Abstract
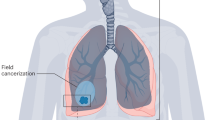
Up to 50% of patients with metastatic cancer develop lung metastases during their disease course. Lung metastases are linked to poor prognosis across various cancer types and might impair the quality of life of patients, causing dyspnoea, cough, haemoptysis and pain, potentially diminishing physical, functional and emotional well-being. Lung metastases arise from a complex interplay of tumour-secreted factors such as VEGF, TGFβ and CCL2, which drive vascular remodelling, immune cell recruitment and extracellular matrix reprogramming. Additionally, tumour-derived exosomes and microparticles contribute to organotropism and immunosuppression by altering the lung microenvironment. The ensemble of these modifications creates a pre-metastatic niche conducive to tumour cell colonization and outgrowth. Lung metastases are primarily diagnosed through imaging; histological confirmation is sometimes required to distinguish them from primary lung cancer. The size and number of lung metastases, timing of primary cancer treatment, histology, and the patient’s clinical condition are all considered to determine the most appropriate treatment. When a locoregional approach is not possible, histology-based, molecular-driven systemic therapy is the choice. No systemic treatment is currently available specifically for lung metastases. Advances in understanding the distinct stages of pre-metastatic niche formation and lung metastasis outgrowth might lead to the development of prevention strategies and tailored treatments.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Chen, H. et al. The epidemiology of lung metastases. Front. Med. 8, 723396 (2021).
Ng, W. H., Varghese, B. & Ren, X. in Engineering Translational Models of Lung Homeostasis and Disease (ed. Magin, C. M.) 247–264 (Springer International, 2023).
Wu, C., Ren, X. & Zhang, Q. Incidence, risk factors, and prognosis in patients with primary hepatocellular carcinoma and lung metastasis: a population-based study. Cancer Manag. Res. 11, 2759–2768 (2019).
Gerratana, L. et al. Pattern of metastasis and outcome in patients with breast cancer. Clin. Exp. Metastasis 32, 125–133 (2015).
Detterbeck, F. C. et al. The IASLC Lung Cancer Staging Project: methodology and validation used in the development of proposals for revision of the stage classification of NSCLC in the forthcoming (Eighth) edition of the TNM Classification of Lung Cancer. J. Thorac. Oncol. 11, 1433–1446 (2016).
Billingsley, K. G. et al. Pulmonary metastases from soft tissue sarcoma: analysis of patterns of diseases and postmetastasis survival. Ann. Surg. 229, 602–610 (1999).
Gadd, M. A., Casper, E. S., Woodruff, J. M., McCormack, P. M. & Brennan, M. F. Development and treatment of pulmonary metastases in adult patients with extremity soft tissue sarcoma. Ann. Surg. 218, 705–712 (1993).
Feng, J., He, Y., Wan, J. & Chen, Z. Pulmonary metastases in newly diagnosed hepatocellular carcinoma: a population-based retrospective study. HPB 22, 1295–1304 (2020).
Neal, R. D. Lung cancer. BMJ 365, l1725 (2019).
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74, 229–263 (2024).
Mangiameli, G., Cioffi, U., Alloisio, M. & Testori, A. in Metastasis (ed. Sergi, C. M.) Ch. 3 (Exon Publications, 2022).
Travis, W. D., Brambilla, E., Müller-Hermelink, H. K. & Harris, C. C. (eds) Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart (IARC, 2004).
Shaha, A. R., Hoover, E. L., Mitrani, M., Marti, J. R. & Krespi, Y. P. Synchronicity, multicentricity, and metachronicity of head and neck cancer. Head Neck Surg. 10, 225–228 (1988).
Hendriks, L. E. L. et al. Non-small-cell lung cancer. Nat. Rev. Dis. Primers 10, 71 (2024).
Albrengues, J. et al. Neutrophil extracellular traps produced during inflammation awaken dormant cancer cells in mice. Science 361, eaao4227 (2018).
Higgins, S. T. et al. A literature review on prevalence of gender differences and intersections with other vulnerabilities to tobacco use in the United States, 2004–2014. Prev. Med. 80, 89–100 (2015).
Siegel, R. L., Kratzer, T. B., Giaquinto, A. N., Sung, H. & Jemal, A. Cancer statistics, 2025. CA Cancer J. Clin. 75, 10–45 (2025).
Irish, W. D., Burch, A. E., Landry, A., Honaker, M. D. & Wong, J. Development and validation of a county deprivation index for assessing socio-economic disparities in the United States: implications for public health outcomes and mitigation strategies. Public Health 240, 56–62 (2025).
Nascimento de Carvalho, F. et al. Disparities in stage at diagnosis of head and neck tumours in Brazil: a comprehensive analysis of hospital-based cancer registries. Lancet Reg. Health Am. 42, 100986 (2025).
Crow, J., Slavin, G. & Kreel, L. Pulmonary metastasis: a pathologic and radiologic study. Cancer 47, 2595–2602 (1981).
van Meerbeeck, J. P., Gosselin, R. & Duyck, P. in Lung Metastases and Isolated Lung Perfusion (ed. van Schil, P. E.) 3–25 (Nova Science, 2007).
Mayinger, M. et al. Stereotactic body radiotherapy for lung oligo-metastases: systematic review and International Stereotactic Radiosurgery Society practice guidelines. Lung Cancer 182, 107284 (2023).
Christ, S. M. et al. Clinical management of oligometastatic cancer: applying multidisciplinary tumor board recommendations in practice. Clin. Transl. Radiat. Oncol. 48, 100838 (2024).
Xie, T. et al. Distant metastasis patterns among lung cancer subtypes and impact of primary tumor resection on survival in metastatic lung cancer using SEER database. Sci. Rep. 14, 22445 (2024).
Riihimäki, M. et al. Metastatic sites and survival in lung cancer. Lung Cancer 86, 78–84 (2014).
Stenbygaard, L. E., Sorensen, J. B. & Olsen, J. E. Metastatic pattern at autopsy in non-resectable adenocarcinoma of the lung — a study from a cohort of 259 consecutive patients treated with chemotherapy. Acta Oncol. 36, 301–306 (1997).
Fong, K. M. et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the M descriptors in the forthcoming 9th edition of the TNM Classification of Lung Cancer. J. Thorac. Oncol. 19, 786–802 (2024).
Rami-Porta, R. et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: proposals for revision of the TNM stage groups in the forthcoming (Ninth) edition of the TNM classification for lung cancer. J. Thorac. Oncol. 19, 1007–1027 (2024).
Riquet, M. et al. Multiple lung cancers prognosis: what about histology? Ann. Thorac. Surg. 86, 921–926 (2008).
Foulkes, W. D., Smith, I. E. & Reis-Filho, J. S. Triple-negative breast cancer. N. Engl. J. Med. 363, 1938–1948 (2010).
Kennecke, H. et al. Metastatic behavior of breast cancer subtypes. J. Clin. Oncol. 28, 3271–3277 (2010).
Smid, M. et al. Subtypes of breast cancer show preferential site of relapse. Cancer Res. 68, 3108–3114 (2008).
Yhim, H.-Y. et al. Prognostic factors for recurrent breast cancer patients with an isolated, limited number of lung metastases and implications for pulmonary metastasectomy. Cancer 116, 2890–2901 (2010).
Edwards, B. K. et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 116, 544–573 (2010).
Wang, J. et al. Metastatic patterns and survival outcomes in patients with stage IV colon cancer: a population-based analysis. Cancer Med. 9, 361–373 (2020).
Jordens, M. S. et al. Prevalence of lung metastases among 19,321 metastatic colorectal cancer patients in eight countries of Europe and Asia. Curr. Oncol. 28, 5035–5040 (2021).
Mitry, E. et al. Epidemiology, management and prognosis of colorectal cancer with lung metastases: a 30-year population-based study. Gut 59, 1383–1388 (2010).
Shou, J., Zhang, Q., Wang, S. & Zhang, D. The prognosis of different distant metastases pattern in prostate cancer: a population based retrospective study. Prostate 78, 491–497 (2018).
Fabozzi, S. J., Schellhammer, P. F. & el-Mahdi, A. M. Pulmonary metastases from prostate cancer. Cancer 75, 2706–2709 (1995).
Bubendorf, L. et al. Metastatic patterns of prostate cancer: an autopsy study of 1,589 patients. Hum. Pathol. 31, 578–583 (2000).
Bianchi, M. et al. Distribution of metastatic sites in renal cell carcinoma: a population-based analysis. Ann. Oncol. 23, 973–980 (2012).
Chandrasekar, T. et al. Metastatic renal cell carcinoma: patterns and predictors of metastases — a contemporary population-based series. Urol. Oncol. 35, 661.e7–661.e14 (2017).
Weiss, L. et al. Metastatic patterns of renal carcinoma: an analysis of 687 necropsies. J. Cancer Res. Clin. Oncol. 114, 605–612 (1988).
Zhang, Z., Liang, C., Hou, B. & Zhou, L. Population-based evaluation of the risk factors and prognosis among renal cell carcinoma patients with initially diagnosed lung metastases. Actas Urol. Esp. 45, 498–506 (2021).
Abdel-Rahman, O. Clinical correlates and prognostic value of different metastatic sites in metastatic renal cell carcinoma. Future Oncol. 13, 1967–1980 (2017).
Vezeridis, M. P., Moore, R. & Karakousis, C. P. Metastatic patterns in soft-tissue sarcomas. Arch. Surg. 118, 915–918 (1983).
Zhang, C. et al. Lung metastases at the initial diagnosis of high-grade osteosarcoma: prevalence, risk factors and prognostic factors. A large population-based cohort study. Sao Paulo Med. J. 137, 423–429 (2019).
Fan, Z. et al. Score for the risk and overall survival of lung metastasis in patients first diagnosed with soft tissue sarcoma: a novel nomogram-based risk assessment system. Technol. Cancer Res. Treat. 21, https://doi.org/10.1177/15330338211066240 (2022).
Xie, L., Huang, W., Wang, H., Zheng, C. & Jiang, J. Risk factors for lung metastasis at presentation with malignant primary osseous neoplasms: a population-based study. J. Orthop. Surg. Res. 15, 32 (2020).
Liu, H. et al. Pan-soft tissue sarcoma analysis of the incidence, survival, and metastasis: a population-based study focusing on distant metastasis and lymph node metastasis. Front. Oncol. 12, 890040 (2022).
Lindsey, B. A., Markel, J. E. & Kleinerman, E. S. Osteosarcoma overview. Rheumatol. Ther. 4, 25–43 (2017).
Vaarwerk, B. et al. Fluorine-18-fluorodeoxyglucose (FDG) positron emission tomography (PET) computed tomography (CT) for the detection of bone, lung, and lymph node metastases in rhabdomyosarcoma. Cochrane Database Syst. Rev. 11, CD012325 (2021).
Uka, K. et al. Clinical features and prognosis of patients with extrahepatic metastases from hepatocellular carcinoma. World J. Gastroenterol. 13, 414–420 (2007).
Shao, G., Zhi, Y., Fan, Z., Qiu, W. & Lv, G. Development and validation of a diagnostic and prognostic model for lung metastasis of hepatocellular carcinoma: a study based on the SEER database. Front. Med. 10, 1171023 (2023).
Li, M. et al. Hepatoid adenocarcinoma-clinicopathological features and molecular characteristics. Cancer Lett. 559, 216104 (2023).
Moorman, A. et al. Progressive plasticity during colorectal cancer metastasis. Nature 637, 947–954 (2025).
Cañellas-Socias, A. et al. Metastatic recurrence in colorectal cancer arises from residual EMP1+ cells. Nature 611, 603–613 (2022).
Gundem, G. et al. The evolutionary history of lethal metastatic prostate cancer. Nature 520, 353–357 (2015).
Martínez-Ruiz, C. et al. Genomic-transcriptomic evolution in lung cancer and metastasis. Nature 616, 543–552 (2023).
Shah, S. P. et al. Mutational evolution in a lobular breast tumour profiled at single nucleotide resolution. Nature 461, 809–813 (2009).
Gerull, W. D., Puri, V. & Kozower, B. D. The epidemiology and biology of pulmonary metastases. J. Thorac. Dis. 13, 2585–2589 (2021).
Kurma, K. & Alix-Panabières, C. Mechanobiology and survival strategies of circulating tumor cells: a process towards the invasive and metastatic phenotype. Front. Cell Dev. Biol. 11, 1188499 (2023).
Au, S. H. et al. Clusters of circulating tumor cells traverse capillary-sized vessels. Proc. Natl Acad. Sci. USA 113, 4947–4952 (2016).
Giancotti, F. G. Mechanisms governing metastatic dormancy and reactivation. Cell 155, 750–764 (2013).
Peinado, H. et al. Pre-metastatic niches: organ-specific homes for metastases. Nat. Rev. Cancer 17, 302–317 (2017).
Kaplan, R. N. et al. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature 438, 820–827 (2005). This study highlights the organotropism underlying lung metastases: the metastatic process necessitates VEGFR1+VLA4+ bone marrow-derived progenitors and their interaction with fibronectin expressed by resident fibroblasts.
Ghouse, S. M. et al. Therapeutic targeting of vasculature in the premetastatic and metastatic niches reduces lung metastasis. J. Immunol. 204, 990–1000 (2020).
Qian, B.-Z. et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature 475, 222–225 (2011).
Nam, J.-S. et al. Chemokine (C-C Motif) ligand 2 mediates the prometastatic effect of dysadherin in human breast cancer cells. Cancer Res. 66, 7176–7184 (2006).
Mestdagt, M. et al. Transactivation of MCP-1/CCL2 by β-catenin/TCF-4 in human breast cancer cells. Int. J. Cancer 118, 35–42 (2006).
Roblek, M. et al. CCL2 is a vascular permeability factor inducing CCR2-dependent endothelial retraction during lung metastasis. Mol. Cancer Res. 17, 783–793 (2019). This study highlights the critical role of endothelial CCR2 in orchestrating tumour cell extravasation and promoting lung metastasis.
Lu, X. & Kang, Y. Chemokine (C-C motif) ligand 2 engages CCR2+ stromal cells of monocytic origin to promote breast cancer metastasis to lung and bone. J. Biol. Chem. 284, 29087–29096 (2009).
Zhang, H. et al. Circulating tumor microparticles promote lung metastasis by reprogramming inflammatory and mechanical niches via a macrophage-dependent pathway. Cancer Immunol. Res. 6, 1046–1056 (2018).
Sceneay, J. et al. Primary tumor hypoxia recruits CD11b+/Ly6Cmed/Ly6G+ immune suppressor cells and compromises NK cell cytotoxicity in the premetastatic niche. Cancer Res. 72, 3906–3911 (2012).
Hiratsuka, S., Watanabe, A., Aburatani, H. & Maru, Y. Tumour-mediated upregulation of chemoattractants and recruitment of myeloid cells predetermines lung metastasis. Nat. Cell Biol. 8, 1369–1375 (2006).
Hiratsuka, S. et al. The S100A8-serum amyloid A3-TLR4 paracrine cascade establishes a pre-metastatic phase. Nat. Cell Biol. 10, 1349–1355 (2008). This study demonstrates that SAA3–TLR4 signalling within the pre-metastatic niche triggers an inflammatory-like state that acts as a positive feedback loop, enhancing tumour cell recruitment to the lung.
Liu, Y. et al. Tumor exosomal RNAs promote lung pre-metastatic niche formation by activating alveolar epithelial TLR3 to recruit neutrophils. Cancer Cell 30, 243–256 (2016).
Simons, M. & Raposo, G. Exosomes–vesicular carriers for intercellular communication. Curr. Opin. Cell Biol. 21, 575–581 (2009).
Liu, Y., Gu, Y. & Cao, X. The exosomes in tumor immunity. Oncoimmunology 4, e1027472 (2015).
Hoshino, A. et al. Tumour exosome integrins determine organotropic metastasis. Nature 527, 329–335 (2015).
Ma, R. et al. Tumor cell-derived microparticles polarize M2 tumor-associated macrophages for tumor progression. OncoImmunology 5, e1118599 (2016).
Gong, Z. et al. Lung fibroblasts facilitate pre-metastatic niche formation by remodeling the local immune microenvironment. Immunity 55, 1483–1500.e9 (2022). This study highlights that, while primary tumours certainly coordinate the invasion of the secondary metastatic site, the lung (specifically its resident fibroblast) facilitates the establishment of a pre-metastatic niche.
Yofe, I. et al. Spatial and temporal mapping of breast cancer lung metastases identify TREM2 macrophages as regulators of the metastatic boundary. Cancer Discov. 13, 2610–2631 (2023).
Zahr, A. et al. Endomucin prevents leukocyte–endothelial cell adhesion and has a critical role under resting and inflammatory conditions. Nat. Commun. 7, 10363 (2016).
Armulik, A., Genové, G. & Betsholtz, C. Pericytes: developmental, physiological, and pathological perspectives, problems, and promises. Dev. Cell 21, 193–215 (2011).
Murgai, M. et al. KLF4-dependent perivascular cell plasticity mediates pre-metastatic niche formation and metastasis. Nat. Med. 23, 1176–1190 (2017).
Padua, D. et al. TGFβ primes breast tumors for lung metastasis seeding through angiopoietin-like 4. Cell 133, 66–77 (2008).
Zhang, G. et al. Loss of endothelial EMCN drives tumor lung metastasis through the premetastatic niche. J. Transl. Med. 20, 446 (2022).
McDonald, D. M. & Baluk, P. Significance of blood vessel leakiness in cancer. Cancer Res. 62, 5381–5385 (2002).
Li, H., Han, Y., Guo, Q., Zhang, M. & Cao, X. Cancer-expanded myeloid-derived suppressor cells induce anergy of NK cells through membrane-bound TGF-β11. J. Immunol. 182, 240–249 (2009).
Olkhanud, P. B. et al. Breast cancer lung metastasis requires expression of chemokine receptor CCR4 and regulatory T cells. Cancer Res. 69, 5996–6004 (2009).
Gong, Z. et al. Immunosuppressive reprogramming of neutrophils by lung mesenchymal cells promotes breast cancer metastasis. Sci. Immunol. 8, eadd5204 (2023).
Wculek, S. K. & Malanchi, I. Neutrophils support lung colonization of metastasis-initiating breast cancer cells. Nature 528, 413–417 (2015). This research letter describes the role of neutrophils, and their secreted leukotrienes, in enhancing the expansion of the subset of tumour cells with the highest metastatic potential.
Qian, B.-Z. & Pollard, J. W. Macrophage diversity enhances tumor progression and metastasis. Cell 141, 39–51 (2010). This study underscores the pivotal role of the CCL2–CCR2 axis in promoting the recruitment of inflammatory monocytes.
Sangaletti, S. et al. Macrophage-derived SPARC bridges tumor cell-extracellular matrix interactions toward metastasis. Cancer Res. 68, 9050–9059 (2008).
Egeblad, M. & Werb, Z. New functions for the matrix metalloproteinases in cancer progression. Nat. Rev. Cancer 2, 161–174 (2002).
Hiratsuka, S. et al. MMP9 induction by vascular endothelial growth factor receptor-1 is involved in lung-specific metastasis. Cancer Cell 2, 289–300 (2002).
Schild, T., Low, V., Blenis, J. & Gomes, A. P. Unique metabolic adaptations dictate distal organ-specific metastatic colonization. Cancer Cell 33, 347–354 (2018).
LeBleu, V. S. et al. PGC-1α mediates mitochondrial biogenesis and oxidative phosphorylation in cancer cells to promote metastasis. Nat. Cell Biol. 16, 992–1003 (2014).
Andrzejewski, S. et al. PGC-1α promotes breast cancer metastasis and confers bioenergetic flexibility against metabolic drugs. Cell Metab. 26, 778–787.e5 (2017).
St-Pierre, J. et al. Suppression of reactive oxygen species and neurodegeneration by the PGC-1 transcriptional coactivators. Cell 127, 397–408 (2006).
Christen, S. et al. Breast cancer-derived lung metastases show increased pyruvate carboxylase-dependent anaplerosis. Cell Rep. 17, 837–848 (2016).
Sellers, K. et al. Pyruvate carboxylase is critical for non-small-cell lung cancer proliferation. J. Clin. Invest. 125, 687–698 (2015).
Jin, L. et al. Breast cancer lung metastasis: molecular biology and therapeutic implications. Cancer Biol. Ther. 19, 858–868 (2018).
Colon cancer (version 2.2024). National Comprehensive Cancer Network https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf (2024).
Gennari, A. et al. ESMO Guidelines Committee. ESMO clinical practice guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer. Ann. Oncol. 2, 1475–1495 (2021).
Escudier, B. et al. ESMO Guidelines Committee. Renal cell carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 30, 706–720 (2019).
Cervantes, A. et al. ESMO Guidelines Committee. Metastatic colorectal cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann. Oncol. 34, 10–32 (2023).
Deniffel, D. et al. Differentiating intrapulmonary metastases from different primary tumors via quantitative dual-energy CT based iodine concentration and conventional CT attenuation. Eur. J. Radiol. 111, 6–13 (2019).
Juan, J. et al. Computer-assisted diagnosis for an early identification of lung cancer in chest X rays. Sci. Rep. 13, 7720 (2023).
Veltri, A. et al. CIRSE guidelines on percutaneous needle biopsy (PNB). Cardiovasc. Interv. Radiol. 40, 1501–1513 (2017).
Venturini, M. et al. CIRSE standards of practice on thermal ablation of primary and secondary lung tumours. Cardiovasc. Interv. Radiol. 43, 667–683 (2020).
Genshaft, S. J. et al. Society of Interventional Radiology multidisciplinary position statement on percutaneous ablation of non-small cell lung cancer and metastatic disease to the lungs: endorsed by the Canadian Association for Interventional Radiology, the Cardiovascular and Interventional Radiological Society of Europe, and the Society of Interventional Oncology. J. Vasc. Interv. Radiol. 32, 1241.e1–1241.e12 (2021).
Bartlett, E. C. et al. Defining growth in small pulmonary nodules using volumetry: results from a ‘coffee-break’ CT study and implications for current nodule management guidelines. Eur. Radiol. 32, 1912–1920 (2022).
Hofman, M. S. et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. Lancet 395, 1208–1216 (2020).
Damjanovic, J. et al. 68 Ga-PSMA-PET/CT for the evaluation of pulmonary metastases and opacities in patients with prostate cancer. Cancer Imaging 18, 20 (2018).
Albanus, D. R. et al. Clinical value of 68Ga-DOTATATE-PET/CT compared to stand-alone contrast enhanced CT for the detection of extra-hepatic metastases in patients with neuroendocrine tumours (NET). Eur. J. Radiol. 84, 1866–1872 (2015).
Mori, Y. et al. FAPI PET: fibroblast activation protein inhibitor use in oncologic and nononcologic disease. Radiology 306, e220749 (2023).
Seo, J. B. et al. Atypical pulmonary metastases: spectrum of radiologic findings. Radiographics 21, 403–417 (2001).
Saifuddin, A., Baig, M. S., Dalal, P. & Strauss, S. J. The diagnosis of pulmonary metastases on chest computed tomography in primary bone sarcoma and musculoskeletal soft tissue sarcoma. Br. J. Radiol. 94, 20210088 (2021).
Tateishi, U. et al. Metastatic angiosarcoma of the lung: spectrum of CT findings. Am. J. Roentgenol. 180, 1671–1674 (2003).
Stella, G. M., Kolling, S., Benvenuti, S. & Bortolotto, C. Lung-seeking metastases. Cancers 11, 1010 (2019).
Deng, C. J. et al. Clinical updates of approaches for biopsy of pulmonary lesions based on systematic review. BMC Pulm. Med. 18, 146 (2018).
Kim, S. H. et al. Clinical outcomes of transbronchial cryobiopsy using a 1.1-mm diameter cryoprobe for peripheral lung lesions — a prospective pilot study. Respir. Med. 217, 107338 (2023).
Giri, M. et al. Efficacy and safety of cryobiopsy vs. forceps biopsy for interstitial lung diseases, lung tumors, and peripheral pulmonary lesions: an updated systematic review and meta-analysis. Front. Med. 9, 840702 (2022).
Genova, C. et al. Potential application of cryobiopsy for histo-molecular characterization of mediastinal lymph nodes in patients with thoracic malignancies: a case presentation series and implications for future developments. BMC Pulm. Med. 22, 5 (2022).
Zhang, J. et al. Transbronchial mediastinal cryobiopsy in the diagnosis of mediastinal lesions: a randomised trial. Eur. Respir. J. 58, 2100055 (2021).
Scholten, E. T. & Kreel, L. Distribution of lung metastases in the axial plane. A combined radiological-pathological study. Radiol. Clin. 46, 248–265 (1977).
Coppage, L., Shaw, C. & Curtis, A. M. Metastatic disease to the chest in patients with extrathoracic malignancy. J. Thorac. Imaging 2, 24–37 (1987).
Libshitz, H. I. & North, L. B. Pulmonary metastases. Radiol. Clin. North Am. 20, 437–451 (1982).
Marchevsky, A. M., Gupta, R. & Balzer, B. Diagnosis of metastatic neoplasms: a clinicopathologic and morphologic approach. Arch. Pathol. Lab. Med. 134, 194–206 (2010).
Jagirdar, J. Application of immunohistochemistry to the diagnosis of primary and metastatic carcinoma to the lung. Arch. Pathol. Lab. Med. 132, 384–396 (2008).
Girard, N. et al. Comprehensive histologic assessment helps to differentiate multiple lung primary nonsmall cell carcinomas from metastases. Am. J. Surg. Pathol. 33, 1752–1764 (2009).
Murphy, S. J. et al. Identification of independent primary tumors and intrapulmonary metastases using DNA rearrangements in non-small-cell lung cancer. J. Clin. Oncol. 32, 4050–4058 (2014).
Murphy, S. J. et al. Using genomics to differentiate multiple primaries from metastatic lung cancer. J. Thorac. Oncol. 14, 1567–1582 (2019).
Chou, T.-Y. et al. Differentiating separate primary lung adenocarcinomas from intrapulmonary metastases with emphasis on pathological and molecular considerations: recommendations from the International Association for the Study of Lung Cancer Pathology Committee. J. Thorac. Oncol. 20, 311–330 (2025). This study provides a practical guide orienting differential diagnosis of a second primary tumour (lung adenocarcinoma) and intrapulmonary metastasis, delving into pathological features, clonal relatedness and molecular analyses.
Bayle, A. et al. ESMO study on the availability and accessibility of biomolecular technologies in oncology in Europe. Ann. Oncol. 34, 934–945 (2023).
Detterbeck, F. C. et al. The IASLC lung cancer staging project: background data and proposed criteria to distinguish separate primary lung cancers from metastatic foci in patients with two lung tumors in the forthcoming eighth edition of the TNM classification for lung cancer. J. Thorac. Oncol. 11, 651–665 (2016).
Chang, J. C. et al. Comprehensive next-generation sequencing unambiguously distinguishes separate primary lung carcinomas from intrapulmonary metastases: comparison with standard histopathologic approach. Clin. Cancer Res. 25, 7113–7125 (2019).
Midha, A., Dearden, S. & McCormack, R. EGFR mutation incidence in non-small-cell lung cancer of adenocarcinoma histology: a systematic review and global map by ethnicity (mutMapII). Am. J. Cancer Res. 5, 2892–2911 (2015).
Dacic, S. et al. Genomic staging of multifocal lung squamous cell carcinomas is independent of the comprehensive morphologic assessment. J. Thorac. Oncol. 19, 273–284 (2024).
Chu, P. G., Chung, L., Weiss, L. M. & Lau, S. K. Determining the site of origin of mucinous adenocarcinoma: an immunohistochemical study of 175 cases. Am. J. Surg. Pathol. 35, 1830–1836 (2011).
Chang, J. C. et al. Comprehensive molecular and clinicopathologic analysis of 200 pulmonary invasive mucinous adenocarcinomas identifies distinct characteristics of molecular subtypes. Clin. Cancer Res. 27, 4066–4076 (2021).
Hwang, D. H. et al. KRAS and NKX2-1 mutations in invasive mucinous adenocarcinoma of the lung. J. Thorac. Oncol. 11, 496–503 (2016).
Hugen, N. et al. The molecular background of mucinous carcinoma beyond MUC2. J. Pathol. Clin. Res. 1, 3–17 (2014).
Fernandez-Cuesta, L. et al. CD74-NRG1 fusions in lung adenocarcinoma. Cancer Discov. 4, 415–422 (2014).
Liu, S. V. et al. Real-world outcomes associated with afatinib use in patients with solid tumors harboring NRG1 gene fusions. Lung Cancer 188, 107469 (2024).
Schweizer, M. T. et al. Clinical determinants for successful circulating tumor DNA analysis in prostate cancer. Prostate 79, 701–708 (2019).
Fiala, C. & Diamandis, E. P. Utility of circulating tumor DNA in cancer diagnostics with emphasis on early detection. BMC Med. 16, 166 (2018).
Umemoto, K. et al. Clinical significance of circulating-tumour DNA analysis by metastatic sites in pancreatic cancer. Br. J. Cancer 128, 1603–1608 (2023).
NNCN guidelines: treatment by cancer type. National Comprehensive Cancer Network https://www.nccn.org/guidelines/category_1 (2025).
Warwick, R. & Page, R. Resection of pulmonary metastases from colorectal carcinoma. Eur. J. Surgical Oncol. 33, S59–S63 (2007).
Pastorino, U. et al. Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. J. Thorac. Cardiovasc. Surg. 113, 37–49 (1997).
Antonoff, M. B., Sofocleous, C. T., Callstrom, M. R. & Nguyen, Q.-N. The roles of surgery, stereotactic radiation, and ablation for treatment of pulmonary metastases. J. Thorac. Cardiovasc. Surg. 163, 495–502 (2022).
Rhun, E. L. et al. EANO–ESMO clinical practice guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours. Ann. Oncol. 32, 1332–1347 (2021).
Lindqvist, J., Jekunen, A., Sihvo, E., Johansson, M. & Andersén, H. Effect of adherence to treatment guidelines on overall survival in elderly non-small-cell lung cancer patients. Lung Cancer 171, 9–17 (2022).
Jumeau, R., Vilotte, F., Durham, A.-D. & Ozsahin, E.-M. Current landscape of palliative radiotherapy for non-small-cell lung cancer. Transl. Lung Cancer Res. 8, S192–S201 (2019).
Fairchild, A. et al. Palliative thoracic radiotherapy for lung cancer: a systematic review. J. Clin. Oncol. 26, 4001–4011 (2008).
Støchkel Frank, M., Schou Nørøxe, D., Nygård, L. & Fredberg Persson, G. Fractionated palliative thoracic radiotherapy in non-small cell lung cancer — futile or worth-while? BMC Palliat. Care 17, 15 (2018).
Rodrigues, G. et al. Palliative thoracic radiotherapy in lung cancer: an American Society for Radiation Oncology evidence-based clinical practice guideline. Pract. Radiat. Oncol. 1, 60–71 (2011).
Moeller, B. et al. Palliative thoracic radiation therapy for non-small cell lung cancer: 2018 update of an American Society for Radiation Oncology (ASTRO) evidence-based guideline. Pract. Radiat. Oncol. 8, 245–250 (2018).
Singh, M. N. in Fundamentals in Gynaecologic Malignancy (eds Kataki, A. C. & Barmon, D.) 99–117 (Springer, 2022).
Azizi, A. H. et al. Superior vena cava syndrome. JACC Cardiovasc. Interv. 13, 2896–2910 (2020).
Guckenberger, M. et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 21, e18–e28 (2020).
Gomez, D. R. et al. Local consolidative therapy vs. maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer: long-term results of a multi-institutional, phase II, randomized study. J. Clin. Oncol. 37, 1558–1565 (2019).
Palma, D. A. et al. Stereotactic ablative radiotherapy for the comprehensive treatment of oligometastatic cancers: long-term results of the SABR-COMET phase II randomized trial. J. Clin. Oncol. 38, 2830–2838 (2020).
Iyengar, P. et al. Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol. 4, e173501 (2018).
Wang, X.-S. et al. Randomized trial of first-line tyrosine kinase inhibitor with or without radiotherapy for synchronous oligometastatic EGFR-mutated non-small cell lung cancer. J. Natl Cancer Inst. 115, 742–748 (2023).
Christ, S. M. et al. Cancer-specific dose and fractionation schedules in stereotactic body radiotherapy for oligometastatic disease: an interim analysis of the EORTC-ESTRO E2-RADIatE OligoCare study. Radiother. Oncol. 195, 110235 (2024).
Lievens, Y. et al. Coverage with evidence development program on stereotactic body radiotherapy in Belgium (2013-2019): a nationwide registry-based prospective study. Lancet Reg. Health Eur. 44, 100992 (2024).
Vaz, S. C. et al. Joint EANM/SNMMI/ESTRO practice recommendations for the use of 2-[18F]FDG PET/CT external beam radiation treatment planning in lung cancer V1.0. Eur. J. Nucl. Med. Mol. Imaging 49, 1386–1406 (2022).
Siva, S. et al. Single-fraction vs multifraction stereotactic ablative body radiotherapy for pulmonary oligometastases (SAFRON II): the Trans Tasman Radiation Oncology Group 13.01 phase 2 randomized clinical trial. JAMA Oncol. 7, 1476–1485 (2021).
Tekatli, H. et al. Local control and toxicity after magnetic resonance imaging (MR)-guided single fraction lung stereotactic ablative radiotherapy. Radiother. Oncol. 187, 109823 (2023).
Iyengar, P. et al. Treatment of oligometastatic non-small cell lung cancer: an ASTRO/ESTRO clinical practice guideline. Pract. Radiat. Oncol. 13, 393–412 (2023).
Cao, C. et al. A systematic review and meta-analysis of stereotactic body radiation therapy for colorectal pulmonary metastases. J. Thorac. Dis. 11, 5187–5198 (2019).
Aznar, M. C. et al. ESTRO-ACROP guideline: recommendations on implementation of breath-hold techniques in radiotherapy. Radiother. Oncol. 185, 109734 (2023).
Klein, T. J. et al. CyberKnife Xsight versus fiducial-based target-tracking: a novel 3D dosimetric comparison in a dynamic phantom. Radiat. Oncol. 17, 154 (2022).
Chang, J. H., Poon, I., Erler, D., Zhang, L. & Cheung, P. The safety and effectiveness of stereotactic body radiotherapy for central versus ultracentral lung tumors. Radiother. Oncol. 129, 277–283 (2018).
Finazzi, T. et al. Clinical outcomes of stereotactic MR-guided adaptive radiation therapy for high-risk lung tumors. Int. J. Radiat. Oncol. Biol. Phys. 107, 270–278 (2020).
Loi, M. et al. Stereotactic radiotherapy for ultra-central lung oligometastases in non-small-cell lung cancer. Cancers 12, 885 (2020).
Andruska, N. et al. Stereotactic radiation for lung cancer: a practical approach to challenging scenarios. J. Thorac. Oncol. 16, 1075–1085 (2021).
Kroeze, S. G. C. et al. Metastases-directed stereotactic body radiotherapy in combination with targeted therapy or immunotherapy: systematic review and consensus recommendations by the EORTC-ESTRO OligoCare consortium. Lancet Oncol. 24, e121–e132 (2023).
Prud’homme, C. et al. Image-guided lung metastasis ablation: a literature review. Int. J. Hyperth. 36, 37–45 (2019).
de Baere, T. et al. Radiofrequency ablation is a valid treatment option for lung metastases: experience in 566 patients with 1037 metastases. Ann. Oncol. 26, 987–991 (2015).
Callstrom, M. R. et al. Multicenter study of metastatic lung tumors targeted by interventional cryoablation evaluation (SOLSTICE). J. Thorac. Oncol. 15, 1200–1209 (2020).
Kurilova, I. et al. Microwave ablation in the management of colorectal cancer pulmonary metastases. Cardiovasc. Interv. Radiol. 41, 1530–1544 (2018).
Fonck, M. et al. Pulmonary thermal ablation enables long chemotherapy-free survival in metastatic colorectal cancer patients. Cardiovasc. Interv. Radiol. 41, 1727–1734 (2018).
Simon, C. J. et al. Pulmonary radiofrequency ablation: long-term safety and efficacy in 153 patients. Radiology 243, 268–275 (2007).
de Baere, T. et al. The ECLIPSE study: efficacy of cryoablation on metastatic lung tumors with a 5-year follow-up. J. Thorac. Oncol. 16, 1840–1849 (2021).
Moding, E. J. et al. Predictors of respiratory decline following stereotactic ablative radiotherapy to multiple lung tumors. Clin. Lung Cancer 20, 461–468.e2 (2019).
Horner-Rieber, J. et al. Parenchymal and functional lung changes after stereotactic body radiotherapy for early-stage non-small cell lung cancer-experiences from a single institution. Front. Oncol. 7, 215 (2017).
Handy, J. R. et al. Expert consensus document on pulmonary metastasectomy. Ann. Thorac. Surg. 107, 631–649 (2019).
Treasure, T. et al. Pulmonary metastasectomy versus continued active monitoring in colorectal cancer (PulMiCC): a multicentre randomised clinical trial. Trials 20, 718 (2019).
Stamenovic, D., Hohenberger, P. & Roessner, E. Pulmonary metastasectomy in soft tissue sarcomas: a systematic review. J. Thorac. Dis. 13, 2649–2660 (2021).
Isbell, J. M., Li, B. T. & Gomez, D. R. The emerging role of local therapy in oligometastatic non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 163, 819–825 (2022).
Sun, H. et al. Thoracic radiotherapy improves the survival in patients with EGFR-mutated oligo-organ metastatic non-small cell lung cancer treated with epidermal growth factor receptor-tyrosine kinase inhibitors: a multicenter, randomized, controlled, phase III trial. J. Clin. Oncol. https://doi.org/10.1200/JCO.23.02075 (2024).
Treasure, T., Macbeth, F., Farewell, V., Williams, N. R. & Fallowfield, L. The fallacy of large survival gains from lung metastasectomy in colorectal cancer. Lancet 397, 97–98 (2021).
Datta, J. et al. Coaltered Ras/B-raf and TP53 is associated with extremes of survivorship and distinct patterns of metastasis in patients with metastatic colorectal cancer. Clin. Cancer Res. 26, 1077–1085 (2020).
Deboever, N. et al. Lung surveillance following colorectal cancer pulmonary metastasectomy: utilization of clinicopathologic risk factors to guide strategy. J. Thorac. Cardiovasc. Surg. 167, 814–819.e2 (2024).
Corsini, E. M. et al. Colorectal cancer mutations are associated with survival and recurrence after pulmonary metastasectomy. J. Surg. Oncol. 120, 729–735 (2019).
Taieb, J. et al. Deficient mismatch repair/microsatellite unstable colorectal cancer: diagnosis, prognosis and treatment. Eur. J. Cancer 175, 136–157 (2022).
Renaud, S. et al. Anatomical resections improve survival following lung metastasectomy of colorectal cancer harboring KRAS mutations. Ann. Surg. 270, 1170–1177 (2019).
Nelson, D. B. et al. Local failure after stereotactic body radiation therapy or wedge resection for colorectal pulmonary metastases. J. Thorac. Cardiovasc. Surg. 158, 1234–1241.e16 (2019).
Schmid, S. et al. Study protocol for a randomised controlled trial on pulmonary metastasectomy vs. standard of care in colorectal cancer patients with ≥ 3 lung metastases (PUCC-trial). Front. Oncol. 12, 913896 (2022).
Moonsamy, P., Hompe, E. & Boland, G. M. Pulmonary metastasectomy for melanoma. Thorac. Surg. Clin. 35, 223–231 (2025).
Matsuda, N. et al. Prognostic impact of tumor-infiltrating lymphocytes, tertiary lymphoid structures, and neutrophil-to-lymphocyte ratio in pulmonary metastases from uterine leiomyosarcoma. Ann. Surg. Oncol. 30, 8727–8734 (2023).
Deboever, N. et al. The role of surgery in the treatment of melanoma pulmonary metastases in the modern era. J. Surg. Res. 277, 125–130 (2022).
Caso, R. et al. Thoracic metastasectomy in germ cell tumor patients treated with first-line versus salvage therapy. Ann. Thorac. Surg. 111, 1141–1149 (2021).
Eckardt, J. & Licht, P. B. Thoracoscopic versus open pulmonary metastasectomy: a prospective, sequentially controlled study. Chest 142, 1598–1602 (2012).
Downey, R. J. & Bains, M. S. Open surgical approaches for pulmonary metastasectomy. Thorac. Surg. Clin. 26, 13–18 (2016).
Porter, J. et al. Initiation of chemotherapy in cancer patients with poor performance status: a population-based analysis. J. Palliat. Care 30, 166–172 (2014).
Facchinetti, F. et al. First-line pembrolizumab in advanced non-small cell lung cancer patients with poor performance status. Eur. J. Cancer 130, 155–167 (2020).
Kumar, D. et al. Revisiting the association of ECOG performance status with clinical outcomes in diverse patients with cancer. J. Natl Compr. Cancer Netw. 22, e237111 (2024).
Hendriks, L. E. et al. Oncogene-addicted metastatic non-small-cell lung cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann. Oncol. 34, 339–357 (2023).
Hendriks, L. E. et al. Non-oncogene-addicted metastatic non-small-cell lung cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann. Oncol. 34, 358–376 (2023).
Machiels, J.-P. et al. Squamous cell carcinoma of the oral cavity, larynx, oropharynx and hypopharynx: EHNS–ESMO–ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 31, 1462–1475 (2020).
Gennari, A. et al. ESMO clinical practice guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer. Ann. Oncol. 32, 1475–1495 (2021).
Tarantino, P. et al. ESMO expert consensus statements (ECS) on the definition, diagnosis, and management of HER2-low breast cancer. Ann. Oncol. 34, 645–659 (2023).
Cervantes, A. et al. Metastatic colorectal cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann. Oncol. 34, 10–32 (2023).
Tabernero, J. et al. Encorafenib plus cetuximab as a new standard of care for previously treated BRAF V600E-mutant metastatic colorectal cancer: updated survival results and subgroup analyses from the BEACON study. J. Clin. Oncol. 39, 273–284 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT05518526 (2022).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT06265350 (2024).
Huland, E., Heinzer, H. & Huland, H. Inhaled interleukin-2 in combination with low-dose systemic interleukin-2 and interferon alpha in patients with pulmonary metastatic renal-cell carcinoma: effectiveness and toxicity of mainly local treatment. J. Cancer Res. Clin. Oncol. 120, 221–228 (1994).
Skubitz, K. M. & Anderson, P. M. Inhalational interleukin-2 liposomes for pulmonary metastases: a phase I clinical trial. Anticancer Drugs 11, 555–563 (2000).
Otterson, G. A. et al. Phase I study of inhaled doxorubicin for patients with metastatic tumors to the lungs. Clin. Cancer Res. 13, 1246–1252 (2007).
Hellman, S. et al. Oligometastases. J. Clin. Oncol. 13, 8–10 (1995).
de Baere, T., Bonnet, B., Tselikas, L. & Deschamps, F. The percutaneous management of pulmonary metastases. J. Med. Imaging Radiat. Oncol. 67, 870–875 (2023).
Shishido, Y. et al. Survival outcomes of lung metastases from colorectal cancer treated with pulmonary metastasectomy or modern systemic chemotherapy: a single institution experience. J. Cardiothorac. Surg. 18, 327 (2023).
Brand, N. R., Qu, L. G., Chao, A. & Ilbawi, A. M. Delays and barriers to cancer care in low‐ and middle‐income countries: a systematic review. Oncologist 24, e1371–e1380 (2019).
Gallach, M. et al. Addressing global inequities in positron emission tomography-computed tomography (PET-CT) for cancer management: a statistical model to guide strategic planning. Med. Sci. Monit. 26, e926544 (2020).
Pramesh, C. S. et al. Delivery of affordable and equitable cancer care in India. Lancet Oncol. 15, e223–e233 (2014).
Clark, M. M. et al. Randomized controlled trial of maintaining quality of life during radiotherapy for advanced cancer. Cancer 119, 880–887 (2013).
Schnipper, L. E. et al. Updating the American Society of Clinical Oncology value framework: revisions and reflections in response to comments received. J. Clin. Oncol. 34, 2925–2934 (2016).
Nestle, U. et al. Quality of life after pulmonary stereotactic fractionated radiotherapy (SBRT): results of the phase II STRIPE trial. Radiother. Oncol. 148, 82–88 (2020).
Montazeri, A., Gillis, C. R. & McEwen, J. Quality of life in patients with lung cancer: a review of literature from 1970 to 1995. Chest 113, 467–481 (1998).
Questionnaires. EORTC https://qol.eortc.org/questionnaires/ (2017).
Kaasa, S. et al. The EORTC core quality of life questionnaire (QLQ-C30): validity and reliability when analysed with patients treated with palliative radiotherapy. Eur. J. Cancer 31, 2260–2263 (1995).
Koller, M. et al. An international study to revise the EORTC questionnaire for assessing quality of life in lung cancer patients. Ann. Oncol. 28, 2874–2881 (2017).
Lou, V. W. Q. et al. Respiratory symptoms, sleep, and quality of life in patients with advanced lung cancer. J. Pain Symptom Manag. 53, 250–256.e1 (2017).
Win, T. et al. Effect of lung cancer surgery on quality of life. Thorax 60, 234–238 (2005).
Petrella, F. et al. Which factors affect pulmonary function after lung metastasectomy? Eur. J. Cardiothorac. Surg. 35, 792–796 (2009).
Salama, J. K. et al. Stereotactic body radiotherapy for multisite extracranial oligometastases. Cancer 118, 2962–2970 (2012).
Kessel, K. A. et al. Stereotactic body radiotherapy (SBRT) in patients with lung metastases — prognostic factors and long-term survival using patient self-reported outcome (PRO). BMC Cancer 20, 442 (2020).
Dammak, S. et al. Distinguishing recurrence from radiation-induced lung injury at the time of RECIST progressive disease on post-SABR CT scans using radiomics. Sci. Rep. 14, 3758 (2024).
De Bruycker, A. et al. Evaluation of chest CT-scans following lung stereotactic ablative radiotherapy: challenges and new insights. Lung Cancer 193, 107848 (2024).
Tsilimigras, D. I. et al. Liver metastases. Nat. Rev. Dis. Primers 7, 27 (2021).
Gofrit, O. N. et al. The varied clonal trajectory of liver and lung metastases of colorectal cancer. Adv. Cancer Biol. Metastasis 11, 100122 (2024).
Erhunmwunsee, L. & Tong, B. C. Preoperative evaluation and indications for pulmonary metastasectomy. Thorac. Surg. Clin. 26, 7–12 (2016).
Rossi, G. et al. Radiomic detection of EGFR mutations in NSCLC. Cancer Res. 81, 724–731 (2021).
Coudray, N. et al. Classification and mutation prediction from non-small cell lung cancer histopathology images using deep learning. Nat. Med. 24, 1559–1567 (2018).
Wu, K.-C. et al. Early prediction of radiotherapy outcomes in pharyngeal cancer using deep learning on baseline [18F]Fluorodeoxyglucose positron emission tomography/computed tomography. Eur. J. Radiol. 181, 111811 (2024).
Sadeghi, A. H. et al. Artificial intelligence-assisted augmented reality robotic lung surgery: navigating the future of thoracic surgery. JTCVS Tech. 26, 121–125 (2024).
Peek, J. J. et al. A novel 3D image registration technique for augmented reality vision in minimally invasive thoracoscopic pulmonary segmentectomy. Int. J. Comput. Assist. Radiol. Surg. 20, 787–795 (2025).
Tie, J. et al. Circulating tumor DNA analysis detects minimal residual disease and predicts recurrence in patients with stage II colon cancer. Sci. Transl. Med. 8, 346ra92 (2016).
Tie, J. et al. Circulating tumor DNA analyses as markers of recurrence risk and benefit of adjuvant therapy for stage III colon cancer. JAMA Oncol. 5, 1710–1717 (2019).
Aldea, M. et al. Detection of additional occult malignancy through profiling of ctDNA in late-stage cancer patients. Ann. Oncol. 32, 1642–1645 (2021).
Dawson, M. R., Duda, D. G., Fukumura, D. & Jain, R. K. VEGFR1-activity-independent metastasis formation. Nature 461, E4–E5 (2009).
Pienta, K. J. et al. Phase 2 study of carlumab (CNTO 888), a human monoclonal antibody against CC-chemokine ligand 2 (CCL2), in metastatic castration-resistant prostate cancer. Invest. New Drugs 31, 760–768 (2013).
Klichinsky, M. et al. Human chimeric antigen receptor macrophages for cancer immunotherapy. Nat. Biotechnol. 38, 947–953 (2020).
Anderson, N. R., Minutolo, N. G., Gill, S. & Klichinsky, M. Macrophage-based approaches for cancer immunotherapy. Cancer Res. 81, 1201–1208 (2021).
Duan, Z. & Luo, Y. Targeting macrophages in cancer immunotherapy. Sig. Transduct. Target. Ther. 6, 127 (2021).
Reiss, K. A. et al. CAR-macrophage therapy for HER2-overexpressing advanced solid tumors: a phase 1 trial. Nat. Med. 31, 1171–1182 (2025).
Herrmann, I. K., Wood, M. J. A. & Fuhrmann, G. Extracellular vesicles as a next-generation drug delivery platform. Nat. Nanotechnol. 16, 748–759 (2021).
Patel, U., Susman, D. & Allan, A. L. Influence of extracellular vesicles on lung stromal cells during breast cancer metastasis. Int. J. Mol. Sci. 24, 11801 (2023).
Gaikwad, A. et al. Primary adenocarcinoma of lung: a pictorial review of recent updates. Eur. J. Radiol. 81, 4146–4155 (2012).
Wang, Z. et al. Clinical and radiological characteristics of central pulmonary adenocarcinoma: a comparison with central squamous cell carcinoma and small cell lung cancer and the impact on treatment response. OncoTargets Ther. 11, 2509 (2018).
Author information
Authors and Affiliations
Contributions
Introduction (L.Z.); Epidemiology (L.E.L.H.); Mechanisms/pathophysiology (L.Z.); Diagnosis, screening and prevention (L.Z., D.F. and I.I.W.); Management (D.F., D.P., J.D.S. and L.Z.); Quality of life (L.Z.); Outlook (L.Z. and L.E.L.H.); overview of the Primer (L.Z. and B.B.).
Corresponding author
Ethics declarations
Competing interests
B.B. declares advisory board participation (paid to institution): Abbvie, Biontech SE, BristolMyerSquibb, Chugai Pharmaceutical, CureVac AG, Daiichi Sankyo, F. Hoffmann-La Roche Ltd., Pharmamar, Regeneron, Sanofi Aventis, Turning Point Therapeutics; conseil (paid to institution): Abbvie, Eli Lilly, Ellipses pharma Ltd, F. Hoffmann-La Roche Ltd., Genmab, Immunocore, Janssen, MSD, Ose Immunotherapeutics, Owkin, Taiho Oncology; Steering Committee (paid to institution): AstraZeneca, Beigene, GENMAB A/S, GlaxoSmithKline, Janssen, MSD, Ose Immunotherapeutics, Pharmamar, Roche-Genentech, Sanofi, Takeda; speaker (paid to institution): Abbvie, AstraZeneca, Chugai Pharmaceutical, Daichii Sankyo, Hedera Dx, Janssen, MSD, Roche, Sanofi Aventis and Springer Healthcare Ltd., none related to this work. L.E.L.H. declares grants and/or research support (all paid to institution) from Roche, Boehringer Ingelheim, AstraZeneca, Takeda, Merck, Pfizer, Novartis and Gilead; is on the advisory boards (all to institution) of Amgen, Boehringer Ingelheim, Lilly, Novartis, Pfizer, Takeda, Merck, Janssen, Merck Sharp & Dohme (MSD), AnHeart Therapeutics, Bayer, Daiichi, Pierre Fabre, BMS, AbbVie, AstraZeneca and Summit Therapeutics; was a speaker on educational seminars or webinars for AstraZeneca, Bayer, Lilly, MSD, high5oncology, Takeda, Janssen, GlaxoSmithKline (GSK), Sanofi and Pfizer (all paid to the institution), and Medtalks, Benecke, VJOncology and Medimix (personal payment); performed local principal investigator pharma studies (all paid to institution) with AstraZeneca, GSK, Novartis, Merck, Roche, Takeda, Blueprint, Mirati, AbbVie, Gilead, MSD, Pfizer, Amgen and Boehringer Ingelheim; and was on member guideline committees in a personal capacity for Dutch guidelines on non-small cell lung cancer, brain metastases and leptomeningeal metastases (personal payment), and ESMO guidelines on non-small cell lung cancer and small cell lung cancer (unpaid). J.D.S. declares grants to the institution from AstraZeneca, MSD, Roche, BMS, CLS Therapeutics, Protalix Biotherapeutics, Pfizer and Regeneron; consulting fees from AstraZeneca, Merck, Roche, BMS, Novartis, Chemocentryx, Amgen, Protalix Biotherapeutics, Xenetic Biosciences, Regeneron, Eisai and Pfizer; payment for a speaking role from Peerview, OncLive and Medscape; support for attending meetings or travel from AstraZeneca, Merck and BMS; participating on a clinical trial safety monitoring board for AstraZeneca; and receiving equipment, materials, drugs, gifts or other services via grants to the institution from Roche, MSD, BMS and AstraZeneca. I.I.W. declares consulting or advisory roles for AstraZeneca/MedImmune, Bayer, Bristol Myers Squibb, Genentech/Roche, GlaxoSmithKline, Guardant Health, HTG Molecular Diagnostics, Merck, MSD Oncology, OncoCyte, Jansen, Novartis, Flame Inc., Regeneron and Pfizer; grants and personal fees from Genentech/Roche, Bristol Myers Squibb, AstraZeneca/MedImmune, HTG Molecular, Merck and Guardant Health; personal fees from GlaxoSmithKline and Oncocyte, Daiichi Sankyo, Roche, AstraZeneca, Regeneron, Sanofi, Pfizer and Bayer; research funding (paid to the institution) from 4D Molecular Therapeutics, Adaptimmune, Adaptive Biotechnologies, Akoya Biosciences, Amgen, Bayer, EMD Serono, Genentech, Guardant Health, HTG Molecular Diagnostics, Iovance Biotherapeutics, Johnson & Johnson, Karus Therapeutics, MedImmune, Merck, Novartis, OncoPlex Diagnostics, Pfizer, Takeda and Novartis. D.P. declares a consulting role for MVision AI. L.Z. and D.F. declare no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks M. Reck; J. Minna; L. Sholl, who co-reviewed with I. Odintsov; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zullo, L., Filippiadis, D., Hendriks, L.E.L. et al. Lung metastases. Nat Rev Dis Primers 11, 60 (2025). https://doi.org/10.1038/s41572-025-00642-1
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-025-00642-1