Abstract
Ageing is characterized by progressive functional decline and increase in disease risk and imposes substantial burdens on human health. Identifying aging biomarkers in primates is crucial for advancing our understanding of human ageing and for informing interventions to mitigate age-related pathologies. However, a comprehensive grasp of these biomarkers is still lacking, hindering the translation of fundamental research into clinical practice. In this Review, we present the current knowledge on biomarkers of ageing at the cellular, tissue and organism levels in humans and non-human primates. Through systematic analysis of representative biomarkers across diverse biological contexts and scales, we discuss both the variability and the conservation of ageing-associated physiological changes, underscoring their importance in assessing and intervening in the ageing process. Finally, we critically assess challenges in ageing research and outline strategic avenues for future investigation.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Cai, Y. et al. The landscape of aging. Sci. China Life Sci. 65, 2354–2454 (2022).
Partridge, L., Deelen, J. & Slagboom, P. E. Facing up to the global challenges of ageing. Nature 561, 45–56 (2018).
Chang, A. Y., Skirbekk, V. F., Tyrovolas, S., Kassebaum, N. J. & Dieleman, J. L. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health 4, e159–e167 (2019).
Crimmins, E. M. Recent trends and increasing differences in life expectancy present opportunities for multidisciplinary research on aging. Nat. Aging 1, 12–13 (2021).
Peng, Y. et al. Ethical concerns in aging research: perspectives of global frontline researchers. Sci. China Life Sci. 67, 2149–2156 (2024).
Moqri, M. et al. Biomarkers of aging for the identification and evaluation of longevity interventions. Cell 186, 3758–3775 (2023).
Bao, H. et al. Biomarkers of aging. Sci. China Life Sci. 66, 893–1066 (2023).
Ying, K. et al. Causality-enriched epigenetic age uncouples damage and adaptation. Nat. Aging 4, 231–246 (2024).
Waziry, R. et al. Effect of long-term caloric restriction on DNA methylation measures of biological aging in healthy adults from the CALERIE trial. Nat. Aging 3, 248–257 (2023).
Liu, X. et al. Resurrection of endogenous retroviruses during aging reinforces senescence. Cell 186, 287–304.e26 (2023).
Yu, L. et al. IgG is an aging factor that drives adipose tissue fibrosis and metabolic decline. Cell Metab. 36, 793–807.e5 (2024).
Yu, Z. et al. Thermal facial image analyses reveal quantitative hallmarks of aging and metabolic diseases. Cell Metab. 36, 1482–1493.e7 (2024).
Ma, S. et al. Spatial transcriptomic landscape unveils immunoglobin-associated senescence as a hallmark of aging. Cell 187, 7025–7044.e34 (2024).
Yang, Y. et al. Metformin decelerates aging clock in male monkeys. Cell 187, 6358–6378.e29 (2024).
Serrano, M., Lin, A. W., McCurrach, M. E., Beach, D. & Lowe, S. W. Oncogenic ras provokes premature cell senescence associated with accumulation of p53 and p16INK4a. Cell 88, 593–602 (1997).
Herbig, U., Ferreira, M., Condel, L., Carey, D. & Sedivy, J. M. Cellular senescence in aging primates. Science 311, 1257 (2006).
Suda, K. et al. Plasma membrane damage limits replicative lifespan in yeast and induces premature senescence in human fibroblasts. Nat. Aging 4, 319–335 (2024).
Zhang, W. et al. Aging stem cells. A Werner syndrome stem cell model unveils heterochromatin alterations as a driver of human aging. Science 348, 1160–1163 (2015).
Wu, Z. et al. Differential stem cell aging kinetics in Hutchinson–Gilford progeria syndrome and Werner syndrome. Protein Cell 9, 333–350 (2018).
Wang, C. et al. RIG-I-driven CDKN1A stabilization reinforces cellular senescence. Sci. China Life Sci. 68, 1646–1661 (2025).
Lin, J. R., Shen, W. L., Yan, C. & Gao, P. J. Downregulation of dynamin-related protein 1 contributes to impaired autophagic flux and angiogenic function in senescent endothelial cells. Arterioscler. Thromb. Vasc. Biol. 35, 1413–1422 (2015).
Diekman, B. O. et al. Expression of p16INK4a is a biomarker of chondrocyte aging but does not cause osteoarthritis. Aging Cell 17, e12771 (2018).
Han, Z. et al. Role of p21 in apoptosis and senescence of human colon cancer cells treated with camptothecin. J. Biol. Chem. 277, 17154–17160 (2002).
Li, Q. et al. NSUN2-mediated m5C methylation and METTL3/METTL14-mediated m6A methylation cooperatively enhance p21 translation. J. Cell. Biochem. 118, 2587–2598 (2017).
Sun, S. et al. CHIT1-positive microglia drive motor neuron ageing in the primate spinal cord. Nature 624, 611–620 (2023).
Victorelli, S. et al. Senescent human melanocytes drive skin ageing via paracrine telomere dysfunction. EMBO J. 38, e101982 (2019).
Jeyapalan, J. C., Ferreira, M., Sedivy, J. M. & Herbig, U. Accumulation of senescent cells in mitotic tissue of aging primates. Mech. Ageing Dev. 128, 36–44 (2007).
Aguado, J. et al. Senolytic therapy alleviates physiological human brain aging and COVID-19 neuropathology. Nat. Aging 3, 1561–1575 (2023).
Shaker, M. R., Aguado, J., Chaggar, H. K. & Wolvetang, E. J. Klotho inhibits neuronal senescence in human brain organoids. npj Aging Mech. Dis. 7, 18 (2021).
Ye, Y. et al. SIRT2 counteracts primate cardiac aging via deacetylation of STAT3 that silences CDKN2B. Nat. Aging 3, 1269–1287 (2023).
Yang, S. et al. A single-nucleus transcriptomic atlas of primate liver aging uncovers the pro-senescence role of SREBP2 in hepatocytes. Protein Cell 15, 98–120 (2024).
Melk, A. et al. Expression of p16INK4a and other cell cycle regulator and senescence associated genes in aging human kidney. Kidney Int. 65, 510–520 (2004).
Wang, W. et al. A genome-wide CRISPR-based screen identifies KAT7 as a driver of cellular senescence. Sci. Transl. Med. 13, eabd2655 (2021).
Park, S. S. et al. p15INK4B is an alternative marker of senescent tumor cells in colorectal cancer. Heliyon 9, e13170 (2023).
Tang, H. et al. NSun2 delays replicative senescence by repressing p27 (KIP1) translation and elevating CDK1 translation. Aging 7, 1143–1158 (2015).
Park, S. H., Lim, J. S. & Jang, K. L. All-trans retinoic acid induces cellular senescence via upregulation of p16, p21, and p27. Cancer Lett. 310, 232–239 (2011).
Ogrodnik, M. et al. Guidelines for minimal information on cellular senescence experimentation in vivo. Cell 187, 4150–4175 (2024).
Dehkordi, S. K. et al. Profiling senescent cells in human brains reveals neurons with CDKN2D/p19 and tau neuropathology. Nat. Aging 1, 1107–1116 (2021).
Suryadevara, V. et al. SenNet recommendations for detecting senescent cells in different tissues. Nat. Rev. Mol. Cell Biol. 25, 1001–1023 (2024).
Beauséjour, C. M. et al. Reversal of human cellular senescence: roles of the p53 and p16 pathways. EMBO J. 22, 4212–4222 (2003).
Kubben, F. J. et al. Proliferating cell nuclear antigen (PCNA): a new marker to study human colonic cell proliferation. Gut 35, 530–535 (1994).
Sun, X. & Kaufman, P. D. Ki-67: more than a proliferation marker. Chromosoma 127, 175–186 (2018).
Davalos, A. R. et al. p53-dependent release of Alarmin HMGB1 is a central mediator of senescent phenotypes. J. Cell Biol. 201, 613–629 (2013).
Kohli, J. et al. Algorithmic assessment of cellular senescence in experimental and clinical specimens. Nat. Protoc. 16, 2471–2498 (2021).
Liang, C. et al. BMAL1 moonlighting as a gatekeeper for LINE1 repression and cellular senescence in primates. Nucleic Acids Res. 50, 3323–3347 (2022).
d’Adda di Fagagna, F. et al. A DNA damage checkpoint response in telomere-initiated senescence. Nature 426, 194–198 (2003).
Alfano, M. et al. Aging, inflammation and DNA damage in the somatic testicular niche with idiopathic germ cell aplasia. Nat. Commun. 12, 5205 (2021).
Wu, M. et al. Spatiotemporal transcriptomic changes of human ovarian aging and the regulatory role of FOXP1. Nat. Aging 4, 527–545 (2024).
Sedelnikova, O. A. et al. Delayed kinetics of DNA double-strand break processing in normal and pathological aging. Aging Cell 7, 89–100 (2008).
Zhang, H. et al. Single-nucleus transcriptomic landscape of primate hippocampal aging. Protein Cell 12, 695–716 (2021).
Liu, Z. et al. Large-scale chromatin reorganization reactivates placenta-specific genes that drive cellular aging. Dev. Cell 57, 1347–1368.e12 (2022).
Hewitt, G. et al. Telomeres are favoured targets of a persistent DNA damage response in ageing and stress-induced senescence. Nat. Commun. 3, 708 (2012).
Fumagalli, M. et al. Telomeric DNA damage is irreparable and causes persistent DNA-damage-response activation. Nat. Cell Biol. 14, 355–365 (2012).
Shim, H. S. et al. TERT activation targets DNA methylation and multiple aging hallmarks. Cell 187, 4030–4042.e13 (2024).
Barnes, R. P. et al. Telomeric 8-oxo-guanine drives rapid premature senescence in the absence of telomere shortening. Nat. Struct. Mol. Biol. 29, 639–652 (2022).
Zou, Z. et al. A single-cell transcriptomic atlas of human skin aging. Dev. Cell 56, 383–397.e8 (2021).
Wang, S. et al. Single-cell transcriptomic atlas of primate ovarian aging. Cell 180, 585–600.e19 (2020).
Huang, Z. et al. Single-cell analysis of somatic mutations in human bronchial epithelial cells in relation to aging and smoking. Nat. Genet. 54, 492–498 (2022).
Choudhury, S. et al. Somatic mutations in single human cardiomyocytes reveal age-associated DNA damage and widespread oxidative genotoxicity. Nat. Aging 2, 714–725 (2022).
Cagan, A. et al. Somatic mutation rates scale with lifespan across mammals. Nature 604, 517–524 (2022).
Krupina, K., Goginashvili, A. & Cleveland, D. W. Causes and consequences of micronuclei. Curr. Opin. Cell Biol. 70, 91–99 (2021).
Miller, K. N., Dasgupta, N., Liu, T., Adams, P. D. & Vizioli, M. G. Cytoplasmic chromatin fragments — from mechanisms to therapeutic potential. eLife 10, e63728 (2021).
Ganz, J. et al. Contrasting somatic mutation patterns in aging human neurons and oligodendrocytes. Cell 187, 1955–1970.e23 (2024).
Dou, Z. et al. Cytoplasmic chromatin triggers inflammation in senescence and cancer. Nature 550, 402–406 (2017).
Vizioli, M. G. et al. Mitochondria-to-nucleus retrograde signaling drives formation of cytoplasmic chromatin and inflammation in senescence. Genes Dev. 34, 428–445 (2020).
Técher, H. et al. MRE11 and TREX1 control senescence by coordinating replication stress and interferon signaling. Nat. Commun. 15, 5423 (2024).
Wu, Z., Qu, J. & Liu, G. H. Roles of chromatin and genome instability in cellular senescence and their relevance to ageing and related diseases. Nat. Rev. Mol. Cell Biol. 25, 979–1000 (2024).
Kaul, Z., Cesare, A. J., Huschtscha, L. I., Neumann, A. A. & Reddel, R. R. Five dysfunctional telomeres predict onset of senescence in human cells. EMBO Rep. 13, 52–59 (2011).
Minamino, T. et al. Endothelial cell senescence in human atherosclerosis: role of telomere in endothelial dysfunction. Circulation 105, 1541–1544 (2002).
Zhang, X. et al. Telomere-dependent and telomere-independent roles of RAP1 in regulating human stem cell homeostasis. Protein Cell 10, 649–667 (2019).
Steinert, S., White, D. M., Zou, Y., Shay, J. W. & Wright, W. E. Telomere biology and cellular aging in nonhuman primate cells. Exp. Cell Res. 272, 146–152 (2002).
Wu, Z., Zhang, W., Qu, J. & Liu, G. H. Emerging epigenetic insights into aging mechanisms and interventions. Trends Pharmacol. Sci. 45, 157–172 (2024).
Seale, K., Horvath, S., Teschendorff, A., Eynon, N. & Voisin, S. Making sense of the ageing methylome. Nat. Rev. Genet. 23, 585–605 (2022).
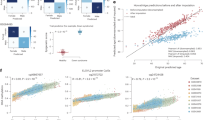
Horvath, S. DNA methylation age of human tissues and cell types. Genome Biol. 14, R115 (2013).
Hannum, G. et al. Genome-wide methylation profiles reveal quantitative views of human aging rates. Mol. Cell 49, 359–367 (2013).
Lu, A. T. et al. Universal DNA methylation age across mammalian tissues. Nat. Aging 3, 1144–1166 (2023).
Horvath, S. et al. Epigenetic clock for skin and blood cells applied to Hutchinson Gilford Progeria syndrome and ex vivo studies. Aging 10, 1758–1775 (2018).
Jasinska, A. J. et al. Epigenetic clock and methylation studies in vervet monkeys. Geroscience 44, 699–717 (2022).
Horvath, S. et al. Pan-primate studies of age and sex. Geroscience 45, 3187–3209 (2023).
Zheng, Z. et al. DNA methylation clocks for estimating biological age in Chinese cohorts. Protein Cell 15, 575–593 (2024).
Scaffidi, P. & Misteli, T. Lamin A-dependent nuclear defects in human aging. Science 312, 1059–1063 (2006).
Della Valle, F. et al. LINE-1 RNA causes heterochromatin erosion and is a target for amelioration of senescent phenotypes in progeroid syndromes. Sci. Transl. Med. 14, eabl6057 (2022).
Zhang, X. et al. The loss of heterochromatin is associated with multiscale three-dimensional genome reorganization and aberrant transcription during cellular senescence. Genome Res. 31, 1121–1135 (2021).
Zhang, H. et al. Nuclear lamina erosion-induced resurrection of endogenous retroviruses underlies neuronal aging. Cell Rep. 42, 112593 (2023).
Zhang, Y. et al. Single-nucleus transcriptomics reveals a gatekeeper role for FOXP1 in primate cardiac aging. Protein Cell 14, 279–293 (2023).
Liang, C. et al. Stabilization of heterochromatin by CLOCK promotes stem cell rejuvenation and cartilage regeneration. Cell Res. 31, 187–205 (2021).
Zhao, H. et al. Destabilizing heterochromatin by APOE mediates senescence. Nat. Aging 2, 303–316 (2022).
Van Meter, M. et al. SIRT6 represses LINE1 retrotransposons by ribosylating KAP1 but this repression fails with stress and age. Nat. Commun. 5, 5011 (2014).
De Cecco, M. et al. L1 drives IFN in senescent cells and promotes age-associated inflammation. Nature 566, 73–78 (2019).
Bi, S. et al. SIRT7 antagonizes human stem cell aging as a heterochromatin stabilizer. Protein Cell 11, 483–504 (2020).
Liu, F. et al. Identification of FOXO1 as a geroprotector in human synovium through single-nucleus transcriptomic profiling. Protein Cell 15, 441–459 (2024).
Hu, Q. et al. Single-nucleus transcriptomics uncovers a geroprotective role of YAP in primate gingival aging. Protein Cell 15, 612–632 (2024).
Mao, J. et al. Reactivation of senescence-associated endogenous retroviruses by ATF3 drives interferon signaling in aging. Nat. Aging 4, 1794–1812 (2024).
Zhou, S., Liu, L. & Lu, X. Endogenous retroviruses make aging go viral. Life Med. 2, lnad001 (2023).
Ren, R. et al. Visualization of aging-associated chromatin alterations with an engineered TALE system. Cell Res. 27, 483–504 (2017).
Ren, X. et al. Maintenance of nucleolar homeostasis by CBX4 alleviates senescence and osteoarthritis. Cell Rep. 26, 3643–3656.e7 (2019).
Swanson, E. C., Manning, B., Zhang, H. & Lawrence, J. B. Higher-order unfolding of satellite heterochromatin is a consistent and early event in cell senescence. J. Cell Biol. 203, 929–942 (2013).
Narita, M. et al. Rb-mediated heterochromatin formation and silencing of E2F target genes during cellular senescence. Cell 113, 703–716 (2003).
Chandra, T. et al. Independence of repressive histone marks and chromatin compaction during senescent heterochromatic layer formation. Mol. Cell 47, 203–214 (2012).
Kreiling, J. A. et al. Age-associated increase in heterochromatic marks in murine and primate tissues. Aging Cell 10, 292–304 (2011).
Diao, Z. et al. SIRT3 consolidates heterochromatin and counteracts senescence. Nucleic Acids Res. 49, 4203–4219 (2021).
Grootaert, M. O. J., Finigan, A., Figg, N. L., Uryga, A. K. & Bennett, M. R. SIRT6 protects smooth muscle cells from senescence and reduces atherosclerosis. Circ. Res. 128, 474–491 (2021).
Criscione, S. W. et al. Reorganization of chromosome architecture in replicative cellular senescence. Sci. Adv. 2, e1500882 (2016).
Bi, S. et al. The sirtuin-associated human senescence program converges on the activation of placenta-specific gene PAPPA. Dev. Cell 59, 991–1009.e12 (2024).
Wu, Z., Ren, J. & Liu, G. H. Deciphering RNA m6A regulation in aging: perspectives on current advances and future directions. Aging Cell 22, e13972 (2023).
Wu, Z. et al. METTL3 counteracts premature aging via m6A-dependent stabilization of MIS12 mRNA. Nucleic Acids Res. 48, 11083–11096 (2020).
Wu, Z. et al. m6A epitranscriptomic regulation of tissue homeostasis during primate aging. Nat. Aging 3, 705–721 (2023).
Zhang, J. et al. Lamin A safeguards the m6A methylase METTL14 nuclear speckle reservoir to prevent cellular senescence. Aging Cell 19, e13215 (2020).
Min, K. W. et al. Profiling of m6A RNA modifications identified an age-associated regulation of AGO2 mRNA stability. Aging Cell 17, e12753 (2018).
Fu, Y. et al. Perturbation of METTL1-mediated tRNA N7-methylguanosine modification induces senescence and aging. Nat. Commun. 15, 5713 (2024).
Cai, D. & Han, J. J. Aging-associated lncRNAs are evolutionarily conserved and participate in NFκB signaling. Nat. Aging 1, 438–453 (2021).
Montes, M. et al. The long non-coding RNA MIR31HG regulates the senescence associated secretory phenotype. Nat. Commun. 12, 2459 (2021).
Zhang, X. et al. KCNQ1OT1 promotes genome-wide transposon repression by guiding RNA–DNA triplexes and HP1 binding. Nat. Cell Biol. 24, 1617–1629 (2022).
Faraonio, R. et al. A set of miRNAs participates in the cellular senescence program in human diploid fibroblasts. Cell Death Differ. 19, 713–721 (2012).
Freund, A., Laberge, R. M., Demaria, M. & Campisi, J. Lamin B1 loss is a senescence-associated biomarker. Mol. Biol. Cell 23, 2066–2075 (2012).
Jing, Y. et al. Single-nucleus profiling unveils a geroprotective role of the FOXO3 in primate skeletal muscle aging. Protein Cell 14, 497–512 (2023).
Zhang, H. et al. Protocols for the application of human embryonic stem cell-derived neurons for aging modeling and gene manipulation. STAR Protoc. 6, 103633 (2025).
Pienta, K. J., Getzenberg, R. H. & Coffey, D. S. Characterization of nuclear morphology and nuclear matrices in ageing human fibroblasts. Mech. Ageing Dev. 62, 13–24 (1992).
Kim, S. Y. et al. Senescence-related functional nuclear barrier by down-regulation of nucleo-cytoplasmic trafficking gene expression. Biochem. Biophys. Res. Commun. 391, 28–32 (2010).
Li, L. Z. et al. CRISPR-based screening identifies XPO7 as a positive regulator of senescence. Protein Cell 14, 623–628 (2023).
Buchwalter, A. & Hetzer, M. W. Nucleolar expansion and elevated protein translation in premature aging. Nat. Commun. 8, 328 (2017).
Li, H. Y. et al. CRISPR screening uncovers nucleolar RPL22 as a heterochromatin destabilizer and senescence driver. Nucleic Acids Res. 52, 11481–11499 (2024).
Pinho, M., Macedo, J. C., Logarinho, E. & Pereira, P. S. NOL12 repression induces nucleolar stress-driven cellular senescence and is associated with normative aging. Mol. Cell. Biol. 39, e00099-19 (2019).
Wang, M. et al. PML2-mediated thread-like nuclear bodies mark late senescence in Hutchinson–Gilford progeria syndrome. Aging Cell 19, e13147 (2020).
Wenger, B. et al. PML-nuclear bodies decrease with age and their stress response is impaired in aged individuals. BMC Geriatr. 14, 42 (2014).
López-Otín, C., Blasco, M. A., Partridge, L., Serrano, M. & Kroemer, G. Hallmarks of aging: an expanding universe. Cell 186, 243–278 (2023).
Liu, Y. et al. Age-related changes in the mitochondria of human mural granulosa cells. Hum. Reprod. 32, 2465–2473 (2017).
He, Y. et al. 4E-BP1 counteracts human mesenchymal stem cell senescence via maintaining mitochondrial homeostasis. Protein Cell 14, 202–216 (2023).
Wang, C. et al. MAVS antagonizes human stem cell senescence as a mitochondrial stabilizer. Research 6, 0192 (2023).
Yu, B. et al. Mitochondrial phosphatase PGAM5 modulates cellular senescence by regulating mitochondrial dynamics. Nat. Commun. 11, 2549 (2020).
Guo, X. et al. High-frequency and functional mitochondrial DNA mutations at the single-cell level. Proc. Natl Acad. Sci. USA 120, e2201518120 (2023).
Vandiver, A. R. et al. Nanopore sequencing identifies a higher frequency and expanded spectrum of mitochondrial DNA deletion mutations in human aging. Aging Cell 22, e13842 (2023).
Victorelli, S. et al. Apoptotic stress causes mtDNA release during senescence and drives the SASP. Nature 622, 627–636 (2023).
Andreux, P. A. et al. The mitophagy activator urolithin A is safe and induces a molecular signature of improved mitochondrial and cellular health in humans. Nat. Metab. 1, 595–603 (2019).
Fang, E. F. et al. NAD+ augmentation restores mitophagy and limits accelerated aging in Werner syndrome. Nat. Commun. 10, 5284 (2019).
Tan, J. X. & Finkel, T. Lysosomes in senescence and aging. EMBO Rep. 24, e57265 (2023).
Moreno-García, A., Kun, A., Calero, O., Medina, M. & Calero, M. An overview of the role of lipofuscin in age-related neurodegeneration. Front. Neurosci. 12, 464 (2018).
Gilissen, E. P. et al. A neuronal aging pattern unique to humans and common chimpanzees. Brain Struct. Funct. 221, 647–664 (2016).
Georgakopoulou, E. A. et al. Specific lipofuscin staining as a novel biomarker to detect replicative and stress-induced senescence. A method applicable in cryo-preserved and archival tissues. Aging 5, 37–50 (2013).
Wang, S. et al. Deciphering primate retinal aging at single-cell resolution. Protein Cell 12, 889–898 (2021).
Dimri, G. P. et al. A biomarker that identifies senescent human cells in culture and in aging skin in vivo. Proc. Natl Acad. Sci. USA 92, 9363–9367 (1995).
Lee, B. Y. et al. Senescence-associated beta-galactosidase is lysosomal beta-galactosidase. Aging Cell 5, 187–195 (2006).
Kurz, D. J., Decary, S., Hong, Y. & Erusalimsky, J. D. Senescence-associated β-galactosidase reflects an increase in lysosomal mass during replicative ageing of human endothelial cells. J. Cell Sci. 113, 3613–3622 (2000).
Ma, S. et al. Single-cell transcriptomic atlas of primate cardiopulmonary aging. Cell Res. 31, 415–432 (2021).
Kavanagh, K. et al. Biomarkers of senescence in non-human primate adipose depots relate to aging. Geroscience 43, 343–352 (2021).
Wang, M. et al. Single-nucleus transcriptomics decodes the link between aging and lumbar disc herniation. Protein Cell https://doi.org/10.1093/procel/pwaf025 (2025).
Roh, K. et al. Lysosomal control of senescence and inflammation through cholesterol partitioning. Nat. Metab. 5, 398–413 (2023).
Li, W. et al. Cellular senescence triggers intracellular acidification and lysosomal pH alkalinized via ATP6AP2 attenuation in breast cancer cells. Commun. Biol. 6, 1147 (2023).
Jin, J. et al. CISH impairs lysosomal function in activated T cells resulting in mitochondrial DNA release and inflammaging. Nat. Aging 3, 600–616 (2023).
Johmura, Y. et al. Senolysis by glutaminolysis inhibition ameliorates various age-associated disorders. Science 371, 265–270 (2021).
Xiao, F. H. et al. ETS1 acts as a regulator of human healthy aging via decreasing ribosomal activity. Sci. Adv. 8, eabf2017 (2022).
Lessard, F. et al. Senescence-associated ribosome biogenesis defects contributes to cell cycle arrest through the Rb pathway. Nat. Cell Biol. 20, 789–799 (2018).
Cheng, Y. et al. A non-canonical role for a small nucleolar RNA in ribosome biogenesis and senescence. Cell 187, 4770–4789.e23 (2024).
Geng, L. et al. Systematic profiling reveals betaine as an exercise mimetic for geroprotection. Cell https://doi.org/10.1016/j.cell.2025.06.001 (2025).
Payea, M. J. et al. Senescence suppresses the integrated stress response and activates a stress-remodeled secretory phenotype. Mol. Cell 84, 4454–4469.e7 (2024).
Fukumoto, H. et al. Beta-secretase activity increases with aging in human, monkey, and mouse brain. Am. J. Pathol. 164, 719–725 (2004).
Gaikwad, S. et al. Tau oligomer induced HMGB1 release contributes to cellular senescence and neuropathology linked to Alzheimer’s disease and frontotemporal dementia. Cell Rep. 36, 109419 (2021).
Uchihara, T. et al. Tau pathology in aged cynomolgus monkeys is progressive supranuclear palsy/corticobasal degeneration — but not Alzheimer disease-like — ultrastructural mapping of tau by EDX. Acta Neuropathol. Commun. 4, 118 (2016).
Bie, J. et al. PKM2 aggregation drives metabolism reprograming during aging process. Nat. Commun. 15, 5761 (2024).
Sabath, N. et al. Cellular proteostasis decline in human senescence. Proc. Natl Acad. Sci. USA 117, 31902–31913 (2020).
Lee, H. J. et al. Cold temperature extends longevity and prevents disease-related protein aggregation through PA28γ-induced proteasomes. Nat. Aging 3, 546–566 (2023).
Cheng, F. et al. Reducing oxidative protein folding alleviates senescence by minimizing ER-to-nucleus H2O2 release. EMBO Rep. 24, e56439 (2023).
Hayashi, T. et al. Endothelial cellular senescence is inhibited by nitric oxide: implications in atherosclerosis associated with menopause and diabetes. Proc. Natl Acad. Sci. USA 103, 17018–17023 (2006).
Li, M. et al. [Gly14]-Humanin ameliorates high glucose-induced endothelial senescence via SIRT6. Sci. Rep. 14, 30924 (2024).
Wu, Y. et al. Phosphoglycerate dehydrogenase activates PKM2 to phosphorylate histone H3T11 and attenuate cellular senescence. Nat. Commun. 14, 1323 (2023).
Han, X. et al. AMPK activation protects cells from oxidative stress-induced senescence via autophagic flux restoration and intracellular NAD+ elevation. Aging Cell 15, 416–427 (2016).
Carroll, B. et al. Persistent mTORC1 signaling in cell senescence results from defects in amino acid and growth factor sensing. J. Cell Biol. 216, 1949–1957 (2017).
Ionescu, R. B. et al. Increased cholesterol synthesis drives neurotoxicity in patient stem cell-derived model of multiple sclerosis. Cell Stem Cell 31, 1574–1590.e11 (2024).
Flor, A. C., Wolfgeher, D., Wu, D. & Kron, S. J. A signature of enhanced lipid metabolism, lipid peroxidation and aldehyde stress in therapy-induced senescence. Cell Death Discov. 3, 17075 (2017).
Haney, M. S. et al. APOE4/4 is linked to damaging lipid droplets in Alzheimer’s disease microglia. Nature 628, 154–161 (2024).
Shota, Y. et al. Mitochondrial fatty acid oxidation drives senescence. Sci. Adv. 10, eado5887 (2024).
Chen, W. et al. The SESAME complex regulates cell senescence through the generation of acetyl-CoA. Nat. Metab. 3, 983–1000 (2021).
Li, X. et al. Lipid metabolism dysfunction induced by age-dependent DNA methylation accelerates aging. Signal. Transduct. Target. Ther. 7, 162 (2022).
Garagnani, P. et al. Methylation of ELOVL2 gene as a new epigenetic marker of age. Aging Cell 11, 1132–1134 (2012).
Li, F. et al. Blocking methionine catabolism induces senescence and confers vulnerability to GSK3 inhibition in liver cancer. Nat. Cancer 5, 131–146 (2024).
Kang, J. et al. Depletion of SAM leading to loss of heterochromatin drives muscle stem cell ageing. Nat. Metab. 6, 153–168 (2024).
Shang, L. et al. S-adenosyl-l-methionine alleviates the senescence of MSCs through the PI3K/AKT/FOXO3a signaling pathway. Stem Cell 42, 475–490 (2024).
Ueno, D. et al. Spermidine improves angiogenic capacity of senescent endothelial cells, and enhances ischemia-induced neovascularization in aged mice. Sci. Rep. 13, 8338 (2023).
Eisenberg, T. et al. Induction of autophagy by spermidine promotes longevity. Nat. Cell Biol. 11, 1305–1314 (2009).
Unterluggauer, H. et al. Premature senescence of human endothelial cells induced by inhibition of glutaminase. Biogerontology 9, 247–259 (2008).
Zhang, Y. et al. Glutamine suppresses senescence and promotes autophagy through glycolysis inhibition-mediated AMPKα lactylation in intervertebral disc degeneration. Commun. Biol. 7, 325 (2024).
Pacifico, F. et al. Glutamine promotes escape from therapy-induced senescence in tumor cells. Aging 13, 20962–20991 (2021).
Yuan, X. et al. NAD+/NADH redox alterations reconfigure metabolism and rejuvenate senescent human mesenchymal stem cells in vitro. Commun. Biol. 3, 774 (2020).
Sanokawa-Akakura, R., Akakura, S. & Tabibzadeh, S. Replicative senescence in human fibroblasts is delayed by hydrogen sulfide in a NAMPT/SIRT1 dependent manner. PLoS ONE 11, e0164710 (2016).
Wiley, C. D. et al. Mitochondrial dysfunction induces senescence with a distinct secretory phenotype. Cell Metab. 23, 303–314 (2016).
Sun, C. et al. Re-equilibration of imbalanced NAD metabolism ameliorates the impact of telomere dysfunction. EMBO J. 39, e103420 (2020).
Nacarelli, T. et al. NAD+ metabolism governs the proinflammatory senescence-associated secretome. Nat. Cell Biol. 21, 397–407 (2019).
Wang, B., Han, J., Elisseeff, J. H. & Demaria, M. The senescence-associated secretory phenotype and its physiological and pathological implications. Nat. Rev. Mol. Cell Biol. 25, 958–978 (2024).
Wu, Z., Qu, J., Zhang, W. & Liu, G. H. Stress, epigenetics, and aging: unraveling the intricate crosstalk. Mol. Cell 84, 34–54 (2024).
Chen, Y. et al. Circadian factors CLOCK and BMAL1 promote nonhomologous end joining and antagonize cellular senescence. Life Med. 3, lnae006 (2024).
Taylor, R. N. et al. Interleukin-1β induces and accelerates human endometrial stromal cell senescence and impairs decidualization via the c-Jun N-terminal kinase pathway. Cell Death Discov. 10, 288 (2024).
Gulen, M. F. et al. cGAS-STING drives ageing-related inflammation and neurodegeneration. Nature 620, 374–380 (2023).
Lee, S. et al. Virus-induced senescence is a driver and therapeutic target in COVID-19. Nature 599, 283–289 (2021).
Schmitt, C. A. et al. COVID-19 and cellular senescence. Nat. Rev. Immunol. 23, 251–263 (2023).
Guo, Y. et al. Senescence-associated tissue microenvironment promotes colon cancer formation through the secretory factor GDF15. Aging Cell 18, e13013 (2019).
Acosta, J. C. et al. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat. Cell Biol. 15, 978–990 (2013).
Jin, H. J. et al. Senescence-associated MCP-1 secretion is dependent on a decline in BMI1 in human mesenchymal stromal cells. Antioxid. Redox Signal. 24, 471–485 (2016).
Xu, M. et al. JAK inhibition alleviates the cellular senescence-associated secretory phenotype and frailty in old age. Proc. Natl Acad. Sci. USA 112, E6301–E6310 (2015).
Acosta, J. C. et al. Chemokine signaling via the CXCR2 receptor reinforces senescence. Cell 133, 1006–1018 (2008).
Freund, A., Patil, C. K. & Campisi, J. p38MAPK is a novel DNA damage response-independent regulator of the senescence-associated secretory phenotype. EMBO J. 30, 1536–1548 (2011).
Amor, C. et al. Senolytic CAR T cells reverse senescence-associated pathologies. Nature 583, 127–132 (2020).
Suda, M. et al. Senolytic vaccination improves normal and pathological age-related phenotypes and increases lifespan in progeroid mice. Nat. Aging 1, 1117–1126 (2021).
Zhu, Y. et al. The Achilles’ heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell 14, 644–658 (2015).
Zhang, B. et al. SenoIndex: S100A8/S100A9 as a novel aging biomarker. Life Med. 2, lnad022 (2023).
Su, Y. et al. S100A13 promotes senescence-associated secretory phenotype and cellular senescence via modulation of non-classical secretion of IL-1α. Aging 11, 549–572 (2019).
Kang, H. T., Lee, K. B., Kim, S. Y., Choi, H. R. & Park, S. C. Autophagy impairment induces premature senescence in primary human fibroblasts. PLoS ONE 6, e23367 (2011).
Lehmann, B. D. et al. Senescence-associated exosome release from human prostate cancer cells. Cancer Res. 68, 7864–7871 (2008).
Liu, X. et al. Migrasomes trigger innate immune activation and mediate transmission of senescence signals across human cells. Life Med. 2, lnad050 (2023).
Segurado-Miravalles, G. et al. Assessment of the effect of 3% diclofenac sodium on photodamaged skin by means of reflectance confocal microscopy. Acta Derm. Venereol. 98, 963–969 (2018).
Montagna, W. & Carlisle, K. Structural changes in aging human skin. J. Invest. Dermatol. 73, 47–53 (1979).
Watt, F. M. & Fujiwara, H. Cell–extracellular matrix interactions in normal and diseased skin. Cold Spring Harb. Perspect. Biol. 3, a005124 (2011).
Liu, N. et al. Stem cell competition orchestrates skin homeostasis and ageing. Nature 568, 344–350 (2019).
Matsumura, H. et al. Hair follicle aging is driven by transepidermal elimination of stem cells via COL17A1 proteolysis. Science 351, aad4395 (2016).
Hasegawa, T. et al. Cytotoxic CD4+ T cells eliminate senescent cells by targeting cytomegalovirus antigen. Cell 186, 1417–1431.e20 (2023).
Xiao, X. et al. Identification of key circadian rhythm genes in skin aging based on bioinformatics and machine learning. Aging 15, 11672–11689 (2023).
Chiou, K. L. et al. Multiregion transcriptomic profiling of the primate brain reveals signatures of aging and the social environment. Nat. Neurosci. 25, 1714–1723 (2022).
Yu, Y. et al. A stress-induced miR-31-CLOCK-ERK pathway is a key driver and therapeutic target for skin aging. Nat. Aging 1, 795–809 (2021).
Sun, C. et al. Integrated analysis of facial microbiome and skin physio-optical properties unveils cutotype-dependent aging effects. Microbiome 12, 163 (2024).
Aging Biomarker Consortium. A framework of biomarkers for brain aging: a consensus statement by the Aging Biomarker Consortium. Life Med. 2, lnad017 (2023).
Groh, J. & Simons, M. White matter aging and its impact on brain function. Neuron 113, 127–139 (2025).
Vickery, S. et al. The uniqueness of human vulnerability to brain aging in great ape evolution. Sci. Adv. 10, eado2733 (2024).
Moguilner, S. et al. Brain clocks capture diversity and disparities in aging and dementia across geographically diverse populations. Nat. Med. 30, 3646–3657 (2024).
Oveisgharan, S. et al. The time course of motor and cognitive decline in older adults and their associations with brain pathologies: a multicohort study. Lancet Healthy Longev. 5, e336–e345 (2024).
Castner, S. A. et al. Longevity factor klotho enhances cognition in aged nonhuman primates. Nat. Aging 3, 931–937 (2023).
Wen, X. et al. Single-cell multiplex chromatin and RNA interactions in ageing human brain. Nature 628, 648–656 (2024).
Green, G. S. et al. Cellular communities reveal trajectories of brain ageing and Alzheimer’s disease. Nature 633, 634–645 (2024).
Herdy, J. R. et al. Increased post-mitotic senescence in aged human neurons is a pathological feature of Alzheimer’s disease. Cell Stem Cell 29, 1637–1652.e6 (2022).
Bae, T. et al. Analysis of somatic mutations in 131 human brains reveals aging-associated hypermutability. Science 377, 511–517 (2022).
Ning, C. et al. Epigenomic landscapes during prefrontal cortex development and aging in rhesus. Natl Sci. Rev. 11, nwae213 (2024).
Liu, S. et al. Annotation and cluster analysis of spatiotemporal- and sex-related lncRNA expression in rhesus macaque brain. Genome Res. 27, 1608–1620 (2017).
Li, D. et al. Aging-induced tRNA(Glu)-derived fragment impairs glutamate biosynthesis by targeting mitochondrial translation-dependent cristae organization. Cell Metab. 36, 1059–1075.e9 (2024).
Fan, Y. et al. Generic amyloid fibrillation of TMEM106B in patient with Parkinson’s disease dementia and normal elders. Cell Res. 32, 585–588 (2022).
Beckman, D. et al. Oligomeric Aβ in the monkey brain impacts synaptic integrity and induces accelerated cortical aging. Proc. Natl Acad. Sci. USA 116, 26239–26246 (2019).
Liu, W. S. et al. Plasma proteomics identify biomarkers and undulating changes of brain aging. Nat. Aging 5, 99–112 (2025).
Khalil, M. et al. Serum neurofilament light levels in normal aging and their association with morphologic brain changes. Nat. Commun. 11, 812 (2020).
Li, Y. et al. Aging-related NADPH diaphorase positive neurodegenerations in the sacral spinal cord of aged non-human primates. Sci. Rep. 14, 27168 (2024).
Steenman, M. & Lande, G. Cardiac aging and heart disease in humans. Biophys. Rev. 9, 131–137 (2017).
Aging Biomarker Consortium. A biomarker framework for cardiac aging: the Aging Biomarker Consortium consensus statement. Life Med. 2, lnad035 (2023).
Aging Biomarker Consortium. A framework of biomarkers for vascular aging: a consensus statement by the Aging Biomarker Consortium. Life Med. 2, lnad033 (2023).
Hastings, M. H. et al. Cardiac aging: from hallmarks to therapeutic opportunities. Cardiovasc. Res. https://doi.org/10.1093/cvr/cvae124 (2024).
Abdellatif, M., Rainer, P. P., Sedej, S. & Kroemer, G. Hallmarks of cardiovascular ageing. Nat. Rev. Cardiol. 20, 754–777 (2023).
Olivetti, G., Melissari, M., Capasso, J. M. & Anversa, P. Cardiomyopathy of the aging human heart. Myocyte loss and reactive cellular hypertrophy. Circ. Res. 68, 1560–1568 (1991).
Wang, M. et al. Aging increases aortic MMP-2 activity and angiotensin II in nonhuman primates. Hypertension 41, 1308–1316 (2003).
Yoshida, Y. et al. Alteration of cardiac performance and serum B-type natriuretic peptide level in healthy aging. J. Am. Coll. Cardiol. 74, 1789–1800 (2019).
de Lemos, J. A. et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA 304, 2503–2512 (2010).
Ding, Y. et al. Comprehensive human proteome profiles across a 50-year lifespan reveal aging trajectories and signatures. Cell https://doi.org/10.1016/j.cell.2025.06.047 (2025).
Sun, D. Y. et al. Pro-ferroptotic signaling promotes arterial aging via vascular smooth muscle cell senescence. Nat. Commun. 15, 1429 (2024).
Zhang, Y. et al. Sirtuin 2 deficiency aggravates ageing-induced vascular remodelling in humans and mice. Eur. Heart J. 44, 2746–2759 (2023).
Zhang, W. et al. A single-cell transcriptomic landscape of primate arterial aging. Nat. Commun. 11, 2202 (2020).
Gossner, J. & Nau, R. Geriatric chest imaging: when and how to image the elderly lung, age-related changes, and common pathologies. Radiol. Res. Pract. 2013, 584793 (2013).
Copley, S. J. et al. Effect of aging on lung structure in vivo: assessment with densitometric and fractal analysis of high-resolution computed tomography data. J. Thorac. Imaging 27, 366–371 (2012).
Baratella, E. et al. Aging-related findings of the respiratory system in chest imaging: pearls and pitfalls. Curr. Radiol. Rep. 11, 1–11 (2023).
Cho, S. J. & Stout-Delgado, H. W. Aging and lung disease. Annu. Rev. Physiol. 82, 433–459 (2020).
Janssens, J. P., Pache, J. C. & Nicod, L. P. Physiological changes in respiratory function associated with ageing. Eur. Respir. J. 13, 197–205 (1999).
Schneider, J. L. et al. The aging lung: physiology, disease, and immunity. Cell 184, 1990–2019 (2021).
Lee, S. et al. Molecular programs of fibrotic change in aging human lung. Nat. Commun. 12, 6309 (2021).
Jia, H. et al. A single-cell atlas of lung homeostasis reveals dynamic changes during development and aging. Commun. Biol. 7, 427 (2024).
Chow, R. D., Majety, M. & Chen, S. The aging transcriptome and cellular landscape of the human lung in relation to SARS-CoV-2. Nat. Commun. 12, 4 (2021).
Cogger, V. C. et al. Hepatic sinusoidal pseudocapillarization with aging in the non-human primate. Exp. Gerontol. 38, 1101–1107 (2003).
McLean, A. J. et al. Age-related pseudocapillarization of the human liver. J. Pathol. 200, 112–117 (2003).
Wynne, H. A. et al. The effect of age upon liver volume and apparent liver blood flow in healthy man. Hepatology 9, 297–301 (1989).
Moon, C. M., Kim, S. K., Heo, S. H. & Shin, S. S. Hemodynamic changes in the portal vein with age: evaluation using four-dimensional flow MRI. Sci. Rep. 13, 7397 (2023).
Aging Biomarker Consortium. A biomarker framework for liver aging: the Aging Biomarker Consortium consensus statement. Life Med. 3, lnae004 (2024).
Kudryavtsev, B. N., Kudryavtseva, M. V., Sakuta, G. A. & Stein, G. I. Human hepatocyte polyploidization kinetics in the course of life cycle. Virchows Arch. B Cell Pathol. Incl. Mol. Pathol. 64, 387–393 (1993).
Ogrodnik, M. et al. Cellular senescence drives age-dependent hepatic steatosis. Nat. Commun. 8, 15691 (2017).
Brazhnik, K. et al. Single-cell analysis reveals different age-related somatic mutation profiles between stem and differentiated cells in human liver. Sci. Adv. 6, eaax2659 (2020).
Bacalini, M. G. et al. Molecular aging of human liver: an epigenetic/transcriptomic signature. J. Gerontol. A Biol. Sci. Med. Sci. 74, 1–8 (2019).
Wiemann, S. U. et al. Hepatocyte telomere shortening and senescence are general markers of human liver cirrhosis. FASEB J. 16, 935–942 (2002).
Deng, D. et al. Aging-induced short-chain acyl-CoA dehydrogenase promotes age-related hepatic steatosis by suppressing lipophagy. Aging Cell 23, e14256 (2024).
Corton, J. C. et al. Determinants of gene expression in the human liver: impact of aging and sex on xenobiotic metabolism. Exp. Gerontol. 169, 111976 (2022).
Arif, M. et al. Data-driven transcriptomics analysis identifies PCSK9 as a novel key regulator in liver aging. Geroscience 45, 3059–3077 (2023).
Du, K. et al. Aging promotes metabolic dysfunction-associated steatotic liver disease by inducing ferroptotic stress. Nat. Aging 4, 949–968 (2024).
Li, J. et al. Determining a multimodal aging clock in a cohort of Chinese women. Med 4, 825–848.e13 (2023).
Tietz, N. W., Shuey, D. F. & Wekstein, D. R. Laboratory values in fit aging individuals — sexagenarians through centenarians. Clin. Chem. 38, 1167–1185 (1992).
Cui, Q. et al. Serum PCSK9 is associated with multiple metabolic factors in a large Han Chinese population. Atherosclerosis 213, 632–636 (2010).
Rezzani, R., Nardo, L., Favero, G., Peroni, M. & Rodella, L. F. Thymus and aging: morphological, radiological, and functional overview. Age 36, 313–351 (2014).
Mittelbrunn, M. & Kroemer, G. Hallmarks of T cell aging. Nat. Immunol. 22, 687–698 (2021).
Zago, M. A., Figueiredo, M. S., Covas, D. T. & Bottura, C. Aspects of splenic hypofunction in old age. Klin. Wochenschr. 63, 590–592 (1985).
Alex, L. et al. Microscopic study of human spleen in different age groups. Int. J. Med. Sci. 3, 1701–1706 (2017).
Turner, V. M. & Mabbott, N. A. Influence of ageing on the microarchitecture of the spleen and lymph nodes. Biogerontology 18, 723–738 (2017).
Murakami, G. & Taniguchi, I. Histologic heterogeneity and intranodal shunt flow in lymph nodes from elderly subjects: a cadaveric study. Ann. Surg. Oncol. 11, 279s–284s (2004).
Blebea, J. S. et al. Structural and functional imaging of normal bone marrow and evaluation of its age-related changes. Semin. Nucl. Med. 37, 185–194 (2007).
Stervbo, U. et al. Effects of aging on human leukocytes (part I): immunophenotyping of innate immune cells. Age 37, 92 (2015).
Mogilenko, D. A. et al. Comprehensive profiling of an aging immune system reveals clonal GZMK+ CD8+ T cells as conserved hallmark of inflammaging. Immunity 54, 99–115.e12 (2021).
Mogilenko, D. A., Shchukina, I. & Artyomov, M. N. Immune ageing at single-cell resolution. Nat. Rev. Immunol. 22, 484–498 (2022).
Chang, Y. et al. An updated immunosenescence exploration in healthy Chinese donors: circular elevated PD-1 on T cell and increased Ki67 on CD8+ T cell towards aging. Aging 16, 10985–10996 (2024).
Bohacova, P. et al. Multidimensional profiling of human T cells reveals high CD38 expression, marking recent thymic emigrants and age-related naive T cell remodeling. Immunity 57, 2362–2379.e10 (2024).
Terekhova, M. et al. Single-cell atlas of healthy human blood unveils age-related loss of NKG2C+GZMB−CD8+ memory T cells and accumulation of type 2 memory T cells. Immunity 56, 2836–2854.e9 (2023).
Luo, O. J. et al. Multidimensional single-cell analysis of human peripheral blood reveals characteristic features of the immune system landscape in aging and frailty. Nat. Aging 2, 348–364 (2022).
Filippov, I., Schauser, L. & Peterson, P. An integrated single-cell atlas of blood immune cells in aging. npj Aging 10, 59 (2024).
Nguyen, T. T. & Corvera, S. Adipose tissue as a linchpin of organismal ageing. Nat. Metab. 6, 793–807 (2024).
Porter, J. W. et al. Age, sex, and depot-specific differences in adipose-tissue estrogen receptors in individuals with obesity. Obesity 28, 1698–1707 (2020).
Mansoor, A. et al. Echocardiographic determination of epicardial adipose tissue in healthy bonnet macaques. Echocardiography 27, 180–185 (2010).
Cefalu, W. T. et al. Caloric restriction and cardiovascular aging in cynomolgus monkeys (Macaca fascicularis): metabolic, physiologic, and atherosclerotic measures from a 4-year intervention trial. J. Gerontol. A Biol. Sci. Med. Sci. 59, 1007–1014 (2004).
Zhang, Y. et al. Adipose tissue senescence: biological changes, hallmarks and therapeutic approaches. Mech. Ageing Dev. 222, 111988 (2024).
Saito, M. et al. High incidence of metabolically active brown adipose tissue in healthy adult humans: effects of cold exposure and adiposity. Diabetes 58, 1526–1531 (2009).
Wang, L. et al. Age and BMI have different effects on subcutaneous, visceral, liver, bone marrow, and muscle adiposity, as measured by CT and MRI. Obesity 32, 1339–1348 (2024).
Xu, P. et al. Integrated multi-omic analyses uncover the effects of aging on cell-type regulation in glucose-responsive tissues. Aging Cell 23, e14199 (2024).
Zhou, W. et al. High-resolution aging niche of human adipose tissues. Signal. Transduct. Target. Ther. 8, 105 (2023).
Sasaki, T. et al. Status and physiological significance of circulating adiponectin in the very old and centenarians: an observational study. eLife 12, e86309 (2023).
Pareja-Galeano, H. et al. Circulating leptin and adiponectin concentrations in healthy exceptional longevity. Mech. Ageing Dev. 162, 129–132 (2017).
Mitchell, W. K. et al. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front. Physiol. 3, 260 (2012).
Wilkinson, D. J., Piasecki, M. & Atherton, P. J. The age-related loss of skeletal muscle mass and function: measurement and physiology of muscle fibre atrophy and muscle fibre loss in humans. Ageing Res. Rev. 47, 123–132 (2018).
Granic, A., Suetterlin, K., Shavlakadze, T., Grounds, M. D. & Sayer, A. A. Hallmarks of ageing in human skeletal muscle and implications for understanding the pathophysiology of sarcopenia in women and men. Clin. Sci. 137, 1721–1751 (2023).
Zhao, Q. et al. SIRT5 safeguards against primate skeletal muscle ageing via desuccinylation of TBK1. Nat. Metab. 7, 556–573 (2025).
Huang, N. et al. A framework of biomarkers for skeletal muscle aging: a consensus statement by the Aging Biomarker Consortium. Life Med. 3, lnaf001 (2024).
Black, A. et al. A nonhuman primate model of age-related bone loss: a longitudinal study in male and premenopausal female rhesus monkeys. Bone 28, 295–302 (2001).
Colman, R. J., Lane, M. A., Binkley, N., Wegner, F. H. & Kemnitz, J. W. Skeletal effects of aging in male rhesus monkeys. Bone 24, 17–23 (1999).
Runolfsdottir, H. L., Sigurdsson, G., Franzson, L. & Indridason, O. S. Gender comparison of factors associated with age-related differences in bone mineral density. Arch. Osteoporos. 10, 214 (2015).
Aging Biomarker Consortium. A framework of biomarkers for skeletal aging: a consensus statement by the Aging Biomarker Consortium. Life Med. 2, lnad045 (2023).
Lotz, M. & Loeser, R. F. Effects of aging on articular cartilage homeostasis. Bone 51, 241–248 (2012).
Grote, C., Reinhardt, D., Zhang, M. & Wang, J. Regulatory mechanisms and clinical manifestations of musculoskeletal aging. J. Orthop. Res. 37, 1475–1488 (2019).
Burr, D. B. Changes in bone matrix properties with aging. Bone 120, 85–93 (2019).
Iijima, H. et al. Age-related matrix stiffening epigenetically regulates α-Klotho expression and compromises chondrocyte integrity. Nat. Commun. 14, 18 (2023).
Lai, Y. et al. Multimodal cell atlas of the ageing human skeletal muscle. Nature 629, 154–164 (2024).
Kedlian, V. R. et al. Human skeletal muscle aging atlas. Nat. Aging 4, 727–744 (2024).
Mi, B. et al. Ageing-related bone and immunity changes: insights into the complex interplay between the skeleton and the immune system. Bone Res. 12, 42 (2024).
Busse, B. et al. Decrease in the osteocyte lacunar density accompanied by hypermineralized lacunar occlusion reveals failure and delay of remodeling in aged human bone. Aging Cell 9, 1065–1075 (2010).
Chung, P. L. et al. Effect of age on regulation of human osteoclast differentiation. J. Cell. Biochem. 115, 1412–1419 (2014).
Pang, W. W. et al. Human bone marrow hematopoietic stem cells are increased in frequency and myeloid-biased with age. Proc. Natl Acad. Sci. USA 108, 20012–20017 (2011).
Barbero, A. et al. Age related changes in human articular chondrocyte yield, proliferation and post-expansion chondrogenic capacity. Osteoarthr. Cartil. 12, 476–484 (2004).
Zhang, X. et al. Characterization of cellular senescence in aging skeletal muscle. Nat. Aging 2, 601–615 (2022).
Jing, Y. et al. SESN1 is a FOXO3 effector that counteracts human skeletal muscle ageing. Cell Prolif. 56, e13455 (2023).
Janssens, G. E. et al. A conserved complex lipid signature marks human muscle aging and responds to short-term exercise. Nat. Aging 4, 681–693 (2024).
Fuerst, M. et al. Calcification of articular cartilage in human osteoarthritis. Arthritis Rheum. 60, 2694–2703 (2009).
Rex, N., Melk, A. & Schmitt, R. Cellular senescence and kidney aging. Clin. Sci. 137, 1805–1821 (2023).
Fang, Y. et al. Age-related GSK3β overexpression drives podocyte senescence and glomerular aging. J. Clin. Invest. 132, e141848 (2022).
Lee, H. J. et al. Marmoset as a model to study kidney changes associated with aging. J. Gerontol. A Biol. Sci. Med. Sci. 74, 315–324 (2019).
Fang, Y. et al. The ageing kidney: molecular mechanisms and clinical implications. Ageing Res. Rev. 63, 101151 (2020).
Schmitt, R. & Melk, A. Molecular mechanisms of renal aging. Kidney Int. 92, 569–579 (2017).
Xie, H. et al. Uremic toxin receptor AhR facilitates renal senescence and fibrosis via suppressing mitochondrial biogenesis. Adv. Sci. 11, e2402066 (2024).
Zhou, S. et al. Cannabinoid receptor 2 plays a central role in renal tubular mitochondrial dysfunction and kidney ageing. J. Cell. Mol. Med. 25, 8957–8972 (2021).
Luo, C. et al. Wnt9a promotes renal fibrosis by accelerating cellular senescence in tubular epithelial cells. J. Am. Soc. Nephrol. 29, 1238–1256 (2018).
Mylonas, K. J. et al. Cellular senescence inhibits renal regeneration after injury in mice, with senolytic treatment promoting repair. Sci. Transl. Med. 13, eabb0203 (2021).
Li, L. et al. Inhibition of ACSS2-mediated histone crotonylation alleviates kidney fibrosis via IL-1β-dependent macrophage activation and tubular cell senescence. Nat. Commun. 15, 3200 (2024).
Jiang, Q. et al. ZFYVE21 promotes endothelial nitric oxide signaling and vascular barrier function in the kidney during aging. Kidney Int. 106, 419–432 (2024).
Oh, H. S. et al. Organ aging signatures in the plasma proteome track health and disease. Nature 624, 164–172 (2023).
Yamazaki, Y. et al. Establishment of sandwich ELISA for soluble alpha-Klotho measurement: age-dependent change of soluble alpha-Klotho levels in healthy subjects. Biochem. Biophys. Res. Commun. 398, 513–518 (2010).
Perheentupa, A. & Huhtaniemi, I. Aging of the human ovary and testis. Mol. Cell. Endocrinol. 299, 2–13 (2009).
Wang, S., Ren, J., Jing, Y., Qu, J. & Liu, G. H. Perspectives on biomarkers of reproductive aging for fertility and beyond. Nat. Aging 4, 1697–1710 (2024).
Lu, H. et al. Aging hallmarks of the primate ovary revealed by spatiotemporal transcriptomics. Protein Cell 15, 364–384 (2024).
Yan, L. et al. Stem cell transplantation extends the reproductive life span of naturally aging cynomolgus monkeys. Cell Discov. 10, 111 (2024).
Zhou, C. et al. Single-cell atlas of human ovaries reveals the role of the pyroptotic macrophage in ovarian aging. Adv. Sci. 11, e2305175 (2024).
Jin, C. et al. Molecular and genetic insights into human ovarian aging from single-nuclei multi-omics analyses. Nat. Aging 5, 275–290 (2025).
Yang, Q. et al. NADase CD38 is a key determinant of ovarian aging. Nat. Aging 4, 110–128 (2024).
Huang, D. et al. A single-nucleus transcriptomic atlas of primate testicular aging reveals exhaustion of the spermatogonial stem cell reservoir and loss of Sertoli cell homeostasis. Protein Cell 14, 888–907 (2023).
Nie, X. et al. Single-cell analysis of human testis aging and correlation with elevated body mass index. Dev. Cell 57, 1160–1176.e5 (2022).
Deng, Z. et al. Targeting dysregulated phago-/auto-lysosomes in Sertoli cells to ameliorate late-onset hypogonadism. Nat. Aging 4, 647–663 (2024).
He, J. et al. Single-cell transcriptomics identifies senescence-associated secretory phenotype (SASP) features of testicular aging in human. Aging 16, 3350–3362 (2024).
Jiang, H. et al. Quantitative histological analysis and ultrastructure of the aging human testis. Int. Urol. Nephrol. 46, 879–885 (2014).
Huber, H. F., Gerow, K. G. & Nathanielsz, P. W. Walking speed as an aging biomarker in baboons (Papio hamadryas). J. Med. Primatol. 44, 373–380 (2015).
Legdeur, N. et al. Associations of brain pathology cognitive and physical markers with age in cognitively normal individuals aged 60–102 years. J. Gerontol. A Biol. Sci. Med. Sci. 75, 1609–1617 (2020).
Shively, C. A., Lacreuse, A., Frye, B. M., Rothwell, E. S. & Moro, M. Nonhuman primates at the intersection of aging biology, chronic disease, and health: an introduction to the American Journal of Primatology Special Issue on aging, cognitive decline, and neuropathology in nonhuman primates. Am. J. Primatol. 83, e23309 (2021).
Kim, S., Myers, L., Wyckoff, J., Cherry, K. E. & Jazwinski, S. M. The frailty index outperforms DNA methylation age and its derivatives as an indicator of biological age. Geroscience 39, 83–92 (2017).
Mamoshina, P. et al. Population specific biomarkers of human aging: a big data study using South Korean, Canadian, and Eastern European patient populations. J. Gerontol. A Biol. Sci. Med. Sci. 73, 1482–1490 (2018).
Kubota, K. et al. [Changes in the blood cell counts with aging]. Nihon Ronen Igakkai Zasshi 28, 509–514 (1991).
Videan, E. N., Fritz, J. & Murphy, J. Effects of aging on hematology and serum clinical chemistry in chimpanzees (Pan troglodytes). Am. J. Primatol. 70, 327–338 (2008).
Puzianowska-Kuźnicka, M. et al. Interleukin-6 and C-reactive protein, successful aging, and mortality: the PolSenior study. Immun. Ageing 13, 21 (2016).
Kaeser, S. A. et al. A neuronal blood marker is associated with mortality in old age. Nat. Aging 1, 218–225 (2021).
Tian, C. R., Qian, L., Shen, X. Z., Li, J. J. & Wen, J. T. Distribution of serum total protein in elderly Chinese. PLoS ONE 9, e101242 (2014).
Semba, R. D. et al. Plasma klotho and mortality risk in older community-dwelling adults. J. Gerontol. A Biol. Sci. Med. Sci. 66, 794–800 (2011).
Liu, Z. et al. Cross-species metabolomic analysis identifies uridine as a potent regeneration promoting factor. Cell Discov. 8, 6 (2022).
Singh, P. et al. Taurine deficiency as a driver of aging. Science 380, eabn9257 (2023).
Shi, F. et al. Oxidative damage of DNA, RNA and their metabolites in leukocytes, plasma and urine of Macaca mulatta: 8-oxoguanosine in urine is a useful marker for aging. Free Radic. Res. 46, 1093–1098 (2012).
Gan, W. et al. Urinary 8-oxo-7,8-dihydroguanosine as a potential biomarker of aging. Front. Aging Neurosci. 10, 34 (2018).
Horvath, S. & Raj, K. DNA methylation-based biomarkers and the epigenetic clock theory of ageing. Nat. Rev. Genet. 19, 371–384 (2018).
Haghani, A. et al. DNA methylation networks underlying mammalian traits. Science 381, eabq5693 (2023).
Levine, M. E. et al. An epigenetic biomarker of aging for lifespan and healthspan. Aging 10, 573–591 (2018).
Horvath, S. et al. DNA methylation age analysis of rapamycin in common marmosets. Geroscience 43, 2413–2425 (2021).
Chen, W. et al. Three-dimensional human facial morphologies as robust aging markers. Cell Res. 25, 574–587 (2015).
Xia, X. et al. Three-dimensional facial-image analysis to predict heterogeneity of the human ageing rate and the impact of lifestyle. Nat. Metab. 2, 946–957 (2020).
Zhavoronkov, A., Kochetov, K., Diamandis, P. & Mitina, M. PsychoAge and SubjAge: development of deep markers of psychological and subjective age using artificial intelligence. Aging 12, 23548–23577 (2020).
Ren, J. et al. The Aging Biomarker Consortium represents a new era for aging research in China. Nat. Med. 29, 2162–2165 (2023).
Franceschi, C. et al. The continuum of aging and age-related diseases: common mechanisms but different rates. Front. Med. 5, 61 (2018).
Ruggiero, A. D. et al. Long-term dasatinib plus quercetin effects on aging outcomes and inflammation in nonhuman primates: implications for senolytic clinical trial design. Geroscience 45, 2785–2803 (2023).
Hickson, L. J. et al. Senolytics decrease senescent cells in humans: preliminary report from a clinical trial of dasatinib plus quercetin in individuals with diabetic kidney disease. eBioMedicine 47, 446–456 (2019).
Millar, C. L. et al. A pilot study of senolytics to improve cognition and mobility in older adults at risk for Alzheimer’s disease. eBioMedicine 113, 105612 (2025).
Lei, J. et al. Senescence-resistant human mesenchymal progenitor cells counter aging in primates. Cell https://doi.org/10.1016/j.cell.2025.05.021 (2025).
Hao, Y. et al. Extracellular vesicles from antler blastema progenitor cells reverse bone loss and mitigate aging-related phenotypes in mice and macaques. Nat. Aging https://doi.org/10.1038/s43587-025-00918-x (2025).
Acknowledgements
The authors thank L. Bai, J. Lu, J. Chen and J. Li for their administrative and technical support, and Y. Yang and S. Luo for their assistance with literature collection. This work was supported by the National Natural Science Foundation of China (82488301, 82125011 and 82361148131), the National Key Research and Development Program of China (2020YFA0804000, 2022YFA1103700 and 2022YFA1103800), Non-Communicable Chronic Diseases-National Science and Technology Major Project (2024ZD0530400), the National Natural Science Foundation of China (92168201, 82330044, 32341001 and 32121001), the Program of the Beijing Natural Science Foundation (JQ24044, Z240018 and F251011), CAS Project for Young Scientists in Basic Research (YSBR-076 and YSBR-012), the Strategic Priority Research Program of the Chinese Academy of Sciences (XDA0460403), New Cornerstone Science Foundation through the XPLORER PRIZE (2021-1045), Young Elite Scientists Sponsorship Program by CAST (2023QNRC001) and Tang Aoqing Scholar Program of Jilin University.
Author information
Authors and Affiliations
Consortia
Contributions
Z.W., J.Q., W.Z. and G.-H.L. contributed equally to researching data for the article, discussion of content, writing and reviewing and/or editing of the manuscript. The members of the Aging Biomarker Consortium contributed to the discussion of content and to reviewing and/or editing of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Molecular Cell Biology thanks Vijay Yadav and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, Z., Qu, J., Zhang, W. et al. Biomarkers of ageing of humans and non-human primates. Nat Rev Mol Cell Biol 26, 826–847 (2025). https://doi.org/10.1038/s41580-025-00883-8
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41580-025-00883-8