Abstract
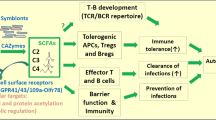
Short-chain fatty acids (SCFAs) are a group of organic compounds produced by the fermentation of dietary fibre by the human gut microbiota. They play diverse roles in different physiological processes of the host with implications for human health and disease. This Review provides an overview of the complex microbial metabolism underlying SCFA formation, considering microbial interactions and modulating factors of the gut environment. We explore the multifaceted mechanistic interactions between SCFAs and the host, with a particular focus on the local actions of SCFAs in the gut and their complex interactions with the immune system. We also discuss how these actions influence intestinal and extraintestinal diseases and emerging therapeutic strategies using SCFAs.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Gill, S. K., Rossi, M., Bajka, B. & Whelan, K. Dietary fibre in gastrointestinal health and disease. Nat. Rev. Gastroenterol. Hepatol. 18, 101–116 (2021).
Louis, P., Solvang, M., Duncan, S. H., Walker, A. W. & Mukhopadhya, I. Dietary fibre complexity and its influence on functional groups of the human gut microbiota. Proc. Nutr. Soc. 80, 386–397 (2021).
Glover, J. S., Ticer, T. D. & Engevik, M. A. Characterizing the mucin-degrading capacity of the human gut microbiota. Sci. Rep. 12, 8456 (2022).
Zhang, D. et al. Short-chain fatty acids in diseases. Cell Commun. Signal. 21, 212 (2023).
Hodgkinson, K. et al. Butyrate’s role in human health and the current progress towards its clinical application to treat gastrointestinal disease. Clin. Nutr. 42, 61–75 (2023).
Drula, E. et al. The carbohydrate-active enzyme database: functions and literature. Nucleic Acids Res. 50, D571–D577 (2022).
Ndeh, D. & Gilbert, H. J. Biochemistry of complex glycan depolymerisation by the human gut microbiota. FEMS Microbiol. Rev. 42, 146–164 (2018).
Louis, P. & Flint, H. J. Formation of propionate and butyrate by the human colonic microbiota. Environ. Microbiol. 19, 29–41 (2017).
Frolova, M. S., Suvorova, I. A., Iablokov, S. N., Petrov, S. N. & Rodionov, D. A. Genomic reconstruction of short-chain fatty acid production by the human gut microbiota. Front. Mol. Biosci. 9, 949563 (2022). This study utilizes human faecal metagenomic data sets to perform an in-depth in silico analysis of SCFA fermentation pathways in different populations.
Reichardt, N. et al. Phylogenetic distribution of three pathways for propionate production within the human gut microbiota. ISME J. 8, 1323–1335 (2014).
Bui, T. P. N. et al. Production of butyrate from lysine and the Amadori product fructoselysine by a human gut commensal. Nat. Commun. 6, 10062 (2015).
Louis, P., Duncan, S. H., Sheridan, P. O., Walker, A. W. & Flint, H. J. Microbial lactate utilisation and the stability of the gut microbiome. Gut Microbiome 3, e3 (2022).
Wang, S. P. et al. Pivotal roles for pH, lactate, and lactate-utilizing bacteria in the stability of a human colonic microbial ecosystem. mSystems 5, 1–18 (2020).
Hackmann, T. J. New biochemical pathways for forming short-chain fatty acids during fermentation in rumen bacteria. JDS Commun. 5, 230–235 (2024).
Walker, A. W., Duncan, S. H., McWilliam Leitch, E. C., Child, M. W. & Flint, H. J. pH and peptide supply can radically alter bacterial populations and short-chain fatty acid ratios within microbial communities from the human colon. Appl. Environ. Microbiol. 71, 3692–3700 (2005).
Duncan, S. H., Louis, P., Thomson, J. M. & Flint, H. J. The role of pH in determining the species composition of the human colonic microbiota. Environ. Microbiol. 11, 2112–2122 (2009).
LaBouyer, M. et al. Higher total faecal short-chain fatty acid concentrations correlate with increasing proportions of butyrate and decreasing proportions of branched-chain fatty acids across multiple human studies. Gut Microbiome 3, e2 (2022).
Flint, H. J., Louis, P. & Duncan, S. H. Why does increased microbial fermentation in the human colon shift toward butyrate? AIMS Microbiol. 10, 311–319 (2024).
Campbell, A., Gdanetz, K., Schmidt, A. W. & Schmidt, T. M. H2 generated by fermentation in the human gut microbiome influences metabolism and competitive fitness of gut butyrate producers. Microbiome 11, 133 (2023).
Joos, R. et al. Examining the healthy human microbiome concept. Nat. Rev. Microbiol. 23, 192–205 (2024).
Park, S.-Y. et al. Strain-level fitness in the gut microbiome is an emergent property of glycans and a single metabolite. Cell 185, 513–529.e21 (2022). Using in vitro and in vivo approaches, this study demonstrates the unique fitness landscape of different Bacteroides strains based on their response to butyrate in the presence of different glycan substrates.
Chung, W. S. F. et al. Impact of carbohydrate substrate complexity on the diversity of the human colonic microbiota. FEMS Microbiol. Ecol. 95, fiy201 (2019).
Puhlmann, M.-L. & de Vos, W. M. Intrinsic dietary fibers and the gut microbiome: rediscovering the benefits of the plant cell matrix for human health. Front. Immunol. 13, 954845 (2022).
So, D. et al. Detection of changes in regional colonic fermentation in response to supplementing a low FODMAP diet with dietary fibres by hydrogen concentrations, but not by luminal pH. Aliment. Pharmacol. Ther. 58, 417–428 (2023).
De Paepe, K. et al. Modification of wheat bran particle size and tissue composition affects colonisation and metabolism by human faecal microbiota. Food Funct. 10, 379–396 (2019).
Solvang, M. et al. Beyond purified dietary fibre supplements: compositional variation between cell wall fibre from different plants influences human faecal microbiota activity and growth in vitro. Environ. Microbiol. 25, 1484–1504 (2023).
Puhlmann, M.-L. et al. Analysis of the fermentation kinetics and gut microbiota modulatory effect of dried chicory root reveals the impact of the plant–cell matrix rationalizing its conversion in the distal colon. Microbiome Res. Rep. 3, 28 (2024).
La Rosa, S. L. et al. The human gut Firmicute Roseburia intestinalis is a primary degrader of dietary β-mannans. Nat. Commun. 10, 905 (2019). This study provides a deep biochemical characterization of Roseburia intestinalis β-mannan utilization and reveals its competitive behaviour with other gut bacteria both in vitro and in vivo.
Feng, J. et al. Polysaccharide utilization loci in Bacteroides determine population fitness and community-level interactions. Cell Host Microbe 30, 200–215.e12 (2022). This study reveals the contribution of different polysaccharide utilization loci (PULs) to nutrient-dependent fitness of Bacteroides uniformis PUL mutants and demonstrates their altered cross-feeding interactions with butyrate-producing bacteria.
Kettle, H., Louis, P. & Flint, H. J. Process-based modelling of microbial community dynamics in the human colon. J. R. Soc. Interface 19, 20220489 (2022).
Quinn-Bohmann, N. et al. Microbial community-scale metabolic modelling predicts personalized short-chain fatty acid production profiles in the human gut. Nat. Microbiol. 9, 1700–1712 (2024).
Gibbons, S. M. et al. Perspective: leveraging the gut microbiota to predict personalized responses to dietary, prebiotic, and probiotic interventions. Adv. Nutr. 13, 1450–1461 (2022).
Cummings, J. H., Pomare, E. W., Branch, W. J., Naylor, C. P. & Macfarlane, G. T. Short chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut 28, 1221–1227 (1987).
Fagundes, R. R. et al. Beyond butyrate: microbial fiber metabolism supporting colonic epithelial homeostasis. Trends Microbiol. 32, 178–189 (2024).
Stumpff, F. A look at the smelly side of physiology: transport of short chain fatty acids. Pflugers Arch. 470, 571–598 (2018).
Wang, Q. & Mackay, C. R. High metabolite concentrations in portal venous blood as a possible mechanism for microbiota effects on the immune system and Western diseases. J. Allergy Clin. Immunol. 153, 980–982 (2024).
O’Riordan, K. J. et al. Short chain fatty acids: microbial metabolites for gut–brain axis signalling. Mol. Cell. Endocrinol. 546, 111572 (2022).
Sukkar, A. H., Lett, A. M., Frost, G. & Chambers, E. S. Regulation of energy expenditure and substrate oxidation by short-chain fatty acids. J. Endocrinol. 242, R1–R8 (2019).
Priyadarshini, M., Kotlo, K. U., Dudeja, P. K. & Layden, B. T. Role of short chain fatty acid receptors in intestinal physiology and pathophysiology. Compr. Physiol. 8, 1091–1115 (2018).
Kimura, I., Ichimura, A., Ohue-Kitano, R. & Igarashi, M. Free fatty acid receptors in health and disease. Physiol. Rev. 100, 171–210 (2020).
Barki, N. et al. Phosphorylation bar-coding of free fatty acid receptor 2 is generated in a tissue-specific manner. eLife 12, RP91861 (2023).
Bolognini, D., Tobin, A. B., Milligan, G. & Moss, C. E. The pharmacology and function of receptors for short-chain fatty acids. Mol. Pharmacol. 89, 388–398 (2016).
Stein, R. A. & Riber, L. Epigenetic effects of short-chain fatty acids from the large intestine on host cells. Microlife 4, uqad032 (2023).
Sarkar, S. et al. Histone deacetylase inhibitors reverse CpG methylation by regulating DNMT1 through ERK signaling. Anticancer Res. 31, 2723–2732 (2011).
Steliou, K., Boosalis, M. S., Perrine, S. P., Sangerman, J. & Faller, D. V. Butyrate histone deacetylase inhibitors. Biores. Open Access 1, 192–198 (2012).
He, J. et al. Short-chain fatty acids and their association with signalling pathways in inflammation, glucose and lipid metabolism. Int. J. Mol. Sci. 21, 6356 (2020).
Rekha, K. et al. Short-chain fatty acid: an updated review on signaling, metabolism, and therapeutic effects. Crit. Rev. Food Sci. Nutr. 64, 2461–2489 (2024).
Donohoe, D. R. et al. The Warburg effect dictates the mechanism of butyrate-mediated histone acetylation and cell proliferation. Mol. Cell 48, 612–626 (2012).
Moffett, J. R., Puthillathu, N., Vengilote, R., Jaworski, D. M. & Namboodiri, A. M. Acetate revisited: a key biomolecule at the nexus of metabolism, epigenetics and oncogenesis — part 1: acetyl-CoA, acetogenesis and acyl-CoA short-chain synthetases. Front. Physiol. 11, 580167 (2020).
Chen, Y. et al. Lysine propionylation and butyrylation are novel post-translational modifications in histones. Mol. Cell. Proteom. 6, 812–819 (2007).
Fellows, R. et al. Microbiota derived short chain fatty acids promote histone crotonylation in the colon through histone deacetylases. Nat. Commun. 9, 105 (2018).
Martin-Gallausiaux, C., Marinelli, L., Blottière, H. M., Larraufie, P. & Lapaque, N. SCFA: mechanisms and functional importance in the gut. Proc. Nutr. Soc. 80, 37–49 (2021).
Modoux, M. et al. Butyrate acts through HDAC inhibition to enhance aryl hydrocarbon receptor activation by gut microbiota-derived ligands. Gut Microbes 14, 2105637 (2022).
Peng, Y. & Croce, C. M. The role of microRNAs in human cancer. Signal Transduct. Target. Ther. 1, 1–9 (2016).
Hu, S. et al. The microbe-derived short chain fatty acid butyrate targets miRNA-dependent p21 gene expression in human colon cancer. PLoS ONE 6, e16221 (2011).
Bishop, K. S., Xu, H. & Marlow, G. Epigenetic regulation of gene expression induced by butyrate in colorectal cancer: involvement of microRNA. Genet. Epigenet. 9, 1179237X17729900 (2017).
Shealy, N. G., Yoo, W. & Byndloss, M. X. Colonization resistance: metabolic warfare as a strategy against pathogenic Enterobacteriaceae. Curr. Opin. Microbiol. 64, 82–90 (2021).
Shelton, C. D. et al. Salmonella enterica serovar Typhimurium uses anaerobic respiration to overcome propionate-mediated colonization resistance. Cell Rep. 38, 110180 (2022).
Whisner, C. M. & Castillo, L. F. Prebiotics, bone and mineral metabolism. Calcif. Tissue Int. 102, 443–479 (2018).
Hyland, N. P. & Cryan, J. F. Microbe–host interactions: influence of the gut microbiota on the enteric nervous system. Dev. Biol. 417, 182–187 (2016).
Anitha, M., Vijay-Kumar, M., Sitaraman, S. V., Gewirtz, A. T. & Srinivasan, S. Gut microbial products regulate murine gastrointestinal motility via toll-like receptor 4 signaling. Gastroenterology 143, 1006–1016.e4 (2012).
Zheng, Z., Tang, J., Hu, Y. & Zhang, W. Role of gut microbiota-derived signals in the regulation of gastrointestinal motility. Front. Med. 9, 961703 (2022).
Sun, Q., Jia, Q., Song, L. & Duan, L. Alterations in fecal short-chain fatty acids in patients with irritable bowel syndrome: a systematic review and meta-analysis. Medicine 98, e14513 (2019).
Burger-van Paassen, N. et al. The regulation of intestinal mucin MUC2 expression by short-chain fatty acids: implications for epithelial protection. Biochem. J. 420, 211–219 (2009).
Willemsen, L. E., Koetsier, M. A., van Deventer, S. J. & van Tol, E. A. Short chain fatty acids stimulate epithelial mucin 2 expression through differential effects on prostaglandin E(1) and E(2) production by intestinal myofibroblasts. Gut 52, 1442–1447 (2003).
Gaudier, E., Rival, M., Buisine, M. P., Robineau, I. & Hoebler, C. Butyrate enemas upregulate Muc genes expression but decrease adherent mucus thickness in mice colon. Physiol. Res. 58, 111–119 (2009).
Hamer, H. M. et al. Effect of butyrate enemas on inflammation and antioxidant status in the colonic mucosa of patients with ulcerative colitis in remission. Clin. Nutr. 29, 738–744 (2010).
Peng, L., He, Z., Chen, W., Holzman, I. R. & Lin, J. Effects of butyrate on intestinal barrier function in a Caco-2 cell monolayer model of intestinal barrier. Pediatr. Res. 61, 37–41 (2007).
Cresci, G. A. et al. Prophylactic tributyrin treatment mitigates chronic-binge ethanol-induced intestinal barrier and liver injury. J. Gastroenterol. Hepatol. 32, 1587–1597 (2017).
Tabat, M. W. et al. Acute effects of butyrate on induced hyperpermeability and tight junction protein expression in human colonic tissues. Biomolecules 10, 766 (2020).
Vancamelbeke, M. et al. Butyrate does not protect against inflammation-induced loss of epithelial barrier function and cytokine production in primary cell monolayers from patients with ulcerative colitis. J. Crohns Colitis 13, 1351–1361 (2019).
Liu, T. et al. Short-chain fatty acids suppress lipopolysaccharide-induced production of nitric oxide and proinflammatory cytokines through inhibition of NF-κB pathway in RAW264.7 cells. Inflammation 35, 1676–1684 (2012).
Schulthess, J. et al. The short chain fatty acid butyrate imprints an antimicrobial program in macrophages. Immunity 50, 432–445.e7 (2019). This study provides the mechanistic pathway by which butyrate induces the differentiation of macrophages to exert their antimicrobial function.
Ji, J. et al. Microbial metabolite butyrate facilitates M2 macrophage polarization and function. Sci. Rep. 6, 24838 (2016).
Wang, Z. et al. Inulin alleviates inflammation of alcoholic liver disease via SCFAs-inducing suppression of M1 and facilitation of M2 macrophages in mice. Int. Immunopharmacol. 78, 106062 (2020).
Aguilar, E. C. et al. Butyrate impairs atherogenesis by reducing plaque inflammation and vulnerability and decreasing NFκB activation. Nutr. Metab. Cardiovasc. Dis. 24, 606–613 (2014).
Zapolska-Downar, D., Siennicka, A., Kaczmarczyk, M., Kolodziej, B. & Naruszewicz, M. Butyrate inhibits cytokine-induced VCAM-1 and ICAM-1 expression in cultured endothelial cells: the role of NF-kappaB and PPARalpha. J. Nutr. Biochem. 15, 220–228 (2004).
Mills, S. W., Montgomery, S. H. & Morck, D. W. Evaluation of the effects of short-chain fatty acids and extracellular pH on bovine neutrophil function in vitro. Am. J. Vet. Res. 67, 1901–1907 (2006).
Li, G. et al. Microbiota metabolite butyrate constrains neutrophil functions and ameliorates mucosal inflammation in inflammatory bowel disease. Gut Microbes 13, 1968257 (2021). This study shows that butyrate inhibited the ability of neutrophils isolated from patients with IBD to produce pro-inflammatory cytokines and suppressed neutrophil migration and formation of neutrophil extracellular traps.
Aoyama, M., Kotani, J. & Usami, M. Butyrate and propionate induced activated or non-activated neutrophil apoptosis via HDAC inhibitor activity but without activating GPR-41/GPR-43 pathways. Nutrition 26, 653–661 (2010).
Liu, B. et al. Butyrate protects rat liver against total hepatic ischemia reperfusion injury with bowel congestion. PLoS ONE 9, e106184 (2014).
Simeoli, R. et al. An orally administered butyrate-releasing derivative reduces neutrophil recruitment and inflammation in dextran sulphate sodium-induced murine colitis. Br. J. Pharmacol. 174, 1484–1496 (2017).
Liu, L. et al. Butyrate interferes with the differentiation and function of human monocyte-derived dendritic cells. Cell. Immunol. 277, 66–73 (2012).
Kaisar, M. M. M., Pelgrom, L. R., van der Ham, A. J., Yazdanbakhsh, M. & Everts, B. Butyrate conditions human dendritic cells to prime type 1 regulatory T cells via both histone deacetylase inhibition and G protein-coupled receptor 109A signaling. Front. Immunol. 8, 1429 (2017).
Nastasi, C. et al. The effect of short-chain fatty acids on human monocyte-derived dendritic cells. Sci. Rep. 5, 16148 (2015).
Tao, R. et al. Deacetylase inhibition promotes the generation and function of regulatory T cells. Nat. Med. 13, 1299–1307 (2007).
Arpaia, N. et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 504, 451–455 (2013).
Park, J. et al. Short-chain fatty acids induce both effector and regulatory T cells by suppression of histone deacetylases and regulation of the mTOR–S6K pathway. Mucosal Immunol. 8, 80–93 (2015).
Kespohl, M. et al. The microbial metabolite butyrate induces expression of Th1-associated factors in CD4(+) T cells. Front. Immunol. 8, 1036 (2017).
Luu, M. et al. Regulation of the effector function of CD8(+) T cells by gut microbiota-derived metabolite butyrate. Sci. Rep. 8, 14430 (2018).
Kim, M., Qie, Y., Park, J. & Kim, C. H. Gut microbial metabolites fuel host antibody responses. Cell Host Microbe 20, 202–214 (2016).
Wu, W. et al. Microbiota metabolite short-chain fatty acid acetate promotes intestinal IgA response to microbiota which is mediated by GPR43. Mucosal Immunol. 10, 946–956 (2017).
Sanchez, H. N. et al. B cell-intrinsic epigenetic modulation of antibody responses by dietary fiber-derived short-chain fatty acids. Nat. Commun. 11, 60 (2020).
Luu, M., Monning, H. & Visekruna, A. Exploring the molecular mechanisms underlying the protective effects of microbial SCFAs on intestinal tolerance and food allergy. Front. Immunol. 11, 1225 (2020).
Daien, C. I. et al. Gut-derived acetate promotes B10 cells with antiinflammatory effects. JCI Insight 6, e144156 (2021). This study shows that acetate induces proliferation of IL-10 producing regulatory B cells (B10 cells) in both in vivo and in vitro models, outlining its anti-inflammatory role.
Cong, J., Zhou, P. & Zhang, R. Intestinal microbiota-derived short chain fatty acids in host health and disease. Nutrients 14, 1977 (2022).
Mukhopadhya, I., Hansen, R., El-Omar, E. M. & Hold, G. L. IBD — what role do Proteobacteria play? Nat. Rev. Gastroenterol. Hepatol. 9, 219–230 (2012).
Machiels, K. et al. A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut 63, 1275–1283 (2014).
Kowalska-Duplaga, K. et al. Differences in the intestinal microbiome of healthy children and patients with newly diagnosed Crohn’s disease. Sci. Rep. 9, 18880 (2019).
Laserna-Mendieta, E. J. et al. Determinants of reduced genetic capacity for butyrate synthesis by the gut microbiome in Crohn’s disease and ulcerative colitis. J. Crohns Colitis 12, 204–216 (2018).
Xu, H. M. et al. Characterization of short-chain fatty acids in patients with ulcerative colitis: a meta-analysis. BMC Gastroenterol. 22, 117 (2022). This meta-analysis of 11 studies shows that patients with ulcerative colitis had significantly decreased concentration of acetate and propionate as opposed to healthy controls.
De Preter, V. et al. Kinetics of butyrate metabolism in the normal colon and in ulcerative colitis: the effects of substrate concentration and carnitine on the β‐oxidation pathway. Aliment. Pharmacol. Ther. 34, 526–532 (2011).
Ferrer-Picón, E. et al. Intestinal inflammation modulates the epithelial response to butyrate in patients with inflammatory bowel disease. Inflamm. Bowel Dis. 26, 43–55 (2020).
Starr, A. E. et al. Associations between cellular energy and pediatric inflammatory bowel disease patient response to treatment. J. Proteome Res. 20, 4393–4404 (2021).
Kaczmarczyk, O. et al. Altered fecal short-chain fatty acid profile as a potential marker of disease activity in patients with ulcerative colitis and Crohn’s disease: a pilot study. Pol. Arch. Intern. Med. 132, 16254 (2022).
Zhuang, X. et al. Systematic review and meta-analysis: short-chain fatty acid characterization in patients with inflammatory bowel disease. Inflamm. Bowel Dis. 25, 1751–1763 (2019).
Vernia, P. et al. Short‐chain fatty acid topical treatment in distal ulcerative colitis. Aliment. Pharmacol. Ther. 9, 309–313 (1995).
Scheppach, W. et al. Effect of butyrate enemas on the colonic mucosa in distal ulcerative colitis. Gastroenterology 103, 51–56 (1992).
Lührs, H. et al. Butyrate inhibits NF-κB activation in lamina propria macrophages of patients with ulcerative colitis. Scand. J. Gastroenterol. 37, 458–466 (2002).
Jamka, M. et al. The effect of sodium butyrate enemas compared with placebo on disease activity, endoscopic scores, and histological and inflammatory parameters in inflammatory bowel diseases: a systematic review of randomised controlled trials. Complement. Med. Res. 28, 344–356 (2021).
Sabatino, A. et al. Oral butyrate for mildly to moderately active Crohn’s disease. Aliment. Pharmacol. Ther. 22, 789–794 (2005).
Vernia, P. et al. Combined oral sodium butyrate and mesalazine treatment compared to oral mesalazine alone in ulcerative colitis. Dig. Dis. Sci. 45, 976–981 (2000).
Bray, F. et al. Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424 (2018).
Reynolds, A. et al. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet 393, 434–445 (2019).
Bingham, S. A. et al. Dietary fibre in food and protection against colorectal cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC): an observational study. Lancet 361, 1496–1501 (2003).
Yusuf, F., Adewiah, S., Syam, A. F. & Fatchiyah, F. Altered profile of gut microbiota and the level short chain fatty acids in colorectal cancer patients. J. Phys. Conf. Ser. 1146, 012037 (2019).
Shuwen, H. et al. Protective effect of the ‘food–microorganism–SCFAs’ axis on colorectal cancer: from basic research to practical application. J. Cancer Res. Clin. Oncol. 145, 2169–2197 (2019).
Vinelli, V. et al. Effects of dietary fibers on short-chain fatty acids and gut microbiota composition in healthy adults: a systematic review. Nutrients 14, 2559 (2022).
Gold, A., Choueiry, F., Jin, N., Mo, X. & Zhu, J. The application of metabolomics in recent colorectal cancer studies: a state-of-the-art review. Cancers 14, 725 (2022).
Louis, P., Hold, G. L. & Flint, H. J. The gut microbiota, bacterial metabolites and colorectal cancer. Nat. Rev. Microbiol. 12, 661–672 (2014).
Scharlau, D. et al. Mechanisms of primary cancer prevention by butyrate and other products formed during gut flora-mediated fermentation of dietary fibre. Mutat. Res. 682, 39–53 (2009).
Kim, Y.-H., Park, J.-W., Lee, J.-Y. & Kwon, T. K. Sodium butyrate sensitizes TRAIL-mediated apoptosis by induction of transcription from the DR5 gene promoter through Sp1 sites in colon cancer cells. Carcinogenesis 25, 1813–1820 (2004).
Waby, J. S. et al. Sp1 acetylation is associated with loss of DNA binding at promoters associated with cell cycle arrest and cell death in a colon cell line. Mol. Cancer 9, 1–16 (2010).
Eslami, M. et al. Importance of the microbiota inhibitory mechanism on the Warburg effect in colorectal cancer cells. J. Gastrointest. Cancer 51, 738–747 (2020).
Luo, Q., Zhou, P., Chang, S., Huang, Z. & Zeng, X. Characterization of butyrate-metabolism in colorectal cancer to guide clinical treatment. Sci. Rep. 13, 5106 (2023). This study utilizes expression of butyrate metabolism-related genes in CRC samples to develop a risk prognostic model that could forecast the response of these patients to immunotherapy and chemotherapy.
Ho, M. H.-K., Wong, W. H.-S. & Chang, C. Clinical spectrum of food allergies: a comprehensive review. Clin. Rev. Allergy Immunol. 46, 225–240 (2014).
Sicherer, S. H. & Sampson, H. A. Food allergy: epidemiology, pathogenesis, diagnosis, and treatment. J. Allergy Clin. Immunol. 133, 291–307.e5 (2014).
Stefka, A. T. et al. Commensal bacteria protect against food allergen sensitization. Proc. Natl Acad. Sci. USA 111, 13145–13150 (2014).
Liu, S., Yang, B., Yang, P. & Liu, Z. Herbal formula-3 ameliorates OVA-induced food allergy in mice may via modulating the gut microbiota. Am. J. Transl. Res. 11, 5812–5823 (2019).
Takahashi, H. et al. Combined oral intake of short and long fructans alters the gut microbiota in food allergy model mice and contributes to food allergy prevention. BMC Microbiol. 23, 266 (2023).
De Paepe, E., Van Gijseghem, L., De Spiegeleer, M., Cox, E. & Vanhaecke, L. A systematic review of metabolic alterations underlying IgE‐mediated food allergy in children. Mol. Nutr. Food Res. 65, e2100536 (2021).
Sasaki, M. et al. Systematic review of the association between short‐chain fatty acids and allergic diseases. Allergy 79, 1789–1811 (2024).
Son, M.-Y. & Cho, H.-S. Anticancer effects of gut microbiota-derived short-chain fatty acids in cancers. J. Microbiol. Biotechnol. 33, 849–856 (2023).
Yang, Q. et al. A review of gut microbiota‐derived metabolites in tumor progression and cancer therapy. Adv. Sci. 10, e2207366 (2023).
Sun, J. et al. Butyrate as a promising therapeutic target in cancer: from pathogenesis to clinic (review). Int. J. Oncol. 64, 44 (2024).
Mayorga-Ramos, A., Barba-Ostria, C., Simancas-Racines, D. & Guamán, L. P. Protective role of butyrate in obesity and diabetes: new insights. Front. Nutr. 9, 1067647 (2022).
Evans, C. E. L. et al. Effects of dietary fibre type on blood pressure. J. Hypertens. 33, 897–911 (2015).
Marques, F. Z. et al. High-fiber diet and acetate supplementation change the gut microbiota and prevent the development of hypertension and heart failure in hypertensive mice. Circulation 135, 964–977 (2017).
Karbach, S. H. et al. Gut microbiota promote angiotensin II-induced arterial hypertension and vascular dysfunction. J. Am. Heart Assoc. 5, e003698 (2016).
Roshanravan, N. et al. Effect of butyrate and inulin supplementation on glycemic status, lipid profile and glucagon-like peptide 1 level in patients with type 2 diabetes: a randomized double-blind, placebo-controlled trial. Horm. Metab. Res. 49, 886–891 (2017).
Verhaar, B. et al. Oral sodium butyrate increases daytime systolic blood pressure in hypertensive patients: a double-blind, randomized, placebo-controlled trial. J. Hypertens. 41, e77 (2023).
Verhaar, B. J. H. et al. Effects of oral butyrate on blood pressure in patients with hypertension: a randomized, placebo-controlled trial. Hypertension 81, 2124–2136 (2024).
Jie, Z. et al. The gut microbiome in atherosclerotic cardiovascular disease. Nat. Commun. 8, 845 (2017).
Zhou, M. et al. The short-chain fatty acid propionate improved ventricular electrical remodeling in a rat model with myocardial infarction. Food Funct. 12, 12580–12593 (2021).
Jiang, X., Huang, X., Tong, Y. & Gao, H. Butyrate improves cardiac function and sympathetic neural remodeling following myocardial infarction in rats. Can. J. Physiol. Pharmacol. 98, 391–399 (2020).
Chambers, E. S. et al. Acute oral sodium propionate supplementation raises resting energy expenditure and lipid oxidation in fasted humans. Diabetes Obes. Metab. 20, 1034–1039 (2018).
Canfora, E. E. et al. Colonic infusions of short-chain fatty acid mixtures promote energy metabolism in overweight/obese men: a randomized crossover trial. Sci. Rep. 7, 2360 (2017).
Eslick, S., Thompson, C., Berthon, B. & Wood, L. Short-chain fatty acids as anti-inflammatory agents in overweight and obesity: a systematic review and meta-analysis. Nutr. Rev. 80, 838–856 (2022).
Bouter, K. E. C. et al. Differential metabolic effects of oral butyrate treatment in lean versus metabolic syndrome subjects. Clin. Transl. Gastroenterol. 9, e155 (2018).
Khosravi, Z. et al. The effects of butyrate supplementation on glycemic control, lipid profile, blood pressure, nitric oxide level and glutathione peroxidase activity in type 2 diabetic patients: a randomized triple-blind, placebo-controlled trial. Clin. Nutr. ESPEN 49, 79–85 (2022).
de Groot, P. F. et al. Oral butyrate does not affect innate immunity and islet autoimmunity in individuals with longstanding type 1 diabetes: a randomised controlled trial. Diabetologia 63, 597–610 (2020).
Coppola, S. et al. Therapeutic effects of butyrate on pediatric obesity: a randomized clinical trial. JAMA Netw. Open 5, e2244912 (2022).
Byrne, C. S., Chambers, E. S., Morrison, D. J. & Frost, G. The role of short chain fatty acids in appetite regulation and energy homeostasis. Int. J. Obes. 39, 1331–1338 (2015).
Haspeslagh, E., Heyndrickx, I., Hammad, H. & Lambrecht, B. N. The hygiene hypothesis: immunological mechanisms of airway tolerance. Curr. Opin. Immunol. 54, 102–108 (2018).
Roduit, C. et al. High levels of butyrate and propionate in early life are associated with protection against atopy. Allergy 74, 799–809 (2019).
Russell, S. L. et al. Early life antibiotic‐driven changes in microbiota enhance susceptibility to allergic asthma. EMBO Rep. 13, 440–447 (2012).
Cait, A. et al. Microbiome-driven allergic lung inflammation is ameliorated by short-chain fatty acids. Mucosal Immunol. 11, 785–795 (2018).
Depner, M. et al. Maturation of the gut microbiome during the first year of life contributes to the protective farm effect on childhood asthma. Nat. Med. 26, 1766–1775 (2020).
Verma, A. et al. Short-chain fatty acid (SCFA) as a connecting link between microbiota and gut–lung axis — a potential therapeutic intervention to improve lung health. ACS Omega 9, 14648–14671 (2024).
Mirzaei, R. et al. Role of microbiota-derived short-chain fatty acids in nervous system disorders. Biomed. Pharmacother. 139, 111661 (2021).
Li, H. et al. Gut microbiota changes in patients with Alzheimer’s disease spectrum based on 16S rRNA sequencing: a systematic review and meta-analysis. Front. Aging Neurosci. 16, 1422350 (2024).
Matt, S. M. et al. Butyrate and dietary soluble fiber improve neuroinflammation associated with aging in mice. Front. Immunol. 9, 1832 (2018).
Fernando, W. M. A. D. B. et al. Sodium butyrate reduces brain amyloid-β levels and improves cognitive memory performance in an Alzheimer’s disease transgenic mouse model at an early disease stage. J. Alzheimers Dis. 74, 91–99 (2020).
Nishiwaki, H. et al. Meta‐analysis of gut dysbiosis in Parkinson’s disease. Mov. Disord. 35, 1626–1635 (2020).
Nishiwaki, H. et al. Meta-analysis of shotgun sequencing of gut microbiota in Parkinson’s disease. NPJ Parkinsons Dis. 10, 106 (2024).
Liu, J. et al. Sodium butyrate exerts protective effect against Parkinson’s disease in mice via stimulation of glucagon like peptide-1. J. Neurol. Sci. 381, 176–181 (2017).
Guo, T.-T. et al. Neuroprotective effects of sodium butyrate by restoring gut microbiota and inhibiting TLR4 signaling in mice with MPTP-induced Parkinson’s disease. Nutrients 15, 930 (2023).
Zeng, Q. et al. Gut dysbiosis and lack of short chain fatty acids in a Chinese cohort of patients with multiple sclerosis. Neurochem. Int. 129, 104468 (2019).
Duscha, A. et al. Propionic acid shapes the multiple sclerosis disease course by an immunomodulatory mechanism. Cell 180, 1067–1080.e16 (2020).
Chen, T., Noto, D., Hoshino, Y., Mizuno, M. & Miyake, S. Butyrate suppresses demyelination and enhances remyelination. J. Neuroinflammation 16, 1–13 (2019).
Chevalier, A. C. & Rosenberger, T. A. Increasing acetyl‐CoA metabolism attenuates injury and alters spinal cord lipid content in mice subjected to experimental autoimmune encephalomyelitis. J. Neurochem. 141, 721–737 (2017).
Mizuno, M., Noto, D., Kaga, N., Chiba, A. & Miyake, S. The dual role of short fatty acid chains in the pathogenesis of autoimmune disease models. PLoS ONE 12, e0173032 (2017).
Macfarlane, G. T., Gibson, G. R. & Cummings, J. H. Comparison of fermentation reactions in different regions of the human colon. J. Appl. Bacteriol. 72, 57–64 (1992).
van der Beek, C. M. et al. Hepatic uptake of rectally administered butyrate prevents an increase in systemic butyrate concentrations in humans. J. Nutr. 145, 2019–2024 (2015).
van der Beek, C. M. et al. Distal, not proximal, colonic acetate infusions promote fat oxidation and improve metabolic markers in overweight/obese men. Clin. Sci. 130, 2073–2082 (2016).
Edelman, M. J. et al. Clinical and pharmacologic study of tributyrin: an oral butyrate prodrug. Cancer Chemother. Pharmacol. 51, 439–444 (2003).
Donovan, J. D., Bauer, L., Fahey, G. C. & Lee, Y. In vitro digestion and fermentation of microencapsulated tributyrin for the delivery of butyrate. J. Food Sci. 82, 1491–1499 (2017).
Di Sabatino, A. et al. Efficacy of butyrate in the treatment of mild to moderate Crohn’s disease. Dig. Liver Dis. Suppl. 1, 31–35 (2007).
Annison, G., Illman, R. J. & Topping, D. L. Acetylated, propionylated or butyrylated starches raise large bowel short-chain fatty acids preferentially when fed to rats. J. Nutr. 133, 3523–3528 (2003).
Mariño, E. et al. Gut microbial metabolites limit the frequency of autoimmune T cells and protect against type 1 diabetes. Nat. Immunol. 18, 552–562 (2017).
Clarke, J. M. et al. Butyrate esterified to starch is released in the human gastrointestinal tract. Am. J. Clin. Nutr. 94, 1276–1283 (2011).
Le Leu, R. K. et al. Butyrylated starch intake can prevent red meat-induced O6-methyl-2-deoxyguanosine adducts in human rectal tissue: a randomised clinical trial. Br. J. Nutr. 114, 220–230 (2015).
Hutkins, R. et al. Classifying compounds as prebiotics — scientific perspectives and recommendations. Nat. Rev. Gastroenterol. Hepatol. 22, 54–70 (2025).
Wolever, T. M., ter Wal, P., Spadafora, P. & Robb, P. Guar, but not psyllium, increases breath methane and serum acetate concentrations in human subjects. Am. J. Clin. Nutr. 55, 719–722 (1992).
Rahat-Rozenbloom, S., Fernandes, J., Cheng, J., Gloor, G. B. & Wolever, T. M. S. The acute effects of inulin and resistant starch on postprandial serum short-chain fatty acids and second-meal glycemic response in lean and overweight humans. Eur. J. Clin. Nutr. 71, 227–233 (2017).
Markowiak-Kopeć, P. & Śliżewska, K. The effect of probiotics on the production of short-chain fatty acids by human intestinal microbiome. Nutrients 12, 1107 (2020).
El-Salhy, M., Valeur, J., Hausken, T. & Gunnar Hatlebakk, J. Changes in fecal short-chain fatty acids following fecal microbiota transplantation in patients with irritable bowel syndrome. Neurogastroenterol. Motil. 33, e13983 (2021).
Smits, L. P., Bouter, K. E. C., de Vos, W. M., Borody, T. J. & Nieuwdorp, M. Therapeutic potential of fecal microbiota transplantation. Gastroenterology 145, 946–953 (2013).
Arnold, J., Glazier, J. & Mimee, M. Genetic engineering of resident bacteria in the gut microbiome. J. Bacteriol. 205, e0012723 (2023). This mini-review highlights recent progress in genetic engineering to create designer bacteria that produce metabolites capable of impacting host health and creating novel biotherapeutics.
Vázquez-Castellanos, J. F., Biclot, A., Vrancken, G., Huys, G. R. & Raes, J. Design of synthetic microbial consortia for gut microbiota modulation. Curr. Opin. Pharmacol. 49, 52–59 (2019).
Pereira, F. C. & Berry, D. Microbial nutrient niches in the gut. Environ. Microbiol. 19, 1366–1378 (2017).
Letourneau, J. et al. Interplay between particle size and microbial ecology in the gut microbiome. ISME J. 18, wrae168 (2024).
Shetty, S. A. et al. Dynamic metabolic interactions and trophic roles of human gut microbes identified using a minimal microbiome exhibiting ecological properties. ISME J. 16, 2144–2159 (2022).
O’Keefe, S. J. D. et al. Fat, fibre and cancer risk in African Americans and rural Africans. Nat. Commun. 6, 6342 (2015).
Tannock, G. W. Understanding the gut microbiota by considering human evolution: a story of fire, cereals, cooking, molecular ingenuity, and functional cooperation. Microbiol. Mol. Biol. Rev. 88, e0012722 (2024).
Sonnenburg, E. D. & Sonnenburg, J. L. The ancestral and industrialized gut microbiota and implications for human health. Nat. Rev. Microbiol. 17, 383–390 (2019).
O’Keefe, S. J. The association between dietary fibre deficiency and high-income lifestyle-associated diseases: Burkitt’s hypothesis revisited. Lancet Gastroenterol. Hepatol. 4, 984–996 (2019).
Ramsteijn, A. S. & Louis, P. Dietary fibre optimisation in support of global health. Microb. Biotechnol. 17, e14542 (2024).
Taras, D., Simmering, R., Collins, M. D., Lawson, P. A. & Blaut, M. Reclassification of Eubacterium formicigenerans Holdeman and Moore 1974 as Dorea formicigenerans gen. nov., comb. nov., and description of Dorea longicatena sp. nov., isolated from human faeces. Int. J. Syst. Evol. Microbiol. 52, 423–428 (2002).
Holdeman, L. V. & Moore, W. E. C. New genus, Coprococcus, twelve new species, and emended descriptions of four previously described species of bacteria from human feces. Int. J. Syst. Bacteriol. 24, 260–277 (1974).
Togo, A. H. et al. Description of Mediterraneibacter massiliensis, gen. nov., sp. nov., a new genus isolated from the gut microbiota of an obese patient and reclassification of Ruminococcus faecis, Ruminococcus lactaris, Ruminococcus torques, Ruminococcus gnavus and Clostridium glycyrrhizinilyticum as Mediterraneibacter faecis comb. nov., Mediterraneibacter lactaris comb. nov., Mediterraneibacter torques comb. nov., Mediterraneibacter gnavus comb. nov. and Mediterraneibacter glycyrrhizinilyticus comb. nov. Antonie van Leeuwenhoek 111, 2107–2128 (2018).
Flaiz, M. et al. Refining and illuminating acetogenic Eubacterium strains for reclassification and metabolic engineering. Microb. Cell Fact. 23, 24 (2024).
Trischler, R., Roth, J., Sorbara, M. T., Schlegel, X. & Müller, V. A functional Wood–Ljungdahl pathway devoid of a formate dehydrogenase in the gut acetogens Blautia wexlerae, Blautia luti and beyond. Environ. Microbiol. 24, 3111–3123 (2022).
Zhang, B., Lingga, C., De Groot, H. & Hackmann, T. J. The oxidoreductase activity of Rnf balances redox cofactors during fermentation of glucose to propionate in Prevotella. Sci. Rep. 13, 16429 (2023).
Robert, C. & Bernalier-Donadille, A. The cellulolytic microflora of the human colon: evidence of microcrystalline cellulose-degrading bacteria in methane-excreting subjects. FEMS Microbiol. Ecol. 46, 81–89 (2003).
Kettle, H., Louis, P., Holtrop, G., Duncan, S. H. & Flint, H. J. Modelling the emergent dynamics and major metabolites of the human colonic microbiota. Environ. Microbiol. 17, 1615–1630 (2015).
Gupta, R. S., Nanda, A. & Khadka, B. Novel molecular, structural and evolutionary characteristics of the phosphoketolases from bifidobacteria and Coriobacteriales. PLoS ONE 12, e0172176 (2017).
Guillemot, F. et al. Treatment of diversion colitis by short-chain fatty acids: prospective and double-blind study. Dis. Colon Rectum 34, 861–864 (1991).
Patz, J., Jacobsohn, W. Z., Gottschalk-Sabag, S., Zeides, S. & Braverman, D. Z. Treatment of refractory distal ulcerative colitis with short chain fatty acid enemas. Am. J. Gastroenterol. 91, 731–734 (1996).
Steinhart, A. H., Hiruki, T., Brzezinski, A. & Baker, J. P. Treatment of left‐sided ulcerative colitis with butyrate enemas: a controlled trial. Aliment. Pharmacol. Ther. 10, 729–736 (1996).
Scheppach, W. et al. Histological changes in the colonic mucosa following irrigation with short-chain fatty acids. Eur. J. Gastroenterol. Hepatol. 9, 163–168 (1997).
Scheppach, W. & Group, G.-A. S. S. Treatment of distal ulcerative colitis with short-chain fatty acid enemas a placebo-controlled trial. Dig. Dis. Sci. 41, 2254–2259 (1996).
Breuer, R. I. et al. Short chain fatty acid rectal irrigation for left-sided ulcerative colitis: a randomised, placebo controlled trial. Gut 40, 485–491 (1997).
Schauber, J. et al. Local short-chain fatty acids supplementation without beneficial effect on inflammation in excluded rectum. Scand. J. Gastroenterol. 35, 184–189 (2000).
Vernia, P. et al. Topical butyrate for acute radiation proctitis: randomised, crossover trial. Lancet 356, 1232–1235 (2000).
Scarpellini, E. et al. Efficacy of butyrate in the treatment of diarrhoea-predominant irritable bowel syndrome. Dig. Liver Dis. Suppl. 1, 19–22 (2007).
Vernero, M. et al. The usefulness of microencapsulated sodium butyrate add-on therapy in maintaining remission in patients with ulcerative colitis: a prospective observational study. J. Clin. Med. 9, 3941 (2020).
Pietrzak, A. et al. Sodium butyrate effectiveness in children and adolescents with newly diagnosed inflammatory bowel diseases — randomized placebo-controlled multicenter trial. Nutrients 14, 3283 (2022).
Buckel, W. & Thauer, R. K. Flavin-based electron bifurcation, a new mechanism of biological energy coupling. Chem. Rev. 118, 3862–3886 (2018).
Acknowledgements
P.L. received funding from the Scottish Government Rural and Environment Service and Analytical Services Division.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Microbiology thanks Ellen Blaak, Hauke Smidt and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mukhopadhya, I., Louis, P. Gut microbiota-derived short-chain fatty acids and their role in human health and disease. Nat Rev Microbiol 23, 635–651 (2025). https://doi.org/10.1038/s41579-025-01183-w
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41579-025-01183-w
This article is cited by
-
Mendelian randomization analysis of gut microbiota-immune cell interactions in malignant neoplasm of nasopharynx
AMB Express (2025)
-
Feasibility of vinegar processing of toxic herbs in Shi–Zao–Tang: toxicity reduction, efficacy preservation in malignant ascites rats and underlying pharmacodynamic mechanisms
Chinese Medicine (2025)
-
Fecal microbiota transplantation in pigs: current status and future perspective
Animal Microbiome (2025)
-
The microbiome is associated with obesity-related metabolome signature in the process of aging
npj Biofilms and Microbiomes (2025)