Abstract
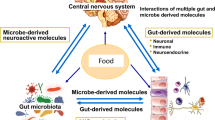
The effects of diet and nutrition extend beyond individual health: food intake before conception or during pregnancy and lactation can affect the health of offspring. Diet is one of the most powerful modulators of the gut microbiome, influencing gene–environment interactions, with several emerging mechanisms pointing to the microbiome–metabolite–epigenome axis. In this Review, we discuss the effect of dietary changes on the gametes (‘gut–germline axis’) or in utero (‘gut–neonatal axis’) that may change the predisposition of offspring to several non-communicable diseases. Examples of diets discussed are those that detrimentally modulate the parental microbiota and lead to epigenetic changes in the progeny, including Western diets characterized by high saturated fat and low protein or fibre intake. We summarize studies using animal models, which suggest that these diets can have long-lasting effects on the offspring microbiome, epigenome and phenotype, particularly across the cardiometabolic and immune systems, and discuss the limitations of current studies as well as future directions for the field. Translational research investigating the benefits of parental dietary interventions before and during pregnancy, mainly using personalized approaches, is needed. This would, in turn, reduce rates of non-communicable diseases in generations to come.
Key points
-
Maternal diet during pregnancy and lactation can shape offspring health by influencing the gut microbiota and epigenetic programming, contributing to the long-term risk of non-communicable diseases.
-
Fetal development is likely influenced by maternal microbial metabolites, rather than live microorganisms, that might cross the placenta; however, birth mode and maternal diet can shape early-life microbiota and epigenetic programming.
-
Maternal intake of methyl-donor nutrients such as choline influences offspring epigenetics via gut microbial metabolism, linking diet to neurodevelopment and long-term health outcomes.
-
Maternal protein, fat and fibre intake during pregnancy modulates offspring microbiota and epigenetics, influencing immune, metabolic and cognitive outcomes through metabolites such as short-chain fatty acids.
-
Paternal gut microbiota and diet influence sperm epigenetics and offspring health, supporting a gut–germline axis that links paternal exposures to metabolic and behavioural outcomes in offspring.
-
Despite promising findings, most evidence to link parental diet, gut microbiota and epigenetics to offspring health is from animal studies, highlighting the need for human data, which is likely to require personalized approaches.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Ho, Z. C. Principles of diet therapy in ancient Chinese medicine: ‘Huang Di Nei Jing’. Asia Pac. J. Clin. Nutr. 2, 91–95 (1993).
Keusch, G. T. The history of nutrition: malnutrition, infection and immunity. J. Nutr. 133, 336S–340S (2003).
Hu, C. et al. A maternal high-fat/low-fiber diet impairs glucose tolerance and induces the formation of glycolytic muscle fibers in neonatal offspring. Eur. J. Nutr. 60, 2709–2718 (2021).
Thone-Reineke, C. et al. High-protein nutrition during pregnancy and lactation programs blood pressure, food efficiency, and body weight of the offspring in a sex-dependent manner. Am. J. Physiol. Regul. Integr. Comp. Physiol. 291, R1025–R1030 (2006).
Barker, D. J., Osmond, C., Golding, J., Kuh, D. & Wadsworth, M. E. Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ 298, 564–567 (1989). First evidence of in utero effects and NCDs.
Schulz, L. C. The Dutch hunger winter and the developmental origins of health and disease. Proc. Natl Acad. Sci. USA 107, 16757–16758 (2010).
Ravelli, A. et al. Glucose tolerance in adults after prenatal exposure to famine. Lancet 351, 173–177 (1998).
Roseboom, T. J. Coronary heart disease after prenatal exposure to the Dutch famine, 1944-45. Heart 84, 595–598 (2000).
Tobi, E. W. et al. DNA methylation as a mediator of the association between prenatal adversity and risk factors for metabolic disease in adulthood. Sci. Adv. 4, eaao4364 (2018).
Fedotkina, O. et al. Perinatal famine is associated with excess risk of proliferative retinopathy in patients with type 2 diabetes. Acta Ophthalmol. 100, e539–e545 (2022).
Lumey, L. H., Khalangot, M. D. & Vaiserman, A. M. Association between type 2 diabetes and prenatal exposure to the Ukraine famine of 1932–33: a retrospective cohort study. Lancet Diabetes Endocrinol. 3, 787–794 (2015).
Chen, C. et al. Prenatal exposure to the Chinese famine of 1959–62 and risk of cardiovascular diseases in adulthood: findings from the China PEACE million persons project. Eur. J. Prev. Cardiol. 29, 2111–2119 (2022).
Yao, W., Li, L., Jiang, H., Yu, Y. & Xu, W. Transgenerational associations of parental famine exposure in early life with offspring risk of adult obesity in China. Obesity 31, 279–289 (2023).
Victora, C. G. et al. Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. Lancet 397, 1388–1399 (2021).
Conterno, L., Fava, F., Viola, R. & Tuohy, K. M. Obesity and the gut microbiota: does up-regulating colonic fermentation protect against obesity and metabolic disease? Genes Nutr. 6, 241–260 (2011).
Saklayen, M. G. The global epidemic of the metabolic syndrome. Curr. Hypertens. Rep. 20, 12 (2018).
Ferreira, S. R., Lerario, D. D., Gimeno, S. G. & Sanudo, A. Obesity and central adiposity in Japanese immigrants: role of the Western dietary pattern. J. Epidemiol. 12, 431–438 (2002).
Fung, T. T. et al. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am. J. Clin. Nutr. 73, 61–67 (2001).
Alae-Carew, C. et al. Analysis of dietary patterns and cross-sectional and longitudinal associations with hypertension, high BMI and type 2 diabetes in Peru. Public Health Nutr. 23, 1009–1019 (2020).
Rai, S. K. et al. The dietary approaches to stop hypertension (DASH) diet, Western diet, and risk of gout in men: prospective cohort study. BMJ 357, j1794 (2017).
Murray, C. J. L. et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396, 1223–1249 (2020).
Férézou-Viala, J. et al. Long-term consequences of maternal high-fat feeding on hypothalamic leptin sensitivity and diet-induced obesity in the offspring. Am. J. Physiol. Regul. Integr. Comp. Physiol. 293, R1056–R1062 (2007).
Maslova, E. et al. Maternal intake of fat in pregnancy and offspring metabolic health – a prospective study with 20 years of follow-up. Clin. Nutr. 35, 475–483 (2016).
Berger, S. L., Kouzarides, T., Shiekhattar, R. & Shilatifard, A. An operational definition of epigenetics. Genes Dev. 23, 781–783 (2009).
Riggs, A. D., Martienssen, R. A. & Russo, V. E. A. in Epigenetic Mechanisms of Gene Regulation. Cold Spring Harbor Monograph Archive vol. 32, 1–4 (Cold Spring Harbor, 1996).
Heijmans, B. T. et al. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc. Natl Acad. Sci. USA 105, 17046–17049 (2008).
Milagro, F. I. et al. CLOCK, PER2 and BMAL1 DNA methylation: association with obesity and metabolic syndrome characteristics and monounsaturated fat intake. Chronobiol. Int. 29, 1180–1194 (2012).
Mandaviya, P. R. et al. Association of dietary folate and vitamin B-12 intake with genome-wide DNA methylation in blood: a large-scale epigenome-wide association analysis in 5841 individuals. Am. J. Clin. Nutr. 110, 437–450 (2019).
Aagaard-Tillery, K. M. et al. Developmental origins of disease and determinants of chromatin structure: maternal diet modifies the primate fetal epigenome. Mol. Endocrinol. 41, 91–102 (2008). First evidence that the maternal diet changes the fetal epigenome.
Kim, Y. J. et al. MicroRNA 21 regulates the proliferation of human adipose tissue-derived mesenchymal stem cells and high-fat diet-induced obesity alters microRNA 21 expression in white adipose tissues. J. Cell. Physiol. 227, 183–193 (2012).
Agarwal, P. et al. Maternal obesity, diabetes during pregnancy and epigenetic mechanisms that influence the developmental origins of cardiometabolic disease in the offspring. Crit. Rev. Clin. Lab. Sci. 55, 71–101 (2018).
Young, L. E. Imprinting of genes and the barker hypothesis. Twin Res. 4, 307–317 (2001).
Krautkramer, K. A. et al. Diet-microbiota interactions mediate global epigenetic programming in multiple host tissues. Mol. Cell 64, 982–992 (2016).
Kumar, H. et al. Gut microbiota as an epigenetic regulator: pilot study based on whole-genome methylation analysis. mBio 5, e02113-14 (2014).
Jugder, B.-E., Kamareddine, L. & Watnick, P. I. Microbiota-derived acetate activates intestinal innate immunity via the Tip60 histone acetyltransferase complex. Immunity 54, 1683–1697.e3 (2021).
Gomez De Agüero, M. et al. The maternal microbiota drives early postnatal innate immune development. Science 351, 1296–1302 (2016).
David, L. A. et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505, 559–563 (2014). Evidence that diet changes the gut microbiota in humans within days.
Argaw-Denboba, A. et al. Paternal microbiome perturbations impact offspring fitness. Nature 629, 652–659 (2024). First and comprehensive evidence that changes to the paternal microbiome affect the offspring via epigenetic mechanisms.
Goodsir, J. & Wilson, G. History of a case in which a fluid periodically ejected from the stomach contained vegetable organisms of an undescribed form. Edinb. Med. Surg. J. 57, 430–443 (1842).
Sender, R., Fuchs, S. & Milo, R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 14, e1002533 (2016).
Luckey, T. D. Introduction to intestinal microecology. Am. J. Clin. Nutr. 25, 1292–1294 (1972).
Ianiro, G. et al. Variability of strain engraftment and predictability of microbiome composition after fecal microbiota transplantation across different diseases. Nat. Med. 28, 1913–1923 (2022).
Valles-Colomer, M. et al. The person-to-person transmission landscape of the gut and oral microbiomes. Nature 614, 125–135 (2023). Comprehensive characterization of how the gut microbiota is transmitted, particularly during early life.
Pasolli, E. et al. Extensive unexplored human microbiome diversity revealed by over 150,000 genomes from metagenomes spanning age, geography, and lifestyle. Cell 176, 649–662.e20 (2019).
Almeida, A. et al. A unified catalog of 204,938 reference genomes from the human gut microbiome. Nat. Biotechnol. 39, 105–114 (2021).
Turnbaugh, P. J. et al. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444, 1027–1031 (2006).
Jumpertz, R. et al. Energy-balance studies reveal associations between gut microbes, caloric load, and nutrient absorption in humans. Am. J. Clin. Nutr. 94, 58–65 (2011).
Pompei, A. et al. Folate production by bifidobacteria as a potential probiotic property. Appl. Environ. Microbiol. 73, 179–185 (2007).
Fawad, J. A. et al. Histone deacetylase inhibition by gut microbe-generated short-chain fatty acids entrains intestinal epithelial circadian rhythms. Gastroenterology 163, 1377–1390.e11 (2022).
Frost, G. et al. The short-chain fatty acid acetate reduces appetite via a central homeostatic mechanism. Nat. Commun. 5, 3611 (2014).
Pronovost, G. N. et al. The maternal microbiome promotes placental development in mice. Sci. Adv. 9, eadk1887 (2023).
Kennedy, K. M. et al. Questioning the fetal microbiome illustrates pitfalls of low-biomass microbial studies. Nature 613, 639–649 (2023). A Perspective article with a consensus on the absence of a fetal microbiome.
Dominguez-Bello, M. G. et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc. Natl Acad. Sci. USA 107, 11971–11975 (2010).
Vatanen, T. et al. Mobile genetic elements from the maternal microbiome shape infant gut microbial assembly and metabolism. Cell 185, 4921–4936.e15 (2022).
Zeng, X. et al. Gut bacterial nutrient preferences quantified in vivo. Cell 185, 3441–3456.e19 (2022).
Rackaityte, E. et al. Viable bacterial colonization is highly limited in the human intestine in utero. Nat. Med. 26, 599–607 (2020).
Aagaard, K. et al. The placenta harbors a unique microbiome. Sci. Transl. Med. 6, 237ra65 (2014).
Collado, M. C., Rautava, S., Aakko, J., Isolauri, E. & Salminen, S. Human gut colonisation may be initiated in utero by distinct microbial communities in the placenta and amniotic fluid. Sci. Rep. 6, 23129 (2016).
Mishra, A. et al. Microbial exposure during early human development primes fetal immune cells. Cell 184, 3394–3409.e20 (2021).
Kuperman, A. A. et al. Deep microbial analysis of multiple placentas shows no evidence for a placental microbiome. BJOG 127, 159–169 (2020).
Kennedy, K. M. et al. Over-celling fetal microbial exposure. Cell 184, 5839–5841 (2021).
Cummings, J. H., Pomare, E. W., Branch, W. J., Naylor, C. P. & Macfarlane, G. T. Short chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut 28, 1221–1227 (1987).
Canfora, E. E., Jocken, J. W. & Blaak, E. E. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat. Rev. Endocrinol. 11, 577–591 (2015).
Marques, F. Z. et al. High-fiber diet and acetate supplementation change the gut microbiota and prevent the development of hypertension and heart failure in hypertensive mice. Circulation 135, 964–977 (2017). Evidence that dietary fibre improves cardiovascular disease via the gut microbiome and SCFAs.
Den Besten, G. et al. Short-chain fatty acids protect against high-fat diet–induced obesity via a PPARγ-dependent switch from lipogenesis to fat oxidation. Diabetes 64, 2398–2408 (2015).
Mariño, E. et al. Gut microbial metabolites limit the frequency of autoimmune T cells and protect against type 1 diabetes. Nat. Immunol. 18, 552–562 (2017).
Tang, C. et al. Loss of FFA2 and FFA3 increases insulin secretion and improves glucose tolerance in type 2 diabetes. Nat. Med. 21, 173–177 (2015).
Zhao, L. et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science 359, 1151–1156 (2018). Evidence that dietary fibre improves type 2 diabetes mellitus via the gut microbiome.
Natarajan, N. et al. Microbial short chain fatty acid metabolites lower blood pressure via endothelial G protein-coupled receptor 41. Physiol. Genom. 48, 826–834 (2016).
Pluznick, J. L. et al. Olfactory receptor responding to gut microbiota-derived signals plays a role in renin secretion and blood pressure regulation. Proc. Natl Acad. Sci. USA 110, 4410–4415 (2013).
Kaye, D. M. et al. Deficiency of prebiotic fiber and insufficient signaling through gut metabolite-sensing receptors leads to cardiovascular disease. Circulation 141, 1393–1403 (2020).
Muralitharan, R. R. et al. Gut microbiota metabolites sensed by host GPR41/43 protect against hypertension. Circ. Res. 136, e20–e33 (2025).
Camargo-Tavares, L., Muralitharan, R. R., Snelson, M. & Marques, F. Z. Rare pathogenic variants in G-protein-coupled receptor genes involved in gut-to-host communication are associated with cardiovascular disease risk. Cardiovasc. Res. https://doi.org/10.1093/cvr/cvaf070 (2025).
Kaiko, G. E. et al. The colonic crypt protects stem cells from microbiota-derived metabolites. Cell 165, 1708–1720 (2016).
Singh, N. et al. Activation of Gpr109a, receptor for niacin and the commensal metabolite butyrate, suppresses colonic inflammation and carcinogenesis. Immunity 40, 128–139 (2014).
Wells, J. M., Rossi, O., Meijerink, M. & Van Baarlen, P. Epithelial crosstalk at the microbiota–mucosal interface. Proc. Natl Acad. Sci. USA 108, 4607–4614 (2011).
Ilyés, T. et al. First comparative evaluation of short-chain fatty acids and vitamin-K-dependent proteins levels in mother-newborn pairs at birth. Life 13, 847 (2023).
Kimura, I. et al. Maternal gut microbiota in pregnancy influences offspring metabolic phenotype in mice. Science 367, eaaw8429 (2020). Evidence that lack of a microbiome influences metabolic responses to a high-fat diet, and this is prevented by SCFAs via GPR41/43 signalling.
Collins, S. L., Stine, J. G., Bisanz, J. E., Okafor, C. D. & Patterson, A. D. Bile acids and the gut microbiota: metabolic interactions and impacts on disease. Nat. Rev. Microbiol. 21, 236–247 (2023).
Blazquez, A. G. et al. Characterization of the role of ABCG2 as a bile acid transporter in liver and placenta. Mol. Pharmacol. 81, 273–283 (2012).
Estiú, M. C. et al. Effect of ursodeoxycholic acid treatment on the altered progesterone and bile acid homeostasis in the mother‐placenta‐foetus trio during cholestasis of pregnancy. Br. J. Clin. Pharmacol. 79, 316–329 (2015).
Davies, M. H., Silva, R. C., da, Jones, S. R., Weaver, J. B. & Elias, E. Fetal mortality associated with cholestasis of pregnancy and the potential benefit of therapy with ursodeoxycholic acid. Gut 37, 580–584 (1995).
Chittim, C. L., Martínez del Campo, A. & Balskus, E. P. Gut bacterial phospholipase Ds support disease-associated metabolism by generating choline. Nat. Microbiol. 4, 155–163 (2019).
Wang, Z. et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472, 57–63 (2011). First evidence of the contribution of the gut microbiota to cardiovascular disease.
Yara, M. et al. Molecular and functional characterization of choline transporter in the human trophoblastic cell line JEG-3 cells. Placenta 36, 631–637 (2015).
Romano, K. A. et al. Metabolic, epigenetic, and transgenerational effects of gut bacterial choline consumption. Cell Host Microbe 22, 279–290.e7 (2017). Gut microbial choline metabolism alters host epigenetics and metabolism, with transgenerational effects on offspring health.
Selma-Royo, M. et al. Birthmode and environment-dependent microbiota transmission dynamics are complemented by breastfeeding during the first year. Cell Host Microbe 32, 996–1010.e4 (2024).
Shao, Y. et al. Stunted microbiota and opportunistic pathogen colonization in caesarean-section birth. Nature 574, 117–121 (2019). Birth via caesarean section leads to stunted microbiota and increased colonization by opportunistic pathogens, affecting early-life immune development.
Bittinger, K. et al. Bacterial colonization reprograms the neonatal gut metabolome. Nat. Microbiol. 5, 838–847 (2020).
Nyangahu, D. D. et al. Disruption of maternal gut microbiota during gestation alters offspring microbiota and immunity. Microbiome 6, 124 (2018).
Zhou, L. et al. Effects of vaginal microbiota transfer on the neurodevelopment and microbiome of cesarean-born infants: a blinded randomized controlled trial. Cell Host Microbe 31, 1232–1247.e5 (2023). Vaginal microbiota transfer to infants born by caesarean section improves neurodevelopment and gut microbiome maturation.
Dubois, L. et al. Paternal and induced gut microbiota seeding complement mother-to-infant transmission. Cell Host Microbe 32, 1011–1024.e4 (2024).
Savage, J. H. et al. Diet during pregnancy and infancy and the infant intestinal microbiome. J. Pediatr. 203, 47–54.e4 (2018).
Aumeistere, L. et al. Impact of maternal diet on human milk composition among lactating women in latvia. Med. Kaunas. Lith. 55, 173 (2019).
Liu, Y., Liu, X. & Wang, L. The investigation of fatty acid composition of breast milk and its relationship with dietary fatty acid intake in 5 regions of China. Medicine 98, e15855 (2019).
Armand, M. et al. Maternal nutritional determinants of colostrum fatty acids in the EDEN mother-child cohort. Clin. Nutr. 37, 2127–2136 (2018).
Wong, V. W.-S. et al. Positive relationship between consumption of specific fish type and n-3 PUFA in milk of Hong Kong lactating mothers. Br. J. Nutr. 121, 1431–1440 (2019).
Liu, M.-J. et al. A correlation study of DHA dietary intake and plasma, erythrocyte and breast milk DHA concentrations in lactating women from coastland, lakeland, and inland areas of China. Nutrients 8, 312 (2016).
Makrides, M., Neumann, M. A. & Gibson, R. A. Effect of maternal docosahexaenoic acid (DHA) supplementation on breast milk composition. Eur. J. Clin. Nutr. 50, 352–357 (1996).
Khandelwal, S. et al. Docosahexaenoic acid supplementation in lactating women increases breast milk and erythrocyte membrane docosahexaenoic acid concentrations and alters infant n–6:n–3 fatty acid ratio. Curr. Dev. Nutr. 7, 102010 (2023).
Davis, D. J. et al. Sex-specific effects of docosahexaenoic acid (DHA) on the microbiome and behavior of socially-isolated mice. Brain. Behav. Immun. 59, 38–48 (2017).
Lu, D. et al. Maternal docosahexaenoic acid supplementation during lactation improves exercise performance, enhances intestinal glucose absorption and modulates gut microbiota in weaning offspring mice. Front. Nutr. 11, 1423576 (2024).
Quin, C. et al. Fish oil supplementation reduces maternal defensive inflammation and predicts a gut bacteriome with reduced immune priming capacity in infants. ISME J. 14, 2090–2104 (2020).
van Dijk, S. J. et al. Effect of prenatal DHA supplementation on the infant epigenome: results from a randomized controlled trial. Clin. Epigenetics 8, 114 (2016).
Menni, C. et al. Omega-3 fatty acids correlate with gut microbiome diversity and production of N-carbamylglutamate in middle aged and elderly women. Sci. Rep. 7, 11079 (2017).
Karimi, M. et al. DHA-rich n-3 fatty acid supplementation decreases DNA methylation in blood leukocytes: the OmegAD study123. Am. J. Clin. Nutr. 106, 1157–1165 (2017).
Kijner, S., Kolodny, O. & Yassour, M. Human milk oligosaccharides and the infant gut microbiome from an eco-evolutionary perspective. Curr. Opin. Microbiol. 68, 102156 (2022).
Azad, M. B. et al. Human milk oligosaccharide concentrations are associated with multiple fixed and modifiable maternal characteristics, environmental factors, and feeding practices. J. Nutr. 148, 1733–1742 (2018).
Lewis, Z. T. et al. Maternal fucosyltransferase 2 status affects the gut bifidobacterial communities of breastfed infants. Microbiome 3, 13 (2015).
Selma‐Royo, M. et al. Maternal diet is associated with human milk oligosaccharide profile. Mol. Nutr. Food Res. 66, 2200058 (2022).
Quin, C. et al. Influence of sulfonated and diet-derived human milk oligosaccharides on the infant microbiome and immune markers. J. Biol. Chem. 295, 4035–4048 (2020).
Fan, Y., Vinjamuri, A., Tu, D., Lebrilla, C. B. & Donovan, S. M. Determinants of human milk oligosaccharides profiles of participants in the STRONG kids 2 cohort. Front. Nutr. 10, 1105668 (2023).
Urrutia-Baca, V. H. et al. Exploring the impact of maternal factors and dietary habits on human milk oligosaccharide composition in early breastfeeding among Mexican women. Sci. Rep. 14, 14685 (2024).
Biddulph, C. et al. Associations between maternal nutrition and the concentrations of human milk oligosaccharides in a cohort of healthy Australian lactating women. Nutrients 15, 2093 (2023).
Seppo, A. E. et al. Association of maternal probiotic supplementation with human milk oligosaccharide composition. JAMA Pediatr. 173, 286–288 (2019).
Mohammad, M. A., Sunehag, A. L. & Haymond, M. W. Effect of dietary macronutrient composition under moderate hypocaloric intake on maternal adaptation during lactation12345. Am. J. Clin. Nutr. 89, 1821–1827 (2009).
Seferovic, M. D. et al. Maternal diet alters human milk oligosaccharide composition with implications for the milk metagenome. Sci. Rep. 10, 22092 (2020).
Yeruva, L. et al. Human milk miRNAs associate to maternal dietary nutrients, milk microbiota, infant gut microbiota and growth. Clin. Nutr. 42, 2528–2539 (2023).
Hicks, S. D., Confair, A., Warren, K. & Chandran, D. Levels of breast milk microRNAs and other non-coding RNAs are impacted by milk maturity and maternal diet. Front. Immunol. 12, 785217 (2021).
Lu, D. et al. Maternal fiber-rich diet promotes early-life intestinal development in offspring through milk-derived extracellular vesicles carrying miR-146a-5p. J. Nanobiotechnol. 22, 65 (2024).
Muralitharan, R. R. et al. Microbial peer pressure. Hypertension 76, 1674–1687 (2020).
Ma, J. et al. High-fat maternal diet during pregnancy persistently alters the offspring microbiome in a primate model. Nat. Commun. 5, 3889 (2014). Maternal high-fat diet during pregnancy persistently alters offspring gut microbiota in primates, affecting metabolic health.
Jama, H. A. et al. Maternal diet and gut microbiota influence predisposition to cardiovascular disease in offspring. Circ. Res. 135, 537–539 (2024).
Thorburn, A. N. et al. Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites. Nat. Commun. 6, 7320 (2015). Maternal diet and microbial metabolites influence offspring immune development and asthma risk, supporting the developmental origins of health and disease.
Koren, O. et al. Host remodeling of the gut microbiome and metabolic changes during pregnancy. Cell 150, 470–480 (2012). Pregnancy induces host-driven remodelling of the gut microbiome, linked to metabolic adaptations.
Ansari, I. et al. The microbiota programs DNA methylation to control intestinal homeostasis and inflammation. Nat. Microbiol. 5, 610–619 (2020).
Jašarević, E., Howard, C. D., Misic, A. M., Beiting, D. P. & Bale, T. L. Stress during pregnancy alters temporal and spatial dynamics of the maternal and offspring microbiome in a sex-specific manner. Sci. Rep. 7, 44182 (2017).
Jašarević, E. & Bale, T. L. Prenatal and postnatal contributions of the maternal microbiome on offspring programming. Front. Neuroendocrinol. 55, 100797 (2019).
Candido, E. Sodium butyrate inhibits histone deacetylation in cultured cells. Cell 14, 105–113 (1978).
Sealy, L. & Chalkley, R. The effect of sodium butyrate on histone modification. Cell 14, 115–121 (1978).
Olaniyi, K. S. & Amusa, O. A. Sodium acetate-mediated inhibition of histone deacetylase alleviates hepatic lipid dysregulation and its accompanied injury in streptozotocin-nicotinamide-induced diabetic rats. Biomed. Pharmacother. 128, 110226 (2020).
Silva, L. G., Ferguson, B. S., Avila, A. S. & Faciola, A. P. Sodium propionate and sodium butyrate effects on histone deacetylase (HDAC) activity, histone acetylation, and inflammatory gene expression in bovine mammary epithelial cells1. J. Anim. Sci. 96, 5244–5252 (2018).
Yu, L., Zhong, X., He, Y. & Shi, Y. Butyrate, but not propionate, reverses maternal diet-induced neurocognitive deficits in offspring. Pharmacol. Res. 160, 105082 (2020).
Lund, P. J. et al. Stable isotope tracing in vivo reveals a metabolic bridge linking the microbiota to host histone acetylation. Cell Rep. 41, 111809 (2022).
Furusawa, Y. et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 504, 446–450 (2013). Microbial butyrate promotes colonic Treg cell differentiation via epigenetic regulation, supporting immune tolerance.
Arpaia, N. et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 504, 451–455 (2013). Commensal bacterial metabolites enhance peripheral Treg cell generation, linking microbiota to immune regulation.
Sun, M. et al. Microbiota-derived short-chain fatty acids promote Th1 cell IL-10 production to maintain intestinal homeostasis. Nat. Commun. 9, 3555 (2018).
Chang, P. V., Hao, L., Offermanns, S. & Medzhitov, R. The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proc. Natl Acad. Sci. USA 111, 2247–2252 (2014).
Thomas, S. P. & Denu, J. M. Short-chain fatty acids activate acetyltransferase p300. eLife 10, e72171 (2021).
Miousse, I. R. et al. Short-term dietary methionine supplementation affects one-carbon metabolism and DNA methylation in the mouse gut and leads to altered microbiome profiles, barrier function, gene expression and histomorphology. Genes. Nutr. 12, 22 (2017).
Zhang, B. et al. Both the folate cycle and betaine-homocysteine methyltransferase contribute methyl groups for DNA methylation in mouse blastocysts. FASEB J. 29, 1069–1079 (2015).
Ilcol, Y. O., Ozbek, R., Hamurtekin, E. & Ulus, I. H. Choline status in newborns, infants, children, breast-feeding women, breast-fed infants and human breast milk. J. Nutr. Biochem. 16, 489–499 (2005).
Thomas, D. & Surdin-Kerjan, Y. The synthesis of the two S-adenosyl-methionine synthetases is differently regulated in Saccharomyces cerevisiae. Mol. Gen. Genet. 226, 224–232 (1991).
Asrar, F. M. & O’Connor, D. L. Bacterially synthesized folate and supplemental folic acid are absorbed across the large intestine of piglets. J. Nutr. Biochem. 16, 587–593 (2005).
Albano, C., Silvetti, T. & Brasca, M. Screening of lactic acid bacteria producing folate and their potential use as adjunct cultures for cheese bio-enrichment. FEMS Microbiol. Lett. 367, fnaa059 (2020).
Malinowska, A. M., Schmidt, M., Kok, D. E. & Chmurzynska, A. Ex vivo folate production by fecal bacteria does not predict human blood folate status: associations between dietary patterns, gut microbiota, and folate metabolism. Food Res. Int. 156, 111290 (2022).
Magnúsdóttir, S., Ravcheev, D., de Crécy-Lagard, V. & Thiele, I. Systematic genome assessment of B-vitamin biosynthesis suggests co-operation among gut microbes. Front. Genet. 6, 148 (2015).
Hoyo, C. et al. Methylation variation at IGF2 differentially methylated regions and maternal folic acid use before and during pregnancy. Epigenetics 6, 928–936 (2011).
Schaible, T. D., Harris, R. A., Dowd, S. E., Smith, C. W. & Kellermayer, R. Maternal methyl-donor supplementation induces prolonged murine offspring colitis susceptibility in association with mucosal epigenetic and microbiomic changes. Hum. Mol. Genet. 20, 1687–1696 (2011).
Alves da Silva, A. V. et al. Murine methyl donor deficiency impairs early growth in association with dysmorphic small intestinal crypts and reduced gut microbial community diversity. Curr. Dev. Nutr. 3, nzy070 (2019).
Sommer, F., Nookaew, I., Sommer, N., Fogelstrand, P. & Bäckhed, F. Site-specific programming of the host epithelial transcriptome by the gut microbiota. Genome Biol. 16, 62 (2015).
Malmuthuge, N. & Guan, L. L. Noncoding RNAs: regulatory molecules of host–microbiome crosstalk. Trends Microbiol. 29, 713–724 (2021).
Singh, N. et al. The murine caecal MicroRNA signature depends on the presence of the endogenous microbiota. Int. J. Biol. Sci. 8, 171–186 (2011).
Dempsey, J., Zhang, A. & Cui, J. Y. Coordinate regulation of long non-coding RNAs and protein-coding genes in germ-free mice. BMC Genom. 19, 834 (2018).
Liu, Q. et al. Short-chain fatty acid decreases the expression of CEBPB to inhibit miR-145-mediated DUSP6 and thus further suppresses intestinal inflammation. Inflammation 45, 372–386 (2022).
Wang, Y. et al. The gut microbiota reprograms intestinal lipid metabolism through long noncoding RNA Snhg9. Science 381, 851–857 (2023). Gut microbiota modulates intestinal lipid metabolism through epigenetic regulation by long non-coding RNA Snhg9.
Korenchevsky, V. & Carr, M. Further experiments on the influence of the parents’ diet upon the young: the influence upon the young of an excessive amount of fat-soluble factor and calcium in the mother’s diet during pregnancy. Biochem. J. 18, 1313–1318 (1924).
Korenchevsky, V. Experimental rickets in rats. Br. Med. J. 2, 547–550 (1921).
Langley-Evans, S. C., Phillips, G. J. & Jackson, A. A. In utero exposure to maternal low protein diets induces hypertension in weanling rats, independently of maternal blood pressure changes. Clin. Nutr. 13, 319–324 (1994).
Dahri, S., Snoeck, A., Reusens-Billen, B., Remacle, C. & Hote, J. J. Islet function in offspring of mothers on low-protein diet during gestation. Diabetes 40, 115–120 (1991).
Chu, D. M. et al. The early infant gut microbiome varies in association with a maternal high-fat diet. Genome Med. 8, 77 (2016).
Musial, B. et al. A Western-style obesogenic diet alters maternal metabolic physiology with consequences for fetal nutrient acquisition in mice. J. Physiol. 595, 4875–4892 (2017).
Shunova, A. et al. Choline content of term and preterm infant formulae compared to expressed breast milk—how do we justify the discrepancies? Nutrients 12, 3815 (2020).
Romano, K. A., Vivas, E. I., Amador-Noguez, D. & Rey, F. E. Intestinal microbiota composition modulates choline bioavailability from diet and accumulation of the proatherogenic metabolite trimethylamine-N-oxide. mBio 6, 02481 (2015).
Hallam, M. C. & Reimer, R. A. A maternal high-protein diet predisposes female offspring to increased fat mass in adulthood whereas a prebiotic fibre diet decreases fat mass in rats. Br. J. Nutr. 110, 1732–1741 (2013).
Andreasyan, K. et al. Higher maternal dietary protein intake in late pregnancy is associated with a lower infant ponderal index at birth. Eur. J. Clin. Nutr. 61, 498–508 (2007).
van Zundert, S. et al. Periconceptional maternal protein intake from animal and plant sources and the impact on early and late prenatal growth and birthweight: the rotterdam periconceptional cohort. Nutrients 14, 5309 (2022).
Maslova, E. et al. Maternal protein intake during pregnancy and offspring overweight 20 y later. Am. J. Clin. Nutr. 100, 1139–1148 (2014).
Liu, Q. et al. Maternal diets have effects on intestinal mucosal flora and susceptibility to colitis of offspring mice during early life. Nutrition 99–100, 111672 (2022).
Langley, S. C. & Jackson, A. A. Increased systolic blood pressure in adult rats induced by fetal exposure to maternal low protein diets. Clin. Sci. 86, 217–222 (1994).
Langley-Evans, S. C., Welham, S. J. M., Sherman, R. C. & Jackson, A. A. Weanling rats exposed to maternal low-protein diets during discrete periods of gestation exhibit differing severity of hypertension. Clin. Sci. 91, 607–615 (1996).
Woods, L. L., Weeks, D. A. & Rasch, R. Programming of adult blood pressure by maternal protein restriction: role of nephrogenesis. Kidney Int. 65, 1339–1348 (2004).
Cong, R. et al. Maternal high-protein diet modulates hepatic growth axis in weaning piglets by reprogramming the IGFBP-3 gene. Eur. J. Nutr. 59, 2497–2506 (2020).
Altmann, S. et al. Dietary protein restriction and excess of pregnant German Landrace sows induce changes in hepatic gene expression and promoter methylation of key metabolic genes in the offspring. J. Nutr. Biochem. 24, 484–495 (2013).
Yousefipour, Z. & Newaz, M. PPARα ligand clofibrate ameliorates blood pressure and vascular reactivity in spontaneously hypertensive rats. Acta Pharmacol. Sin. 35, 476–482 (2014).
Verouti, S., Hummler, E. & Vanderriele, P.-E. Role of glucocorticoid receptor mutations in hypertension and adrenal gland hyperplasia. Pflug. Arch. 474, 829–840 (2022).
Desai, M. et al. Maternal obesity and high-fat diet program offspring metabolic syndrome. Am. J. Obstet. Gynecol. 211, 237.e1–237.e13 (2014).
Suarez- Trujillo, A. et al. Maternal high-fat diet exposure during gestation, lactation, or gestation and lactation differentially affects intestinal morphology and proteome of neonatal mice. Nutr. Res. 66, 48–60 (2019).
Saben, J. L. et al. Maternal metabolic syndrome programs mitochondrial dysfunction via germline changes across three generations. Cell Rep. 16, 1–8 (2016).
Thompson, M. D. et al. Maternal obesogenic diet regulates offspring bile acid homeostasis and hepatic lipid metabolism via the gut microbiome in mice. Am. J. Physiol. Gastrointest. Liver Physiol. 322, G295–G309 (2022).
Babu, S. T. et al. Maternal high-fat diet results in microbiota-dependent expansion of ILC3s in mice offspring. JCI Insight 3, e99223 (2018).
Zheng, J. et al. The effects of maternal and post-weaning diet interaction on glucose metabolism and gut microbiota in male mice offspring. Biosci. Rep. 36, e00341 (2016).
Gesù, C. M. D. et al. Maternal gut microbiota mediate intergenerational effects of high-fat diet on descendant social behavior. Cell Rep. 41, 111461 (2022).
Zhang, Q. et al. DNA methylation regulates pancreatic gene expression and links maternal high-fat diet to the offspring glucose metabolism. J. Nutr. Biochem. 123, 109490 (2024).
Chen, F. et al. Maternal high-fat diet increases vascular contractility in adult offspring in a sex-dependent manner. Hypertens. Res. 44, 36–46 (2021).
Phang, M. et al. Epigenetic aging in newborns: role of maternal diet. Am. J. Clin. Nutr. 111, 555–561 (2020).
Koemel, N. A. et al. Maternal dietary fatty acid composition and newborn epigenetic aging—a geometric framework approach. Am. J. Clin. Nutr. 115, 118–127 (2022).
Gill, S. K., Rossi, M., Bajka, B. & Whelan, K. Dietary fibre in gastrointestinal health and disease. Nat. Rev. Gastroenterol. Hepatol. 18, 101–116 (2021). Key Review summarizing evidence that dietary fibre supports gastrointestinal health by modulating microbiota, barrier function and inflammation.
Lin, D. et al. Association of dietary fibre intake and gut microbiota in adults. Br. J. Nutr. 120, 1014–1022 (2018).
Høverstad, T. & Midtvedt, T. Short-chain fatty acids in germfree mice and rats. J. Nutr. 116, 1772–1776 (1986).
Maslowski, K. M. et al. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 461, 1282–1286 (2009).
Macia, L. et al. Metabolite-sensing receptors GPR43 and GPR109A facilitate dietary fibre-induced gut homeostasis through regulation of the inflammasome. Nat. Commun. 6, 6734 (2015).
Li, Y. J. et al. Dietary fiber protects against diabetic nephropathy through short-chain fatty acid-mediated activation of G protein-coupled receptors GPR43 and GPR109A. J. Am. Soc. Nephrol. 31, 1267–1281 (2020).
Jama, H. A. et al. Prebiotic intervention with HAMSAB in untreated essential hypertensive patients assessed in a phase II randomized trial. Nat. Cardiovasc. Res. 2, 35–43 (2023). SCFA-targeted prebiotic randomized clinical trial lowers blood pressure in patients untreated for hypertension.
Desai, M. S. et al. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell 167, 1339–1353.e21 (2016).
Cheng, C. et al. Maternal soluble fiber diet during pregnancy changes the intestinal microbiota, improves growth performance, and reduces intestinal permeability in piglets. Appl. Environ. Microbiol. 84, e01047-18 (2018).
Deng, P. et al. Untargeted stable-isotope probing of the gut microbiota metabolome using 13C-labeled dietary fibers. J. Proteome Res. 20, 2904–2913 (2021).
Nakajima, A. et al. Maternal high fiber diet during pregnancy and lactation influences regulatory T cell differentiation in offspring in mice. J. Immunol. 199, 3516–3524 (2017).
Zhou, Y. et al. Dietary fiber and microbiota metabolite receptors enhance cognition and alleviate disease in the 5xFAD mouse model of Alzheimer’s disease. J. Neurosci. 43, 6460–6475 (2023).
Szajewska, H. et al. Antibiotic-perturbed microbiota and the role of probiotics. Nat. Rev. Gastroenterol. Hepatol. 22, 155–172 (2024).
Masson, B. A. et al. Depletion of the paternal gut microbiome alters sperm small RNAs and impacts offspring physiology and behavior in mice. Brain Behav. Immun. 123, 290–305 (2025).
Lambrot, R. et al. Low paternal dietary folate alters the mouse sperm epigenome and is associated with negative pregnancy outcomes. Nat. Commun. 4, 2889 (2013).
Zhang, X. et al. Paternal programming of liver function and lipid profile induced by a paternal pre-conceptional unhealthy diet: potential association with altered gut microbiome composition. Kidney Blood Press. Res. 44, 133–148 (2019).
Fullston, T. et al. Paternal obesity initiates metabolic disturbances in two generations of mice with incomplete penetrance to the F2 generation and alters the transcriptional profile of testis and sperm microRNA content. FASEB J. 27, 4226–4243 (2013).
Chleilat, F. et al. Paternal high protein diet modulates body composition, insulin sensitivity, epigenetics, and gut microbiota intergenerationally in rats. FASEB J. 35, e21847 (2021).
Watkins, A. J. et al. Paternal diet programs offspring health through sperm- and seminal plasma-specific pathways in mice. Proc. Natl Acad. Sci. USA 115, 10064–10069 (2018).
Tomar, A. et al. Epigenetic inheritance of diet-induced and sperm-borne mitochondrial RNAs. Nature 630, 720–727 (2024).
Wilck, N. et al. Salt-responsive gut commensal modulates TH17 axis and disease. Nature 551, 585–589 (2017).
Koleganova, N. et al. Both high and low maternal salt intake in pregnancy alter kidney development in the offspring. Am. J. Physiol. Ren. Physiol. 301, F344–F354 (2011).
Gray, C. et al. Excess maternal salt intake produces sex-specific hypertension in offspring: putative roles for kidney and gastrointestinal sodium handling. PLoS ONE 8, e72682 (2013).
Valles-Colomer, M. et al. Cardiometabolic health, diet and the gut microbiome: a meta-omics perspective. Nat. Med. 29, 551–561 (2023).
Pinto, Y. & Bhatt, A. S. Sequencing-based analysis of microbiomes. Nat. Rev. Genet. 25, 829–845 (2024).
Edlow, A. G. et al. Males are from Mars, and females are from Venus: sex-specific fetal brain gene expression signatures in a mouse model of maternal diet-induced obesity. Am. J. Obstet. Gynecol. 214, 623.e1–623.e10 (2016).
Nicholas, L. M. et al. Exposure to maternal obesity programs sex differences in pancreatic islets of the offspring in mice. Diabetologia 63, 324–337 (2020).
Robb, J.-L. et al. A maternal diet high in saturated fat impairs offspring hippocampal function in a sex-specific manner. Behav. Brain Res. 326, 187–199 (2017).
Yang, C. et al. Faecal metaproteomics analysis reveals a high cardiovascular risk profile across healthy individuals and heart failure patients. Gut Microbes 17, 2441356 (2025).
O’Donnell, J. A., Zheng, T., Meric, G. & Marques, F. Z. The gut microbiome and hypertension. Nat. Rev. Nephrol. 19, 153–167 (2023).
Devarakonda, S. L. S. et al. Gut microbial features and dietary fiber intake predict gut microbiota response to resistant starch supplementation. Gut Microbes 16, 2367301 (2024).
Muralitharan, R. R. et al. Influence of angiotensin II on the gut microbiome: modest effects in comparison to experimental factors. Cardiovasc. Res. 120, 1155–1163 (2024).
Muralitharan, R. R., Buikema, J. W. & Marques, F. Z. Minimizing gut microbiome confounding factors in cardiovascular research. Cardiovasc. Res. 120, e60–e62 (2024).
Tito, R. Y. et al. Microbiome confounders and quantitative profiling challenge predicted microbial targets in colorectal cancer development. Nat. Med. 30, 1339–1348 (2024).
Nishijima, S. et al. Fecal microbial load is a major determinant of gut microbiome variation and a confounder for disease associations. Cell 188, 222–236.e15 (2025).
Akhtar, A. The flaws and human harms of animal experimentation. Camb. Q. Healthc. Ethics 24, 407–419 (2015).
Gomez-Baya, D., Salinas-Perez, J. A., Rodero-Cosano, M. L. & Alvarez-Galvez, J. Socioeconomic inequalities in health through lifestyles: analysing gender and age differences in Andalusia, Spain. J. Community Health 45, 836–845 (2020).
Kim, S., Symons, M. & Popkin, B. M. Contrasting socioeconomic profiles related to healthier lifestyles in China and the United States. Am. J. Epidemiol. 159, 184–191 (2004).
Aaltonen, J. et al. Impact of maternal diet during pregnancy and breastfeeding on infant metabolic programming: a prospective randomized controlled study. Eur. J. Clin. Nutr. 65, 10–19 (2011).
Donnelly, J. M., Walsh, J. M., Byrne, J., Molloy, E. J. & McAuliffe, F. M. Impact of maternal diet on neonatal anthropometry: a randomized controlled trial. Pediatr. Obes. 10, 52–56 (2015).
Wu, Y. et al. Dietary exposures, epigenetics and pubertal tempo. Environ. Epigenet. 5, dvz002 (2019).
Shim, J.-S., Oh, K. & Kim, H. C. Dietary assessment methods in epidemiologic studies. Epidemiol. Health 36, e2014009 (2014).
Lundgren, S. N. et al. Maternal diet during pregnancy is related with the infant stool microbiome in a delivery mode-dependent manner. Microbiome 6, 109 (2018).
Zmora, N. et al. Personalized gut mucosal colonization resistance to empiric probiotics is associated with unique host and microbiome features. Cell 174, 1388–1405.e21 (2018).
Berry, S. E. et al. Human postprandial responses to food and potential for precision nutrition. Nat. Med. 26, 964–973 (2020). A large-scale study showing human postprandial responses to food vary widely, even among twins, highlighting the need for precision nutrition.
Kosorok, M. R. & Laber, E. B. Precision medicine. Annu. Rev. Stat. Appl. 6, 263–286 (2019).
Chambers, E. S. et al. Effects of targeted delivery of propionate to the human colon on appetite regulation, body weight maintenance and adiposity in overweight adults. Gut 64, 1744–1754 (2015).
Romero, R. et al. The composition and stability of the vaginal microbiota of normal pregnant women is different from that of non-pregnant women. Microbiome 2, 4 (2014).
MacIntyre, D. A. et al. The vaginal microbiome during pregnancy and the postpartum period in a European population. Sci. Rep. 5, 8988 (2015).
Baud, A. et al. Microbial diversity in the vaginal microbiota and its link to pregnancy outcomes. Sci. Rep. 13, 9061 (2023).
Jašarević, E. et al. The composition of human vaginal microbiota transferred at birth affects offspring health in a mouse model. Nat. Commun. 12, 6289 (2021).
Jang, H., Patoine, A., Wu, T. T., Castillo, D. A. & Xiao, J. Oral microflora and pregnancy: a systematic review and meta-analysis. Sci. Rep. 11, 16870 (2021).
Russo, M. et al. Influence of maternal oral microbiome on newborn oral microbiome in healthy pregnancies. Ital. J. Pediatr. 49, 140 (2023).
Lhuillery, C. et al. Fatty acid composition of lipids in the maternal diet and establishment of a Lactobacillus sp. strain in the digestive tract of suckling gnotobiotic mice and rats. Am. J. Clin. Nutr. 34, 1513–1519 (1981).
Rees, W. D., Hay, S. M., Brown, D. S., Antipatis, C. & Palmer, R. M. Maternal protein deficiency causes hypermethylation of DNA in the livers of rat fetuses. J. Nutr. 130, 1821–1826 (2000).
Ly, L. et al. Impact of mothers’ early life exposure to low or high folate on progeny outcome and DNA methylation patterns. Environ. Epigenet. 6, dvaa018 (2020).
Collins, P. L. et al. DNA double-strand breaks induce H2Ax phosphorylation domains in a contact-dependent manner. Nat. Commun. 11, 3158 (2020).
Lee, K. K. & Workman, J. L. Histone acetyltransferase complexes: one size doesn’t fit all. Nat. Rev. Mol. Cell Biol. 8, 284–295 (2007).
Grunstein, M. Histone acetylation in chromatin structure and transcription. Nature 389, 349–352 (1997).
Ichimura, T. et al. Transcriptional repression and heterochromatin formation by MBD1 and MCAF/AM family proteins*. J. Biol. Chem. 280, 13928–13935 (2005).
Nan, X., Tate, P., Li, E. & Bird, A. DNA methylation specifies chromosomal localization of MeCP2. Mol. Cell. Biol. 16, 414–421 (1996).
Acknowledgements
F.Z.M. is supported by a Senior Medical Research Fellowship from the Sylvia and Charles Viertel Charitable Foundation, a National Heart Foundation Future Leader Fellowship (105663), a National Health & Medical Research Council (NHMRC) Emerging Leader Fellowship (GNT2017382), and a grant from the Australian Research Council (DP230102725). A.E.-O. is supported by a fellowship from the NHMRC (GTN1154650) and NHMRC – CTCS (2014763). M.S. is supported by a National Heart Foundation Postdoctoral Fellowship (106698).
Author information
Authors and Affiliations
Contributions
C.Y. and F.Z.M. conceived, designed and drafted most of the article. C.Y. and M.S. created the initial draft of the figures. M.S. and A.E.-O. provided critical feedback and drafted some sections.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks Eldin Jasarevic, Raffaele Teperino and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, C., Snelson, M., El-Osta, A. et al. Parental diet and offspring health: a role for the gut microbiome via epigenetics. Nat Rev Gastroenterol Hepatol 22, 755–772 (2025). https://doi.org/10.1038/s41575-025-01106-3
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41575-025-01106-3