Abstract
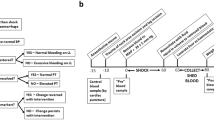
Uncontrolled haemorrhage is a major preventable cause of death in patients with traumatic injury. Trauma-induced coagulopathy (TIC) describes abnormal coagulation processes that are attributable to trauma. In the early hours of TIC development, hypocoagulability is typically present, resulting in bleeding, whereas later TIC is characterized by a hypercoagulable state associated with venous thromboembolism and multiple organ failure. Several pathophysiological mechanisms underlie TIC; tissue injury and shock synergistically provoke endothelial, immune system, platelet and clotting activation, which are accentuated by the ‘lethal triad’ (coagulopathy, hypothermia and acidosis). Traumatic brain injury also has a distinct role in TIC. Haemostatic abnormalities include fibrinogen depletion, inadequate thrombin generation, impaired platelet function and dysregulated fibrinolysis. Laboratory diagnosis is based on coagulation abnormalities detected by conventional or viscoelastic haemostatic assays; however, it does not always match the clinical condition. Management priorities are stopping blood loss and reversing shock by restoring circulating blood volume, to prevent or reduce the risk of worsening TIC. Various blood products can be used in resuscitation; however, there is no international agreement on the optimal composition of transfusion components. Tranexamic acid is used in pre-hospital settings selectively in the USA and more widely in Europe and other locations. Survivors of TIC experience high rates of morbidity, which affects short-term and long-term quality of life and functional outcome.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others

Change history
22 April 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41572-022-00360-y
References
World Health Organization. Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016 (WHO, 2018).
Tisherman, S. A. et al. Detailed description of all deaths in both the shock and traumatic brain injury hypertonic saline trials of the Resuscitation Outcomes Consortium. Ann. Surg. 261, 586–590 (2015).
Eastridge, B. J. et al. Death on the battlefield (2001-2011): implications for the future of combat casualty care. J. Trauma Acute Care Surg. 73, S431–S437 (2012).
Fox, E. E. et al. Earlier endpoints are required for hemorrhagic shock trials among severely injured patients. Shock. 47, 567–573 (2017).
Moore, H. B. et al. Plasma-first resuscitation to treat haemorrhagic shock during emergency ground transportation in an urban area: a randomised trial. Lancet 392, 283–291 (2018). This randomized controlled trial shows that pre-hospital plasma in a ground ambulance system does not improve survival in seriously injured patients.
Sperry, J. L. et al. Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock. N. Engl. J. Med. 379, 315–326 (2018). This randomized controlled trial shows that pre-hospital plasma during helicopter transport improves survival in seriously injured patients.
Sauaia A., Moore E. E., Wade C., Holcomb J. B. in Trauma Induced Coagulopathy 2nd edn (eds Moore H. B., Neal M. D. & Moore E. E.) 13-27 (Springer, 2021).
Kalkwarf, K. J. et al. Bleeding to death in a big city: an analysis of all trauma deaths from hemorrhage in a metropolitan area over one year. J. Trauma Acute Care Surg. 89, 716–722 (2020).
Moore, H. B. et al. Hyperfibrinolysis, physiologic fibrinolysis, and fibrinolysis shutdown: the spectrum of postinjury fibrinolysis and relevance to antifibrinolytic therapy. J. Trauma Acute Care Surg. 77, 811–817 (2014). Distinct phenotypes of fibrinolysis were identified by thromboelastography, indicating increased mortality for both hyperfibrinolysis and fibrinolysis shutdown.
Macfarlane, R. G. & Biggs, R. Fibrinolysis; its mechanism and significance. Blood 3, 1167–1187 (1948).
Innes, D. & Sevitt, S. Coagulation and fibrinolysis in injured patients. J. Clin. Pathol. 17, 1–13 (1964).
Kashuk, J. L., Moore, E. E., Millikan, J. S. & Moore, J. B. Major abdominal vascular trauma–a unified approach. J. Trauma 22, 672–679 (1982). The first clinical study to propose the ‘lethal triad’ as a unifying mechanism for hypocoagulable TIC.
Morton, A. P. et al. Revisiting early postinjury mortality: are they bleeding because they are dying or dying because they are bleeding? J. Surg. Res. 179, 5–9 (2013). This clinical review highlights the challenge of determining whether a critically injured patient is dying because the patient has acquired TIC or TIC reflects irreversible metabolic failure.
Chang, R. et al. Abnormalities of laboratory coagulation tests versus clinically evident coagulopathic bleeding: results from the prehospital resuscitation on helicopters study (PROHS). Surgery. 163, 819–826 (2018).
Moore E. & Moore H. in Trauma Induced Coagulopathy 2nd edn (ed. Moore H. B. Moore, E. E. & Neal M. D.) 3-11(Springer 2020).
Gando, S., Levi, M. & Toh, C. H. Disseminated intravascular coagulation. Nat. Rev. Dis. Prim. 2, 16037 (2016).
Moore, H. B. et al. Defining trauma-induced coagulopathy with respect to future implications for patient management: communication from the SSC of the ISTH. J. Thromb. Haemost. 18, 740–747 (2020). The ISTH developed a consensus statement that outlines the key differences between TIC and DIC; DIC is well described in association with sepsis.
Coleman J. J., et al. Whole blood thrombin generation is impaired in injured patients requiring a massive transfusion. J. Am. Coll. Surg. https://doi.org/10.1016/j.jamcollsurg.2020.12.058 (2021).Together with Cardenas et al. (J. Trauma Acute Care Surg., 2014), this study shows that thrombin generation, measured in plasma or whole blood, is impaired in injured patients requiring a massive transfusion.
Sobrino, J. & Shafi, S. Timing and causes of death after injuries. Proceedings 26, 120–123 (2013).
Sauaia, A. et al. Epidemiology of trauma deaths: a reassessment. J. Trauma. 38, 185–193 (1995).
CRASH-2 Collaborators. The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. Lancet 377, 1096–1101 (2011).
Kahl, J. E. et al. The changing nature of death on the trauma service. J. Trauma Acute Care Surg. 75, 195–201 (2013).
Shackford, S. R. et al. The epidemiology of traumatic death. A population-based analysis. Arch. Surg. 128, 571–575 (1993).
Callcut, R. A. et al. The why and how our trauma patients die: a prospective multicenter Western Trauma Association study. J. Trauma Acute Care Surg. 86, 864–870 (2019).
Evans, J. A. et al. Epidemiology of traumatic deaths: comprehensive population-based assessment. World J. Surg. 34, 158–163 (2010).
Soreide, K. et al. Epidemiology and contemporary patterns of trauma deaths: changing place, similar pace, older face. World J. Surg. 31, 2092–2103 (2007).
Oyeniyi, B. T. et al. Trends in 1029 trauma deaths at a level 1 trauma center: impact of a bleeding control bundle of care. Injury 48, 5–12 (2017).
Teixeira, P. G. R. et al. Preventable or potentially preventable mortality at a mature trauma center. J. Trauma Acute Care Surg. 63, 1338–1347 (2007).
Brohi, K., Singh, J., Heron, M. & Coats, T. Acute traumatic coagulopathy. J. Trauma Acute Care Surg. 54, 1127–1130 (2003). Together with MacLeod et al. (2003), this article documents evidence of TIC in 25% of injured patients arriving at the hospital prior to resuscitation.
Roberts, D. J. et al. One thousand consecutive in-hospital deaths following severe injury: has the etiology of traumatic inpatient death changed in Canada? Can. J. Surg. 61, 150–152 (2018).
Arslan, E. D. et al. Assessment of traumatic deaths in a level one trauma center in Ankara, Turkey. Eur. J. Trauma Emerg. Surg. 41, 319–323 (2015).
Trajano, A. D., Pereira, B. M. & Fraga, G. P. Epidemiology of in-hospital trauma deaths in a Brazilian university hospital. BMC Emerg. Med. 14, 22 (2014).
Kleber, C. et al. Overall distribution of trauma-related deaths in Berlin 2010: advancement or stagnation of German trauma management? World J. Surg. 36, 2125–2130 (2012).
Jochems, D., Leenen, L. P. H., Hietbrink, F., Houwert, R. M. & van Wessem, K. J. P. Increased reduction in exsanguination rates leaves brain injury as the only major cause of death in blunt trauma. Injury 49, 1661–1667 (2018).
Drake, S. A. et al. Establishing a regional trauma preventable/potentially preventable death rate. Ann. Surg. 271, 375–382 (2018).
Koh, E. Y. et al. Trends in potentially preventable trauma deaths between 2005-2006 and 2012-2013. Am. J. Surg. 218, 501–506 (2019).
Brenner, A. et al. Outcome measures in clinical trials of treatments for acute severe haemorrhage. Trials 19, 533 (2018).
Holcomb, J. B. et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA 313, 471–482 (2015). This randomized controlled trial did not detect a difference in survival employing a transfusion strategy of 1:1:1 ratio versus a 1:1:2 ratio of plasma to platelets to RBCs, but more patients in the 1:1:1 group achieved haemostasis and fewer experienced death due to exsanguination by 24 hours.
Gonzalez, E. et al. Goal-directed hemostatic resuscitation of trauma-induced coagulopathy: a pragmatic randomized clinical trial comparing a viscoelastic assay to conventional coagulation assays. Ann. Surg. 263, 1051–1059 (2016). This randomized controlled trial indicates improved survival when blood products are delivered to seriously injured patients on the basis of thromboelastography compared with conventional coagulation testing.
Roberts, I. et al. The CRASH-2 trial: a randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health Technol. Assess. 17, 1–79 (2013).
Moore, E. E. et al. Human polymerized hemoglobin for the treatment of hemorrhagic shock when blood is unavailable: the USA multicenter trial. J. Am. Coll. Surg. 208, 1–13 (2009).
Holcomb, J. B. et al. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 148, 127–136 (2013).
Holcomb, J. B. et al. Evidence based and clinically relevant outcomes for hemorrhage control trauma trials. Ann. Surg. 273, 395–401 (2021).
Strumwasser, A. et al. The impact of acute coagulopathy on mortality in pediatric trauma patients. J. Trauma Acute Care Surg. 81, 312–318 (2016).
Wafaisade, A. et al. Acute coagulopathy in isolated blunt traumatic brain injury. Neurocriti. Care 12, 211–219 (2010).
Peltan, I. D., Vande Vusse, L. K., Maier, R. V. & Watkins, T. R. An international normalized ratio-based definition of acute traumatic coagulopathy is associated with mortality, venous thromboembolism, and multiple organ failure after injury. Crit. Care Med. 43, 1429–1438 (2015).
Frith, D. et al. Definition and drivers of acute traumatic coagulopathy: clinical and experimental investigations. J. Thromb. Haemost. 8, 1919–1925 (2010).
Niles, S. E. et al. Increased mortality associated with the early coagulopathy of trauma in combat casualties. J. Trauma 64, 1459–1463; discussion 1463–1465 (2008).
Kutcher, M. E. et al. Evolving beyond the vicious triad: differential mediation of traumatic coagulopathy by injury, shock, and resuscitation. J. Trauma Acute Care Surg. 78, 516–523 (2015).
Maegele, M. et al. Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8724 patients. Injury. 38, 298–304 (2007).
Brohi, K. et al. Acute traumatic coagulopathy: initiated by hypoperfusion: modulated through the protein C pathway? Ann. Surg. 245, 812–818 (2007). This provocative report describes the potential role of activated protein C in the pathogenesis of TIC.
Cohen, M. J. et al. Early coagulopathy after traumatic brain injury: the role of hypoperfusion and the protein C pathway. J. trauma. 63, 1254–1261; discussion 1261–1262 (2007).
Moore, H. B. et al. Forgot calcium? Admission ionized-calcium in two civilian randomized controlled trials of pre-hospital plasma for traumatic hemorrhagic shock. J. Trauma Acute Care Surg. 88, 588–596 (2020).
Ditzel, R. M. Jr. et al. A review of transfusion- and trauma-induced hypocalcemia: is it time to change the lethal triad to the lethal diamond? J. Trauma Acute Care Surg. 88, 434–439 (2020).
van ‘t Veer, C. & Mann, K. G. Regulation of tissue factor initiated thrombin generation by the stoichiometric inhibitors tissue factor pathway inhibitor, antithrombin-III, and heparin cofactor-II. J. Biol. Chem. 272, 4367–4377 (1997).
Hoffman, M. & Monroe, D. M. III A cell-based model of hemostasis. Thromb. Haemost. 85, 958–965 (2001). The seminal work that introduced the novel concept of the essential role of cellular elements in clot formation.
Li, Z., Delaney, M. K., O’Brien, K. A. & Du, X. Signaling during platelet adhesion and activation. Arterioscler. Thromb. Vasc. Biol. 30, 2341–2349 (2010).
Rossaint, R. et al. Key issues in advanced bleeding care in trauma. Shock 26, 322–331 (2006).
Martini, W. Z., Pusateri, A. E., Uscilowicz, J. M., Delgado, A. V. & Holcomb, J. B. Independent contributions of hypothermia and acidosis to coagulopathy in swine. J. Trauma 58, 1002–1009; discussion 1009–1010 (2005).
Engström, M., Schött, U., Romner, B. & Reinstrup, P. Acidosis impairs the coagulation: a thromboelastographic study. J. Trauma 61, 624–628 (2006).
Martini, W. Z. & Holcomb, J. B. Acidosis and coagulopathy: the differential effects on fibrinogen synthesis and breakdown in pigs. Ann. Surg. 246, 831–835 (2007).
Lier, H., Krep, H., Schroeder, S. & Stuber, F. Preconditions of hemostasis in trauma: a review. The influence of acidosis, hypocalcemia, anemia, and hypothermia on functional hemostasis in trauma. J. Trauma. 65, 951–960 (2008).
Mitrophanov, A. Y., Szlam, F., Sniecinski, R. M., Levy, J. H. & Reifman, J. Controlled multifactorial coagulopathy: effects of dilution, hypothermia, and acidosis on thrombin generation in vitro. Anesth. Analg. 130, 1063–1076 (2020).
Marumo, M., Suehiro, A., Kakishita, E., Groschner, K. & Wakabayashi, I. Extracellular pH affects platelet aggregation associated with modulation of store-operated Ca2+ entry. Thromb. Res. 104, 353–360 (2001).
Meng, Z. H., Wolberg, A. S., Monroe, D. M. III & Hoffman, M. The effect of temperature and pH on the activity of factor VIIa: implications for the efficacy of high-dose factor VIIa in hypothermic and acidotic patients. J. Trauma. 55, 886–891 (2003).
Butler F. K., Jr., et al. Advanced resuscitative care in tactical combat casualty care: TCCC guidelines change 18-01:14 October 2018. J. Spec. Oper. Med.18:37-55.
Magnotti, L. J. et al. Admission ionized calcium levels predict the need for multiple transfusions: a prospective study of 591 critically ill trauma patients. J. Trauma. 70, 391–395; discussion 395–397 (2011).
Wolberg, A. S., Meng, Z. H., Monroe, D. M. III & Hoffman, M. A systematic evaluation of the effect of temperature on coagulation enzyme activity and platelet function. J. Trauma Acute Care Surg. 56, 1221–1228 (2004).
Kashuk, J. L. et al. Postinjury life threatening coagulopathy: is 1:1 fresh frozen plasma:packed red blood cells the answer? J. Trauma. 65, 261–270; discussion 270–271 (2008).
Tauber, H. et al. Prevalence and impact of abnormal ROTEM® assays in severe blunt trauma: results of the ‘Diagnosis and Treatment of Trauma-Induced Coagulopathy (DIA-TRE-TIC) study’. Br. J. Anaesth. 107, 378–387 (2011).
Thorn, S., Lefering, R., Maegele, M., Gruen, R. L. & Mitra, B. Early prediction of acute traumatic coagulopathy: a validation of the COAST score using the German Trauma Registry. Eur. J. Trauma Emerg. Surg. https://doi.org/10.1007/s00068-019-01142-0 (2019).
Cap, A. & Hunt, B. Acute traumatic coagulopathy. Curr. Opin. Crit. Care 20, 638–645 (2014).
Cohen, M. J. et al. Critical role of activated protein C in early coagulopathy and later organ failure, infection and death in trauma patients. Ann. Surg. 255, 379–385 (2012).
Cap, A. & Hunt, B. J. The pathogenesis of traumatic coagulopathy. Anaesthesia. 70, 96–101 (2015).
Peltz, E. D. et al. Pathologic metabolism: an exploratory study of the plasma metabolome of critical injury. J. Trauma Acute Care Surg. 78, 742–751 (2015).
White, N. J. et al. Post-translational oxidative modification of fibrinogen is associated with coagulopathy after traumatic injury. Free Radic. Biol. Med. 96, 181–189 (2016).
Weisel, J. W. & Litvinov, R. I. Mechanisms of fibrin polymerization and clinical implications. Blood. 121, 1712–1719 (2013).
Steele, T., Kolamunnage-Dona, R., Downey, C., Toh, C. H. & Welters, I. Assessment and clinical course of hypocalcemia in critical illness. Crit. Care 17, R106 (2013).
Hardaway, R. M. & Mc, K. D. Intravascular thrombi and the intestinal factor of irreversible shock. Ann. Surg. 150, 261–265 (1959).
Vulliamy, P. et al. Alterations in platelet behavior after major trauma: adaptive or maladaptive? Platelets 32, 295–304 (2020). This review reflects our current understanding of adaptive and maladaptive alterations in platelet biology induced by severe trauma, and identifies existing knowledge gaps as well as their therapeutic implications.
Gando, S. Tissue factor in trauma and organ dysfunction. Semin. Thromb. Hemost. 32, 48–53 (2006).
MacLeod, J. B., Lynn, M., McKenney, M. G., Cohn, S. M. & Murtha, M. Early coagulopathy predicts mortality in trauma. J. trauma. 55, 39–44 (2003).
Neal, M. D. The great platelet paradox: evolution of platelet contribution to hemostasis, inflammation, and thrombosis after injury. Blood Adv. 4, 2556 (2020).
Maegele, M. et al. Coagulopathy and haemorrhagic progression in traumatic brain injury: advances in mechanisms, diagnosis, and management. Lancet Neurol. 16, 630–647 (2017).
Zhang, J., Zhang, F. & Dong, J. F. Coagulopathy induced by traumatic brain injury: systemic manifestation of a localized injury. Blood 131, 2001–2006 (2018).
Moore, H. B. et al. Hemolysis exacerbates hyperfibrinolysis, whereas platelolysis shuts down fibrinolysis: evolving concepts of the spectrum of fibrinolysis in response to severe injury. Shock 43, 39–46 (2015).
Deguchi, H. et al. Prothrombotic skeletal muscle myosin directly enhances prothrombin activation by binding factors Xa and Va. Blood 128, 1870–1878 (2016).
Dyer, M. R. et al. Platelet-derived extracellular vesicles released after trauma promote hemostasis and contribute to DVT in mice. J. Thromb. Haemost. 17, 1733–1745 (2019).
Vulliamy, P. et al. Histone H4 induces platelet ballooning and microparticle release during trauma hemorrhage. Proc. Natl Acad. Sci. USA 116, 17444–17449 (2019).
Kozar, R. A. & Pati, S. Syndecan-1 restitution by plasma after hemorrhagic shock. J. Trauma Acute Care Surg. 78, S83–S86 (2015).
Simão, F. & Feener, E. P. The effects of the contact activation system on hemorrhage. Front. Med. 4, 121 (2017).
Johansson, P. I., Stensballe, J., Rasmussen, L. S. & Ostrowski, S. R. A high admission syndecan-1 level, a marker of endothelial glycocalyx degradation, is associated with inflammation, protein C depletion, fibrinolysis, and increased mortality in trauma patients. Ann. Surg. 254, 194–200 (2011).
Gonzalez Rodriguez, E. et al. Syndecan-1: a quantitative marker for the endotheliopathy of trauma. J. Am. Coll. Surg. 225, 419–427 (2017).
Ban, K. et al. Plasma-Mediated gut protection after hemorrhagic shock is lessened in syndecan-1−/− mice. Shock 44, 452–457 (2015).
Ostrowski, S. R. & Johansson, P. I. Endothelial glycocalyx degradation induces endogenous heparinization in patients with severe injury and early traumatic coagulopathy. J. Trauma Acute Care Surg. 73, 60–66 (2012).
Brohi, K. et al. Acute coagulopathy of trauma: hypoperfusion induces systemic anticoagulation and hyperfibrinolysis. J. Trauma 64, 1211–1217; discussion 1217 (2008).
Johansson, P. I. et al. High sCD40L levels early after trauma are associated with enhanced shock, sympathoadrenal activation, tissue and endothelial damage, coagulopathy and mortality. J. Thromb. Haemost. 10, 207–216 (2012).
Dyer, M. R. et al. Traumatic injury results in prolonged circulation of ultralarge von Willebrand factor and a reduction in ADAMTS13 activity. Transfusion 60, 1308–1318 (2020).
Kornblith, L. Z. et al. Perhaps it’s not the platelet: ristocetin uncovers the potential role of von Willebrand factor in impaired platelet aggregation following traumatic brain injury. J. Trauma Acute Care Surg. 85, 873–880 (2018).
Xu, X., Kozar, R., Zhang, J. & Dong, J.-F. Diverse activities of von Willebrand factor in traumatic brain injury and associated coagulopathy. J. Thromb. Haemost. 18, 3154–3162 (2020).
Pati, S. et al. Protective effects of fresh frozen plasma on vascular endothelial permeability, coagulation, and resuscitation after hemorrhagic shock are time dependent and diminish between days 0 and 5 after thaw. J. Trauma 69, S55–S63 (2010).
Kozar, R. A. et al. Plasma restoration of endothelial glycocalyx in a rodent model of hemorrhagic shock. Anesth. Analg. 112, 1289–1295 (2011). This study shows that plasma resuscitation of haemorrhagic shock restores the endothelial glycocalyx and alleviates trauma endotheliopathy.
Peng, Z. et al. Fresh frozen plasma lessens pulmonary endothelial inflammation and hyperpermeability after hemorrhagic shock and is associated with loss of syndecan 1. Shock 40, 195–202 (2013).
Haywood-Watson, R. J. et al. Modulation of syndecan-1 shedding after hemorrhagic shock and resuscitation. PLoS ONE 6, e23530 (2011).
Gruen, D. S. et al. Prehospital plasma is associated with distinct biomarker expression following injury. JCI Insight 5, e135350 (2020).
Fitzgerald, M. L., Wang, Z., Park, P. W., Murphy, G. & Bernfield, M. Shedding of syndecan-1 and -4 ectodomains is regulated by multiple signaling pathways and mediated by a TIMP-3-sensitive metalloproteinase. J. Cell Biol. 148, 811–824 (2000).
Prudovsky, I. et al. Tranexamic acid suppresses the release of mitochondrial DNA, protects the endothelial monolayer and enhances oxidative phosphorylation. J. Cell Physiol. 234, 19121–19129 (2019).
Diebel, M. E., Martin, J. V., Liberati, D. M. & Diebel, L. N. The temporal response and mechanism of action of tranexamic acid in endothelial glycocalyx degradation. J. Trauma Acute Care Surg. 84, 75–80 (2018).
Weyrich, A. S. & Zimmerman, G. A. Platelets: signaling cells in the immune continuum. Trends Immunol. 25, 489–495 (2004).
Rondina, M. T., Weyrich, A. S. & Zimmerman, G. A. Platelets as cellular effectors of inflammation in vascular diseases. Circ. Res. 112, 1506–1519 (2013).
Nachman, R. L. & Rafii, S. Platelets, petechiae, and preservation of the vascular wall. N. Engl. J. Med. 359, 1261–1270 (2008).
Kutcher, M. E. et al. Characterization of platelet dysfunction after trauma. J. Trauma Acute Care Surg. 73, 13–19 (2012). This seminal report characterizes platelet dysfunction in the majority of injured patients evident at the time of hospital presentation.
Tweardy, D. J. et al. Essential role for platelets in organ injury and inflammation in resuscitated hemorrhagic shock. Shock 26, 386–390 (2006).
Ding, N. et al. Toll-like receptor 4 regulates platelet function and contributes to coagulation abnormality and organ injury in hemorrhagic shock and resuscitation. Circ. Cardiovasc. Genet. 7, 615–624 (2014).
Brown, L. M., Call, M. S., Knudson, M. M. & Cohen, M. J., Trauma Outcomes Group. A normal platelet count may not be enough: the impact of admission platelet count on mortality and transfusion in severely injured trauma patients. J. Trauma 71, S337–S342 (2011).
Stansbury, L. G. et al. The clinical significance of platelet counts in the first 24 hours after severe injury. Transfusion 53, 783–789 (2013).
Kornblith, L. Z. et al. Fibrinogen and platelet contributions to clot formation: implications for trauma resuscitation and thromboprophylaxis. J. Trauma Acute Care Surg. 76, 255–256; discussion 262–263 (2014).
Zipperle, J. et al. Potential role of platelet-leukocyte aggregation in trauma-induced coagulopathy: ex vivo findings. J. Trauma Acute Care Surg. 82, 921–926 (2017).
Starr, N. E. et al. Identification of injury and shock driven effects on ex-vivo platelet aggregometry: a cautionary tale of phenotyping. J. Trauma Acute Care Surg. 89, 20–28 (2020).
Plautz, W. E. et al. Von Willebrand factor as a thrombotic and inflammatory mediator in critical illness. Transfusion 60, S158–S166 (2020).
Moore, H. B. et al. Shock induced systemic hyperfibrinolysis is attenuated by plasma first resuscitation. J. Trauma Acute Care Surg. 79, 897–903; discussion 903–904 (2015).
Kornblith, L. Z. et al. It’s about time: transfusion effects on postinjury platelet aggregation over time. J. Trauma Acute Care Surg. 87, 1042–1051 (2019).
Vulliamy, P. et al. Platelet transfusions reduce fibrinolysis but do not restore platelet function during trauma hemorrhage. J. Trauma Acute Care Surg. 83, 388–397 (2017).
Fields, A. T. et al. Good platelets gone bad: the effects of trauma patient plasma on healthy platelet aggregation. Shock 55, 189–197 (2021).
Nair, P. M., Pidcoke, H. F., Cap, A. P. & Ramasubramanian, A. K. Effect of cold storage on shear-induced platelet aggregation and clot strength. J. Trauma Acute Care Surg. 77, S88–S93 (2014).
Reddoch, K. M. et al. Hemostatic function of apheresis platelets stored at 4°C and 22°C. Shock 41, 54–61 (2014).
Kornblith, L. Z. et al. A journey upstream: fluctuating platelet-specific genes in cell free plasma as proof-of-concept for using RNA sequencing to improve understanding of post-injury platelet biology. J. Trauma Acute Care Surg. 88, 742–751 (2020).
Li, R., Elmongy, H., Sims, C. & Diamond, S. L. Ex vivo recapitulation of trauma-induced coagulopathy and preliminary assessment of trauma patient platelet function under flow using microfluidic technology. J. Trauma Acute Care Surg. 80, 440–449 (2016).
Colace, T. V., Jobson, J. & Diamond, S. L. Relipidated tissue factor linked to collagen surfaces potentiates platelet adhesion and fibrin formation in a microfluidic model of vessel injury. Bioconjug Chem. 22, 2104–2109 (2011).
Neeves, K. B. et al. Microfluidic focal thrombosis model for measuring murine platelet deposition and stability: PAR4 signaling enhances shear-resistance of platelet aggregates. J. Thromb. Haemost. 6, 2193–2201 (2008).
Vogel, S. et al. Platelet-derived HMGB1 is a critical mediator of thrombosis. J. Clin. Invest. 125, 4638–4654 (2015).
Dyer, M. R. et al. Deep vein thrombosis in mice is regulated by platelet HMGB1 through release of neutrophil-extracellular traps and DNA. Sci. Rep. 8, 2068 (2018).
Stark, K. et al. Disulfide HMGB1 derived from platelets coordinates venous thrombosis in mice. Blood. 128, 2435–2449 (2016).
Verni, C. C., Davila, A. Jr., Balian, S., Sims, C. A. & Diamond, S. L. Platelet dysfunction during trauma involves diverse signaling pathways and an inhibitory activity in patient-derived plasma. J. Trauma Acute Care Surg. 86, 250–259 (2019).
Lee, M. Y., Verni, C. C., Herbig, B. A. & Diamond, S. L. Soluble fibrin causes an acquired platelet glycoprotein VI signaling defect: implications for coagulopathy. J. Thromb. Haemost. 15, 2396–2407 (2017).
Butenas, S., van’t Veer, C. & Mann, K. G. “Normal” thrombin generation. Blood. 94, 2169–2178 (1999).
Park, M. S. et al. Thrombin generation profiles as predictors of symptomatic venous thromboembolism after trauma: a prospective cohort study. J. Trauma Acute Care Surg. 83, 381–387 (2017). This study shows that postinjury enhanced thrombin generation is a risk factor for venous thromboembolism.
Martini, W. Z. Coagulopathy by hypothermia and acidosis: mechanisms of thrombin generation and fibrinogen availability. J. Trauma 67, 202–208; discussion 208–209 (2009).
Floccard, B. et al. Early coagulopathy in trauma patients: an on-scene and hospital admission study. Injury 43, 26–32 (2012).
Rizoli, S. B. et al. Clotting factor deficiency in early trauma-associated coagulopathy. J. Trauma 71, S427–S434 (2011).
Woolley, T. et al. A prospective observational study of acute traumatic coagulopathy in traumatic bleeding from the battlefield. Transfusion 60, S52–S61 (2020).
Dzik, W. H. The James Blundell Award Lecture 2006: transfusion and the treatment of haemorrhage: past, present and future. Transfus. Med. 17, 367–374 (2007).
Dunbar, N. M. & Chandler, W. L. Thrombin generation in trauma patients. Transfusion 49, 2652–2660 (2009).
Negrier, C., Shima, M. & Hoffman, M. The central role of thrombin in bleeding disorders. Blood Rev. 38, 100582 (2019).
Cardenas, J. C. et al. Measuring thrombin generation as a tool for predicting hemostatic potential and transfusion requirements following trauma. J. Trauma Acute Care Surg. 77, 839–845 (2014).
Coleman, J. R. et al. Whole blood thrombin generation is distinct from plasma thrombin generation in healthy volunteers and after severe injury. Surgery 166, 1122–1127 (2019).
Mosesson, M. W. Fibrinogen and fibrin structure and functions. J. Thromb. Haemost. 3, 1894–1904 (2005).
Muszbek, L., Bereczky, Z., Bagoly, Z., Komaromi, I. & Katona, E. Factor XIII: a coagulation factor with multiple plasmatic and cellular functions. Physiol. Rev. 91, 931–972 (2011).
Kononova, O. et al. Mechanistic basis for the binding of RGD- and AGDV-peptides to the platelet integrin αIIbβ3. Biochemistry 56, 1932–1942 (2017).
Tennent, G. A. et al. Human plasma fibrinogen is synthesized in the liver. Blood. 109, 1971–1974 (2007).
Levy, J. H., Szlam, F., Tanaka, K. A. & Sniecienski, R. M. Fibrinogen and hemostasis: a primary hemostatic target for the management of acquired bleeding. Anesth. Analg. 114, 261–274 (2012).
Hiippala, S. T., Myllyla, G. J. & Vahtera, E. M. Hemostatic factors and replacement of major blood loss with plasma-poor red cell concentrates. Anesth. Analg. 81, 360–365 (1995).
Schlimp, C. J. & Schochl, H. The role of fibrinogen in trauma-induced coagulopathy. Hamostaseologie 34, 29–39 (2014). Fibrinogen is the first clotting factor to become depleted in the bleeding injured patient; based on this study, fibrinogen levels should be maintained at >150 mg/dl in bleeding patients.
Raza, I. et al. The incidence and magnitude of fibrinolytic activation in trauma patients. J. Thromb. Haemost. 11, 307–314 (2013).
Chapman, M. P. et al. Overwhelming tPA release, not PAI-1 degradation, is responsible for hyperfibrinolysis in severely injured trauma patients. J. Trauma Acute Care Surg. 80, 16–23; discussion 23–25 (2016). This study shows that hyperfibrinolysis seems to be due to extensive tPA release that overwhelms circulating PAI-1 levels.
Rourke, C. et al. Fibrinogen levels during trauma hemorrhage, response to replacement therapy, and association with patient outcomes. J. Thromb. Haemost. 10, 1342–1351 (2012).
McQuilten, Z. K., Wood, E. M., Bailey, M., Cameron, P. A. & Cooper, D. J. Fibrinogen is an independent predictor of mortality in major trauma patients: a five-year statewide cohort study. Injury 48, 1074–1081 (2017).
Inaba, K. et al. Impact of fibrinogen levels on outcomes after acute injury in patients requiring a massive transfusion. J. Am. Coll. Surg. 216, 290–297 (2013).
Cotton, B. A. et al. Hyperfibrinolysis at admission is an uncommon but highly lethal event associated with shock and prehospital fluid administration. J. Trauma Acute Care Surg. 73, 365–370; discussion 370 (2012).
Schochl, H., Frietsch, T., Pavelka, M. & Jambor, C. Hyperfibrinolysis after major trauma: differential diagnosis of lysis patterns and prognostic value of thrombelastometry. J. Trauma. 67, 125–131 (2009).
Moore, H. B. et al. Acute fibrinolysis shutdown after injury occurs frequently and increases mortality: a multicenter evaluation of 2,540 severely injured patients. J. Am. Coll. Surg. 222, 347–355 (2016).
Moore, H. B. et al. Does tranexamic acid improve clot strength in severely injured patients who have elevated fibrin degradation products and low fibrinolytic activity, measured by thrombelastography? J. Am. Coll. Surg. 229, 92–101 (2019).
Cardenas, J. C. et al. Elevated tissue plasminogen activator and reduced plasminogen activator inhibitor promote hyperfibrinolysis in trauma patients. Shock 41, 514–521 (2014).
Schillemans, M., Karampini, E., Kat, M. & Bierings, R. Exocytosis of Weibel-Palade bodies: how to unpack a vascular emergency kit. J. Thromb. Haemost. 17, 6–18 (2019).
Huber, D. et al. Tissue-type plasminogen activator (t-PA) is stored in Weibel-Palade bodies in human endothelial cells both in vitro and in vivo. Blood 99, 3637–3645 (2002).
Moore, H. B. et al. Fibrinolysis shutdown is associated with a fivefold increase in mortality in trauma patients lacking hypersensitivity to tissue plasminogen activator. J. Trauma acute care Surg. 83, 1014–1022 (2017).
Barrett, C. D. et al. Plasmin TEG rapidly identifies trauma patients at risk for massive transfusion, mortality and hyperfibrinolysis: a diagnostic tool to resolve an international debate on TXA? J. Trauma Acute Care Surg. 89, 991–998 (2020).
Moore, H. B. et al. Viscoelastic measurements of platelet function, not fibrinogen function, predicts sensitivity to tissue-type plasminogen activator in trauma patients. J. Thromb. Haemost. 13, 1878–1887 (2015).
Davenport, R. A. et al. Activated protein C drives the hyperfibrinolysis of acute traumatic coagulopathy. Anesthesiology. 126, 115–127 (2017).
Morrow, G. B., Whyte, C. S. & Mutch, N. J. Functional plasminogen activator inhibitor 1 is retained on the activated platelet membrane following platelet activation. Haematologica. 105, 2824–2833 (2019).
Bouma, B. N. & Mosnier, L. O. Thrombin activatable fibrinolysis inhibitor (TAFI) at the interface between coagulation and fibrinolysis. Pathophysiol. Haemost. Thromb. 33, 375–381 (2003).
Mutch, N. J. et al. Model thrombi formed under flow reveal the role of factor XIII-mediated cross-linking in resistance to fibrinolysis. J. Thromb. Haemost. 8, 2017–2024 (2010).
Fraser, S. R., Booth, N. A. & Mutch, N. J. The antifibrinolytic function of factor XIII is exclusively expressed through α2-antiplasmin cross-linking. Blood 117, 6371–6374 (2011).
Moore, H. B. et al. Reperfusion shutdown: delayed onset of fibrinolysis resistance after resuscitation from hemorrhagic shock is associated with increased circulating levels of plasminogen activator inhibitor-1 and postinjury complications. Blood 128, 206 (2016).
Chakrabarti, R., Hocking, E. D. & Fearnley, G. R. Reaction pattern to three stresses–electroplexy, surgery, and myocardial infarction–of fibrinolysis and plasma fibrinogen. J. Clin. Pathol. 22, 659–662 (1969).
Wright, F. L. et al. Fibrinolysis shutdown correlates to thromboembolic events in severe COVID-19 infection. JACS. 231, 193–203.e1 (2020).
Moore, H. B. et al. Fibrinolysis shutdown in trauma: historical review and clinical implications. Anesth Analg. 129, 762–773 (2019). Postinjury fibrinolysis shutdown has been documented recently with the advent of viscoelastic haemostatic assays, but has been recognized in experimental work for the past 50 years.
Gall, L. S. et al. The S100A10 pathway mediates an occult hyperfibrinolytic subtype in trauma patients. Ann. Surg. 269, 1184–1191 (2019).
Cardenas, J. C. et al. TEG lysis shutdown represents coagulopathy in bleeding trauma patients: analysis of the PROPPR cohort. Shock 51, 273–283 (2019).
Roberts, D. J. et al. Time course and outcomes associated with transient versus persistent fibrinolytic phenotypes after injury: a nested, prospective, multicenter cohort study. J. Trauma Acute Care Surg. 86, 206–213 (2019).
Meizoso, J. P. et al. Persistent fibrinolysis shutdown is associated with increased mortality in severely injured trauma patients. J. Am. Coll. Surg. 224, 575–582 (2017).
Leeper, C. M., Neal, M. D., McKenna, C. J. & Gaines, B. A. Trending fibrinolytic dysregulation: fibrinolysis shutdown in the days after injury is associated with poor outcome in severely injured children. Ann. Surg. 266, 508–515 (2017).
Barrett, C. D. et al. Human neutrophil elastase mediates fibrinolysis shutdown through competitive degradation of plasminogen and generation of angiostatin. J. Trauma. Acute Care Surg. 83, 1053–1061 (2017).
Gorton, H. J., Warren, E. R., Simpson, N. A., Lyons, G. R. & Columb, M. O. Thromboelastography identifies sex-related differences in coagulation. Anesth. Analg. 91, 1279–1281 (2000).
Haider, A. H. et al. Evidence of hormonal basis for improved survival among females with trauma-associated shock: an analysis of the National Trauma Data Bank. J. Trauma 69, 537–540 (2010).
Napolitano, L. M. et al. Gender differences in adverse outcomes after blunt trauma. J. Trauma 50, 274–280 (2001).
Brown, J. B. et al. Characterization of acute coagulopathy and sexual dimorphism after injury: females and coagulopathy just do not mix. J. Trauma Acute Care Surg. 73, 1395–1400 (2012).
Magnotti, L. J., Fischer, P. E., Zarzaur, B. L., Fabian, T. C. & Croce, M. A. Impact of gender on outcomes after blunt injury: a definitive analysis of more than 36,000 trauma patients. J. Am. Coll. Surg. 206, 984–991; discussion 991–992 (2008).
George, R. L. et al. Age-related gender differential in outcome after blunt or penetrating trauma. Shock 19, 28–32 (2003).
Wohltmann, C. D. et al. A multicenter evaluation of whether gender dimorphism affects survival after trauma. Am. J. Surg. 181, 297–300 (2001).
Croce, M. A., Fabian, T. C., Malhotra, A. K., Bee, T. K. & Miller, P. R. Does gender difference influence outcome? J. Trauma 53, 889–894 (2002).
Roach, R. E. J., Cannegieter, S. C. & Lijfering, W. M. Differential risks in men and women for first and recurrent venous thrombosis: the role of genes and environment. J. Thromb. Haemost. 12, 1593–1600 (2014).
Park, M. S. et al. Risk factors for venous thromboembolism after acute trauma: a population-based case-cohort study. Thromb. Res. 144, 40–45 (2016).
Knudson, M. M., Gomez, D., Haas, B., Cohen, M. J. & Nathens, A. B. Three thousand seven hundred thirty-eight posttraumatic pulmonary emboli: a new look at an old disease. Ann. Surg. 254, 625–632 (2011).
Berndtson, A. E., Costantini, T. W., Smith, A. M., Kobayashi, L. & Coimbra, R. Does sex matter? Effects on venous thromboembolism risk in screened trauma patients. J. Trauma Acute Care Surg. 81, 493–499 (2016).
Francis, J. L., Francis, D. A. & Gunathilagan, G. J. Assessment of hypercoagulability in patients with cancer using the Sonoclot analyzer and thromboelastography. Thromb. Res. 74, 335–346 (1994).
Farsetti, A. et al. Molecular basis of estrogen regulation of Hageman factor XII gene expression. Endocrinology 136, 5076–5083 (1995).
Sowers, M. R. et al. Hemostatic factors and estrogen during the menopausal transition. J. Clin. Endocrinol. Metab. 90, 5942–5948 (2005).
Knol, H. M., Kemperman, R. F., Kluin-Nelemans, H. C., Mulder, A. B. & Meijer, K. Haemostatic variables during normal menstrual cycle. A systematic review. Thromb. Haemost. 107, 22–29 (2012).
Coleman, J. R. et al. Trauma resuscitation consideration: sex matters. J. Am. Coll. Surg. 228, 760–768.e1 (2019).
Heldring, N. et al. Estrogen receptors: how do they signal and what are their targets. Physiol. Rev. 87, 905–931 (2007).
Coleman, J. R. et al. Untangling sex dimorphisms in coagulation: initial steps towards precision medicine for trauma resuscitation. Ann. Surg. 271, e128–e130 (2020).
Gee, A. C. et al. The influence of sex hormones on coagulation and inflammation in the trauma patient. Shock 29, 334–341 (2008).
Dupuis, M. et al. Effects of estrogens on platelets and megakaryocytes. Int. J. Mol. Sci. 20, 3111 (2019).
Haque, S. F. et al. Sex difference in platelet aggregation detected by new aggregometry using light scattering. Endocr. J. 48, 33–41 (2001).
Berlin, G., Hammar, M., Tapper, L. & Tynngård, N. Effects of age, gender and menstrual cycle on platelet function assessed by impedance aggregometry. Platelets 30, 473–479 (2019).
Teran, E., Escudero, C. & Vivero, S. Physiological changes in platelet aggregation and nitric oxide levels during menstrual cycle in healthy women. Nitric Oxide 7, 217–220 (2002).
Coleman, J. R. et al. Female platelets have distinct functional activity compared with male platelets: implications in transfusion practice and treatment of trauma-induced coagulopathy. J. Trauma Acute Care Surg. 87, 1052–1060 (2019).
Schreiber, M. A., Differding, J., Thorborg, P., Mayberry, J. C. & Mullins, R. J. Hypercoagulability is most prevalent early after injury and in female patients. J. Trauma 58, 475–480; discussion 480–481 (2005).
Borgman, M. A. et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J. Trauma 63, 805–813 (2007). This military study introduces the concept of a high ratio of plasma to RBCs for haemostatic resuscitation.
Meyer, D. E. et al. A comparison of resuscitation intensity and critical administration threshold in predicting early mortality among bleeding patients: a multicenter validation in 680 major transfusion patients. J. Trauma Acute Care Surg. 85, 691–696 (2018).
Savage, S. A. et al. The new metric to define large-volume hemorrhage: results of a prospective study of the critical administration threshold. J. Trauma Acute Care Surg. 78, 224–229; discussion 229–230 (2015).
Nunns, G. R. et al. Empiric transfusion strategies during life-threatening hemorrhage. Surgery 164, 306–311 (2018).
CRASH-2 Trial Collaborators. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet 376, 23–32 (2010). This randomized controlled trial of 20,211 injured patients conducted in 40 countries indicates a survival benefit of TXA when given <3 hours from injury.
Holcomb, J. B. et al. Admission rapid thrombelastography can replace conventional coagulation tests in the emergency department: experience with 1974 consecutive trauma patients. Ann. Surg. 256, 476–486 (2012).
Moore, H. B. et al. Viscoelastic tissue plasminogen activator challenge predicts massive transfusion in 15 minutes. J. Am. Coll. Surg. 225, 138–147 (2017).
Ives, C. et al. Hyperfibrinolysis elicited via thromboelastography predicts mortality in trauma. J. Am. Coll. Surg. 215, 496–502 (2012).
Kelly, J. M., Rizoli, S., Veigas, P., Hollands, S. & Min, A. Using rotational thromboelastometry clot firmness at 5 minutes (ROTEM((R)) EXTEM A5) to predict massive transfusion and in-hospital mortality in trauma: a retrospective analysis of 1146 patients. Anaesthesia 73, 1103–1109 (2018).
Neal, M. D. et al. Clinical assessment of trauma-induced coagulopathy and its contribution to postinjury mortality: a TACTIC proposal. J. Trauma Acute Care Surg. 79, 490–492 (2015).
Baksaas-Aasen, K. et al. Viscoelastic haemostatic assay augmented protocols for major trauma haemorrhage (ITACTIC): a randomized, controlled trial. Intensive Care Med. 47, 49–59 (2020).
Dias, J. D., Sauaia, A., Achneck, H. E., Hartmann, J. & Moore, E. E. Thromboelastography-guided therapy improves patient blood management and certain clinical outcomes in elective cardiac and liver surgery and emergency resuscitation: a systematic review and analysis. J. Thromb. Haemost. 17, 984–994 (2019).
McCully, S. P. et al. The international normalized ratio overestimates coagulopathy in stable trauma and surgical patients. J. Trauma Acute Care Surg. 75, 947–953 (2013).
Stettler, G. R. et al. Variability in international normalized ratio and activated partial thromboplastin time after injury are not explained by coagulation factor deficits. J. Trauma Acute Care Surg. 87, 582–589 (2019).
Prat, N. J. et al. Rotational thromboelastometry significantly optimizes transfusion practices for damage control resuscitation in combat casualties. J. Trauma Acute Care Surg. 83, 373–380 (2017). Implementation of ROTEM at a military base improved blood product use compared with an approach involving a fixed ratio of plasma to RBCs.
Kashuk, J. L. et al. Postinjury coagulopathy management: goal directed resuscitation via POC thrombelastography. Ann. Surg. 251, 604–614 (2010).
Cotton, B. A. et al. Rapid thrombelastography delivers real-time results that predict transfusion within 1 hour of admission. J. Trauma 71, 71:407–414; discussion 414–417 (2011).
Cotton, B. A. et al. Admission rapid thrombelastography predicts development of pulmonary embolism in trauma patients. J. Trauma Acute Care Surg. 72, 1470–1475; discussion 1475–1477 (2012).
Holbrook, T. L., Hoyt, D. B. & Anderson, J. P. The importance of gender on outcome after major trauma: functional and psychologic outcomes in women versus men. J. Trauma 50, 270–273 (2001).
Pezold, M. et al. Viscoelastic clot strength predicts coagulation-related mortality within 15 minutes. Surgery 151, 48–54 (2012).
Nystrup, K. B., Windelov, N. A., Thomsen, A. B. & Johansson, P. I. Reduced clot strength upon admission, evaluated by thrombelastography (TEG), in trauma patients is independently associated with increased 30-day mortality. Scand. J. Trauma. Resusc. Emerg. Med. 19, 52 (2011).
Plotkin, A. J. et al. A reduction in clot formation rate and strength assessed by thrombelastography is indicative of transfusion requirements in patients with penetrating injuries. J. Trauma 64, S64–S68 (2008).
Vigneshwar, N. et al. Precision medicine or one size does not fit all: clinical tolerance to hyperfibrinolysis differs by shock and injury severity. Ann. Surg. https://doi.org/10.1097/SLA.0000000000004548 (2020).
Kornblith, L. Z., Moore, H. B. & Cohen, M. J. Trauma-induced coagulopathy: the past, present, and future. J. Thromb. Haemost. 17, 852–862 (2019).
Leeper, C. M., Neal, M. D., McKenna, C., Sperry, J. L. & Gaines, B. A. Abnormalities in fibrinolysis at the time of admission are associated with deep vein thrombosis, mortality, and disability in a pediatric trauma population. J. Trauma Acute Care Surg. 82, 27–34 (2017).
Moore, H. B. & Moore, E. E. Temporal changes in fibrinolysis following injury. Semin. Thromb. Hemost. 46, 189–198 (2020).
Coleman, J. R. et al. It’s sooner than you think: blunt solid organ injury patients are already hypercoagulable upon hospital admission – results of a bi-institutional, prospective study. Am. J. Surg. 218, 1065–1073 (2019).
Chapman, B. C. et al. Hypercoagulability following blunt solid abdominal organ injury: when to initiate anticoagulation. Am. J. Surg. 206, 917–922; discussion 922–923 (2013).
Gary, J. L. et al. Can thrombelastography predict venous thromboembolic events in patients with severe extremity trauma? J. Orthop. Trauma 30, 294–298 (2016).
Sumislawski, J. J. et al. Not all in your head (and neck): stroke after blunt cerebrovascular injury is associated with systemic hypercoagulability. J. Trauma Acute Care Surg. 87, 1082–1087 (2019).
Holcomb, J. B. et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J. Trauma 62, 307–310 (2007).
Moore, E. E. Staged laparotomy for the hypothermia, acidosis, and coagulopathy syndrome. Am. J. Surg. 172, 405–410 (1996).
Stone, H. H., Strom, P. R. & Mullins, R. J. Management of the major coagulopathy with onset during laparotomy. Ann. Surg. 197, 532–535 (1983).
Spahn, D. R. et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit. Care 23, 98 (2019). These European guidelines reflect the currently most accepted protocol for the management of TIC, although there is some variation among western European countries. It brings a wealth of curated references on TIC mechanisms, diagnosis and treatment.
Goolsby, C. et al. Stop the Bleed Education Consortium: education program content and delivery recommendations. J. Trauma Acute Care Surg. 84, 205–210 (2018).
Rossaint, R. et al. The STOP the bleeding campaign. Crit. Care 17, 136 (2013).
Shaftan, G. W., Chiu, C. J., Dennis, C. & Harris, B. Fundamentals of physiologic control of arterial hemorrhage. Surgery 58, 851–856 (1965).
Moore, H. B. et al. Plasma is the physiologic buffer of tissue plasminogen activator-mediated fibrinolysis: rationale for plasma-first resuscitation after life-threatening hemorrhage. J. Am. Coll. Surg. 220, 872–879 (2015).
Neal, M. D. et al. Crystalloid to packed red blood cell transfusion ratio in the massively transfused patient: when a little goes a long way. J. Trauma Acute Care Surg. 72, 892–898 (2012).
Bickell, W. H. et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N. Engl. J. Med. 331, 1105–1109 (1994).
Pusateri, A. E. et al. Association of prehospital plasma transfusion with survival in trauma patients with hemorrhagic shock when transport times are longer than 20 minutes: a post hoc analysis of the PAMPer and COMBAT clinical trials. JAMA Surg. 155, e195085 (2019).
Nadler, R. et al. Early experience with transfusing low titer group O whole blood in the pre-hospital setting in Israel. Transfusion 60, S10–S16 (2020).
Leeper, C. M., Yazer, M. H. & Neal, M. D. Whole-blood resuscitation of injured patients: innovating from the past. JAMA Surg. 155, 771–772 (2020).
World Health Organization. Summary of the Report of the 18th Meeting of the WHO Expert Committee on the Selection and Use of Essential Medicines. https://www.who.int/selection_medicines/committees/TRS_web_summary.pdf (2021).
Guyette, F. X. et al. Tranexamic acid during prehospital transport in patients at risk for hemorrhage after injury: a double-blind, placebo-controlled, randomized clinical trial. JAMA Surg. 156, 11–20 (2020). This randomized controlled trial of pre-hospital TXA administered during air medical or ground transport of severely injured patients without TBI does not indicate improved survival, but shows that it is safe and improves survival in patients in severe shock.
Rowell, S. E. et al. Effect of out-of-hospital tranexamic acid vs placebo on 6-month functional neurologic outcomes in patients with moderate or severe traumatic brain injury. JAMA 324, 961–974 (2020). This randomized controlled trial of pre-hospital TXA for TBI does not indicate improved neurological recovery, although a subgroup receiving a dose of 2 g appeared to have improved survival.
Myers, S. P. et al. Tranexamic acid administration is associated with an increased risk of posttraumatic venous thromboembolism. J. Trauma Acute Care Surg. 86, 20–27 (2019).
Morrison, J. J., Dubose, J. J., Rasmussen, T. E. & Midwinter, M. J. Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) study. Arch. Surg. 147, 113–119 (2012).
Moore, E. E. et al. Rationale for the selective administration of tranexamic acid to inhibit fibrinolysis in the severely injured patient. Transfusion 56, S110–S114 (2016).
Moore, H. B. et al. Tranexamic acid is associated with increased mortality in patients with physiological fibrinolysis. J. Surg. Res. 220, 438–443 (2017).
Spinella, P. C. et al. The immunologic effect of early intravenous two and four gram bolus dosing of tranexamic acid compared to placebo in patients with severe traumatic bleeding (TAMPITI): a randomized, double-blind, placebo-controlled, single-center trial. Front. Immunol. 11, 2085 (2020).
Roberts, I. et al. Effects of a high-dose 24-h infusion of tranexamic acid on death and thromboembolic events in patients with acute gastrointestinal bleeding (HALT-IT): an international randomised, double-blind, placebo-controlled trial. Lancet 395, 1927–1936 (2020).
CRASH-3 Trial Collaborators. Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury (CRASH-3): a randomised, placebo-controlled trial. Lancet 394, 1713–1723 (2019).
Shakur, H. et al. Antifibrinolytic drugs for treating primary postpartum haemorrhage. Cochrane Database Syst. Rev. 2, CD012964 (2018).
Myers, S. P. & Neal, M. D. Venous thromboembolism after tranexamic acid administration: legitimate risk or statistical confounder? ANZ. J. Surg. 90, 425–426 (2020).
Etchill, E. et al. The confusion continues: results from an American Association for the Surgery of Trauma survey on massive transfusion practices among United States trauma centers. Transfusion 56, 2478–2486 (2016).
National Blood Authority. Patient blood management guidelines: module 1. Critical bleeding massive transfusion. https://www.blood.gov.au/system/files/documents/pbm-module1_0.pdf (2011).
American College of Surgeons. ACS TQIP massive transfusion in trauma guidelines. https://www.facs.org/-/media/files/quality-programs/trauma/tqip/transfusion_guildelines.ashx (2014).
Norfolk D. (ed.) Handbook of Transfusion Medicine 5th edn 82–87 (TSO, 2014).
Miyata, S. et al. Transfusion guidelines for patients with massive bleeding. Jpn. J. Transfus. Cell Ther. 65, 21–92 (2019).
Carney, N. et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery 80, 6–15 (2017).
Nevin, D. G. & Brohi, K. Permissive hypotension for active haemorrhage in trauma. Anaesthesia. 72, 1443–1448 (2017).
Holcomb, J. B. et al. Increased platelet:RBC ratios are associated with improved survival after massive transfusion. J. Trauma 71, S318–S328 (2011).
Itagaki, Y. et al. Early administration of fibrinogen concentrate is associated with improved survival among severe trauma patients: a single-centre propensity score-matched analysis. World J. Emerg. Surg. 15, 7 (2020).
Black, J. A., Pierce, V. S., Kerby, J. D. & Holcomb, J. B. The evolution of blood transfusion in the trauma patient: whole blood has come full circle. Semin. Thromb. Hemost. 46, 215–220 (2020).
Yazer, M. H. et al. Initial safety and feasibility of cold-stored uncrossmatched whole blood transfusion in civilian trauma patients. J. Trauma Acute Care Surg. 81, 21–26 (2016).
Shea, S. M. et al. The use of low-titer group O whole blood is independently associated with improved survival compared to component therapy in adults with severe traumatic hemorrhage. Transfusion 60 (Suppl 3), S2–S9 (2020).
Williams, J. et al. Safety profile and impact of low-titer group O whole blood for emergency use in trauma. J. Trauma Acute Care Surg. 88, 87–93 (2020).
Wilson, R. F., Spencer, A. R., Tyburski, J. G., Dolman, H. & Zimmerman, L. H. Bicarbonate therapy in severely acidotic trauma patients increases mortality. J. Trauma Acute Care Surg. 74, 45–50; discussion 50 (2013).
Corwin, G. S. et al. Characterization of acidosis in trauma patient. J. Emerg. Trauma. Shock 13, 213–218 (2020).
Moore, H. B. et al. Targeting resuscitation to normalization of coagulating status: hyper and hypocoagulability after severe injury are both associated with increased mortality. Am. J. Surg. 214, 1041–1045 (2017).
Einersen, P. M. et al. Rapid thrombelastography thresholds for goal-directed resuscitation of patients at risk for massive transfusion. J. Trauma Acute Care Surg. 82, 114–119 (2017).
Baksaas-Aasen, K. et al. Data-driven development of ROTEM and TEG algorithms for the management of trauma hemorrhage: a prospective observational multicenter study. Ann. Surg. 270, 1178–1185 (2019).
Stettler, G. R. et al. Rotational thromboelastometry thresholds for patients at risk for massive transfusion. J. Surg. Res. 228, 154–159 (2018).
Henriksen, H. H. et al. Impact of blood products on platelet function in patients with traumatic injuries: a translational study. J. Surg. Res. 214, 154–161 (2017).
Spano, P. J. II et al. Anticoagulant chemoprophylaxis in patients with traumatic brain injuries: a systematic review. J. Trauma Acute Care Surg. 88, 454–460 (2020).
Benjamin, E., Recinos, G., Aiolfi, A., Inaba, K. & Demetriades, D. Pharmacological thromboembolic prophylaxis in traumatic brain injuries: low molecular weight heparin is superior to unfractionated heparin. Ann. Surg. 266, 463–469 (2017).
Hecht, J. P. et al. Association of timing of initiation of pharmacologic venous thromboembolism prophylaxis with outcomes in trauma patients. J. Trauma Acute Care Surg. 90, 54–63 (2021).
Spyropoulos, A. C. et al. Scientific and Standardization Committee communication: clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J. Thromb. Haemost. 18, 1859–1865 (2020).
Haagsma, J. A. et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Injury Prev. 22, 3–18 (2016).
Holbrook, T. L. & Hoyt, D. B. The impact of major trauma: quality-of-life outcomes are worse in women than in men, independent of mechanism and injury severity. J. Trauma Acute Care Surg. 56, 284–290 (2004).
Holbrook, T. L., Anderson, J. P., Sieber, W. J., Browner, D. & Hoyt, D. B. Outcome after major trauma: 12-month and 18-month follow-up results from the Trauma Recovery Project. J. Trauma 46, 765–771; discussion 771–773 (1999).
Holbrook, T. L. et al. High rates of acute stress disorder impact quality-of-life outcomes in injured adolescents: mechanism and gender predict acute stress disorder risk. J. Trauma 59, 1126–1130 (2005).
Holbrook, T. L. et al. Long-term posttraumatic stress disorder persists after major trauma in adolescents: new data on risk factors and functional outcome. J. Trauma 58, 764–769; discussion 769–771 (2005).
Winthrop, A. L. et al. Quality of life and functional outcome after pediatric trauma. J. Trauma. Acute Care Surg. 58, 468–474 (2005).
Christensen, M. C., Banner, C., Lefering, R., Vallejo-Torres, L. & Morris, S. Quality of life after severe trauma: results from the global trauma trial with recombinant factor VII. J. Trauma 70, 1524–1531 (2011).
Mitra, B. et al. Long-term outcomes of patients receiving a massive transfusion after trauma. Shock 42, 307–312 (2014).
Mira, J. C. et al. The epidemiology of chronic critical illness after severe traumatic injury at two level one trauma centers. Crit. Care Med. 45, 1989–1996 (2017).
Stortz, J. A. et al. Evidence for persistent immune suppression in patients who develop chronic critical illness after sepsis. Shock 49, 249–258 (2018).
Gardner, A. K. et al. The development of chronic critical illness determines physical function, quality of life, and long-term survival among early survivors of sepsis in surgical ICUs. Crit. Care Med. 47, 566–573 (2019).
Shackford, S. R. et al. Determining the magnitude of surveillance bias in the assessment of lower extremity deep venous thrombosis: a prospective observational study of two centers. J. Trauma Acute Care Surg. 80, 734–739; discussion 740–741 (2016).
Coleman, J. J. et al. Factors associated with pulmonary embolism within 72 hours of admission after trauma: a multicenter study. J. Am. Coll. Surg. 220, 731–736 (2015).
Nastasi, A. J. et al. Characterizing the relationship between age and venous thromboembolism in adult trauma patients: findings from the National Trauma Data Bank and the National Inpatient Sample. J. Surg. Res. 216, 115–122 (2017).
Dietch, Z. C. et al. Rate of lower-extremity ultrasonography in trauma patients is associated with rate of deep venous thrombosis but not pulmonary embolism. Surgery 158, 379–385 (2015).
Stein, A. L. et al. Impact of a goal-directed factor-based coagulation management on thromboembolic events following major trauma. Scand. J. Trauma Resusc. Emerg. Med. 27, 117 (2019).
Paffrath, T. et al. Venous thromboembolism after severe trauma: incidence, risk factors and outcome. Injury. 41, 97–101 (2010).
Hutchison, T. N. et al. Venous thromboembolism during combat operations: a 10-y review. J. Surg. Res. 187, 625–630 (2014).
Holley, A. B., Petteys, S., Mitchell, J. D., Holley, P. R. & Collen, J. F. Thromboprophylaxis and VTE rates in soldiers wounded in Operation Enduring Freedom and Operation Iraqi Freedom. Chest 144, 966–973 (2013).
Lundy, J. B. et al. Frequency and relevance of acute peritraumatic pulmonary thrombus diagnosed by computed tomographic imaging in combat casualties. J. Trauma Acute Care Surg. 75, S215–S220 (2013).
Klok, F. A. et al. The post-PE syndrome: a new concept for chronic complications of pulmonary embolism. Blood Rev. 28, 221–226 (2014).
Pengo, V. et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N. Engl. J. Med. 350, 2257–2264 (2004).
Anderson, D. R. et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 3, 3898–3944 (2019).
Cannon, W. B. & Grabfield, G. P. Factors affecting the coagulation time of blood. Am. J. Physiol. 34, 232–242 (1914).
Stefanini, M. Basic mechanisms of hemostasis. Bull. N. Y. Acad. Med. 30, 239–277 (1954).
Kitchen, D. P., Kitchen, S., Jennings, I., Woods, T. & Walker, I. Quality assurance and quality control of thrombelastography and rotational thromboelastometry: the UK NEQAS for blood coagulation experience. Semin. Thromb. Hemost. 36, 757–763 (2010).
Takayama, W. et al. The impact of blood type O on mortality of severe trauma patients: a retrospective observational study. Crit. Care 22, 100 (2018).
Griffin, R. L., Jansen, J. O., Bosarge, P. L., Marques, M. B. & Kerby, J. D. The association between ABO blood type and mortality among severely injured trauma patients. Shock 54, 205–208 (2020).
Hamsen, U. et al. The influence of ABO blood group on mortality in major trauma. Orthop. Rev. 11, 8214 (2019).
Hoffman, M. & Cichon, L. J. H. Practical coagulation for the blood banker. Transfusion 53, 1594–1602 (2013).
Crawley, J. T., Zanardelli, S., Chion, C. K. & Lane, D. A. The central role of thrombin in hemostasis. J. Thromb. Haemost. 5, 95–101 (2007).
Gonzalez, E., Moore, E. E. & Moore, H. B. Management of trauma-induced coagulopathy with thrombelastography. Crit. Care Clin. 33, 119–134 (2017).
Veigas, P. V., Callum, J., Rizoli, S., Nascimento, B. & da Luz, L. T. A systematic review on the rotational thrombelastometry (ROTEM®) values for the diagnosis of coagulopathy, prediction and guidance of blood transfusion and prediction of mortality in trauma patients. Scand. J. Trauma. Resusc. Emerg. Med. 24, 114 (2016).
Harr, J. N. et al. Viscoelastic hemostatic fibrinogen assays detect fibrinolysis early. Eur. J. Trauma. Emerg. Surg. 41, 49–56 (2015).
Acknowledgements
E.E.M. and A.S. appreciate the generous support from the National Institutes of Health for their inflammation and coagulation research over the past 35 years (NIGMS: 1-6 P50 GM49222, 1-6 T32 GM08315, 1-2 U54 GM 62119, RM1 GM 131968 and NHLBI: UM1 HL120877). H.B.M. acknowledges the generous support from the National Institutes of Health (NHBLI: K99HL1518870) L.Z.K. acknowledges the generous support from the National Institutes of Health for her platelet biology research (NIGMS: K23GM130892-01). M.D.N. acknowledges the generous support by the National Institutes of Health (NIGMS: R35 GM119526 and NHLBI R01 HL141080).
Author information
Authors and Affiliations
Contributions
Introduction (all authors); Epidemiology (all authors); Mechanisms/pathophysiology (all authors); Diagnosis, screening and prevention (all authors); Management (all authors); Quality of life (all authors); Outlook (all authors); Overview of Primer (E.E.M.).
Corresponding author
Ethics declarations
Competing interests
E.E.M. currently receives research support from Haemonetics, Instrumentation Laboratory, Stago, Hemosonics, Diapharma, Prytime, Humacyte and Genentech; he is a co-founder of ThromboTherapeutics; he is listed as inventor on the following patents relating to blood coagulation or fibrinolysis (including assays): WO-2016073668-A1 (assignee: The Regents Of The University Of Colorado; status: published); US-9354243-B2 (assignee: Haemonetics Corporation, The Regents Of The University Of Colorado, A Body Corporate; status: granted); WO-2019014595-A1 (assignee: Thrombo Therapeutics, Inc.; status: published); EP-3215634-A1 (assignee: The Regents of the University of Colorado; status: published); EP-3303943-A1 (assignee: The Regents of The University of Colorado, A Body Corporate; status: published); WO-2021158799-A1 (assignee: The Regents Of The University Of Colorado, A Body Corporate; status: published); US-2020208194-A1 (assignee: Massachusetts Institute Of Technology, University Of Colorado; status: published). H.B.M. receives research support from Haemonetics and Instrumentation Laboratory; he is a co-founder of ThromboTherapeutics; he is listed as inventor on the following patents relating to blood coagulation or fibrinolysis (including assays): WO-2016073668-A1 (assignee: The Regents Of The University Of Colorado; status: published); WO-2019014595-A1 (assignee: Thrombo Therapeutics, Inc.; status: published); EP-3215634-A1 (assignee: The Regents of the University of Colorado; status: published); US-2020208194-A1 (assignee: Massachusetts Institute Of Technology, University Of Colorado; status: published). M.D.N. receives research support from Haemonetics, Janssen Pharmaceuticals, Accriva Diagnostics and Instrumentation Laboratory; he serves on the Scientific Advisory Board with equity stake in Haima Therapeutics. All other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks P. Cabrales, M. Levi, I. Marzi, S. Ostrowski, P. Spinella and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Glossary
- Potentially preventable deaths
-
The three criteria that must be present in a trauma-related death to qualify as potentially preventable are: the injury must have been survivable, the delivery of care was suboptimal, and the error in care must have been directly or indirectly implicated in the death of the patient.
- Bleeding control bundle-of-care
-
A series of measures to optimize bleeding control, including: accurate identification of the bleeding patient; damage control resuscitation; haemostatic techniques with tourniquets, pelvic binders or haemostatic dressings; resuscitative endovascular balloon occlusion of the aorta; thromboelastography coagulation monitoring; tranexamic acid administration for substantial hyperfibrinolysis; decreased time to operating room and interventional radiology; and goal-directed resuscitation with blood products.
- Massive transfusion
-
Several definitions exist. The most frequently used is >10 units of red blood cells (RBCs) per 24 hours, although this definition is liable to substantial survivor bias. Other definitions include: the critical administration threshold (CAT, ≥3 RBC units per hour in the first hour or in any of the first 4 hours from arrival); >4 RBC units or death in the first hour after injury, a definition that has the advantage of minimizing survivor bias; and >4 RBC units within the first hour, which is also known as the resuscitation intensity definition.
- Crystalloid solutions
-
Isotonic plasma volume expanders that contain electrolytes.
- Viscoelastic haemostatic assays
-
These assays measure change in viscoelastic properties of the whole blood during clot formation, strengthening and dissolution. The most commonly used devices are thromboelastography (TEG) and rotational thromboelastometry (ROTEM).
- Goal-directed resuscitation
-
A procedure consisting of haemostatic resuscitation with blood components guided by viscoelastic haemostatic assays that is directed at normalizing coagulation.
- Auto-dilution
-
A shift of interstitial fluid into the vascular compartment in response to haemorrhagic shock, which may impair haemostatic capacity.
- Secondary haemostasis
-
Secondary haemostasis refers to the deposition of insoluble fibrin, generated by the proteolytic coagulation cascade, into the platelet plug, which forms a mesh that is incorporated into and around the platelet plug.
- Primary haemostasis
-
Primary haemostasis refers to platelet aggregation and plug formation on an injury site.
- Prothrombin time
-
(PT). A conventional coagulation assay that evaluates the extrinsic and the common pathways of the coagulation cascade. The PT result (measured in seconds) in a healthy individual varies between different types and batches of the tissue factor used by the manufacturer.
- International normalized ratio
-
(INR). The INR was devised to standardize the PT results. Manufacturers assign an International Sensitivity Index (IST) for their tissue factor and the INR is calculated as (PT test/PT normal)
- Activated partial thromboplastin time
-
(aPTT). PTT is a conventional coagulation assay that measures the clotting activity of the intrinsic pathway cascade. It tests the function of all clotting factors except factor VII and factor XIII (fibrin stabilizing factor). aPTT is often used to monitor patients’ responses to unfractionated heparin infusion, to target therapeutic anticoagulation. Activation occurs via exposure to a negatively charged substrate, which replicates contact activation and enhances the speed of the test.
- Damage control resuscitation
-
A procedure consisting of limited (to avoid haemodilution) crystalloid fluid, permissive hypotension and administration of balanced blood components in severely injured patients to attenuate TIC.
- Damage control surgery
-
A procedure consisting of essential operative manoeuvres: control of mechanical bleeding, shunting critical arteries, controlling gastrointestinal spillage and temporary packing of bleeding sites in patients manifesting TIC due to ongoing shock. Patients will need to return to the operating room to complete definitive reconstruction after they have stabilized.
- Cryoprecipitate
-
A plasma-derived blood product for transfusion that contains fibrinogen (factor I), factor VIII, factor XIII, von Willebrand factor and fibronectin.
- Glasgow Outcome Score–Extended
-
(GOSE). Global scale for functional outcome that rates patient status into eight categories (death, vegetative state, lower severe disability, upper severe disability, lower moderate disability, upper moderate disability, lower good recovery and upper good recovery).
Rights and permissions
About this article
Cite this article
Moore, E.E., Moore, H.B., Kornblith, L.Z. et al. Trauma-induced coagulopathy. Nat Rev Dis Primers 7, 30 (2021). https://doi.org/10.1038/s41572-021-00264-3
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41572-021-00264-3
This article is cited by
-
Role of the admission muscle injury indicators in early coagulopathy, inflammation and acute kidney injury in patients with severe multiple injuries
World Journal of Emergency Surgery (2025)
-
Hemostatic abnormalities after trauma resuscitation: challenges and strategies in caring for the critically injured patient
Annals of Intensive Care (2025)
-
Effect of early administration of fibrinogen replacement therapy in traumatic haemorrhage: a systematic review and meta-analysis of randomised controlled trials with narrative synthesis of observational studies
Critical Care (2025)
-
Clinical and surgical outcomes of pediatric pelvic fractures: experience from a mass-casualty and routine trauma cohort
Journal of Orthopaedic Surgery and Research (2025)
-
High ratio of plasma to red cells in contemporary resuscitation of haemorrhagic shock after trauma: a secondary analysis of the PATCH-trauma trial
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2025)