Abstract
In patients with disorders of gut–brain interaction (DGBI), overlapping non-gastrointestinal conditions such as fibromyalgia, headaches, gynaecological and urological conditions, sleep disturbances and fatigue are common, as is overlap among DGBI in different regions of the gastrointestinal tract. These overlaps strongly influence patient management and outcome. Shared pathophysiology could explain this scenario, but details are not fully understood. This overlap has been shown to be of great relevance for DGBI. In addition, symptoms considered to be caused by a DGBI could have a detectable organic cause, and in patients with a diagnosed organic gastrointestinal disease, symptoms not clearly explained by the pathology defining this organic disease are common. Thus, the aims of this Rome Foundation Working Team Report were to review the literature on overlapping conditions among patients with paediatric and adult DGBI and, based on the available epidemiological and clinical evidence, make recommendations for the current diagnostic and therapeutic approach, and for future research. Specifically, we focused on other DGBI in the same or different gastrointestinal anatomical region(s), DGBI overlap with organic bowel diseases in remission, and DGBI overlap with non-gastrointestinal, non-structural conditions.
Key points
-
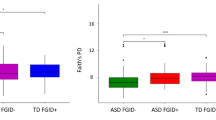
Overlap in disorders of gut–brain interaction (DGBI) diagnoses across and within anatomical regions is commonly observed in both children and adults.
-
With an increasing number of DGBI diagnoses there is a gradual increase in the severity of symptoms and psychological comorbidity and health-care utilization, and a decrease in quality of life.
-
Treating DGBI overlaps requires a comprehensive strategy, and therapeutic regimens can be strategically selected based on the type of overlapping symptoms.
-
In patients with a diagnosed organic gastrointestinal disease, symptoms not clearly explained by the pathology defining this organic disease are common.
-
The recognition of the occurrence of DGBI in patients with organic gastrointestinal disease in remission helps to avoid overtreatment with drugs with potential adverse effects.
-
In patients with DGBI, overlapping non-gastrointestinal conditions such as fibromyalgia, headaches, gynaecological and urological conditions, sleep disturbances and fatigue are common; these are best managed with a multidisciplinary approach.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Drossman, D. A. & Hasler, W. L. Rome IV – functional GI disorders: disorders of gut–brain interaction. Gastroenterology 150, 1257–1261 (2016).
Sperber, A. D. et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome Foundation global study. Gastroenterology 160, 99–114.e3 (2021).
Robin, S. G. et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the Rome IV criteria. J. Pediatr. 195, 134–139 (2018).
Aziz, I. et al. The prevalence and impact of overlapping Rome IV-diagnosed functional gastrointestinal disorders on somatization, quality of life, and healthcare utilization: a cross-sectional general population study in three countries. Am. J. Gastroenterol. 113, 86–96 (2018).
Sperber, A. D. et al. Greater overlap of Rome IV disorders of gut–brain interactions leads to increased disease severity and poorer quality of life. Clin. Gastroenterol. Hepatol. 20, e945–e956 (2022).
Whitehead, W. E., Palsson, O. & Jones, K. R. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology 122, 1140–1156 (2002).
Vandvik, P. O., Wilhelmsen, I., Ihlebaek, C. & Farup, P. G. Comorbidity of irritable bowel syndrome in general practice: a striking feature with clinical implications. Aliment. Pharmacol. Ther. 20, 1195–1203 (2004).
Balsiger, L. M., Carbone, F., Raymenants, K., Scarpellini, E. & Tack, J. Understanding and managing patients with overlapping disorders of gut–brain interaction. Lancet Gastroenterol. Hepatol. 8, 383–390 (2023).
Aziz, I. & Simrén, M. The overlap between irritable bowel syndrome and organic gastrointestinal diseases. Lancet Gastroenterol. Hepatol. 6, 139–148 (2021).
Fairlie, T. et al. Overlap of disorders of gut–brain interaction: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 8, 646–659 (2023).
Lacy, B. E. et al. Bowel disorders. Gastroenterology 150, 1393–1407 (2016).
Aziz, Q. et al. Functional esophageal disorders. Gastroenterology 150, 1368–1379 (2016).
Fass, R., Zerbib, F. & Gyawali, C. P. AGA clinical practice update on functional heartburn: expert review. Gastroenterology 158, 2286–2293 (2020).
Rengarajan, A., Pomarat, M., Zerbib, F. & Gyawali, C. P. Overlap of functional heartburn and reflux hypersensitivity with proven gastroesophageal reflux disease. Neurogastroenterol. Motil. 33, e14056 (2021).
Mudipalli, R. S., Remes-Troche, J. M., Andersen, L. & Rao, S. S. Functional chest pain: esophageal or overlapping functional disorder. J. Clin. Gastroenterol. 41, 264–269 (2007).
Bang, C. S. et al. Functional gastrointestinal disorders in young military men. Gut Liver 9, 509–515 (2015).
Stanghellini, V. et al. Gastroduodenal disorders. Gastroenterology 150, 1380–1392 (2016).
Carbone, F., Vanuytsel, T. & Tack, J. Analysis of postprandial symptom patterns in subgroups of patients with Rome III or Rome IV functional dyspepsia. Clin. Gastroenterol. Hepatol. 18, 838–846.e3 (2020).
Fang, Y. J. et al. Distinct aetiopathogenesis in subgroups of functional dyspepsia according to the Rome III criteria. Gut 64, 1517–1528 (2015).
Hsu, Y. C. et al. Psychopathology and personality trait in subgroups of functional dyspepsia based on Rome III criteria. Am. J. Gastroenterol. 104, 2534–2542 (2009).
Manabe, N. et al. Clinical characteristics of Japanese dyspeptic patients: is the Rome III classification applicable? Scand. J. Gastroenterol. 45, 567–572 (2010).
Nwokediuko, S. C., Ijoma, U. & Obienu, O. Functional dyspepsia: subtypes, risk factors, and overlap with irritable bowel syndrome in a population of African patients. Gastroenterol. Res. Pract. 2012, 562393 (2012).
Vakil, N., Halling, K., Ohlsson, L. & Wernersson, B. Symptom overlap between postprandial distress and epigastric pain syndromes of the Rome III dyspepsia classification. Am. J. Gastroenterol. 108, 767–774 (2013).
Vanheel, H. et al. Pathophysiological abnormalities in functional dyspepsia subgroups according to the Rome III criteria. Am. J. Gastroenterol. 112, 132–140 (2017).
Wang, A. et al. The clinical overlap between functional dyspepsia and irritable bowel syndrome based on Rome III criteria. BMC Gastroenterol. 8, 43 (2008).
Yamawaki, H. et al. Impact of sleep disorders, quality of life and gastric emptying in distinct subtypes of functional dyspepsia in Japan. J. Neurogastroenterol. Motil. 20, 104–112 (2014).
Zagari, R. M. et al. Epidemiology of functional dyspepsia and subgroups in the Italian general population: an endoscopic study. Gastroenterology 138, 1302–1311 (2010).
Van den Houte, K. et al. Effects of Rome IV definitions of functional dyspepsia subgroups in secondary care. Clin. Gastroenterol. Hepatol. 19, 1620–1626 (2021).
Carbone, F., Holvoet, L. & Tack, J. Rome III functional dyspepsia subdivision in PDS and EPS: recognizing postprandial symptoms reduces overlap. Neurogastroenterol. Motil. 27, 1069–1074 (2015).
Aono, S. et al. Epidemiology and clinical characteristics based on the Rome III and IV criteria of Japanese patients with functional dyspepsia. J. Clin. Med. 11, 2342 (2022).
Cheng, J. et al. The overlap subgroup of functional dyspepsia exhibits more severely impaired gastric and autonomic functions. J. Clin. Gastroenterol. 58, 31–38 (2024).
Turco, R. et al. Do distinct functional dyspepsia subtypes exist in children? J. Pediatr. Gastroenterol. Nutr. 62, 387–392 (2016).
Aziz, I. et al. Epidemiology, clinical characteristics, and associations for Rome IV functional nausea and vomiting disorders in adults. Clin. Gastroenterol. Hepatol. 17, 878–886 (2019).
Josefsson, A. et al. Global prevalence and impact of rumination syndrome. Gastroenterology 162, 731–742.e9 (2022).
Heidelbaugh, J. J., Stelwagon, M., Miller, S. A., Shea, E. P. & Chey, W. D. The spectrum of constipation-predominant irritable bowel syndrome and chronic idiopathic constipation: US survey assessing symptoms, care seeking, and disease burden. Am. J. Gastroenterol. 110, 580–587 (2015).
Wong, R. K. et al. Inability of the Rome III criteria to distinguish functional constipation from constipation-subtype irritable bowel syndrome. Am. J. Gastroenterol. 105, 2228–2234 (2010).
Yadav, Y. S., Eslick, G. D. & Talley, N. J. Review article: irritable bowel syndrome: natural history, bowel habit stability and overlap with other gastrointestinal disorders. Aliment. Pharmacol. Ther. 54, S24–S32 (2021).
Ford, A. C. et al. Characteristics of functional bowel disorder patients: a cross-sectional survey using the Rome III criteria. Aliment. Pharmacol. Ther. 39, 312–321 (2014).
Rey, E., Balboa, A. & Mearin, F. Chronic constipation, irritable bowel syndrome with constipation and constipation with pain/discomfort: similarities and differences. Am. J. Gastroenterol. 109, 876–884 (2014).
Bouchoucha, M. et al. Painful or mild-pain constipation? A clinically useful alternative to classification as irritable bowel syndrome with constipation versus functional constipation. Dig. Dis. Sci. 63, 1763–1773 (2018).
Drossman, D. A. et al. Further characterization of painful constipation (PC): clinical features over one year and comparison with IBS. J. Clin. Gastroenterol. 42, 1080–1088 (2008).
Hyams, J. S. et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology 150, 1456–1468 (2016).
Rajindrajith, S., Devanarayana, N. M. & Benninga, M. A. Constipation and constipation-predominant irritable bowel syndrome: a comparative study using Rome III criteria. J. Pediatr. Gastroenterol. Nutr. 64, 679–684 (2017).
Di Lorenzo, C. et al. Efficacy and safety of linaclotide in treating functional constipation in paediatric patients: a randomised, double-blind, placebo-controlled, multicentre, phase 3 trial. Lancet Gastroenterol. Hepatol. 9, 238–250 (2024).
Singh, P. et al. Similarities in clinical and psychosocial characteristics of functional diarrhea and irritable bowel syndrome with diarrhea. Clin. Gastroenterol. Hepatol. 18, 399–405.e1 (2020).
Savarino, E. et al. Functional bowel disorders with diarrhoea: clinical guidelines of the United European Gastroenterology and European Society for Neurogastroenterology and Motility. United Eur. Gastroenterol. J. 10, 556–584 (2022).
Black, C. J., Ng, C. E., Goodoory, V. C. & Ford, A. C. Novel symptom subgroups in individuals with irritable bowel syndrome predict disease impact and burden. Clin. Gastroenterol. Hepatol. 22, 386–396.e10 (2024).
Van Oudenhove, L., Holvoet, L., Vandenberghe, J., Vos, R. & Tack, J. Do we have an alternative for the Rome III gastroduodenal symptom-based subgroups in functional gastroduodenal disorders? A cluster analysis approach. Neurogastroenterol. Motil. 23, 730–738 (2011).
Bouchoucha, M. et al. Data mining approach for the characterization of functional bowel disorders according to symptom intensity provides a small number of homogenous groups. Dig. Dis. 38, 310–319 (2020).
Black, C. J., Houghton, L. A. & Ford, A. C. Latent class analysis does not support the existence of Rome IV functional bowel disorders as discrete entities. Neurogastroenterol. Motil. 34, e14391 (2022).
Koloski, N. A., Jones, M., Young, M. & Talley, N. J. Differentiation of functional constipation and constipation predominant irritable bowel syndrome based on Rome III criteria: a population-based study. Aliment. Pharmacol. Ther. 41, 856–866 (2015).
Hreinsson, J. P. et al. Factor analysis of the Rome IV criteria for major disorders of gut-brain interaction (DGBI) globally and across geographical, sex, and age groups. Gastroenterology 164, 1211–1222 (2023).
Shekhar, C. et al. Rome III functional constipation and irritable bowel syndrome with constipation are similar disorders within a spectrum of sensitization, regulated by serotonin Gastroenterology 145, 749–757 (2013).
Bouchoucha, M. et al. Is-it possible to distinguish irritable bowel syndrome with constipation from functional constipation? Tech. Coloproctol. 21, 125–132 (2017).
Bouchoucha, M. et al. Is the colonic response to food different in IBS in contrast to simple constipation or diarrhea without abdominal pain? Dig. Dis. Sci. 56, 2947–2956 (2011).
Chiarioni, G., Kim, S. M., Vantini, I. & Whitehead, W. E. Validation of the balloon evacuation test: reproducibility and agreement with findings from anorectal manometry and electromyography. Clin. Gastroenterol. Hepatol. 12, 2049–2054 (2014).
Scarpato, E. et al. Prevalence of functional gastrointestinal disorders in children and adolescents in the Mediterranean region of Europe. Clin. Gastroenterol. Hepatol. 16, 870–876 (2018).
Steutel, N. F. et al. Prevalence of functional gastrointestinal disorders in European infants and toddlers. J. Pediatr. 221, 107–114 (2020).
Futagami, S. et al. Impact of coexisting irritable bowel syndrome and non-erosive reflux disease on postprandial abdominal fullness and sleep disorders in functional dyspepsia. J. Nippon. Med. Sch. 80, 362–370 (2013).
Kovacs, D. B., Szekely, A., Hubai, A. G. & Palsson, O. Prevalence, epidemiology and associated healthcare burden of Rome IV irritable bowel syndrome and functional dyspepsia in the adult population of Gibraltar. BMJ Open. Gastroenterol. 9, e000979 (2022).
Loosen, S. H., Kostev, K., Jordens, M. S., Luedde, T. & Roderburg, C. Overlap between irritable bowel syndrome and common gastrointestinal diagnoses: a retrospective cohort study of 29,553 outpatients in Germany. BMC Gastroenterol. 22, 48 (2022).
Barberio, B. et al. Overlap of Rome IV irritable bowel syndrome and functional dyspepsia and effect on natural history: a longitudinal follow-up study. Clin. Gastroenterol. Hepatol. 20, e89–e101 (2022).
Nam, K. et al. Gender difference in the overlap of irritable bowel syndrome and functional dyspepsia: a prospective nationwide multicenter study in Korea. J. Gastroenterol. 56, 537–546 (2021).
Choi, Y. J. et al. Overlap between irritable bowel syndrome and functional dyspepsia including subtype analyses. J. Gastroenterol. Hepatol. 32, 1553–1561 (2017).
Oshima, T. et al. Impacts of the COVID-19 pandemic on functional dyspepsia and irritable bowel syndrome: a population-based survey. J. Gastroenterol. Hepatol. 36, 1820–1827 (2021).
Nakov, R. et al. Prevalence of irritable bowel syndrome, functional dyspepsia and their overlap in Bulgaria: a population-based study. J. Gastrointest. Liver Dis. 29, 329–338 (2020).
von Wulffen, M. et al. Overlap of irritable bowel syndrome and functional dyspepsia in the clinical setting: prevalence and risk factors. Dig. Dis. Sci. 64, 480–486 (2019).
Perveen, I., Rahman, M. M., Saha, M., Rahman, M. M. & Hasan, M. Q. Prevalence of irritable bowel syndrome and functional dyspepsia, overlapping symptoms, and associated factors in a general population of Bangladesh. Indian. J. Gastroenterol. 33, 265–273 (2014).
Corsetti, M., Caenepeel, P., Fischler, B., Janssens, J. & Tack, J. Impact of coexisting irritable bowel syndrome on symptoms and pathophysiological mechanisms in functional dyspepsia. Am. J. Gastroenterol. 99, 1152–1159 (2004).
Kim, S. Y. et al. Self-reported sleep impairment in functional dyspepsia and irritable bowel syndrome. J. Neurogastroenterol. Motil. 24, 280–288 (2018).
Colombo, J. M., Deacy, A. D., Schurman, J. V. & Friesen, C. A. Heartburn in children and adolescents in the presence of functional dyspepsia and/or irritable bowel syndrome correlates with the presence of sleep disturbances, anxiety, and depression. Medicine 100, e25426 (2021).
Edwards, T., Friesen, C. & Schurman, J. V. Classification of pediatric functional gastrointestinal disorders related to abdominal pain using Rome III vs. Rome IV criterions. BMC Gastroenterol. 18, 41 (2018).
Helgeland, H. et al. Diagnosing pediatric functional abdominal pain in children (4–15 years old) according to the Rome III criteria: results from a Norwegian prospective study. J. Pediatr. Gastroenterol. Nutr. 49, 309–315 (2009).
Karabulut, G. S. et al. The incidence of irritable bowel syndrome in children using the Rome III criteria and the effect of trimebutine treatment. J. Neurogastroenterol. Motil. 19, 90–93 (2013).
Schurman, J. V. et al. Diagnosing functional abdominal pain with the Rome II criteria: parent, child, and clinician agreement. J. Pediatr. Gastroenterol. Nutr. 41, 291–295 (2005).
Schurman, J. V., Karazsia, B. T. & Friesen, C. A. Examination of competing diagnostic models of functional gastrointestinal disorders related to pain in children. Neurogastroenterol. Motil. 29 (2017).
Friesen, C. A., Rosen, J. M. & Schurman, J. V. Prevalence of overlap syndromes and symptoms in pediatric functional dyspepsia. BMC Gastroenterol. 16, 75 (2016).
Saps, M., Velasco-Benitez, C. A., Langshaw, A. H. & Ramirez-Hernandez, C. R. Prevalence of functional gastrointestinal disorders in children and adolescents: comparison between Rome III and Rome IV criteria. J. Pediatr. 199, 212–216 (2018).
de Bortoli, N. et al. Functional heartburn overlaps with irritable bowel syndrome more often than GERD. Am. J. Gastroenterol. 111, 1711–1717 (2016).
Neumann, H., Monkemuller, K., Kandulski, A. & Malfertheiner, P. Dyspepsia and IBS symptoms in patients with NERD, ERD and Barrett’s esophagus. Dig. Dis. 26, 243–247 (2008).
Noh, Y. W., Jung, H. K., Kim, S. E. & Jung, S. A. Overlap of erosive and non-erosive reflux diseases with functional gastrointestinal disorders according to Rome III criteria. J. Neurogastroenterol. Motil. 16, 148–156 (2010).
Sun, G. et al. Co-occurrence of fecal incontinence with constipation or irritable bowel syndrome indicates the need for personalized treatment. Neurogastroenterol. Motil. 35, e14633 (2023).
Atarodi, S., Rafieian, S. & Whorwell, P. J. Faecal incontinence – the hidden scourge of irritable bowel syndrome: a cross-sectional study. BMJ Open. Gastroenterol. 1, e000002 (2014).
Goodoory, V. C., Ng, C. E., Black, C. J. & Ford, A. C. Prevalence and impact of faecal incontinence among individuals with Rome IV irritable bowel syndrome. Aliment. Pharmacol. Ther. 57, 1083–1092 (2023).
Hunt, M. G., Wong, C., Aajmain, S. & Dawodu, I. Fecal incontinence in people with self-reported irritable bowel syndrome: prevalence and quality of life. J. Psychosom. Res. 113, 45–51 (2018).
Simren, M. et al. Fecal incontinence in irritable bowel syndrome: prevalence and associated factors in Swedish and American patients. Neurogastroenterol. Motil. 29, nmo.12919 (2017).
Sze, E. H., Barker, C. D. & Hobbs, G. A cross-sectional survey of the relationship between fecal incontinence and constipation. Int. Urogynecol. J. 24, 61–65 (2013).
Andy, U. U., Harvie, H. S., Pahwa, A. P., Markland, A. & Arya, L. A. The relationship between fecal incontinence, constipation and defecatory symptoms in women with pelvic floor disorders. Neurourol. Urodyn. 36, 495–498 (2017).
Meinds, R. J., van Meegdenburg, M. M., Trzpis, M. & Broens, P. M. On the prevalence of constipation and fecal incontinence, and their co-occurrence, in the Netherlands. Int. J. Colorectal Dis. 32, 475–483 (2017).
Andy, U. U. et al. Shared risk factors for constipation, fecal incontinence, and combined symptoms in older U.S. adults. J. Am. Geriatr. Soc. 64, e183–e188 (2016).
Gulewitsch, M. D., Enck, P., Schwille-Kiuntke, J., Weimer, K. & Schlarb, A. A. Rome III criteria in parents’ hands: pain-related functional gastrointestinal disorders in community children and associations with somatic complaints and mental health. Eur. J. Gastroenterol. Hepatol. 25, 1223–1229 (2013).
Bouzios, I., Chouliaras, G., Chrousos, G. P., Roma, E. & Gemou-Engesaeth, V. Functional gastrointestinal disorders in Greek children based on ROME III criteria: identifying the child at risk. Neurogastroenterol. Motil. 29, nmo.12951 (2017).
Velasco-Benitez, C. A. et al. Overlapping of functional gastrointestinal disorders in latinamerican schoolchildrens and adolescents [Spanish]. Rev. Chil. Pediatr. 89, 726–731 (2018).
Mulak, A. & Paradowski, L. Anorectal function and dyssynergic defecation in different subgroups of patients with irritable bowel syndrome. Int. J. Colorectal Dis. 25, 1011–1016 (2010).
Ahadi, T. et al. The effect of biofeedback therapy on dyssynergic constipation in patients with or without irritable bowel syndrome. J. Res. Med. Sci. 19, 950–955 (2014).
Patcharatrakul, T. & Gonlachanvit, S. Outcome of biofeedback therapy in dyssynergic defecation patients with and without irritable bowel syndrome. J. Clin. Gastroenterol. 45, 593–598 (2011).
Goyal, O., Bansal, M. & Sood, A. Clinical and anorectal manometry profile of patients with functional constipation and constipation-predominant irritable bowel syndrome. Indian. J. Gastroenterol. 38, 211–219 (2019).
Kaplan, A. I. et al. Experiencing multiple concurrent functional gastrointestinal disorders is associated with greater symptom severity and worse quality of life in chronic constipation and defecation disorders. Neurogastroenterol. Motil. 35, e14524 (2023).
Lv, C. L. et al. Colorectal motility patterns and psychiatric traits in functional constipation and constipation-predominant irritable bowel syndrome: a study from China. World J. Gastroenterol. 29, 5657–5667 (2023).
Shah, N. et al. Clinical and investigative assessment of constipation: a study from a referral center in western India. Indian. J. Gastroenterol. 33, 530–536 (2014).
Nyam, D. C., Pemberton, J. H., Ilstrup, D. M. & Rath, D. M. Long-term results of surgery for chronic constipation. Dis. Colon. Rectum 40, 273–279 (1997).
Glia, A., Lindberg, G., Nilsson, L. H., Mihocsa, L. & Akerlund, J. E. Constipation assessed on the basis of colorectal physiology. Scand. J. Gastroenterol. 33, 1273–1279 (1998).
Nullens, S. et al. Regional colon transit in patients with dys-synergic defaecation or slow transit in patients with constipation. Gut 61, 1132–1139 (2012).
Tanner, S. et al. Prevalence and clinical characteristics of dyssynergic defecation and slow transit constipation in patients with chronic constipation. J. Clin. Med. 10, 2027 (2021).
Bouin, M. et al. Intolerance to visceral distension in functional dyspepsia or irritable bowel syndrome: an organ specific defect or a pan intestinal dysregulation? Neurogastroenterol. Motil. 16, 311–314 (2004).
Simren, M. et al. Visceral hypersensitivity is associated with GI symptom severity in functional GI disorders: consistent findings from five different patient cohorts. Gut 67, 255–262 (2018).
Stanghellini, V. et al. Dyspeptic symptoms and gastric emptying in the irritable bowel syndrome. Am. J. Gastroenterol. 97, 2738–2743 (2002).
Gonlachanvit, S., Maurer, A. H., Fisher, R. S. & Parkman, H. P. Regional gastric emptying abnormalities in functional dyspepsia and gastro-oesophageal reflux disease. Neurogastroenterol. Motil. 18, 894–904 (2006).
Shimura, S. et al. Small intestinal bacterial overgrowth in patients with refractory functional gastrointestinal disorders. J. Neurogastroenterol. Motil. 22, 60–68 (2016).
JohnBritto, J. S. et al. Gender-specific insights into the irritable bowel syndrome pathophysiology. Focus on gut dysbiosis and permeability. Eur. J. Intern. Med. 125, 10–18 (2024).
Pecyna, P. et al. Gender influences gut microbiota among patients with irritable bowel syndrome. Int J. Mol. Sci. 24, 10424 (2023).
Alonso, C. et al. Acute experimental stress evokes a differential gender-determined increase in human intestinal macromolecular permeability. Neurogastroenterol. Motil. 24, 740–746 (2012).
Van den Houte, K., Bercik, P., Simren, M., Tack, J. & Vanner, S. Mechanisms underlying food-triggered symptoms in disorders of gut–brain interactions. Am. J. Gastroenterol. 117, 937–946 (2022).
Burns, G. et al. Evidence for local and systemic immune activation in functional dyspepsia and the irritable bowel syndrome: a systematic review. Am. J. Gastroenterol. 114, 429–436 (2019).
Ronkainen, J. et al. Duodenal eosinophilia is associated with functional dyspepsia and new onset gastro-oesophageal reflux disease. Aliment. Pharmacol. Ther. 50, 24–32 (2019).
Lembo, A., Zaman, M., Jones, M. & Talley, N. J. Influence of genetics on irritable bowel syndrome, gastro-oesophageal reflux and dyspepsia: a twin study. Aliment. Pharmacol. Ther. 25, 1343–1350 (2007).
Schruers, K., Koning, K., Luermans, J., Haack, M. J. & Griez, E. Obsessive-compulsive disorder: a critical review of therapeutic perspectives. Acta Psychiatr. Scand. 111, 261–271 (2005).
Chey, W. D., Pare, P., Viegas, A., Ligozio, G. & Shetzline, M. A. Tegaserod for female patients suffering from IBS with mixed bowel habits or constipation: a randomized controlled trial. Am. J. Gastroenterol. 103, 1217–1225 (2008).
Tack, J. & Camilleri, M. New developments in the treatment of gastroparesis and functional dyspepsia. Curr. Opin. Pharmacol. 43, 111–117 (2018).
Garsed, K. et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut 63, 1617–1625 (2014).
Ingrosso, M. R. et al. Systematic review and meta-analysis: efficacy of peppermint oil in irritable bowel syndrome. Aliment. Pharmacol. Ther. 56, 932–941 (2022).
Li, J. et al. A combination of peppermint oil and caraway oil for the treatment of functional dyspepsia: a systematic review and meta-analysis. Evid. Based Complement. Altern. Med. 2019, 7654947 (2019).
Jones, M. P., Guthrie-Lyons, L., Sato, Y. A. & Talley, N. J. Factors associated with placebo treatment response in functional dyspepsia clinical trials. Am. J. Gastroenterol. 118, 685–691 (2023).
Black, C. J., Staudacher, H. M. & Ford, A. C. Efficacy of a low FODMAP diet in irritable bowel syndrome: systematic review and network meta-analysis. Gut 71, 1117–1126 (2022).
Goyal, O. et al. Low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols diet versus traditional dietary advice for functional dyspepsia: a randomized controlled trial. J. Gastroenterol. Hepatol. 37, 301–309 (2022).
Nojkov, B. et al. The influence of co-morbid IBS and psychological distress on outcomes and quality of life following PPI therapy in patients with gastro-oesophageal reflux disease. Aliment. Pharmacol. Ther. 27, 473–482 (2008).
Piacentino, D. et al. Psychopathological features of irritable bowel syndrome patients with and without functional dyspepsia: a cross sectional study. BMC Gastroenterol. 11, 94 (2011).
Basnayake, C. et al. Long-term outcome of multidisciplinary versus standard gastroenterologist care for functional gastrointestinal disorders: a randomized trial. Clin. Gastroenterol. Hepatol. 20, 2102–2111.e9 (2022).
Basnayake, C. et al. Standard gastroenterologist versus multidisciplinary treatment for functional gastrointestinal disorders (MANTRA): an open-label, single-centre, randomised controlled trial. Lancet Gastroenterol. Hepatol. 5, 890–899 (2020).
Chey, W. D., Keefer, L., Whelan, K. & Gibson, P. R. Behavioral and diet therapies in integrated care for patients with irritable bowel syndrome. Gastroenterology 160, 47–62 (2021).
Sainsbury, A., Sanders, D. S. & Ford, A. C. Prevalence of irritable bowel syndrome-type symptoms in patients with celiac disease: a meta-analysis. Clin. Gastroenterol. Hepatol. 11, 359–365.e1 (2013).
Silvester, J. A. et al. Symptoms of functional intestinal disorders are common in patients with celiac disease following transition to a gluten-free diet. Dig. Dis. Sci. 62, 2449–2454 (2017).
Parker, S. et al. Functional gastrointestinal disorders and associated health impairment in individuals with celiac disease. Clin. Gastroenterol. Hepatol. 20, 1315–1325.e4 (2022).
Saps, M., Adams, P., Bonilla, S. & Nichols-Vinueza, D. Abdominal pain and functional gastrointestinal disorders in children with celiac disease. J. Pediatr. 162, 505–509 (2013).
Saps, M. et al. Abdominal pain-associated functional gastrointestinal disorder prevalence in children and adolescents with celiac disease on gluten-free diet: a multinational study. J. Pediatr. 182, 150–154 (2017).
Cristofori, F. et al. Functional abdominal pain disorders and constipation in children on gluten-free diet. Clin. Gastroenterol. Hepatol. 19, 2551–2558 (2021).
Turco, R. et al. The association of coeliac disease in childhood with functional gastrointestinal disorders: a prospective study in patients fulfilling Rome III criteria. Aliment. Pharmacol. Ther. 34, 783–789 (2011).
Veeraraghavan, G. et al. Non-responsive celiac disease in children on a gluten free diet. World J. Gastroenterol. 27, 1311–1320 (2021).
Fairbrass, K. M., Costantino, S. J., Gracie, D. J. & Ford, A. C. Prevalence of irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease in remission: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 5, 1053–1062 (2020).
Nigam, G. B., Limdi, J. K., Hamdy, S. & Vasant, D. H. The prevalence and burden of Rome IV functional colorectal disorders in ulcerative colitis. Gut 68, A203–A204 (2019).
Zimmerman, L. A. et al. The overlap of functional abdominal pain in pediatric Crohn’s disease. Inflamm. Bowel Dis. 19, 826–831 (2013).
Diederen, K. et al. The prevalence of irritable bowel syndrome-type symptoms in paediatric inflammatory bowel disease, and the relationship with biochemical markers of disease activity. Aliment. Pharmacol. Ther. 44, 181–188 (2016).
Watson, K. L. Jr., Kim, S. C., Boyle, B. M. & Saps, M. Prevalence and impact of functional abdominal pain disorders in children with inflammatory bowel diseases (IBD-FAPD). J. Pediatr. Gastroenterol. Nutr. 65, 212–217 (2017).
Tran, L. C. et al. Functional abdominal pain disorders and patient- and parent-reported outcomes in children with inflammatory bowel disease in remission. Dig. Liver Dis. 53, 1268–1275 (2021).
Limbri, L. F., Wilson, T. G. & Oliver, M. R. Prevalence of irritable bowel syndrome and functional abdominal pain disorders in children with inflammatory bowel disease in remission. JGH Open. 6, 818–823 (2022).
Kamp, E. J., Kane, J. S. & Ford, A. C. Irritable bowel syndrome and microscopic colitis: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 14, 659–668 (2016).
Kane, J. S., Irvine, A. J., Derwa, Y., Rotimi, O. & Ford, A. C. High prevalence of irritable bowel syndrome-type symptoms in microscopic colitis: implications for treatment. Ther. Adv. Gastroenterol. 11, 1756284818783600 (2018).
Pagoldh, J., Lundgren, D., Suhr, O. B. & Karling, P. Irritable bowel syndrome-like symptoms in treated microscopic colitis patients compared with controls: a cross-sectional study. Gastroenterol. Rep. 8, 374–380 (2020).
Cohen, E. et al. Increased risk for irritable bowel syndrome after acute diverticulitis. Clin. Gastroenterol. Hepatol. 11, 1614–1619 (2013).
Carabotti, M. et al. Site and duration of abdominal pain discriminate symptomatic uncomplicated diverticular disease from previous diverticulitis patients. Intern. Emerg. Med. 19, 1235-1245 (2024).
Barbara, G. et al. Rome Foundation Working Team Report on post-infection irritable bowel syndrome. Gastroenterology 156, 46–58.e7 (2019).
Klem, F. et al. Prevalence, risk factors, and outcomes of irritable bowel syndrome after infectious enteritis: a systematic review and meta-analysis. Gastroenterology 152, 1042–1054.e1 (2017).
Futagami, S., Itoh, T. & Sakamoto, C. Systematic review with meta-analysis: post-infectious functional dyspepsia. Aliment. Pharmacol. Ther. 41, 177–188 (2015).
Saps, M. et al. Post-infectious functional gastrointestinal disorders in children. J. Pediatr. 152, 812-816.e1 (2008).
Pensabene, L. et al. Postinfectious functional gastrointestinal disorders in children: a multicenter prospective study. J. Pediatr. 166, 903–907.e1 (2015).
Cremon, C. et al. Salmonella gastroenteritis during childhood is a risk factor for irritable bowel syndrome in adulthood. Gastroenterology 147, 69–77 (2014).
Wadhwa, A. et al. High risk of post-infectious irritable bowel syndrome in patients with Clostridium difficile infection. Aliment. Pharmacol. Ther. 44, 576–582 (2016).
Gutiérrez, R. L., Riddle, M. S. & Porter, C. K. Increased risk of functional gastrointestinal sequelae after Clostridium difficile infection among active duty United States military personnel (1998–2010). Gastroenterology 149, 1408–1414 (2015).
Rahman, M. M. et al. Long-term gastrointestinal consequences are frequent following sporadic acute infectious diarrhea in a tropical country: a prospective cohort study. Am. J. Gastroenterol. 113, 1363–1375 (2018).
Marasco, G. et al. Post COVID-19 irritable bowel syndrome. Gut 72, 484–492 (2023).
Marasco, G. et al. Meta-analysis: post-COVID-19 functional dyspepsia and irritable bowel syndrome. Aliment. Pharmacol. Ther. 58, 6–15 (2023).
Farello, G. et al. Analysis of the impact of COVID-19 pandemic on functional gastrointestinal disorders among paediatric population. Eur. Rev. Med. Pharmacol. Sci. 25, 5836–5842 (2021).
Stepan, M. D. et al. Pediatric functional abdominal pain disorders following COVID-19. Life 12, 509 (2022).
Velasco-Benítez, C. A. & Ortiz-Rivera, C. J. Post-infectious functional gastrointestinal disorders in children after a non-severe dengue episode without warning signs. Biomedica 39, 93–100 (2019).
Tan, T. K., Saps, M., Lin, C. L. & Wei, C. C. Risks of irritable bowel syndrome in children with infantile urinary tract infection: a 13-year nationwide cohort study. J. Investig. Med. 66, 998–1003 (2018).
Barbara, G. et al. The intestinal microenvironment and functional gastrointestinal disorders. Gastroenterology 150, 1305–1318 (2016).
Boeckxstaens, G. et al. Fundamentals of neurogastroenterology: physiology/motility – sensation. Gastroenterology 150, 1292–1304 (2016).
Vanner, S. et al. Fundamentals of neurogastroenterology: basic science. Gastroenterology 150, 1280–1291 (2016).
Trott, N., Rej, A., Coleman, S. H. & Sanders, D. S. Adult celiac disease with persistent IBS-type symptoms: a pilot study of an adjuvant FODMAP diet. Gastroenterol. Hepatol. Bed Bench 14, 304–310 (2021).
Roncoroni, L. et al. A low FODMAP gluten-free diet improves functional gastrointestinal disorders and overall mental health of celiac disease patients: a randomized controlled trial. Nutrients. 10 (2018).
van Megen, F. et al. A low FODMAP diet reduces symptoms in treated celiac patients with ongoing symptoms – a randomized controlled trial. Clin. Gastroenterol. Hepatol. 20, 2258–2266.e3 (2022).
Barbaro, M. R. et al. Non-celiac gluten sensitivity in the context of functional gastrointestinal disorders. Nutrients 12, 3735 (2020).
Borghini, R. et al. Beneficial effects of a low-nickel diet on relapsing IBS-like and extraintestinal symptoms of celiac patients during a proper gluten-free diet: nickel allergic contact mucositis in suspected non-responsive celiac disease. Nutrients 12, 2277 (2020).
Keohane, J. et al. Irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease: a real association or reflection of occult inflammation? Am. J. Gastroenterol. 105, 1789–1794 (2010).
Vivinus-Nebot, M. et al. Functional bowel symptoms in quiescent inflammatory bowel diseases: role of epithelial barrier disruption and low-grade inflammation. Gut 63, 744–752 (2014).
van Hoboken, E. A. et al. Symptoms in patients with ulcerative colitis in remission are associated with visceral hypersensitivity and mast cell activity. Scand. J. Gastroenterol. 46, 981–987 (2011).
Faure, C. & Giguere, L. Functional gastrointestinal disorders and visceral hypersensitivity in children and adolescents suffering from Crohn’s disease. Inflamm. Bowel Dis. 14, 1569–1574 (2008).
Mavroudis, G., Strid, H., Jonefjall, B. & Simren, M. Visceral hypersensitivity is together with psychological distress and female gender associated with severity of IBS-like symptoms in quiescent ulcerative colitis. Neurogastroenterol. Motil. 33, e13998 (2021).
Casén, C. et al. Deviations in human gut microbiota: a novel diagnostic test for determining dysbiosis in patients with IBS or IBD. Aliment. Pharmacol. Ther. 42, 71–83 (2015).
Gracie, D. J., Guthrie, E. A., Hamlin, P. J. & Ford, A. C. Bi-directionality of brain–gut interactions in patients with inflammatory bowel disease. Gastroenterology 154, 1635–1646.e3 (2018).
Duboc, H. et al. Connecting dysbiosis, bile-acid dysmetabolism and gut inflammation in inflammatory bowel diseases. Gut 62, 531–539 (2013).
Walter, S. A., Münch, A., Ost, A. & Ström, M. Anorectal function in patients with collagenous colitis in active and clinically quiescent phase, in comparison with healthy controls. Neurogastroenterol. Motil. 22, 534–e118 (2010).
Hertz, S. et al. Microscopic colitis patients possess a perturbed and inflammatory gut microbiota. Dig. Dis. Sci. 67, 2433–2443 (2022).
Moayyedi, P. et al. Small intestine in lymphocytic and collagenous colitis: mucosal morphology, permeability, and secretory immunity to gliadin. J. Clin. Pathol. 50, 527–529 (1997).
Münch, A. et al. Low levels of bile acids increase bacterial uptake in colonic biopsies from patients with collagenous colitis in remission. Aliment. Pharmacol. Ther. 33, 954–960 (2011).
Kvasnovsky, C. L. et al. Clinical and symptom scores are significantly correlated with fecal microbiota features in patients with symptomatic uncomplicated diverticular disease: a pilot study. Eur. J. Gastroenterol. Hepatol. 30, 107–112 (2018).
Barbara, G. et al. Gut microbiota, metabolome and immune signatures in patients with uncomplicated diverticular disease. Gut 66, 1252–1261 (2017).
Barbaro, M. R. et al. Nerve fiber overgrowth in patients with symptomatic diverticular disease. Neurogastroenterol. Motil. 31, e13575 (2019).
Bassotti, G., Battaglia, E., Spinozzi, F., Pelli, M. A. & Tonini, M. Twenty-four hour recordings of colonic motility in patients with diverticular disease: evidence for abnormal motility and propulsive activity. Dis. Colon. Rectum 44, 1814–1820 (2001).
Golder, M. et al. Longitudinal muscle shows abnormal relaxation responses to nitric oxide and contains altered levels of NOS1 and elastin in uncomplicated diverticular disease. Colorectal Dis. 9, 218–228 (2007).
Horgan, A. F., McConnell, E. J., Wolff, B. G. & Paterson, S The, C. Atypical diverticular disease: surgical results. Dis. Colon. Rectum 44, 1315-1318 (2001).
Narayan, R. & Floch, M. Microscopic colitis as part of the the natural history of diverticular disease. Am. J. Gastroenterol. 97, S112 (2002).
Turco, F. et al. Bacterial stimuli activate nitric oxide colonic mucosal production in diverticular disease. Protective effects of L. casei DG® (Lactobacillus paracasei CNCM I-1572). United Eur. Gastroenterol. J. 5, 715–724 (2017).
Jalanka, J., Salonen, A., Fuentes, S. & de Vos, W. M. Microbial signatures in post-infectious irritable bowel syndrome – toward patient stratification for improved diagnostics and treatment. Gut Microbes 6, 364–369 (2015).
Jalanka-Tuovinen, J. et al. Faecal microbiota composition and host–microbe cross-talk following gastroenteritis and in postinfectious irritable bowel syndrome. Gut 63, 1737–1745 (2014).
Sundin, J. et al. Altered faecal and mucosal microbial composition in post-infectious irritable bowel syndrome patients correlates with mucosal lymphocyte phenotypes and psychological distress. Aliment. Pharmacol. Ther. 41, 342–351 (2015).
Edogawa, S. et al. Serine proteases as luminal mediators of intestinal barrier dysfunction and symptom severity in IBS. Gut 69, 62–73 (2020).
Marshall, J. K. et al. Intestinal permeability in patients with irritable bowel syndrome after a waterborne outbreak of acute gastroenteritis in Walkerton, Ontario. Aliment. Pharmacol. Ther. 20, 1317–1322 (2004).
Dunlop, S. P. et al. Abnormal intestinal permeability in subgroups of diarrhea-predominant irritable bowel syndromes. Am. J. Gastroenterol. 101, 1288–1294 (2006).
Spiller, R. C. et al. Increased rectal mucosal enteroendocrine cells, T lymphocytes, and increased gut permeability following acute Campylobacter enteritis and in post-dysenteric irritable bowel syndrome. Gut 47, 804–811 (2000).
Wang, L. H., Fang, X. C. & Pan, G. Z. Bacillary dysentery as a causative factor of irritable bowel syndrome and its pathogenesis. Gut 53, 1096–1101 (2004).
Park, J. H. et al. Mucosal mast cell counts correlate with visceral hypersensitivity in patients with diarrhea predominant irritable bowel syndrome. J. Gastroenterol. Hepatol. 21, 71–78 (2006).
Cremon, C. et al. Mucosal immune activation in irritable bowel syndrome: gender-dependence and association with digestive symptoms. Am. J. Gastroenterol. 104, 392–400 (2009).
Sundin, J., Rangel, I., Kumawat, A. K., Hultgren-Hörnquist, E. & Brummer, R. J. Aberrant mucosal lymphocyte number and subsets in the colon of post-infectious irritable bowel syndrome patients. Scand. J. Gastroenterol. 49, 1068–1075 (2014).
Chen, J., Zhang, Y. & Deng, Z. Imbalanced shift of cytokine expression between T helper 1 and T helper 2 (Th1/Th2) in intestinal mucosa of patients with post-infectious irritable bowel syndrome. BMC Gastroenterol. 12, 91 (2012).
Sundin, J., Rangel, I., Repsilber, D. & Brummer, R. J. Cytokine response after stimulation with key commensal bacteria differ in post-infectious irritable bowel syndrome (PI-IBS) patients compared to healthy controls. PLoS ONE 10, e0134836 (2015).
Villani, A. C. et al. Genetic risk factors for post-infectious irritable bowel syndrome following a waterborne outbreak of gastroenteritis. Gastroenterology 138, 1502–1513 (2010).
Swan, C. et al. Identifying and testing candidate genetic polymorphisms in the irritable bowel syndrome (IBS): association with TNFSF15 and TNFα. Gut 62, 985–994 (2013).
Baggus, E. M. R. et al. How to manage adult coeliac disease: perspective from the NHS England Rare Diseases Collaborative Network for Non-Responsive and Refractory Coeliac Disease. Frontline Gastroenterol. 11, 235–242 (2020).
Green, P. H. et al. An association between microscopic colitis and celiac disease. Clin. Gastroenterol. Hepatol. 7, 1210–1216 (2009).
Vijayvargiya, P. et al. Increased fecal bile acid excretion in a significant subset of patients with other inflammatory diarrheal diseases. Dig. Dis. Sci. 67, 2413–2419 (2022).
Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition Cephalalgia 38 1 211 (2018).
Jones, K. R. et al. Comorbid disorders and symptons in irritable bowel syndrome (IBS) compared to other gastroenterology patients. Gastroenterology 120, A66 (2001).
Si, J.-M., Wang, L.-J., Chen, S.-J., Sun, L.-M. & Dai, N. Irritable bowel syndrome consulters in Zhejiang province: the symptoms pattern, predominant bowel habit subgroups and quality of life. World J. Gastroenterol. 10, 1059–1064 (2004).
Whitehead, W. E. et al. Comorbidity in irritable bowel syndrome. Am. J. Gastroenterol. 102, 2767–2776 (2007).
Bin Abdulrahman, K. A., Alenazi, N. S., Albishri, S. B. & Alshehri, F. F. Association of migraine and irritable bowel syndrome in Saudi Arabia: a nationwide survey. BioMed. Res. Int. 2022, e8690562 (2022).
Cole, J. A., Rothman, K. J., Cabral, H. J., Zhang, Y. & Farraye, F. A. Migraine, fibromyalgia, and depression among people with IBS: a prevalence study. BMC Gastroenterol. 6, 26 (2006).
Lacy, B. et al. Factors associated with more frequent diagnostic tests and procedures in patients with irritable bowel syndrome. Ther. Adv. Gastroenterol. 12, 1756284818818326 (2019).
Ladabaum, U. et al. Diagnosis, comorbidities, and management of irritable bowel syndrome in patients in a large health maintenance organization. Clin. Gastroenterol. Hepatol 10, 37–45 (2012).
Wang, X. J., Ebbert, J. O., Loftus, C. G., Rosedahl, J. K. & Philpot, L. M. Comorbid extra-intestinal central sensitization conditions worsen irritable bowel syndrome in primary care patients. Neurogastroenterol. Motil. 35, e14546 (2023).
Chumpitazi, B. P. et al. Multisite pain is highly prevalent in children with functional abdominal pain disorders and is associated with increased morbidity. J. Pediatr. 236, 131–136 (2021).
Friesen, C., Singh, M., Singh, V. & Schurman, J. V. An observational study of headaches in children and adolescents with functional abdominal pain: relationship to mucosal inflammation and gastrointestinal and somatic symptoms. Medicine 97, e11395 (2018).
Devanarayana, N. M. et al. Abdominal pain-predominant functional gastrointestinal diseases in children and adolescents: prevalence, symptomatology, and association with emotional stress. J. Pediatr. Gastroenterol. Nutr. 53, 659–665 (2011).
Zanchi, C. et al. Fifteen-years follow-up in a cohort of children with functional gastrointestinal disorders: prevalence and risk factors to develop neuropsychiatric disorders and other comorbidities. Children 8, 838 (2021).
Cooper, B. C. & Kleinberg, I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders. Cranio 25, 114–126 (2007).
Gallotta, S. et al. High risk of temporomandibular disorder in irritable bowel syndrome: is there a correlation with greater illness severity? World J. Gastroenterol. 23, 103–109 (2017).
Sanders, A. E. et al. General health status and incidence of first-onset temporomandibular disorder: OPPERA prospective cohort study. J. Pain. 14, T51–T62 (2013).
Bair, M. J. & Krebs, E. E. Fibromyalgia. Ann. Intern. Med. 172, ITC33–ITC48 (2020).
Barton, A., Pal, B., Whorwell, P. J. & Marshall, D. Increased prevalence of sicca complex and fibromyalgia in patients with irritable bowel syndrome. Am. J. Gastroenterol. 94, 1898–1901 (1999).
Veale, D., Kavanagh, G., Fielding, J. F. & Fitzgerald, O. Primary fibromyalgia and the irritable bowel syndrome: different expressions of a common pathogenetic process. Br. J. Rheumatol. 30, 220–222 (1991).
Sperber, A. D. et al. Fibromyalgia in the irritable bowel syndrome: studies of prevalence and clinical implications. Am. J. Gastroenterol. 94, 3541–3546 (1999).
Sperber, A. D. et al. Use of the functional bowel disorder severity index (FBDSI) in a study of patients with the irritable bowel syndrome and fibromyalgia. Am. J. Gastroenterol. 95, 995–998 (2000).
Settembre, C. et al. Association among disorders of gut–brain interaction (DGBI) and fibromyalgia: a prospective study. J. Clin. Med. 11, 809 (2022).
Vandvik, P. O., Lydersen, S. & Farup, P. G. Prevalence, comorbidity and impact of irritable bowel syndrome in Norway. Scand. J. Gastroenterol. 41, 650–656 (2006).
Wojczynski, M. K., North, K. E., Pedersen, N. L. & Sullivan, P. F. Irritable bowel syndrome: a co-twin control analysis. Am. J. Gastroenterol. 102, 2220–2229 (2007).
Lee, O. Y. et al. Impact of advertisement and clinic populations in symptoms and perception of irritable bowel syndrome. Aliment. Pharmacol. Ther. 13, 1631–1638 (1999).
Aggarwal, V. R., McBeth, J., Zakrzewska, J. M., Lunt, M. & Macfarlane, G. J. The epidemiology of chronic syndromes that are frequently unexplained: do they have common associated factors? Int. J. Epidemiol. 35, 468–476 (2006).
Poitras, P., Gougeon, A., Binn, M. & Bouin, M. Extra digestive manifestations of irritable bowel syndrome: intolerance to drugs? Dig. Dis. Sci. 53, 2168–2176 (2008).
Yanartaş, Ö. et al. Depression and anxiety have unique contributions to somatic complaints in depression, irritable bowel syndrome and inflammatory bowel diseases. Psychiatry Clin. Psychopharmacol. 29, 418–426 (2019).
Fikree, A. et al. Functional gastrointestinal disorders are associated with the joint hypermobility syndrome in secondary care: a case-control study. Neurogastroenterol. Motil. 27, 569–579 (2015).
Locke, G. R., Zinsmeister, A. R., Talley, N. J., Fett, S. L. & Melton, L. J. Risk factors for irritable bowel syndrome: role of analgesics and food sensitivities. Am. J. Gastroenterol. 95, 157–165 (2000).
Schauer, B. et al. Irritable bowel syndrome, mental health, and quality of life: data from a population-based survey in Germany (SHIP-Trend-0). Neurogastroenterol. Motil. 31, e13511 (2019).
Laden, B. F. et al. Comorbidities in a nationwide, heterogenous population of veterans with interstitial cystitis/bladder pain syndrome. Urology 156, 37–43 (2021).
Clayton, A. H. & Valladares Juarez, E. M. Female sexual dysfunction. Med. Clin. North. Am. 103, 681–698 (2019).
Fass, R., Fullerton, S., Naliboff, B., Hirsh, T. & Mayer, E. A. Sexual dysfunction in patients with irritable bowel syndrome and non-ulcer dyspepsia. Digestion 59, 79–85 (1998).
Moore, J. S., Gibson, P. R., Perry, R. E. & Burgell, R. E. Endometriosis in patients with irritable bowel syndrome: specific symptomatic and demographic profile, and response to the low FODMAP diet. Aust. N. Z. J. Obstet. Gynaecol. 57, 201–205 (2017).
Ferries-Rowe, E., Corey, E. & Archer, J. S. Primary dysmenorrhea: diagnosis and therapy. Obstet. Gynecol. 136, 1047–1058 (2020).
Olafsdottir, L. B., Gudjonsson, H., Jonsdottir, H. H., Björnsson, E. & Thjodleifsson, B. Natural history of irritable bowel syndrome in women and dysmenorrhea: a 10-year follow-up study. Gastroenterol. Res. Pract. 2012, 534204 (2012).
Yamamoto, Y. et al. Association between menstrual pain and functional dyspepsia in a Japanese young population. Neurogastroenterol. Motil. 34, e14324 (2022).
Walker, E. A., Gelfand, A. N., Gelfand, M. D., Green, C. & Katon, W. J. Chronic pelvic pain and gynecological symptoms in women with irritable bowel syndrome. J. Psychosom. Obstet. Gynaecol. 17, 39–46 (1996).
Gagnon, C., Bélanger, L., Ivers, H. & Morin, C. M. Validation of the insomnia severity index in primary care. J. Am. Board. Fam. Med. 26, 701–710 (2013).
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213 (1989).
Ballou, S. et al. Sleep disturbances are commonly reported among patients presenting to a gastroenterology clinic. Dig. Dis. Sci. 63, 2983–2991 (2018).
Borji, R., Fereshtehnejad, S.-M., Vakili, S. T. T., Daryani, N. E. & Ajdarkosh, H. Association between irritable bowel syndrome and restless legs syndrome: a comparative study with control group. J. Neurogastroenterol. Motil. 18, 426–433 (2012).
Yun, C.-H. et al. Association between irritable bowel syndrome and restless legs syndrome in the general population. J. Sleep. Res. 21, 569–576 (2012).
Fass, R., Fullerton, S., Tung, S. & Mayer, E. A. Sleep disturbances in clinic patients with functional bowel disorders. Am. J. Gastroenterol. 95, 1195–2000 (2000).
Tang, B. et al. Epidemiology of globus symptoms and associated psychological factors in China. J. Dig. Dis. 17, 319–324 (2016).
Lacy, B. E., Everhart, K. & Crowell, M. D. Functional dyspepsia is associated with sleep disorders. Clin. Gastroenterol. Hepatol. 9, 410–414 (2011).
Wang, B., Duan, R. & Duan, L. Prevalence of sleep disorder in irritable bowel syndrome: a systematic review with meta-analysis. Saudi J. Gastroenterol. 24, 141–150 (2018).
Murphy, L. K. et al. Comorbid sleep disturbance in adolescents with functional abdominal pain. Behav. Sleep. Med. 19, 471–480 (2021).
Robbertz, A. S., Shneider, C., Cohen, L. L. & Reed, B. Sleep problems in pediatric disorders of gut–brain interaction: a systematic review. J. Pediatr. Psychol. 48, 778–786 (2023).
Thompson, P., Friesen, H. J., Schurman, J. V., Colombo, J. M. & Friesen, C. A. A cross-sectional study of sleep disturbances in children and adolescents with abdominal pain-associated disorders of gut–brain interaction. Clin. Pediatr. 63, 697-702 (2024).
Committee on the Diagnostic Criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome; Board on the Health of Select Populations; Institute of Medicine. Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness (National Academies Press, 2015).
Dansie, E. J. et al. Conditions comorbid with chronic fatigue in a population-based sample. Psychosomatics 53, 44–50 (2012).
Van Oudenhove, L., Vandenberghe, J., Vos, R., Holvoet, L. & Tack, J. Factors associated with co-morbid irritable bowel syndrome and chronic fatigue-like symptoms in functional dyspepsia. Neurogastroenterol. Motil. 23, 524–e202 (2011).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613 (2001).
Löwe, B. et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 122, 86–95 (2010).
Esterita, T., Dewi, S., Suryatenggara, F. G. & Glenardi, G. Association of functional dyspepsia with depression and anxiety: a systematic review. J. Gastrointestin Liver Dis. 30, 259–266 (2021).
Hu, Z. et al. The level and prevalence of depression and anxiety among patients with different subtypes of irritable bowel syndrome: a network meta-analysis. BMC Gastroenterol. 21, 23 (2021).
Zamani, M., Alizadeh-Tabari, S. & Zamani, V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment. Pharmacol. Ther. 50, 132–143 (2019).
Gale, C. R., Wilson, J. A. & Deary, I. J. Globus sensation and psychopathology in men: the Vietnam experience study. Psychosom. Med. 71, 1026–1031 (2009).
Robertson, A. R. What becomes of the frequent hospital attenders with centrally mediated gastrointestinal pain syndrome? Visc. Med. 36, 312–317 (2020).
Chitkara, D. K., Bredenoord, A. J., Rucker, M. J. & Talley, N. J. Aerophagia in adults: a comparison with functional dyspepsia. Aliment. Pharmacol. Ther. 22, 855–858 (2005).
Tse, A. W. Y. et al. Validation of self-administrated questionnaire for psychiatric disorders in patients with functional dyspepsia. J. Neurogastroenterol. Motil. 16, 52–60 (2010).
Shiha, M. G. et al. Increased psychological distress and somatization in patients with irritable bowel syndrome compared with functional diarrhea or functional constipation, based on Rome IV criteria. Neurogastroenterol. Motil. 33, e14121 (2021).
Thavamani, A., Umapathi, K. K., Velayuthan, S. & Sankararaman, S. Burden of psychiatric disorders in patients with cyclic vomiting syndrome – need for aggressive screening and early intervention. Dig. Liver Dis. 54, 287–289 (2022).
Goodoory, V. C. et al. Impact of psychological comorbidity on the prognosis of irritable bowel syndrome. Am. J. Gastroenterol. 116, 1485–1494 (2021).
Hosseinzadeh, S. T., Poorsaadati, S., Radkani, B. & Forootan, M. Psychological disorders in patients with chronic constipation. Gastroenterol. Hepatol. Bed Bench 4, 159–163 (2011).
Robertson, N., Javed, N., Samani, N. J. & Khunti, K. Psychological morbidity and illness appraisals of patients with cardiac and non-cardiac chest pain attending a rapid access chest pain clinic: a longitudinal cohort study. Heart 94, e12 (2008).
Rommel, N. et al. Esophageal sensorimotor function and psychological factors each contribute to symptom severity in globus patients. Am. J. Gastroenterol. 111, 1382–1388 (2016).
Foldes-Busque, G. et al. Unexplained chest pain in the ED: could it be panic? Am. J. Emerg. Med. 29, 743–751 (2011).
Goodoory, V.C., Houghton, L.A., Black, C.J. & Ford, A.C. Characteristics of, and natural history among, individuals with Rome IV functional bowel disorders. Neurogastroenterol. Motil. e14268 (2021).
von Gontard, A., Moritz, A.-M., Thome-Granz, S. & Equit, M. Abdominal pain symptoms are associated with anxiety and depression in young children. Acta Paediatr. 104, 1156–1163 (2015).
Nicolai, M. P. J. et al. The impact of sexual abuse in patients undergoing colonoscopy. PLoS ONE 9, e85034 (2014).
Shin, A., Xu, H. & Imperiale, T. F. The prevalence, humanistic burden, and health care impact of irritable bowel syndrome among United States veterans. Clin. Gastroenterol. Hepatol. 21, 1061–1069.e1 (2023).
Burton Murray, H. & Calabrese, S. Identification and management of eating disorders (including ARFID) in GI patients. Gastroenterol. Clin. North. Am. 51, 765–783 (2022).
Atkins, M. et al. History of trying exclusion diets and association with avoidant/restrictive food intake disorder in neurogastroenterology patients: a retrospective chart review. Neurogastroenterol. Motil. 35, e14513 (2023).
Murray, H. B. et al. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin. Gastroenterol. Hepatol. 18, 1995–2002.e1 (2020).
Kaul, I. et al. Avoidant/restrictive food intake disorder prevalence is high in children with gastroparesis and functional dyspepsia. Neurogastroenterol Motil. 2024:e14777.
Murray, H. B. et al. Prevalence and characteristics of avoidant/restrictive food intake disorder in pediatric neurogastroenterology patients. J. Pediatr. Gastroenterol. Nutr. 74, 588–592 (2022).
Azpiroz, F. et al. Mechanisms of hypersensitivity in IBS and functional disorders. Neurogastroenterol. Motil. 19, 62–88 (2007).
Bouin, M. et al. Rectal distention testing in patients with irritable bowel syndrome: sensitivity, specificity, and predictive values of pain sensory thresholds. Gastroenterology 122, 1771–1777 (2002).
Mertz, H., Naliboff, B., Munakata, J., Niazi, N. & Mayer, E. A. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology 109, 40–52 (1995).
Craig, A. D. How do you feel? Interoception: the sense of the physiological condition of the body. Nat. Rev. Neurosci. 3, 655–666 (2002).
Chang, L., Mayer, E. A., Johnson, T., FitzGerald, L. Z. & Naliboff, B. Differences in somatic perception in female patients with irritable bowel syndrome with and without fibromyalgia. Pain 84, 297–307 (2000).
Keefer, L. et al. Centrally mediated disorders of gastrointestinal pain. Gastroenterology 150, 1408–1419 (2016).
Drossman, D. A. et al. Neuromodulators for functional gastrointestinal disorders (disorders of gut−brain interaction): a Rome Foundation Working Team Report. Gastroenterology 154, 1140–1171.e1 (2018).
Sagami, Y. et al. Effect of a corticotropin releasing hormone receptor antagonist on colonic sensory and motor function in patients with irritable bowel syndrome. Gut 53, 958–964 (2004).
Gale, J. D. & Houghton, L. A. Alpha 2 delta (α2δ) ligands, gabapentin and pregabalin: what is the evidence for potential use of these ligands in irritable bowel syndrome. Front. Pharmacol. 2, 28 (2011).
Saito, Y. A. et al. Randomised clinical trial: pregabalin vs placebo for irritable bowel syndrome. Aliment. Pharmacol. Ther. 49, 389–397 (2019).
Klooker, T. K. et al. The mast cell stabiliser ketotifen decreases visceral hypersensitivity and improves intestinal symptoms in patients with irritable bowel syndrome. Gut 59, 1213–1221 (2010).
Wouters, M. M. et al. Histamine receptor H1-mediated sensitization of TRPV1 mediates visceral hypersensitivity and symptoms in patients with irritable bowel syndrome. Gastroenterology 150, 875–887.e9 (2016).
Houghton, L. A. et al. Age, gender and women’s health and the patient. Gastroenterology 150, 1332–1343 (2016).
Black, C. J. et al. A novel method to classify and subgroup patients with IBS based on gastrointestinal symptoms and psychological profiles. Am. J. Gastroenterol. 116, 372–381 (2021).
Han, C. J., Pike, K., Jarrett, M. E. & Heitkemper, M. M. Symptom-based latent classes of persons with irritable bowel syndrome. Res. Nurs. Health 42, 382–391 (2019).
Polster, A. et al. Mixture model analysis identifies irritable bowel syndrome subgroups characterised by specific profiles of gastrointestinal, extraintestinal somatic and psychological symptoms. Aliment. Pharmacol. Ther. 46, 529–539 (2017).
Polster, A. V. et al. Subgroups of IBS patients are characterized by specific, reproducible profiles of GI and non-GI symptoms and report differences in healthcare utilization: a population-based study. Neurogastroenterol. Motil. 31, e13483 (2019).
Chen, J. et al. Irritable bowel syndrome and migraine: evidence from Mendelian randomization analysis in the UK Biobank. Expert. Rev. Gastroenterol. Hepatol. 15, 1233–1239 (2021).
Eijsbouts, C. et al. Genome-wide analysis of 53,400 people with irritable bowel syndrome highlights shared genetic pathways with mood and anxiety disorders. Nat. Genet. 53, 1543–1552 (2021).
Gong, W. et al. Role of the gut–brain axis in the shared genetic etiology between gastrointestinal tract diseases and psychiatric disorders: a genome-wide pleiotropic analysis. JAMA Psychiatry 80, 360–370 (2023).
Bonfiglio, F. et al. Female-specific association between variants on chromosome 9 and self-reported diagnosis of irritable bowel syndrome. Gastroenterology 155, 168–179 (2018).
So, S. Y. & Savidge, T. C. Sex-bias in irritable bowel syndrome: linking steroids to the gut–brain axis. Front. Endocrinol. 12, 684096 (2021).
Callan, N. G. L., Mitchell, E. S., Heitkemper, M. M. & Woods, N. F. Abdominal pain during the menopause transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. Womens Midlife Health 5, 2 (2019).
Heitkemper, M. M. et al. Symptoms across the menstrual cycle in women with irritable bowel syndrome. Am. J. Gastroenterol. 98, 420–430 (2003).
Houghton, L. A., Lea, R., Jackson, N. & Whorwell, P. J. The menstrual cycle affects rectal sensitivity in patients with irritable bowel syndrome but not healthy volunteers. Gut 50, 471–474 (2002).
Koloski, N. A., Talley, N. J. & Boyce, P. M. Predictors of health care seeking for irritable bowel syndrome and nonulcer dyspepsia: a critical review of the literature on symptom and psychosocial factors. Am. J. Gastroenterol. 96, 1340–1349 (2001).
Maxion-Bergemann, S., Thielecke, F., Abel, F. & Bergemann, R. Costs of irritable bowel syndrome in the UK and US. Pharmacoeconomics 24, 21–37 (2006).
Midenfjord, I., Polster, A., Sjövall, H., Törnblom, H. & Simrén, M. Anxiety and depression in irritable bowel syndrome: exploring the interaction with other symptoms and pathophysiology using multivariate analyses. Neurogastroenterol. Motil. 31, e13619 (2019).
Spiegel, B. M. et al. Clinical determinants of health-related quality of life in patients with irritable bowel syndrome. Arch. Intern. Med. 164, 1773–1780 (2004).
Singh, P. et al. Psychiatric, somatic and other functional gastrointestinal disorders in patients with irritable bowel syndrome at a tertiary care center. J. Neurogastroenterol. Motil. 18, 324–331 (2012).
Norlin, A. K., Faresjo, A., Falk, M., Jones, M. P. & Walter, S. Primary healthcare utilisation and self-rated health among patients with irritable bowel syndrome: what are the impacts of comorbidities, gastrointestinal symptom burden, sense of coherence and stress? J. Psychosom. Res. 119, 1–7 (2019).
Clemens, J. Q., Erickson, D. R., Varela, N. P. & Lai, H. H. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J. Urol. 208, 34–42 (2022).
Shoohanizad, E., Garajei, A., Enamzadeh, A. & Yari, A. Nonsurgical management of temporomandibular joint autoimmune disorders. AIMS Public. Health 6, 554–567 (2019).
Sorensen, J., Bautista, K. E., Lamvu, G. & Feranec, J. Evaluation and treatment of female sexual pain: a clinical review. Cureus 10, e2379 (2018).
Marum, A. P., Moreira, C., Saraiva, F., Tomas-Carus, P. & Sousa-Guerreiro, C. A low fermentable oligo-di-mono saccharides and polyols (FODMAP) diet reduced pain and improved daily life in fibromyalgia patients. Scand. J. Pain. 13, 166–172 (2016).
Ringstrom, G., Abrahamsson, H., Strid, H. & Simren, M. Why do subjects with irritable bowel syndrome seek health care for their symptoms? Scand. J. Gastroenterol. 42, 1194–1203 (2007).
Burgell, R. E., Hoey, L., Norton, K. & Fitzpatrick, J. Treating disorders of brain–gut interaction with multidisciplinary integrated care. Moving towards a new standard of care. JGH Open. 8, e13072 (2024).
Staudacher, H. M., Black, C. J., Teasdale, S. B., Mikocka-Walus, A. & Keefer, L. Irritable bowel syndrome and mental health comorbidity – approach to multidisciplinary management. Nat. Rev. Gastroenterol. Hepatol. 20, 582–596 (2023).
Van Oudenhove, L. et al. Biopsychosocial aspects of functional gastrointestinal disorders. Gastroenterology 150, 1355–1367 (2016).
Keefer, L. et al. A Rome Working Team Report on brain–gut behavior therapies for disorders of gut–brain interaction. Gastroenterology 162, 300–315 (2022).
Aranburu, E. et al. Gluten and FODMAPs relationship with mental disorders: systematic review. Nutrients. 13 (2021).
Kortlever, T. L. et al. Low-FODMAP diet is associated with improved quality of life in IBS patients – a prospective observational study. Nutr. Clin. Pract. 34, 623–630 (2019).
Acknowledgements
This Working Team Report was supported by the Rome Foundation.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
G.B., L.C., S.N. and M. Simrén are on the Rome Foundation Board of Directors. G.B. declares consultancies, business interests or sources of honoraria payments from Aboca, AB Biotics, Agave, Alfa Sigma, AGPharma, Bayer, Biocodex, Boehringer, Bromatech, Cadigroup, Danone, Diadema, Falk Pharma, GE Healthcare, Giuliani, Mayoly, Malesci, Sanofi, Sofar and Yakult. L.C. is a consultant for AbbVie, Ardelyx, Atmo, Bausch Health, Food Marble, Ironwood Pharmaceuticals, Trellus Health and Vibrant; and receives grant support from AnX Robotica and Ironwood Pharmaceuticals. L.C. also has stock options in Food Marble, ModifyHealth and Trellus Health. S.N. is a consultant for Abbvie. M. Saps is a consultant for AbbVie and Ironwood, and has received study funding from QOL Medical. G.S. is a speaker and consultant for Sanofi/Regeneron, Salix, Phathom, Ardelyx, Ironwood, AbbVie and GI Health Foundation, and is a Council member of the American Neurogastroenterology and Motility Society. M. Simrén. is a consultant for Danone Nutricia Research, Biocodex, Tillotts, Takeda, Kyowa Kirin, Abbvie, BioGaia, Renapharma and Cinclus Pharma; and has received speaker fees from Tillotts, Kyowa Kirin, Takeda, Biocodex, Sanofi, Abbvie, Janssen Immunology, Pfizer, BioGaia, Renapharma, Mayoly and Bromatech. M. Simrén has also received unrestricted research grants from Genetic Analysis AS and BioGaia. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks Carolina Malagelada, Jose Remes-Troche and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barbara, G., Aziz, I., Ballou, S. et al. Rome Foundation Working Team Report on overlap in disorders of gut–brain interaction. Nat Rev Gastroenterol Hepatol 22, 228–251 (2025). https://doi.org/10.1038/s41575-024-01033-9
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41575-024-01033-9
This article is cited by
-
Overlap of ‘disorders of gut-brain interaction’: A type of diseases that require special attention
Indian Journal of Gastroenterology (2025)