Abstract
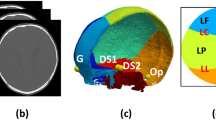
Craniosynostosis is characterized by the premature fusion of one or more major cranial sutures at birth or soon after. Single-suture non-syndromic craniosynostosis (NSC) is the most common form of craniosynostosis and includes the sagittal, metopic, unicoronal and unilambdoid subtypes. Characterized by an abnormal head shape specific to the fused suture type, NSC can cause increased intracranial pressure. Cranial sutures either originate from the neural crest or arise from mesoderm-derived mesenchymal stem cells. A mixture of environmental and genetic factors contributes to NSC, with genetic causes following a largely polygenic model. Physical examination is used to identify the majority of patients, but accompanying radiographic imaging can be confirmatory. The three major surgical techniques in use to treat NSC are cranial vault remodelling, strip craniectomy and spring-assisted cranioplasty. Surgical intervention is ideally performed in the first year of life, with a mortality of <1%. Health-care disparities contribute to delayed initial presentation and timely repair. Optimal timing of surgery and comparative outcomes by surgical technique remain under active study. School-age children with treated NSC on average have subtle, but lower cognitive and behavioural performance. However, patient-reported quality of life outcomes are comparable to those in control individuals.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Doro, D., Liu, A., Grigoriadis, A. E. & Liu, K. J. The osteogenic potential of the neural crest lineage may contribute to craniosynostosis. Mol. Syndromol. 10, 48–57 (2019).
Shruthi, N. M. & Gulati, S. Craniosynostosis: a pediatric neurologist’s perspective. J. Pediatr. Neurosci. 17, S54–S60 (2022).
Maliepaard, M., Mathijssen, I. M., Oosterlaan, J. & Okkerse, J. M. Intellectual, behavioral, and emotional functioning in children with syndromic craniosynostosis. Pediatrics 133, e1608–e1615 (2014).
Dempsey, R. F. et al. Nonsyndromic craniosynostosis. Clin. Plast. Surg. 46, 123–139 (2019).
French, L. R., Jackson, I. T. & Melton, L. J. 3rd A population-based study of craniosynostosis. J. Clin. Epidemiol. 43, 69–73 (1990).
Shuper, A., Merlob, P., Grunebaum, M. & Reisner, S. H. The incidence of isolated craniosynostosis in the newborn infant. Am. J. Dis. Child. 139, 85–86 (1985).
Lattanzi, W., Barba, M., Di Pietro, L. & Boyadjiev, S. A. Genetic advances in craniosynostosis. Am. J. Med. Genet. A 173, 1406–1429 (2017).
Kolar, J. C. An epidemiological study of nonsyndromal craniosynostoses. J. Craniofac Surg. 22, 47–49 (2011).
Ursitti, F. et al. Evaluation and management of nonsyndromic craniosynostosis. Acta Paediatr. 100, 1185–1194 (2011).
Persing, J. A. MOC-PS(SM) CME article: management considerations in the treatment of craniosynostosis. Plast. Reconstr. Surg. 121, 1–11 (2008).
Ramsey, J. A. et al. Comprehensive craniometry for sagittal synostosis. Neurosurg. Focus. 58, E8 (2025).
Beckett, J. S., Chadha, P., Persing, J. A. & Steinbacher, D. M. Classification of trigonocephaly in metopic synostosis. Plast. Reconstr. Surg. 130, 442e–447e (2012).
Birgfeld, C. B. et al. Making the diagnosis: metopic ridge versus metopic craniosynostosis. J. Craniofac Surg. 24, 178–185 (2013).
van der Meulen, J. Metopic synostosis. Childs Nerv. Syst. 28, 1359–1367 (2012).
Gabrick, K. S., Wu, R. T., Singh, A., Persing, J. A. & Alperovich, M. Radiographic severity of metopic craniosynostosis correlates with long-term neurocognitive outcomes. Plast. Reconstr. Surg. 145, 1241–1248 (2020).
Sakamoto, Y. et al. Geometric morphometric study on distinguishing metopic craniosynostosis from metopic ridging. Plast. Reconstr. Surg. Glob. Open. 12, e6034 (2024).
Wu, R. T. et al. Comparison of neurocognitive outcomes in postoperative adolescents with unilateral coronal synostosis. Plast. Reconstr. Surg. 146, 614–619 (2020).
Beckett, J. S., Persing, J. A. & Steinbacher, D. M. Bilateral orbital dysmorphology in unicoronal synostosis. Plast. Reconstr. Surg. 131, 125–130 (2013).
Allam, O. et al. Distinguishing craniomorphometric characteristics of unilateral lambdoid craniosynostosis. J. Craniofac Surg. 32, 125–129 (2021).
Junn, A. H. et al. Long-term neurocognitive outcomes in 204 single-suture craniosynostosis patients. Childs Nerv. Syst. 39, 1921–1928 (2023).
Fearon, J. A. Evidence-based medicine: craniosynostosis. Plast. Reconstr. Surg. 133, 1261–1275 (2014).
Shlobin, N. A. et al. Global epidemiology of craniosynostosis: a systematic review and meta-analysis. World Neurosurg. 164, 413–423.e3 (2022).
Gaillard, L. et al. Genetic diagnostic yield in an 11-year cohort of craniosynostosis patients. Eur. J. Med. Genet. 66, 104843 (2023).
Tonne, E. et al. Benefits of clinical criteria and high-throughput sequencing for diagnosing children with syndromic craniosynostosis. Eur. J. Hum. Genet. 29, 920–929 (2021).
Wang, J. C., Nagy, L. & Demke, J. C. Syndromic craniosynostosis. Facial Plast. Surg. Clin. North. Am. 24, 531–543 (2016).
Cornelissen, M. et al. Increase of prevalence of craniosynostosis. J. Craniomaxillofac Surg. 44, 1273–1279 (2016).
van der Meulen, J. et al. The increase of metopic synostosis: a pan-European observation. J. Craniofac Surg. 20, 283–286 (2009).
Di Rocco, F., Arnaud, E., Meyer, P., Sainte-Rose, C. & Renier, D. Focus session on the changing “epidemiology” of craniosynostosis (comparing two quinquennia: 1985-1989 and 2003-2007) and its impact on the daily clinical practice: a review from Necker Enfants Malades. Childs Nerv. Syst. 25, 807–811 (2009).
Gonzalez, S. R., Han, A. & Golinko, M. S. Shifting epidemiology of single-suture craniosynostosis and the need for a more granular ICD classification system: a national survey of members from the American Society of Pediatric Neurosurgeons (ASPN) and the American Society of Craniofacial Surgeons (ASCFS). Childs Nerv. Syst. 35, 1443–1444 (2019).
Calpena, E. et al. SMAD6 variants in craniosynostosis: genotype and phenotype evaluation. Genet. Med. 22, 1498–1506 (2020).
Timberlake, A. T. et al. De novo mutations in inhibitors of Wnt, BMP, and Ras/ERK signaling pathways in non-syndromic midline craniosynostosis. Proc. Natl Acad. Sci. USA 114, E7341–E7347 (2017).
Tooze, R. S. et al. Review of recurrently mutated genes in craniosynostosis supports expansion of diagnostic gene panels. Genes 14, 615 (2023).
Wilkie, A. O. M., Johnson, D. & Wall, S. A. Clinical genetics of craniosynostosis. Curr. Opin. Pediatr. 29, 622–628 (2017).
Kennedy, D., Novak, C. B., Phillips, J. H., Der, T. & Forrest, C. R. Catastrophic and critical intraoperative events during pediatric craniofacial surgery. Plast. Reconstr. Surg. Glob. Open. 11, e4784 (2023).
Garza, R. M. & Khosla, R. K. Nonsyndromic craniosynostosis. Semin. Plast. Surg. 26, 53–63 (2012).
Lynn, J. V., Buchman, L. K., Breuler, C. J. & Buchman, S. R. Surgical timing and neurocognitive development among patients with craniosynostosis: analysis of confounders. Plast. Reconstr. Surg. 151, 821–829 (2023). This study highlights the increased proportion of socioeconomically at-risk individuals with craniosynostosis presenting late for craniosynostosis surgery.
Valenti, A. B. et al. Healthcare disparities in the care of children with craniosynostosis in the United States: a systematic review. Cleft Palate Craniofac. J. https://doi.org/10.1177/10556656231222318 (2023).
Wireko, A. A. et al. Insights into craniosynostosis management in low- and middle-income countries: a narrative review of outcomes, shortcomings and paediatric neurosurgery capacity. SAGE Open. Med. 12, 20503121241226891 (2024).
Mozaffari, M. A. et al. Socioeconomic disparities in the surgical management of craniosynostosis. J. Craniofac Surg. 33, 294–297 (2022).
Lin, Y., Pan, I. W., Harris, D. A., Luerssen, T. G. & Lam, S. The impact of insurance, race, and ethnicity on age at surgical intervention among children with nonsyndromic craniosynostosis. J. Pediatr. 166, 1289–1296 (2015).
Couly, G. F., Coltey, P. M. & Le Douarin, N. M. The triple origin of skull in higher vertebrates: a study in quail-chick chimeras. Development 117, 409–429 (1993).
Jiang, X., Iseki, S., Maxson, R. E., Sucov, H. M. & Morriss-Kay, G. M. Tissue origins and interactions in the mammalian skull vault. Dev. Biol. 241, 106–116 (2002).
Lawson, K. A. & Pedersen, R. A. Clonal analysis of cell fate during gastrulation and early neurulation in the mouse. Ciba Found. Symp. 165, 3–21 (1992). discussion 21-26.
Morriss-Kay, G. M. & Wilkie, A. O. Growth of the normal skull vault and its alteration in craniosynostosis: insights from human genetics and experimental studies. J. Anat. 207, 637–653 (2005).
Mathijssen, I. M. et al. Tracing craniosynostosis to its developmental stage through bone center displacement. J. Craniofac Genet. Dev. Biol. 19, 57–63 (1999).
Twigg, S. R. & Wilkie, A. O. A genetic-pathophysiological framework for craniosynostosis. Am. J. Hum. Genet. 97, 359–377 (2015). This review discusses the pathways and processes that lead to cranial suture fusion as well as its genetic underpinnings.
Bok, S. et al. A multi-stem cell basis for craniosynostosis and calvarial mineralization. Nature 621, 804–812 (2023).
Deckelbaum, R. A. et al. Regulation of cranial morphogenesis and cell fate at the neural crest-mesoderm boundary by engrailed 1. Development 139, 1346–1358 (2012).
Ishii, M., Sun, J., Ting, M. C. & Maxson, R. E. The development of the calvarial bones and sutures and the pathophysiology of craniosynostosis. Curr. Top. Dev. Biol. 115, 131–156 (2015).
Ting, M. C. et al. EphA4 as an effector of Twist1 in the guidance of osteogenic precursor cells during calvarial bone growth and in craniosynostosis. Development 136, 855–864 (2009).
Yoshida, T., Vivatbutsiri, P., Morriss-Kay, G., Saga, Y. & Iseki, S. Cell lineage in mammalian craniofacial mesenchyme. Mech. Dev. 125, 797–808 (2008).
Taylor, J. C. et al. Factors influencing success of clinical genome sequencing across a broad spectrum of disorders. Nat. Genet. 47, 717–726 (2015).
Twigg, S. R. et al. Gain-of-function mutations in ZIC1 are associated with coronal craniosynostosis and learning disability. Am. J. Hum. Genet. 97, 378–388 (2015).
Twigg, S. R. et al. Mutations of ephrin-B1 (EFNB1), a marker of tissue boundary formation, cause craniofrontonasal syndrome. Proc. Natl Acad. Sci. USA 101, 8652–8657 (2004).
Wieland, I. et al. Mutations of the ephrin-B1 gene cause craniofrontonasal syndrome. Am. J. Hum. Genet. 74, 1209–1215 (2004).
Merrill, A. E. et al. Cell mixing at a neural crest-mesoderm boundary and deficient ephrin-Eph signaling in the pathogenesis of craniosynostosis. Hum. Mol. Genet. 15, 1319–1328 (2006).
Yen, H. Y., Ting, M. C. & Maxson, R. E. Jagged1 functions downstream of Twist1 in the specification of the coronal suture and the formation of a boundary between osteogenic and non-osteogenic cells. Dev. Biol. 347, 258–270 (2010).
Carter, D. H., Sloan, P. & Aaron, J. E. Immunolocalization of collagen types I and III, tenascin, and fibronectin in intramembranous bone. J. Histochem. Cytochem. 39, 599–606 (1991).
Neve, A., Corrado, A. & Cantatore, F. P. Osteoblast physiology in normal and pathological conditions. Cell Tissue Res. 343, 289–302 (2011).
Ornitz, D. M. & Marie, P. J. FGF signaling pathways in endochondral and intramembranous bone development and human genetic disease. Genes. Dev. 16, 1446–1465 (2002).
Anderson, H. C. Matrix vesicles and calcification. Curr. Rheumatol. Rep. 5, 222–226 (2003).
Yoshiko, Y., Candeliere, G. A., Maeda, N. & Aubin, J. E. Osteoblast autonomous Pi regulation via Pit1 plays a role in bone mineralization. Mol. Cell Biol. 27, 4465–4474 (2007).
Zhao, H. et al. The suture provides a niche for mesenchymal stem cells of craniofacial bones. Nat. Cell Biol. 17, 386–396 (2015).
Thomas, S. & Jaganathan, B. G. Signaling network regulating osteogenesis in mesenchymal stem cells. J. Cell Commun. Signal. 16, 47–61 (2022).
Wu, X. & Gu, Y. Signaling mechanisms underlying genetic pathophysiology of craniosynostosis. Int. J. Biol. Sci. 15, 298–311 (2019).
Holmes, G. et al. Single-cell analysis identifies a key role for Hhip in murine coronal suture development. Nat. Commun. 12, 7132 (2021).
Stanton, E., Urata, M., Chen, J. F. & Chai, Y. The clinical manifestations, molecular mechanisms and treatment of craniosynostosis. Dis. Model. Mech. 15, dmm049390 (2022).
Holmes, G. et al. Integrated transcriptome and network analysis reveals spatiotemporal dynamics of calvarial suturogenesis. Cell Rep. 32, 107871 (2020).
Farmer, D. T. et al. The developing mouse coronal suture at single-cell resolution. Nat. Commun. 12, 4797 (2021).
Iseki, S. et al. Fgfr2 and osteopontin domains in the developing skull vault are mutually exclusive and can be altered by locally applied FGF2. Development 124, 3375–3384 (1997).
Iseki, S., Wilkie, A. O. & Morriss-Kay, G. M. Fgfr1 and Fgfr2 have distinct differentiation- and proliferation-related roles in the developing mouse skull vault. Development 126, 5611–5620 (1999).
Lin, G. L. & Hankenson, K. D. Integration of BMP, Wnt, and notch signaling pathways in osteoblast differentiation. J. Cell Biochem. 112, 3491–3501 (2011).
Krakow, D. Skeletal dysplasias. Clin. Perinatol. 42, 301–319 (2015).
Nieminen, P. et al. Inactivation of IL11 signaling causes craniosynostosis, delayed tooth eruption, and supernumerary teeth. Am. J. Hum. Genet. 89, 67–81 (2011).
Kido, S. et al. Mechanical stress induces interleukin-11 expression to stimulate osteoblast differentiation. Bone 45, 1125–1132 (2009).
Sims, N. A. et al. Interleukin-11 receptor signaling is required for normal bone remodeling. J. Bone Min. Res. 20, 1093–1102 (2005).
Bille, A., Foss-Skiftesvik, J. & Juhler, M. The current understanding of germline predisposition in non-syndromic sagittal craniosynostosis: a systematic review. Childs Nerv. Syst. 39, 689–700 (2023).
Justice, C. M. et al. A genome-wide association study implicates the BMP7 locus as a risk factor for nonsyndromic metopic craniosynostosis. Hum. Genet. 139, 1077–1090 (2020).
Nicoletti, P. et al. Regulatory elements in SEM1-DLX5-DLX6 (7q21.3) locus contribute to genetic control of coronal nonsyndromic craniosynostosis and bone density-related traits. Genet. Med. Open. 2, 101851 (2024).
Goovaerts, S. et al. Joint multi-ancestry and admixed GWAS reveals the complex genetics behind human cranial vault shape. Nat. Commun. 14, 7436 (2023).
Timberlake, A. T. & Persing, J. A. Genetics of nonsyndromic craniosynostosis. Plast. Reconstr. Surg. 141, 1508–1516 (2018).
Kiziltug, E. et al. Concurrent impact of de novo mutations on cranial and cortical development in nonsyndromic craniosynostosis. J. Neurosurg. Pediatr. 33, 59–72 (2024).
Timberlake, A. T. et al. Mutations in TFAP2B and previously unimplicated genes of the BMP, Wnt, and Hedgehog pathways in syndromic craniosynostosis. Proc. Natl Acad. Sci. USA 116, 15116–15121 (2019).
Timberlake, A. T. et al. De novo mutations in the BMP signaling pathway in lambdoid craniosynostosis. Hum. Genet. 142, 21–32 (2023).
Timberlake, A. T. et al. De novo variants implicate chromatin modification, transcriptional regulation, and retinoic acid signaling in syndromic craniosynostosis. Am. J. Hum. Genet. 110, 846–862 (2023).
Blessing, M. & Gallagher, E. R. Epidemiology, genetics, and pathophysiology of craniosynostosis. Oral. Maxillofac. Surg. Clin. North. Am. 34, 341–352 (2022).
Justice, C. M. et al. A genome-wide association study identifies susceptibility loci for nonsyndromic sagittal craniosynostosis near BMP2 and within BBS9. Nat. Genet. 44, 1360–1364 (2012).
Komatsu, Y. & Mishina, Y. An epistatic explanation. eLife 5, e21162 (2016).
Timberlake, A. T. et al. Two locus inheritance of non-syndromic midline craniosynostosis via rare SMAD6 and common BMP2 alleles. eLife 5, e20125 (2016).
Fuller, Z. L., Berg, J. J., Mostafavi, H., Sella, G. & Przeworski, M. Measuring intolerance to mutation in human genetics. Nat. Genet. 51, 772–776 (2019).
Timberlake, A. T. et al. Genetic influence on neurodevelopment in nonsyndromic craniosynostosis. Plast. Reconstr. Surg. 149, 1157–1165 (2022).
Sur, M. & Rubenstein, J. L. Patterning and plasticity of the cerebral cortex. Science 310, 805–810 (2005).
Richtsmeier, J. T. & Flaherty, K. Hand in glove: brain and skull in development and dysmorphogenesis. Acta Neuropathol. 125, 469–489 (2013).
Duy, P. Q., Timberlake, A. T., Lifton, R. P. & Kahle, K. T. Molecular genetics of human developmental neurocranial anomalies: towards “precision surgery”. Cereb. Cortex 33, 2912–2918 (2023).
Wu, R. T. et al. SMAD6 genotype predicts neurodevelopment in nonsyndromic craniosynostosis. Plast. Reconstr. Surg. 145, 117e–125e (2020). This study provides clinical evidence supporting the poor prognosis from identified genetic mutations on neurocognition in non-syndromic craniosynostosis.
Cohen, M. M. Jr. Sutural biology and the correlates of craniosynostosis. Am. J. Med. Genet. 47, 581–616 (1993).
Cohen, M. M. Jr. Etiopathogenesis of craniosynostosis. Neurosurg. Clin. N. Am. 2, 507–513 (1991).
Cinalli, G. et al. Hydrocephalus and craniosynostosis. J. Neurosurg. 88, 209–214 (1998).
Weinzweig, J. et al. Cranial vault expansion in the management of postshunt craniosynostosis and slit ventricle syndrome. Plast. Reconstr. Surg. 122, 1171–1180 (2008).
Albright, A. L. & Tyler-Kabara, E. Slit-ventricle syndrome secondary to shunt-induced suture ossification. Neurosurgery 48, 764–769 (2001); discussion 769–770.
Bryant, J. R. et al. Craniosynostosis develops in half of infants treated for hydrocephalus with a ventriculoperitoneal shunt. Plast. Reconstr. Surg. 147, 1390–1399 (2021).
Al-Rekabi, Z., Cunningham, M. L. & Sniadecki, N. J. Cell mechanics of craniosynostosis. ACS Biomater. Sci. Eng. 3, 2733–2743 (2017).
Petrovic, V., Zivkovic, P., Petrovic, D. & Stefanovic, V. Craniofacial bone tissue engineering. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 114, e1–e9 (2012).
Jacob, S., Wu, C., Freeman, T. A., Koyama, E. & Kirschner, R. E. Expression of Indian Hedgehog, BMP-4 and Noggin in craniosynostosis induced by fetal constraint. Ann. Plast. Surg. 58, 215–221 (2007).
Sanchez-Lara, P. A. et al. Fetal constraint as a potential risk factor for craniosynostosis. Am. J. Med. Genet. A 152A, 394–400 (2010).
Heller, J. B. et al. Cranial suture response to stress: expression patterns of Noggin and Runx2. Plast. Reconstr. Surg. 119, 2037–2045 (2007).
Chawla, R. et al. Squamosal suture craniosynostosis due to hyperthyroidism caused by an activating thyrotropin receptor mutation (T632I). Thyroid 25, 1167–1172 (2015).
Higashino, T. & Hirabayashi, S. A secondary craniosynostosis associated with juvenile hyperthyroidism. J. Plast. Reconstr. Aesthet. Surg. 66, e284–e286 (2013).
Akita, S., Nakamura, T., Hirano, A., Fujii, T. & Yamashita, S. Thyroid hormone action on rat calvarial sutures. Thyroid 4, 99–106 (1994).
Jentink, J. et al. Valproic acid monotherapy in pregnancy and major congenital malformations. N. Engl. J. Med. 362, 2185–2193 (2010).
Lajeunie, E. et al. Craniosynostosis and fetal exposure to sodium valproate. J. Neurosurg. 95, 778–782 (2001).
Singh, R. P. et al. Role of parental risk factors in the aetiology of isolated non-syndromic metopic craniosynostosis. Br. J. Oral. Maxillofac. Surg. 48, 438–442 (2010).
Gardner, J. S. et al. Maternal exposure to prescription and non-prescription pharmaceuticals or drugs of abuse and risk of craniosynostosis. Int. J. Epidemiol. 27, 64–67 (1998).
Carmichael, S. L. et al. Craniosynostosis and maternal smoking. Birth Defects Res. A Clin. Mol. Teratol. 82, 78–85 (2008).
Carmichael, S. L. et al. Craniosynostosis and nutrient intake during pregnancy. Birth Defects Res. A Clin. Mol. Teratol. 88, 1032–1039 (2010).
Di Rocco, F. et al. Craniosynostosis and metabolic bone disorder. A review. Neurochirurgie 65, 258–263 (2019).
Vega, R. A. et al. Hypophosphatemic rickets and craniosynostosis: a multicenter case series. J. Neurosurg. Pediatr. 17, 694–700 (2016).
Sheth, R. D., Mullett, M. D., Bodensteiner, J. B. & Hobbs, G. R. Longitudinal head growth in developmentally normal preterm infants. Arch. Pediatr. Adolesc. Med. 149, 1358–1361 (1995).
Cacciaguerra, G. et al. The evolution of the role of imaging in the diagnosis of craniosynostosis: a narrative review. Children https://doi.org/10.3390/children8090727 (2021).
Fahradyan, A., Daneshgaran, G., Hoffman, T. L., Wexler, A. & Francis, S. H. Challenging the norm: is routine use of cranial CT in evaluation of craniosynostosis necessary? J. Craniofac Surg. 32, 2496–2499 (2021).
Schweitzer, T. et al. Avoiding CT scans in children with single-suture craniosynostosis. Childs Nerv. Syst. 28, 1077–1082 (2012).
DeFreitas, C. A. et al. Prenatal diagnosis of craniosynostosis using ultrasound. Plast. Reconstr. Surg. 150, 1084–1089 (2022).
Montoya, J. C. et al. Low-dose CT for craniosynostosis: preserving diagnostic benefit with substantial radiation dose reduction. AJNR Am. J. Neuroradiol. 38, 672–677 (2017).
Eley, K. A., Watt-Smith, S. R., Sheerin, F. & Golding, S. J. “Black bone” MRI: a potential alternative to CT with three-dimensional reconstruction of the craniofacial skeleton in the diagnosis of craniosynostosis. Eur. Radiol. 24, 2417–2426 (2014).
Delashaw, J. B., Persing, J. A. & Jane, J. A. Cranial deformation in craniosynostosis. A new explanation. Neurosurg. Clin. N. Am. 2, 611–620 (1991).
Spazzapan, P. & Velnar, T. Isolated sagittal craniosynostosis: a comprehensive review. Diagnostics https://doi.org/10.3390/diagnostics14040435 (2024).
Mathijssen, I. M. J. Updated guideline on treatment and management of craniosynostosis. J. Craniofac Surg. 32, 371–450 (2021).
Chandler, L. et al. Distinguishing craniomorphometric characteristics and severity in metopic synostosis patients. Int. J. Oral. Maxillofac. Surg. 50, 1040–1046 (2021).
Junn, A. et al. Validation of artificial intelligence severity assessment in metopic craniosynostosis. Cleft Palate Craniofac J. 60, 274–279 (2023).
Di Rocco, C., Paternoster, G., Caldarelli, M., Massimi, L. & Tamburrini, G. Anterior plagiocephaly: epidemiology, clinical findings, diagnosis, and classification. A review. Childs Nerv. Syst. 28, 1413–1422 (2012).
Gabrick, K. S. et al. Assessing facial asymmetry in postoperative patients with unilateral coronal craniosynostosis. J. Craniofac Surg. 31, 1000–1005 (2020).
Hauc, S. C. et al. Orthotic helmet therapy for deformational plagiocephaly: stratifying outcomes by insurance. Cleft Palate Craniofac J. 61, 1027–1032 (2024).
Park, K. E. et al. Neurocognitive outcomes in deformational plagiocephaly: is there an association between morphologic severity and results? Plast. Reconstr. Surg. 152, 488e–498e (2023).
Birgfeld, C. B. & Heike, C. Distinguishing between lambdoid craniosynostosis and deformational plagiocephaly: a review of this paradigm shift in clinical decision-making and lesson for the future. Craniomaxillofac Trauma. Reconstr. 13, 248–252 (2020).
Bir, S. C., Ambekar, S., Notarianni, C. & Nanda, A. Odilon Marc Lannelongue (1840-1911) and strip craniectomy for craniosynostosis. Neurosurg. Focus. 36, E16 (2014).
Belza, C. C. et al. Perioperative comparison between open cranial vault remodeling and distraction osteogenesis for unilateral lambdoid craniosynostosis. J. Craniofac Surg. 34, 1222–1225 (2023).
Mundinger, G. S. et al. Distraction osteogenesis for surgical treatment of craniosynostosis: a systematic review. Plast. Reconstr. Surg. 138, 657–669 (2016).
Park, D. H. & Yoon, S. H. Transsutural distraction osteogenesis for 285 children with craniosynostosis: a single-institution experience. J. Neurosurg. Pediatr. 17, 230–239 (2016).
Elawadly, A. et al. 3-dimensional morphometric outcomes after endoscopic strip craniectomy for unicoronal synostosis. J. Craniofac Surg. 34, 322–331 (2023).
Ha, A. Y. et al. School-aged anthropometric outcomes after endoscopic or open repair of metopic synostosis. Pediatrics https://doi.org/10.1542/peds.2020-0238 (2020).
Nguyen, D. C. et al. Are endoscopic and open treatments of metopic synostosis equivalent in treating trigonocephaly and hypotelorism. J. Craniofac Surg. 26, 129–134 (2015).
Tan, S. P., Proctor, M. R., Mulliken, J. B. & Rogers, G. F. Early frontofacial symmetry after correction of unilateral coronal synostosis: frontoorbital advancement vs endoscopic strip craniectomy and helmet therapy. J. Craniofac Surg. 24, 1190–1194 (2013).
Williams, C. T. et al. Evaluation of endoscopic strip craniectomy and orthotic therapy for bilateral coronal craniosynostosis. J. Craniofac Surg. 30, 453–457 (2019).
Barone, C. M. & Jimenez, D. F. Endoscopic craniectomy for early correction of craniosynostosis. Plast. Reconstr. Surg. 104, 1965–1973 (1999); discussion 1974–1965.
Nguyen, D. C. et al. One hundred consecutive endoscopic repairs of sagittal craniosynostosis: an evolution in care. J. Neurosurg. Pediatr. 20, 410–418 (2017).
Badiee, R. K. et al. Superior long-term appearance of strip craniectomy compared with cranial vault reconstruction in metopic craniosynostosis. Plast. Reconstr. Surg. Glob. Open. 10, e4097 (2022).
Proctor, M. R. & Meara, J. G. A review of the management of single-suture craniosynostosis, past, present, and future. J. Neurosurg. Pediatr. 24, 622–631 (2019).
Massenburg, B. B., Tolley, P. D., Lee, A. & Susarla, S. M. Fronto-orbital advancement for metopic and unilateral coronal craniosynostoses. Oral. Maxillofac. Surg. Clin. North. Am. 34, 367–380 (2022).
Lauritzen, C. G. K., Davis, C., Ivarsson, A., Sanger, C. & Hewitt, T. D. The evolving role of springs in craniofacial surgery: the first 100 clinical cases. Plast. Reconstr. Surg. 121, 545–554 (2008).
Persing, J. A., Babler, W. J., Nagorsky, M. J., Edgerton, M. T. & Jane, J. A. Skull expansion in experimental craniosynostosis. Plast. Reconstr. Surg. 78, 594–603 (1986).
Kalmar, C. L. et al. Spring-mediated cranioplasty for sagittal craniosynostosis. Neurosurg. Focus. Video 4, V6 (2021).
Mellgren, J. et al. Spring-assisted surgery of unilambdoid craniosynostosis. J. Craniofac Surg. 35, 715–720 (2024).
Shen, W. et al. Correction of craniosynostosis using modified spring-assisted surgery. J. Craniofac Surg. 26, 522–525 (2015).
Duan, M., Skoch, J., Pan, B. S. & Shah, V. Neuro-ophthalmological manifestations of craniosynostosis: current perspectives. Eye Brain 13, 29–40 (2021).
Alperovich, M., Vyas, R. M. & Staffenberg, D. A. Is craniosynostosis repair keeping up with the times? Results from the largest national survey on craniosynostosis. J. Craniofac Surg. 26, 1909–1913 (2015).
Bonfield, C. M., Sharma, J., Cochrane, D. D., Singhal, A. & Steinbok, P. Minimizing blood transfusions in the surgical correction of craniosynostosis: a 10-year single-center experience. Childs Nerv. Syst. 32, 143–151 (2016).
Suarez, A. D. et al. Predictors of blood transfusion for endoscopic assisted craniosynostosis surgery. J. Craniofac Surg. 33, 1327–1330 (2022).
Belouaer, A. et al. The enhanced recovery after surgery protocol for the surgical management of craniosynostosis: Lausanne experience. Neurosurg. Focus. 55, E14 (2023).
Dadure, C. et al. Intraoperative tranexamic acid reduces blood transfusion in children undergoing craniosynostosis surgery: a randomized double-blind study. Anesthesiology 114, 856–861 (2011).
Fearon, J. A. Reducing allogenic blood transfusions during pediatric cranial vault surgical procedures: a prospective analysis of blood recycling. Plast. Reconstr. Surg. 113, 1126–1130 (2004).
Taylor, J. A. & Maugans, T. A. Comparison of spring-mediated cranioplasty to minimally invasive strip craniectomy and barrel staving for early treatment of sagittal craniosynostosis. J. Craniofac Surg. 22, 1225–1229 (2011).
Wolfswinkel, E. M. et al. Is postoperative intensive care unit care necessary following cranial vault remodeling for sagittal synostosis. Plast. Reconstr. Surg. 140, 1235–1239 (2017).
Seruya, M. et al. Analysis of routine intensive care unit admission following fronto-orbital advancement for craniosynostosis. Plast. Reconstr. Surg. 131, 582e–588e (2013).
Branch, L. G. et al. Long-term outcomes of pediatric cranial reconstruction using resorbable plating systems for the treatment of craniosynostosis. J. Craniofac Surg. 28, 26–29 (2017).
Greene, A. K., Mulliken, J. B., Proctor, M. R. & Rogers, G. F. Primary grafting with autologous cranial particulate bone prevents osseous defects following fronto-orbital advancement. Plast. Reconstr. Surg. 120, 1603–1611 (2007).
Jubbal, K. T., Agrawal, N. & Hollier, L. H. Jr. Analysis of morbidity, readmission, and reoperation after craniosynostosis repair in children. J. Craniofac Surg. 28, 401–405 (2017).
Nguyen, C., Hernandez-Boussard, T., Khosla, R. K. & Curtin, C. M. A national study on craniosynostosis surgical repair. Cleft Palate Craniofac J. 50, 555–560 (2013).
Massenburg, B. B., Nassar, A. H. & Hopper, R. A. National database reported outcomes following craniosynostosis reconstruction. J. Craniofac Surg. 31, 154–157 (2020).
Skolnick, G. B. et al. Long-term characterization of cranial defects after surgical correction for single-suture craniosynostosis. Ann. Plast. Surg. 82, 679–685 (2019).
Woerdeman, P. A. et al. Patient-reported outcome measures more than fifteen years after treatment of sagittal or metopic craniosynostosis: a prospective cohort study. Childs Nerv. Syst. 40, 769–777 (2024).
McClugage, S. G. 3rd et al. Incidence of delayed intracranial hypertension in children with isolated sagittal synostosis following open calvarial vault reconstruction. Childs Nerv. Syst. 36, 545–550 (2020).
Da Costa, A. C. et al. Longitudinal study of the neurodevelopmental characteristics of treated and untreated nonsyndromic craniosynostosis in infancy. Childs Nerv. Syst. 29, 985–995 (2013).
Patel, A. et al. The impact of age at surgery on long-term neuropsychological outcomes in sagittal craniosynostosis. Plast. Reconstr. Surg. 134, 608e–617e (2014). The study most commonly cited to demonstrate the clinical benefit of earlier surgery in infancy on neurocognitive outcomes in craniosynostosis.
Renier, D. & Marchac, D. Craniofacial surgery for craniosynostosis: functional and morphological results. Ann. Acad. Med. Singap. 17, 415–426 (1988).
Hashim, P. W. et al. The effects of whole-vault cranioplasty versus strip craniectomy on long-term neuropsychological outcomes in sagittal craniosynostosis. Plast. Reconstr. Surg. 134, 491–501 (2014).
Alperovich, M. et al. Long-term neurocognitive outcomes of spring-assisted surgery versus cranial vault remodeling for sagittal synostosis. Plast. Reconstr. Surg. 147, 661–671 (2021).
Chandler, L. et al. Spring-assisted strip craniectomy versus cranial vault remodeling: long-term psychological, behavioral, and executive function outcomes. J. Craniofac Surg. 31, 2101–2105 (2020).
Magge, S. N. et al. Cognitive outcomes of children with sagittal craniosynostosis treated with either endoscopic or open calvarial vault surgery. JAMA Netw. Open. 7, e248762 (2024).
Junn, A. et al. Quantifying the impact of genetics on neurocognition in nonsyndromic sagittal craniosynostosis. Plast. Reconstr. Surg. 152, 300e–306e (2023).
Duggan, C., Irvine, A. D., J, O. B. H., Kiely, M. E. & Murray, D. M. ASQ-3 and BSID-III’s concurrent validity and predictive ability of cognitive outcome at 5 years. Pediatr. Res. 94, 1465–1471 (2023).
Kapp-Simon, K. A., Figueroa, A., Jocher, C. A. & Schafer, M. Longitudinal assessment of mental development in infants with nonsyndromic craniosynostosis with and without cranial release and reconstruction. Plast. Reconstr. Surg. 92, 831–839 (1993); discussion 840–831.
Arnaud, E., Renier, D. & Marchac, D. Prognosis for mental function in scaphocephaly. J. Neurosurg. 83, 476–479 (1995).
Kapp-Simon, K. A. et al. Language, learning, and memory in children with and without single-suture craniosynostosis. J. Neurosurg. Pediatr. 17, 578–588 (2016).
Speltz, M. L., Endriga, M. C. & Mouradian, W. E. Presurgical and postsurgical mental and psychomotor development of infants with sagittal synostosis. Cleft Palate Craniofac J. 34, 374–379 (1997).
Virtanen, R., Korhonen, T., Fagerholm, J. & Viljanto, J. Neurocognitive sequelae of scaphocephaly. Pediatrics 103, 791–795 (1999).
Magge, S. N., Westerveld, M., Pruzinsky, T. & Persing, J. A. Long-term neuropsychological effects of sagittal craniosynostosis on child development. J. Craniofac Surg. 13, 99–104 (2002).
Speltz, M. L. et al. Intellectual and academic functioning of school-age children with single-suture craniosynostosis. Pediatrics 135, e615–e623 (2015).
Speltz, M. L., Collett, B. R., Wallace, E. R. & Kapp-Simon, K. Behavioral adjustment of school-age children with and without single-suture craniosynostosis. Plast. Reconstr. Surg. 138, 435–445 (2016).
Kelleher, M. O. et al. Behavioral, developmental, and educational problems in children with nonsyndromic trigonocephaly. J. Neurosurg. 105, 382–384 (2006).
Edwards-Bailey, L. et al. The craniofacial collaboration UK: developmental outcomes in 7- and 10-year-old children with metopic synostosis. J. Craniofac Surg. 35, 96–103 (2024).
Lloyd-White, S. et al. The craniofacial collaboration UK: developmental outcomes in 7- and 10-year-old children with sagittal synostosis. J. Craniofac. Surg. 35, 1707–1714 (2024).
Collett, B. R. et al. Attention and executive function in children with and without single-suture craniosynostosis. Child. Neuropsychol. 23, 83–98 (2017).
Chieffo, D. et al. Long-term neuropsychological development in single-suture craniosynostosis treated early. J. Neurosurg. Pediatr. 5, 232–237 (2010).
Renier, D., Sainte-Rose, C., Marchac, D. & Hirsch, J. F. Intracranial pressure in craniostenosis. J. Neurosurg. 57, 370–377 (1982).
Kljajic, M., Maltese, G., Tarnow, P., Sand, P. & Kolby, L. Health-related quality of life of children treated for non-syndromic craniosynostosis. J. Plast. Surg. Hand Surg. 57, 408–414 (2023).
Shavlokhova, V., Gruninger, S., Hoffmann, J., Freudlsperger, C. & Engel, M. Health-related quality of life in children after surgical treatment of non-syndromal craniosynostosis. J. Craniomaxillofac Surg. 49, 655–658 (2021).
Mazzaferro, D. M. et al. Quality of life in adults with nonsyndromic craniosynostosis. Plast. Reconstr. Surg. 141, 1474–1482 (2018). This study includes the longest period of follow-up to assess quality of life in adulthood in individuals with non-syndromic craniosynostosis.
Junn, A. et al. Long-term follow-up of preoperative infant event-related potentials in school-age children with craniosynostosis. Plast. Reconstr. Surg. Glob. Open. 9, e3844 (2021).
Moscarelli, J. et al. A diffusion tensor imaging comparison of white matter development in nonsyndromic craniosynostosis to neurotypical infants. Childs Nerv. Syst. 40, 1477–1487 (2024).
Bruce, M. K. et al. 3D photography to quantify the severity of metopic craniosynostosis. Cleft Palate Craniofac J. 60, 971–979 (2023).
Porras, A. R. et al. Quantification of head shape from three-dimensional photography for presurgical and postsurgical evaluation of craniosynostosis. Plast. Reconstr. Surg. 144, 1051e–1060e (2019).
Callejas Pastor, C. A. et al. Two-dimensional image-based screening tool for infants with positional cranial deformities: a machine learning approach. Diagnostics https://doi.org/10.3390/diagnostics10070495 (2020).
Author information
Authors and Affiliations
Contributions
Introduction (M.A. and C.T.); Epidemiology (M.A. and C.T.); Mechanisms/pathophysiology (M.A. and K.T.K.); Diagnosis, screening and prevention (M.A.); Management (M.A.); Quality of life (M.A. and L.C.M.); Outlook (all authors); overview of the Primer (M.A.).
Corresponding author
Ethics declarations
Competing interests
M.A. consults for Johnson & Johnson. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks K. B. Patel; S. P. Bartlett, who co-reviewed with P. Tolley; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alperovich, M., Tonello, C., Mayes, L.C. et al. Non-syndromic craniosynostosis. Nat Rev Dis Primers 11, 24 (2025). https://doi.org/10.1038/s41572-025-00607-4
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41572-025-00607-4
This article is cited by
-
Cognitive and neuropsychomotor development in craniosynostosis: an evaluation of the most affected functions
Child's Nervous System (2026)