Abstract
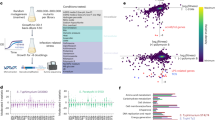
Bacterial pathogens such as Salmonella Typhimurium (S.Tm) can deliver large repertoires of effector proteins directly into host cells. Due to the genetic and functional redundancies found in these systems, it has been difficult to determine how individual effector proteins cooperate with one another to elicit pathogenic phenotypes in vivo. To overcome this challenge, targeted genome minimization has been used to identify small effector protein networks sufficient for S.Tm colonization of complex tissues. Here we used mass cytometry to generate a comprehensive map of minimal effector network functions at single-cell resolution. This approach revealed the temporal progression of S.Tm transmission and uncovered a CD62L+ monocyte population as a major bottleneck to cell-to-cell dissemination in the spleen. We further show how cooperation between two effector gene networks acquired during distinct episodes of bacterial evolution has shaped the cellular and tissue tropism of non-typhoidal Salmonella species.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The data generated in this study are available via Open Science Framework at https://osf.io/r32e4/?view_only=fd5219960e024b9eb783f3030067255e. All FCS files, along with detailed sample annotations and panel information (including metal tags), are available within the repository. Preprocessing and gating strategies were performed using the OMIQ data platform (https://www.omiq.ai) and are described in the Methods section and Extended Data Fig. 5. The high-dimensional clustering and downstream analyses (for example, UMAP and PhenoGraph) were performed using the OMIQ platform, and the data parameters available in the Methods. Further information and requests for raw data or materials should be directed to the corresponding author. Source data are provided with this paper.
References
Costa, T. R. et al. Secretion systems in Gram-negative bacteria: structural and mechanistic insights. Nat. Rev. Microbiol. 13, 343–359 (2015).
Mondino, S. et al. Legionnaires’ disease: state of the art knowledge of pathogenesis mechanisms of Legionella. Annu Rev Pathol 15, 439–466 (2020).
Green, E. R. & Mecsas, J. Bacterial secretion systems: an overview. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.VMBF-0012-2015 (2016).
Venter, J. C., Glass, J. I., Hutchison, C. A. 3rd & Vashee, S. Synthetic chromosomes, genomes, viruses, and cells. Cell 185, 2708–2724 (2022).
Martinez-Garcia, E. & de Lorenzo, V. The quest for the minimal bacterial genome. Curr. Opin. Biotechnol. 42, 216–224 (2016).
Sung, B. H., Choe, D., Kim, S. C. & Cho, B. K. Construction of a minimal genome as a chassis for synthetic biology. Essays Biochem 60, 337–346 (2016).
O’Connor, T. J., Adepoju, Y., Boyd, D. & Isberg, R. R. Minimization of the Legionella pneumophila genome reveals chromosomal regions involved in host range expansion. Proc. Natl Acad. Sci. USA 108, 14733–14740 (2011).
Ruano-Gallego, D. et al. Type III secretion system effectors form robust and flexible intracellular virulence networks. Science https://doi.org/10.1126/science.abc9531 (2021).
Chen, D. et al. Systematic reconstruction of an effector-gene network reveals determinants of Salmonella cellular and tissue tropism. Cell Host Microbe 29, 1531–1544 e1539 (2021).
Jennings, E., Thurston, T. L. M. & Holden, D. W. Salmonella SPI-2 type III secretion system effectors: molecular mechanisms and physiological consequences. Cell Host Microbe 22, 217–231 (2017).
Pillay, T. D. et al. Speaking the host language: how Salmonella effector proteins manipulate the host. Microbiology https://doi.org/10.1099/mic.0.001342 (2023).
Nuccio, S. P. & Baumler, A. J. Comparative analysis of Salmonella genomes identifies a metabolic network for escalating growth in the inflamed gut. mBio 5, e00929–00914 (2014).
Lesnick, M. L., Reiner, N. E., Fierer, J. & Guiney, D. G. The Salmonella spvB virulence gene encodes an enzyme that ADP-ribosylates actin and destabilizes the cytoskeleton of eukaryotic cells. Mol. Microbiol. 39, 1464–1470 (2001).
Haneda, T. et al. Salmonella type III effector SpvC, a phosphothreonine lyase, contributes to reduction in inflammatory response during intestinal phase of infection. Cell Microbiol. 14, 485–499 (2012).
Grabe, G. J. et al. The Salmonella effector SpvD is a cysteine hydrolase with a serovar-specific polymorphism influencing catalytic activity, suppression of immune responses, and bacterial virulence. J. Biol. Chem. 291, 25853–25863 (2016).
Steele-Mortimer, O., Meresse, S., Gorvel, J. P., Toh, B. H. & Finlay, B. B. Biogenesis of Salmonella Typhimurium-containing vacuoles in epithelial cells involves interactions with the early endocytic pathway. Cell. Microbiol. 1, 33–49 (1999).
Buchmeier, N. A. & Heffron, F. Inhibition of macrophage phagosome–lysosome fusion by Salmonella Typhimurium. Infect. Immun. 59, 2232–2238 (1991).
Galan, J. E. & Curtiss, R. 3rd Cloning and molecular characterization of genes whose products allow Salmonella Typhimurium to penetrate tissue culture cells. Proc. Natl Acad. Sci. USA 86, 6383–6387 (1989).
Brown, N. F. et al. Salmonella Pathogenicity Island 2 is expressed prior to penetrating the intestine. PLoS Pathog. 1, e32 (2005).
Cirillo, D. M., Valdivia, R. H., Monack, D. M. & Falkow, S. Macrophage-dependent induction of the Salmonella Pathogenicity Island 2 type III secretion system and its role in intracellular survival. Mol. Microbiol. 30, 175–188 (1998).
Becht, E. et al. Dimensionality reduction for visualizing single-cell data using UMAP. Nat. Biotechnol. https://doi.org/10.1038/nbt.4314 (2018).
Levine, J. H. et al. Data-driven phenotypic dissection of AML reveals progenitor-like cells that correlate with prognosis. Cell 162, 184–197 (2015).
Geddes, K., Cruz, F. & Heffron, F. Analysis of cells targeted by Salmonella type III secretion in vivo. PLoS Pathog. 3, e196 (2007).
Helaine, S. et al. Internalization of Salmonella by macrophages induces formation of nonreplicating persisters. Science 343, 204–208 (2014).
Hickey, M. J. et al. L-selectin facilitates emigration and extravascular locomotion of leukocytes during acute inflammatory responses in vivo. J. Immunol. 165, 7164–7170 (2000).
Xu, H., Manivannan, A., Crane, I., Dawson, R. & Liversidge, J. Critical but divergent roles for CD62L and CD44 in directing blood monocyte trafficking in vivo during inflammation. Blood 112, 1166–1174 (2008).
Scharer, C. D. et al. Antibody-secreting cell destiny emerges during the initial stages of B-cell activation. Nat. Commun. 11, 3989 (2020).
Ito, Y., Nakahara, F., Kagoya, Y. & Kurokawa, M. CD62L expression level determines the cell fate of myeloid progenitors. Stem Cell Rep. 16, 2871–2886 (2021).
Rydstrom, A. & Wick, M. J. Monocyte and neutrophil recruitment during oral Salmonella infection is driven by MyD88-derived chemokines. Eur. J. Immunol. 39, 3019–3030 (2009).
Adachi, O. et al. Targeted disruption of the MyD88 gene results in loss of IL-1- and IL-18-mediated function. Immunity 9, 143–150 (1998).
Akira, S. & Takeda, K. Toll-like receptor signalling. Nat. Rev. Immunol. 4, 499–511 (2004).
Kofoed, E. M. & Vance, R. E. Innate immune recognition of bacterial ligands by NAIPs determines inflammasome specificity. Nature 477, 592–595 (2011).
Zhao, Y. et al. The NLRC4 inflammasome receptors for bacterial flagellin and type III secretion apparatus. Nature 477, 596–600 (2011).
Rauch, I. et al. NAIP proteins are required for cytosolic detection of specific bacterial ligands in vivo. J. Exp. Med. 213, 657–665 (2016).
Perkins, D. J. et al. Salmonella Typhimurium co-opts the host type I IFN system to restrict macrophage innate immune transcriptional responses selectively. J. Immunol. 195, 2461–2471 (2015).
Wilson, R. P. et al. STAT2 dependent type I interferon response promotes dysbiosis and luminal expansion of the enteric pathogen Salmonella Typhimurium. PLoS Pathog. 15, e1007745 (2019).
Mastroeni, P. & Sheppard, M. Salmonella infections in the mouse model: host resistance factors and in vivo dynamics of bacterial spread and distribution in the tissues. Microbes Infect. 6, 398–405 (2004).
Carter, P. B. & Collins, F. M. The route of enteric infection in normal mice. J. Exp. Med. 139, 1189–1203 (1974).
Jones, B. D., Ghori, N. & Falkow, S. Salmonella Typhimurium initiates murine infection by penetrating and destroying the specialized epithelial M cells of the Peyer’s patches. J. Exp. Med. 180, 15–23 (1994).
Dieye, Y., Ameiss, K., Mellata, M. & Curtiss, R. 3rd The Salmonella Pathogenicity Island (SPI) 1 contributes more than SPI2 to the colonization of the chicken by Salmonella enterica serovar Typhimurium. BMC Microbiol. 9, 3 (2009).
Kappeli, R., Kaiser, P., Stecher, B. & Hardt, W. D. Roles of spvB and spvC in S. Typhimurium colitis via the alternative pathway. Int. J. Med. Microbiol. 301, 117–124 (2011).
Salcedo, S. P., Noursadeghi, M., Cohen, J. & Holden, D. W. Intracellular replication of Salmonella Typhimurium strains in specific subsets of splenic macrophages in vivo. Cell Microbiol. 3, 587–597 (2001).
Dunlap, N. E., Benjamin, W. H. Jr., McCall, R. D. Jr., Tilden, A. B. & Briles, D. E. A ‘safe-site’ for Salmonella Typhimurium is within splenic cells during the early phase of infection in mice. Microb. Pathog. 10, 297–310 (1991).
Hoffman, D. et al. A non-classical monocyte-derived macrophage subset provides a splenic replication niche for intracellular Salmonella. Immunity 54, 2712–2723 e2716 (2021).
Rosche, K. L., Aljasham, A. T., Kipfer, J. N., Piatkowski, B. T. & Konjufca, V. Infection with Salmonella enterica serovar Typhimurium leads to increased proportions of F4/80+ red pulp macrophages and decreased proportions of B and T lymphocytes in the spleen. PLoS ONE 10, e0130092 (2015).
Rydstrom, A. & Wick, M. J. Monocyte recruitment, activation, and function in the gut-associated lymphoid tissue during oral Salmonella infection. J. Immunol. 178, 5789–5801 (2007).
Richter-Dahlfors, A., Buchan, A. M. & Finlay, B. B. Murine salmonellosis studied by confocal microscopy: Salmonella Typhimurium resides intracellularly inside macrophages and exerts a cytotoxic effect on phagocytes in vivo. J. Exp. Med. 186, 569–580 (1997).
van der Velden, A. W., Lindgren, S. W., Worley, M. J. & Heffron, F. Salmonella pathogenicity island 1-independent induction of apoptosis in infected macrophages by Salmonella enterica serotype Typhimurium. Infect. Immun. 68, 5702–5709 (2000).
Robinson, N. et al. Type I interferon induces necroptosis in macrophages during infection with Salmonella enterica serovar Typhimurium. Nat. Immunol. 13, 954–962 (2012).
Hiyoshi, H. et al. Virulence factors perforate the pathogen-containing vacuole to signal efferocytosis. Cell Host Microbe 30, 163–170 e166 (2022).
Libby, S. J., Lesnick, M., Hasegawa, P., Weidenhammer, E. & Guiney, D. G. The Salmonella virulence plasmid spv genes are required for cytopathology in human monocyte-derived macrophages. Cell Microbiol. 2, 49–58 (2000).
Hoiseth, S. K. & Stocker, B. A. Aromatic-dependent Salmonella Typhimurium are non-virulent and effective as live vaccines. Nature 291, 238–239 (1981).
Kovach, M. E. et al. Four new derivatives of the broad-host-range cloning vector pBBR1MCS, carrying different antibiotic-resistance cassettes. Gene 166, 175–176 (1995).
Rong, S. et al. Expression of SREBP-1c requires SREBP-2-mediated generation of a sterol ligand for LXR in livers of mice. eLife https://doi.org/10.7554/eLife.25015 (2017).
Acknowledgements
We thank S. Winter and the Winter lab (UC Davis) for their assistance in developing our bacterial strains and mouse experiments used in this experiment. We further acknowledge the UT Southwestern Microbiology Department Live Cell Imaging Facility (NIH: 1S10OD034383) for the use of their microscope and technical expertise, We also acknowledge A. Mobley and the other members of the UT Southwestern Flow Cytometry Core Facility for their assistance with mass cytometry. Furthermore, we would like to mention the UT Southwestern Histopathology Core, including J. Shelton and A. Daniel, for their histopathology and imaging mass cytometry staining. This work was funded by the National Institute of Health (grant nos. AI083359 to N.M.A. and AI158357 to A.R. and N.M.A.), The Welch Foundation (grant nos. I-1704 to N.M.A. and I-1793 to A.R.) and The Burroughs Welcome Fund (grant no. 1011019 to N.M.A.).
Author information
Authors and Affiliations
Contributions
N.M.A. and W.B.B. designed the study and wrote the manuscript. W.B.B., L.T.A., H.D., D.M. and A.B.M. performed the experiments and participated in the data analysis. J.D.F. assisted in the mass cytometry experiment design and data analysis. A.R. assisted in the metabolic activation experiment design and data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Microbiology thanks Leigh Knodler and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Characterization of S.Tm minimal effector strains.
(a-b) Quantification of the number of individual bacteria per HeLa cell (a) or RAW 264.7 macrophage (b) infected with the indicated S.Tm strains. A total 150 cells from 3 biological replicates were counted. Infections were conducted on Hela (MOI = 50) and RAW 264.7 (MOI=1) and the number of bacteria per cell were quantified 18 hours post infection (hpi) and 24 hpi, respectively. Mean (red bars). Statistics: one-way ANOVA with Dunnett’s multiple comparison. p<0.05 considered significant and values are shown on the graphs as compared to S.Tm. (c) Food intake by C57BL/6J mice uninfected or infected intragastrically (i.g.) with 1x109 S.Tm, S.Tm Efl, S.Tm θ, and S.Tm θ spv+ (n=5 mice/S.Tm strain). Food intake was measured at three different time points during a four day infection 24-48h, 48-72h, 72-96h. Food intake measurements for each cohort of mice included the entire cage (n=5 mice/cage). (d) Model of SREBP1 activation during feeding and fasting conditions. During feeding SREBP1 is processed and its N-terminal transcription factor domain translocates to the nucleus to initiate lipogenesis. During fasting SREBP1 levels decline. Western blots against SREBP1 showing full length unprocessed SREBP1 (P) or processed Nuclear (N) SREBP1 in livers from mice infected intragastrically (i.g.) with the S.Tm strains indicated. S.Tm strains used to infect mice (i.g.) with 1x109 bacteria from the strains represented are shown at the top and each lane represents one mouse (n=3 mice for each S.Tm genotype).
Extended Data Fig. 2 Characterization of CyTOF for in vivo detection of S.Tm.
(a) An antibody recognizing Salmonella lipopolysaccharide (LPS) was conjugated with the lanthanide metal Dysoprosium-163 (Dy163). (b, c) The LPS antibody recognized intracellular S.Tm as assessed by immunofluorescence microscopy (b) and by conventional flow cytometry (c). (b) Representative immunofluorescence images of Hela cells infected for 18 hours with a GFP expressing S.Tm (MOI = 25) (left image) labeled by immunocytochemistry using the anti-LPS antibody (right image). GFP and LPS signals colocalize in these images verifying the LPS staining of Salmonella. (c) Representative flow cytometry histogram analysis of H1299 cells infected for 18 hours with S.Tm (MOI = 25), labeled with the anti-LPS antibody and analyzed by flow cytometry. Uninfected cells (top), infected cells (bottom). Experiments were repeated three times. (d) We tested the LPS-Dy163 antibody to detect S.Tm in primary immune cells. C57BL/6 mice were uninfected (n=3) or intraperitoneally (i.p.) (1x104 S.Tm bacteria) (n=3) or infected intragastrically (i.g.) (1x109 S.Tm bacteria) (n=3) and sacrificed 7 dpi and 4 dpi, respectively. Splenocytes were fixed and labelled with anti-CD45-Y89 antibody to detect the leukocyte common antigen. We then permeabilized and labelled these cells with LPS-Dy163. Mass cytometry contour plot analysis of murine splenocytes immunolabeled with anti-S.Tm LPS-Dy163 and anti-CD45-Y89 antibodies showing the percentage of cells within the LPSpos region (box). As expected, CD45pos immune cells from uninfected mice exhibited low background levels of LPS-Dy163 signal. In contrast, high LPS signal (LPSpos) was detected in CD45pos splenocytes from mice challenged with S.Tm by both the i.p. and i.g. routes of infection.
Extended Data Fig. 3 The LPS antibody detects intracellular replicating S.Tm in vivo.
(a) An antibody directed at LPS could detect living bacteria or LPS particles that are ingested by phagocytes or displayed on the surface of antigen presenting cells. To test the specificity of LPS antibody for living bacteria, we first examined LPS particles in cells grown in vitro. RAW264.7 murine macrophages were infected with S.Tm-GFP or heat killed S.Tm-GFP (MOI = 100) and fixed for imaging 24 hpi. Cells were immunolabeled with anti-LPS antibody and stained with DAPI. Maximum intensity projections of confocal images spanning the entire z-dimension of the cell are shown. Dotted lines show the cell borders. Right panels are higher magnification images of the white boxed regions in left panels. Experiments were repeated in triplicate. These data show that the antibody directed at LPS could detect living bacteria and LPS particles ingested by phagocytes in vitro. We then sought to determine if the antibody to LPS also detected LPS particles on the surface of antigen presenting cells (b) or intracellularly in vivo (c). (b) C57BL/6 mice infected with 1x109 S.Tm by i.g. route and splenocytes were collected from these samples and subjected to CyTOF with the following modifications: Mouse splenocytes were either permeabilized or unpermeablized with Perm-S buffer (see Methods) and then immunolabeled with anti-CD45-Y89 and anti-S.Tm LPS-Dy163 antibodies (top). Contour plots from each samples is shown (top plots) and quantification of the number of LPSpos cells within total CD45pos splenocytes collected from C57BL/6 mice from three independent experiments is shown (bottom). Error bars show: Mean +/− SEM, Statistics: multiple T-tests. Detergent permeabilization was required to detect LPSpos signal in infected CD45pos splenocytes, indicating that LPS-Dy163 does not primarily detect LPS particles displayed on the surface of antigen presenting cells in vivo. (c) We next tested if the LPS-Dy163 detected LPS particles within immune cells. C57BL/6 mice infected intraperitoneally (i.p.) with PBS (n=3), or 1x104 S.Tm (n=3) or heat killed S.Tm (n=3) and stained with anti-S.Tm LPS-Dy163 and anti-CD45-Y89 antibodies. Data was analyzed by CyTOF. Representative contour plots are shown to the left and quantification of LPS signal in CD45pos splenocytes from three experiments is shown to the right. Graph error bars show Mean +/− SEM. Statistics show one-way ANOVA with Dunnett’s multiple comparison. p<0.05 compared to uninfected control is shown. We did not detect LPSpos signal in CD45pos splenocytes isolated from mice infected with heat killed S.Tm by the i.p route of infection consistent with CyTOF detection of living intracellular bacteria and not LPS particles in vivo. (d) We tested whether the CyTOF procedure accurately portrayed the levels of intracellular replicating S.Tm in vivo. C57BL/6 mice were either uninfected or infected i.g. with 1x109 S.Tm for 4 days. Splenocytes were collected from each mouse and analyzed for total CFUs per spleen and processes for CyTOF. Mass cytometry contour plots as in (d) of splenocytes collected from an uninfected mouse or from three individual i.g. infected mice are shown. CFU/g of bacteria in the spleen of each mouse is shown above the plots. (n=1 mouse per CFU value, 1x109 S.Tm bacteria/infection). These data show an increase of LPSpos staining with an increased CFU/g S.Tm. (e) We sought to confirm that the LPSpos signal in our large immune cell analysis correlated with bacterial burden so we analyzed the wild-type S.Tm samples from our large cohort analysis (Extended Data Table 1) for correlation between %LPSpos cells and CFU recovered from mouse splenocytes infected i.g. with S.Tm. The total number of LPSpos CD45pos signal detected in spleen tissue increased linearly with the total number of living bacteria (CFU/g of spleen tissue) recovered from these animals. Linear regression analysis performed on GraphPad Prism R2 = 0.967, F(1,32), p<0.0001. These data confirm that total LPSpos staining correlates with the increasing levels of S.Tm infection in vivo.
Extended Data Fig. 4 Imaging mass cytometry of S.Tm infected spleens.
(a–m) To further characterize the anti-LPS-Dy163 antibody, we applied imaging mass cytometry to spleen tissue samples from S.Tm infected mice displaying severe signs of Typhoid-like disease. Paraffin embedded tissue sections were stained with an antibody panel that included markers for canonical immune cell subsets (for example B-cells, T-cells, myeloid cells), markers for spleen architecture (for example endothelial cells, smooth muscle, and extra cellular matrix), and our anti-S.Tm LPS-Dy163. (a) Representative mouse spleen sections in bright field (left) and imaged with the Helios mass cytometer (right, higher magnification view of the red boxed region at (left) from uninfected (top) and i.g. infected (1x109 S.Tm) (bottom). Sections labeled with DNA (blue), membrane marker (red), and S.Tm LPS (green). Experiments repeated in triplicate. (b) The LPSpos signal was adjacent to the nucleus and within the plasma membrane borders of individual cells consistent with the perinuclear localization of intracellular Salmonella that we detected in tissue culture cells and has been reported in vitro. (b’ – b’’) Insets from (a, right). Hexagons indicate the rough outline of individual cells identified by plasma membrane and nuclear labeling that are infected with S.Tm (identified by anti-LPS-Dy163). (c-d) Representative images from imaging mass cytometry data collected on a Helios Mass Cytometer from spleen tissue sections of C57BL/6 mice uninfected (c) or infected i.g. (d) with 1x109 S.Tm. Tissue sections are immunolabeled for CD11b-Sm149 (magenta), B220-Dy162 (cyan), and CD8-Yb176 (yellow) (top panels) LPS immunolabeling (green) in the same region as above (middle panels). Higher magnification of LPS immunolabeling in white boxed regions (lower panels). Arrows (white) show large colonies of S.Tm and arrowheads (yellow) show possible individual bacteria within cells. (e–m) Imaging mass cytometry data as in (d) showing anti-LPS signal (green) with the cell markers shown (red). DNA - Nuclei (e), plasma membrane (f), endothelial cells CD31 (g), smooth muscle actin (S.M.A.) (h), fibronectin (i), collagen (j), myeloid cells CD11b (k), myeloid cells F4/80 (l), and Cytotoxic lymphocytes Granzyme B (m). Hyperion mass cytometry revealed the splenic architecture at high resolution as denoted by the distinct zones of B-cells (B220pos) and CD8 T-cells (CD8pos) enriched within the white pulp of uninfected and infected mice. Importantly, LPSpos staining was apparent in tissues of mice infected with S.Tm, but not in uninfected samples. The LPSpos signal was adjacent to the nucleus and within the plasma membrane borders of individual cells consistent with the perinuclear localization of intracellular Salmonella that has been reported in vitro. The LPSpos signal in the cell ranged in size from what appeared to be potentially single bacteria to colonies likely consisting of multiple bacteria per cell. As previously observed, S.Tm was partially associated with splenic endothelial cells, but S.Tm was not enriched in tissue regions dominated by smooth muscle cells, or structural components of the spleen and vasculature. LPSpos signal was also detected in tissue regions enriched with myeloid cells (CD11bpos or F4/80pos), reflecting previous observations made with traditional immunohistochemistry. Experiments were repeated in triplicate.
Extended Data Fig. 5 Gating strategy and UMAP signal distribution of immune markers for immune cell subsets.
(a) Representative gating strategy for the 13 manually defined immune cell populations (see also Materials and Methods). Axes are labeled with the antibody epitope and the metal associated with the antibody. Red boxes are the gates used in the analysis pipeline to designate cells. Red arrows represent the next gate in the series. (b) UMAP Graphs showing heatmaps for the individual antibody markers in the immune panel. All graphs represent equal subsampling of each mouse (35,714 cells/mouse). Heatmaps include all 34 mouse spleens analyzed from all strains. The protein recognized by the antibody is labeled in the top left corner.
Extended Data Fig. 6 Quantitative analysis of immune cell subsets during Salmonella infection.
(a) UMAP graphs of the entire splenocyte population were used to analyze the host immune response to different S.Tm strains. 3 uninfected mice, as well as 3 mice infected i.g. with 1x109 bacteria with each of the strains S.Tm, S.Tm Efl, S.Tm θ, or S.Tm θ spv+ and sacrificed at 7 dpi were included in this analysis (see Extended Data Table 1). Each UMAP is a concatenation of the 3 mice infected with the indicated S.Tm strain. Dotted lines represent the position in the UMAP graph of cell populations in uninfected murine samples. (b) Total number of cells in spleen samples for each immune cell type shown in (a). Mean +/− SEM (n=3 mice/group). Statistics: one-way ANOVA with Dunnett’s multiple comparison. p<0.05 compared to uninfected control is shown. In general, we observed either an increase in cell number, a decrease in cell number or an alteration in activation state for nearly every immune cell type in response to wildtype S.Tm infection. For example, S.Tm induced an influx of neutrophils, macrophage, and active CD8pos T-cells into splenic tissue. We also observed a retraction of the effector memory and central memory T-cell populations under these conditions. While there was no change in total B-cell numbers within the spleen, these cells were highly activated by S.Tm infection. Interestingly, the UMAPs from mice infected with S.Tm Efl or S.Tm θ strains show an overall immune cell pattern that is similar to uninfected mice. This is consistent with the low levels of spleen colonization (Extended Data Table 1) and the low clinical scores (lack of symptoms) caused by infection with these strains (Fig. 1). In contrast, the host immune cell response to S.Tm θ spv+ infection was nearly identical to wildtype S.Tm. These data reinforce our conclusion that co-expression of the θ and spv operon effectors is the primary driver of cell-to-cell dissemination of S.Tm, which consequently drives the host immune cell responses to infection in the spleen.
Supplementary information
Supplementary Tables 1–3
Supplementary Table 1. Bacterial strains used in this study. Supplementary Table 2. Antibodies used for imaging mass cytometry. Supplementary Table 3. Antibodies used for mass cytometry.
Source data
Source Data Extended Data Fig. 1
Unmodified western blot for SREBP1 in Extended Data Fig. 1.
Source Data Extended Data Fig. 1
Unmodified western blot for actin in Extended Data Fig. 1.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Burford, W.B., Dilabazian, H., Alto, L.T. et al. Single-cell analysis of genetically minimized Salmonella reveals effector gene cooperation in vivo. Nat Microbiol 10, 2565–2578 (2025). https://doi.org/10.1038/s41564-025-02099-0
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41564-025-02099-0