Abstract
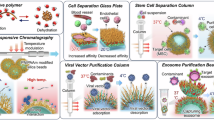
Versatile technologies that can deliver both RNA and protein payloads could streamline development, simplify manufacturing and expand the capabilities of combination therapies. Here we demonstrate an efficient approach to forming ca. 100 nm polymer vesicles (polymersomes) capable of rapid self-assembly without organic solvents, avoiding the need for post-encapsulation purification. Block copolymers are designed with a lower critical solution temperature that renders them soluble in aqueous medium under standard refrigeration, but they spontaneously assemble at room temperature into large batches of nanoparticles with predictable size and morphology. The nanomaterials are designed with charged and biofunctional moieties to drive payload affinity and in vivo targeting, while both siRNA and proteins can be encapsulated during warming at >75% loading efficiencies. Formulations can be stored in a dry state for greater hydrolytic stability under standard refrigeration and can be diluted directly from the vial, bypassing the need for purification required for high scalability. We use our system for in vivo delivery in protein subunit vaccination, immune tolerance induction and siRNA interference therapy in cancer.
Similar content being viewed by others
Main
Advancements in nanomedicine have allowed researchers to develop biomacromolecular therapies efficiently and precisely, for example, small-interfering RNA (siRNA), messenger RNA (mRNA) and protein therapies, including vaccines and tolerogenic, or inverse, vaccines1,2,3,4,5. However, effective payload protection and delivery are key requirements for immunological efficacy as these payloads are highly sensitive to clearance and degradation when administered in vivo. To this extent, much promise has been demonstrated by the lipid nanoparticle (LNP) technology used by Pfizer/BioNTech and Moderna for their mRNA-based vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)6. Furthermore, LNPs designed by Alnylam Pharmaceuticals have successfully demonstrated intravenous (i.v.) delivery of siRNA for the treatment of hereditary transthyretin-mediated amyloidosis in the liver using the RNA interference (RNAi) pathway4. However, issues with storage stability and complex processing limit broader access to such nanoparticulate therapies and motivate improvements in materials for formulation. LNPs are highly specialized for nucleic acid delivery and no such formulations exist for protein payloads. Polymer nanoparticles have long been considered a key alternative to LNPs, as the high molecular weight (typically >5 kDa) of their substituents imparts good stability, which is combined with high tunability on account of extensive advances in polymer chemistry. Furthermore, their synthetic versatility is particularly attractive for achieving delivery of a wide range of payloads such as proteins, small molecules and nucleic acids.
Polymersomes (PSs) are a class of vesicular polymer nanoparticles composed of self-assembled amphiphilic block copolymers (BCPs), first described by Discher and Eisenberg in the mid-1990s7. These vesicles consist of a lyotropic membrane formed by polymer chain interactions between hydrophobic domains, making them more stable than LNPs7,8. The hydrophilic polymer block forms the PS corona and can reduce protein adsorption and unwanted immune recognition, prolonging circulation time. Moreover, their size (50–200 nm) and stability make PSs ideal for cellular uptake1. Despite these benefits, formulation is complex as the organic solvents that are required to solubilize both domains must then be evaporated or diluted in an aqueous medium9. Self-assembly therefore occurs at an interface, either water–polymer or water–organic solvent, leading to kinetic trapping of structures and therefore inhomogeneous aggregates that must be processed into uniform morphologies10,11,12. Postprocessing techniques require filter extrusions to ensure monodisperse populations and often lead to suboptimal payload encapsulation and material loss13. Approaches address these limitations by rapidly mixing solutions with specialized microfluidic devices, but these require extensive operation time and greatly dilute the formulation, which then requires further concentrating14,15,16. Furthermore, organic solvents can be toxic and denature biological payloads, particularly detrimental to those that require their complex three-dimensional (3D) architecture for retaining activity or immune recognition features, for example, protein conformational antigens. Despite their synthetic tunability, PSs typically show modest loading efficiencies (≤20% for proteins), and the complexities described above have prevented widespread clinical translation10.
In this work, we have advanced PSs as a delivery vehicle for protein, nucleic acid adjuvant and siRNA payloads by enhancing encapsulation efficiency through copolymer design, enabling facile, streamlined processing. The formulations herein demonstrate rapid assembly of near-monodisperse PSs without organic solvents to circumvent purification issues. This is achieved through two design principles: thermoresponsive PS assembly and affinity-driven payload encapsulation. The BCPs are solubilized in aqueous medium when refrigerated (4–7 °C) and self-assemble at room temperature (above 20 °C) into homogeneous PSs. This is achieved by incorporating polymer segments with a lower critical solution temperature (LCST) below room temperature but above the freezing point of water17,18,19. The BCPs are dissolved alongside a hydrophilic payload and their uniform self-assembly bypasses the need for solvent and size-exclusion purifications. Furthermore, cationic moieties are incorporated within the hydrophilic domains to attract negatively charged groups in protein and nucleic acid payloads. Electrostatics drives high loading efficiencies (75–99%) and reduces the amount of synthetic material (50–200 µg) required for treatment. Our ability to dissolve polymers at high solids content (~20 wt%) improves scalability and encapsulation of protein payloads. As is known in the LNP literature, low concentrations often prevent appreciable loading for protein payloads owing to the sparse charge distribution, which requires modifications to the native protein20. The components of our system can even be co-lyophilized for improved storage stability during distribution then reconstituted below the LCST, self-assembled at room temperature and still retain all material properties and performance. We demonstrate the use of such facile formulations in the contexts of protein subunit vaccination, protein inverse vaccination for tolerance induction and RNAi for cancer immunotherapy. Such a platform may prove useful in growing efforts to develop non-viral vectors for biomacromolecule delivery1.
Results
Thermosensitive polymers for rapid, streamlined PS assembly
In prior work, materials scientists demonstrated the utility of poly(oligo(ethylene glycol) acrylate)s as a versatile LCST polymer, whose LCST is tunable from 0 to 100 °C by varying the number of ethylene glycol units in the side chain18,19,21,22. Chilkoti further demonstrated a biological utility of such polymers for increasing hydrodynamic radius and reducing protein clearance as an alternative to the widely used poly(ethylene glycol) (PEG), as the short oligoethylene glycol side chains avoid the development of a humoral immune response, in contrast with the development of anti-PEG antibodies23. Here, we chose poly(diethylene glycol ethyl ether acrylate) (pDEGEA) as our PS membrane-forming block as its LCST transition is around 13–15 °C, allowing for it be soluble at ca. 4 °C and form self-assemblies at room temperature. The pDEGEA-containing BCPs were designed with block lengths chosen to allow for the self-assembly of vesicular structures characteristic of PSs (Fig. 1a and Supplementary Fig. 1). On the basis of previous literature, block lengths of 120–175 repeat units for the membrane-forming pDEGEA (denoted ‘D’) and block lengths of 15–70 repeat units for the hydrophilic, corona-forming blocks were chosen to maintain the hydrophilic weight fraction at 10–25% and yield vesicular morphology9 (Fig. 1b). For all studies herein, D130 (subscript denotes the number of repeat units) was used as the membrane-forming material, and either poly(hydroxyethyl acrylate) (pHEA) (‘H70’) or poly(trimethylamino ethyl acrylate) (pTMAEA) or (‘TM25’) was the hydrophilic segment for uncharged and charged polymers, respectively (Fig. 1b–d). Work from Eisenberg demonstrated that asymmetric vesicles comprising a BCP blend can be formed by synthesizing the hydrophilic component in one BCP to be much shorter than the hydrophilic chain in the other, while maintaining the same length of membrane-forming segments in both24. For this reason, the TM25 segment in our polymers was designed to be much shorter than H70 segment, while the same length of pDEGEA was used in both BCPs to ensure self-assembly of monomodally distributed particles. Degrees of polymerization were determined by 1H NMR (Supplementary Fig. 2) and BCP end groups were modified to enhance particle stability and introduce bioactivity (below).
a, A schematic representation of the proposed mechanism for thermally mediated PS self-assembly described herein. Polymers are fully dispersed in aqueous solution at standard refrigeration temperatures and self-assemble homogeneously upon warming to room temperature. Red domains are thermoresponsive to form the PS membrane and blue are hydrophilic domains. b, BCPs used for blended formulations of PSs, with degrees of polymerization (subscripts) measured by NMR. End groups for pDEGEA-block–pHEA (D130–H70) are modified to incorporate either a single mannose moiety at the chain end or a bioinert hydroxyl moiety. All polymers are synthesized from the parent D130 homopolymer and therefore the membrane-forming segment is the same chain length in all formulations. NC refers to the cyano group (‘N triple bonded to C’). c, GPC for BCPs indicates monomodal distributions with low polydispersity (Đ <1.3), plotted as differential refractive index (dRI) versus elution time. D130–DM25 denotes pDEGEA-block–p(DMAEA) (pDEGEA-b–p(DMAEA)) before quaternization. d, A table of the full chemical characterization of parent D130 and subsequent BCPs. Mn (NMR) was determined before end-group modification to retain the RAFT chain end protons, and Mn and polydispersity (Đ) by GPC was measured post-modification. N/A, not available.
End-group functionalization of the D130–H70 and D130–TM25 polymers was achieved by aminolysis of the trithiocarbonate terminal group25, followed by a thia-Michael reaction with a compound containing an acrylate moiety. For example, D130–H70-Mann was modified by reaction with a mannose-bearing acrylate26 (Supplementary Fig. 3). Owing to the high molecular weight of the polymers, 1H NMR could not quantify chain ends and successful end-group functionalization was determined by a combination of UV–visible spectroscopy (UV–Vis), to monitor the loss of the trithiocarbonate absorbance peak at 308 nm during aminolysis (Supplementary Fig. 4), followed by two colorimetric assays, Ellman’s and phenol-H2SO4, to determine the efficiency of the thia-Michael reaction27,28. The former was used to validate the absence of any remaining free thiols (which are generated as a part of the aminolysis reaction), while the latter was used to determine the quantity of mannose moieties in the mannosylated formulations (Fig. 2a). The theoretical amount of mannose under our assay conditions (assuming one molecule per polymer chain) was 60 nmol per 2 mg of material and the slightly lower determined amount (ca. 50 nmol mannose per 2 mg polymer) is attributed to variances in sample heating when following the literature procedure for the phenol-H2SO4 assay, along with some loss in BCP chain-end fidelity during purification. Final BCPs were characterized using gel permeation chromatography (GPC) for molecular weight distribution. D130–H75 shows a monomodal molecular weight distribution with low dispersity (Đ = 1.2), relative to poly(methyl methacrylate) (PMMA) standards (Fig. 1c,d). It was difficult to obtain good-quality GPC data on D130–TM25 owing to the quaternary ammonium groups29,30. However, the polymer before quaternization, D130–DM25, showed relatively low dispersity (Đ = 1.3), with slight tailing due to the presence of tertiary amines31.
a, BCP end-group measured with colorimetric assays to determine amounts of mannose (phenol-H2SO4 assay) and residual free thiol (Ellman’s assay) (n = 2 for both). b, Thermal response of D130–H70 in PBS as measured by temperature-varied DLS to probe total scattering intensity as well as particle size. An increase in scattering intensity is indicative of nanoparticle formation from freely dissolved unimers. A gradual increase followed by sudden drop in radius demonstrates distinct behaviour associated with micelle-worm–vesicle transition. c, A schematic representation for blended formulations consisting of three BCPs: D130–H70 (inert), D130–H70-Mann (mannosylated) and D130–TM25 (charged). For brevity, formulations are referred to only as weight per cent of charged and mannosylated BCPs used (TxMy), with the remainder being the bioinert D130–H70. d, Size distributions of all nanoparticle formulations were measured by DLS and show favourable sizes (ca. 100 nm) with low dispersity (PDI <0.2) for blended formulations. e, Representative negative-stain TEM image of T0M0 PSs prepared at room temperature showing vesicular morphology. f, MALS data for the samples in d, using the Rayleigh–Gans approximation for spherical particles and denoting form factor (RG/RH). RG/RH ≈ 1 suggests a vesicular structure. Scattering intensity, Rθ/Kc, is plotted as a function of scattering angle, sin2(θ/2). P, the particle form factor as a function of light scattering angle θ; u, a substitution variable; λ, the wavelength of the laser, which is 658 nm. g, Loading efficiency as determined by non-reducing, detergent-free gel electrophoresis for protein and siRNA. Faintness in bands shows effective loading relative to free payload control, demonstrating high loading efficiency for the BCP blend formulations indicated. OVA was used as a model protein, and fluorescent (FAM)-siRNA. Data in a are technical replicates plotted as mean ± s.d. and are compared using an unpaired, two-tailed Student’s t-test.
The LCSTs of our materials along with resulting nanoparticle size were determined using dynamic light scattering (DLS) in phosphate buffered saline (PBS, pH 7.4). A sharp increase in scattering intensity at 17 °C suggests a morphology transition from unimers to polymer nanoparticles (Fig. 2b). It is noteworthy that a sharp peak in hydrodynamic radius was observed upon initial transition, followed by a decrease to a stable radius once the system reached room temperature (20 °C). Previous work from Armes and coworkers attributes this behaviour to the micelle-worm–vesicle transition, as determined by rigorous microscopy studies32. Polymer blends were made by mixing charged and uncharged BCPs at different weight ratios to formulate nanoparticles with varying degrees of charge to enhance payload encapsulation efficiency. Nanoparticles are therefore reported here as the relative weight fractions of the charged BCP, D130–TM25 (‘T’) and mannosylated BCP, D130–H70-Mann (‘M’). The remainder of the nanoparticle weight fraction consists of the inert BCP, D130–H70. The blended particles are referred to as ‘TxMy’, with ‘x’ and ‘y’ being the relative weight percentages of charged and mannosylated BCPs, respectively (Fig. 2c).
The polymers were highly soluble in aqueous media at low temperatures and could be dissolved at high concentrations, although the concentrations were kept less than 100 mg ml−1 to favour vesicular assembly, as demonstrated by Battaglia and coworkers33. Following self-assembly by warming to room temperature, size and morphology were determined by DLS (Fig. 2d), transmission electron microscopy (TEM) (Fig. 2e) and multi-angle light scattering (MALS) for determining the radius of gyration (RG) (Fig. 2f). By DLS, we noted hydrodynamic radii (RH) of favourable size (~100 nm) and distribution (polydispersity index, PDI <0.1) with a single peak in distribution (Fig. 2d), indicating uniform assembly for our BCP blended system. The zeta potential for the charged BCP-only PS (T100M0) is highly positive (+14 mV), but incorporating the uncharged BCPs lowers this charge of these mixed PSs, as expected, to within biologically non-toxic values34 (Supplementary Fig. 5). To quantitatively assess vesicular structure for nanoparticles used in vitro and in vivo, we determined a form factor, RG/RH, which should be equal to 1 for hollow sphere or vesicle35. This is because RG quantifies the mass distribution of a particle, which is theoretically distributed along its radius rather than its core for a PS. All structures used in these experiments have RG/RH between 0.93 and 1.18 and can be reasonably approximated as being spherical vesicles (Fig. 2f). Morphologies are also qualitatively confirmed with negative-staining TEM, showing sizes similar to those observed by light scattering, with slight deviations attributed to drying upon sample preparation (Fig. 2e). As determined by both RG/RH and TEM imaging, all particles used in biological studies were indeed vesicular when assembled under physiological salt concentrations in saline or PBS. Importantly, it was possible to obtain reproducible particle sizes given that the self-assembly is dictated by polymer block lengths and relative weight fractions, rather than assembly kinetics, thus leading to structures near thermodynamic equilibrium12. It is hypothesized that narrow size distributions (PDI <0.1) are due to the complete solubility of the polymers when cooled, thus avoiding inhomogeneities in dispersion36,37. Taken together, this material circumvents previous issues reported in PS processing by avoiding organic solvents for self-assembly along with yielding narrow, predictable sizes to address issues of quality control38,39.
High macromolecule loading in PSs enhances cellular uptake
Encapsulating protein payloads has often proved challenging due to their weaker electrostatic interactions relative to nucleic acids, along with the generally dilute conditions under which nanoparticles are formed40,41. Though some reports do show LNPs encapsulating protein, these instances often required modification of the payload and still require solubilizing the amphiphilic components of the delivery vehicle in an organic solvent such as ethanol20. On account of the use of organic solvents, high concentrations are not achievable with typical formulations, and the use of ionizable amines is insufficient for complexation with the sparse negative charges on proteins. By contrast, our temperature-sensitive PSs can be fully suspended in aqueous medium at high concentrations (100 mg ml−1), and the permanently charged ammonium moieties were hypothesized to have enhanced electrostatic affinity for weakly charged residues on proteins42. Such high solids content is critical for maximizing encapsulation efficiency while still maintaining vesicular morphology33,43. Previous attempts to achieve this rely on complex synthetic or processing approaches, such as polymerization-induced self-assembly, microfluidic devices or flash nanoprecipitation, which require specialized reactors for scale-up and complex manipulations that present challenges for translation to the clinic44.
Our PSs consisting of BCP blends without mannosylated polymer, TxM0, encapsulate 75–90% of dissolved protein (here, the model protein ovalbumin, or OVA) in solution as determined by gel electrophoresis, with increased efficiency using higher weight percent of charged polymer (‘x’ from 33 to 100) (Fig. 2g, top). As to nucleotide payload, siRNA can be completely encapsulated (~100% efficiency) using polymer/payload weight ratios as low as 1:5 for formulations using the T50M0 BCP blend (Fig. 2g, bottom). The loading efficiencies are consistent and reproducible, and they are similar when incorporating mannosylated D130–H70-Mann BCPs (Supplementary Fig. 6a). Since OVA has a net-negative charge (isoelectric point ~4.7) at physiologic pH (7.4), other therapeutically relevant biologics such as Enbrel, anti-programme cell death protein 1 (PD-1) antibody and SARS-CoV-2 RBD peptide were encapsulated (Supplementary Fig. 6b). All of these payloads have a slight net-positive charge at physiologic pH, but could still be incorporated in our particles due to the presence of negatively charged amino acids. However, we noticed that this efficiency is decreased for low molecular weight peptides compared with larger macromolecules such as antibodies. To demonstrate successful loading from dry formulations, we also dissolved our BCPs alongside the same protein and siRNA payloads, lyophilized the fully soluble mixture and then reconstituted in deionized water on ice. Samples were then allowed to warm to room temperature, and we detected similar, high loading efficiencies for both payloads (Supplementary Fig. 7a,b). The reconstituted polymers are then able to deliver OVA to in vitro cell lines and demonstrate retained bioactivity in antigen presentation assays (see below and Supplementary Fig. 7c). Such an approach to loading may be particularly beneficial for PS storage and distribution at large scales, with sensitive payloads prone to hydrolysis. Our materials were also characterized post-loading and demonstrate similar sizes and spherical morphology with both protein and siRNA payloads (Supplementary Fig. 8). Zeta potential was payload dependent, with PS-siRNA having more negative zeta potential (−0.2 to −2 mV) and PS-OVA being positive (0.6 to 9 mV). Admixing with the nucleic acid adjuvant CpG 1826 post-encapsulation also lowered the zeta potential for protein-based formulations to being slightly negative. Owing to high loading efficiency and homogeneous particle sizes upon warming, we can bypass tedious processing such as size exclusion and membrane filtration45. Furthermore, the high solids content remains a highly attractive feature of our system, as current polymer and LNP technologies rely on further processing for concentration of suspensions to achieve a robust biological response44. As a result, our materials can simply be diluted for administration without needing further processing.
Indeed, uptake studies in murine bone-marrow derived dendritic cells (BMDCs) show enhanced uptake when delivering OVA formulations in this way. Viability studies were performed to determine dose and relative charge fraction based on the MTT assay (Supplementary Fig. 9a). On account of the toxicity of highly charged moieties, we chose to use T33My based formulations to preserve cell viability. Subsequent screening studies also determined ideal ranges for mannosylation be between 10 and 33 wt% of the total particle formulation (T33M10 or T33M33) for optimal uptake. Previous literature also supports this observation that sparse ligand density is often favourable over full coverage of the particle with mannose46. For these formulations, nanoparticle-encapsulated FITC-OVA achieved 3–6-fold greater uptake by BMDCs compared with unencapsulated OVA based on the geometric mean fluorescence intensity (gMFI) in flow cytometry (Fig. 3a). To mechanistically demonstrate the utility of mannosylation for BMDC uptake, we conducted the same study using a mannose-receptor blocking cocktail consisting of mannose-receptor blocking peptide26. After blocking, mannosylated PSs showed a statistically significant decrease in uptake compared with bioinert PSs and free protein (Supplementary Fig. 9b). This suggests that incorporating targeting moieties favours uptake in a mannose-receptor dependent manner, which may prove beneficial for in vivo nanoparticle delivery in the context of antigen delivery.
a, Uptake of fluorescent OVA (FITC-OVA) by BMDCs measured by flow cytometry with corresponding fluorescence histograms on the right. Quantification of gMFI of the single, live population demonstrates significant uptake when the same amount of OVA is encapsulated in PSs compared with free FITC-OVA. b, Antigen presentation probed using BMDC co-culture with OTI labelled with CFSE, benchmarking against free OVA control. The histograms on the left show the distribution of CFSE fluorescence signal, and populations left of the dotted line are new generations of OTI cells (‘CFSE-diluted’) quantified by the bar graph on the right. c, Antibody levels measured by ELISA for C57BL/6 mice (n = 5) injected in all four hocks with a single prime vaccination. All non-saline treatments were with 10 µg OVA adjuvanted with 20 µg CpG ODN 1826. Blood was sampled periodically during a 90 day period and benchmarked to unencapsulated, adjuvanted OVA. d, Antibody levels measured 1 year post prime vaccination (vax). e, IVIS for relative fluorescence in hock-draining lymph nodes of OVA647 injected either free or with PSs in all 4 hocks, where animals were killed 4 h after administration. Lymph nodes (n = 2 from each mouse) were collected from both sides and the following locations (top to bottom): axillary, brachial, inguinal and popliteal. f, Total radiant efficiency from brachial lymph nodes quantified. Data in a and b are technical replicates (n = 3) plotted as mean ± s.d. and compared using ordinary one-way ANOVA with Tukey’s post-test for multiple comparisons. Data in c and d are biological replicates (n = 5) plotted as mean ± s.e.m. for c and box plots with max/min, median and quartiles for d. P values for day 84 (c) and 1 year antibody levels from one-way ANOVA with Tukey’s post-test for multiple comparisons.
PSs promote antigen presentation and antibody responses
After demonstrating enhanced uptake, we sought to determine the ability of our material to allow for antigen presentation once the protein has been delivered to the antigen-presenting cell (APC). Thus, functional in vitro assays were conducted to determine the efficacy of our material as an antigen delivery platform for prophylactic subunit vaccines. With the growing interest for eliciting strong CD8+ T cell responses, we first probed the ability of our material to trigger proliferation in the OVA-specific transgenic CD8+ T cell line (OTI)47. Upon co-culture with BMDCs treated with our formulations, carboxyfluorescein succinimidyl ester (CFSE)-labelled OTIs underwent varying degrees of proliferation as measured by flow cytometry (Fig. 3b). A ‘CFSE-diluted’ population (that is, proliferated to various generations) was determined as all T cells with diluted fluorescence compared with that of the original population (Fig. 3b, left of dotted line). Based on fluorescence histograms, we observed enhanced OTI proliferation (%CFSE-diluted population) when OVA was delivered encapsulated in our PSs versus free in solution. We hypothesize that endosomal escape occurs due to the hydrolytic instability of the acrylate backbone, which is prone to cleavage by the slightly acidic environment and esterase activity within the endosome48. We then probed this phenomenon using fluorescence microscopy studies co-delivering a fluorescently quenched DQ-OVA and fluorescently active OVA647 in RAW 264.7 macrophages to probe endosomal processing and uptake, respectively49 (Supplementary Fig. 9c). We observed that our nanoparticle constructs not only enhance uptake based on increased Alexa-Fluor 647 signal, but also promote endosomal processing and release into cytosol as observed by the diffuse fluorescence of DQ-OVA compared with more punctate fluorescence seen when delivering free protein alone. On the basis of these results, we envisioned that our materials would lead to stronger CD8+ T cell responses upon protein subunit vaccination compared with free antigens under equivalent adjuvant stimulation. To establish the capabilities of our materials for robust immunity, we also probed the humoral response to demonstrate that our PSs can also elicit antigen-specific antibodies, which necessitated in vivo studies. Polymer alone was first delivered intravenously to ensure no systemic toxicity, as identified by blood chemistry and inflammatory cytokine secretion (Supplementary Fig. 10).
Considering humoral responses, a pilot experiment was conducted as a single-dose vaccine using OVA admixed with the Toll-like receptor 9 (TLR9) agonist CpG ODN 1826 (Fig. 3c). CpG was the benchmark due to its current use as a clinical adjuvant for a protein-based subunit vaccines, including HEPLISAV-B and PreHevbrio, and it is particularly known to stimulate strong antibody responses. CpG is also attractive due to its solubility in aqueous buffer, broad safety profile in elderly and immune-suppressed patients and well-understood mechanism of action50. Mice were vaccinated in all four hocks using either mannosylated (T33M33) or non-mannosylated (T33M0) PS-encapsulated OVA admixed with CpG and compared with free, adjuvanted OVA formulations. We observed potent antibody responses characterized by total OVA-specific IgG measured periodically over 3 months following initial vaccination, with PS formulations significantly outperforming free protein with CpG (Fig. 3c). Though differences were not seen between the mannosylated and non-mannosylated PS groups, it became apparent that even a single administration of either formulation significantly enhanced antibody levels over that of free adjuvanted protein at equal doses. Remarkably, our PS-encapsulated OVA maintained antibody levels even 1 year after single vaccination, while antibodies from unencapsulated OVA-CpG declined to levels similar to those of untreated animals (Fig. 3d). In addition to antigen delivery, the surface charges on our PSs cause association with CpG, which may further contribute to immune stimulation in vivo, though no such effect was seen in vitro (Supplementary Fig. 11).
Initial biodistribution studies suggest that this response may be due to the enhanced retention of PS-encapsulated OVA in injection site-draining lymph nodes following vaccination (Fig. 3e,f). Interestingly, Alexa-Fluor 647-tagged OVA showed greater fluorescence in the brachial and popliteal lymph nodes when delivered in a PS formulation, whereas free OVA showed low measurable fluorescence 4 h after administration. The differences in lymph node distribution could be associated with the varying tissue architecture at each of the injection sites along with the time point chosen for measurement (4 h). Our results suggest greater consistency of lymph node trafficking when protein was delivered in encapsulated formulations, with mannosylation enhancing delivery to the brachial lymph nodes. This observation further motivated probing the lymphocyte response upon vaccination, as we hypothesized that the enhanced delivery from this platform may lead to greater immunogenicity of encapsulated OVA in both cellular and humoral responses.
PSs enhance cellular immunity in adjuvanted subunit vaccines
In a model for protein subunit vaccines, C57BL/6 mice were treated with formulations of our PSs (T33M10 and T33M0) encapsulating OVA and adjuvanted with CpG ODN 1826 in a prime-boost regimen. Our benchmark for this study was free OVA admixed with equivalent CpG, akin to clinical subunit vaccine formulations50 (Fig. 4a). Draining lymph nodes (dLNs) and spleens were collected for analysing T cell responses, while blood samples were taken at weeks 2 and 4 to determine antibody levels 1 week before and after boost. Relative to protein delivered without encapsulation, both mannosylated and non-mannosylated PSs demonstrated enhanced CD8+ T cell responses (Fig. 4b–f). As measured by peptide-MHC-I tetramer staining of lymphocytes, both formulations greatly increased populations in both CD8+ T cells (Supplementary Fig. 12a) and antigen-experienced CD44+CD8+ T cells that were tetramer positive, that is, that recognize the vaccinal antigen, relative to free protein with the same adjuvant (Fig. 4e,f). To explore the functionality of OVA-specific T cells, lymphocytes and splenocytes were subjected to 6 h restimulation studies to probe the CD8+ and CD4+ T cell responses, as measured by intracellular cytokine staining. Importantly, responses from mannosylated particles trended towards a greater percentage of IFNγ+ and IFNγ+TNF+ double-positive CD8+ T cells in the dLNs following peptide restimulation compared with our non-mannosylated PS formulation (Fig. 4b–d and Supplementary Fig. 12b). This strong response in the CD8+ T cell compartment is promising as it is known that CD8+ T cell immunity is particularly important in clearing viral infections such as SARS-CoV-2 and other respiratory infections, as well as in cancer immunotherapy51,52,53. Furthermore, CD4+ T cells also demonstrated a greater percentage of proinflammatory cytokine-secreting populations, measured by IL-2 and IFNγ (Supplementary Fig. 13a). Similarly, whole protein, 3 day restimulation of splenocytes, indicative of a systemic immune response, showed strong type-1 immunity, which has also been shown using a different PS formulation from our laboratory54. Briefly, restimulations of splenocytes led to secretions of significant levels of IFNγ and TNF over that of free, adjuvanted protein, suggesting robust T-helper responses in addition to cytotoxic T cells (Fig. 4g,h). Splenocytes also demonstrated enhanced secretion of IL-6 in response to the PS-encapsulated formulations, though significance was only observed in the mannosylated formulation (Supplementary Fig. 13b (i)), and similar trends were observed in the draining lymph nodes for IFNγ and IL-6 (Supplementary Fig. 13b (ii) and (iii)). We hypothesize that the enhanced immunogenicity of PS-encapsulated OVA is a result of enhanced uptake and cross presentation, as seen in vitro (Fig. 3a,b and Supplementary Fig. 9c), and a greater loss of free protein from the injection site55. However, given the enhanced uptake of nanoparticles in general, both delivery systems show improvements over free protein, also adjuvanted with CpG. In summary, cellular and type-1 immunity was enhanced using our PS formulations when delivering OVA antigen. Slight improvements were seen when using the mannosylated particles, as determined by functional assays for stimulating the CD8+ T cell response in the presence of the OVA peptide epitope SIINFEKL and the systemic immune response observed by whole-OVA protein stimulation.
a, Vaccination timeline with prime-boost schedule in C57BL/6 mice (n = 6). Four hocks were injected, and dLNs and the spleen were collected post-killing. All treatments were 10 µg OVA adjuvanted with 20 µg CpG ODN 1826, except saline and empty PSs (T33M10-empty). Encapsulated formulations consisted of 100 µg polymer and are benchmarked to the unencapsulated, adjuvanted OVA control. b, IFNγ-secreting CD8+ T cells were measured in dLNs and spleen after 6 h SIINFEKL restimulation using intracellular staining, with percentages reported by subtracting unstimulated from stimulated to remove non-specific responses. c, Double-positive TNF+IFNγ+-secreting CD8+ T cells measured in dLNs and spleen after 6 h SIINFEKL restimulation. d, A representative gating strategy for 6 h restimulation for intracellular cytokines. Samples are first gated on single, live CD8+ T cells. e, The gating strategy for SIINFEKL/MHC-I tetramer staining on antigen-experienced CD8+CD44+ T cells to measure antigen specificity. f, Quantification of antigen-specific CD8+ T cells. g,h, Splenocytes stimulated for 3 days using the full OVA protein, where IFNγ (g) and TNF (h) levels were measured in the supernatants to indicate a type-1 immune response. i, Total OVA-specific IgG levels measured by ELISA and reported as logAUC from serum samples taken 2 weeks post prime vaccination (day 14) and 1 week post boost (day 27). Data are biological replicates plotted as box plots with max/min, median and quartiles, and compared using ordinary one-way ANOVA with Tukey’s post-test for multiple comparisons (b and c) and a Kruskal–Wallis test with Dunn’s post-test for multiple comparisons (f). Welch’s one-way ANOVA with Dunnett post-test was used for g and h and two-way ANOVA with Sidak’s post-test was used for i. Panel a created with BioRender.com.
The OVA-specific antibody response was also investigated in this prime-boost model by measuring the antigen-specific IgG area under the curve (AUC) (Fig. 4i). Not surprisingly, total IgG for encapsulated and free OVA formulations showed modest (albeit statistically significant) differences when using CpG ODN 1826 as the adjuvant is known for its robust B cell activation56. Though the antigen-specific IgG response appears similar to that of the adjuvanted free protein, the highlight of our nanoparticle system is enhanced cellular immunity, which is believed to be more robust against antigenic drift47. Furthermore, upon looking at specific subtypes of IgG, we see enhancements in IgG2b relative to vaccination with free protein, with similar amounts of IgG1 (Supplementary Fig. 13c). This is a vital result as higher levels of IgG2b are associated with enhanced type-1 immunity, critical in controlling antiviral responses57. Taken together, we demonstrate that these thermoresponsive PSs present a facile delivery system for subunit vaccines intended for robust cellular and humoral immunity. The enhancement in type-1 and cytotoxic T cell immunity over that of free protein admixed with adjuvant demonstrates the benefit of the PS platform as a subunit vaccine, which commonly have not elicited strong cellular immunity in the clinic using CpG as an adjuvant50. Owing to the enhanced effects of our formulation, it may also be possible to lower the overall dose of antigen and adjuvant for more vulnerable populations. The ease of formulation and lack of purification may prove beneficial in the context of vaccine clinics where large therapeutic dose batches can be made simply by diluting a stock of room temperature solution.
PS encapsulation promotes tolerance against allergic asthma
In addition to subunit vaccination, the use of our material was also expanded for applications in tolerance induction towards a protein antigen, for which we also used OVA as a model protein antigen. To determine the ability of our nanoparticle system in preventing an allergic immune response, a study was conducted by intravenously administering C57BL/6J mice with either T33M10 without payload or both T33M10 and T33M0 encapsulating OVA. Mice were then subjected to an experimental model of allergic airway inflammation, during which mice are sensitized through intraperitoneal (i.p.) injections of OVA adsorbed to alum (Fig. 5a). Upon challenge with intratracheal (i.tr.) instillations of OVA, hallmarks of allergic airway disease in allergic asthma are measured, including airway eosinophilia, systemic levels of IgE and CD4+ T cell inflammation58. As a negative control, mice were treated with T33M10 without payload and sensitized using alum without OVA, thus preventing any OVA-specific allergic responses upon challenge. The key benchmark and positive control in this study was empty T33M10 PS without payload, sensitized using alum/OVA. Compared with mice treated with empty PSs, mice that were prophylactically administered PSs encapsulating OVA showed decreases in lung and airway eosinophilia (Fig. 5b–d). Flow cytometric quantification of eosinophils (Siglecf+CD11c−) in the bronchoalveolar lavage fluid (BALF) as well as lungs showed significant decreases only for the mannosylated T33M10 delivering OVA when compared with the positive control. Furthermore, a reduction in CD4+ T cells is indicative of a productive tolerogenic response, as allergies are known to be a type-2-mediated immune response59. In all cases, our mannosylated T33M10 platform delivered OVA in a systemic manner to reduce the total number of CD4+ T cells infiltrating the lungs and airways upon pulmonary challenge (Fig. 5d,e).
a, A schematic depicting a prophylactic treatment schedule for allergic airway inflammation. C57BL/6 mice (n = 4 for T33M10-empty and T33M0-OVA, n = 5 for T33M10-OVA, and n = 2 for naive control) were prophylactically treated through i.v. injections of empty mannosylated (T33M10) PSs or OVA-loaded mannosylated (T33M10) or non-mannosylated (T33M0) PSs before induction of allergic airway inflammation. All encapsulated formulations consist of 100 µg polymer with 10 µg OVA and are benchmarked to the naive control. Mice were sensitized (sens.) through i.p. injections of OVA (or saline) adsorbed to alum (1:1, with 50 µg OVA), before i.tr. instillations with 25 µg OVA (chall.). b, Representative flow cytometry plots depicting airway eosinophils (highlighted in the box) isolated from BALF. c, Airway eosinophil and CD4+ T cell quantification as determined by flow cytometry. d, Lung eosinophil and CD4 + T cell quantification as determined by flow cytometry. e, Lung CD4+ effector T cells (Teff) (FoxP3−CD44+CD62L−) and type-II lymphocytes (FoxP3−CD44+ST2+Gata3hi) (Th2) as identified by flow cytometry. f, Systemic total IgE levels as determined by ELISA, quantified through AUC of concentration versus time (left, *P = 0.0430 for the comparison between T33M10-empty and T33M10-OVA. Comparison between T33M10-empty and T33M0-OVA, P = 0.6337) as well as final amount determined on day 20 (d20) of study (right). g, Ex vivo liver delivery comparing mannosylated to non-mannosylated PS delivery measured with IVIS. h, Total radiance quantification from IVIS (n = 2). Data are biological replicates plotted as box plots with max/min, median and quartiles (c–f), line graphs (f, left) or bar graphs (h) with mean ± s.e.m. and compared using ordinary one-way ANOVA with Sidak’s post-test for multiple comparisons. Panel a created with BioRender.com.
In addition to T cells and eosinophils, B cells are known to mediate the allergic response through class switching and antibody secretion. Specifically, IgE binds antigen and stimulates mast cell degranulation. We therefore examined systemic levels of IgE post-sensitization and during the challenge phase of the model (Fig. 5f). Not surprisingly, a sharp increase in systemic IgE was observed upon challenge of the empty T33M10 PS treated group sensitized with alum/OVA. Though not a complete return to baseline, T33M10-encapsulating OVA was able to mitigate this response, as seen by significantly reduced IgE levels following initial i.tr. challenge and at endpoint. Furthermore, allergic B cell responses were also measured by flow cytometry, with reductions seen in class switching (IgM−IgD−), germinal central formation (GL-7+CD95+) and differentiation into IgE+ plasma cells (CD138+) (Supplementary Fig. 14). Taken together, the T33M10 nanoparticles provide a platform system for protein antigen delivery to effectively target immune cells in the context of tolerance induction (inverse vaccination) in the absence of an adjuvant (Fig. 5), as well as vaccination in the presence of an adjuvant (Fig. 4). Though both PS systems show trends towards reducing the allergic response, mannosylation plays a key role in further suppression, consistent with previous results from our laboratory using a soluble polymer–antigen conjugate platform60. This may be due to the mannosylated PSs promoting delivery to APCs in the liver, which is known to present antigen in a tolerogenic manner61,62 (Fig. 5g,h).
PSs outperform clinically used LNPs in RNAi
As a demonstration of the utility of our PS platform in siRNA therapy, we turned to siRNA to downregulate cancer-promoting pathways via RNAi, employing validated pathways for clear interpretation3,63,64. Vascular endothelial growth factor A (VEGF-A) is known to promote tumour cell survival and proliferation via induction of angiogenesis65,66,67. Bcl-2 is an anti-apoptotic protein that can be upregulated via the VEGFR pathway, providing a positive feedback loop for enhanced tumour cell survival68. Therefore, we chose VEGF-A and Bcl-2 as target molecules for RNAi in the human breast cancer line MCF-7, which is known to upregulate both66,69. Without chemical modification, siRNA degrades rapidly in the presence of serum in cell-culture medium, thus necessitating cationic delivery vehicles such as LNPs for transfection. For this reason, we first compared our PSs with the commercially available transfection agent, Lipofectamine 2000 (Lipo)70. In this head-to-head comparison, our PSs achieved greater gene downregulation when delivering siVEGF-A (~60% downregulation) and siBcl-2 (50% downregulation) and therefore were investigated further in in vivo cancer studies (Fig. 6a). Control studies determined the optimal dosing for PS formulations, that vehicle alone does not downregulate mRNA expression and that there is no off-target downregulation for housekeeping genes such as β-actin (Supplementary Fig. 15a–d). Since the MCF-7 cancer line does not express the mannose receptor, only the inert PS formulations T33M0 were used for RNAi studies.
a, In vitro gene knockdown efficacy in MCF-7 tumour lines using siVEGF-A and siBcl-2 encapsulated in PSs or Lipo with mRNA expression measured by RT–PCR relative to untreated controls. b, Treatment timeline for intratumoural administration in nude mice (n = 5) inoculated with MCF-7 tumour cells behind the shoulder. Tumours were allowed to grow for 10 days, then treated i.t. every alternate day for 10 days using 40 µg free or encapsulated siRNAs with 200 µg polymer. Mice were killed when tumour size reached 600 mm3. c, Tumour growth curve shows stagnation during nanoparticle treatment from day 10 until day 35, indicated by arrows. d, Survival curve for treated mice, demonstrating enhanced survival for animals receiving nanoparticle-encapsulated siRNA. e, Components for in-house LNPs dissolved in ethanol following molar ratios from a clinical formulation (based on publications and patents by Alnylam71) at a total mass concentration of 25 mg ml−1. f, The resulting sizes of LNPs when ethanol stock is rapidly mixed and diluted to 1 mg ml−1 in PBS. g, Tumour growth in nude mice inoculated (n = 5) with MCF-7 tumours and treated with either LNP-encapsulated or PS-encapsulated siRNAs. The arrows indicate days of i.t. treatment. h, Corresponding survival curves for a head-to-head comparison of LNPs and PSs as the siRNA delivery material. Data in a are technical replicates (n = 3) plotted as mean ± s.d. compared with two-way ANOVA with Sidak’s post-test for multiple comparisons. Tumour growth curves are plotted as mean ± s.e.m. P values in d and h were determined by a log-rank (Mantel–Cox) test against corresponding free siRNA and LNP-siRNA, respectively, as control groups. Panel b created with BioRender.com.
To establish the capability of our formulations for in vivo siRNA delivery, mice inoculated with MCF-7 tumours were treated intratumourally (i.t.) with encapsulated and unencapsulated siVEGF-A and siBcl-2 (Fig. 6b). Nude mice were chosen for this study to avoid immune rejection of the human tumours. As in our in vitro work, the cellular target of this RNAi therapy is the tumour cells themselves, so mannosylated PSs were not used in this study. To ensure downregulation of siRNA targets in vivo, tumour-bearing mice were treated days 11 and 13 post-inoculation and killed on day 14 to ensure tumour sizes in control-treated groups did not grow to the criteria for killing. Both mRNA and protein content were measured to confirm downregulation of both VEGF-A and Bcl-2 (Supplementary Fig. 15e–g). We then proceeded with an efficacy study to determine whether this downregulation provides therapeutic benefit. During treatment, tumour growth was halted when either siVEGF-A and siBcl-2 were delivered i.t. as encapsulated formulations (Fig. 6c,d). Statistically significant differences were observed when comparing tumour sizes taken at day 20 (Supplementary Fig. 16a), at which point intratumoural treatment was stopped and neither unformulated siRNA nor empty PSs alone had antitumour efficacy in vivo (Fig. 6c). Furthermore, a clear enhancement in survival was observed for mice treated with the siRNA-loaded PSs (Fig. 6d). Tumours rapidly grew out once treatment was stopped owing to the lack of an adaptive immune response in the host mice, but this pilot study demonstrates the ability of our material to deliver siRNA therapeutics in vivo via halting tumour growth progression. Finally, to benchmark our materials against a clinically relevant siRNA delivery technology, we formulated LNPs using lipids at molar ratios similar to those of Alnylam6,71,72 (Fig. 6e,f and Supplementary Fig. 17). Following a treatment schedule similar to that described above, we demonstrate that our PS-siRNA formulations indeed enhance survival and suppress tumour growth over that of LNPs when delivered i.t. (Fig. 6g,h). Alnylam’s formulations have been optimized for i.v. liver targeting, but we believe our approach demonstrates the versatility of the PS platform in its ability to deliver multiple payloads with a variety of administration routes. Furthermore, the intratumoural efficacy of our technology could be attributed to the greater stability of PSs due to their macromolecular chain entanglements and may present an approach for delivering biomacromolecules without requiring payload-specific optimization.
Though the study was conducted with intratumoural injections, biodistribution studies administering a fluorescent nanoparticle show trafficking to tumours upon i.v. and subcutaneous injections (Supplementary Fig. 18). Kidney accumulation is also observed, suggesting clearance particularly upon i.v. delivery. Future work will optimize nanoparticle size, surface charge and additional targeting moieties to allow for i.v. or subcutaneous delivery as it pertains to cancer therapy. As a result, we envision that this platform may allow for nanoparticle trafficking to the tumour site when parentally administered other than i.t., a topic for future study.
Discussion
In this work, we have designed and developed thermoresponsive PSs that address many of the challenges that currently limit the broad progression of the polymer nanoparticle field to clinic. Namely, we tackle issues in processing, loading efficiency and quality control by developing a scalable platform with predictable nanoparticle morphologies. This was done by designing a room temperature-forming particle system decorated with cationic moieties to enhance payload affinity and thus encapsulation efficiency. The use of electrostatic interactions allows for macromolecule encapsulation when specific chemistries are unknown and can therefore expedite testing and formulation both in clinical and laboratory settings. Compared with current LNPs, the PS platform is highly stable due to its polymer components and is adaptable to a variety of payloads, here considering proteins and nucleic acids, without further modification. Furthermore, enhancements in therapy localization can be achieved by introducing targeting moieties such as mannose for vaccine or inverse vaccine applications. By simply warming a solution to room temperature, one can rapidly form large batches of nanoparticle therapies, providing a practical solution to issues in scalability of previous polymer formulations. The PSs are then ready to inject upon dilution, without requiring purification, since 75–99% of payload is encapsulated and the nanoparticles are of predictable size and polydispersity, addressing the industry’s quality-by-design principles73. Furthermore, we envision these materials being used as dry formulations alongside sensitive biomacromolecular payloads, with reconstitution in cold aqueous medium before room temperature warming. In this way, we retain maximal stability potentially without (or at least less stringent) the need for cold-chain logistics and storage, depending on the inherent thermal stability of the payload in the lyophilized state. As a result, these stable, easy-to-use materials may provide an avenue for improving distribution and accessibility of next-generation vaccines, particularly in areas with limited resources for cold-chain logistics, storage and manufacturing.
Outlook
We have demonstrated the development of a PS that accommodates both protein and nucleic acid payloads, and we have shown applications in a subunit (protein) vaccine, an inverse (protein) vaccine and an siRNA-based cancer therapy. The key benefit of this payload-agnostic vehicle is that it allows for rapid formulation of multiple types of biomacromolecules for in vitro and in vivo delivery without any payload modification. This not only streamlines development, but may allow for subunit vaccines with greater immunogenicity, inverse vaccines inducing multi-antigen tolerance, and nucleic acid delivery vehicles that can be stored at room temperature. As to subunit vaccines, our laboratory has previously described glycopolymer–antigen conjugate vaccines, where the polymer is mannosylated and comprises TLR7/8 agonist moieties, thus producing strong cellular and humoral responses26,74. By comparison, our PS system is much simpler and thus more economical to produce, requiring mere formulation in the vial, and can be used to develop more potent subunit vaccines consisting of multiple antigens75,76. Furthermore, our benchmarking against formulations akin to HEPLISAV-B demonstrates superior, long-lasting antibodies after a single immunization, which may be critical for communities with limited vaccine supply or patient hesitancy77. As to tolerogenic, or inverse, vaccines, our laboratory has also developed glycopolymer–antigen conjugate inverse vaccines used in autoimmune therapy78,79, food allergy prevention and therapy60 and antidrug antibody80 prevention cases. The need for multi-antigen delivery is emphasized in cases of hypersensitivity, such as in allergic asthma where a single patient may respond to multiple allergens81. Once again, delivering proteins using our antigen-agnostic, non-immunogenic platform facilitates implementing therapies quickly and broadly. Finally, for nucleotide delivery—specifically siRNA therapy in cancer—we outperform clinically used LNPs. In addition to efficacy, the PS platform also offers distinct advantages over LNPs and other siRNA delivery methods, such as mild storage conditions as a lyophilized, room temperature stable powder without additional preservative, rapid formulation without tedious processing (for example, concentrating, dialysis and so on) and payload-agnostic biofunctionalization through targeting moieties as demonstrated in this work.
We demonstrate the capabilities of our material to deliver macromolecules in three distinct in vivo contexts. Further studies are still required to establish the specific mechanism of action for these materials as they pertain to complex systems in tolerance, oncology and vaccinology. Future work will explore efficacy in more clinically relevant contexts such as in subunit vaccine models with pathogen challenge, therapeutic (for example, asthma treatment) as well as prophylactic (for example, antidrug antibody prevention) tolerance induction and i.v./subcutaneous cancer therapy in immune-competent animal models. Furthermore, combination therapies using clinically established standards (for example, with checkpoint inhibitors82) may show dose-sparing benefits when using our platform, further showcasing broader therapeutic access in addition to streamlined processing. In multiple use cases, our thermoresponsive PSs demonstrate efficacy but, broadly speaking, this material may be amenable to a variety of immunological applications with features that simplify production and ultimately increase formulation potency.
Methods
Reagents
Di(ethylene glycol) ethyl ether acrylate (DEGEA), 2-(dimethylamino)ethyl acrylate (DMAEA) and 2-hydroxyethyl acrylate (HEA) were purchased from Sigma-Aldrich. DEGEA and DMAEA were distilled, passed through a basic alumina plug and stored at −80 °C before polymerization. HEA was purified following protocols from Matyjaszewski and coworkers then stored at −80 °C (ref. 83). Azobisisobutyronitrile (AIBN) was purchased from Sigma-Aldrich, recrystallized from methanol and stored at −20 °C before use. Cyanomethyl dodecyl trithiocarbonate (CDT) was purchased from Sigma-Aldrich and used as received. OVA, endotoxin-free OVA and CpG ODN 1826 (sequence: 5′-TCCATGACGTTCCTGACGTT-3′) were purchased from Invivogen. Fluorescent OVA conjugates (FITC-OVA and OVA-647) were produced by reacting either fluorescein isothiocyanate N-hydroxysuccinimide ester (FITC-NHS ester) or Alexa-Fluor 647 NHS ester (AF647 NHS ester) to OVA following standard literature procedures in carbonate/bicarbonate buffer. DQ-OVA was purchased from Fisher Scientific. All lipids used for formulating LNPs were ordered from Broadpharm. Fluorescent antibodies were ordered through BD and Biolegend (Supplementary Tables 1 and 2). Peptide tetramers were diluted 1:50, all other flow cytometry antibodies were diluted 1:200, except for the Live–Dead stains, which were diluted 1:500 in PBS containing anti-CD16/32 (Fc-block, also diluted 1:200). Surface staining was done using PBS containing 2% fetal bovine serum (FBS) and 10 mM EDTA, while intracellular staining was done using permeation buffer (BD Bioscience, 554714, for 6 h restimulation, or FoxP3/transcription factor staining kit for allergic asthma model, Invitrogen, 00-5523-00). Western blot antibodies (all rabbit origin anti-human mAbs; Bcl-2 (D17C4), VEGF-A (E9X8Q) and GAPDH (D16H11)) were ordered through Cell Signaling Technologies, the dilutions can be found below. All other reagents and solvents were ordered through Sigma-Aldrich unless otherwise noted. Solvents used in polymerizations were dried overnight on molecular sieves before use. Silencer FAM-labelled negative control #1 siRNA (MW of 13,837 Da) was purchased through Thermo Fisher Scientific (AM4620). All other siRNA sequences were designed and ordered through IDT, with dT sequences introduced to provide stability for the double-stranded structures.
The siRNA sequences (denoted as sense strands (SS) and antisense strands (AS)) used in our studies are as follows:
Human VEGF-A (SS): 5′-AAAUGUGAAUGCAGACCAAAGdTdT-3′
Human VEGF-A (AS): 5′-CUUUGGUCUGCAUUCACAUUUdTdT-3′
Human Bcl-2 (SS): 5′-AGUCAUCCACAGGGCGAUGUUdTdT-3′
Human Bcl-2 (AS): 5′-AACAUCGCCCUGUGGAUGACUdTdT-3′
The following PCR primers were also ordered through IDT:
Human VEGF-A (forward): 5′-AGGAGGGCAGAATCATCACG-3′
Human VEGF-A (reverse): 5′-CAAGGCCCACAGGCATTTTCT-3′
Human Bcl-2 (forward): 5′-TCCCTCGCTGCACAAATACTC-3′
Human Bcl-2 (reverse): 5′-ACGACCCGATGGCCATAGA-3′
Human β-actin (forward): 5′-GGAGATTACTGCCCTGGCTCCTA-3′
Human β-actin (reverse): 5′-GACTCATCGTACTCCTGCTTGCTG-3′
Instrumentation
Proton nuclear magnetic resonance (1H NMR) was conducted on a Bruker Avance II + 500 MHz spectrometer. For polymers, 32 scans were taken using a 10 s relaxation time. Molecular weight distributions (Mn) and polydispersity (Đ = Mw/Mn) were determined by GPC in dimethylformamide (DMF) with 0.01 M LiBr on a Tosoh EcoSEC using PMMA standards. Small molecules were characterized via NMR and electrospray ionization mass spectrometry on an Agilent 6130 LCMS using methanol as the eluent. DLS measurements were taken on a Wyatt Mobius at a fixed detection angle of 163.5° using 532 nm light. Data were analysed using Dynamics software and plotted using GraphPad Prism 9. MALS measurements were taken on a Wyatt DAWN HELEOS II MALS detector with a 658 nm light source using 1× PBS as the eluent. UV–Vis spectroscopy was conducted on a Shimadzu UV-3600 Plus UV-VIS-NIR, scanning from 450 to 200 nm wavelength. TEM was conducted on an FEI Technai G20 F30 with 300 kV acceleration voltage. Images were taken with a digital, CCD camera with 4k × 4k image resolution. Flow cytometry measurements were taken on a Novoctye Penteon 5-30 or BD LSR Fortessa 4-15. Data were analysed using BD FlowJo and plotted in GraphPad Prism 10. Fluorescence microscopy was conducted on a Leica Microsystems microscope equipped with 96-well plate holder.
Polymer syntheses
All BCPs were synthesized using reversible addition fragmentation chain-transfer (RAFT) polymerization, following standard literature protocols. CDT was employed as the initial chain transfer agent (CTA) for the parent polymer, which was then used for sequential chain extensions. Crude and purified materials were characterized by NMR throughout the synthetic steps and GPC was used to determine molecular weight of purified polymers. All degrees of polymerization are based on NMR measurements.
pDEGEA macro-CTA synthesis
In a 25 ml, three-neck flask, 3.33 g DEGEA monomer (18 mmol, 2 M in solution) and 26 mg CDT were dissolved in 8.6 ml DMF. AIBN was added as a stock solution of 1.3 mg in 50 µl DMF. The solution was degassed with four freeze–pump–thaw cycles and placed in a 70 °C oil bath for 1.8 h under nitrogen flow to attain ~60% conversion of monomer. This was done to maintain polymer chain-end livingness84. The solution was quenched by immersion in liquid nitrogen and opening to air. DMF was removed via a rotary evaporator and the crude mixture was reconstituted in minimal THF and precipitated into hexanes (×6). The resulting polymer was dried overnight and obtained as a yellow, viscous oil (yield: 99%). This was used as the ‘parent polymer’ (RAFT macro-CTA) for all BCP constructs.
pDEGEA-b–pHEA
First, 1.4 g pDEGEA macro-CTA and 770 mg HEA monomer (6.67 mmol, 0.6 M in solution) were dissolved in 9 ml DMF. Then 1 mg of AIBN was added and the solution was degassed and placed in a 70 °C oil bath for 3.75 h to achieve ~60% monomer conversion. The solution was diluted and dialysed extensively against water for 48 h with repeated buffer changes. pDEGEA-b-pHEA was lyophilized and obtained as a yellow, sticky solid (yield: 93%).
pDEGEA-b–pTMAEA
First, 670 mg pDEGEA macro-CTA and 290 mg DMAEA monomer (2 mmol, 0.6 M in solution) were dissolved in 2.4 ml 1,4 dioxane. Then 0.4 mg AIBN was added as a stock solution and the solution was degassed and placed in a 70 °C oil bath for 1.5 h. Owing to the slower kinetics of the polymerization and relatively short target block length (~25 units) for DMAEA, the monomer amount was adjusted to achieve the desired degree of polymerization at 20% conversion. Upon quenching, a small portion was precipitated in hexanes for GPC and NMR analysis of the resulting BCP, pDEGEA–pDMAEA. The remainder of the crude mixture was diluted with THF to a concentration of 2 wt% polymer, and 500 µl of iodomethane (8 mmol) was added via positive pressure pipette. The reaction was run overnight at room temperature, dried via rotary evaporator and the crude mixture was reconstituted in DMF for end-group modification.
Mannose acrylate synthesis
Acrylate-modified mannose was synthesized using a modified protocol for the acetal exchange at the C1 position of mannose26. First, 2 g mannose was dissolved in 1 ml water and added to 12 g of HEA. Then 500 µl acetyl chloride was added to the reaction at 0 °C, which was then placed in a 70 °C oil bath for 4 h. The reaction was monitored with thin-layer chromatography using p-anisaldehyde and potassium permanganate stains. The crude mixture was adsorbed onto silica and purified by flash column chromatography using 20% MeOH in DCM as the eluent. The purified material was characterized by 1H NMR and electrospray ionization mass spectrometry. [M+Na]+theoretical = m/z 301.1, [M+Na]+found = m/z 301.25, 10% yield. The acrylate was stored as a stock solution in DMF with 0.5 wt% MEHQ to prevent polymerization.
Polymer chain-end modification
All polymers were modified via aminolysis of the trithiocarbonate chain-end followed by thia-Michael addition of acrylate-functionalized moieties, using previously published techniques25,85. Reactions were carried out by dissolving 50 mg ml−1 polymer in DMF, 20× molar excess acrylate and 5× molar excess TEA (relative to RAFT chain end). Reaction mixtures were degassed by four freeze–pump–thaw cycles and 5× molar excess hexylamine was added under nitrogen as a stock solution in DMF after the first cycle. Reactions were run overnight, and UV–Vis was used to determine full cleavage of the polymers before workup (based on the loss of RAFT chain-end absorbance at 308 nm). The resulting polymers were obtained by 2× precipitation in a 1:1 mixture of ether/hexanes, followed by extensive dialysis against water. All purified polymers were then characterized with NMR, GPC and two colorimetric assays: Ellman’s assay was used for all formulations to ensure no residual free thiols and successful mannosylation is determined by the phenol-H2SO4 assay27,28. For pDEGEA-b–pHEA, the chain end was cleaved and functionalized using either HEA monomer (final material referred to as ‘D130–H70’) or mannose acrylate (‘D130–H70-Mann’). Both materials appear as a white, sticky solid after lyophilization. Yield: 93% (mannose modified), 95% (HEA modified). For pDEGEA-b–pTMAEA, the chain end was cleaved and reacted with residual, unreacted TMAEA monomer remaining (~30× excess relative to chain end) from the crude mixture. The material is a white, fluffy solid after lyophilization and referred to hereafter as ‘D130-TM25’. Yield: 50%.
PS formation and loading efficiency for proteins and nucleic acids
BCP stock solutions were prepared by dissolving at 200 mg ml−1 in PBS overnight and stored at 4 °C. All stock solutions are used within 1 month to avoid appreciable hydrolysis of the acrylate backbone. The thermal transition of materials was determined by preparing a 1 wt% solution of polymer in PBS and then placing in a quartz cuvette for DLS measurement. The instrument was cooled to 4 °C with a constant flow of nitrogen to prevent condensation. Once cooled, the solution was warmed to 37 °C with a slow heating rate of 0.1 °C min−1 and light scattering measurements taken every 3 min. For determining particle size and morphology, the stock solutions were diluted 1:1 in cold PBS (~20–50 µl) and left at room temperature for 5 min to ensure warming and complete self-assembly. For DLS, particles were further diluted to 0.01 wt% in 0.22 µm filtered PBS and analysed as the average of three sets of five scans, each with a 3 s relaxation time. Particle hydrodynamic radius (RH) was determined using the Stokes–Einstein equation. MALS measurements were conducted by further diluting the same samples to 0.01 mg ml−1 in PBS. Scattering intensity (as Rθ/Kc) was plotted as a function of angle (sin2(θ/2)) and analysed using a Rayleigh–Gans approximation for spherical particles86. The radius of gyration (RG) was obtained for polymer nanoparticles and compared against the RH from DLS to ascertain vesicular structure. For TEM, samples were diluted to 1 mg ml−1, dropped on 200 (lines per inch) mesh copper grids and rinsed with deionized water. Grids were then stained with uranyl acetate and dried overnight before imaging. Loading efficiencies of protein and nucleic acids were measured using gel electrophoresis with non-reducing, detergent-free buffers. For protein loading, a stock solution of OVA in cold PBS was mixed 1:1 with BCP stock to provide a solution of 10:1 polymer:payload (wt/wt). The nanoparticles were formed at room temperature for 15 min, diluted and then run on a 4–20% gradient, stain-free polyacrylamide gel (Bio-Rad) using Tris–glycine running buffer. The gels were removed, activated with UV and analysed using Bio-Rad ImageLab. For nucleic acid loading, stock solutions in nuclease-free water are diluted to 300 ng polymer with 30 ng FAM-siRNA (Thermo Fisher, Silencer Select). After room temperature assembly for 15 min, samples were diluted with loading dye and run on a 15% polyacrylamide gel using TBE buffer to prevent RNA degradation. Gels were analysed using the fluorescein channel as well as staining with SYBR Safe nucleic acid dye on ImageLab. To determine the loading efficiency for materials reconstituted from dry formulations, BCPs were mixed with either OVA or FAM-siRNA as above, then lyophilized before gel electrophoresis. Once fully dried, polymer/payload powder was resuspended with cold, nuclease-free water to similar concentrations as before drying. Solutions were then allowed to warm to room temperature, followed by similar conditions for gel electrophoresis as above.
OVA cellular uptake, antigen processing and presentation in vitro
For protein uptake studies, FITC-OVA was encapsulated following the above procedures in nanoparticles at 20:1 (polymer/payload, wt/wt) using 100 mg ml−1 of polymer. Nanoparticles were then diluted to 50–100 µg ml−1 in serum-free, RPMI-1640 media (Gibco) before treatment. BMDCs were then plated at 100,000 cells per well in 96-well U-bottom plates and treated with nanoparticle formulations for 30 min. Cells were then washed with PBS and incubated in complete Lutz media for 2 h (ref. 87). Cells were then stained for viability and fixed with 2% paraformaldehyde before flow cytometry. For mannose-receptor blocking, 50 µg ml−1 of mannose blocking peptide (LSBio, LS-E4304-500) was prepared in serum-free media and BMDCs were treated for 30 min before nanoparticle treatment to ensure binding. For antigen presentation studies, BMDCs were plated at 10,000 cells per well in 96-well U-bottom plates and treated in complete Lutz media containing lipopolysaccharide with formulations for 6 h. OVA-specific T cells (OTs) were isolated from 6–10-week-old male OTI transgenic mice by collecting spleens and magnetically sorting for CD8+ T cells. Then, OTI T cells were CFSE labelled and co-cultured with BMDCs for 3 days in complete IMDM media (Gibco). Cells were then washed, stained for viability and fixed with 2% paraformaldehyde before flow cytometry. Proliferation was demonstrated by a decrease in fluorescence intensity owing to the CFSE stain becoming diluted as T cells divide. To probe antigen processing, RAW 264.7 macrophages were treated with 100 µg ml−1 polymer and 10 µg ml−1 fluorescent OVA. A high concentration of polymer, 100 mg ml−1, encapsulated a mixture of DQ-OVA and OVA647 (1:1 mass ratio) at a total concentration of 10 mg ml−1. The concentrated solution was diluted in complete DMEM and RAW macrophages plated at a concentration of 10k cells per well in a 96-well plate were treated overnight with 100 µl medium. The medium was removed the next day, cells were washed with PBS and then stained with 4,6-diamidino-2-phenylindole (DAPI) (diluted 1:5,000) for 5 min. The cells were washed again, PBS was added and then 96-well plates were imaged on a Leica microscope using the DAPI channel for cell nuclei, the FITC channel for DQ-OVA and the APC channel for OVA647 visualization.
In vitro immune stimulation using NF-kB reporter line
RAW-Blue macrophages were plated at a concentration of 100k cells per well in 96-well plates for overnight incubation with CpG ODN 1826 and polymers. CpG was either delivered free, encapsulated or admixed with polymer formulations. For encapsulated formulations, polymers (10 mg ml−1) were fully dissolved alongside CpG (500 µg ml−1) in cold PBS and then the solution was warmed to room temperature. Admixed formulations had polymers assembled at 100 mg ml−1 and then diluted 100× in 200 µg ml−1 CpG. All formulations were then diluted to equivalent concentrations of CpG in RAW-Blue media and cells were treated with 100 µl of this suspension. NF-kB activation was measured the following day by collecting 20 µl supernatant, mixing with 180 µl QUANTI-Blue solution (Invivogen) and measuring the OD650 with a plate reader.
Biodistribution upon hock and i.v. injection using IVIS
First, 5 µg of fluorescent OVA-647 was encapsulated in PSs (100 µg) as above or delivered unencapsulated in 100 µl saline into all four hocks (intradermal) of healthy C57BL/6 (Charles River, 6-week-old male mice (n = 2). For tail vein i.v. injections, encapsulated OVA-647 was similarly administered (n = 2). For lymph node collection, animals were killed after 4 h for the collection of all four pairs of hock-draining lymph nodes: axillary, brachial, inguinal and popliteal. Lymph nodes were immediately stored in PBS and then arranged onto a black background for imaging on an in vivo imaging system (IVIS) Spectrum (Perkin Elmer) for OVA fluorescence. For i.v. administration, livers were collected after 3 h and OVA fluorescence quantified using an IVIS Spectrum. For tumour distribution, subcutaneous (rear flank, the same side as the tumour) and tail vein injections were similarly conducted in MCF-7 tumour-bearing nude mice (Jackson Laboratory, n = 2 or 1 if untreated), using fluorescently labelled (AF647) polymer. Liver, spleen, heart, lungs, thymus, kidney, pancreas and tumour were collected at 3 h post i.v. and 24 h post subcutaneous injection and polymer fluorescence visualized on an IVIS Spectrum.
OVA subunit vaccination
Six-week-old, female, C57BL/6 (Charles River) mice were vaccinated intradermally in all four hocks with 100 µl of nanoparticle formulations. Besides the saline treatment, all mice were treated with 10 µg OVA adjuvanted with 20 µg CpG ODN 1826, which was admixed post-encapsulation (Invivogen). OVA was first encapsulated into the PSs at high concentration (100 mg ml−1 polymer, 10 mg ml−1 protein) in PBS, then diluted 100× into sterile saline containing 200 µg ml−1 CpG. Then 100 µg polymer was delivered for nanoparticle treatments. Blood was drawn weekly via submandibular bleeding and sera were collected and stored at −20 °C. All mice were boosted on day 21 following prime vaccination and killed at day 28. dLNs and spleens were collected for analysing the OVA-specific T cell response using fluorescent probes and restimulation. After collection, dLNs were treated with collagenase IV and D for 30 min at 37 °C and passed through a 70 µm filter with complete IMDM media. Spleens were passed through a 70 µm filter, treated with ACK lysis buffer (Thermo Fisher) for 5 min and then quenched with complete IMDM. Single-cell suspensions were counted and all samples were brought to a concentration of 20 million cells per millilitre in complete IMDM. For MHC-I/SIINFEKL tetramer (National Institutes of Health, APC-labelled) staining, isolated cells were plated at 1 million cells per well, stained following literature protocols and analysed with flow cytometry (LSR Fortessa)88. Briefly, lymphocytes were plated on 96-well U-bottom plates, washed with PBS and stained for viability. To prevent membrane turnover of the T cell receptor, cells were then treated with 50 nM of dasatinib for 30 min at 37 °C, washed and then stained with tetramer for 15 min at room temperature. All other surface stains were done after, along with cell fixation following standard literature procedures. Tetramer+CD8+ T cells were identified on bulk (all live, TCRb+CD8+ cells) and antigen-experienced CD44+CD8+ T cells. The 6 h restimulation experiments were conducted by plating 2 million cells per well, followed by the addition of 100 µl complete IMDM containing either saline (‘unstimulated’ condition), SIINFEKL peptide (Invivogen, 1 µg ml−1, ‘CD8-stimulated’ condition) or a high concentration of endotoxin-free OVA (1 mg ml−1, ‘CD4-stimulated’ condition). Pooled samples stimulated with PMA/Ionomycin were used as a positive control. After 6 h, cells were isolated, stained for viability, surface markers (CD4 and CD8), and intracellular cytokines and markers (IFNγ, TNF, IL-2 and CD3ε) following standard protocols. Cells were then analysed by flow cytometry (LSR Fortessa). The 6 h restimulation studies are plotted as stimulated minus unstimulated response. For whole-protein restimulation studies, 500,000 cells per well were plated in 96-well U-bottom plates and stimulated with IMDM containing 100 µg ml−1 OVA. Cells were centrifuged after 3 days and media were collected for cytokine analysis using Legendplex (Murine Th 12-plex, Biolegend) following the manufacturer’s protocol (Novocyte Penteon flow cytometer). Serum antibodies (total IgG) were detected using a direct enzyme-linked immunosorbent assay (ELISA) on Corning 9018 plates coated overnight with 10 µg ml−1 OVA in carbonate/bicarbonate buffer (pH 9.8). Sera were diluted in 1× casein buffer as tenfold serial dilutions (1:102–107), incubated on coated plates and standard ELISA procedures were followed. Absorbance was read at 450 nm (characteristic for TMB buffer) and 570 nm (background) on a plate reader. Total IgG was reported as the AUC for the absorbance (A450–A570) versus the dilution curve of sera taken at 2 and 4 weeks. It should be noted that panels in the figures represent separate ELISAs, so AUC values can only be compared within one panel (that is, between treatment groups), and not between panels (that is, Fig. 3c,d are not comparable to each other).
OVA prophylactic inverse vaccination
In a murine prophylactic allergy model, nanoparticles (either with or without protein antigen, OVA) were administered intravenously weekly for 2 weeks. At 1 week post therapy, mice were sensitized using OVA mixed in a 1:1 (v/v) ratio with Imject Alum solution (Thermo Fisher Scientific). Mice were sensitized through two i.p. injections set 1 week apart with 100 μg of alum/OVA. A week after the second sensitization, mice were challenged for four consecutive days with 25 μg of OVA grade V in PBS through i.tr. instillations. The submandibular vein was sampled through lancet puncture, and blood plasma was isolated through centrifugation at 20,000g in a tabletop centrifuge. Mice were euthanized 3 days after the last challenge to assess the extent of allergic airway inflammation. BALF was isolated by cannulating the trachea and washing the lungs with PBS for a total recovery of 3 ml. Perfused mouse lungs were mechanically dissociated and digested with Collagenase IV and Collagenase D in 3 ml DMEM for 1 h. After red blood cell lysis, samples were then washed, filtered and counted before flow cytometry analysis. For immunophenotyping, 5 × 105 cells were suspended in 50 μl buffer (PBS, 2% FBS), blocked using anti-CD16/32, and stained with surface antibodies. For intracellular staining, cells were fixed and permeabilized with the FoxP3/Transcription Factor Staining Buffer Set (Invitrogen) following the manufacturer’s instructions. Samples were analysed using an LSR Fortessa (BD Biosciences) or Cytek Aurora (Cytek Biosciences) and the data analysed using FlowJo software. To determine total IgE levels in the plasma, we utilized an anti-IgE ELISA (Thermo Fisher Scientific) following the manufacturer’s instructions.
siRNA-mediated gene knockdown in vitro and in vivo
MCF-7 cells, a human breast cancer line, were plated at 5 × 104 cells per well in a 48-well plate and incubated for 24 h. Cell media were removed and the cells were washed using PBS. Various doses of siRNA (VEGF-A or Bcl-2 targeted siRNA, purchased through IDT, sequences listed above) and polymer or Lipo (Thermo Fisher Scientific) complex were suspended in RPMI media with 2% FBS and cells were treated for 6 h. Then, the cells were washed using PBS and incubated with complete media for 48 h. After incubation, the cells were collected for RNA isolation (RNEasy Mini kit, Qiagen) following the manufacturer’s protocols, and target mRNA expression was evaluated using standard RT–PCR techniques with commercially available primers for human VEGF-A and Bcl-2 (IDT, sequences above). cDNA (Superscript III, Invivogen) was synthesized using the manufacturer’s protocols and PCR was conducted using an annealing temperature of 5 °C below the melting temperature for primers (usually ~55 °C) and run for 26 amplification cycles to prevent signal saturation.
For in vivo measurements, nude mice were inoculated with 2 million MCF-7 cancer cells in a Matrigel extracellular matrix. Tumours were allowed to grow for 10 days to a size of 50–70 mm3 before starting intratumoural treatment of siVEGF-A and siBcl-2 on days 11 and 13. Mice were killed at day 14, and tumours were collected and stored at −80 °C. For measuring mRNA knockdown, RT–PCR protocols were used as outlined above, after tumours were sectioned. Roughly 20% of tumour was excised, while the rest remained frozen. For measuring protein, similarly sized tumour sections were taken from siRNA-treated animals and protein was extracted using RIPA buffer containing protease inhibitors (Pierce, Invivogen) with light sonication for western blot. The total protein concentration was measured using a BCA assay, and equivalent amounts of protein (50 µg) were loaded onto a 4–20% PAGE gel under reducing, detergent-containing conditions (TGS buffer, 6× reducing loading dye). The separated protein was electrophoretically transferred onto a PVDF membrane and then blocked with 5% skim milk in PBS with 0.1% Tween20 (PBS-T) for 1 h at room temperature. Subsequent staining was done with rabbit antibodies in 2% milk (in PBS-T) against human VEGF-A (E9X8Q, diluted 1:1,000), Bcl-2 (D17C4, diluted 1:1,000) and GAPDH (D16H11, diluted 1:10,000, loading control) overnight at 4 °C, washed with PBS-T and then stained with secondary antibody–HRP conjugate for 1 h at room temperature. Blots were washed and imaged using a Bio-Rad blot chemiluminescence imager following treatment with western blot substrate (Bio-Rad).
siRNA cancer therapy
For in vivo cancer studies probing RNAi of VEGF-A and Bcl-2, nude mice were inoculated subcutaneously behind the shoulder with 2 million MCF-7 cancer cells (cultured in DMEM media) in a Matrigel extracellular matrix. Tumours were allowed to grow for 10 days to a size of 50–70 mm3 before starting treatment. Then, mice were treated i.t. on days 11, 13, 15, 17 and 19 using nanoparticle-encapsulated or free siRNA (either siVEGF-A or siBcl-2) formulations and 40 µg of siRNA and 200 µg of polymer were administered. Tumour sizes were measured until day 35, and mice were killed when tumours reached a size of 600 mm3. For LNP benchmarking studies, 20 µg of siRNA was used with 100 µg of either polymer or LNP formulation. Mice were treated every 5 days starting at day 11 and killed when tumours grew to 600 mm3.
LNP formulation for in vivo cancer therapy
To serve as an in vivo control for siRNA delivery, we formulated LNPs to mimic those of Onpattro (Alnylam Pharmaceuticals), following published structures and weight ratios of the relevant components6,89. Stock solutions of DLin-MC3-DMA, DSPC, cholesterol and PEG2k-DMG (Broadpharm) were prepared in ethanol at concentrations of 157, 15.7, 30.4 and 4.72 mM respectively. When ready for use, stock solutions were mixed at a volumetric ratio of 5:10:15:5, to give the prescribed molar ratio of 50:10:38.5:1.5 (ionizable lipid:cationic lipid:cholesterol:PEG-lipid). Since the LNPs are only needed in small batches, dilution and rapid vortexing was chosen as our method for encapsulating RNA72. LNPs were formed by diluting the EtOH-mixed stock solution 1:15 in nuclease-free water (either with or without RNA) under vortexing. For loading efficiency quantification, LNPs are diluted to identical mass concentration with FAM-siRNA as for polymers. Size, reproducibility and loading efficiency was then quantified with similar analytical techniques as above (Supplementary Fig. 17).
Statistics and reproducibility
All statistical analyses were conducted using GraphPad Prism 10. In vitro and in vivo statistics were based on one-way or two-way (when appropriate) analysis of variance (ANOVA) comparisons or Kruskal–Wallis tests for non-parametric data. Welch’s ANOVA was used when assumptions could not be made regarding standard deviations of samples. All comparisons are shown in the figures and multiple comparisons are corrected for using post tests as described in the figures. Exact P values are denoted in the figures and may also appear as follows: *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001. Survival analyses in Fig. 6 were determined using a log-rank Mantel–Cox test separately conducted for the denoted comparisons.
All in vivo experiments were repeated two to three times, and in vitro experiments were repeated three times with similar results. Datasets were never pooled together. Micrographs for TEM (Fig. 2e) and fluorescence microscopy (Supplementary Fig. 9) are representative of overall populations and experiments were conducted a minimum of three times with three different locations for a given sample being imaged. Gel electrophoresis for loading (as in Fig. 2g and Supplementary Fig. 17b) was done for all nanoparticle characterization studies as well in vitro and in vivo experiments, and was therefore conducted a minimum of ten times for both protein and siRNA with similar results.
Animal experimentation ethics
All the animal experiments performed in this research were approved by the University of Chicago IACUC under protocols 72456 and 72470.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data that support the results of this study are available within the article and its Supplementary Information. Source data are provided with this paper. These data are also available on figshare at https://doi.org/10.6084/m9.figshare.28857794 (ref. 90). Any other datasets generated and analysed during the study are available from the corresponding authors upon request.
References
Mitchell, M. J. et al. Engineering precision nanoparticles for drug delivery. Nat. Rev. Drug Discov. https://doi.org/10.1038/s41573-020-0090-8 (2020).
Serra, P. & Santamaria, P. Antigen-specific therapeutic approaches for autoimmunity. Nat. Biotechnol. 37, 238–251 (2019).
Sioud, M. Releasing the immune system brakes using siRNAs enhances cancer immunotherapy. Cancers 11, 176 (2019).
Morrison, C. Alnylam prepares to land first RNAi drug approval. Nat. Rev. Drug Discov. 17, 156–157 (2018).
Shae, D., Postma, A. & Wilson, J. T. Vaccine delivery: where polymer chemistry meets immunology. Ther. Deliv. 7, 193–196 (2016).
Suzuki, Y. & Ishihara, H. Difference in the lipid nanoparticle technology employed in three approved siRNA (Patisiran) and mRNA (COVID-19 vaccine) drugs. Drug Metab. Pharmacokinet. 41, 100424 (2021).
Discher, D. E. & Eisenberg, A. Polymer vesicles. Science 297, 967–973 (2002).
Aibani, N., Khan, T. N. & Callan, B. Liposome mimicking polymersomes; a comparative study of the merits of polymersomes in terms of formulation and stability. Int. J. Pharm. X 2, 100040 (2020).
Mai, Y. & Eisenberg, A. Self-assembly of block copolymers. Chem. Soc. Rev. 41, 5969 (2012).
Scott, E. A. et al. Dendritic cell activation and T cell priming with adjuvant- and antigen-loaded oxidation-sensitive polymersomes. Biomaterials 33, 6211–6219 (2012).
Bartenstein, J. E., Robertson, J., Battaglia, G. & Briscoe, W. H. Stability of polymersomes prepared by size exclusion chromatography and extrusion. Colloids Surf. A 506, 739–746 (2016).
Fielden, S. D. P. Kinetically controlled and nonequilibrium assembly of block copolymers in solution. J. Am. Chem. Soc. 146, 18781–18796 (2024).
Rideau, E., Dimova, R., Schwille, P., Wurm, F. R. & Landfester, K. Liposomes and polymersomes: a comparative review towards cell mimicking. Chem. Soc. Rev. 47, 8572–8610 (2018).
Allen, S., Osorio, O., Liu, Y.-G. & Scott, E. Facile assembly and loading of theranostic polymersomes via multi-impingement flash nanoprecipitation. J. Control. Release 262, 91–103 (2017).
Martin, A., Lalanne, P., Weber-Vax, A., Mutschler, A. & Lecommandoux, S. Controlling polymersome size through microfluidic-assisted self-assembly: enabling ‘ready to use’ formulations for biological applications. Int. J. Pharm. 642, 123157 (2023).
Shepherd, S. J. et al. Throughput-scalable manufacturing of SARS-CoV-2 mRNA lipid nanoparticle vaccines. Proc. Natl Acad. Sci. USA 120, e2303567120 (2023).
Pasparakis, G. & Tsitsilianis, C. LCST polymers: thermoresponsive nanostructured assemblies towards bioapplications. Polymer 211, 123146 (2020).
Vancoillie, G. et al. Understanding the effect of monomer structure of oligoethylene glycol acrylate copolymers on their thermoresponsive behavior for the development of polymeric sensors. Polym. Chem. 10, 5778–5789 (2019).
De, P. & Sumerlin, B. S. Precision control of temperature response by copolymerization of di(ethylene glycol) acrylate and an acrylamide comonomer. Macromol. Chem. Phys. 214, 272–279 (2013).
Haley, R. M. et al. Lipid nanoparticle delivery of small proteins for potent in vivo RAS inhibition. ACS Appl. Mater. Interfaces https://doi.org/10.1021/acsami.3c01501 (2023).
Lutz, J.-F. Polymerization of oligo(ethylene glycol) (meth)acrylates: toward new generations of smart biocompatible materials. J. Polym. Sci. A 46, 3459–3470 (2008).
Agarwal, A., Bobay, B. G. & Becker, M. L. Observation of dynamic aggregation behavior in thermoresponsive micro- and nanoparticles via diffusion-ordered NMR spectroscopy. J. Am. Chem. Soc. 147, 9386–9395 (2025).
Ozer, I. et al. Polyethylene glycol-like brush polymer conjugate of a protein drug does not induce an antipolymer immune response and has enhanced pharmacokinetics than its polyethylene glycol counterpart. Adv. Sci. 9, e2103672 (2022).
Luo, L. & Eisenberg, A. One-step preparation of block copolymer vesicles with preferentially segregated acidic and basic corona chains. Angew. Chem. Int. Ed. 41, 1001–1004 (2002).
Qiu, X.-P. & Winnik, F. M. Facile and efficient one-pot transformation of RAFT polymer end groups via a mild aminolysis/Michael addition sequence. Macromol. Rapid Commun. 27, 1648–1653 (2006).
Wilson, D. S. et al. Antigens reversibly conjugated to a polymeric glyco-adjuvant induce protective humoral and cellular immunity. Nat. Mater. 18, 175–185 (2019).
Moser, M. et al. Ellman’s and aldrithiol assay as versatile and complementary tools for the quantification of thiol groups and ligands on nanomaterials. Anal. Chem. 88, 8624–8631 (2016).
Masuko, T. et al. Carbohydrate analysis by a phenol–sulfuric acid method in microplate format. Anal. Biochem. 339, 69–72 (2005).
Skandalis, A. & Pispas, S. PDMAEMA-b-PLMA-b-POEGMA triblock terpolymers via RAFT polymerization and their self-assembly in aqueous solutions. Polym. Chem. 8, 4538–4547 (2017).
Zhang, Y. et al. Possibility for double optimization of siRNA intracellular delivery efficiency and antibacterial activity: structure screening of pH-sensitive triblock amphiphilic polycation micelles. Colloids Surf. B 209, 112178 (2022).
Zhu, L., Powell, S. & Boyes, S. G. Synthesis of tertiary amine-based pH-responsive polymers by RAFT polymerization. J. Polym. Sci. A 53, 1010–1022 (2015).
Ratcliffe, L. P. D., Derry, M. J., Ianiro, A., Tuinier, R. & Armes, S. P. A single thermoresponsive diblock copolymer can form spheres, worms or vesicles in aqueous solution. Angew. Chem. Int. Ed. 58, 18964–18970 (2019).
Battaglia, G. & Ryan, A. J. The evolution of vesicles from bulk lamellar gels. Nat. Mater. 4, 869–876 (2005).
Cho, W.-S. et al. Zeta potential and solubility to toxic ions as mechanisms of lung inflammation caused by metal/metal oxide nanoparticles. Toxicol. Sci. 126, 469–477 (2012).
Patterson, J. P., Robin, M. P., Chassenieux, C., Colombani, O. & O’Reilly, R. K. The analysis of solution self-assembled polymeric nanomaterials. Chem. Soc. Rev. 43, 2412–2425 (2014).
Kozlovskaya, V. et al. Temperature-responsive polymersomes of poly(3-methyl-N-vinylcaprolactam)-block-poly(N -vinylpyrrolidone) to decrease doxorubicin-induced cardiotoxicity. Biomacromolecules 20, 3989–4000 (2019).
Du, J., Tang, Y., Lewis, A. L. & Armes, S. P. pH-Sensitive vesicles based on a biocompatible zwitterionic diblock copolymer. J. Am. Chem. Soc. 127, 17982–17983 (2005).
Saunders, C., De Villiers, C. A. & Stevens, M. M. Single particle chemical characterisation of nanoformulations for cargo delivery. AAPS J. 25, 94 (2023).
Wang, F., Harker, A., Edirisinghe, M. & Parhizkar, M. Micro‐ and nanomanufacturing for biomedical applications and nanomedicine: a perspective. Small Sci. 3, 2300039 (2023).
O’Neil, C. P., Suzuki, T., Demurtas, D., Finka, A. & Hubbell, J. A. A novel method for the encapsulation of biomolecules into polymersomes via direct hydration. Langmuir 25, 9025–9029 (2009).
Hong, S. et al. Protein-based nanoparticles as drug delivery systems. Pharmaceutics 12, 604 (2020).
Nam, J., Son, S., Park, K. S. & Moon, J. J. Modularly programmable nanoparticle vaccine based on polyethyleneimine for personalized cancer immunotherapy. Adv. Sci. 8, 2002577 (2021).
Hochreiner, E. G. & Van Ravensteijn, B. G. P. Polymerization‐induced self‐assembly for drug delivery: a critical appraisal. J. Polym. Sci. https://doi.org/10.1002/pol.20230579 (2023).
Wong, C. K., Lai, R. Y. & Stenzel, M. H. Dynamic metastable polymersomes enable continuous flow manufacturing. Nat. Commun 14, 6237 (2023).
Matoori, S. & Leroux, J.-C. Twenty-five years of polymersomes: lost in translation? Mater. Horiz. 7, 1297–1309 (2020).
Elias, D. R., Poloukhtine, A., Popik, V. & Tsourkas, A. Effect of ligand density, receptor density, and nanoparticle size on cell targeting. Nanomed. Nanotechnol. Biol. Med. 9, 194–201 (2013).
Sauer, K. & Harris, T. An effective COVID-19 vaccine needs to engage T cells. Front. Immunol. 11, 581807 (2020).
Dong, H., Pang, L., Cong, H., Shen, Y. & Yu, B. Application and design of esterase-responsive nanoparticles for cancer therapy. Drug Deliv. 26, 416–432 (2019).
Bikorimana, J.-P. et al. Promoting antigen escape from dendritic cell endosomes potentiates anti-tumoral immunity. Cell Rep. Med. 3, 100534 (2022).
Bode, C., Zhao, G., Steinhagen, F., Kinjo, T. & Klinman, D. M. CpG DNA as a vaccine adjuvant. Expert Rev. Vaccines 10, 499–511 (2011).
Schmidt, M. E. & Varga, S. M. The CD8 T cell response to respiratory virus infections. Front. Immunol. 9, 678 (2018).
Moon, J. J. et al. Interbilayer-crosslinked multilamellar vesicles as synthetic vaccines for potent humoral and cellular immune responses. Nat. Mater. 10, 243–251 (2011).
Carson, C. S. et al. A nanovaccine for enhancing cellular immunity via cytosolic co-delivery of antigen and polyIC RNA. J. Control. Release 345, 354–370 (2022).
Stano, A., Scott, E. A., Dane, K. Y., Swartz, M. A. & Hubbell, J. A. Tunable T cell immunity towards a protein antigen using polymersomes vs. solid-core nanoparticles. Biomaterials 34, 4339–4346 (2013).
Chou, P.-Y. et al. Glycosylation of OVA antigen-loaded PLGA nanoparticles enhances DC-targeting for cancer vaccination. J. Control. Release 351, 970–988 (2022).
Ballas, Z. K. et al. Divergent therapeutic and immunologic effects of oligodeoxynucleotides with distinct CpG motifs. J. Immunol. 167, 4878–4886 (2001).
Volpatti, L. R. et al. Polymersomes decorated with the SARS-CoV-2 spike protein receptor-binding domain elicit robust humoral and cellular immunity. ACS Cent. Sci. 7, 1368–1380 (2021).
Nials, A. T. & Uddin, S. Mouse models of allergic asthma: acute and chronic allergen challenge. Dis. Model. Mech. 1, 213–220 (2008).
Hammad, H. & Lambrecht, B. N. The basic immunology of asthma. Cell 184, 1469–1485 (2021).
Cao, S. et al. Glycosylation-modified antigens as a tolerance-inducing vaccine platform prevent anaphylaxis in a pre-clinical model of food allergy. Cell Rep. Med. https://doi.org/10.1016/j.xcrm.2023.101346 (2023).
Ahmad, H. I. et al. Immune tolerance vs. immune resistance: the interaction between host and pathogens in infectious diseases. Front. Vet. Sci. 9, 827407 (2022).
Horst, A. K., Neumann, K., Diehl, L. & Tiegs, G. Modulation of liver tolerance by conventional and nonconventional antigen-presenting cells and regulatory immune cells. Cell. Mol. Immunol. 13, 277–292 (2016).
Charbe, N. B. et al. Small interfering RNA for cancer treatment: overcoming hurdles in delivery. Acta Pharm. Sin. B 10, 2075–2109 (2020).
Nam, J. et al. Cancer nanomedicine for combination cancer immunotherapy. Nat. Rev. Mater. 4, 398–414 (2019).
Guo, P. et al. Overexpression of vascular endothelial growth factor by MCF-7 breast cancer cells promotes estrogen-independent tumor growth in vivo. Cancer Res. 63, 4684–4691 (2003).
Ge, Y.-L., Zhang, X., Zhang, J.-Y., Hou, L. & Tian, R.-H. The mechanisms on apoptosis by inhibiting VEGF expression in human breast cancer cells. Int. Immunopharmacol. 9, 389–395 (2009).
Goel, H. L. & Mercurio, A. M. VEGF targets the tumour cell. Nat. Rev. Cancer 13, 871–882 (2013).
Oh, S. et al. Downregulation of autophagy by Bcl-2 promotes MCF7 breast cancer cell growth independent of its inhibition of apoptosis. Cell Death Differ. 18, 452–464 (2011).
Liang, Y., Brekken, R. A. & Hyder, S. M. Vascular endothelial growth factor induces proliferation of breast cancer cells and inhibits the anti-proliferative activity of anti-hormones. Endocr. Relat. Cancer 13, 905–919 (2006).
Dalby, B. et al. Advanced transfection with Lipofectamine 2000 reagent: primary neurons, siRNA, and high-throughput applications. Methods 33, 95–103 (2004).
Zhang, X. et al. Patisiran pharmacokinetics, pharmacodynamics, and exposure‐response analyses in the phase 3 APOLLO trial in patients with hereditary transthyretin‐mediated (hATTR) amyloidosis. J. Clin. Pharmacol. 60, 37–49 (2020).
Wang, X. et al. Preparation of selective organ-targeting (SORT) lipid nanoparticles (LNPs) using multiple technical methods for tissue-specific mRNA delivery. Nat. Protoc. 18, 265–291 (2023).
Yu, L. X. et al. Understanding pharmaceutical quality by design. AAPS J. 16, 771–783 (2014).
Gray, L. T. et al. Generation of potent cellular and humoral immunity against SARS-CoV-2 antigens via conjugation to a polymeric glyco-adjuvant. Biomaterials 278, 121159 (2021).
Schwarz, B. et al. Viruslike particles encapsidating respiratory syncytial virus M and M2 proteins induce robust T cell responses. ACS Biomater. Sci. Eng. 2, 2324–2332 (2016).
Etz, H. et al. Identification of in vivo expressed vaccine candidate antigens from Staphylococcus aureus. Proc. Natl Acad. Sci. USA 99, 6573–6578 (2002).
Inam, A. et al. Vaccine hesitancy and post-vaccination adherence to safety measures: a mixed-method study. Front. Public Health 11, 1072740 (2023).
Tremain, A. C. et al. Synthetically glycosylated antigens for the antigen-specific suppression of established immune responses. Nat. Biomed. Eng. 7, 1142–1155 (2023).
Wilson, D. S. et al. Synthetically glycosylated antigens induce antigen-specific tolerance and prevent the onset of diabetes. Nat. Biomed. Eng. 3, 817–829 (2019).
Wallace, R. P. et al. Synthetically mannosylated antigens induce antigen-specific humoral tolerance and reduce anti-drug antibody responses to immunogenic biologics. Cell Rep. Med. 5, 101345 (2024).
Gómez Medellín, J. E. et al. Liver-targeted allergen immunotherapy rapidly and safely induces antigen-specific tolerance to treat allergic airway disease in mice. Sci. Transl. Med. 17, eadl0406 (2025).
Yap, T. A. et al. Development of immunotherapy combination strategies in cancer. Cancer Discov. 11, 1368–1397 (2021).
Coca, S., Jasieczek, C. B., Beers, K. L. & Matyjaszewski, K. Polymerization of acrylates by atom transfer radical polymerization. Homopolymerization of 2-hydroxyethyl acrylate. J. Polym. Sci. A 36, 1417–1424 (1998).
Perrier, S. 50th anniversary perspective: RAFT polymerization—a user guide. Macromolecules 50, 7433–7447 (2017).
Boyer, C., Granville, A., Davis, T. P. & Bulmus, V. Modification of RAFT-polymers via thiol-ene reactions: a general route to functional polymers and new architectures. J. Polym. Sci. A 47, 3773–3794 (2009).
Wyatt, P. J. Measurement of special nanoparticle structures by light scattering. Anal. Chem. 86, 7171–7183 (2014).
Lutz, M. B. et al. An advanced culture method for generating large quantities of highly pure dendritic cells from mouse bone marrow. J. Immunol. Methods 223, 77–92 (1999).
Dolton, G. et al. More tricks with tetramers: a practical guide to staining T cells with peptide-MHC multimers. Immunology 146, 11–22 (2015).
Schoenmaker, L. et al. mRNA-lipid nanoparticle COVID-19 vaccines: structure and stability. Int. J. Pharm. 601, 120586 (2021).
Hossainy, S. et al. Source data for the figures of the article. figshare https://doi.org/10.6084/m9.figshare.28857794 (2025).
Acknowledgements
We thank A. Esser-Kahn (University of Chicago) and W. Leitner (National Institutes of Health (NIH)/National Institute of Allergy and Infectious Diseases (NIAID)) for helpful discussions regarding subunit vaccination readouts. We also thank P. Griffin (UChicago Soft Matter Characterization Facility), J. Kurutz (NMR Core Facility), J. Souris (iSAIRR Optical Core) and T. Lavoie (Electron Microscopy Facility) and the Antibody and Flow Cytometry Core for instrument assistance and helpful experimental advice. We thank S. Gomes (University of Chicago) for maintaining and providing cell-culture lines while also providing overall support of the work. We thank C. Garza and A. Mukherjee (University of Chicago) for helpful discussions regarding fluorescence microscopy studies. We also acknowledge A. Agarwal (Duke University) for help in figure design and formatting. We also thank N. Stanic (University of Chicago) for assistance in portions of organ processing for the subunit vaccination studies. This work was supported in part by National Institute of Allergy and Infectious Diseases of the NIH under the Discovery of Adjuvant Program: award NIH 75N93019C00041 and the Chicago Immunoengineering Innovation Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
S.J.R. and J.A.H. oversaw all research. S.H., S.K., J.E.G.M., S.J.R. and J.A.H. designed the research strategy. S.H., S.J.R. and J.A.H. conceptualized the polymers. S.H. synthesized and characterized the polymers and nanoparticles. S.H., S.K., J.E.G.M., A.T.A., K.C.R., Y.Y.M., I.V., K.C., T.W. and A.S. performed the experiments. S.H., S.K., J.E.G.M., A.T.A., K.C.R. and Y.Y.M. analysed the experiments. S.H., J.E.G.M., S.R. and J.A.H. wrote the paper. All authors approved the paper.
Corresponding authors
Ethics declarations
Competing interests
S.H., S.K., J.E.G.M., A.T.A., S.J.R. and J.A.H. are inventors on a provisional patent filed by the University of Chicago. The other authors declare no competing interests.
Peer review
Peer review information
Nature Biomedical Engineering thanks Zhiyong Qian, Hangxiang Wang, John Wilson and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Source Data Fig. 1
Source data for all main figures.
Source Data Fig. 2
Figure 2g and Supplementary Figs. 7 and 17 uncropped gels.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hossainy, S., Kang, S., Gómez Medellín, J.E. et al. Thermoreversibly assembled polymersomes for highly efficient loading, processing and delivery of protein and siRNA biologics. Nat. Biomed. Eng (2025). https://doi.org/10.1038/s41551-025-01469-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41551-025-01469-7