Abstract
Long coronavirus disease (COVID) — commonly defined as symptoms and/or long-term effects that persist for at least 3 months after acute infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and cannot be explained by an alternative diagnosis — is a complex, multifaceted and heterogeneous disease that affects many organ systems, including the kidney. COVID-19 can cause acute kidney injury, and several studies have reported an increased risk of chronic kidney disease (CKD) following COVID-19, suggesting that CKD can be a manifestation of long COVID. Furthermore, patients with CKD are at an increased risk of severe COVID-19 and of long COVID. COVID-19 has also been associated with the development of COVID-19-associated nephropathy, which is a collapsing form of focal segmental glomerulosclerosis, and an increased incidence of new-onset vasculitis. Some early reports described associations of COVID-19 and/or SARS-CoV-2 vaccines with relapse or new-onset of other glomerular diseases, but this link was not confirmed in large population-based studies. SARS-CoV-2 vaccination reduces the risk of COVID-19 and long COVID and is particularly important for protecting vulnerable populations such as patients with CKD. Structured long-term follow-up of patients with COVID-19 and post-infectious sequelae is needed to provide further insight into the trajectory of long COVID and enable identification of those at risk of CKD.
Key points
-
Long coronavirus disease (COVID) is commonly defined as symptoms or long-term effects that persist for at least 3 months after acute infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and cannot be explained by an alternative diagnosis; this disorder can affect many organ systems, including the kidney.
-
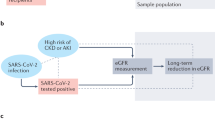
Pathophysiological mechanisms that underlie the high risk of acute kidney injury in patients with COVID-19 might also contribute to the development of chronic kidney disease (CKD) as one of the manifestations of long COVID.
-
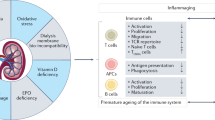
Patients with CKD are at an increased risk of SARS-CoV-2 infection and severe COVID-19 outcomes and might also be at increased risk of long COVID.
-
COVID-19 is associated with COVID-associated nephropathy, which is a rare but severe kidney disease; other relapsing or new-onset glomerular diseases have not been consistently associated with COVID-19, and there is also no proven causative association with SARS-CoV-2 vaccines.
-
SARS-CoV vaccines are safe and efficacious in patients with CKD and are associated with a reduced risk of long COVID.
-
Structured long-term follow-up of patients with COVID-19 is required to provide further insight into long COVID and enable the identification of patients who are at risk of the development or progression of CKD to facilitate timely intervention.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
A Long COVID Definition: A Chronic, Systemic Disease State with Profound Consequences. (National Academies Press, 2024). https://doi.org/10.17226/27768.
Greenhalgh, T., Sivan, M., Perlowski, A. & Nikolich, J. Ž Long COVID: a clinical update. Lancet 404, 707–724 (2024).
Ely, E. W., Brown, L. M., Fineberg, H. V. & National Academies of Sciences, Engineering, and Medicine Committee on Examining the Working Definition for Long Covid Long Covid defined. N. Engl. J. Med. 391, 1746–1753 (2024).
Coste, J. et al. Difference in long COVID prevalence due to different definitions and long COVID related risk factors. Eur. J. Public. Health 34, ckae144.811 (2024).
Chou, R. et al. Long COVID definitions and models of care: a scoping review. Ann. Intern. Med. 177, 929–940 (2024).
Al-Aly, Z. et al. Long COVID science, research and policy. Nat. Med. 30, 2148–2164 (2024).
Jeffrey, K. et al. Prevalence and risk factors for long COVID among adults in Scotland using electronic health records: a national, retrospective, observational cohort study. EClinicalMedicine 71, 102590 (2024).
Hastie, C. E. et al. True prevalence of long-COVID in a nationwide, population cohort study. Nat. Commun. 14, 7892 (2023).
Ballering, A. V., van Zon, S. K. R., Olde Hartman, T. C., Rosmalen, J. G. M. & Lifelines Corona Research Initiative Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet 400, 452–461 (2022).
Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK — Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/2february2023.
Ll, O. et al. The prevalence and long-term health effects of long Covid among hospitalised and non-hospitalised populations: a systematic review and meta-analysis. EClinicalMedicine 55, 101762 (2022).
Xie, Y., Choi, T. & Al-Aly, Z. Long-term outcomes following hospital admission for COVID-19 versus seasonal influenza: a cohort study. Lancet Infect. Dis. 24, 239–255 (2024).
Diexer, S. et al. Association between virus variants, vaccination, previous infections, and post-COVID-19 risk. Int. J. Infect. Dis. 136, 14–21 (2023).
Agergaard, J., Gunst, J. D., Schiøttz-Christensen, B., Østergaard, L. & Wejse, C. Long-term prognosis at 1.5 years after infection with wild-type strain of SARS-CoV-2 and Alpha, Delta, as well as Omicron variants. Int. J. Infect. Dis. 137, 126–133 (2023).
Al-Aly, Z., Bowe, B. & Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med. 28, 1461–1467 (2022).
ERA-EDTA Council & ERACODA Working Group Chronic kidney disease is a key risk factor for severe COVID-19: a call to action by the ERA-EDTA. Nephrol. Dial. Transplant. 36, 87–94 (2021).
Huang, C. et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 401, e21–e33 (2023).
Arias-Cabrales, C. et al. Short- and long-term outcomes after non-severe acute kidney injury. Clin. Exp. Nephrol. 22, 61–67 (2018).
Salgueira, M. et al. Characterization of hospitalized patients with acute kidney injury associated with COVID-19 in Spain: renal replacement therapy and mortality. FRA-COVID SEN registry data. Nefrologia 44, 527–539 (2024).
Al-Aly, Z., Xie, Y. & Bowe, B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 594, 259–264 (2021).
Chan, L. et al. AKI in hospitalized patients with COVID-19. J. Am. Soc. Nephrol. 32, 151–160 (2021).
Matsumoto, K. & Prowle, J. R. COVID-19-associated AKI. Curr. Opin. Crit. Care 28, 630–637 (2022).
Pan, X. et al. Identification of a potential mechanism of acute kidney injury during the COVID-19 outbreak: a study based on single-cell transcriptome analysis. Intensive Care Med. 46, 1114–1116 (2020).
Joseph, A., Zafrani, L., Mabrouki, A., Azoulay, E. & Darmon, M. Acute kidney injury in patients with SARS-CoV-2 infection. Ann. Intensive Care 10, 117 (2020).
Wang, F. et al. Highly pathogenic coronaviruses and the kidney. Biomed. Pharmacother. 156, 113807 (2022).
Eckerle, I., Müller, M. A., Kallies, S., Gotthardt, D. N. & Drosten, C. In-vitro renal epithelial cell infection reveals a viral kidney tropism as a potential mechanism for acute renal failure during Middle East respiratory syndrome (MERS) coronavirus infection. Virol. J. 10, 359 (2013).
Batlle, D. et al. Acute kidney injury in COVID-19: emerging evidence of a distinct pathophysiology. J. Am. Soc. Nephrol. 31, 1380–1383 (2020).
Soler, M. J. & Batlle, D. COVID-19 and its impact on the kidney and the nephrology community. Clin. Kidney J. 14, i1–i5 (2021).
Jansen, J. et al. SARS-CoV-2 infects the human kidney and drives fibrosis in kidney organoids. Cell Stem Cell 29, 217–231.e8 (2022).
Puelles, V. G. et al. Multiorgan and renal tropism of SARS-CoV-2. N. Engl. J. Med. 383, 590–592 (2020).
Cassol, C. A., Gokden, N., Larsen, C. P. & Bourne, T. D. Appearances can be deceiving — viral-like inclusions in COVID-19 negative renal biopsies by electron microscopy. Kidney360 1, 824–828 (2020).
Bärreiter, V. A. & Meister, T. L. Renal implications of coronavirus disease 2019: insights into viral tropism and clinical outcomes. Curr. Opin. Microbiol. 79, 102475 (2024).
Bowe, B., Xie, Y., Xu, E. & Al-Aly, Z. Kidney outcomes in long COVID. J. Am. Soc. Nephrol. 32, 2851–2862 (2021).
Atiquzzaman, M. et al. Long-term effect of COVID-19 infection on kidney function among COVID-19 patients followed in post-COVID-19 recovery clinics in British Columbia, Canada. Nephrol. Dial. Transplant. 38, 2816–2825 (2023).
Schmidt-Lauber, C. et al. Kidney outcome after mild to moderate COVID-19. Nephrol. Dial. Transplant. 38, 2031–2040 (2023).
Mehrotra-Varma, S. et al. Patients with type 1 diabetes are at elevated risk of developing new hypertension, chronic kidney disease and diabetic ketoacidosis after COVID-19: up to 40 months’ follow-up. Diabetes Obes. Metab. 26, 5368–5375 (2024).
Xie, Y. & Al-Aly, Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 10, 311–321 (2022).
Zhang, V., Fisher, M., Hou, W., Zhang, L. & Duong, T. Q. Incidence of new-onset hypertension post-COVID-19: comparison with influenza. Hypertension 80, 2135–2148 (2023).
Xie, Y., Xu, E., Bowe, B. & Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 28, 583–590 (2022).
Tsampasian, V. et al. Cardiovascular disease as part of Long COVID: a systematic review. Eur. J. Prev. Cardiol. 32, 485–498 (2025).
Salah, H. M. et al. Post-recovery COVID-19 and incident heart failure in the National COVID cohort collaborative (N3C) study. Nat. Commun. 13, 4117 (2022).
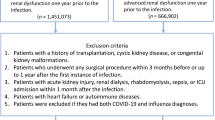
Aklilu, A. M. et al. COVID-19-associated acute kidney injury and longitudinal kidney outcomes. JAMA Intern. Med. 184, 414–423 (2024).
Mahalingasivam, V. et al. Kidney function decline after COVID-19 infection. JAMA Netw. Open 7, e2450014 (2024).
Li, L. et al. Kidney function following COVID-19 in children and adolescents. JAMA Netw. Open 8, e254129 (2025).
Chen, I.-W. et al. Association between COVID-19 and the development of chronic kidney disease in patients without initial acute kidney injury. Sci. Rep. 15, 10924 (2025).
Braun, F. et al. SARS-CoV-2 renal tropism associates with acute kidney injury. Lancet 396, 597–598 (2020).
Rafiee, M. J. & Friedrich, M. G. MRI of cardiac involvement in COVID-19. Br. J. Radiol. 97, 1367–1377 (2024).
McGroder, C. F. et al. Pulmonary fibrosis 4 months after COVID-19 is associated with severity of illness and blood leucocyte telomere length. Thorax 76, 1242–1245 (2021).
George, P. M., Wells, A. U. & Jenkins, R. G. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir. Med. 8, 807–815 (2020).
Bailey, J. I. et al. Profibrotic monocyte-derived alveolar macrophages are expanded in patients with persistent respiratory symptoms and radiographic abnormalities after COVID-19. Nat. Immunol. 25, 2097–2109 (2024).
Xu, S.-W., Ilyas, I. & Weng, J.-P. Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies. Acta Pharmacol. Sin. 44, 695–709 (2023).
Yilmaz, M. I. et al. The determinants of endothelial dysfunction in CKD: oxidative stress and asymmetric dimethylarginine. Am. J. Kidney Dis. 47, 42–50 (2006).
Chiang, K. C., Imig, J. D., Kalantar-Zadeh, K. & Gupta, A. Kidney in the net of acute and long-haul coronavirus disease 2019: a potential role for lipid mediators in causing renal injury and fibrosis. Curr. Opin. Nephrol. Hypertens. 31, 36–46 (2022).
Alexander, M. P. et al. Acute kidney injury in severe COVID-19 has similarities to sepsis-associated kidney injury: a multi-omics study. Mayo Clin. Proc. 96, 2561–2575 (2021).
Poyatos, P. et al. Endothelial dysfunction and cardiovascular risk in post-COVID-19 patients after 6- and 12-months SARS-CoV-2 infection. Infection 52, 1269–1285 (2024).
Kuchler, T. et al. Persistent endothelial dysfunction in post-COVID-19 syndrome and its associations with symptom severity and chronic inflammation. Angiogenesis 26, 547–563 (2023).
Forte, E. Abnormal complement activation is a sign of long COVID. Nat. Cardiovasc. Res. 3, 95 (2024).
Cervia-Hasler, C. et al. Persistent complement dysregulation with signs of thromboinflammation in active long Covid. Science 383, eadg7942 (2024).
Lee, J. D. & Woodruff, T. M. Complement(ing) long-COVID thromboinflammation and pathogenesis. Trends Immunol. 45, 397–399 (2024).
Hawley, H. B. Long COVID: clinical findings, pathology, and endothelial molecular mechanisms. Am. J. Med. 138, 91–97 (2025).
Baillie, K. et al. Complement dysregulation is a prevalent and therapeutically amenable feature of long COVID. Med. N. Y. N. 5, 239–253.e5 (2024).
Bumiller-Bini, V. et al. MASPs at the crossroad between the complement and the coagulation cascades — the case for COVID-19. Genet. Mol. Biol. 44, e20200199 (2021).
Khorashadi, M., Beunders, R., Pickkers, P. & Legrand, M. Proenkephalin: a new biomarker for glomerular filtration rate and acute kidney injury. Nephron 144, 655–661 (2020).
Wang, J. et al. Pulmonary and renal long COVID at two-year revisit. iScience 27, 110344 (2024).
Yin, K. et al. Long COVID manifests with T cell dysregulation, inflammation and an uncoordinated adaptive immune response to SARS-CoV-2. Nat. Immunol. 25, 218–225 (2024).
Klein, J. et al. Distinguishing features of long COVID identified through immune profiling. Nature 623, 139–148 (2023).
Glynne, P., Tahmasebi, N., Gant, V. & Gupta, R. Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines. J. Investig. Med. 70, 61–67 (2022).
Davis, H. E., McCorkell, L., Vogel, J. M. & Topol, E. J. Long COVID: major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 21, 133–146 (2023).
Bellinvia, S. et al. The unleashing of the immune system in COVID-19 and sepsis: the calm before the storm? Inflamm. Res. 69, 757–763 (2020).
Cao, M., Wang, G. & Xie, J. Immune dysregulation in sepsis: experiences, lessons and perspectives. Cell Death Discov. 9, 465 (2023).
Karakike, E. et al. Coronavirus disease 2019 as cause of viral sepsis: a systematic review and meta-analysis. Crit. Care Med. 49, 2042–2057 (2021).
de Araújo, G. C., Pardini, A. & Lima, C. The impact of comorbidities and COVID-19 on the evolution of community onset sepsis. Sci. Rep. 13, 10589 (2023).
Laterre, P. F. et al. Association of interleukin 7 immunotherapy with lymphocyte counts among patients with severe coronavirus disease 2019 (COVID-19). JAMA Netw. Open 3, e2016485 (2020).
Monneret, G. et al. Immune monitoring of interleukin-7 compassionate use in a critically ill COVID-19 patient. Cell. Mol. Immunol. 17, 1001–1003 (2020).
Bidar, F. et al. Recombinant human interleukin-7 reverses T cell exhaustion ex vivo in critically ill COVID-19 patients. Ann. Intensive Care 12, 21 (2022).
Syed-Ahmed, M. & Narayanan, M. Immune dysfunction and risk of infection in chronic kidney disease. Adv. Chronic Kidney Dis. 26, 8–15 (2019).
Tecklenborg, J., Clayton, D., Siebert, S. & Coley, S. M. The role of the immune system in kidney disease. Clin. Exp. Immunol. 192, 142–150 (2018).
Kreutmair, S. et al. Preexisting comorbidities shape the immune response associated with severe COVID-19. J. Allergy Clin. Immunol. 150, 312–324 (2022).
DiIorio, M. et al. Prolonged COVID-19 symptom duration in people with systemic autoimmune rheumatic diseases: results from the COVID-19 global rheumatology alliance vaccine survey. RMD Open. 8, e002587 (2022).
Teles, M. S. et al. Prevalence and risk factors of postacute sequelae of COVID-19 in adults with systemic autoimmune rheumatic diseases. J. Rheumatol. 51, 928–933 (2024).
Tesch, F. et al. Incident autoimmune diseases in association with SARS-CoV-2 infection: a matched cohort study. Clin. Rheumatol. 42, 2905–2914 (2023).
Chang, R. et al. Risk of autoimmune diseases in patients with COVID-19: a retrospective cohort study. EClinicalMedicine 56, 101783 (2023).
Heo, Y.-W., Jeon, J. J., Ha, M. C., Kim, Y. H. & Lee, S. Long-term risk of autoimmune and autoinflammatory connective tissue disorders following COVID-19. JAMA Dermatol. 160, 1278–1287 (2024).
Filev, R. et al. Post-acute sequelae of SARS-CoV-2 infection (PASC) for patients-3-year follow-up of patients with chronic kidney disease. Biomedicines 12, 1259 (2024).
Zhao, X. et al. Prevalence and risk factors of long COVID among maintenance hemodialysis patients post SARS-CoV-2 infection: a one-year follow-up study in China. J. Med. Virol. 96, e29932 (2024).
Amorim, C. E. N. et al. Long COVID among kidney transplant recipients appears to be attenuated during the omicron predominance. Transplantation 108, 963–969 (2024).
Bouwmans, P. et al. Post COVID-19 condition imposes significant burden in patients with advanced chronic kidney disease: a nested case-control study. Int. J. Infect. Dis. 142, 106990 (2024).
Bruchfeld, A. The COVID-19 pandemic: consequences for nephrology. Nat. Rev. Nephrol. 17, 81–82 (2021).
Tsampasian, V. et al. Risk factors associated with post-COVID-19 condition: a systematic review and meta-analysis. JAMA Intern. Med. 183, 566–580 (2023).
Wang, H.-I. et al. Prevalence, risk factors and characterisation of individuals with long COVID using electronic health records in over 1.5 million COVID cases in England. J. Infect. 89, 106235 (2024).
Català, M. et al. The effectiveness of COVID-19 vaccines to prevent long COVID symptoms: staggered cohort study of data from the UK, Spain, and Estonia. Lancet Respir. Med. 12, 225–236 (2024).
Tubiana, S. et al. Long-term health outcomes following hospitalisation for COVID-19: a 30- month cohort analysis. Infect. Dis. 57, 433–443 (2025).
Lu, J. Y. et al. Long term outcomes of patients with chronic kidney disease after COVID-19 in an urban population in the Bronx. Sci. Rep. 15, 6119 (2025).
Atiquzzaman, M. et al. COVID-19 infection and the progression of kidney disease in British Columbia, Canada. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfaf040 (2025).
Lambourg, E. J. et al. Cardiovascular outcomes in patients with chronic kidney disease and COVID-19: a multi-regional data-linkage study. Eur. Respir. J. 60, 2103168 (2022).
Choi, Y. J. et al. Effectiveness of antiviral therapy on long COVID: a systematic review and meta-analysis. J. Clin. Med. 12, 7375 (2023).
Cheng, M. et al. Remdesivir in patients with severe kidney dysfunction: a secondary analysis of the CATCO randomized trial. JAMA Netw. Open. 5, e2229236 (2022).
Cheng, F. W. T. et al. Effectiveness of molnupiravir and nirmatrelvir-ritonavir in CKD patients with COVID-19. Kidney Int. Rep. 9, 1244–1253 (2024).
Chen, X. et al. Efficacy and safety of nirmatrelvir/ritonavir in severe hospitalized patients with COVID-19 and in patients at high risk for progression to critical illness: a real-world study. J. Intensive Care Med. 39, 742–750 (2024).
Chan, G. C. K. et al. Safety profile and clinical and virological outcomes of nirmatrelvir-ritonavir treatment in patients with advanced chronic kidney disease and coronavirus disease 2019. Clin. Infect. Dis. 77, 1406–1412 (2023).
Hiremath, S. et al. Early experience with modified dose nirmatrelvir/ritonavir in dialysis patients with coronavirus disease 2019. Clin. J. Am. Soc. Nephrol. 18, 485–490 (2023).
Chu, W. M. et al. Comparison of safety and efficacy between nirmatrelvir-ritonavir and molnupiravir in the treatment of COVID-19 infection in patients with advanced kidney disease: a retrospective observational study. EClinicalMedicine 72, 102620 (2024).
Akilesh, S. et al. Multicenter clinicopathologic correlation of kidney biopsies performed in COVID-19 patients presenting with acute kidney injury or proteinuria. Am. J. Kidney Dis. 77, 82–93.e1 (2021).
Vinayagam, S. & Sattu, K. SARS-CoV-2 and coagulation disorders in different organs. Life Sci. 260, 118431 (2020).
Sharma, P. et al. COVID-19-associated kidney injury: a case series of kidney biopsy findings. J. Am. Soc. Nephrol. 31, 1948–1958 (2020).
Golmai, P. et al. Histopathologic and ultrastructural findings in postmortem kidney biopsy material in 12 patients with AKI and COVID-19. J. Am. Soc. Nephrol. 31, 1944–1947 (2020).
Connors, J. M. & Levy, J. H. COVID-19 and its implications for thrombosis and anticoagulation. Blood 135, 2033–2040 (2020).
Pfister, F. et al. Complement activation in kidneys of patients with COVID-19. Front. Immunol. 11, 594849 (2020).
Perico, L. et al. Immunity, endothelial injury and complement-induced coagulopathy in COVID-19. Nat. Rev. Nephrol. 17, 46–64 (2021).
Av, W., J, C. L. & Ca, R. Human IgG and IgA responses to COVID-19 mRNA vaccines. PLoS ONE 16, e0249499 (2021).
Sahin, U. et al. COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell responses. Nature 586, 594–599 (2020).
Ooi, J. D., Kitching, A. R. & Holdsworth, S. R. Review: T helper 17 cells: their role in glomerulonephritis. Nephrol. Carlton Vic. 15, 513–521 (2010).
Vojdani, A., Vojdani, E. & Kharrazian, D. Reaction of human monoclonal antibodies to SARS-CoV-2 proteins with tissue antigens: implications for autoimmune diseases. Front. Immunol. 11, 617089 (2020).
Li, N. L., Coates, P. T. & Rovin, B. H. COVID-19 vaccination followed by activation of glomerular diseases: does association equal causation? Kidney Int. 100, 959–965 (2021).
Geetha, D. et al. Impact of the COVID-19 pandemic on the kidney community: lessons learned and future directions. Nat. Rev. Nephrol. 18, 724–737 (2022).
Gauckler, P. et al. COVID-19 outcomes in patients with a history of immune-mediated glomerular diseases. Front. Immunol. 14, 1228457 (2023).
Waldman, M. et al. Results from the IRoc-GN international registry of patients with COVID-19 and glomerular disease suggest close monitoring. Kidney Int. 99, 227–237 (2021).
Waldman, M. et al. COVID-19 in patients with glomerular disease: follow-up results from the IRoc-GN international registry. Kidney360 3, 293–306 (2022).
Strangfeld, A. et al. Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 global rheumatology alliance physician-reported registry. Ann. Rheum. Dis. 80, 930–942 (2021).
Antovic, A. et al. Risks and treatment related aspects of COVID-19 infection in patients with ANCA-associated vasculitis. Scand. J. Rheumatol. 52, 418–423 (2023).
Cheng, Y. et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 97, 829–838 (2020).
Kim, H. W. et al. Glomerulonephritis following COVID-19 infection or vaccination: a multicenter study in South Korea. Kidney Res. Clin. Pract. 43, 165–176 (2024).
Sethi, S., D’Costa, M. R., Hermann, S. M., Nasr, S. H. & Fervenza, F. C. Immune-complex glomerulonephritis after COVID-19 infection. Kidney Int. Rep. 6, 1170–1173 (2021).
Kudose, S. et al. Kidney biopsy findings in patients with COVID-19. J. Am. Soc. Nephrol. 31, 1959–1968 (2020).
Nasr, S. H. et al. Kidney biopsy findings in patients with COVID-19, kidney injury, and proteinuria. Am. J. Kidney Dis. 77, 465–468 (2021).
Volbeda, M. et al. Acute and chronic histopathological findings in renal biopsies in COVID-19. Clin. Exp. Med. 23, 1003–1014 (2023).
Shetty, A. A. et al. COVID-19-associated glomerular disease. J. Am. Soc. Nephrol. 32, 33–40 (2021).
de Las Mercedes Noriega, M. et al. Kidney biopsy findings in patients with SARS-CoV-2 infection or after COVID-19 vaccination. Clin. J. Am. Soc. Nephrol. 18, 613–625 (2023).
May, R. M. et al. A multi-center retrospective cohort study defines the spectrum of kidney pathology in Coronavirus 2019 Disease (COVID-19). Kidney Int. 100, 1303–1315 (2021).
Klomjit, N., Zand, L., Cornell, L. D. & Alexander, M. P. COVID-19 and glomerular diseases. Kidney Int. Rep. 8, 1137–1150 (2023).
Velez, J. C. Q., Caza, T. & Larsen, C. P. COVAN is the new HIVAN: the re-emergence of collapsing glomerulopathy with COVID-19. Nat. Rev. Nephrol. 16, 565–567 (2020).
Giannini, G. et al. Renal prognosis of COVID-19 associated nephropathy. Kidney Int. Rep. 7, 2722–2725 (2022).
Diebold, M. et al. Incidence of common glomerular diseases other than collapsing glomerulopathy is not increased after SARS-CoV-2 infection. Kidney Int. Rep. 9, 1122–1126 (2024).
Kronbichler, A. & Anders, H.-J. mRNA COVID-19 vaccines and their risk to induce a relapse of glomerular diseases. J. Am. Soc. Nephrol. 33, 2128–2131 (2022).
Stevens, K. I. et al. Perspective on COVID-19 vaccination in patients with immune-mediated kidney diseases: consensus statements from the ERA-IWG and EUVAS. Nephrol. Dial. Transplant. 37, 1400–1410 (2022).
Fenoglio, R. et al. New onset biopsy-proven nephropathies after COVID vaccination. Am. J. Nephrol. 53, 325–330 (2022).
Klomjit, N. et al. COVID-19 vaccination and glomerulonephritis. Kidney Int. Rep. 6, 2969–2978 (2021).
Radhakrishnan, Y. & Zand, L. New onset glomerular disease post-COVID-19 vaccination: is there a link? Kidney360 4, 294–296 (2023).
Caza, T. N. et al. Glomerular disease in temporal association with SARS-CoV-2 vaccination: a series of 29 cases. Kidney360 2, 1770–1780 (2021).
Bomback, A. S., Kudose, S. & D’Agati, V. D. De novo and relapsing glomerular diseases after COVID-19 vaccination: what do we know so far? Am. J. Kidney Dis. 78, 477–480 (2021).
Hummel, A. et al. Idiopathic nephrotic syndrome relapse following COVID-19 vaccination: a series of 25 cases. Clin. Kidney J. 15, 1574–1582 (2022).
Canney, M. et al. A population-based analysis of the risk of glomerular disease relapse after COVID-19 vaccination. J. Am. Soc. Nephrol. 33, 2247–2257 (2022).
Matsuzaki, K. et al. Gross hematuria after SARS-CoV-2 vaccination: questionnaire survey in Japan. Clin. Exp. Nephrol. 26, 316–322 (2022).
Lionaki, S. et al. Adverse events associated with SARS-CoV-2 vaccination in patients with glomerular diseases and the potential risk of disease reactivation. Kidney Int. Rep. 9, 3324–3327 (2024).
Ishimoto, T. et al. Minimal change disease: a CD80 podocytopathy? Semin. Nephrol. 31, 320–325 (2011).
Pan, Y. et al. Assessing acute kidney injury risk after COVID vaccination and infection in a large cohort study. NPJ Vaccines 9, 213 (2024).
Wang, C.-S. et al. Association of COVID-19 versus COVID-19 vaccination with kidney function and disease activity in primary glomerular disease: a report of the cure glomerulonephropathy study. Am. J. Kidney Dis. 83, 37–46 (2024).
Teisseyre, M. et al. Humoral and cellular responses after a third dose of SARS-CoV-2 mRNA vaccine in patients with glomerular disease. Nephrol. Dial. Transplant. 38, 249–251 (2023).
Frodlund, M. et al. The serological immunogenicity of the third and fourth doses of COVID-19 vaccine in patients with inflammatory rheumatic diseases on different biologic or targeted DMARDs: a Swedish nationwide study (COVID-19-REUMA). Microbiol. Spectr. 12, e0298123 (2024).
Embi, P. J. et al. Effectiveness of 2-dose vaccination with mRNA COVID-19 vaccines against COVID-19-associated hospitalizations among immunocompromised adults — Nine states, January–September 2021. MMWR Morb. Mortal. Wkly. Rep. 70, 1553–1559 (2021).
OpenSAFELY Collaborative et al. Comparative effectiveness of two- and three-dose COVID-19 vaccination schedules involving AZD1222 and BNT162b2 in people with kidney disease: a linked OpenSAFELY and UK renal registry cohort study. Lancet Reg. Health Eur. 30, 100636 (2023).
Chen, C.-H., Wu, M.-J. & Tsai, S.-F. Safety and effectiveness of COVID-19 vaccines in patients with IgA nephropathy: a retrospective cohort study from the TriNetX global collaborative networks. EClinicalMedicine 65, 102306 (2023).
Wijkström, J. et al. Results of the first nationwide cohort study of outcomes in dialysis and kidney transplant patients before and after vaccination for COVID-19. Nephrol. Dial. Transplant. 38, 2607–2616 (2023).
Quiroga, B. et al. Humoral response after the fourth dose of the SARS-CoV-2 vaccine in the CKD spectrum: a prespecified analysis of the SENCOVAC study. Nephrol. Dial. Transplant. 38, 969–981 (2023).
Hwang, H. S. et al. Global burden of vaccine-associated kidney injury using an international pharmacovigilance database. Sci. Rep. 15, 5177 (2025).
Arsenault, C. et al. Health system quality and COVID-19 vaccination: a cross-sectional analysis in 14 countries. Lancet Glob. Health 12, e156–e165 (2024).
Pramod, S. et al. Effectiveness of Covishield vaccine in preventing Covid-19 — a test-negative case-control study. Vaccine 40, 3294–3297 (2022).
Maier, H. E. et al. Reduction in long COVID symptoms and symptom severity in vaccinated compared to unvaccinated adults. Open. Forum Infect. Dis. 11, ofae039 (2024).
Lundberg-Morris, L. et al. Covid-19 vaccine effectiveness against post-covid-19 condition among 589 722 individuals in Sweden: population based cohort study. BMJ 383, e076990 (2023).
Xu, Y. et al. Cardiovascular events following coronavirus disease 2019 vaccination in adults: a nationwide Swedish study. Eur. Heart J. 46, 147–157 (2025).
Ghafari, M. et al. Prevalence of persistent SARS-CoV-2 in a large community surveillance study. Nature 626, 1094–1101 (2024).
Yang, C., Zhao, H., Espín, E. & Tebbutt, S. J. Association of SARS-CoV-2 infection and persistence with long COVID. Lancet Respir. Med. 11, 504–506 (2023).
Li, H. et al. Vaccination reduces viral load and accelerates viral clearance in SARS-CoV-2 Delta variant-infected patients. Ann. Med. 55, 419–427 (2023).
Boufidou, F. et al. SARS-CoV-2 reinfections and long COVID in the post-omicron phase of the pandemic. Int. J. Mol. Sci. 24, 12962 (2023).
Hadley, E. et al. Insights from an N3C RECOVER EHR-based cohort study characterizing SARS-CoV-2 reinfections and Long COVID. Commun. Med. 4, 129 (2024).
Jang, J. et al. Vaccine effectiveness in symptom and viral load mitigation in COVID-19 breakthrough infections in South Korea. PLoS ONE 18, e0290154 (2023).
Tandon, P. et al. Unraveling links between chronic inflammation and long COVID: workshop report. J. Immunol. 212, 505–512 (2024).
Trinh, N. T. et al. Effectiveness of COVID-19 vaccines to prevent long COVID: data from Norway. Lancet Respir. Med. 12, e33–e34 (2024).
COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19. (National Institute for Health and Care Excellence, 2024).
Munblit, D. et al. Long COVID: aiming for a consensus. Lancet Respir. Med. 10, 632–634 (2022).
National academies of sciences, engineering, and medicine; health and medicine division; board on health care services; committee on the long-term health effects stemming from COVID-19 and implications for the social security administration. Long-Term Health Effects of COVID-19: Disability and Function Following SARS-CoV-2 Infection. (National Academies Press, 2024).
Thaweethai, T. et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA 329, 1934–1946 (2023).
Soriano, J. B. et al. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 22, e102–e107 (2022).
Yonts, A. Pediatric long-COVID: a review of the definition, epidemiology, presentation, and pathophysiology. Pediatr. Ann. 51, e416–e420 (2022).
Nystrom, S. E. et al. APOL1 high-risk genotype is not associated with new or worsening of proteinuria or kidney function decline following COVID-19 vaccination. Kidney Int. Rep. 9, 2657–2666 (2024).
Waldman, M. et al. COVID-19 vaccination and new onset glomerular disease: results from the IRocGN2 international registry. Kidney360 4, 349–362 (2023).
Kechagias, K. S. et al. Minimal change disease following COVID-19 vaccination: a systematic review. PLoS ONE 19, e0297568 (2024).
Timmermans, S. A. M. E. G. et al. Primary podocytopathies after COVID-19 vaccination. Kidney Int. Rep. 7, 892–894 (2022).
Lim, C. A. et al. Focal segmental glomerulosclerosis following the Pfizer-BioNTech COVID-19 vaccine. Kidney Res. Clin. Pract. 41, 263–266 (2022).
Sato, T. et al. Increase in the number of new cases of ANCA-associated vasculitis in the COVID-19 vaccine era. Clin. Immunol. 252, 109656 (2023).
Sekar, A., Campbell, R., Tabbara, J. & Rastogi, P. ANCA glomerulonephritis after the Moderna COVID-19 vaccination. Kidney Int. 100, 473–474 (2021).
Villa, M. et al. A case of ANCA-associated vasculitis after AZD1222 (Oxford-AstraZeneca) SARS-CoV-2 vaccination: casualty or causality? Kidney Int. 100, 937–938 (2021).
Prabhahar, A. et al. ANCA-associated vasculitis following ChAdOx1 nCoV19 vaccination: case-based review. Rheumatol. Int. 42, 749–758 (2022).
David, R., Hanna, P., Lee, K. & Ritchie, A. Relapsed ANCA associated vasculitis following Oxford AstraZeneca ChAdOx1-S COVID-19 vaccination: a case series of two patients. Nephrology 27, 109–110 (2022).
Moradiya, P., Khandelwal, P., Raina, R. & Mahajan, R. G. Systematic review of individual patient data COVID-19 infection and vaccination-associated thrombotic microangiopathy. Kidney Int. Rep. 9, 3134–3144 (2024).
Gueguen, L., Loheac, C., Saidani, N. & Khatchatourian, L. Membranous nephropathy following anti-COVID-19 mRNA vaccination. Kidney Int. 100, 1140–1141 (2021).
Aoki, R. et al. Gross hematuria after the COVID-19 mRNA vaccination: nationwide multicenter prospective cohort study in Japan. Kidney360 5, 1322–1332 (2024).
Okabe, M. et al. Does COVID-19 vaccination trigger gross hematuria in patients with IgA nephropathy? Clin. Kidney J. 17, sfae160 (2024).
Kimura, H. et al. Two-year follow-up of IgA nephropathy patients who developed gross hematuria following COVID-19 vaccination: a case series and literature review. Intern. Med. https://doi.org/10.2169/internalmedicine.5548-25 (2025).
Kim, H. J., Jung, M., Lim, B. J. & Han, S. H. New-onset class III lupus nephritis with multi-organ involvement after COVID-19 vaccination. Kidney Int. 101, 826–828 (2022).
Zavala-Miranda, M. F., González-Ibarra, S. G., Pérez-Arias, A. A., Uribe-Uribe, N.O. & Mejia-Vilet, J. M. New-onset systemic lupus erythematosus beginning as class V lupus nephritis after COVID-19 vaccination. Kidney Int. 100, 1340–1341 (2021).
Tuschen, K., Bräsen, J. H., Schmitz, J., Vischedyk, M. & Weidemann, A. Relapse of class V lupus nephritis after vaccination with COVID-19 mRNA vaccine. Kidney Int. 100, 941–944 (2021).
Vanjarapu, J. M. R. et al. Proliferative glomerulonephritis with monotypic immunoglobulin deposits: an unusual presentation in the setting of multiple inciting events including COVID-19 vaccination. Cureus 14, e25949 (2022).
Li, Y. et al. Clinical phenotype of AAV, anti-GBM disease and double-positive patients after SARS-CoV-2 vaccination. Autoimmun. Rev. 23, 103521 (2024).
Ritter, A. et al. Clinical spectrum of gross haematuria following SARS-CoV-2 vaccination with mRNA vaccines. Clin. Kidney J. 15, 961–973 (2022).
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, contributed substantially to discussion of the content, wrote the article and reviewed and/or edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
U.A. reports no competing interests; V.I. has received a Long-term Fellowship grant from the European Renal Association (ERA) and is an Editorial Board member of NDT; S.B. reports consultancy fees from AstraZeneca, Bayer and GSK; A.K. reports consulting fees from Amgen, AstraZeneca, Boehringer Ingelheim, CSL Vifor, Delta4, GlaxoSmithKline, Novartis, Otsuka, Roche and Walden Biosciences, all outside of the submitted work. A.K. serves as an Associate Editor of Glomerular Diseases and an Editor of NDT. M.J.S. reports personal fees from NovoNordisk, Jansen, Mundipharma, AstraZeneca, Esteve, Fresenius, Ingelheim Lilly, Vifor and ICU, and grants and personal fees from Boehringer Ingelheim; A.B. received consultancy fees from Amgen, AstraZeneca, Boehringer Ingelheim, CSL Vifor, Otsuka and Sobi and payment or honoraria for lectures, presentations, speaker’s bureaus, manuscript writing or educational events from AstraZeneca, Bayer, Boehringer Ingelheim, ChemoCentryx, CSL Vifor, Fresenius, GlaxoSmithKline and Otsuka; A.B. is an Editorial Board member of CKJ.
Peer review
Peer review information
Nature Reviews Nephrology thanks Luuk Hilbrands, Giuseppe Remuzzi and the other, anonymous, reviewer for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ivković, V., Anandh, U., Bell, S. et al. Long COVID and the kidney. Nat Rev Nephrol 21, 833–845 (2025). https://doi.org/10.1038/s41581-025-00997-4
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41581-025-00997-4
This article is cited by
-
Effects of social determinants of health on the landscape of kidney disease
Nature Reviews Nephrology (2026)