Abstract
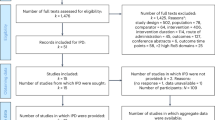
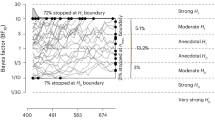
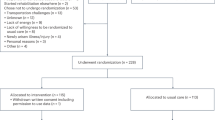
The increasing prevalence of stress underscores the demand for effective, self-administered mobile mental health interventions, yet their efficacy and accessibility are still unclear. Here, this systematic review and meta-analysis aimed to classify self-administered mobile stress management interventions, compare their efficacy and examine their moderators. We searched PsycINFO, PubMed, Web of Science, MEDLINE, Embase, CINAHL, Scopus and PsycARTICLES from database inception to 20 November 2023. Eligible studies were randomized controlled trials on peer-reviewed, Internet-based, self-administered psychological interventions for stress reduction in healthy or subhealthy adults. A total of 63 studies with 20,454 participants were included (68.18% female; mean age 39.14 years). Integrated expert insights with large language models to develop a three-dimensional framework encompassing theoretical foundation, human support and mobile technology. Intervention labels were independently coded by the authors and ChatGPT. The included studies’ quality was assessed using the Cochrane Risk of Bias 2.0 tool. Bayesian network meta-analysis and Bayesian meta-regression were used to explore comparative efficacy and potential moderators. The framework classified and compared 19 mobile stress interventions, identifying key moderating factors for optimization. Stress management programmes, problem-solving therapy and mindfulness meditation ranked the top. There was no conclusive evidence that human support or mobile technology significantly enhanced intervention outcomes. The evidence is subject to sex imbalance and quality risk, while the limited statistical power of meta-regression warrants caution in interpreting moderator effects. Our findings provide insights for designing more effective and scalable stress interventions and offer promising strategies to reduce health service disparities and advance the Sustainable Development Goals.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All data that support the findings of this study are available via figshare at https://doi.org/10.6084/m9.figshare.27174252.v3 (ref. 61). Source data are provided with this paper.
Code availability
All code for data analyses associated with the current submission are available via figshare at https://doi.org/10.6084/m9.figshare.27174252.v3 (ref. 61).
References
Costa, A. C. et al. Mental health in the post COVID-19 era: future perspectives. Einstein 20, eCE6760 (2022).
World Health Statistics 2020: Monitoring Health for the SDGs, Sustainable Development Goals (World Health Organization, 2020).
Geneva: Classification of Digital Health Interventions (World Health Organization, 2018).
Pineda, B. S. et al. Updated taxonomy of digital mental health interventions: a conceptual framework. mHealth https://doi.org/10.21037/mhealth-23-6 (2023).
Fiedler, J., Eckert, T., Wunsch, K. & Woll, A. Key facets to build up eHealth and mHealth interventions to enhance physical activity, sedentary behavior and nutrition in healthy subjects—an umbrella review. BMC Public Health https://doi.org/10.1186/s12889-020-09700-7 (2020).
Chib, A. & Lin, S. H. Theoretical advancements in mHealth: a systematic review of mobile apps. J. Health Commun. 23, 909–955 (2018).
Gan, D. Z. Q. et al. Technology-supported strategies for promoting user engagement with digital mental health interventions: a systematic review. Digit. Health https://doi.org/10.1177/20552076221098268 (2022).
Firth, J. et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry 16, 287–298 (2017).
Schueller, S. M., Tomasino, K. N. & Mohr, D. C. Integrating human support into behavioral intervention technologies: the efficiency model of support. Clin. Psychol. 24, 27–45 (2017).
Bernstein, E. E. et al. Human support in app-based cognitive behavioral therapies for emotional disorders: scoping review. J. Med. Internet Res. 24, e33307 (2022).
Werntz, A., Amado, S., Jasman, M., Ervin, A. & Rhodes, J. E. Providing human support for the use of digital mental health interventions: systematic meta-review. J. Med. Internet Res. 25, e42864 (2023).
Hicks, J. L. et al. Leveraging mobile technology for public health promotion: a multidisciplinary perspective. Annu. Rev. Public Health 44, 131–150 (2023).
Mohr, D. C., Burns, M. N., Schueller, S. M., Clarke, G. & Klinkman, M. Behavioral intervention technologies: evidence review and recommendations for future research in mental health. Gen. Hosp. Psychiatry 35, 332–338 (2013).
Dugas, M., Gao, G. & Agarwal, R. Unpacking mHealth interventions: a systematic review of behavior change techniques used in randomized controlled trials assessing mHealth effectiveness. Digit. Health https://doi.org/10.1177/2055207620905411 (2020).
Demszky, D. et al. Using large language models in psychology. Nat. Rev. Psychol. 2, 688–701 (2023).
Ke, L., Tong, S., Cheng, P. & Peng, K. Exploring the frontiers of LLMs in psychological applications: a comprehensive review. Preprint at https://arxiv.org/abs/2401.01519 (2024).
Pan, S. et al. Unifying large language models and knowledge graphs: a roadmap. IEEE Trans. Knowl. Data Eng. 36, 3580–3599 (2024).
Lecomte, T. et al. Mobile apps for mental health issues: meta-review of meta-analyses. JMIR Mhealth Uhealth 8, e17458 (2020).
Chen, B., Yang, T., Xiao, L., Xu, C. & Zhu, C. Effects of mobile mindfulness meditation on mental health of university students: systematic review and meta-analysis. J. Med. Internet Res. 25, e39128 (2023).
Shin, Y., Kim, S. K., Kim, Y. & Go, Y. Effects of app-based mobile interventions for dementia family caregivers: a systematic review and meta-analysis. Dement. Geriatr. Cogn. Disord. 51, 203–213 (2022).
Zheng, S. et al. Effectiveness of holistic mobile health interventions on diet, and physical, and mental health outcomes: a systematic review and meta-analysis. EClinicalMedicine https://doi.org/10.1016/j.eclinm.2023.102309 (2023).
Goldberg, S. B., Lam, S. U., Simonsson, O., Torous, J. & Sun, S. Mobile phone-based interventions for mental health: a systematic meta-review of 14 meta-analyses of randomized controlled trials. PLoS Digit. Health 1, e0000002 (2022).
Linardon, J., Cuijpers, P., Carlbring, P., Messer, M. & Fuller‐Tyszkiewicz, M. The efficacy of app‐supported smartphone interventions for mental health problems: a meta‐analysis of randomized controlled trials. World Psychiatry 18, 325–336 (2019).
Zhang, K. et al. Effects of psychological or exercise interventions on problematic mobile phone use: a systematic review and meta-analysis. Curr. Addict. Rep. 10, 230–253 (2023).
Rathbone, A. L. & Prescott, J. The use of mobile apps and SMS messaging as physical and mental health interventions: systematic review. J. Med. Internet Res. 19, e295 (2017).
Efthimiou, O. et al. GetReal in network meta-analysis: a review of the methodology. Res. Synth. Methods 7, 236–263 (2016).
Novais, A., Monteiro, S., Roque, S., Correia-Neves, M. & Sousa, N. How age, sex and genotype shape the stress response. Neurobiol. Stress 6, 44–56 (2016).
Conn, V. S. & Chan, K. C. How much, how often, how long? Addressing dosage in intervention studies. West. J. Nurs. Res. 38, 3–4 (2016).
Lorca-Cabrera, J. et al. Effectiveness of health web-based and mobile app-based interventions designed to improve informal caregiver’s well-being and quality of life: a systematic review. Int. J. Med. Inform. https://doi.org/10.1016/j.ijmedinf.2019.104003 (2020).
Call to Action on Global eHealth Evaluation: Consensus Statement of the WHO Global eHealth Evaluation Meeting (World Health Organization, 2011).
Nixon, P. et al. The efficacy of a web-based stress management intervention for employees experiencing adverse working conditions and occupational self-efficacy as mediator: a randomized controlled trial. J. Med. Internet Res. 24, e40488 (2022).
Ates, H. C., Ates, C. & Dincer, C. Stress monitoring with wearable technology and AI. Nat. Electron. 7, 98–99 (2024).
Mahuli, S. A., Rai, A., Mahuli, A. V. & Kumar, A. Application ChatGPT in conducting systematic reviews and meta-analyses. Br. Dent. J. 235, 90–92 (2023).
Macpherson, M. How well can GPT do scientific literature meta-analysis? Finedataproducts https://finedataproducts.com/posts/2023-12-31-llm-based-metaanalysis/ (2023).
Maydych, V. The interplay between stress, inflammation, and emotional attention: relevance for depression. Front. Neurosci. https://doi.org/10.3389/fnins.2019.00384 (2019).
Daviu, N. et al. Neurobiological links between stress and anxiety. Neurobiol. Stress https://doi.org/10.1016/j.ynstr.2019.100191 (2019).
Rosiek, A., Rosiek-Kryszewska, A., Leksowski, Ł. & Leksowski, K. Chronic stress and suicidal thinking among medical students. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph13020212 (2016).
Dutcher, J. M., Cole, S. W., Williams, A. C. & Creswell, J. D. Smartphone mindfulness meditation training reduces pro-inflammatory gene expression in stressed adults: a randomized controlled trial. Brain Behav. Immun. 103, 171–177 (2022).
Lehrer, P. M., Woolfolk, R. L., & Sime, W. E. (eds) Principles and Practice of Stress Management (Guilford Press, 2007).
Ebert, D. D. et al. Efficacy of an internet-based problem-solving training for teachers: results of a randomized controlled trial. Scand. J. Work Environ. Health. 40, 582–596 (2014).
Heber, E. et al. The benefit of web- and computer-based interventions for stress: a systematic review and meta-analysis. J. Med. Internet Res. 19, e32 (2017).
Cookson, R. et al. Using cost-effectiveness analysis to address health equity concerns. Value Health 20, 206–212 (2017).
Reiners, F., Sturm, J., Bouw, L. J. W. & Wouters, E. J. M. Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph16040645 (2019).
Daniels, K. & Bonnechère, B. Harnessing digital health interventions to bridge the gap in prevention for older adults. Front. Public Health https://doi.org/10.3389/fpubh.2023.1281923 (2024).
Pywell, J., Vijaykumar, S., Dodd, A. & Coventry, L. Barriers to older adults’ uptake of mobile-based mental health interventions. Digit. Health https://doi.org/10.1177/2055207620905422 (2020).
Lazarou, E. & Exarchos, T. P. Predicting stress levels using physiological data: real-time stress prediction models utilizing wearable devices. AIMS Neurosci. 11, 76–102 (2024).
Vos, G., Trinh, K., Sarnyai, Z. & Rahimi Azghadi, M. Generalizable machine learning for stress monitoring from wearable devices: a systematic literature review. Int. J. Med. Inform. https://doi.org/10.1016/j.ijmedinf.2023.105026 (2023).
Hedges, L. V. & Pigott, T. D. The power of statistical tests for moderators in meta-analysis. Psychol. Methods 9, 426–445 (2004).
Ouyang, L. et al. Training language models to follow instructions with human feedback. Adv. Neural Inf. Process. Syst. 35, 27730–27744 (2022).
Goh, Y. S., Ow Yong, J. Q. Y., Chee, B. Q. H., Kuek, J. H. L. & Ho, C. S. H. Machine learning in health promotion and behavioral change: scoping review. J. Med. Internet Res. 24, e35831 (2022).
Liu, C. et al. Early prediction of MODS interventions in the intensive care unit using machine learning. J. Big Data https://doi.org/10.1186/s40537-023-00719-2 (2023).
Higgins, J., Thompson, S., Deeks, J. & Altman, D. Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. J. Health Serv. Res. Policy 7, 51–61 (2002).
Sterne, J. A. C. et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Br. Med. J. 366, l4898 (2019).
Schulhoff, S. et al. The prompt report: a systematic survey of prompt engineering techniques. Preprint at https://arxiv.org/abs/2406.06608 (2024).
Stemler, S. E. A comparison of consensus, consistency, and measurement approaches to estimating interrater reliability. Pract. Assess. Res. Eval. https://doi.org/10.7275/96jp-xz07 (2004).
Mbuagbaw, L. et al. Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst. Rev. https://doi.org/10.1186/s13643-017-0473-z (2017).
Wu, Y. C., Shih, M. C. & Tu, Y. K. Using normalized entropy to measure uncertainty of rankings for network meta-analyses. Med. Decis. Making 41, 706–713 (2021).
Brooks, S. P. & Gelman, A. General methods for monitoring convergence of iterative simulations. J. Comput. Graph. Stat. 7, 434–455 (1998).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br. Med. J. 372, n71 (2021).
Ebert, D. D. et al. Effectiveness and moderators of an internet-based mobile-supported stress management intervention as a universal prevention approach: randomized controlled trial. J. Med. Internet Res. 23, e22107 (2021).
Zhu, H. Y. Data, R code and other files. figshare https://doi.org/10.6084/m9.figshare.27174252.v3 (2024).
Acknowledgements
This research was supported by the National Natural Science Foundation of China under grant nos. 32171076 and 32471135, received by Y.G. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. We thank Y. Hu for help in plotting the leverage plot; J. Tang for help in prompt engineering and metrics evaluation of ChatGPT; X. Gao and X. Jiang for their help with the early literature review, study screening and coding; and S. Fan, J. Su, X. Guo, H. Huang, J. Hu and B. Li for their help with coding and rating.
Author information
Authors and Affiliations
Contributions
H.Z., Q.C. J.L. and Y.G conceived this work. H.Z., Q.C. and X.W. developed the methodology. H.Z., Q.C., X.W. and Q.J. produced the software. H.Z. and Q.C. obtained the resources and undertook the formal analysis. S.W., X.W. and H.Z carried out data curation. H.Z., Q.C. J.L. and Y.G created the figures. Y.G. supervised the project and obtained funding. H.Z., Q.C., S.W. and Y.G. wrote the original draft of the paper. J.L., H.Z., Q.C., X.W. and Y.G. revised the draft of the manuscript. H.Z., Q.C., S.W., X.W., Q.J., J.L.and Y.G. were involved in reviewing and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks C. Bockting, S. U. Lam, Y. Liu and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, H., Chen, Q., Wei, S. et al. A systematic review and Bayesian network meta-analysis on the efficacy and potential of mobile interventions for stress management. Nat Hum Behav 9, 1431–1441 (2025). https://doi.org/10.1038/s41562-025-02162-0
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41562-025-02162-0