Abstract
The management of brain metastases is challenging and should ideally be coordinated through a multidisciplinary approach. Stereotactic radiosurgery (SRS) has been the cornerstone of management for most patients with oligometastatic central nervous system involvement (one to four brain metastases), and several technological and therapeutic advances over the past decade have broadened the indications for SRS to include polymetastatic central nervous system involvement (>4 brain metastases), preoperative application and fractionated SRS, as well as combinatorial approaches with targeted therapy and immune-checkpoint inhibitors. For example, improved imaging and frameless head-immobilization technologies have facilitated fractionated SRS for large brain metastases or postsurgical cavities, or lesions in proximity to organs at risk. However, these opportunities come with new challenges and questions, including the implications of tumour histology as well as the role and sequencing of concurrent systemic treatments. In this Review, we discuss these advances and associated challenges in the context of ongoing clinical trials, with insights from a global group of experts, including recommendations for current clinical practice and future investigations. The updates provided herein are meaningful for all practitioners in clinical oncology.
Key points
-
Advances in imaging, patient immobilization techniques and radiotherapy-planning software have expanded the scope of stereotactic radiosurgery (SRS) for the treatment of brain metastases.
-
Paradigms for determining suitability for SRS are gradually shifting away from strict thresholds of number and size of brain metastases to total intracranial tumour volume along with increased consideration of the influence of tumour histology.
-
Fractionated SRS can increase efficacy while minimizing the risk of adverse radiation events, particularly for larger brain metastases; however, the optimal fractionation schedule and dosing remains to be established.
-
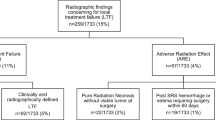
Reliable detection of adverse radiation events, specifically distinguishing radionecrosis from tumour recurrence, remains challenging, although trials using advanced imaging approaches are under way.
-
Neoadjuvant SRS might minimize the risk of leptomeningeal dissemination and simplify radiation-dose planning. Ongoing trials will better define strategies for patient selection (for example, amenable tumour types) as well as the optimal dosing, schedule and timing of SRS before surgery.
-
Immune-checkpoint inhibitors and brain-penetrant targeted therapies have added to our armamentarium of treatment for brain metastases. However, further research is needed to determine the optimal sequencing of these systemic therapies in relation to SRS — or potentially whether SRS can be omitted altogether.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Change history
03 October 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41571-025-01083-1
References
Schnurman, Z. et al. Causes of death in patients with brain metastases. Neurosurgery 93, 986–993 (2023).
Lamba, N., Wen, P. Y. & Aizer, A. A. Epidemiology of brain metastases and leptomeningeal disease. Neuro-Oncol. 23, 1447–1456 (2021).
Ladbury, C. et al. Stereotactic radiosurgery in the management of brain metastases: a case-based radiosurgery society practice guideline. Adv. Radiat. Oncol. 9, 101402 (2024).
Vogelbaum, M. A. et al. Treatment for brain metastases: ASCO-SNO-ASTRO guideline. J. Clin. Oncol. 40, 492–516 (2022).
Schiff, D. et al. Radiation therapy for brain metastases: ASCO guideline endorsement of ASTRO guideline. J. Clin. Oncol. 40, 2271–2276 (2022).
Aizer, A. A. et al. Brain metastases: a Society for Neuro-Oncology (SNO) consensus review on current management and future directions. Neuro-Oncol. 24, 1613–1646 (2022).
Nahed, B. V. et al. Congress of neurological surgeons systematic review and evidence-based guidelines on the role of surgery in the management of adults with metastatic brain tumors. Neurosurgery 84, E152–e155 (2019).
Ammirati, M., Nahed, B. V., Andrews, D., Chen, C. C. & Olson, J. J. Congress of neurological surgeons systematic review and evidence-based guidelines on treatment options for adults with multiple metastatic brain tumors. Neurosurgery 84, E180–e182 (2019).
Gaspar, L. E. et al. Congress of neurological surgeons systematic review and evidence-based guidelines on the role of whole brain radiation therapy in adults with newly diagnosed metastatic brain tumors. Neurosurgery 84, E159–e162 (2019).
Kim, M. M. et al. National Cancer Institute collaborative workshop on shaping the landscape of brain metastases research: challenges and recommended priorities. Lancet Oncol. 24, e344–e354 (2023).
Kondziolka, D., Kalkanis, S. N., Mehta, M. P., Ahluwalia, M. & Loeffler, J. S. It is time to reevaluate the management of patients with brain metastases. Neurosurgery 75, 1–9 (2014).
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Central Nervous System Cancers version 4.2024 (National Comprehensive Cancer Network, 2025).
Fadul, C. E. et al. Defining the quality of interdisciplinary care for patients with brain metastases: modified Delphi panel recommendations. Lancet Oncol. 25, e432–e440 (2024).
Borius, P. Y. et al. Safety of radiosurgery concurrent with systemic therapy (chemotherapy, targeted therapy, and/or immunotherapy) in brain metastases: a systematic review. Cancer Metastasis Rev. 40, 341–354 (2021).
Milano, M. T. et al. Executive summary from American Radium Society’s appropriate use criteria on neurocognition after stereotactic radiosurgery for multiple brain metastases. Neuro-Oncol. 22, 1728–1741 (2020).
Le Rhun, E. et al. EANO–ESMO clinical practice guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours. Ann. Oncol. 32, 1332–1347 (2021).
Le Rhun, E. et al. EANO–ESMO clinical practice guidelines for diagnosis, treatment and follow-up of patients with leptomeningeal metastasis from solid tumours. Ann. Oncol. 28, iv84–iv99 (2017).
Chen, W. C. et al. Efficacy and safety of stereotactic radiosurgery for brainstem metastases: a systematic review and meta-analysis. JAMA Oncol. 7, 1033–1040, (2021).
Borm, K. J. et al. DEGRO guideline for personalized radiotherapy of brain metastases and leptomeningeal carcinomatosis in patients with breast cancer. Strahlenther. Onkol. 200, 259–275 (2024).
Chougule, P. et al. Randomized treatment of brain metastasis with gamma knife radiosurgery, whole brain radiotherapy or both. Int. J. Radiat. Oncol. Biol. Phys. 48, 114–114 (2000).
Andrews, D. W. et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363, 1665–1672 (2004).
Kondziolka, D., Patel, A., Lunsford, L. D., Kassam, A. & Flickinger, J. C. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 45, 427–434 (1999).
Patil, C. G. et al. Whole brain radiation therapy (WBRT) alone versus WBRT and radiosurgery for the treatment of brain metastases. Cochrane Database Syst. Rev. 9, Cd006121 (2017).
Sahgal, A. et al. Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. Int. J. Radiat. Oncol. Biol. Phys. 91, 710–717 (2015).
Kocher, M. et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J. Clin. Oncol. 29, 134–141 (2011).
Aoyama, H. et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastasesa randomized controlled trial. JAMA 295, 2483–2491 (2006).
Chang, E. L. et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 10, 1037–1044 (2009).
Brown, P. D. et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316, 401–409 (2016).
Roth, P. et al. Neurological and vascular complications of primary and secondary brain tumours: EANO–ESMO clinical practice guidelines for prophylaxis, diagnosis, treatment and follow-up. Ann. Oncol. 32, 171–182 (2021).
Brastianos, P. K. et al. Genomic characterization of brain metastases reveals branched evolution and potential therapeutic targets. Cancer Discov. 5, 1164–1177 (2015).
Graber, J. J., Cobbs, C. S. & Olson, J. J. Congress of neurological surgeons systematic review and evidence-based guidelines on the use of stereotactic radiosurgery in the treatment of adults with metastatic brain tumors. Neurosurgery 84, E168–e170 (2019).
Mahajan, A. et al. Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol. 18, 1040–1048 (2017).
Brown, P. D. et al. Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC·3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol. 18, 1049–1060 (2017).
Shafie, R. E. et al. Neurocognition and quality of life for hypofractionated stereotactic radiotherapy (HFSRT) of the resection cavity vs. whole-brain radiotherapy (WBRT) following brain metastasis resection — results of the ESTRON randomized phase 2 trial. Int. J. Radiat. Oncol. Biol. Phys. 120, S39–S40 (2024).
Rusthoven, C. G., Camidge, D. R., Robin, T. P. & Brown, P. D. Radiosurgery for small-cell brain metastases: challenging the last bastion of preferential whole-brain radiotherapy delivery. J. Clin. Oncol. 38, 3587–3591 (2020).
Rusthoven, C. G. et al. Evaluation of first-line radiosurgery vs whole-brain radiotherapy for small cell lung cancer brain metastases: the FIRE-SCLC cohort study. JAMA Oncol. 6, 1028–1037 (2020).
Rusthoven, C. G. et al. Comparison of first-line radiosurgery for small-cell and non-small cell lung cancer brain metastases (CROSS-FIRE). J. Natl Cancer Inst. 115, 926–936 (2023).
Gaebe, K. et al. Stereotactic radiosurgery versus whole brain radiotherapy in patients with intracranial metastatic disease and small-cell lung cancer: a systematic review and meta-analysis. Lancet Oncol. 23, 931–939 (2022).
Zeng, M. et al. Stereotactic radiotherapy vs whole brain radiation therapy in EGFR mutated NSCLC: results and reflections from the prematurely closed phase III HYBRID trial. Radiother. Oncol. 197, 110334 (2024).
Hong, A. M. et al. Adjuvant whole-brain radiation therapy compared with observation after local treatment of melanoma brain metastases: a multicenter, randomized phase III trial. J. Clin. Oncol. 37, 3132–3141 (2019).
Berger, A. et al. Extended survival in patients with non-small-cell lung cancer-associated brain metastases in the modern era. Neurosurgery 93, 50–59 (2023).
Mashiach, E. et al. Long-term survival from breast cancer brain metastases in the era of modern systemic therapies. Neurosurgery 94, 154–164 (2024).
Berger, A. et al. Significant survival improvements for patients with melanoma brain metastases: can we reach cure in the current era? J. Neurooncol. 158, 471–480 (2022).
Magnuson, W. J. et al. Management of brain metastases in tyrosine kinase inhibitor-naïve epidermal growth factor receptor-mutant non-small-cell lung cancer: a retrospective multi-institutional analysis. J. Clin. Oncol. 35, 1070–1077 (2017).
Johung, K. L. et al. Extended survival and prognostic factors for patients with ALK-rearranged non-small-cell lung cancer and brain metastasis. J. Clin. Oncol. 34, 123–129 (2016).
Subbiah, V., Burris H. A. 3rd & Kurzrock, R. Revolutionizing cancer drug development: harnessing the potential of basket trials. Cancer 130, 186–200 (2023).
Wahida, A. et al. The coming decade in precision oncology: six riddles. Nat. Rev. Cancer 23, 43–54 (2023).
Shaw, E. et al. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int. J. Radiat. Oncol. Biol. Phys. 47, 291–298 (2000).
Milano, M. T. et al. Single- and multifraction stereotactic radiosurgery dose/volume tolerances of the brain. Int. J. Radiat. Oncol. Biol. Phys. 110, 68–86 (2021).
Murphy, E. S. et al. Phase I trial of dose escalation for preoperative stereotactic radiosurgery for patients with large brain metastases. Neuro-Oncol. 26, 1651–1659 (2024).
Harary, P. M. et al. Genomic predictors of radiation response: recent progress towards personalized radiotherapy for brain metastases. Cell Death Discov. 10, 501 (2024).
Lamba, N. et al. A genomic score to predict local control among patients with brain metastases managed with radiation. Neuro-Oncol. 25, 1815–1827 (2023).
McTyre, E. et al. Multi-institutional competing risks analysis of distant brain failure and salvage patterns after upfront radiosurgery without whole brain radiotherapy for brain metastasis. Ann. Oncol. 29, 497–503 (2018).
Yamamoto, M. et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol. 15, 387–395 (2014).
Yamamoto, M. et al. A multi-institutional prospective observational study of stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901 study update): irradiation-related complications and long-term maintenance of mini-mental state examination scores. Int. J. Radiat. Oncol. Biol. Phys. 99, 31–40 (2017).
Farris, M. et al. Brain metastasis velocity: a novel prognostic metric predictive of overall survival and freedom from whole-brain radiation therapy after distant brain failure following upfront radiosurgery alone. Int. J. Radiat. Oncol. Biol. Phys. 98, 131–141 (2017).
Achrol, A. S. et al. Brain metastases. Nat. Rev. Dis. Primers 5, 5 (2019).
Robin, T. P. et al. Excellent outcomes with radiosurgery for multiple brain metastases in ALK and EGFR driven non-small cell lung cancer. J. Thorac. Oncol. 13, 715–720 (2018).
Peters, S. et al. Antibody–drug conjugates in lung and breast cancer: current evidence and future directions — a position statement from the ETOP IBCSG Partners Foundation. Ann. Oncol. 35, 607–629 (2024).
Likhacheva, A. et al. Predictors of survival in contemporary practice after initial radiosurgery for brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 85, 656–661 (2013).
Baschnagel, A. M. et al. Tumor volume as a predictor of survival and local control in patients with brain metastases treated with Gamma Knife surgery. J. Neurosurg. 119, 1139–1144 (2013).
Bhatnagar, A. K., Flickinger, J. C., Kondziolka, D. & Lunsford, L. D. Stereotactic radiosurgery for four or more intracranial metastases. Int. J. Radiat. Oncol. Biol. Phys. 64, 898–903 (2006).
Yri, O. E. et al. Survival and quality of life after first-time diagnosis of brain metastases: a multicenter, prospective, observational study. Lancet Reg. Health Eur. 49, 101181 (2025).
El Shafie, R. A. et al. Stereotactic radiosurgery for 1–10 brain metastases to avoid whole-brain radiotherapy: results of the CYBER-SPACE randomized phase 2 trial. Neuro-Oncol. 27, 479–491 (2025).
Mehta, M. P. et al. Results from METIS (EF-25), an international, multicenter phase III randomized study evaluating the efficacy and safety of tumor treating fields (TTFields) therapy in NSCLC patients with brain metastases. J. Clin. Oncol. 42, 2008–2008 (2024).
Ayala-Peacock, D. N. et al. A nomogram for predicting distant brain failure in patients treated with gamma knife stereotactic radiosurgery without whole brain radiotherapy. Neuro-Oncol. 16, 1283–1288 (2014).
Yang, W. C. et al. Hippocampal avoidance whole-brain radiotherapy without memantine in preserving neurocognitive function for brain metastases: a phase II blinded randomized trial. Neuro-Oncol. 23, 478–486 (2021).
Westover, K. D. et al. Phase II trial of hippocampal-sparing whole brain irradiation with simultaneous integrated boost for metastatic cancer. Neuro-Oncol. 22, 1831–1839 (2020).
Brown, P. D. et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro-Oncol. 15, 1429–1437 (2013).
Brown, P. D. et al. Hippocampal avoidance during whole-brain radiotherapy plus memantine for patients with brain metastases: phase III trial NRG Oncology CC001. J. Clin. Oncol. 38, 1019–1029 (2020).
Rapp, S. R. et al. Donepezil for irradiated brain tumor survivors: a phase III randomized placebo-controlled clinical trial. J. Clin. Oncol. 33, 1653–1659 (2015).
Hartgerink, D. et al. A Dutch phase III randomized multicenter trial: whole brain radiotherapy versus stereotactic radiotherapy for 4–10 brain metastases. Neurooncol. Adv. 3, vdab021 (2021).
Markowitsch, H. J. & Staniloiu, A. Amygdala in action: relaying biological and social significance to autobiographical memory. Neuropsychologia 49, 718–733 (2011).
Bernardes da Cunha, S., Carneiro, M. C., Miguel Sa, M., Rodrigues, A. & Pina, C. Neurodevelopmental outcomes following prenatal diagnosis of isolated corpus callosum agenesis: a systematic review. Fetal Diagn. Ther. 48, 88–95 (2021).
Ferguson, M. A. et al. A human memory circuit derived from brain lesions causing amnesia. Nat. Commun. 10, 3497 (2019).
Cherng, H. R. R. et al. Evaluating neurocognitive recovery following stereotactic radiosurgery and whole brain radiation therapy: insights from a pooled analysis of three phase III trials. Int. J. Radiat. Oncol. Biol. Phys. 120, S39 (2024).
Kerschbaumer, J. et al. Risk factors for radiation necrosis in patients undergoing cranial stereotactic radiosurgery. Cancers 13, 4736 (2021).
Korytko, T. et al. 12 Gy gamma knife radiosurgical volume is a predictor for radiation necrosis in non-AVM intracranial tumors. Int. J. Radiat. Oncol. Biol. Phys. 64, 419–424 (2006).
Wiggenraad, R. et al. Dose-effect relation in stereotactic radiotherapy for brain metastases. A systematic review. Radiother. Oncol. 98, 292–297 (2011).
Pichardo-Rojas, P. S. et al. Comparative effectiveness of frame-based and mask-based Gamma Knife stereotactic radiosurgery in brain metastases: a 509 patient meta-analysis. J. Neurooncol. 170, 53–66 (2024).
Minniti, G. et al. Single-fraction versus multifraction (3 × 9 Gy) stereotactic radiosurgery for large (>2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int. J. Radiat. Oncol. Biol. Phys. 95, 1142–1148 (2016).
Yan, M. et al. Gamma knife icon based hypofractionated stereotactic radiosurgery (GKI-HSRS) for brain metastases: impact of dose and volume. J. Neurooncol. 159, 705–712 (2022).
Mengue, L. et al. Brain metastases treated with hypofractionated stereotactic radiotherapy: 8 years experience after Cyberknife installation. Radiat. Oncol. 15, 82 (2020).
Lehrer, E. J. et al. Single versus multifraction stereotactic radiosurgery for large brain metastases: an international meta-analysis of 24 trials. Int. J. Radiat. Oncol. Biol. Phys. 103, 618–630 (2019).
July, J. & Pranata, R. Hypofractionated versus single-fraction stereotactic radiosurgery for the treatment of brain metastases: a systematic review and meta-analysis. Clin. Neurol. Neurosurg. 206, 106645 (2021).
Lee, E. J., Choi, K. S., Park, E. S. & Cho, Y. H. Single- and hypofractionated stereotactic radiosurgery for large (>2 cm) brain metastases: a systematic review. J. Neurooncol. 154, 25–34 (2021).
Di Perri, D., Tanguy, R., Malet, C., Robert, A. & Sunyach, M. P. Risk of radiation necrosis after hypofractionated stereotactic radiotherapy (HFSRT) for brain metastases: a single center retrospective study. J. Neurooncol. 149, 447–453 (2020).
Myrehaug, S. et al. Hypofractionated stereotactic radiation therapy for intact brain metastases in 5 daily fractions: effect of dose on treatment response. Int. J. Radiat. Oncol. Biol. Phys. 112, 342–350 (2022).
Sperduto, P. W. et al. Survival in patients with brain metastases: summary report on the updated diagnosis-specific graded prognostic assessment and definition of the eligibility quotient. J. Clin. Oncol. 38, 3773–3784 (2020).
Alzate, J. D. et al. Low-dose radiosurgery for brain metastases in the era of modern systemic therapy. Neurosurgery 93, 1112–1120 (2023).
Crouzen, J. A. et al. SAFESTEREO: phase II randomized trial to compare stereotactic radiosurgery with fractionated stereotactic radiosurgery for brain metastases. BMC Cancer 23, 273 (2023).
Redmond, K. J. et al. Tumor control probability of radiosurgery and fractionated stereotactic radiosurgery for brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 110, 53–67 (2021).
Ene, C. I. et al. Response of treatment-naive brain metastases to stereotactic radiosurgery. Nat. Commun. 15, 3728 (2024).
Bennett, S. et al. Quantifying gadolinium-based nanoparticle uptake distributions in brain metastases via magnetic resonance imaging. Sci. Rep. 14, 11959 (2024).
Chambrelant, I. et al. Stereotactic radiation therapy of single brain metastases: a literature review of dosimetric studies. Cancers 15, 3937 (2023).
Nath, S. K. et al. Optically-guided frameless linac-based radiosurgery for brain metastases: clinical experience. J. Neurooncol. 97, 67–72 (2010).
Andrevska, A., Knight, K. A. & Sale, C. A. The feasibility and benefits of using volumetric arc therapy in patients with brain metastases: a systematic review. J. Med. Radiat. Sci. 61, 267–276 (2014).
Shaw, E. et al. Radiation Therapy Oncology Group: radiosurgery quality assurance guidelines. Int. J. Radiat. Oncol. Biol. Phys. 27, 1231–1239 (1993).
Grishchuk, D. et al. ISRS technical guidelines for stereotactic radiosurgery: treatment of small brain metastases (≤1 cm in diameter). Pract. Radiat. Oncol. 13, 183–194 (2023).
Paddick, I. et al. Benchmarking tests of contemporary SRS platforms: have technological developments resulted in improved treatment plan quality? Pract. Radiat. Oncol. 13, e451–e459 (2023).
Scorsetti, M. et al. Radiosurgery of limited brain metastases from primary solid tumor: results of the randomized phase III trial (NCT02355613) comparing treatments executed with a specialized or a C-arm linac-based platform. Radiat. Oncol. 18, 28 (2023).
Leith, J. T. et al. Intrinsic and extrinsic characteristics of human tumors relevant to radiosurgery: comparative cellular radiosensitivity and hypoxic percentages. Acta Neurochir. Suppl. 62, 18–27 (1994).
Tomé, W. A. & Fowler, J. F. Selective boosting of tumor subvolumes. Int. J. Radiat. Oncol. Biol. Phys. 48, 593–599 (2000).
Lucia, F. et al. Inhomogeneous tumor dose distribution provides better local control than homogeneous distribution in stereotactic radiotherapy for brain metastases. Radiother. Oncol. 130, 132–138 (2019).
Kohutek, Z. A. et al. Long-term risk of radionecrosis and imaging changes after stereotactic radiosurgery for brain metastases. J. Neurooncol. 125, 149–156 (2015).
Duan, Y. et al. Dosimetric comparison, treatment efficiency estimation, and biological evaluation of popular stereotactic radiosurgery options in treating single small brain metastasis. Front. Oncol. 11, 716152 (2021).
Shireman, J. M. et al. Genomic analysis of human brain metastases treated with stereotactic radiosurgery reveals unique signature based on treatment failure. iScience 27, 109601 (2024).
Bernhardt, D. et al. DEGRO practical guideline for central nervous system radiation necrosis part 2: treatment. Strahlenther. Onkol. 198, 971–980 (2022).
Bernhardt, D. et al. DEGRO practical guideline for central nervous system radiation necrosis part 1: classification and a multistep approach for diagnosis. Strahlenther. Onkol. 198, 873–883 (2022).
Martin, A. M. et al. Immunotherapy and symptomatic radiation necrosis in patients with brain metastases treated with stereotactic radiation. JAMA Oncol. 4, 1123–1124 (2018).
Minniti, G. et al. Stereotactic radiosurgery combined with nivolumab or Ipilimumab for patients with melanoma brain metastases: evaluation of brain control and toxicity. J. Immunother. Cancer 7, 102 (2019).
Chun, S. J. et al. Risk of radionecrosis in HER2-positive breast cancer with brain metastasis receiving trastuzumab emtansine (T-DM1) and brain stereotactic radiosurgery. Radiother. Oncol. 199, 110461 (2024).
Id Said, B. et al. Trastuzumab emtansine increases the risk of stereotactic radiosurgery-induced radionecrosis in HER2+ breast cancer. J. Neurooncol. 159, 177–183 (2022).
Stumpf, P. K. et al. Combination of trastuzumab emtansine and stereotactic radiosurgery results in high rates of clinically significant radionecrosis and dysregulation of aquaporin-4. Clin. Cancer Res. 25, 3946–3953 (2019).
Dagher, R. et al. Umbrella review and network meta-analysis of diagnostic imaging test accuracy studies in differentiating between brain tumor progression versus pseudoprogression and radionecrosis. J. Neurooncol. 166, 1–15 (2024).
Klausner, G. et al. Stereotactic radiation therapy for renal cell carcinoma brain metastases in the tyrosine kinase inhibitors era: outcomes of 120 patients. Clin. Genitourin. Cancer 17, 191–200 (2019).
Miller, J. A. et al. Association between radiation necrosis and tumor biology after stereotactic radiosurgery for brain metastasis. Int. J. Radiat. Oncol. Biol. Phys. 96, 1060–1069 (2016).
Lehrer, E. J. et al. Radiation necrosis in renal cell carcinoma brain metastases treated with checkpoint inhibitors and radiosurgery: an international multicenter study. Cancer 128, 1429–1438 (2022).
Mayo, Z. S., Billena, C., Suh, J. H., Lo, S. S. & Chao, S. T. The dilemma of radiation necrosis from diagnosis to treatment in the management of brain metastases. Neuro-Oncol. 26, S56–s65 (2024).
Lee, D., Riestenberg, R. A., Haskell-Mendoza, A. & Bloch, O. Brain metastasis recurrence versus radiation necrosis: evaluation and treatment. Neurosurg. Clin. N. Am. 31, 575–587 (2020).
Vellayappan, B. et al. A systematic review informing the management of symptomatic brain radiation necrosis after stereotactic radiosurgery and International Stereotactic Radiosurgery Society recommendations. Int. J. Radiat. Oncol. Biol. Phys. 118, 14–28 (2024).
Dequesada, I. M., Quisling, R. G., Yachnis, A. & Friedman, W. A. Can standard magnetic resonance imaging reliably distinguish recurrent tumor from radiation necrosis after radiosurgery for brain metastases? A radiographic-pathological study. Neurosurgery 63, 898–903 (2008).
Leeman, J. E. et al. Extent of perilesional edema differentiates radionecrosis from tumor recurrence following stereotactic radiosurgery for brain metastases. Neuro-Oncol. 15, 1732–1738 (2013).
Zhang, Z. et al. A predictive model for distinguishing radiation necrosis from tumour progression after gamma knife radiosurgery based on radiomic features from MR images. Eur. Radiol. 28, 2255–2263 (2018).
Bae, J. et al. Pretreatment spatially aware magnetic resonance imaging radiomics can predict distant brain metastases (DBMs) after stereotactic radiosurgery/radiation therapy (SRS/SRT). Adv. Radiat. Oncol. 9, 101457 (2024).
Basree, M. M. et al. Leveraging radiomics and machine learning to differentiate radiation necrosis from recurrence in patients with brain metastases. J. Neurooncol. 168, 307–316 (2024).
Mayo, Z. S. et al. Radiation necrosis or tumor progression? A review of the radiographic modalities used in the diagnosis of cerebral radiation necrosis. J. Neurooncol. 161, 23–31 (2023).
Muto, M. et al. Dynamic susceptibility contrast (DSC) perfusion MRI in differential diagnosis between radionecrosis and neoangiogenesis in cerebral metastases using rCBV, rCBF and K2. Radiol. Med. 123, 545–552 (2018).
Morabito, R. et al. DCE and DSC perfusion MRI diagnostic accuracy in the follow-up of primary and metastatic intra-axial brain tumors treated by radiosurgery with cyberknife. Radiat. Oncol. 14, 65 (2019).
Hoefnagels, F. W. et al. Radiological progression of cerebral metastases after radiosurgery: assessment of perfusion MRI for differentiating between necrosis and recurrence. J. Neurol. 256, 878–887 (2009).
Barajas, R. F. et al. Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following gamma knife radiosurgery using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. Am. J. Neuroradiol. 30, 367–372 (2009).
Aseel, A., McCarthy, P. & Mohammed, A. Brain magnetic resonance spectroscopy to differentiate recurrent neoplasm from radiation necrosis: A systematic review and meta-analysis. J. Neuroimaging 33, 189–201 (2023).
Chuang, M. T., Liu, Y. S., Tsai, Y. S., Chen, Y. C. & Wang, C. K. Differentiating radiation-induced necrosis from recurrent brain tumor using MR perfusion and spectroscopy: a meta-analysis. PLoS ONE 11, e0141438 (2016).
Chao, S. T., Suh, J. H., Raja, S., Lee, S. Y. & Barnett, G. The sensitivity and specificity of FDG PET in distinguishing recurrent brain tumor from radionecrosis in patients treated with stereotactic radiosurgery. Int. J. Cancer 96, 191–197 (2001).
Belohlávek, O., Simonová, G., Kantorová, I., Novotný, J. Jr. & Liscák, R. Brain metastases after stereotactic radiosurgery using the Leksell gamma knife: can FDG PET help to differentiate radionecrosis from tumour progression? Eur. J. Nucl. Med. Mol. Imaging 30, 96–100 (2003).
Hotta, M., Minamimoto, R. & Miwa, K. 11C-methionine-PET for differentiating recurrent brain tumor from radiation necrosis: radiomics approach with random forest classifier. Sci. Rep. 9, 15666 (2019).
Yomo, S. & Oguchi, K. Prospective study of (11)C-methionine PET for distinguishing between recurrent brain metastases and radiation necrosis: limitations of diagnostic accuracy and long-term results of salvage treatment. BMC Cancer 17, 713 (2017).
Cicone, F. et al. Accuracy of F-DOPA PET and perfusion-MRI for differentiating radionecrotic from progressive brain metastases after radiosurgery. Eur. J. Nucl. Med. Mol. Imaging 42, 103–111 (2015).
Cicone, F. et al. Long-term metabolic evolution of brain metastases with suspected radiation necrosis following stereotactic radiosurgery: longitudinal assessment by F-DOPA PET. Neuro-Oncol. 23, 1024–1034 (2021).
Meyer, H. S. et al. [(18)F]FET PET uptake indicates high tumor and low necrosis content in brain metastasis. Cancers 13, 355 (2021).
Galldiks, N. et al. PET imaging in patients with brain metastasis-report of the RANO/PET group. Neuro-Oncol. 21, 585–595 (2019).
Kotecha, R. et al. Neim-05 pursue: results from a prospective, phase 2b trial to define image interpretation criteria for (18)F-fluciclovine-pet for detection of recurrent brain metastases after radiation therapy. Neurooncol. Adv. 5, 15 (2023).
Beckers, C., Pruschy, M. & Vetrugno, I. Tumor hypoxia and radiotherapy: a major driver of resistance even for novel radiotherapy modalities. Semin. Cancer Biol. 98, 19–30 (2024).
Albarrán, V. et al. Negative association of steroids with immunotherapy efficacy in a multi-tumor cohort: time and dose-dependent. Cancer Immunol. Immunother. 73, 186 (2024).
Jessurun, C. A. C. et al. The combined use of steroids and immune checkpoint inhibitors in brain metastasis patients: a systematic review and meta-analysis. Neuro-Oncol. 23, 1261–1272 (2021).
Upadhyay, R. et al. Initial report of Boswellia serrata for management of cerebral radiation necrosis after stereotactic radiosurgery for brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 117, S172–S173 (2023).
Barnett G. et al. Position statement on MR-guided laser interstitial thermal therapy (LITT) for brain tumors and radiation necrosis. American Association of Neurological Surgeons and Congress of Neurological Surgeons (2021).
Bastos, D. C. D. A. et al. Laser interstitial thermal therapy in the treatment of brain metastases and radiation necrosis. Cancer Lett. 489, 9–18 (2020).
Rammo, R. et al. The safety of magnetic resonance imaging-guided laser interstitial thermal therapy for cerebral radiation necrosis. J. Neurooncol. 138, 609–617 (2018).
Ahluwalia, M. et al. Laser ablation after stereotactic radiosurgery: a multicenter prospective study in patients with metastatic brain tumors and radiation necrosis. J. Neurosurg. 130, 804–811 (2018).
Chan, M. et al. Efficacy of laser interstitial thermal therapy for biopsy-proven radiation necrosis in radiographically recurrent brain metastases. Neurooncol. Adv. 5, vdad031 (2023).
Ginalis, E. E. & Danish, S. F. Magnetic resonance-guided laser interstitial thermal therapy for brain tumors in geriatric patients. Neurosurg. Focus 49, E12 (2020).
Jensdottir, M., Sandvik, U., Fagerlund, M. & Bartek, J. Jr. Laser interstitial thermal therapy using the Leksell Stereotactic System and a diagnostic MRI suite: how I do it. Acta Neurochir. 165, 549–554 (2023).
Haskell-Mendoza, A. P. et al. The LITT Fit in neuro-oncology: indications, imaging, and adjunctive therapies. J. Neurooncol. 172, 1–11 (2025).
Chen, C., Guo, Y., Chen, Y., Li, Y. & Chen, J. The efficacy of laser interstitial thermal therapy for brain metastases with in-field recurrence following SRS: systemic review and meta-analysis. Int. J. Hyperth. 38, 273–281 (2021).
Redmond, K. J. et al. Stereotactic radiosurgery for postoperative metastatic surgical cavities: a critical review and International Stereotactic Radiosurgery Society (ISRS) practice guidelines. Int. J. Radiat. Oncol. Biol. Phys. 111, 68–80 (2021).
McKay, W. H. et al. Repeat stereotactic radiosurgery as salvage therapy for locally recurrent brain metastases previously treated with radiosurgery. J. Neurosurg. 127, 148–156 (2017).
Eitz, K. A. et al. Multi-institutional analysis of prognostic factors and outcomes after hypofractionated stereotactic radiotherapy to the resection cavity in patients with brain metastases. JAMA Oncol. 6, 1901–1909, (2020).
Teyateeti, A., Brown, P. D., Mahajan, A., Laack, N. N. & Pollock, B. E. Outcome comparison of patients who develop leptomeningeal disease or distant brain recurrence after brain metastases resection cavity radiosurgery. Neurooncol. Adv. 3, vdab036 (2021).
Prabhu, R. S. et al. Leptomeningeal disease and neurologic death after surgical resection and radiosurgery for brain metastases: a multi-institutional analysis. Adv. Radiat. Oncol. 6, 100644 (2021).
Prabhu, R. S. et al. A multi-institutional analysis of presentation and outcomes for leptomeningeal disease recurrence after surgical resection and radiosurgery for brain metastases. Neuro-Oncol. 21, 1049–1059 (2019).
Dankner, M. et al. Invasive growth associated with cold-inducible RNA-binding protein expression drives recurrence of surgically resected brain metastases. Neuro-Oncol. 23, 1470–1480 (2021).
Cagney, D. N. et al. Association of neurosurgical resection with development of pachymeningeal seeding in patients with brain metastases. JAMA Oncol. 5, 703–709 (2019).
Ozair, A. et al. Leptomeningeal metastatic disease: new frontiers and future directions. Nat. Rev. Clin. Oncol. 22, 134–154 (2025).
Patel, K. R. et al. Comparing preoperative with postoperative stereotactic radiosurgery for resectable brain metastases: a multi-institutional analysis. Neurosurgery 79, 279–285 (2016).
Nguyen, T. K. et al. Predictors of leptomeningeal disease following hypofractionated stereotactic radiotherapy for intact and resected brain metastases. Neuro-Oncol. 22, 84–93 (2020).
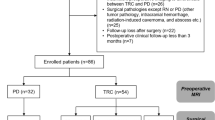
Prabhu, R. S. et al. Risk factors for progression and toxic effects after preoperative stereotactic radiosurgery for patients with resected brain metastases. JAMA Oncol. 9, 1066–1073, (2023).
Prabhu, R. S. et al. Preoperative radiosurgery for resected brain metastases: the PROPS-BM multicenter cohort study. Int. J. Radiat. Oncol. Biol. Phys. 111, 764–772 (2021).
Jansen, C. S. et al. Pre-operative stereotactic radiosurgery and peri-operative dexamethasone for resectable brain metastases: a two-arm pilot study evaluating clinical outcomes and immunological correlates. Nat. Commun. 15, 8854 (2024).
Fiagbedzi, E., Hasford, F. & Tagoe, S. N. Impact of planning target volume margins in stereotactic radiosurgery for brain metastasis: a review. Prog. Med. Phys. 35, 1–9 (2024).
Soliman, H. et al. Consensus contouring guidelines for postoperative completely resected cavity stereotactic radiosurgery for brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 100, 436–442 (2018).
Acker, G. et al. What if: a retrospective reconstruction of resection cavity stereotactic radiosurgery to mimic neoadjuvant stereotactic radiosurgery. Front. Oncol. 13, 1056330 (2023).
Kirkpatrick, J. P. et al. Defining the optimal planning target volume in image-guided stereotactic radiosurgery of brain metastases: results of a randomized trial. Int. J. Radiat. Oncol. Biol. Phys. 91, 100–108 (2015).
Singh, R. et al. The impact of margin expansions on local control and radionecrosis following stereotactic radiosurgery for brain metastases: a systematic review and meta-analysis. Pract. Radiat. Oncol. https://doi.org/10.1016/j.prro.2025.01.012 (2025).
Cheok, S. K. et al. Comparison of preoperative versus postoperative treatment dosimetry plans of single-fraction stereotactic radiosurgery for surgically resected brain metastases. Neurosurg. Focus 55, E9 (2023).
Agrawal, N. et al. Preoperative stereotactic radiosurgery for patients with 1–4 brain metastases: a single-arm phase 2 trial outcome analysis (NCT03398694). Neurooncol. Pract. 11, 593–603 (2024).
Putz, F. et al. Quality requirements for MRI simulation in cranial stereotactic radiotherapy: a guideline from the German Taskforce ‘Imaging in Stereotactic Radiotherapy’. Strahlenther. Onkol. 200, 1–18 (2024).
Kutuk, T. et al. Impact of MRI timing on tumor volume and anatomic displacement for brain metastases undergoing stereotactic radiosurgery. Neurooncol. Pract. 8, 674–683 (2021).
Roth O’Brien, D. A. et al. Time to administration of stereotactic radiosurgery to the cavity after surgery for brain metastases: a real-world analysis. J. Neurosurg. 135, 1695–1705 (2021).
Atalar, B. et al. Cavity volume dynamics after resection of brain metastases and timing of postresection cavity stereotactic radiosurgery. Neurosurgery 72, 180–185 (2013).
Jarvis, L. A. et al. Tumor bed dynamics after surgical resection of brain metastases: implications for postoperative radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 84, 943–948 (2012).
Ahmed, S. et al. Change in postsurgical cavity size within the first 30 days correlates with extent of surrounding edema: consequences for postoperative radiosurgery. J. Comput. Assist. Tomogr. 38, 457–460 (2014).
Tan, H. et al. Inter-fraction dynamics during post-operative 5 fraction cavity hypofractionated stereotactic radiotherapy with a MR LINAC: a prospective serial imaging study. J. Neurooncol. 156, 569–577 (2022).
Edwards, D. M. & Kim, M. M. Effective personalization of stereotactic radiosurgery for brain metastases in the modern era: opportunities for innovation. Cancer J. 30, 393–400 (2024).
Navarria, P. et al. P03.12. A phase III randomized trial comparing preoperative hypofractionated radiosurgery (HSRS) to postoperative hypofractionated radiosurgery (HSRS) for patients with large brain metastases suitable for surgical resection support trial. Neuro-Oncol. 25, ii39 (2023).
Sharma, P. et al. Immune checkpoint therapy-current perspectives and future directions. Cell 186, 1652–1669 (2023).
Long, G. V. et al. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: a multicentre randomised phase 2 study. Lancet Oncol. 19, 672–681 (2018).
Long, G. V. et al. Ipilimumab plus nivolumab versus nivolumab alone in patients with melanoma brain metastases (ABC): 7-year follow-up of a multicentre, open-label, randomised, phase 2 study. Lancet Oncol. https://doi.org/10.1016/s1470-2045(24)00735-6 (2025).
Tawbi, H. A. et al. Long-term outcomes of patients with active melanoma brain metastases treated with combination nivolumab plus ipilimumab (CheckMate 204): final results of an open-label, multicentre, phase 2 study. Lancet Oncol. 22, 1692–1704 (2021).
Powell, S. F. et al. Outcomes with pembrolizumab plus platinum-based chemotherapy for patients with NSCLC and stable brain metastases: pooled analysis of KEYNOTE-021, -189, and -407. J. Thorac. Oncol. 16, 1883–1892 (2021).
Sharabi, A. B., Lim, M., DeWeese, T. L. & Drake, C. G. Radiation and checkpoint blockade immunotherapy: radiosensitisation and potential mechanisms of synergy. Lancet Oncol. 16, e498–e509 (2015).
Lugade, A. A. et al. Radiation-induced IFN-γ production within the tumor microenvironment influences antitumor immunity. J. Immunol. 180, 3132–3139 (2008).
Yoo, K. H. et al. Optimizing the synergy between stereotactic radiosurgery and immunotherapy for brain metastases. Front. Oncol. 13, 1223599 (2023).
Schreurs, L. D. et al. The immune landscape in brain metastasis. Neuro-Oncol. 27, 50–62 (2025).
Klemm, F. et al. Interrogation of the microenvironmental landscape in brain tumors reveals disease-specific alterations of immune cells. Cell 181, 1643–1660 e1617 (2020).
Vanpouille-Box, C. et al. DNA exonuclease Trex1 regulates radiotherapy-induced tumour immunogenicity. Nat. Commun. 8, 15618 (2017).
Hudson, W. H., Olson, J. J. & Sudmeier, L. J. Immune microenvironment remodeling after radiation of a progressing brain metastasis. Cell Rep. Med. 4, 101054 (2023).
Demaria, S. et al. Immune-mediated inhibition of metastases after treatment with local radiation and CTLA-4 blockade in a mouse model of breast cancer. Clin. Cancer Res. 11, 728–734 (2005).
Dewan, M. Z. et al. Fractionated but not single-dose radiotherapy induces an immune-mediated abscopal effect when combined with anti-CTLA-4 antibody fractionated radiation synergizes with immunotherapy. Clin. Cancer Res. 15, 5379–5388 (2009).
Shabason, J. E. & Minn, A. J. Radiation and immune checkpoint blockade: from bench to clinic. Semin. Radiat. Oncol. 27, 289–298 (2017).
Buchwald, Z. S. et al. Radiation, immune checkpoint blockade and the abscopal effect: a critical review on timing, dose and fractionation. Front. Oncol. 8, 612 (2018).
Dovedi, S. J. et al. Acquired resistance to fractionated radiotherapy can be overcome by concurrent PD-L1 blockade. Cancer Res. 74, 5458–5468 (2014).
Niesel, K. et al. The immune suppressive microenvironment affects efficacy of radio-immunotherapy in brain metastasis. EMBO Mol. Med. 13, e13412 (2021).
Pomeranz Krummel, D. A. et al. Impact of sequencing radiation therapy and immune checkpoint inhibitors in the treatment of melanoma brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 108, 157–163 (2020).
Randall Patrinely, J. Jr. et al. A multicenter analysis of immune checkpoint inhibitors as adjuvant therapy following treatment of isolated brain metastasis. Oncologist 26, e505–e507 (2021).
Lehrer, E. J. et al. Stereotactic radiosurgery and immune checkpoint inhibitors in the management of brain metastases. Int. J. Mol. Sci. 19, 3054 (2018).
Amaral, T. et al. Combined immunotherapy with nivolumab and ipilimumab with and without local therapy in patients with melanoma brain metastasis: a DeCOG* study in 380 patients. J. Immunother. Cancer https://doi.org/10.1136/jitc-2019-000333 (2020).
Dohm, A. E. et al. Clinical outcomes of non-small cell lung cancer brain metastases treated with stereotactic radiosurgery and immune checkpoint inhibitors, EGFR tyrosine kinase inhibitors, chemotherapy and immune checkpoint inhibitors, or chemotherapy alone. J. Neurosurg. 138, 1600–1607 (2023).
Martins, F. et al. The combination of stereotactic radiosurgery with immune checkpoint inhibition or targeted therapy in melanoma patients with brain metastases: a retrospective study. J. Neurooncol. 146, 181–193 (2020).
Chen, L. et al. Concurrent immune checkpoint inhibitors and stereotactic radiosurgery for brain metastases in non-small cell lung cancer, melanoma, and renal cell carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 100, 916–925 (2018).
Kotecha, R. et al. The impact of sequencing PD-1/PD-L1 inhibitors and stereotactic radiosurgery for patients with brain metastasis. Neuro-Oncol. 21, 1060–1068 (2019).
Qian, J. M., Yu, J. B., Kluger, H. M. & Chiang, V. L. Timing and type of immune checkpoint therapy affect the early radiographic response of melanoma brain metastases to stereotactic radiosurgery. Cancer 122, 3051–3058 (2016).
Minniti, G. et al. Leptomeningeal disease and brain control after postoperative stereotactic radiosurgery with or without immunotherapy for resected brain metastases. J. Immunother. Cancer https://doi.org/10.1136/jitc-2021-003730 (2021).
Lehrer, E. J. et al. Imaging-defined necrosis after treatment with single-fraction stereotactic radiosurgery and immune checkpoint inhibitors and its potential association with improved outcomes in patients with brain metastases: an international multicenter study of 697 patients. J. Neurosurg. 138, 1178–1187 (2023).
Jessurun, C. A. C. et al. Hyperprogression of brain metastases following initiation of immune checkpoint inhibitors. J. Neurooncol. https://doi.org/10.1007/s11060-025-04955-9 (2025).
Wong, P. et al. Phase II multicenter trial combining nivolumab and radiosurgery for NSCLC and RCC brain metastases. Neurooncol. Adv. 5, vdad018 (2023).
Williams, N. L. et al. Phase 1 study of ipilimumab combined with whole brain radiation therapy or radiosurgery for melanoma patients with brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 99, 22–30 (2017).
Dohopolski, M. et al. Exploratory evaluation of personalized ultrafractionated stereotactic adaptive radiation therapy (PULSAR) with central nervous system-active drugs in brain metastases treatment. Int. J. Radiat. Oncol. Biol. Phys. https://doi.org/10.1016/j.ijrobp.2024.11.067 (2024).
Bellur, S. et al. Management of brain metastases: a review of novel therapies. Semin. Neurol. 43, 845–858 (2023).
Mair, M. J. et al. Understanding the activity of antibody-drug conjugates in primary and secondary brain tumours. Nat. Rev. Clin. Oncol. 20, 372–389 (2023).
Pan, K. et al. Emerging therapeutics and evolving assessment criteria for intracranial metastases in patients with oncogene-driven non-small-cell lung cancer. Nat. Rev. Clin. Oncol. 20, 716–732 (2023).
Wu, Y. L. et al. CNS efficacy of osimertinib in patients with T790M-positive advanced non-small-cell lung cancer: data from a randomized phase III trial (AURA3). J. Clin. Oncol. 36, 2702–2709 (2018).
Jänne, P. A. et al. CNS efficacy of osimertinib with or without chemotherapy in epidermal growth factor receptor-mutated advanced non-small-cell lung cancer. J. Clin. Oncol. 42, 808–820 (2024).
Gadgeel, S. et al. Alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive (ALK+) non-small-cell lung cancer: CNS efficacy results from the ALEX study. Ann. Oncol. 29, 2214–2222 (2018).
Shaw, A. T. et al. First-line lorlatinib or crizotinib in advanced ALK-positive lung cancer. N. Engl. J. Med. 383, 2018–2029 (2020).
Solomon, B. J. et al. Post hoc analysis of lorlatinib intracranial efficacy and safety in patients with. J. Clin. Oncol. 40, 3593–3602 (2022).
Solomon, B. J. et al. Lorlatinib versus crizotinib in patients with advanced ALK-positive non-small cell lung cancer: 5-year outcomes from phathe se III CROWN study. J. Clin. Oncol. 42, 3400–3409 (2024).
Michels, S. et al. Overall survival and central nervous system activity of crizotinib in ROS1-rearranged lung cancer-final results of the EUCROSS trial. ESMO Open 9, 102237 (2024).
Drilon, A. et al. Entrectinib in ROS1 fusion-positive non-small-cell lung cancer: integrated analysis of three phase 1–2 trials. Lancet Oncol. 21, 261–270 (2020).
Subbiah, V. et al. Intracranial efficacy of selpercatinib in RET fusion-positive non-small cell lung cancers on the LIBRETTO-001 trial. Clin. Cancer Res. 27, 4160–4167 (2021).
Cheng, Y. et al. Intracranial activity of selpercatinib in Chinese patients with advanced RET fusion-positive non-small-cell lung cancer in the phase II LIBRETTO-321 trial. JCO Precis. Oncol. 7, e2200708 (2023).
Davies, M. A. et al. Dabrafenib plus trametinib in patients with BRAF(V600)-mutant melanoma brain metastases (COMBI-MB): a multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol. 18, 863–873 (2017).
Hirsch, L. et al. Clinical activity and safety of cabozantinib for brain metastases in patients with renal cell carcinoma. JAMA Oncol. 7, 1815–1823, (2021).
Negrier, S. et al. Cabozantinib in patients (pts) with non-locally pretreated brain metastases (BM) from renal cell carcinoma (RCC): results of the multicenter CABRAMET phase II trial (NCT03967522). J. Clin. Oncol. 43, 533–533 (2025).
Murthy, R. K. et al. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N. Engl. J. Med. 382, 597–609 (2020).
Lin, N. U. et al. Tucatinib vs placebo, both in combination with trastuzumab and capecitabine, for previously treated ERBB2 (HER2)-positive metastatic breast cancer in patients with brain metastases: updated exploratory analysis of the HER2CLIMB randomized clinical trial. JAMA Oncol. 9, 197–205 (2023).
Pérez-García, J. M. et al. Trastuzumab deruxtecan in patients with central nervous system involvement from HER2-positive breast cancer: the DEBBRAH trial. Neuro-Oncol. 25, 157–166 (2023).
Niikura, N. et al. Treatment with trastuzumab deruxtecan in patients with HER2-positive breast cancer and brain metastases and/or leptomeningeal disease (ROSET-BM). npj Breast Cancer 9, 82 (2023).
Jerusalem, G. et al. Trastuzumab deruxtecan in HER2-positive metastatic breast cancer patients with brain metastases: a DESTINY-Breast01 subgroup analysis. Cancer Discov. 12, 2754–2762 (2022).
Hurvitz, S. A. et al. Trastuzumab deruxtecan versus trastuzumab emtansine in patients with HER2-positive metastatic breast cancer: updated results from DESTINY-Breast03, a randomised, open-label, phase 3 trial. Lancet 401, 105–117 (2023).
Bartsch, R. et al. Trastuzumab deruxtecan in HER2-positive breast cancer with brain metastases: a single-arm, phase 2 trial. Nat. Med. 28, 1840–1847 (2022).
Soffietti, R. et al. Diagnosis and treatment of brain metastases from solid tumors: guidelines from the European Association of Neuro-oncology (EANO). Neuro-Oncol. 19, 162–174 (2017).
Langston, J. et al. CNS downstaging: an emerging treatment paradigm for extensive brain metastases in oncogene-addicted lung cancer. Lung Cancer 178, 103–107 (2023).
Adua, S. J. et al. Brain metastatic outgrowth and osimertinib resistance are potentiated by RhoA in EGFR-mutant lung cancer. Nat. Commun. 13, 7690 (2022).
Alexander, B. M. et al. Brain Malignancy Steering Committee clinical trials planning workshop: report from the Targeted Therapies working group. Neuro-Oncol. 17, 180–188 (2015).
Camidge, D. R. et al. Clinical trial design for systemic agents in patients with brain metastases from solid tumours: a guideline by the Response Assessment in Neuro-Oncology Brain Metastases working group. Lancet Oncol. 19, e20–e32 (2018).
Pike, L. R. G. et al. Tyrosine kinase inhibitors with and without up-front stereotactic radiosurgery for brain metastases from EGFR and ALK oncogene-driven non-small cell lung cancer (TURBO-NSCLC). J. Clin. Oncol. https://doi.org/10.1200/jco.23.02668 (2024).
Tozuka, T. et al. Osimertinib plus local treatment for brain metastases versus osimertinib alone in patients with EGFR-mutant non-small cell lung cancer. Lung Cancer 191, 107540 (2024).
Montemurro, F. et al. Trastuzumab emtansine (T-DM1) in patients with HER2-positive metastatic breast cancer and brain metastases: exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trial☆. Ann. Oncol. 31, 1350–1358 (2020).
Carlson, J. A. et al. Trastuzumab emtansine and stereotactic radiosurgery: an unexpected increase in clinically significant brain edema. Neuro-Oncol. 16, 1006–1009 (2014).
Lebow, E. S. et al. Symptomatic necrosis with antibody-drug conjugates and concurrent stereotactic radiotherapy for brain metastases. JAMA Oncol. 9, 1729–1733 (2023).
Khatri, V. M. et al. Multi-institutional report of trastuzumab deruxtecan and stereotactic radiosurgery for HER2 positive and HER2-low breast cancer brain metastases. npj Breast Cancer 10, 100 (2024).
Debbi, K. et al. Safety and efficacy of combined trastuzumab-deruxtecan and concurrent radiation therapy in breast cancer. The TENDANCE multicentric French study. Breast 80, 104421 (2025).
Patel, K. R. et al. BRAF inhibitor and stereotactic radiosurgery is associated with an increased risk of radiation necrosis. Melanoma Res. 26, 387–394 (2016).
Dohm, A. E. et al. Stereotactic radiosurgery and anti-PD-1 + CTLA-4 therapy, anti-PD-1 therapy, anti-CTLA-4 therapy, BRAF/MEK inhibitors, BRAF inhibitors, or conventional chemotherapy for the management of melanoma brain metastases. Eur. J. Cancer 192, 113287 (2023).
Kotecha, R. et al. Melanoma brain metastasis: the impact of stereotactic radiosurgery, BRAF mutational status, and targeted and/or immune-based therapies on treatment outcome. J. Neurosurg. 129, 50–59 (2018).
Ahmed, K. A. et al. Clinical outcomes of melanoma brain metastases treated with stereotactic radiosurgery and anti-PD-1 therapy, anti-CTLA-4 therapy, BRAF/MEK inhibitors, BRAF inhibitor, or conventional chemotherapy. Ann. Oncol. 27, 2288–2294 (2016).
Hecht, M. et al. Radiosensitization by BRAF inhibitor therapy-mechanism and frequency of toxicity in melanoma patients. Ann. Oncol. 26, 1238–1244 (2015).
Yan, M. et al. Hypofractionated stereotactic radiosurgery (HSRS) as a salvage treatment for brain metastases failing prior stereotactic radiosurgery (SRS). J. Neurooncol. 162, 119–128 (2023).
Hung, J. S. et al. Is it advisable to perform radiosurgery for EGFR-TKI-controlled brain metastases? A retrospective study of the role of radiosurgery in lung cancer treatment. J. Neurooncol. 164, 413–422 (2023).
Scott, J. G. et al. A genome-based model for adjusting radiotherapy dose (GARD): a retrospective, cohort-based study. Lancet Oncol. 18, 202–211 (2017).
Corbett, K. et al. Central nervous system-specific outcomes of phase 3 randomized clinical trials in patients with advanced breast cancer, lung cancer, and melanoma. JAMA Oncol. 7, 1062–1064 (2021).
US Food and Drug Administration. FDA–NBTS public workshop: product development for central nervous system (CNS) metastases. FDA (2019).
Acknowledgements
The authors acknowledge the contributions of T. Wang, medical illustrator at the University of Maryland School of Medicine, to the drafting of Figs. 1–4. A.O. acknowledges support through the Bagley Research Fellowship from the Department of Neurosurgery at the University of Maryland School of Medicine.
Author information
Authors and Affiliations
Contributions
A.M., D.B., A.O., H.W. and E.M. researched data for the article. A.M., A.O., P.D.B. and R.K. contributed substantially to discussion of the content. A.M., D.B., A.O., H.W., E.M. and W.H. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
D.K. declares institutional grant funding from Neuropoint Alliance; and is named on US Patent 11,253,726: Method to select radiation dosage for tumour treatment based on cellular imaging. L.D.L. has acted as a consultant for Insightec and holds stock in Elekta. G.M. has received honoraria for seminars from Accuray and BrainLAB. J.L. has received funding support for clinical trials from Bristol Myer Squibb. P.Y.W. has received research support from AstraZeneca, Black Diamond, Bristol Myers Squibb, Chimerix, Eli Lily, Erasca, Global Coalition for Adaptive Research, Kazia Therapeutics, MediciNova, Merck, Novartis, Quadriga, Servier and VBI Vaccines; and consultancy fees from Anheart, AstraZeneca, Black Diamond, Celularity, Chimerix, Day One Bio, Genenta, GSK, Kintara, Merck, Mundipharma, Novartis, Novocure, Prelude Therapeutics, Sagimet, Sapience, Servier, Symbio, Tango, Telix and VBI Vaccines. R.K. has received honoraria from Accuray, BrainLAB, Castle Biosciences, Elekta, Elsevier, Ion Beam Applications, Kazia Therapeutics, Novocure and ViewRay; and institutional research funding from AstraZeneca, Blue Earth Diagnostics, BrainLAB, Cantex Pharmaceuticals, Exelixis, GT Medical Technologies, Ion Beam Applications, Kazia Therapeutics, Medtronic, Novocure and ViewRay. G.F.W. has received funding support for clinical trials from Insightec and the Keep Punching Foundation. P.D.B. has received honoraria from UpToDate. A.S. has acted as a consultant for Abbvie, BrainLAB, Elekta (Gamma Knife Icon), Merck, Roche and Varian; has received honorarium for educational seminars from Accuray, AstraZeneca, BrainLAB, Elekta, Seagen and Varian; research grants from BrainLAB, Elekta, Seagen and Varian; travel accommodations/expenses from BrainLAB, Elekta and Varian; and is also a Clinical Steering Committee Member of the Elekta MR-Linac Research Consortium and chairs the Elekta Oligometastases Group and the Elekta Gamma Knife Icon Group. M.S.A. has received research grants from AstraZeneca, Bayer, Bristol Myers Squibb, Incyte, Merck, Mimivax, Novocure and Pharmacyclics; consultancy fees from Allovir, Anheart Therapeutics, Apollomics, Autem, Bayer, Cairn Therapeutics, Caris Lifesciences, Celularity, GSK, Insightec, Janssen, Kiyatec, Novocure, Nuvation, Prelude Therapeutics, Pyramid Biosciences, SDP Oncology, Theraguix, Tocagen, Varian Medical Systems, Viewray, Voyager Therapeutics and Xoft; is a scientific advisory board member for Cairn Therapeutics, Modifi Biosciences and Pyramid Biosciences; and holds stock in Cytodyn, MedInnovate Advisors and MimiVax. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Clinical Oncology thanks F. Moraes, B.S. Skeie and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Review criteria
This review utilizes data from landmark trials reported over the past two decades along with recent published literature (through database searches using appropriate combinations of search terms related to ‘brain metastasis’, ‘brain malignancies’, ‘SRS’, ‘stereotactic radiosurgery’, ‘radiotherapy’, ‘whole brain radiotherapy’, ‘WBRT’, ‘brain radiation’, ‘Gamma Knife’, ‘Cyber Knife’, ‘LINAC’) as well as works presented at the 2022, 2023 and 2024 annual meetings of the Society for Neuro-Oncology (SNO), American Society for Radiation Oncology (ASTRO), American Society for Clinical Oncology (ASCO), and the SNO/ASCO Annual Conferences on CNS Clinical Trials and Brain Metastases. References were also curated from major reviews in the field as well as guideline publications from professional societies. Clinical trials pertaining to brain metastases were also reviewed from ClinicalTrials.gov (accessed 20 September 2024). The final reference list was refined by a multidisciplinary panel with expertise in radiation oncology, medical oncology, neuro-oncology, neurosurgery, neuroradiology and clinical trial design.
Supplementary information
Glossary
- Adverse radiation events (AREs)
-
are any negative adverse effects or complications arising secondary to radiotherapy, which affect non-tumour tissues and organs near the treatment site, can occur during or following treatment and range in severity. AREs reflecting necrosis or leaky blood vessels resulting in oedema are sometimes referred to as radiation necrosis or radionecrosis or radiation-induced contrast enhancement.
- Beam modulation
-
refers to the technique of varying the intensity and shape of radiation beams as they are delivered to the patient. This enables more precise targeting of the tumour while minimizing exposure and thus damage to surrounding non-tumour tissues.
- Biologically effective dose (BED)
-
is a measure that quantifies the biological effect of a given dose of radiation, taking into account the dose per fraction and the total dose delivered, relative to the tissue-specific sensitivity to radiation.
- Clinical target volume (CTV)
-
as defined broadly, is the volume of tissue that contains the gross tumour volume visible on imaging, along with a potential margin of surrounding tissue potentially invaded by malignant cells. For whole-brain radiotherapy, the CTV is typically the entire brain. With stereotactic radiosurgery for small intact lesions, the CTV is the same as gross tumour volume on imaging as microscopic spread is considered minimal.
- Co-planar beams
-
refer to multiple radiation beams that are directed from different angles but lie within the same plane. This technique is used to ensure uniform dose distribution across the target area while sparing surrounding non-tumour tissues.
- Gross tumour volume
-
is the volume of the tumour that is clearly visible on imaging, typically a fine-cut contrast-enhanced T1-weighted MRI for SRS targeting intact lesions.
- Isocentres
-
are crucial in radiotherapy planning as the focal points of radiation beam intersection, around which the gantry, the treatment couch and the collimators all rotate to ensure accurate tumour targeting.
- Isodose
-
refers to lines on a radiation treatment plan that connect points receiving the same dose of radiation. These lines help visualize the distribution of radiation within the target area and surrounding tissues, facilitating treatment planning.
- Planning target volume (PTV)
-
includes the clinical target volume plus a margin of surrounding tissue (such as an added 1–2 mm for stereotactic radiosurgery or 3–5 mm for whole-brain radiotherapy — referred to as the PTV expansion) to account for variations in lesion size, shape and position, relative to the radiotherapy beam.
- Simultaneous-integrated boost techniques
-
involve delivering different doses of radiation to different areas of the tumour simultaneously within a single treatment session. This approach enables higher doses to be targeted at the tumour while sparing surrounding non-tumour tissues, potentially improving treatment efficacy and reducing overall treatment time.
- Stereotactic radiosurgery (SRS)
-
is a highly conformal radiation therapy approach that is predicated on the ability to immobilize the target organ for precise targeting of radiation beams. The skull being a fixed and rigid space is an ideal region for SRS, as there is minimal motion during therapy.
- Tumour treating fields (TTFields)
-
is a novel treatment modality involving non-invasive delivery of low-intensity, intermediate-frequency alternating electrical fields, typically via several electrodes placed on the scalp — ideally near the tumour — for brain metastases, to disrupt the ability of cancer cells to grow and divide.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mansouri, A., Ozair, A., Bhanja, D. et al. Stereotactic radiosurgery for patients with brain metastases: current principles, expanding indications and opportunities for multidisciplinary care. Nat Rev Clin Oncol 22, 327–347 (2025). https://doi.org/10.1038/s41571-025-01013-1
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41571-025-01013-1
This article is cited by
-
A systematic review of stereotactic radiosurgery for pituitary metastases
Journal of Neuro-Oncology (2026)
-
Epidemiology and survival of adolescent and young adults with brain metastases compared to older adults
Journal of Neuro-Oncology (2026)
-
Gamma knife radiosurgery for cerebellar brain metastases: clinical outcomes and artificial intelligence-based predictive modeling
Clinical & Experimental Metastasis (2026)
-
Evaluation of clinical and volumetric outcomes following adaptive gamma knife radiosurgery for brain metastases
Journal of Neuro-Oncology (2025)