Abstract
Plasmodium parasites, which cause malaria, invade and remodel our red blood cells, creating niches in which they replicate. If erythrocyte invasion is blocked during the blood stage of infection, malaria can be prevented. Indeed, a vaccine that targets a component of the erythrocyte invasion machinery has recently shown efficacy against malaria. Erythrocyte invasion occurs through a sequence of temporally organized molecular processes, such as bridging of the erythrocyte and parasite membranes during invasion by the Plasmodium falciparum PCRCR complex. Structural investigations of human antibodies that target invasion machinery, induced by vaccination or natural infection, have revealed neutralizing epitopes and uncovered mechanisms by which antibodies can potentiate the activity of other antibodies. Using rational, structure-guided protein design, these insights are being leveraged to develop targeted vaccine components, with the first rationally designed blood-stage malaria vaccine immunogen now entering clinical trials.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
World Health Organization. World Malaria Report: Addressing Inequity in the Global Malaria Response (WHO, 2024).
Cowman, A. F., Healer, J., Marapana, D. & Marsh, K. Malaria: biology and disease. Cell 167, 610–624 (2016).
Duffy, P. E., Gorres, J. P., Healy, S. A. & Fried, M. Malaria vaccines: a new era of prevention and control. Nat. Rev. Microbiol. 22, 756–772 (2024).
Koch, M. & Baum, J. The mechanics of malaria parasite invasion of the human erythrocyte — towards a reassessment of the host cell contribution. Cell Microbiol. 18, 319–329 (2016).
Moreau, A. et al. Physical mechanisms of red blood cell splenic filtration. Proc. Natl Acad. Sci. USA 120, e2300095120 (2023).
Martinez, M. et al. Rhoptry secretion system structure and priming in Plasmodium falciparum revealed using in situ cryo-electron tomography. Nat. Microbiol. 7, 1230–1238 (2022).
Kadekoppala, M. & Holder, A. A. Merozoite surface proteins of the malaria parasite: the MSP1 complex and the MSP7 family. Int. J. Parasitol. 40, 1155–1161 (2010).
Zuccala, E. S. et al. Subcompartmentalisation of proteins in the rhoptries correlates with ordered events of erythrocyte invasion by the blood stage malaria parasite. PLoS ONE 7, e46160 (2012).
Riglar, D. T. et al. Super-resolution dissection of coordinated events during malaria parasite invasion of the human erythrocyte. Cell Host Microbe 9, 9–20 (2011). This paper provides a powerful demonstration through super-resolution microscopy of the stages of invasion.
Bannister, L. H. & Mitchell, G. H. The fine structure of secretion by Plasmodium knowlesi merozoites during red cell invasion. J. Protozool. 36, 362–367 (1989).
Frenal, K., Dubremetz, J. F., Lebrun, M. & Soldati-Favre, D. Gliding motility powers invasion and egress in apicomplexa. Nat. Rev. Microbiol. 15, 645–660 (2017).
Yahata, K. et al. Gliding motility of Plasmodium merozoites. Proc. Natl Acad. Sci. USA 118, e2114442118 (2021). This article demonstrates that merozoites glide.
Hart, M. N. et al. Sequential roles for red blood cell binding proteins enable phased commitment to invasion for malaria parasites. Nat. Commun. 14, 4619 (2023).
Scally, S. W. et al. PCRCR complex is essential for invasion of human erythrocytes by Plasmodium falciparum. Nat. Microbiol. 7, 2039–2053 (2022).
Weiss, G. E. et al. Revealing the sequence and resulting cellular morphology of receptor-ligand interactions during Plasmodium falciparum invasion of erythrocytes. PLoS Pathog. 11, e1004670 (2015).
Ben Chaabene, R., Lentini, G. & Soldati-Favre, D. Biogenesis and discharge of the rhoptries: key organelles for entry and hijack of host cells by the apicomplexa. Mol. Microbiol. 115, 453–465 (2021).
Cova, M. M., Lamarque, M. H. & Lebrun, M. How apicomplexa parasites secrete and build their invasion machinery. Annu. Rev. Microbiol. 76, 619–640 (2022).
Besteiro, S., Dubremetz, J. F. & Lebrun, M. The moving junction of apicomplexan parasites: a key structure for invasion. Cell Microbiol. 13, 797–805 (2011).
Harris, P. K. et al. Molecular identification of a malaria merozoite surface sheddase. PLoS Pathog. 1, 241–251 (2005).
Pavlou, G. et al. Toxoplasma parasite twisting motion mechanically induces host cell membrane fission to complete invasion within a protective vacuole. Cell Host Microbe 24, 81–96.e5 (2018).
Bisio, H. & Soldati-Favre, D. Signaling cascades governing entry into and exit from host cells by Toxoplasma gondii. Annu. Rev. Microbiol. 73, 579–599 (2019).
Singh, S., Alam, M. M., Pal-Bhowmick, I., Brzostowski, J. A. & Chitnis, C. E. Distinct external signals trigger sequential release of apical organelles during erythrocyte invasion by malaria parasites. PLoS Pathog. 6, e1000746 (2010).
Tham, W. H., Healer, J. & Cowman, A. F. Erythrocyte and reticulocyte binding-like proteins of Plasmodium falciparum. Trends Parasitol. 28, 23–30 (2012).
Iyer, J., Gruner, A. C., Renia, L., Snounou, G. & Preiser, P. R. Invasion of host cells by malaria parasites: a tale of two protein families. Mol. Microbiol. 65, 231–249 (2007).
Sim, B. K., Chitnis, C. E., Wasniowska, K., Hadley, T. J. & Miller, L. H. Receptor and ligand domains for invasion of erythrocytes by Plasmodium falciparum. Science 264, 1941–1944 (1994).
Orlandi, P. A., Klotz, F. W. & Haynes, J. D. A malaria invasion receptor, the 175-kilodalton erythrocyte binding antigen of Plasmodium falciparum recognizes the terminal Neu5Ac(alpha 2-3)Gal- sequences of glycophorin A. J. Cell Biol. 116, 901–909 (1992).
Tolia, N. H., Enemark, E. J., Sim, B. K. & Joshua-Tor, L. Structural basis for the EBA-175 erythrocyte invasion pathway of the malaria parasite Plasmodium falciparum. Cell 122, 183–193 (2005).
Tham, W. H. et al. Complement receptor 1 is the host erythrocyte receptor for Plasmodium falciparum PfRh4 invasion ligand. Proc. Natl Acad. Sci. USA 107, 17327–17332 (2010).
Duraisingh, M. T., Maier, A. G., Triglia, T. & Cowman, A. F. Erythrocyte-binding antigen 175 mediates invasion in Plasmodium falciparum utilizing sialic acid-dependent and -independent pathways. Proc. Natl Acad. Sci. USA 100, 4796–4801 (2003).
Stubbs, J. et al. Molecular mechanism for switching of P. falciparum invasion pathways into human erythrocytes. Science 309, 1384–1387 (2005). This paper shows that merozoites can switch between different invasion pathways that use different EBL and RBL proteins.
Gruszczyk, J. et al. Cryo-EM structure of an essential Plasmodium vivax invasion complex. Nature 559, 135–139 (2018).
Gruszczyk, J. et al. Transferrin receptor 1 is a reticulocyte-specific receptor for Plasmodium vivax. Science 359, 48–55 (2018).
Moon, R. W. et al. Normocyte-binding protein required for human erythrocyte invasion by the zoonotic malaria parasite Plasmodium knowlesi. Proc. Natl Acad. Sci. USA 113, 7231–7236 (2016).
Tham, W. H. et al. Plasmodium falciparum adhesins play an essential role in signalling and activation of invasion into human erythrocytes. PLoS Pathog. 11, e1005343 (2015).
Volz, J. C. et al. Essential role of the PfRh5/PfRipr/CyRPA complex during Plasmodium falciparum invasion of erythrocytes. Cell Host Microbe 20, 60–71 (2016).
Farrell, B. et al. The PfRCR complex bridges malaria parasite and erythrocyte during invasion. Nature 625, 578–584 (2024). Using cryoEM, this paper visualises the bridge between merozoite and erythrocyte formed by the PfPCRCR complex.
Baum, J. et al. Reticulocyte-binding protein homologue 5 — an essential adhesin involved in invasion of human erythrocytes by Plasmodium falciparum. Int. J. Parasitol. 39, 371–380 (2009).
Crosnier, C. et al. Basigin is a receptor essential for erythrocyte invasion by Plasmodium falciparum. Nature 480, 534–537 (2011). This article presents the discovery that basigin is the erythrocyte ligand for PfRH5.
Wright, K. E. et al. Structure of malaria invasion protein RH5 with erythrocyte basigin and blocking antibodies. Nature 515, 427–430 (2014). This paper shows how PfRH5 binds to basigin and inhibitory antibodies.
Zenonos, Z. A. et al. Basigin is a druggable target for host-oriented antimalarial interventions. J. Exp. Med. 212, 1145–1151 (2015).
Douglas, A. D. et al. The blood-stage malaria antigen PfRH5 is susceptible to vaccine-inducible cross-strain neutralizing antibody. Nat. Commun. 2, 601 (2011).
Patel, S. D. et al. Plasmodium falciparum merozoite surface antigen, PfRH5, elicits detectable levels of invasion-inhibiting antibodies in humans. J. Infect. Dis. 208, 1679–1687 (2013).
Tran, T. M. et al. Naturally acquired antibodies specific for Plasmodium falciparum reticulocyte-binding protein homologue 5 inhibit parasite growth and predict protection from malaria. J. Infect. Dis. 209, 789–798 (2014).
Douglas, A. D. et al. Neutralization of Plasmodium falciparum merozoites by antibodies against PfRH5. J. Immunol. 192, 245–258 (2014).
Alanine, D. G. W. et al. Human antibodies that slow erythrocyte invasion potentiate malaria-neutralizing antibodies. Cell 178, 216–228 (2019). This article characterizes human antibodies that target PfRH5.
Wang, L. T. et al. Natural malaria infection elicits rare but potent neutralizing antibodies to the blood-stage antigen RH5. Cell 187, 4981–4995 (2024).
Wong, W. et al. Structure of Plasmodium falciparum Rh5–CyRPA–Ripr invasion complex. Nature 565, 118–121 (2019).
Aniweh, Y. et al. P. falciparum RH5-Basigin interaction induces changes in the cytoskeleton of the host RBC. Cell Microbiol. 19, e12747 (2017).
Schmidt, N. et al. Neuroplastin and basigin are essential auxiliary subunits of plasma membrane Ca2+-ATPases and key regulators of Ca2+ clearance. Neuron 96, 827–838 (2017).
Jamwal, A. et al. Erythrocyte invasion-neutralising antibodies prevent Plasmodium falciparum RH5 from binding to basigin-containing membrane protein complexes. eLife 12, e83681 (2023).
Reddy, K. S. et al. Multiprotein complex between the GPI-anchored CyRPA with PfRH5 and PfRipr is crucial for Plasmodium falciparum erythrocyte invasion. Proc. Natl Acad. Sci. USA 112, 1179–1184 (2015).
Chen, L. et al. An EGF-like protein forms a complex with PfRh5 and is required for invasion of human erythrocytes by Plasmodium falciparum. PLoS Pathog. 7, e1002199 (2011).
Chen, L. et al. Structural basis for inhibition of erythrocyte invasion by antibodies to Plasmodium falciparum protein CyRPA. eLife 6, e21347 (2017).
Favuzza, P. et al. Structure of the malaria vaccine candidate antigen CyRPA and its complex with a parasite invasion inhibitory antibody. eLife 6, e20383 (2017).
Knuepfer, E. et al. Divergent roles for the RH5 complex components, CyRPA and RIPR in human-infective malaria parasites. PLoS Pathog. 15, e1007809 (2019).
Thompson, J. et al. PTRAMP; a conserved Plasmodium thrombospondin-related apical merozoite protein. Mol. Biochem. Parasitol. 134, 225–232 (2004).
Siddiqui, F. A. et al. A thrombospondin structural repeat containing rhoptry protein from Plasmodium falciparum mediates erythrocyte invasion. Cell Microbiol. 15, 1341–1356 (2013).
Triglia, T. et al. Plasmepsin X activates the PCRCR complex of Plasmodium falciparum by processing PfRh5 for erythrocyte invasion. Nat. Commun. 14, 2219 (2023).
Moskovitz, R. et al. Structural basis for DARC binding in reticulocyte invasion by Plasmodium vivax. Nat. Commun. 14, 3637 (2023).
Horuk, R. et al. A receptor for the malarial parasite Plasmodium vivax: the erythrocyte chemokine receptor. Science 261, 1182–1184 (1993).
Alexander, D. L., Mital, J., Ward, G. E., Bradley, P. & Boothroyd, J. C. Identification of the moving junction complex of Toxoplasma gondii: a collaboration between distinct secretory organelles. PLoS Pathog. 1, e17 (2005). This study identifies the RON complexes as a binding partner of AMA1.
Lamarque, M. et al. The RON2-AMA1 interaction is a critical step in moving junction-dependent invasion by apicomplexan parasites. PLoS Pathog. 7, e1001276 (2011).
Vulliez-Le Normand, B. et al. Structural and functional insights into the malaria parasite moving junction complex. PLoS Pathog. 8, e1002755 (2012).
Tonkin, M. L. et al. Host cell invasion by apicomplexan parasites: insights from the co-structure of AMA1 with a RON2 peptide. Science 333, 463–467 (2011).
Richard, D. et al. Interaction between Plasmodium falciparum apical membrane antigen 1 and the rhoptry neck protein complex defines a key step in the erythrocyte invasion process of malaria parasites. J. Biol. Chem. 285, 14815–14822 (2010).
Srinivasan, P. et al. Binding of Plasmodium merozoite proteins RON2 and AMA1 triggers commitment to invasion. Proc. Natl Acad. Sci. USA 108, 13275–13280 (2011).
Soldati, D., Foth, B. J. & Cowman, A. F. Molecular and functional aspects of parasite invasion. Trends Parasitol. 20, 567–574 (2004).
Gonzalez, V. et al. Host cell entry by apicomplexa parasites requires actin polymerization in the host cell. Cell Host Microbe 5, 259–272 (2009).
Dobrowolski, J. M. & Sibley, L. D. Toxoplasma invasion of mammalian cells is powered by the actin cytoskeleton of the parasite. Cell 84, 933–939 (1996).
Angrisano, F. et al. Spatial localisation of actin filaments across developmental stages of the malaria parasite. PLoS ONE 7, e32188 (2012).
Guerin, A. et al. Efficient invasion by Toxoplasma depends on the subversion of host protein networks. Nat. Microbiol. 2, 1358–1366 (2017).
Bargieri, D. et al. Host cell invasion by apicomplexan parasites: the junction conundrum. PLoS Pathog. 10, e1004273 (2014).
Dasgupta, S. et al. Membrane-wrapping contributions to malaria parasite invasion of the human erythrocyte. Biophys. J. 107, 43–54 (2014).
Cohen, S., Mc, G. I. & Carrington, S. Gamma-globulin and acquired immunity to human malaria. Nature 192, 733–737 (1961).
Siddiqui, W. A. An effective immunization of experimental monkeys against a human malaria parasite, Plasmodium falciparum. Science 197, 388–389 (1977).
Chauhan, V. S., Yazdani, S. S. & Gaur, D. Malaria vaccine development based on merozoite surface proteins of Plasmodium falciparum. Hum. Vaccin. 6, 757–762 (2010).
Siddiqui, W. A. et al. Merozoite surface coat precursor protein completely protects Aotus monkeys against Plasmodium falciparum malaria. Proc. Natl Acad. Sci. USA 84, 3014–3018 (1987).
Stowers, A. W. et al. Vaccination of monkeys with recombinant Plasmodium falciparum apical membrane antigen 1 confers protection against blood-stage malaria. Infect. Immun. 70, 6961–6967 (2002).
Thera, M. A. et al. A field trial to assess a blood-stage malaria vaccine. N. Engl. J. Med. 365, 1004–1013 (2011).
Ogutu, B. R. et al. Blood stage malaria vaccine eliciting high antigen-specific antibody concentrations confers no protection to young children in Western Kenya. PLoS ONE 4, e4708 (2009).
Patel, P. N. et al. Structure-based design of a strain transcending AMA1-RON2L malaria vaccine. Nat. Commun. 14, 5345 (2023).
Blank, A. et al. Immunization with full-length Plasmodium falciparum merozoite surface protein 1 is safe and elicits functional cytophilic antibodies in a randomized first-in-human trial. npj Vaccines 5, 10 (2020).
Natama, H. M. et al. Safety and efficacy of the blood-stage malaria vaccine RH5.1/Matrix-M in Burkina Faso: interim results of a double-blind, randomised, controlled, phase 2b trial in children. Lancet Infect. Dis. 25, 495–506 (2024). This trial demonstrates efficacy from a blood stage malaria vaccine in humans.
Douglas, A. D. et al. A PfRH5-based vaccine is efficacious against heterologous strain blood-stage Plasmodium falciparum infection in Aotus monkeys. Cell Host Microbe 17, 130–139 (2015).
Stowers, A. W. & Miller, L. H. Are trials in new world monkeys on the critical path for blood-stage malaria vaccine development? Trends Parasitol. 17, 415–419 (2001).
Douglas, A. D. et al. A defined mechanistic correlate of protection against Plasmodium falciparum malaria in non-human primates. Nat. Commun. 10, 1953 (2019).
Cooper, M. M., Loiseau, C., McCarthy, J. S. & Doolan, D. L. Human challenge models: tools to accelerate the development of malaria vaccines. Expert Rev. Vaccines 18, 241–251 (2019).
Miura, K. et al. Assessment of precision in growth inhibition assay (GIA) using human anti-PfRH5 antibodies. Malar. J. 22, 159 (2023).
Payne, R. O. et al. Human vaccination against RH5 induces neutralizing antimalarial antibodies that inhibit RH5 invasion complex interactions. JCI Insight 2, e96381 (2017).
Minassian, A. M. et al. Reduced blood-stage malaria growth and immune correlates in humans following RH5 vaccination. Med 2, 701–719 (2021).
Silk, S. E. et al. Superior antibody immunogenicity of a viral-vectored RH5 blood-stage malaria vaccine in Tanzanian infants as compared to adults. Med 4, 668–686 (2023).
Silk, S. E. et al. Blood-stage malaria vaccine candidate RH5.1/Matrix-M in healthy Tanzanian adults and children; an open-label, non-randomised, first-in-human, single-centre, phase 1b trial. Lancet Infect. Dis. 24, 1105–1117 (2024).
Barrett, J. R. et al. Analysis of the diverse antigenic landscape of the malaria protein RH5 identifies a potent vaccine-induced human public antibody clonotype. Cell 187, 4964–4980 (2024).
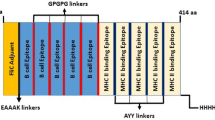
Harrison, T. E. et al. Rational structure-guided design of a blood stage malaria vaccine immunogen presenting a single epitope from PfRH5. EMBO Mol. Med. 16, 2539–2559 (2024).
Wang, N. et al. Structural basis of human monocarboxylate transporter 1 inhibition by anti-cancer drug candidates. Cell 184, 370–383 (2021).
Gong, D. et al. Structure of the human plasma membrane Ca2+-ATPase 1 in complex with its obligatory subunit neuroplastin. Nat. Commun. 9, 3623 (2018).
Ragotte, R. J. et al. Heterotypic interactions drive antibody synergy against a malaria vaccine candidate. Nat. Commun. 13, 933 (2022).
Campeotto, I. et al. One-step design of a stable variant of the malaria invasion protein RH5 for use as a vaccine immunogen. Proc. Natl Acad. Sci. USA 114, 998–1002 (2017). This paper reports the design of RH5.2 vaccine.
King, L. D. W. et al. Preclinical development of a stabilized RH5 virus-like particle vaccine that induces improved antimalarial antibodies. Cell Rep. Med. 5, 101654 (2024).
Andrews, M., Baum, J., Gilson, P. R. & Wilson, D. W. Bottoms up! Malaria parasite invasion the right way around. Trends Parasitol. 39, 1004–1013 (2023).
Jumper, J. et al. Highly accurate protein structure prediction with AlphaFold. Nature 596, 583–589 (2021).
Varadi, M. et al. AlphaFold protein structure database: massively expanding the structural coverage of protein-sequence space with high-accuracy models. Nucleic Acids Res. 50, D439–D444 (2021).
Rts, S. C. T. P. Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet 386, 31–45 (2015).
Datoo, M. S. et al. Safety and efficacy of malaria vaccine candidate R21/Matrix-M in African children: a multicentre, double-blind, randomised, phase 3 trial. Lancet 403, 533–544 (2024).
Kappe, S. H., Vaughan, A. M., Boddey, J. A. & Cowman, A. F. That was then but this is now: malaria research in the time of an eradication agenda. Science 328, 862–866 (2010).
Acknowledgements
For the studies of erythrocyte invasion, the authors are grateful for funding in the form of an Investigator Award from Wellcome (220797/Z/20/Z). For the structural studies of inhibitory monoclonal antibodies and structure-guided vaccine design projects, the authors are grateful for funding from the Medical Research Council (APP22787 and APP36549) and the Gates Foundation.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
M.K.H. and N.A. are named inventors on patents relating to antibodies targeting PfRH5 and structure-guided design of PfRH5-based and PfCyRPA-based vaccine immunogens. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Microbiology thanks Alan Cowman, who co-reviewed with Stephen Scally, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alam, N., Farrell, B., Jamwal, A. et al. Erythrocyte invasion in malaria: from molecular mechanisms to rational vaccines. Nat Rev Microbiol 24, 97–110 (2026). https://doi.org/10.1038/s41579-025-01235-1
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41579-025-01235-1