge. We and others have profiled several latency-associated antigens and designed vaccines containing corresponding antigens54,154,155,156,157,158, but analysis of response to these antigens has not yet led to the identification of CoPs.
The term “TB resisters” was defined as individuals who were heavily and repeatedly exposed to Mtb but resistant to active TB disease and consistently tested negative for reactivity in the IGRA and TST assays159. The basis of IGRA and TST negativity is not established but may be due to minimal bacterial multiplication that the antigen dose does not reach a threshold for those responses. A cohort study in 2019 showed that TB resisters possessed IgM and class-switched IgG antibody responses and non-IFN-γ T cell responses to Mtb-specific antigens56. Thus, TB resisters, at least some of them, mounted those host immune responses after Mtb exposure. In 2020, we also found that the T cell activation status marker CD69 was associated with Mtb infection and may have the potential to distinguish LTBI and TB resisters160. More recently, several adaptive immune states were reported to be elevated in TB resisters, such as higher levels of circulating CD8+ glucose monomycolate+ granzyme-B+ T cells161, antigen-specific antibody Fc galactosylation/sialylation162, anti-LpqH human monoclonal antibody163, and MR1-restricted T cells164, as well as innate immune responses, such as enrichment of the TNF signaling gene set165, higher free fatty acid transcriptional responses166, lipid accumulation in monocytes167, and histone deacetylase 6 in monocyte-derived macrophages168. Moreover, pantothenate (vitamin B5) was significantly elevated in blood cells169, and some non-coding RNAs were enriched in PBMCs from TB resisters170. Whether any of these features, separately or together, will correlate with the elimination of the infection or yield a useful CoP remains to be seen.
Omics and artificial intelligence
Systems vaccinology leverages high-throughput omics technologies, such as transcriptomics, metabolomics, epigenomics, and mass cytometry, coupled with computational approaches to construct a global map of the complex processes that mediate the protective immune response to vaccination. These technologies provide the opportunity to interrogate biological models at a comprehensive systems-level instead of empirical approaches that characterize a few genes or proteins in an experiment. With multilayered omics data generated in the case-cohort studies, an integrative multivariate framework that draws together and analyzes data from the different technologies should provide key insights. The cross-talk between innate and adaptive immune responses before and after immunization and/or infection might conceal new candidate biomarkers or verify the hypothesized CoPs. The advent of sophisticated artificial intelligence based on deep learning and machine learning algorithms marks a seminal point in multimodal omics data integration. It will create powerful tools for determining novel correlates of vaccine protection171.
Conclusions
Despite Mtb co-evolving with human beings for centuries and being intensely studied for decades, the CoPs, especially vaccine-induced CoPs, against Mtb infection and TB disease have yet to be fully defined. Their discovery has been hindered by an incomplete understanding of host protective immunity against Mtb and uncertainty as to the predictive value of animal models. The finding of CoPs is particularly important in TB vaccine development since it is a slow-growing bacterium, and it takes months to years for a Mtb-exposed person to progress into active TB disease and reveal the effect of vaccination. This incurs tremendous costs in clinical trials to measure differences in clinical endpoints. However, the positive results of the M72/AS01E vaccine recently evaluated in clinical trials not only strengthen our confidence in designing an effective novel TB vaccine but also provide new opportunities to find CoPs. Moreover, new models, such as the controlled human Mtb infection model and new state-of-the-art technologies, will further facilitate the findings of CoPs. The sterilizing immunity induced by i.v. BCG and CMV-vectored TB vaccines in the NHPs model may provide a crucial benchmark to understand the immune correlates and mechanisms of sterilizing protection against TB. Thus, there is renewed optimism that a reliable CoP or a tailored combination of independent biomarkers might be realizable. When realized, a reliable CoP would enable the down-selection of vaccines that enter the clinical pipelines, accelerate the process of clinical trials, and become the game-changer of TB vaccine development.
References
World Health Organization. Global Tuberculosis Report. (2023).
Targeted tuberculin testing and treatment of latent tuberculosis infection. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. This is a Joint Statement of the American Thoracic Society (ATS) and the Centers for Disease Control and Prevention (CDC). This statement was endorsed by the Council of the Infectious Diseases Society of America. (IDSA), September 1999, and the sections of this statement. Am. J. Respir. Crit. Care Med. 161, S221–S247 (2000).
Lillebaek, T. et al. Molecular evidence of endogenous reactivation of Mycobacterium tuberculosis after 33 years of latent infection. J. Infect. Dis. 185, 401–404 (2002).
Mangtani, P. et al. Protection by BCG vaccine against tuberculosis: a systematic review of randomized controlled trials. Clin. Infect. Dis. 58, 470–480 (2014).
Lai, R., Ogunsola, A. F., Rakib, T. & Behar, S. M. Key advances in vaccine development for tuberculosis-success and challenges. NPJ Vaccines 8, 158 (2023).
Bhatt, K., Verma, S., Ellner, J. J. & Salgame, P. Quest for correlates of protection against tuberculosis. Clin. Vaccin. Immunol. 22, 258–266 (2015).
Britto, C. & Alter, G. The next frontier in vaccine design: blending immune correlates of protection into rational vaccine design. Curr. Opin. Immunol. 78, 102234 (2022).
Escudero-Perez, B., Lawrence, P. & Castillo-Olivares, J. Immune correlates of protection for SARS-CoV-2, Ebola and Nipah virus infection. Front. Immunol. 14, 1156758 (2023).
Chandra, P., Grigsby, S. J. & Philips, J. A. Immune evasion and provocation by Mycobacterium tuberculosis. Nat. Rev. Microbiol 20, 750–766 (2022).
Yang, J., Zhang, L., Qiao, W. & Luo, Y. Mycobacterium tuberculosis: pathogenesis and therapeutic targets. MedComm (2020) 4, e353 (2023).
Prezzemolo, T. et al. Functional signatures of human CD4 and CD8 T cell responses to Mycobacterium tuberculosis. Front. Immunol. 5, 180 (2014).
Derrick, S. C., Yabe, I. M., Yang, A. & Morris, S. L. Vaccine-induced anti-tuberculosis protective immunity in mice correlates with the magnitude and quality of multifunctional CD4 T cells. Vaccine 29, 2902–2909 (2011).
Sakai, S., Mayer-Barber, K. D. & Barber, D. L. Defining features of protective CD4 T cell responses to Mycobacterium tuberculosis. Curr. Opin. Immunol. 29, 137–142 (2014).
Flynn, J. L. et al. An essential role for interferon gamma in resistance to Mycobacterium tuberculosis infection. J. Exp. Med. 178, 2249–2254 (1993).
Cooper, A. M. et al. Disseminated tuberculosis in interferon gamma gene-disrupted mice. J. Exp. Med. 178, 2243–2247 (1993).
Sakai, S. et al. CD4 T cell-derived IFN-gamma plays a minimal role in control of pulmonary Mycobacterium tuberculosis infection and must be actively repressed by PD-1 to prevent lethal disease. PLoS Pathog. 12, e1005667 (2016).
McShane, H., Brookes, R., Gilbert, S. C. & Hill, A. V. Enhanced immunogenicity of CD4(+) t-cell responses and protective efficacy of a DNA-modified vaccinia virus Ankara prime-boost vaccination regimen for murine tuberculosis. Infect. Immun. 69, 681–686 (2001).
Williams, A. et al. Boosting with poxviruses enhances Mycobacterium bovis BCG efficacy against tuberculosis in guinea pigs. Infect. Immun. 73, 3814–3816 (2005).
Vordermeier, H. M. et al. Cellular immune responses induced in cattle by heterologous prime-boost vaccination using recombinant viruses and bacille Calmette-Guerin. Immunology 112, 461–470 (2004).
Verreck, F. A. et al. MVA.85A boosting of BCG and an attenuated, phoP deficient M. tuberculosis vaccine both show protective efficacy against tuberculosis in Rhesus macaques. PLoS ONE 4, e5264 (2009).
McShane, H. et al. Recombinant modified vaccinia virus Ankara expressing antigen 85A boosts BCG-primed and naturally acquired antimycobacterial immunity in humans. Nat. Med. 10, 1240–1244 (2004).
Scriba, T. J. et al. Modified vaccinia Ankara-expressing Ag85A, a novel tuberculosis vaccine, is safe in adolescents and children, and induces polyfunctional CD4+ T cells. Eur. J. Immunol. 40, 279–290 (2010).
Tameris, M. D. et al. Safety and efficacy of MVA85A, a new tuberculosis vaccine, in infants previously vaccinated with BCG: a randomised, placebo-controlled phase 2b trial. Lancet 381, 1021–1028 (2013).
Khader, S. A. et al. IL-23 and IL-17 in the establishment of protective pulmonary CD4+ T cell responses after vaccination and during Mycobacterium tuberculosis challenge. Nat. Immunol. 8, 369–377 (2007).
Okamoto Yoshida, Y. et al. Essential role of IL-17A in the formation of a mycobacterial infection-induced granuloma in the lung. J. Immunol. 184, 4414–4422 (2010).
Shanmugasundaram, U. et al. Pulmonary Mycobacterium tuberculosis control associates with CXCR3- and CCR6-expressing antigen-specific Th1 and Th17 cell recruitment. JCI Insight 5, e137858 (2020).
Ottenhoff, T. H. New pathways of protective and pathological host defense to mycobacteria. Trends Microbiol. 20, 419–428 (2012).
Miranda, N. & Hoyer, K. K. Coccidioidomycosis granulomas informed by other diseases: advancements, gaps, and challenges. J Fungi (Basel) 9, 650 (2023).
Ogongo, P. et al. Tissue-resident-like CD4+ T cells secreting IL-17 control Mycobacterium tuberculosis in the human lung. J. Clin. Invest. 131, e142014 (2021).
Freches, D. et al. Mice genetically inactivated in interleukin-17A receptor are defective in long-term control of Mycobacterium tuberculosis infection. Immunology 140, 220–231 (2013).
Dijkman, K. et al. Pulmonary MTBVAC vaccination induces immune signatures previously correlated with prevention of tuberculosis infection. Cell Rep. Med. 2, 100187 (2021).
Jong, R. M. et al. Mucosal vaccination with cyclic dinucleotide adjuvants induces effective T cell homing and IL-17-dependent protection against Mycobacterium tuberculosis infection. J. Immunol. 208, 407–419 (2022).
Aguilo, N. et al. Pulmonary but not subcutaneous delivery of BCG vaccine confers protection to tuberculosis-susceptible mice by an interleukin 17-dependent mechanism. J. Infect. Dis. 213, 831–839 (2016).
Counoupas, C. et al. Mucosal delivery of a multistage subunit vaccine promotes development of lung-resident memory T cells and affords interleukin-17-dependent protection against pulmonary tuberculosis. NPJ Vaccines 5, 105 (2020).
Butcher, D. L. & Deng, H. W. Hypothetical SisterKiller. Nature 369, 26 (1994).
Wu, J. et al. Incorporation of immunostimulatory motifs in the transcribed region of a plasmid DNA vaccine enhances Th1 immune responses and therapeutic effect against Mycobacterium tuberculosis in mice. Vaccine 29, 7624–7630 (2011).
Desvignes, L. & Ernst, J. D. Interferon-gamma-responsive nonhematopoietic cells regulate the immune response to Mycobacterium tuberculosis. Immunity 31, 974–985 (2009).
Blanco, F. C. et al. Increased IL-17 expression is associated with pathology in a bovine model of tuberculosis. Tuberculosis 91, 57–63 (2011).
Jurado, J. O. et al. IL-17 and IFN-gamma expression in lymphocytes from patients with active tuberculosis correlates with the severity of the disease. J. Leukoc. Biol. 91, 991–1002 (2012).
Cruz, A. et al. Pathological role of interleukin 17 in mice subjected to repeated BCG vaccination after infection with Mycobacterium tuberculosis. J. Exp. Med. 207, 1609–1616 (2010).
Kaufmann, S. H. Immunity to intracellular bacteria. Annu. Rev. Immunol. 11, 129–163 (1993).
Ali, A. et al. Recent advancement, immune responses, and mechanism of action of various vaccines against intracellular bacterial infections. Life Sci. 314, 121332 (2023).
van Pinxteren, L. A., Cassidy, J. P., Smedegaard, B. H., Agger, E. M. & Andersen, P. Control of latent Mycobacterium tuberculosis infection is dependent on CD8 T cells. Eur. J. Immunol. 30, 3689–3698 (2000).
Sousa, A. O. et al. Relative contributions of distinct MHC class I-dependent cell populations in protection to tuberculosis infection in mice. Proc. Natl Acad. Sci. USA 97, 4204–4208 (2000).
Villarreal-Ramos, B. et al. Investigation of the role of CD8+ T cells in bovine tuberculosis in vivo. Infect. Immun. 71, 4297–4303 (2003).
Chen, C. Y. et al. A critical role for CD8 T cells in a nonhuman primate model of tuberculosis. PLoS Pathog. 5, e1000392 (2009).
Wang, J., Santosuosso, M., Ngai, P., Zganiacz, A. & Xing, Z. Activation of CD8 T cells by mycobacterial vaccination protects against pulmonary tuberculosis in the absence of CD4 T cells. J. Immunol. 173, 4590–4597 (2004).
Wu, Y., Woodworth, J. S., Shin, D. S., Morris, S. & Behar, S. M. Vaccine-elicited 10-kilodalton culture filtrate protein-specific CD8+ T cells are sufficient to mediate protection against Mycobacterium tuberculosis infection. Infect. Immun. 76, 2249–2255 (2008).
Hu, Z. et al. Sendai virus mucosal vaccination establishes lung-resident memory CD8 T cell immunity and boosts BCG-primed protection against TB in mice. Mol. Ther. 25, 1222–1233 (2017).
Moliva, J. I. et al. Exposure to human alveolar lining fluid enhances Mycobacterium bovis BCG vaccine efficacy against Mycobacterium tuberculosis infection in a CD8(+) T-cell-dependent manner. Mucosal Immunol. 11, 968–978 (2018).
Vasilyev, K. et al. Enhancement of the local CD8(+) T-cellular immune response to Mycobacterium tuberculosis in BCG-primed mice after intranasal administration of influenza vector vaccine carrying TB10.4 and HspX antigens. Vaccines (Basel) 9, 1273 (2021).
Baldwin, S. L. et al. Protection against tuberculosis with homologous or heterologous protein/vector vaccine approaches is not dependent on CD8+ T cells. J. Immunol. 191, 2514–2525 (2013).
Lindenstrom, T., Aagaard, C., Christensen, D., Agger, E. M. & Andersen, P. High-frequency vaccine-induced CD8(+) T cells specific for an epitope naturally processed during infection with Mycobacterium tuberculosis do not confer protection. Eur. J. Immunol. 44, 1699–1709 (2014).
Hu, Z. et al. A multistage Sendai virus vaccine incorporating latency-associated antigens induces protection against acute and latent tuberculosis. Emerg. Microbes Infect. 13, 2300463 (2024).
Ashhurst, A. S. et al. PLGA particulate subunit tuberculosis vaccines promote humoral and Th17 responses but do not enhance control of Mycobacterium tuberculosis infection. PLoS ONE 13, e0194620 (2018).
Lu, L. L. et al. IFN-gamma-independent immune markers of Mycobacterium tuberculosis exposure. Nat. Med. 25, 977–987 (2019).
Davies, L. R. L. et al. Age and sex influence antibody profiles associated with tuberculosis progression. Nat. Microbiol. 9, 1513–1525 (2024).
Ishida, E. et al. Mucosal and systemic antigen-specific antibody responses correlate with protection against active tuberculosis in nonhuman primates. EBioMedicine 99, 104897 (2024).
Chen, T. et al. Capsular glycan recognition provides antibody-mediated immunity against tuberculosis. J. Clin. Invest. 130, 1808–1822 (2020).
Lu, L. L. et al. A functional role for antibodies in tuberculosis. Cell 167, 433–443 e414 (2016).
du Plessis, W. J. et al. The functional response of B cells to antigenic stimulation: a preliminary report of latent tuberculosis. PLoS ONE 11, e0152710 (2016).
Dubois Cauwelaert, N. et al. Antigen presentation by B cells guides programing of memory CD4(+) T-cell responses to a TLR4-agonist containing vaccine in mice. Eur. J. Immunol. 46, 2719–2729 (2016).
Phuah, J. Y., Mattila, J. T., Lin, P. L. & Flynn, J. L. Activated B cells in the granulomas of nonhuman primates infected with Mycobacterium tuberculosis. Am. J. Pathol. 181, 508–514 (2012).
Hunter, L., Hingley-Wilson, S., Stewart, G. R., Sharpe, S. A. & Salguero, F. J. Dynamics of macrophage, T and B cell infiltration within pulmonary granulomas induced by Mycobacterium tuberculosis in two non-human primate models of aerosol infection. Front. Immunol. 12, 776913 (2021).
Carpenter, S. M. & Lu, L. L. Leveraging antibody, B cell and Fc receptor interactions to understand heterogeneous immune responses in tuberculosis. Front Immunol. 13, 830482 (2022).
Stewart, P. et al. Role of B cells in Mycobacterium tuberculosis infection. Vaccines (Basel) 11, 955 (2023).
Rijnink, W. F., Ottenhoff, T. H. M. & Joosten, S. A. B-cells and antibodies as contributors to effector immune responses in tuberculosis. Front. Immunol. 12, 640168 (2021).
Achkar, J. M., Chan, J. & Casadevall, A. B cells and antibodies in the defense against Mycobacterium tuberculosis infection. Immunol. Rev. 264, 167–181 (2015).
Schenkel, J. M. & Masopust, D. Tissue-resident memory T cells. Immunity 41, 886–897 (2014).
Mueller, S. N. & Mackay, L. K. Tissue-resident memory T cells: local specialists in immune defence. Nat. Rev. Immunol. 16, 79–89 (2016).
Beverley, P. C., Sridhar, S., Lalvani, A. & Tchilian, E. Z. Harnessing local and systemic immunity for vaccines against tuberculosis. Mucosal Immunol. 7, 20–26 (2014).
Urdahl, K. B. Understanding and overcoming the barriers to T cell-mediated immunity against tuberculosis. Semin. Immunol. 26, 578–587 (2014).
Hu, Z., Lu, S. H., Lowrie, D. B. & Fan, X. Y. Research advances for virus-vectored tuberculosis vaccines and latest findings on tuberculosis vaccine development. Front. Immunol. 13, 895020 (2022).
Sakai, S. et al. Cutting edge: control of Mycobacterium tuberculosis infection by a subset of lung parenchyma-homing CD4 T cells. J. Immunol. 192, 2965–2969 (2014).
Torrado, E. et al. Interleukin 27R regulates CD4+ T cell phenotype and impacts protective immunity during Mycobacterium tuberculosis infection. J. Exp. Med 212, 1449–1463 (2015).
Hu, Z. et al. The role of KLRG1 in human CD4+ T-cell immunity against tuberculosis. J. Infect. Dis. 217, 1491–1503 (2018).
Perdomo, C. et al. Mucosal BCG vaccination induces protective lung-resident memory T cell populations against tuberculosis. mBio 7, e01686-16 (2016).
Woodworth, J. S. et al. Subunit vaccine H56/CAF01 induces a population of circulating CD4 T cells that traffic into the Mycobacterium tuberculosis-infected lung. Mucosal Immunol. 10, 555–564 (2017).
Carpenter, S. M., Yang, J. D., Lee, J., Barreira-Silva, P. & Behar, S. M. Vaccine-elicited memory CD4+ T cell expansion is impaired in the lungs during tuberculosis. PLoS Pathog. 13, e1006704 (2017).
Jeyanathan, M. et al. CXCR3 signaling is required for restricted homing of parenteral tuberculosis vaccine-induced T cells to both the lung parenchyma and airway. J. Immunol. 199, 2555–2569 (2017).
Lindenstrom, T. et al. T cells primed by live mycobacteria versus a tuberculosis subunit vaccine exhibit distinct functional properties. EBioMedicine 27, 27–39 (2018).
Darrah, P. A. et al. Prevention of tuberculosis in macaques after intravenous BCG immunization. Nature 577, 95–102 (2020).
Netea, M. G., Quintin, J. & van der Meer, J. W. Trained immunity: a memory for innate host defense. Cell Host Microbe 9, 355–361 (2011).
Netea, M. G. & van der Meer, J. W. Trained immunity: an ancient way of remembering. Cell Host Microbe 21, 297–300 (2017).
Hu, Z., Lu, S. H., Lowrie, D. B. & Fan, X. Y. Trained immunity: a Yin-Yang balance. MedComm (2020) 3, e121 (2022).
Cheng, S. H. et al. Demonstration of increased anti-mycobacterial activity in peripheral blood monocytes after BCG vaccination in British school children. Clin. Exp. Immunol. 74, 20–25 (1988).
Cheng, S. H. et al. Monocyte antimycobacterial activity before and after Mycobacterium bovis BCG vaccination in Chingleput, India, and London, United Kingdom. Infect. Immun. 61, 4501–4503 (1993).
Kleinnijenhuis, J. et al. Bacille Calmette-Guerin induces NOD2-dependent nonspecific protection from reinfection via epigenetic reprogramming of monocytes. Proc. Natl Acad. Sci. USA 109, 17537–17542 (2012).
Kleinnijenhuis, J. et al. Long-lasting effects of BCG vaccination on both heterologous Th1/Th17 responses and innate trained immunity. J. Innate Immun. 6, 152–158 (2014).
Arts, R. J. W. et al. Immunometabolic pathways in BCG-induced trained immunity. Cell Rep. 17, 2562–2571 (2016).
Kaufmann, E. et al. BCG educates hematopoietic stem cells to generate protective innate immunity against tuberculosis. Cell 172, 176–190.e119 (2018).
Giamarellos-Bourboulis, E. J. et al. Activate: randomized clinical trial of BCG vaccination against infection in the elderly. Cell 183, 315–323.e319 (2020).
Xu, J. C. et al. Multi-omics analysis reveals that linoleic acid metabolism is associated with variations of trained immunity induced by distinct BCG strains. Sci. Adv. 10, eadk8093 (2024).
Cohen, S. B. et al. Alveolar macrophages provide an early mycobacterium tuberculosis niche and initiate dissemination. Cell Host Microbe 24, 439–446 e434 (2018).
Rothchild, A. C. et al. Alveolar macrophages generate a noncanonical NRF2-driven transcriptional response to Mycobacterium tuberculosis in vivo. Sci. Immunol. 4, eaaw6693 (2019).
Rajaram, M. V., Ni, B., Dodd, C. E. & Schlesinger, L. S. Macrophage immunoregulatory pathways in tuberculosis. Semin. Immunol. 26, 471–485 (2014).
Lovey, A. et al. Early alveolar macrophage response and IL-1R-dependent T cell priming determine transmissibility of Mycobacterium tuberculosis strains. Nat. Commun. 13, 884 (2022).
Mai, D. et al. Exposure to Mycobacterium remodels alveolar macrophages and the early innate response to Mycobacterium tuberculosis infection. PLoS Pathog. 20, e1011871 (2024).
Yao, Y. et al. Induction of autonomous memory alveolar macrophages requires T cell help and is critical to trained immunity. Cell 175, 1634–1650.e1617 (2018).
D’Agostino, M. R. et al. Airway macrophages mediate mucosal vaccine-induced trained innate immunity against Mycobacterium tuberculosis in early stages of infection. J. Immunol. 205, 2750–2762 (2020).
Mata, E. et al. Pulmonary BCG induces lung-resident macrophage activation and confers long-term protection against tuberculosis. Sci. Immunol. 6, eabc2934 (2021).
Jeyanathan, M. et al. Parenteral BCG vaccine induces lung-resident memory macrophages and trained immunity via the gut-lung axis. Nat. Immunol. 23, 1687–1702 (2022).
Ravesloot-Chavez, M. M., Van Dis, E. & Stanley, S. A. The innate immune response to Mycobacterium tuberculosis infection. Annu Rev. Immunol. 39, 611–637 (2021).
Larsen, S. E., Williams, B. D., Rais, M., Coler, R. N. & Baldwin, S. L. It takes a village: the multifaceted immune response to Mycobacterium tuberculosis infection and vaccine-induced immunity. Front. Immunol. 13, 840225 (2022).
Kim, H., Choi, H. G. & Shin, S. J. Bridging the gaps to overcome major hurdles in the development of next-generation tuberculosis vaccines. Front. Immunol. 14, 1193058 (2023).
Morrison, H. & McShane, H. Local pulmonary immunological biomarkers in tuberculosis. Front. Immunol. 12, 640916 (2021).
Huang, X., Lowrie, D. B., Fan, X. Y. & Hu, Z. Natural products in anti-tuberculosis host-directed therapy. Biomed. Pharmacother. 171, 116087 (2024).
Tanner, R., O’Shea, M. K., Fletcher, H. A. & McShane, H. In vitro mycobacterial growth inhibition assays: a tool for the assessment of protective immunity and evaluation of tuberculosis vaccine efficacy. Vaccine 34, 4656–4665 (2016).
Tanner, R. et al. The in vitro direct mycobacterial growth inhibition assay (MGIA) for the early evaluation of TB vaccine candidates and assessment of protective immunity: a protocol for non-human primate cells. F1000Res 10, 257 (2021).
Tanner, R. et al. A non-human primate in vitro functional assay for the early evaluation of TB vaccine candidates. NPJ Vaccines 6, 3 (2021).
Painter, H. et al. Demonstrating the utility of the ex vivo murine mycobacterial growth inhibition assay (MGIA) for high-throughput screening of tuberculosis vaccine candidates against multiple Mycobacterium tuberculosis complex strains. Tuberculosis 146, 102494 (2024).
Hoft, S. G. et al. Imprinting of gut-homing receptors on Mtb-specific Th1* cells is associated with reduced lung homing after gavage BCG vaccination of Rhesus macaques. mBio 14, e0022023 (2023).
Nemeth, J. et al. Contained Mycobacterium tuberculosis infection induces concomitant and heterologous protection. PLoS Pathog. 16, e1008655 (2020).
Hamasur, B. et al. Rapid diagnosis of tuberculosis by detection of mycobacterial lipoarabinomannan in urine. J. Microbiol. Methods 45, 41–52 (2001).
Flores, J., Cancino, J. C. & Chavez-Galan, L. Lipoarabinomannan as a point-of-care assay for diagnosis of tuberculosis: how far are we to use it? Front. Microbiol. 12, 638047 (2021).
Gu, W. F. et al. Effectiveness of Histopathological Examination of Ultrasound-guided Puncture Biopsy Samples for Diagnosis of Extrapulmonary Tuberculosis. Biomed. Environ. Sci. 37, 170–177 (2024).
Bohrer, A. C. et al. Eosinophils are part of the granulocyte response in tuberculosis and promote host resistance in mice. J. Exp. Med. 218, e20210469 (2021).
Hu, Z. et al. Pathomorphological characteristics of tuberculous placenta and its clinical implication. Diagn. Pathol. 18, 128 (2023).
Saktiawati, A. M. I., Putera, D. D., Setyawan, A., Mahendradhata, Y. & van der Werf, T. S. Diagnosis of tuberculosis through breath test: a systematic review. EBioMedicine 46, 202–214 (2019).
Phillips, M. et al. Point-of-care breath test for biomarkers of active pulmonary tuberculosis. Tuberculosis 92, 314–320 (2012).
Coussens, A. K. et al. Classification of early tuberculosis states to guide research for improved care and prevention: an international Delphi consensus exercise. Lancet Respir. Med. 12, 484–498 (2024).
Gordon, S. B. et al. A framework for Controlled Human Infection Model (CHIM) studies in Malawi: report of a Wellcome Trust workshop on CHIM in Low Income Countries held in Blantyre, Malawi. Wellcome Open Res. 2, 70 (2017).
Minassian, A. M. et al. A human challenge model for Mycobacterium tuberculosis using Mycobacterium bovis bacille Calmette-Guerin. J. Infect. Dis. 205, 1035–1042 (2012).
Harris, S. A. et al. Evaluation of a human BCG challenge model to assess antimycobacterial immunity induced by BCG and a candidate tuberculosis vaccine, MVA85A, alone and in combination. J. Infect. Dis. 209, 1259–1268 (2014).
Blazevic, A. et al. Phase 1 open-label dose escalation trial for the development of a human bacillus Calmette-Guerin challenge model for assessment of tuberculosis immunity in vivo. J. Infect. Dis. 229, 1498–1508 (2024).
Satti, I. et al. Safety of a controlled human infection model of tuberculosis with aerosolised, live-attenuated Mycobacterium bovis BCG versus intradermal BCG in BCG-naive adults in the UK: a dose-escalation, randomised, controlled, phase 1 trial. Lancet Infect. Dis. 24, 909–921 (2024).
Davids, M. et al. A human lung challenge model to evaluate the safety and immunogenicity of PPD and live bacillus Calmette-Guerin. Am. J. Respir. Crit. Care Med. 201, 1277–1291 (2020).
Basu Roy, R. et al. An auto-luminescent fluorescent BCG whole blood assay to enable evaluation of paediatric mycobacterial responses using minimal blood volumes. Front. Pediatr. 7, 151 (2019).
Bekeredjian-Ding, I. et al. Human challenge trial workshop: focus on quality requirements for challenge agents, Langen, Germany, October 22, 2019. Biologicals 66, 53–61 (2020).
Wang, X. et al. Development of an engineered Mycobacterium tuberculosis strain for a safe and effective tuberculosis human challenge model. bioRxiv https://doi.org/10.1101/2023.11.19.567569 (2023).
Balasingam, S. et al. Review of the current TB human infection studies for use in accelerating TB vaccine development: a meeting report. J. Infect. Dis. 230, e457–e464 (2024).
Donald, P. R. et al. Droplets, dust and guinea pigs: an historical review of tuberculosis transmission research, 1878-1940. Int. J. Tuberc. Lung Dis. 22, 972–982 (2018).
Plumlee, C. R. et al. Ultra-low dose aerosol infection of mice with Mycobacterium tuberculosis more closely models human tuberculosis. Cell Host Microbe 29, 68–82 e65 (2021).
Vidal, S. J. et al. Attenuated Mycobacterium tuberculosis vaccine protection in a low-dose murine challenge model. iScience 26, 106963 (2023).
Plumlee, C. R. et al. Assessing vaccine-mediated protection in an ultra-low dose Mycobacterium tuberculosis murine model. PLoS Pathog. 19, e1011825 (2023).
Kwon, K. W. et al. Immunogenicity and protective efficacy of RipA, a peptidoglycan hydrolase, against Mycobacterium tuberculosis Beijing outbreak strains. Vaccine 42, 1941–1952 (2024).
Smith, C. M. et al. Host-pathogen genetic interactions underlie tuberculosis susceptibility in genetically diverse mice. Elife 11, e74419 (2022).
Lai, R. et al. Host genetic background is a barrier to broadly effective vaccine-mediated protection against tuberculosis. J. Clin. Invest. 133, e167762 (2023).
Ahmed, M. et al. Immune correlates of tuberculosis disease and risk translate across species. Sci. Transl. Med. 12, eaay0233 (2020).
Kurtz, S. L. et al. The diversity outbred mouse population is an improved animal model of vaccination against tuberculosis that reflects heterogeneity of protection. mSphere 5, https://doi.org/10.1128/msphere.00097-20 (2020).
Kurtz, S. L. et al. Multiple genetic loci influence vaccine-induced protection against Mycobacterium tuberculosis in genetically diverse mice. PLoS Pathog. 20, e1012069 (2024).
Leroux-Roels, I. et al. Improved CD4(+) T cell responses to Mycobacterium tuberculosis in PPD-negative adults by M72/AS01 as compared to the M72/AS02 and Mtb72F/AS02 tuberculosis candidate vaccine formulations: a randomized trial. Vaccine 31, 2196–2206 (2013).
Tait, D. R. et al. Final analysis of a trial of M72/AS01(E) vaccine to prevent tuberculosis. N. Engl. J. Med. 381, 2429–2439 (2019).
Nemes, E. et al. The quest for vaccine-induced immune correlates of protection against tuberculosis. Vaccin. Insights 1, 165–181 (2022).
Hansen, S. G. et al. Prevention of tuberculosis in rhesus macaques by a cytomegalovirus-based vaccine. Nat. Med. 24, 130–143 (2018).
Larson, E. C. et al. Intravenous Bacille Calmette-Guerin vaccination protects simian immunodeficiency virus-infected macaques from tuberculosis. Nat. Microbiol. 8, 2080–2092 (2023).
Darrah, P. A. et al. Airway T cells are a correlate of i.v. Bacille Calmette-Guerin-mediated protection against tuberculosis in rhesus macaques. Cell Host Microbe 31, 962–977 e968 (2023).
Peters, J. M. et al. Protective intravenous BCG vaccination induces enhanced immune signaling in the airways. bioRxiv https://doi.org/10.1101/2023.07.16.549208 (2023).
Irvine, E. B. et al. Humoral correlates of protection against Mycobacterium tuberculosis following intravenous Bacille Calmette-Guerin vaccination in Rhesus macaques. bioRxiv https://doi.org/10.1101/2023.07.31.551245 (2023).
Simonson, A. W. et al. CD4 T cells and CD8alpha+ lymphocytes are necessary for intravenous BCG-induced protection against tuberculosis in macaques. bioRxiv https://doi.org/10.1101/2024.05.14.594183 (2024).
Liu, Y. E. et al. Blood transcriptional correlates of BCG-induced protection against tuberculosis in Rhesus macaques. Cell Rep. Med. 4, 101096 (2023).
Flores-Valdez, M. A., Kupz, A. & Subbian, S. Recent developments in mycobacteria-based live attenuated vaccine candidates for tuberculosis. Biomedicines 10, 2749 (2022).
Shah, M. & Dorman, S. E. Latent tuberculosis infection. N. Engl. J. Med. 385, 2271–2280 (2021).
Zhao, H. M. et al. Differential T cell responses against DosR-associated antigen Rv2028c in BCG-vaccinated populations with tuberculosis infection. J. Infect. 78, 275–280 (2019).
Jenum, S. et al. A phase I/II randomized trial of H56:IC31 vaccination and adjunctive cyclooxygenase-2-inhibitor treatment in tuberculosis patients. Nat. Commun. 12, 6774 (2021).
Day, T. A. et al. Safety and immunogenicity of the adjunct therapeutic vaccine ID93 + GLA-SE in adults who have completed treatment for tuberculosis: a randomised, double-blind, placebo-controlled, phase 2a trial. Lancet Respir. Med. 9, 373–386 (2021).
Sagawa, Z. K. et al. Safety and immunogenicity of a thermostable ID93 + GLA-SE tuberculosis vaccine candidate in healthy adults. Nat. Commun. 14, 1138 (2023).
Chen, Z. et al. A multistage protein subunit vaccine as BCG-booster confers protection against Mycobacterium tuberculosis infection in murine models. Int. Immunopharmacol. 139, 112811 (2024).
Simmons, J. D. et al. Immunological mechanisms of human resistance to persistent Mycobacterium tuberculosis infection. Nat. Rev. Immunol. 18, 575–589 (2018).
Chen, Z. Y. et al. Decreased expression of CD69 on T cells in tuberculosis infection resisters. Front. Microbiol. 11, 1901 (2020).
Jalbert, E. et al. Comparative immune responses to Mycobacterium tuberculosis in people with latent infection or sterilizing protection. iScience 26, 107425 (2023).
Davies, L. R. L. et al. IFN-gamma independent markers of Mycobacterium tuberculosis exposure among male South African gold miners. EBioMedicine 93, 104678 (2023).
Krishnananthasivam, S. et al. An anti-LpqH human monoclonal antibody from an asymptomatic individual mediates protection against Mycobacterium tuberculosis. NPJ Vaccines 8, 127 (2023).
Cross, D. L. et al. MR1-restricted T cell clonotypes are associated with “resistance” to Mycobacterium tuberculosis infection. JCI Insight 9, e166505 (2024).
Simmons, J. D. et al. Monocyte transcriptional responses to Mycobacterium tuberculosis associate with resistance to tuberculin skin test and interferon gamma release assay conversion. mSphere 7, e0015922 (2022).
Simmons, J. D. et al. Monocyte metabolic transcriptional programs associate with resistance to tuberculin skin test/interferon-gamma release assay conversion. J. Clin. Invest. 131, e140073 (2021).
Dill-McFarland, K. A. et al. Epigenetic programming of host lipid metabolism associates with resistance to TST/IGRA conversion after exposure to Mycobacterium tuberculosis. bioRxiv https://doi.org/10.1101/2024.02.27.582348 (2024).
Zhang, F. et al. HDAC6 contributes to human resistance against Mycobacterium tuberculosis infection via mediating innate immune responses. FASEB J. 35, e22009 (2021).
Weiner, J. et al. Changes in transcript, metabolite, and antibody reactivity during the early protective immune response in humans to Mycobacterium tuberculosis infection. Clin. Infect. Dis. 71, 30–40 (2020).
Ran, F. et al. Whole-transcriptome sequencing of phagocytes reveals a ceRNA network contributing to natural resistance to tuberculosis infection. Micro Pathog. 192, 106681 (2024).
Nam, Y. et al. Harnessing artificial intelligence in multimodal omics data integration: paving the path for the next frontier in precision medicine. Annu. Rev. Biomed. Data Sci. 7, 225–250 (2024).
Acknowledgements
We are thankful for the grants from the National Natural and Science Foundation of China (82171739, 82171815, 32394014, and 81873884), the National Key Research and Development Program of China (2021YFC2301503 and 2022YFC2302900), and the Shanghai Municipal Health Bureau (2022XD060). We thank Dr. Douglas B. Lowrie for his editing contribution to this paper.
Author information
Authors and Affiliations
Contributions
J.W., X.-Y.F., and Z.H. conceived and designed and the paper, J.W. and Z.H. wrote the paper, X.-Y.F. reviewed the paper, Z.H. revised the paper. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, J., Fan, XY. & Hu, Z. Immune correlates of protection as a game changer in tuberculosis vaccine development. npj Vaccines 9, 208 (2024). https://doi.org/10.1038/s41541-024-01004-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41541-024-01004-w
This article is cited by
-
Discovery of a multi-epitope tuberculosis vaccine targeting phospholipase C virulence factors: an insilico approach
Biotechnology Letters (2026)
-
A temperature-responsive PLA-based nanosponge as a novel nanoadjuvant and efficient delivery carrier of Ag85B for effective vaccine against Mycobacterium tuberculosis
Cell Communication and Signaling (2025)
-
Global threshold dynamics of a novel TB model with post-exposure vaccination and preventive treatment: China’s roadmap to 2035
Advances in Continuous and Discrete Models (2025)
-
Strong immune responses and robust protection following a novel protein in adjuvant tuberculosis vaccine candidate
Scientific Reports (2025)