Abstract
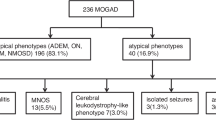
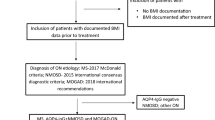
Myelin oligodendrocyte glycoprotein (MOG) antibody-associated disease (MOGAD) is an immune-mediated demyelinating disease that is challenging to differentiate from multiple sclerosis (MS), as the clinical phenotypes overlap, and people with MOGAD can fulfil the current MRI-based diagnostic criteria for MS. In addition, the MOG antibody assays that are an essential component of MOGAD diagnosis are not standardized. Accurate diagnosis of MOGAD is crucial because the treatments and long-term prognosis differ from those for MS. This Expert Recommendation summarizes the outcomes from a Magnetic Resonance Imaging in MS workshop held in Oxford, UK in May 2022, in which MS and MOGAD experts reflected on the pathology and clinical features of these disorders, the contributions of MRI to their diagnosis and the clinical use of the MOG antibody assay. We also critically reviewed the literature to assess the validity of distinctive imaging features in the current MS and MOGAD criteria. We conclude that dedicated orbital and spinal cord imaging (with axial slices) can inform MOGAD diagnosis and also illuminate differential diagnoses. We provide practical guidance to neurologists and neuroradiologists on how to navigate the current MOGAD and MS criteria. We suggest a strategy that includes useful imaging discriminators on standard clinical MRI and discuss imaging features detected by non-conventional MRI sequences that demonstrate promise in differentiating these two disorders.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Thompson, A. J. et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 17, 162–173 (2018).
Geraldes, R. et al. The current role of MRI in differentiating multiple sclerosis from its imaging mimics. Nat. Rev. Neurol. 14, 199–213 (2018).
Marignier, R. et al. Myelin-oligodendrocyte glycoprotein antibody-associated disease. Lancet Neurol. 20, 762–772 (2021).
Walton, C. et al. Rising prevalence of multiple sclerosis worldwide: insights from the atlas of MS, third edition. Mult. Scler. J. 26, 1816–1821 (2020).
Filippi, M. et al. Multiple sclerosis. Nat. Rev. Dis. Prim. 4, 43 (2018).
Thompson, A. J., Baranzini, S. E., Geurts, J., Hemmer, B. & Ciccarelli, O. Multiple sclerosis. Lancet 391, 1622–1636 (2018).
Hohlfeld, R., Dornmair, K., Meinl, E. & Wekerle, H. The search for the target antigens of multiple sclerosis, part 1: autoreactive CD4+ T lymphocytes as pathogenic effectors and therapeutic targets. Lancet Neurol. 15, 198–209 (2016).
Reindl, M. & Waters, P. Myelin oligodendrocyte glycoprotein antibodies in neurological disease. Nat. Rev. Neurol. 15, 89–102 (2019).
O’Connell, K. et al. Prevalence and incidence of neuromyelitis optica spectrum disorder, aquaporin-4 antibody-positive NMOSD and MOG antibody-positive disease in Oxfordshire, UK. J. Neurol. Neurosurg. Psychiatry 91, 1126–1128 (2020).
Papp, V. et al. Worldwide incidence and prevalence of neuromyelitis optica: a systematic review. Neurology 96, 59–77 (2021).
Hor, J. Y. et al. Epidemiology of neuromyelitis optica spectrum disorder and its prevalence and incidence worldwide. Front. Neurol. 11, 543047 (2020).
Cobo-Calvo, A. et al. Clinical spectrum and prognostic value of CNS MOG autoimmunity in adults: the MOGADOR study. Neurology 90, e1858–e1869 (2018).
Jurynczyk, M. et al. Clinical presentation and prognosis in MOG-antibody disease: a UK study. Brain 140, 3128–3138 (2017).
Molazadeh, N. et al. Progression independent of relapses in aquaporin4-IgG-seropositive neuromyelitis optica spectrum disorder, myelin oligodendrocyte glycoprotein antibody-associated disease, and multiple sclerosis. Mult. Scler. Relat. Disord. 80, 105093 (2023).
Chen, B. et al. Do early relapses predict the risk of long-term relapsing disease in an adult and paediatric cohort with MOGAD? Ann. Neurol. 94, 508–517 (2023).
Cobo-Calvo, A. et al. Clinical features and risk of relapse in children and adults with myelin oligodendrocyte glycoprotein antibody-associated disease. Ann. Neurol. 89, 30–41 (2021).
Satukijchai, C. et al. Factors associated with relapse and treatment of myelin oligodendrocyte glycoprotein antibody-associated disease in the United Kingdom. JAMA Netw. Open 5, e2142780 (2022).
Shahriari, M., Sotirchos, E. S., Newsome, S. D. & Yousem, D. M. MOGAD: how it differs from and resembles other neuroinflammatory disorders. Am. J. Roentgenol. 216, 1031–1039 (2021).
Fadda, G., Armangue, T., Hacohen, Y., Chitnis, T. & Banwell, B. Paediatric multiple sclerosis and antibody-associated demyelination: clinical, imaging, and biological considerations for diagnosis and care. Lancet Neurol. 20, 136–149 (2021).
Ciccone, A. et al. Corticosteroids for the long-term treatment in multiple sclerosis. Cochrane Database Syst. Rev. 23, CD006264 (2008).
Hauser, S. L. & Cree, B. A. C. Treatment of multiple sclerosis: a review. Am. J. Med. 133, 1380–1390.e2 (2020).
Hacohen, Y. et al. Disease course and treatment responses in children with relapsing myelin oligodendrocyte glycoprotein antibody-associated disease. JAMA Neurol. 75, 478–487 (2018).
Wang, X. et al. Effectiveness and tolerability of different therapies in preventive treatment of MOG-IgG-associated disorder: a network meta-analysis. Front. Immunol. 13, 953993 (2022).
Jarius, S. et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 2: epidemiology, clinical presentation, radiological and laboratory features, treatment responses, and long-term outcome. J. Neuroinflamm. 13, 280 (2016).
Corbali, O. & Chitnis, T. Pathophysiology of myelin oligodendrocyte glycoprotein antibody disease. Front. Neurol. 14, 1137998 (2023).
Dendrou, C. A., Fugger, L. & Friese, M. A. Immunopathology of multiple sclerosis. Nat. Rev. Immunol. 15, 545–558 (2015).
Yandamuri, S. S. et al. MOGAD patient autoantibodies induce complement, phagocytosis, and cellular cytotoxicity. JCI Insight 8, e165373 (2023).
Prüss, H. Autoantibodies in neurological disease. Nat. Rev. Immunol. 21, 798–813 (2021).
Sun, B., Ramberger, M., O’Connor, K. C., Bashford-Rogers, R. J. M. & Irani, S. R. The B cell immunobiology that underlies CNS autoantibody-mediated diseases. Nat. Rev. Neurol. 16, 481–492 (2020).
Kwon, Y. N. et al. Peripherally derived macrophages as major phagocytes in MOG encephalomyelitis. Neurol. Neuroimmunol. NeuroInflamm. 6, e60 (2019).
Saadoun, S. et al. Neuromyelitis optica MOG-IgG causes reversible lesions in mouse brain. Acta Neuropathol. Commun. 2, 35 (2014).
Höftberger, R. et al. The pathology of central nervous system inflammatory demyelinating disease accompanying myelin oligodendrocyte glycoprotein autoantibody. Acta Neuropathol. 139, 875–892 (2020).
Lassmann, H. Multiple sclerosis: lessons from molecular neuropathology. Exp. Neurol. 262, 2–7 (2014).
Calahorra, L., Camacho-Toledano, C., Serrano-Regal, M. P., Ortega, M. C. & Clemente, D. Regulatory cells in multiple sclerosis: from blood to brain. Biomedicines 10, 335 (2022).
Banwell, B. et al. Diagnosis of myelin oligodendrocyte glycoprotein antibody-associated disease: International MOGAD Panel proposed criteria. Lancet Neurol. 22, 268–282 (2023).
Villacieros‐Álvarez, J. et al. MOG antibodies in adults with a first demyelinating event suggestive of multiple sclerosis. Ann. Neurol. https://doi.org/10.1002/ana.26793 (2023).
Waters, P. J. et al. A multicenter comparison of MOG-IgG cell-based assays. Neurology 92, e1250–e1255 (2019).
Hyun, J.-W. et al. Longitudinal analysis of myelin oligodendrocyte glycoprotein antibodies in CNS inflammatory diseases. J. Neurol. Neurosurg. Psychiatry 88, 811–817 (2017).
Gastaldi, M. et al. Prognostic relevance of quantitative and longitudinal MOG antibody testing in patients with MOGAD: a multicentre retrospective study. J. Neurol. Neurosurg. Psychiatry 94, 201–210 (2023).
Waters, P. et al. Serial anti-myelin oligodendrocyte glycoprotein antibody analyses and outcomes in children with demyelinating syndromes. JAMA Neurol. 77, 82–93 (2020).
Carta, S. et al. Significance of myelin oligodendrocyte glycoprotein antibodies in CSF: a retrospective multicenter study. Neurology 100, e1095–e1108 (2023).
Kim, H. J. & Palace, J. Should we test for IgG antibodies against MOG in both serum and CSF in patients with suspected MOGAD? Neurology 100, 497–498 (2023).
Kwon, Y. N. et al. Myelin oligodendrocyte glycoprotein-immunoglobulin G in the CSF: clinical implication of testing and association with disability. Neurol. Neuroimmunol. Neuroinflamm. 9, e1095 (2022).
Armangue, T. et al. Associations of paediatric demyelinating and encephalitic syndromes with myelin oligodendrocyte glycoprotein antibodies: a multicentre observational study. Lancet Neurol. 19, 234–246 (2020).
de Mol, C. L. et al. The clinical spectrum and incidence of anti-MOG-associated acquired demyelinating syndromes in children and adults. Mult. Scler. 26, 806–814 (2020).
Wendel, E.-M. et al. High association of MOG-IgG antibodies in children with bilateral optic neuritis. Eur. J. Paediatr. Neurol. 27, 86–93 (2020).
Yang, M. et al. Clinical predictive factors for diagnosis of MOG-IgG and AQP4-IgG related paediatric optic neuritis: a Chinese cohort study. Br. J. Ophthalmol. 106, 262–266 (2022).
Chen, J. J. et al. MOG-IgG among participants in the pediatric optic neuritis prospective outcomes study. JAMA Ophthalmol. 139, 583–585 (2021).
Jurynczyk, M. et al. Distinct brain imaging characteristics of autoantibody-mediated CNS conditions and multiple sclerosis. Brain 140, 617–627 (2017).
Cortese, R. et al. Clinical and MRI measures to identify non-acute MOG-antibody disease in adults. Brain 146, 2489–2501 (2022).
Carandini, T. et al. Distinct patterns of MRI lesions in MOG antibody disease and AQP4 NMOSD: a systematic review and meta-analysis. Mult. Scler. Relat. Disord. 54, 103118 (2021).
Carnero Contentti, E. et al. MRI to differentiate multiple sclerosis, neuromyelitis optica, and myelin oligodendrocyte glycoprotein antibody disease. J. Neuroimaging 33, 688–702 (2023).
Varley, J. A. et al. Validation of the 2023 International Diagnostic criteria for MOGAD in a selected cohort of adults and children. Neurology 103, e209321 (2024).
Kim, K. H., Kim, S.-H., Park, N. Y., Hyun, J.-W. & Kim, H. J. Validation of the International MOGAD Panel proposed criteria. Mult. Scler. J. 29, 1680–1683 (2023).
Forcadela, M. et al. Timing of MOG-IgG testing is key to 2023 MOGAD diagnostic criteria. Neurol. Neuroimmunol. Neuroinflamm. 11, e200183 (2024).
Lipps, P. et al. Ongoing challenges in the diagnosis of myelin oligodendrocyte glycoprotein antibody-associated disease. JAMA Neurol. 80, 1377–1379 (2023).
Ciccarelli, O., Toosy, A. T., Thompson, A. & Hacohen, Y. Navigating through the recent diagnostic criteria for MOGAD: challenges and practicalities. Neurology 100, 689–690 (2023).
Lassmann, H. & Bradl, M. Multiple sclerosis: experimental models and reality. Acta Neuropathol. 133, 223–244 (2017).
Takai, Y. et al. Myelin oligodendrocyte glycoprotein antibody-associated disease: an immunopathological study. Brain 143, 1431–1446 (2020).
Gilli, F. & Ceccarelli, A. Magnetic resonance imaging approaches for studying mouse models of multiple sclerosis: a mini review. J. Neurosci. Res. 101, 1259–1274 (2023).
Sechi, E. et al. Comparison of MRI lesion evolution in different central nervous system demyelinating disorders. Neurology 97, e1097–e1109 (2021).
Beltrán, E. et al. Archeological neuroimmunology: resurrection of a pathogenic immune response from a historical case sheds light on human autoimmune encephalomyelitis and multiple sclerosis. Acta Neuropathol. 141, 67–83 (2021).
Carta, S. et al. Antibodies to MOG in CSF only: pathological findings support the diagnostic value. Acta Neuropathol. 141, 801–804 (2021).
Nicaise, A. M. et al. Cellular senescence in progenitor cells contributes to diminished remyelination potential in progressive multiple sclerosis. Proc. Natl Acad. Sci. USA 116, 9030–9039 (2019).
Junker, A. et al. Extensive subpial cortical demyelination is specific to multiple sclerosis. Brain Pathol. 30, 641–652 (2020).
Ciotti, J. R. et al. Central vein sign and other radiographic features distinguishing myelin oligodendrocyte glycoprotein antibody disease from multiple sclerosis and aquaporin-4 antibody-positive neuromyelitis optica. Mult. Scler. 28, 49–60 (2022).
Lassmann, H. Neuroinflammation: 2021 update. Free Neuropathol. 2, 1 (2021).
Wattjes, M. P. et al. 2021 MAGNIMS–CMSC–NAIMS consensus recommendations on the use of MRI in patients with multiple sclerosis. Lancet Neurol. 20, 653–670 (2021).
Soelberg, K. et al. A population-based prospective study of optic neuritis. Mult. Scler. J. 23, 1893–1901 (2017).
Asseyer, S. et al. Prodromal headache in MOG-antibody positive optic neuritis. Mult. Scler. Relat. Disord. 40, 101965 (2020).
Hassan, M. B. et al. Population-based incidence of optic neuritis in the era of aquaporin-4 and myelin oligodendrocyte glycoprotein antibodies. Am. J. Ophthalmol. 220, 110–114 (2020).
Winter, A. & Chwalisz, B. MRI characteristics of NMO, MOG and MS related optic neuritis. Semin. Ophthalmol. 35, 333–342 (2020).
Vicini, R., Brügger, D., Abegg, M., Salmen, A. & Grabe, H. M. Differences in morphology and visual function of myelin oligodendrocyte glycoprotein antibody and multiple sclerosis associated optic neuritis. J. Neurol. 268, 276–284 (2021).
Falcão-Gonçalves, A. B., Bichuetti, D. B. & de Oliveira, E. M. L. Recurrent optic neuritis as the initial symptom in demyelinating diseases. J. Clin. Neurol. 14, 351–358 (2018).
Kraker, J. A. & Chen, J. J. An update on optic neuritis. J. Neurol. 270, 5113–5126 (2023).
Chen, J. J. et al. Myelin oligodendrocyte glycoprotein antibody-positive optic neuritis: clinical characteristics, radiologic clues, and outcome. Am. J. Ophthalmol. 195, 8–15 (2018).
Oertel, F. C. et al. Longitudinal retinal changes in MOGAD. Ann. Neurol. 92, 476–485 (2022).
Roca-Fernández, A. et al. The use of OCT in good visual acuity MOGAD and AQP4-NMOSD patients; with and without optic neuritis. Mult. Scler. J. Exp. Transl. Clin. 7, 20552173211066446 (2021).
Petzold, A. et al. Diagnosis and classification of optic neuritis. Lancet Neurol. 21, 1120–1134 (2022).
Schroeder, A. et al. Detection of optic neuritis on routine brain MRI without and with the assistance of an image postprocessing algorithm. Am. J. Neuroradiol. 42, 1130–1135 (2021).
Petzold, A. et al. The investigation of acute optic neuritis: a review and proposed protocol. Nat. Rev. Neurol. 10, 447–458 (2014).
Riederer, I., Mühlau, M., Hoshi, M.-M., Zimmer, C. & Kleine, J. F. Detecting optic nerve lesions in clinically isolated syndrome and multiple sclerosis: double-inversion recovery magnetic resonance imaging in comparison with visually evoked potentials. J. Neurol. 266, 148–156 (2019).
Hodel, J. et al. Comparison of 3D double inversion recovery and 2D STIR FLAIR MR sequences for the imaging of optic neuritis: pilot study. Eur. Radiol. 24, 3069–3075 (2014).
Fadda, G. et al. Myelitis features and outcomes in CNS demyelinating disorders: comparison between multiple sclerosis, MOGAD, and AQP4-IgG-positive NMOSD. Front. Neurol. 13, 1011579 (2022).
Mariano, R. et al. Comparison of clinical outcomes of transverse myelitis among adults with myelin oligodendrocyte glycoprotein antibody vs aquaporin-4 antibody disease. JAMA Netw. Open 2, e1912732 (2019).
Sechi, E. et al. Myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD): a review of clinical and MRI features, diagnosis, and management. Front. Neurol. 13, 885218 (2022).
Budhram, A. et al. Unilateral cortical FLAIR-hyperintense lesions in anti-MOG-associated encephalitis with seizures (FLAMES): characterization of a distinct clinico-radiographic syndrome. J. Neurol. 266, 2481–2487 (2019).
Budhram, A., Sechi, E., Nguyen, A., Lopez-Chiriboga, A. S. & Flanagan, E. P. FLAIR-hyperintense lesions in anti-MOG-associated encephalitis with seizures (FLAMES): is immunotherapy always needed to put out the fire? Mult. Scler. Relat. Disord. 44, 102283 (2020).
Wang, Y.-F. et al. The clinical features of FLAIR-hyperintense lesions in anti-MOG antibody associated cerebral cortical encephalitis with seizures: case reports and literature review. Front. Immunol. 12, 582768 (2021).
Banks, S. A. et al. Brainstem and cerebellar involvement in MOG-IgG-associated disorder versus aquaporin-4-IgG and MS. J. Neurol. Neurosurg. Psychiatry 92, 384–390 (2020).
Jarius, S. et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 3: brainstem involvement — frequency, presentation and outcome. J. Neuroinflamm. 13, 281 (2016).
Kunchok, A. et al. Does area postrema syndrome occur in myelin oligodendrocyte glycoprotein-IgG-associated disorders (MOGAD)? Neurology 94, 85–88 (2020).
Zhao-Fleming, H. H. et al. CNS demyelinating attacks requiring ventilatory support with myelin oligodendrocyte glycoprotein or aquaporin-4 antibodies. Neurology 97, e1351–e1358 (2021).
Sinha, S. et al. Hemicraniectomy and externalized ventricular drain placement in a pediatric patient with myelin oligodendrocyte glycoprotein-associated tumefactive demyelinating disease. Childs Nerv. Syst. 38, 185–189 (2022).
McLendon, L. A. et al. Dramatic response to anti-IL-6 receptor therapy in children with life-threatening myelin oligodendrocyte glycoprotein-associated disease. Neurol. Neuroimmunol. Neuroinflamm. 10, e200150 (2023).
Hümmert, M. W. et al. Cognition in patients with neuromyelitis optica spectrum disorders: a prospective multicentre study of 217 patients (CogniNMO-Study). Mult. Scler. 29, 819–831 (2023).
Juryńczyk, M., Jacob, A., Fujihara, K. & Palace, J. Myelin oligodendrocyte glycoprotein (MOG) antibody-associated disease: practical considerations. Pract. Neurol. 19, 187–195 (2019).
Yılmaz, Ü., Edizer, S., Songür, Ç. Y., Güzin, Y. & Durak, F. S. Atypical presentation of MOG-related disease: slowly progressive behavioral and personality changes following a seizure. Mult. Scler. Relat. Disord. 36, 101394 (2019).
Jarius, S. et al. Cerebrospinal fluid findings in patients with myelin oligodendrocyte glycoprotein (MOG) antibodies. Part 1: results from 163 lumbar punctures in 100 adult patients. J. Neuroinflamm. 17, 261 (2020).
Sechi, E. et al. Variability of cerebrospinal fluid findings by attack phenotype in myelin oligodendrocyte glycoprotein-IgG-associated disorder. Mult. Scler. Relat. Disord. 47, 102638 (2021).
Tintoré, M. et al. Isolated demyelinating syndromes: comparison of CSF oligoclonal bands and different MR imaging criteria to predict conversion to CDMS. Mult. Scler. J. 7, 359–363 (2001).
Dobson, R., Ramagopalan, S., Davis, A. & Giovannoni, G. Cerebrospinal fluid oligoclonal bands in multiple sclerosis and clinically isolated syndromes: a meta-analysis of prevalence, prognosis and effect of latitude. J. Neurol. Neurosurg. Psychiatry 84, 909–914 (2013).
Ramanathan, S. et al. Radiological differentiation of optic neuritis with myelin oligodendrocyte glycoprotein antibodies, aquaporin-4 antibodies, and multiple sclerosis. Mult. Scler. 22, 470–482 (2016).
Dubey, D. et al. Clinical, radiologic, and prognostic features of myelitis associated with myelin oligodendrocyte glycoprotein autoantibody. JAMA Neurol. 76, 301–309 (2019).
Tzanetakos, D. et al. Cortical involvement and leptomeningeal inflammation in myelin oligodendrocyte glycoprotein antibody disease: a three-dimensional fluid-attenuated inversion recovery MRI study. Mult. Scler. 28, 718–729 (2022).
Ogawa, R. et al. MOG antibody-positive, benign, unilateral, cerebral cortical encephalitis with epilepsy. Neurol. Neuroimmunol. Neuroinflamm. 4, e322 (2017).
Budhram, A., Kunchok, A. C. & Flanagan, E. P. Unilateral leptomeningeal enhancement in myelin oligodendrocyte glycoprotein immunoglobulin G-associated disease. JAMA Neurol. 77, 648 (2020).
Salama, S., Khan, M., Pardo, S., Izbudak, I. & Levy, M. MOG antibody-associated encephalomyelitis/encephalitis. Mult. Scler. J. 25, 1427–1433 (2019).
Elsbernd, P. et al. Cerebral enhancement in MOG antibody-associated disease. J. Neurol. Neurosurg. Psychiatry 95, 14–18 (2023).
Salama, S., Khan, M., Levy, M. & Izbudak, I. Radiological characteristics of myelin oligodendrocyte glycoprotein antibody disease. Mult. Scler. Relat. Disord. 29, 15–22 (2019).
Chia, N. H., Redenbaugh, V., Chen, J. J., Pittock, S. J. & Flanagan, E. P. Corpus callosum involvement in MOG antibody-associated disease in comparison to AQP4-IgG-seropositive neuromyelitis optica spectrum disorder and multiple sclerosis. Mult. Scler. 29, 748–752 (2023).
Cai, M.-T., Zhang, Y.-X., Zheng, Y., Fang, W. & Ding, M.-P. Callosal lesions on magnetic resonance imaging with multiple sclerosis, neuromyelitis optica spectrum disorder and acute disseminated encephalomyelitis. Mult. Scler. Relat. Disord. 32, 41–45 (2019).
Mastrangelo, V. et al. Bilateral extensive corticospinal tract lesions in MOG antibody-associated disease. Neurology 95, 648–649 (2020).
Hacohen, Y. et al. ‘Leukodystrophy-like’ phenotype in children with myelin oligodendrocyte glycoprotein antibody-associated disease. Dev. Med. Child Neurol. 60, 417–423 (2018).
Baumann, M. et al. MRI of the first event in pediatric acquired demyelinating syndromes with antibodies to myelin oligodendrocyte glycoprotein. J. Neurol. 265, 845–855 (2018).
Maranzano, J. et al. MRI evidence of acute inflammation in leukocortical lesions of patients with early multiple sclerosis. Neurology 89, 714–721 (2017).
Cortese, R. et al. Differentiating multiple sclerosis from AQP4-neuromyelitis optica spectrum disorder and MOG-antibody disease with imaging. Neurology 100, e308–e323 (2023).
Messina, S. et al. Contrasting the brain imaging features of MOG-antibody disease, with AQP4-antibody NMOSD and multiple sclerosis. Mult. Scler. 28, 217–227 (2022).
Biotti, D. et al. Optic neuritis in patients with anti-MOG antibodies spectrum disorder: MRI and clinical features from a large multicentric cohort in France. J. Neurol. 264, 2173–2175 (2017).
Carnero Contentti, E. et al. Chiasmatic lesions on conventional magnetic resonance imaging during the first event of optic neuritis in patients with neuromyelitis optica spectrum disorder and myelin oligodendrocyte glycoprotein‐associated disease in a Latin American cohort. Eur. J. Neurol. 29, 802–809 (2022).
Fadda, G. et al. MRI and laboratory features and the performance of international criteria in the diagnosis of multiple sclerosis in children and adolescents: a prospective cohort study. Lancet Child. Adolesc. Health 2, 191–204 (2018).
Cobo-Calvo, A. et al. Cranial nerve involvement in patients with MOG antibody-associated disease. Neurol. Neuroimmunol. Neuroinflamm. 6, e543 (2019).
Haider, L. et al. Cranial nerve enhancement in multiple sclerosis is associated with younger age at onset and more severe disease. Front. Neurol. 10, 1085 (2019).
Denève, M. et al. MRI features of demyelinating disease associated with anti-MOG antibodies in adults. J. Neuroradiol. 46, 312–318 (2019).
Pekcevik, Y. et al. Differentiating neuromyelitis optica from other causes of longitudinally extensive transverse myelitis on spinal magnetic resonance imaging. Mult. Scler. 22, 302–311 (2016).
Mariano, R. et al. Quantitative spinal cord MRI in MOG-antibody disease, neuromyelitis optica and multiple sclerosis. Brain 144, 198–212 (2021).
Webb, L. M. et al. Marked central canal T2-hyperintensity in MOGAD myelitis and comparison to NMOSD and MS. J. Neurol. Sci. 450, 120687 (2023).
Mohseni, S. H. et al. Leptomeningeal and intraparenchymal blood barrier disruption in a MOG-IgG-positive patient. Case Rep. Neurol. Med. 2018, 1365175 (2018).
El Naggar, I. et al. MR imaging in children with transverse myelitis and acquired demyelinating syndromes. Mult. Scler. Relat. Disord. 67, 104068 (2022).
Fadda, G. et al. Comparison of spinal cord magnetic resonance imaging features among children with acquired demyelinating syndromes. JAMA Netw. Open 4, e2128871 (2021).
Cacciaguerra, L. et al. Timing and predictors of T2-lesion resolution in patients with myelin-oligodendrocyte-glycoprotein-antibody-associated disease. Neurology 101, e1376–e1381 (2023).
Abdel-Mannan, O. et al. Evolution of brain MRI lesions in paediatric myelin-oligodendrocyte glycoprotein antibody-associated disease (MOGAD) and its relevance to disease course. J. Neurol. Neurosurg. Psychiatry 95, 426–433 (2023).
Kitley, J. et al. Neuromyelitis optica spectrum disorders with aquaporin-4 and myelin-oligodendrocyte glycoprotein antibodies. JAMA Neurol. 71, 276 (2014).
Fadda, G. et al. Silent new brain MRI lesions in children with MOG-antibody associated disease. Ann. Neurol. 89, 408–413 (2021).
Verhey, L. H. et al. Clinical and MRI activity as determinants of sample size for pediatric multiple sclerosis trials. Neurology 81, 1215–1221 (2013).
Camera, V. et al. Frequency of new silent MRI lesions in myelin oligodendrocyte glycoprotein antibody disease and aquaporin-4 antibody neuromyelitis optica spectrum disorder. JAMA Netw. Open 4, e2137833 (2021).
Syc-Mazurek, S. B. et al. Frequency of new or enlarging lesions on MRI outside of clinical attacks in patients with MOG-antibody-associated disease. Neurology 99, 795–799 (2022).
Schmidt, F. A. et al. Differences in advanced magnetic resonance imaging in MOG-IgG and AQP4-IgG seropositive neuromyelitis optica spectrum disorders: a comparative study. Front. Neurol. 11, 499910 (2020).
Chien, C. et al. Spinal cord lesions and atrophy in NMOSD with AQP4-IgG and MOG-IgG associated autoimmunity. Mult. Scler. J. 25, 1926–1936 (2019).
Duan, Y. et al. Brain structural alterations in MOG antibody diseases: a comparative study with AQP4 seropositive NMOSD and MS. J. Neurol. Neurosurg. Psychiatry 92, 709–716 (2021).
Lotan, I. et al. Volumetric brain changes in MOGAD: a cross-sectional and longitudinal comparative analysis. Mult. Scler. Relat. Disord. 69, 104436 (2023).
Rechtman, A. et al. Volumetric brain loss correlates with a relapsing MOGAD disease course. Front. Neurol. 13, 867190 (2022).
Zhuo, Z. et al. Brain structural and functional alterations in MOG antibody disease. Mult. Scler. J. 27, 1350–1363 (2021).
Fadda, G. et al. Deviation from normative whole brain and deep gray matter growth in children with MOGAD, MS, and monophasic seronegative demyelination. Neurology 101, e425–e437 (2023).
Gao, C. et al. Structural and functional alterations in visual pathway after optic neuritis in MOG antibody disease: a comparative study with AQP4 seropositive NMOSD. Front. Neurol. 12, 673472 (2021).
Brier, M. R. et al. Quantitative MRI identifies lesional and non-lesional abnormalities in MOGAD. Mult. Scler. Relat. Disord. 73, 104659 (2023).
Castellaro, M. et al. The use of the central vein sign in the diagnosis of multiple sclerosis: a systematic review and meta-analysis. Diagnostics 10, 1025 (2020).
Cagol, A. et al. Diagnostic performance of cortical lesions and the central vein sign in multiple sclerosis. JAMA Neurol. 81, 143–153 (2024).
Clarke, M. A. et al. Paramagnetic rim lesions and the central vein sign: characterizing multiple sclerosis imaging markers. J. Neuroimaging 34, 86–94 (2024).
Sinnecker, T. et al. MRI phase changes in multiple sclerosis vs neuromyelitis optica lesions at 7 T. Neurol. Neuroimmunol. Neuroinflamm. 3, e259 (2016).
Juryńczyk, M., Jakuszyk, P., Kurkowska-Jastrzębska, I. & Palace, J. Increasing role of imaging in differentiating MS from non-MS and defining indeterminate borderline cases. Neurol. Neurochir. Pol. 56, 210–219 (2021).
Sacco, S. et al. Susceptibility-based imaging aids accurate distinction of pediatric-onset MS from myelin oligodendrocyte glycoprotein antibody-associated disease. Mult. Scler. 29, 1736–1747 (2023).
Harrison, K. L. et al. Central vein sign in pediatric multiple sclerosis and myelin oligodendrocyte glycoprotein antibody-associated disease. Pediatr. Neurol. 146, 21–25 (2023).
Clarke, L. et al. Magnetic resonance imaging in neuromyelitis optica spectrum disorder. Clin. Exp. Immunol. 206, 251–265 (2021).
Matthews, L. et al. Distinction of seropositive NMO spectrum disorder and MS brain lesion distribution. Neurology 80, 1330–1337 (2013).
Juryńczyk, M. et al. Brain lesion distribution criteria distinguish MS from AQP4-antibody NMOSD and MOG-antibody disease. J. Neurol. Neurosurg. Psychiatry 88, 132–136 (2017).
Huh, S.-Y. et al. The usefulness of brain MRI at onset in the differentiation of multiple sclerosis and seropositive neuromyelitis optica spectrum disorders. Mult. Scler. 20, 695–704 (2014).
Carnero Contentti, E. et al. Towards imaging criteria that best differentiate MS from NMOSD and MOGAD: large multi-ethnic population and different clinical scenarios. Mult. Scler. Relat. Disord. 61, 103778 (2022).
Bensi, C. et al. Brain and spinal cord lesion criteria distinguishes AQP4-positive neuromyelitis optica and MOG-positive disease from multiple sclerosis. Mult. Scler. Relat. Disord. 25, 246–250 (2018).
Cacciaguerra, L. et al. Brain and cord imaging features in neuromyelitis optica spectrum disorders. Ann. Neurol. 85, 371–384 (2019).
Solomon, A. J. et al. Differential diagnosis of suspected multiple sclerosis: an updated consensus approach. Lancet Neurol. 22, 750–768 (2023).
Abdel‐Mannan, O. et al. Incidence of paediatric multiple sclerosis and other acquired demyelinating syndromes: 10‐year follow‐up surveillance study. Dev. Med. Child Neurol. 64, 502–508 (2022).
Hacohen, Y. et al. Diagnostic algorithm for relapsing acquired demyelinating syndromes in children. Neurology 89, 269–278 (2017).
Author information
Authors and Affiliations
Consortia
Contributions
R.G., G.A., B.B., A.R., R.C., H.L., S.M., M.A.R. and P.W. researched data for the article. R.G., B.B., A.R., H.L., P.W. and J.P. contributed substantially to discussion of the content. R.G., G.A. and J.P. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
R.G. has received support for scientific meetings and courses from Bayer, Biogen, Merck, Novartis and Janssen and honoraria for advisory work or talks from Biogen, Novartis, UCB and MIAC. G.A. has received compensation for consulting services, speaking honoraria or participation in advisory boards from Roche and Horizon Therapeutics; and travel support for scientific meetings from Novartis, Roche, Horizon Therapeutics, ECTRIMS and EAN. She serves as an editor for Europe for Multiple Sclerosis Journal — Experimental, Translational and Clinical and as a member of the editorial and scientific committee of Acta Neurológica Colombiana. She is a member of the International Women in Multiple Sclerosis (iWiMS) network executive committee, the European Biomarkers in Multiple Sclerosis (BioMS-eu) steering committee and the MOGAD Eugene Devic European Network (MEDEN) steering group. B.B. has received or will potentially receive financial compensation for consultancy for Novartis, Roche, UCB, Horizon Therapeutics, Biogen and Immunic Therapeutics for advice on clinical trial design. B.B. is funded by the National Multiple Sclerosis Society and NIH and was previously funded by the Canadian Multiple Sclerosis Society. A.R. serves or has served on scientific advisory boards for Novartis, Sanofi-Genzyme, Synthetic MR, TensorMedical, Roche and Biogen and has received speaker honoraria from Bayer, Sanofi-Genzyme, Merck-Serono, Teva Pharmaceutical Industries, Novartis, Roche, Bristol-Myers and Biogen, is Chief Marketing Officer and co-founder of TensorMedical and receives research support from Fondo de Investigación en Salud (PI19/00950 and PI22/01589) from Instituto de Salud Carlos III, Spain. R.C. has received speaker honoraria and/or travel support from Roche, Merck, Sanofi-Genzyme, Novartis, Janssen and UCB. H.L. has received honoraria from Novartis, Sanofi, Genzyme, BMS and UCB Biopharma for lectures, unrelated to the topic of this manuscript. S.M. has received travel grants from Roche, Merck and Sanofi and has received speaking honoraria from UCB. M.A.R. has received consulting fees from Biogen, Bristol Myers Squibb, Eli Lilly, Janssen and Roche and speaker honoraria from AstraZeneca, Biogen, Bristol Myers Squibb, Bromatech, Celgene, Genzyme, Horizon Therapeutics Italy, Merck Serono, Novartis, Roche, Sanofi and Teva. She receives research support from the MS Society of Canada, the Italian Ministry of Health, the Italian Ministry of University and Research and Fondazione Italiana Sclerosi Multipla. She is Associate Editor for Multiple Sclerosis and Related Disorders. P.W. has received research grants from Euroimmun, CSL Behring and patent royalties for antibody testing (W02010046716A1). He is the Co-Director of the Oxford Autoimmune Neurology Diagnostic Laboratory (Oxford University, Oxford, UK) where MOG-IgG1 autoantibodies are tested, and both he and the University of Oxford receive royalties for antibody tests for LGI1 and CASPR2 (W02010046716A1). He has received honoraria or consulting fees from Biogen Idec, F Hoffmann La-Roche, Mereo BioPharma, Retrogenix, UBC, Euroimmun, University of British Columbia and Alexion; and travel grants from the Guthy-Jackson Charitable Foundation. Work in the Oxford Autoimmune Neurology Diagnostic Laboratory is supported by the UK National Health Service Commissioning service for NMOSD. D.C. is a consultant for Hoffmann-La Roche. In the past 3 years, he has been a consultant for Biogen and has received research funding from Hoffmann-La Roche, the International Progressive MS Alliance, the MS Society, the Medical Research Council and the National Institute for Health Research (NIHR) University College London Hospitals (UCLH) Biomedical Research Centre and a speaker’s honorarium from Novartis. He co-supervises a clinical fellowship at the National Hospital for Neurology and Neurosurgery, London, which is supported by Merck. C.G. reports personal fees from Biogen, Merck Serono, Teva Pharmaceuticals, Sanofi Genzyme, Almirall, Novartis, Roche and Bayer, outside the submitted work. R.M. undertook graduate studies funded by the Rhodes Trust and the Oppenheimer Memorial Trust. F.P. has received honoraria and research support from Alexion, Bayer, Biogen, Chugai, Merck Serono, Novartis, Genyzme, MedImmune, Shire and Teva Pharmaceuticals and serves on scientific advisory boards for Alexion, MedImmune, Novartis and UCB. He has received funding from Deutsche Forschungsgemeinschaft (DFG Exc 257), Bundesministerium für Bildung und Forschung (Competence Network Multiple Sclerosis), Guthy-Jackson Charitable Foundation, EU Framework Program 7 and National Multiple Sclerosis Society of the USA. He serves on the steering committee of the N-Momentum study of inebilizumab (Horizon Therapeutics) and the OCTiMS Study (Novartis). He is an associate editor for Neurology, Neuroimmunology, and Neuroinflammation and academic editor with PLoS ONE. G.C.D. has received support from the NIHR Biomedical Research Centre (BRC), Oxford; and research funding from the Oxford BRC, MRC(UK), UK MS Society, National Health and Medical Research (Australia), Department of Defense (USA), European Charcot Foundation, American Academy of Neurology (AAN), Merck-Serono and Oxford-Quinnipiac Partnership. G.C.D. has also received travel expenses from Genzyme, Merck Serono, Novartis, Roche, the MS Academy and AAN and honoraria as an invited speaker or faculty for Novartis, Roche, the MS Academy and AAN. C.E. reports personal fees from Biogen, Bayer HealthCare Pharmaceuticals, Merck Serono, Novartis, Shire, Genzyme, Teva Pharmaceuticals, Sanofi, Celgene and Roche, outside the submitted work. L.K. received no personal compensation. His institutions (University Hospital Basel/Stiftung Neuroimmunology and Neuroscience Basel) have received and used exclusively for research support payments for steering committee and advisory board participation, consultancy services and participation in educational activities from Bayer, BMS, Celgene, Dörries-Frank Molnia & Pohlmann, Eli Lilly, EMD Serono, Genentech, Glaxo Smith Kline, Janssen Pharmaceuticals, Japan Tobacco, Merck, MH Consulting, Minoryx, Novartis, F. Hoffmann-La Roche, Senda Biosciences, Sanofi, Santhera, Shionogi, TG Therapeutics and Wellmera; licence fees for Neurostatus-UHB products; and grants from Novartis, Innosuisse and Roche. M.I.L. is funded by the NHS (Myasthenia and Related Disorders Service and National Specialized Commissioning Group for Neuromyelitis Optica, UK) and by the University of Oxford, UK. She has been awarded research grants from the UK Association for Patients with Myasthenia (Myaware), Muscular Dystrophy Campaign (MDUK) and the University of Oxford. She has received speaker honoraria and travel grants from UCB Pharma and Horizon Therapeutics and consultancy fees from UCB Pharma. She serves on scientific or educational advisory boards for UCB Pharma, Argenx and Horizon Therapeutics and on the Steering Committee for Horizon Therapeutics. J.S.-G. reports grants and personal fees from Sanofi Genzyme and personal fees from Almirall, Biogen, Celgene, Merck Serono, Novartis, Roche and Teva Pharmaceuticals, outside the submitted work, and is a member of the Editorial Committee of Multiple Sclerosis Journal and Director of the Scientific Committee of Revista de Neurologia. T.Y. reports personal fees from Biogen, Novartis, Bayer HealthCare Pharmaceuticals and Hikma, outside the submitted work, and has received research support from Biogen, GlaxoSmithKline, Novartis and Schering. O.C. is an NIHR Research Professor (RP-2017-08-ST2-004); over the past 2 years, she has been a member of an independent data and safety monitoring board for Novartis; she gave a teaching talk in a Merck local symposium and contributed to an Advisory Board for Biogen; she is Deputy Editor of Neurology, for which she receives an honorarium; she has received research grant support from the MS Society of Great Britain and Northern Ireland, the NIHR UCLH Biomedical Research Centre, the Rosetree Trust, the National MS Society and the NIHR-HTA. M.F. is Editor-in-Chief of the Journal of Neurology, Associate Editor of Human Brain Mapping, Neurological Sciences and Radiology; received compensation for consulting services from Alexion, Almirall, Biogen, Merck, Novartis, Roche and Sanofi; speaking activities from Bayer, Biogen, Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck Serono, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda and TEVA; participation in advisory boards for Alexion, Biogen, Bristol-Myers Squibb, Merck, Novartis, Roche, Sanofi, Sanofi-Aventis, Sanofi-Genzyme and Takeda; and scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol-Myers Squibb, Lilly, Novartis and Sanofi-Genzyme. He receives research support from Biogen Idec, Merck Serono, Novartis, Roche, the Italian Ministry of Health, the Italian Ministry of University and Research and Fondazione Italiana Sclerosi Multipla. F.B. is supported by the NIHR biomedical research centre at University College London Hospitals. F.B. is part of the steering committee or a data safety monitoring board member for Biogen, Merck, ATRI/ACTC and Prothena, is a consultant for Roche, Celltrion, Rewind Therapeutics, Merck, IXICO, Jansen and Combinostics, has research agreements with Merck, Biogen, GE Healthcare and Roche and is a co-founder and shareholder of Queen Square Analytics. J.P. has received support for scientific meetings and honoraria for advisory work from Merck Serono, Novartis, Chugai, Alexion, Roche, Medimmune, Argenx, Vitaccess, UCB, Mitsubishi, Amplo and Janssen, and grants from Alexion, Argenx, Clene, Roche, Medimmune and Amplo Biotechnology. She holds patent ref. P37347WO, a licence agreement with Numares multimarker MS diagnostics and shares in AstraZeneca. Her group has been awarded an ECTRIMS fellowship and a Sumaira Foundation grant to start later this year. A Charcot fellow worked in Oxford 2019–2021. She acknowledges partial funding to the Oxford University Hospitals Trust by Highly Specialized Services NHS England. She is on the medical advisory boards of the Sumaira Foundation and MOG project charities, is a member of the Guthy Jackon Foundation Charity and is on the Board of the European Charcot Foundation, the steering committee of MAGNIMS and the UK NHSE IVIG Committee. She is Chair of the NHSE neuroimmunology patient pathway and has been an ECTRIMS Council member on the educational committee since June 2023. She is also on the Association of British Neurologists advisory groups for MS and neuroinflammation and neuromuscular diseases. Y.H. declares no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks I. Nakashima, E. Flanagan, R. Dale and E. Sechi for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
MAGNIMS: https://www.magnims.eu/
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geraldes, R., Arrambide, G., Banwell, B. et al. The influence of MOGAD on diagnosis of multiple sclerosis using MRI. Nat Rev Neurol 20, 620–635 (2024). https://doi.org/10.1038/s41582-024-01005-2
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41582-024-01005-2
This article is cited by
-
Performance of the 2023 diagnostic criteria for MOGAD: real-world application in a Chinese multicenter cohort of pediatric and adult patients
BMC Medicine (2025)
-
Multiple sclerosis: molecular pathogenesis and therapeutic intervention
Signal Transduction and Targeted Therapy (2025)
-
MOG antibody-positive patients meeting diagnostic criteria for MS: is it MOGAD with an MS-like phenotype or true MS?
Neurological Sciences (2025)
-
The importance of ALPK1 kinase functionality as a potential biomarker for inflammatory diseases
Molecular Biology Reports (2025)
-
Reconsideration of conversion to multiple sclerosis: one-year cerebral lesion appearance rate of Japanese aquaporin-4 antibody-negative optic neuritis patients
Japanese Journal of Ophthalmology (2025)