Abstract
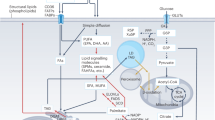
Lipid metabolism encompasses the catabolism and anabolism of lipids, and is fundamental for the maintenance of cellular homeostasis, particularly within the lipid-rich CNS. Increasing evidence further underscores the importance of lipid remodelling and transfer within and between glial cells and neurons as key orchestrators of CNS lipid homeostasis. In this Review, we summarize and discuss the complex landscape of processes involved in lipid metabolism, remodelling and intercellular transfer in the CNS. Highlighted are key pathways, including those mediating lipid (and lipid droplet) biogenesis and breakdown, lipid oxidation and phospholipid metabolism, as well as cell–cell lipid transfer mediated via lipoproteins, extracellular vesicles and tunnelling nanotubes. We further explore how the dysregulation of these pathways contributes to the onset and progression of neurodegenerative diseases, and examine the homeostatic and pathogenic impacts of environment, diet and lifestyle on CNS lipid metabolism.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Yoon, J. H. et al. Brain lipidomics: from functional landscape to clinical significance. Sci. Adv. 8, eadc9317 (2022).
Sastry, P. S. Lipids of nervous tissue: composition and metabolism. Prog. Lipid Res. 24, 69–176 (1985).
van Echten-Deckert, G. The role of sphingosine 1-phosphate metabolism in brain health and disease. Pharmacol. Ther. 244, 108381 (2023).
Baggelaar, M. P., Maccarrone, M. & van der Stelt, M. 2-Arachidonoylglycerol: a signaling lipid with manifold actions in the brain. Prog. Lipid Res. 71, 1–17 (2018).
Valles, A. S. & Barrantes, F. J. The synaptic lipidome in health and disease. Biochim. Biophys. Acta Biomembr. 1864, 184033 (2022).
Osetrova, M. et al. Lipidome atlas of the adult human brain. Nat. Commun. 15, 4455 (2024).
Tracey, T. J., Kirk, S. E., Steyn, F. J. & Ngo, S. T. The role of lipids in the central nervous system and their pathological implications in amyotrophic lateral sclerosis. Semin. Cell Dev. Biol. 112, 69–81 (2021).
Jiménez-Rojo, N. & Riezman, H. On the road to unraveling the molecular functions of ether lipids. FEBS Lett. 593, 2378–2389 (2019).
van Meer, G., Voelker, D. R. & Feigenson, G. W. Membrane lipids: where they are and how they behave. Nat. Rev. Mol. Cell Biol. 9, 112–124 (2008).
Zhang, W., Trible, R. P. & Samelson, L. E. LAT palmitoylation: its essential role in membrane microdomain targeting and tyrosine phosphorylation during T cell activation. Immunity 9, 239–246 (1998).
Montaner, A. et al. Specific phospholipids regulate the acquisition of neuronal and astroglial identities in post-mitotic cells. Sci. Rep. 8, 460 (2018).
Saher, G. et al. High cholesterol level is essential for myelin membrane growth. Nat. Neurosci. 8, 468–475 (2005).
Coelho, R. P., Saini, H. S. & Sato-Bigbee, C. Sphingosine-1-phosphate and oligodendrocytes: from cell development to the treatment of multiple sclerosis. Prostaglandins Other Lipid Mediat. 91, 139–144 (2010).
Walther, T. C. & Farese, R. V. Jr The life of lipid droplets. Biochim. Biophys. Acta 1791, 459–466 (2009).
Arendt, K. L. et al. PIP3 controls synaptic function by maintaining AMPA receptor clustering at the postsynaptic membrane. Nat. Neurosci. 13, 36–44 (2010).
Jiang, X. et al. Simvastatin blocks blood–brain barrier disruptions induced by elevated cholesterol both in vivo and in vitro. Int. J. Alzheimers Dis. 2012, 109324 (2012).
Mehdi, S. M. A. et al. Depression and cognition are associated with lipid dysregulation in both a multigenerational study of depression and the National Health and Nutrition Examination Survey. Transl. Psychiatry 14, 142 (2024).
Vanherle, S. et al. Extracellular vesicle-associated cholesterol supports the regenerative functions of macrophages in the brain. J. Extracell. Vesicles 12, e12394 (2023). This study demonstrates that EVs from repair-associated macrophages enhance OPC differentiation and remyelination by delivering cholesterol, highlighting a key role for EV-mediated cholesterol trafficking in CNS repair.
Bogie, J. F. J. et al. Stearoyl-CoA desaturase-1 impairs the reparative properties of macrophages and microglia in the brain. J. Exp. Med. 217, e20191660 (2020). This paper reveals that sustained myelin accumulation in phagocytes drives a lesion-promoting phenotype via desaturase SCD1-regulated lipid metabolism, and inhibiting SCD1 enhances remyelination.
Wu, J. et al. Nonvesicular lipid transfer drives myelin growth in the central nervous system. Nat. Commun. 15, 9756 (2024).
Bogie, J. F. J., Haidar, M., Kooij, G. & Hendriks, J. J. A. Fatty acid metabolism in the progression and resolution of CNS disorders. Adv. Drug. Deliv. Rev. 159, 198–213 (2020).
Valenza, M., Birolini, G. & Cattaneo, E. The translational potential of cholesterol-based therapies for neurological disease. Nat. Rev. Neurol. 19, 583–598 (2023).
Dietschy, J. M. Central nervous system: cholesterol turnover, brain development and neurodegeneration. Biol. Chem. 390, 287–293 (2009).
Dietschy, J. M. & Turley, S. D. Thematic review series: brain lipids. Cholesterol metabolism in the central nervous system during early development and in the mature animal. J. Lipid Res. 45, 1375–1397 (2004).
Berghoff, S. A., Spieth, L. & Saher, G. Local cholesterol metabolism orchestrates remyelination. Trends Neurosci. 45, 272–283 (2022).
Orth, M. & Bellosta, S. Cholesterol: its regulation and role in central nervous system disorders. Cholesterol 2012, 292598 (2012).
Quan, G., Xie, C., Dietschy, J. M. & Turley, S. D. Ontogenesis and regulation of cholesterol metabolism in the central nervous system of the mouse. Brain Res. Dev. Brain Res. 146, 87–98 (2003).
Morell, P. & Jurevics, H. Origin of cholesterol in myelin. Neurochem. Res. 21, 463–470 (1996).
Andersson, M., Elmberger, P. G., Edlund, C., Kristensson, K. & Dallner, G. Rates of cholesterol, ubiquinone, dolichol and dolichyl-P biosynthesis in rat brain slices. FEBS Lett. 269, 15–18 (1990).
Wang, H. & Eckel, R. H. What are lipoproteins doing in the brain? Trends Endocrinol. Metab. 25, 8–14 (2014).
Valenza, M. et al. Dysfunction of the cholesterol biosynthetic pathway in Huntington’s disease. J. Neurosci. 25, 9932–9939 (2005).
Thelen, K. M., Falkai, P., Bayer, T. A. & Lütjohann, D. Cholesterol synthesis rate in human hippocampus declines with aging. Neurosci. Lett. 403, 15–19 (2006).
Stommel, A., Berlet, H. H. & Debuch, H. Buoyant density and lipid composition of purified myelin of aging human brain. Mech. Ageing Dev. 48, 1–14 (1989).
Boisvert, M. M., Erikson, G. A., Shokhirev, M. N. & Allen, N. J. The aging astrocyte transcriptome from multiple regions of the mouse brain. Cell Rep. 22, 269–285 (2018).
Habib, N. et al. Disease-associated astrocytes in Alzheimer’s disease and aging. Nat. Neurosci. 23, 701–706 (2020). This paper shows that disease-associated astrocytes, identified through single-nucleus RNA sequencing in an Alzheimer disease mouse model, emerge early in disease progression and increase with age, and are also present in aged wild-type mice and human brains, linking them to genetic and age-related factors.
Miron, V. E. et al. Statin therapy inhibits remyelination in the central nervous system. Am. J. Pathol. 174, 1880–1890 (2009).
Leitmeyer, K. et al. Simvastatin results in a dose-dependent toxic effect on spiral ganglion neurons in an in vitro organotypic culture assay. Biomed. Res. Int. 2016, 3580359 (2016).
Schulz, J. G. et al. HMG-CoA reductase inhibition causes neurite loss by interfering with geranylgeranylpyrophosphate synthesis. J. Neurochem. 89, 24–32 (2004).
Wood, W. G., Eckert, G. P., Igbavboa, U. & Muller, W. E. Statins and neuroprotection: a prescription to move the field forward. Ann. N. Y. Acad. Sci. 1199, 69–76 (2010).
Wang, M., Wang, J., Liu, M. & Chen, G. Fluvastatin protects neuronal cells from hydrogen peroxide-induced toxicity with decreasing oxidative damage and increasing PI3K/Akt/mTOR signalling. J. Pharm. Pharmacol. 73, 515–521 (2021).
Ekladious, S. T. & El Sayed, N. S. Effect of pioglitazone and simvastatin in lipopolysaccharide-induced amyloidogenesis and cognitive impairment in mice: possible role of glutamatergic pathway and oxidative stress. Behav. Pharmacol. 30, 5–15 (2019).
Miron, V. E. et al. Simvastatin regulates oligodendroglial process dynamics and survival. Glia 55, 130–143 (2007).
Refolo, L. M. et al. A cholesterol-lowering drug reduces β-amyloid pathology in a transgenic mouse model of Alzheimer’s disease. Neurobiol Dis 8, 890–899 (2001).
Simons, M. et al. Cholesterol depletion inhibits the generation of β-amyloid in hippocampal neurons. Proc. Natl Acad. Sci. USA 95, 6460–6464 (1998).
Wang, H. et al. Regulation of β-amyloid production in neurons by astrocyte-derived cholesterol. Proc. Natl Acad. Sci. USA 118, e2102191118 (2021).
Marquer, C. et al. Increasing membrane cholesterol of neurons in culture recapitulates Alzheimer’s disease early phenotypes. Mol. Neurodegener. 9, 60 (2014).
van der Kant, R., Goldstein, L. S. B. & Ossenkoppele, R. Amyloid-β-independent regulators of tau pathology in Alzheimer disease. Nat. Rev. Neurosci. 21, 21–35 (2020).
Wang, H. et al. Biphasic effects of statins on neuron cell functions under oxygen–glucose deprivation and normal culturing conditions via different mechanisms. Pharmacol. Res. Perspect. 10, e01001 (2022).
Garcia Corrales, A. V., Haidar, M., Bogie, J. F. J. & Hendriks, J. J. A. Fatty acid synthesis in glial cells of the CNS. Int. J. Mol. Sci. 22, 8159 (2021).
Dimas, P. et al. CNS myelination and remyelination depend on fatty acid synthesis by oligodendrocytes. eLife 8, e44702 (2019).
Lebrun-Julien, F. et al. Balanced mTORC1 activity in oligodendrocytes is required for accurate CNS myelination. J. Neurosci. 34, 8432–8448 (2014).
Knobloch, M. et al. Metabolic control of adult neural stem cell activity by Fasn-dependent lipogenesis. Nature 493, 226–230 (2013).
Ziegler, A. B. et al. Cell-autonomous control of neuronal dendrite expansion via the fatty acid synthesis regulator SREBP. Cell Rep. 21, 3346–3353 (2017).
Garcia Corrales, A. V. et al. Fatty acid elongation by ELOVL6 hampers remyelination by promoting inflammatory foam cell formation during demyelination. Proc. Natl Acad. Sci. USA 120, e2301030120 (2023).
Grajchen, E. et al. Fatty acid desaturation by stearoyl-CoA desaturase-1 controls regulatory T cell differentiation and autoimmunity. Cell Mol. Immunol. 20, 666–679 (2023). This paper shows that the desaturase SCD1 regulates regulatory T cell differentiation and autoimmunity by influencing fatty acid metabolism in T cells, providing insights into potential therapeutic strategies for autoimmune disorders such as multiple sclerosis.
Hamilton, L. K. et al. Aberrant lipid metabolism in the forebrain niche suppresses adult neural stem cell proliferation in an animal model of Alzheimer’s disease. Cell Stem Cell 17, 397–411 (2015).
Fanning, S. et al. Lipidomic analysis of ɑ-synuclein neurotoxicity identifies stearoyl CoA desaturase as a target for Parkinson treatment. Mol. Cell 73, 1001–1014 (2019).
Loix, M. et al. Stearoyl-CoA desaturase-1: a potential therapeutic target for neurological disorders. Mol. Neurodegener. 19, 85 (2024).
Bazinet, R. P. & Laye, S. Polyunsaturated fatty acids and their metabolites in brain function and disease. Nat. Rev. Neurosci. 15, 771–785 (2014).
Brennan, E., Kantharidis, P., Cooper, M. E. & Godson, C. Pro-resolving lipid mediators: regulators of inflammation, metabolism and kidney function. Nat. Rev. Nephrol. 17, 725–739 (2021).
Serhan, C. N. Pro-resolving lipid mediators are leads for resolution physiology. Nature 510, 92–101 (2014).
Dunn, H. C. et al. Restoration of lipoxin A4 signaling reduces Alzheimer’s disease-like pathology in the 3xTg-AD mouse model. J. Alzheimers Dis. 43, 893–903 (2015).
Derada Troletti, C. et al. Pro-resolving lipid mediator lipoxin A4 attenuates neuro-inflammation by modulating T cell responses and modifies the spinal cord lipidome. Cell Rep. 35, 109201 (2021).
Kooij, G. et al. Specialized pro-resolving lipid mediators are differentially altered in peripheral blood of patients with multiple sclerosis and attenuate monocyte and blood–brain barrier dysfunction. Haematologica 105, 2056–2070 (2020).
Duffney, P. F. et al. Key roles for lipid mediators in the adaptive immune response. J. Clin. Invest. 128, 2724–2731 (2018).
Jiang, X., Stockwell, B. R. & Conrad, M. Ferroptosis: mechanisms, biology and role in disease. Nat. Rev. Mol. Cell Biol. 22, 266–282 (2021).
Dong, Y. et al. Oxidized phosphatidylcholines found in multiple sclerosis lesions mediate neurodegeneration and are neutralized by microglia. Nat. Neurosci. 24, 489–503 (2021). This study identifies oxidized PCs as potent neurotoxins driving neurodegeneration in multiple sclerosis and highlights the protective role of TREM2-expressing microglia in mitigating oxidized PC-induced damage, suggesting therapeutic potential in enhancing microglia-mediated oxidized PC clearance.
Dong, Y. & Yong, V. W. Oxidized phospholipids as novel mediators of neurodegeneration. Trends Neurosci. 45, 419–429 (2022).
Bjorkhem, I. et al. From brain to bile. Evidence that conjugation and omega-hydroxylation are important for elimination of 24S-hydroxycholesterol (cerebrosterol) in humans. J. Biol. Chem. 276, 37004–37010 (2001).
Bjorkhem, I. & Meaney, S. Brain cholesterol: long secret life behind a barrier. Arterioscler. Thromb. Vasc. Biol. 24, 806–815 (2004).
Brown, J. 3rd et al. Differential expression of cholesterol hydroxylases in Alzheimer’s disease. J. Biol. Chem. 279, 34674–34681 (2004).
Abildayeva, K. et al. 24(S)-Hydroxycholesterol participates in a liver X receptor-controlled pathway in astrocytes that regulates apolipoprotein E-mediated cholesterol efflux. J. Biol. Chem. 281, 12799–12808 (2006).
Testa, G. et al. Changes in brain oxysterols at different stages of Alzheimer’s disease: their involvement in neuroinflammation. Redox Biol. 10, 24–33 (2016).
Gamba, P. et al. Up-regulation of β-amyloidogenesis in neuron-like human cells by both 24- and 27-hydroxycholesterol: protective effect of N-acetyl-cysteine. Aging Cell 13, 561–572 (2014).
Marwarha, G., Dasari, B., Prasanthi, J. R., Schommer, J. & Ghribi, O. Leptin reduces the accumulation of Aβ and phosphorylated tau induced by 27-hydroxycholesterol in rabbit organotypic slices. J. Alzheimers Dis. 19, 1007–1019 (2010).
Wang, Y. et al. 27-Hydroxycholesterol-induced dysregulation of cholesterol metabolism impairs learning and memory ability in apoe ε4 transgenic mice. Int. J. Mol. Sci. 23, 11639 (2022).
Chen, S. et al. 27-Hydroxycholesterol contributes to lysosomal membrane permeabilization-mediated pyroptosis in co-cultured SH-SY5Y cells and C6 cells. Front. Mol. Neurosci. 12, 14 (2019).
Merino-Serrais, P. et al. 27-Hydroxycholesterol induces aberrant morphology and synaptic dysfunction in hippocampal neurons. Cereb. Cortex 29, 429–446 (2019).
Loera-Valencia, R. et al. High levels of 27-hydroxycholesterol results in synaptic plasticity alterations in the hippocampus. Sci. Rep. 11, 3736 (2021).
Alanko, V. et al. 27-Hydroxycholesterol promotes oligodendrocyte maturation: implications for hypercholesterolemia-associated brain white matter changes. Glia 71, 1414–1428 (2023).
Anderson, A. et al. 7-Ketocholesterol in disease and aging. Redox Biol. 29, 101380 (2020).
Mahalakshmi, K. et al. Influential role of 7-ketocholesterol in the progression of Alzheimer’s disease. Prostaglandins Other Lipid Mediat. 156, 106582 (2021).
Cohen, S. Lipid droplets as organelles. Int. Rev. Cell Mol. Biol. 337, 83–110 (2018).
Valm, A. M. et al. Applying systems-level spectral imaging and analysis to reveal the organelle interactome. Nature 546, 162–167 (2017).
Shai, N. et al. Systematic mapping of contact sites reveals tethers and a function for the peroxisome–mitochondria contact. Nat. Commun. 9, 1761 (2018).
Marschallinger, J. et al. Lipid-droplet-accumulating microglia represent a dysfunctional and proinflammatory state in the aging brain. Nat. Neurosci. 23, 194–208 (2020). This paper reveals a novel population of lipid droplet-accumulating microglia in ageing brains, which are dysfunctional, inflammatory and linked to neurodegenerative diseases.
Haney, M. S. et al. APOE4/4 is linked to damaging lipid droplets in Alzheimer’s disease microglia. Nature 628, 154–161 (2024). This paper uncovers a microglial state marked by acyl-CoA synthetase long-chain family member 1 (ACSL1) expression and lipid droplet accumulation in Alzheimer disease, influenced by the APOE4/4 genotype and associated with neurotoxic factors, offering insights into potential therapeutic strategies.
Fanning, S., Selkoe, D. & Dettmer, U. Parkinson’s disease: proteinopathy or lipidopathy? NPJ Parkinson Dis. 6, 3 (2020).
Cantuti-Castelvetri, L. et al. Defective cholesterol clearance limits remyelination in the aged central nervous system. Science 359, 684–688 (2018). This study shows that in aged mice the inability to clear myelin debris due to impaired cholesterol efflux leads to cholesterol crystal formation, inflammasome activation and impaired remyelination, highlighting the role of cholesterol transport in tissue regeneration.
Liu, L. et al. Glial lipid droplets and ROS induced by mitochondrial defects promote neurodegeneration. Cell 160, 177–190 (2015). This paper demonstrates that mitochondrial dysfunction and ROS in neurons lead to lipid droplet accumulation in glial cells, which promotes neurodegeneration, and that targeting lipid peroxidation and ROS can delay disease onset.
Zhu, Y. et al. In vitro exploration of ACAT contributions to lipid droplet formation during adipogenesis. J. Lipid Res. 59, 820–829 (2018).
Sienski, G. et al. APOE4 disrupts intracellular lipid homeostasis in human iPSC-derived glia. Sci. Transl. Med. 13, eaaz4564 (2021).
Victor, M. B. et al. Lipid accumulation induced by APOE4 impairs microglial surveillance of neuronal-network activity. Cell Stem Cell 29, 1197–1212.e8 (2022).
Jarc, E. & Petan, T. A twist of FATe: lipid droplets and inflammatory lipid mediators. Biochimie 169, 69–87 (2020).
Loix, M. et al. Perilipin-2 limits remyelination by preventing lipid droplet degradation. Cell Mol. Life Sci. 79, 515 (2022).
Wang, H. et al. Unique regulation of adipose triglyceride lipase (ATGL) by perilipin 5, a lipid droplet-associated protein. J. Biol. Chem. 286, 15707–15715 (2011).
Khatchadourian, A., Bourque, S. D., Richard, V. R., Titorenko, V. I. & Maysinger, D. Dynamics and regulation of lipid droplet formation in lipopolysaccharide (LPS)-stimulated microglia. Biochim. Biophys. Acta 1821, 607–617 (2012).
Robb, J. L. et al. Blockage of ATGL-mediated breakdown of lipid droplets in microglia alleviates neuroinflammatory and behavioural responses to lipopolysaccharides. Brain Behav. Immun. 123, 315–333 (2025).
Vanherle, S. et al. The ApoA-I mimetic peptide 5A enhances remyelination by promoting clearance and degradation of myelin debris. Cell Rep. 41, 111591 (2022). This paper shows that the ApoA-I mimetic peptide 5A promotes CNS repair by enhancing the clearance and breakdown of myelin debris via the ABCA1–JAK2–STAT3 signalling pathway and fatty acid translocase CD36.
Hofer, P. et al. Cooperative lipolytic control of neuronal triacylglycerol by spastic paraplegia-associated enzyme DDHD2 and ATGL. J. Lipid Res. 64, 100457 (2023).
Schonfeld, P. & Reiser, G. Why does brain metabolism not favor burning of fatty acids to provide energy? Reflections on disadvantages of the use of free fatty acids as fuel for brain. J. Cereb. Blood Flow. Metab. 33, 1493–1499 (2013).
Singh, R. et al. Autophagy regulates lipid metabolism. Nature 458, 1131–1135 (2009).
Griffey, C. J. & Yamamoto, A. Macroautophagy in CNS health and disease. Nat. Rev. Neurosci. 23, 411–427 (2022).
Haidar, M., Loix, M., Bogie, J. F. J. & Hendriks, J. J. A. Lipophagy: a new player in CNS disorders. Trends Endocrinol. Metab. 32, 941–951 (2021).
Nixon, R. A. & Rubinsztein, D. C. Mechanisms of autophagy–lysosome dysfunction in neurodegenerative diseases. Nat. Rev. Mol. Cell Biol. 25, 926–946 (2024).
Haidar, M. et al. Targeting lipophagy in macrophages improves repair in multiple sclerosis. Autophagy 18, 2697–2710 (2022). This study demonstrates that impaired lipophagy contributes to a disease-promoting inflammatory phenotype in foamy phagocytes and shows that stimulating autophagy reduces lipid accumulation and enhances remyelination in mouse multiple sclerosis models.
Tabrizi, S. J., Flower, M. D., Ross, C. A. & Wild, E. J. Huntington disease: new insights into molecular pathogenesis and therapeutic opportunities. Nat. Rev. Neurol. 16, 529–546 (2020).
Rui, Y. N. et al. Huntingtin functions as a scaffold for selective macroautophagy. Nat. Cell Biol. 17, 262–275 (2015).
Kloska, A., Wesierska, M., Malinowska, M., Gabig-Ciminska, M. & Jakobkiewicz-Banecka, J. Lipophagy and lipolysis status in lipid storage and lipid metabolism diseases. Int. J. Mol. Sci. 21, 6113 (2020).
Wong, D. A., Bassilian, S., Lim, S. & Paul Lee, W. N. Coordination of peroxisomal β-oxidation and fatty acid elongation in HepG2 cells. J. Biol. Chem. 279, 41302–41309 (2004).
Cui, W. et al. Lipophagy-derived fatty acids undergo extracellular efflux via lysosomal exocytosis. Autophagy 17, 690–705 (2021).
Ouimet, M. et al. Autophagy regulates cholesterol efflux from macrophage foam cells via lysosomal acid lipase. Cell Metab. 13, 655–667 (2011).
Haemmerle, G. et al. ATGL-mediated fat catabolism regulates cardiac mitochondrial function via PPAR-ɑ and PGC-1. Nat. Med. 17, 1076–1085 (2011).
Mathiowetz, A. J. & Olzmann, J. A. Lipid droplets and cellular lipid flux. Nat. Cell Biol. 26, 331–345 (2024).
Tavasoli, M., Lahire, S., Reid, T., Brodovsky, M. & McMaster, C. R. Genetic diseases of the Kennedy pathways for membrane synthesis. J. Biol. Chem. 295, 17877–17886 (2020).
Gibellini, F. & Smith, T. K. The Kennedy pathway—de novo synthesis of phosphatidylethanolamine and phosphatidylcholine. IUBMB Life 62, 414–428 (2010).
Eichmann, T. O. & Lass, A. DAG tales: the multiple faces of diacylglycerol—stereochemistry, metabolism, and signaling. Cell Mol. Life Sci. 72, 3931–3952 (2015).
Skripuletz, T. et al. Pivotal role of choline metabolites in remyelination. Brain 138, 398–413 (2015).
Magaquian, D., Delgado Ocana, S., Perez, C. & Banchio, C. Phosphatidylcholine restores neuronal plasticity of neural stem cells under inflammatory stress. Sci. Rep. 11, 22891 (2021).
Guttenplan, K. A. et al. Neurotoxic reactive astrocytes induce cell death via saturated lipids. Nature 599, 102–107 (2021).
Mi, Y. et al. Loss of fatty acid degradation by astrocytic mitochondria triggers neuroinflammation and neurodegeneration. Nat. Metab. 5, 445–465 (2023). This paper reveals that impaired mitochondrial oxidative phosphorylation in astrocytes leads to lipid droplet accumulation, neuroinflammation and neurodegeneration, mimicking Alzheimer disease pathology through disrupted fatty acid degradation and intercellular signalling.
Fitz, N. F. et al. Phospholipids of APOE lipoproteins activate microglia in an isoform-specific manner in preclinical models of Alzheimer’s disease. Nat. Commun. 12, 3416 (2021).
Hachem, M., Ahmmed, M. K. & Nacir-Delord, H. Phospholipidomics in clinical trials for brain disorders: advancing our understanding and therapeutic potentials. Mol. Neurobiol. 61, 3272–3295 (2024).
Schutter, M., Giavalisco, P., Brodesser, S. & Graef, M. Local fatty acid channeling into phospholipid synthesis drives phagophore expansion during autophagy. Cell 180, 135–149.e14 (2020).
Kim, J. W., Lee, J. Y., Oh, M. & Lee, E. W. An integrated view of lipid metabolism in ferroptosis revisited via lipidomic analysis. Exp. Mol. Med. 55, 1620–1631 (2023).
Bazinet, R. P., Rao, J. S., Chang, L., Rapoport, S. I. & Lee, H. J. Chronic carbamazepine decreases the incorporation rate and turnover of arachidonic acid but not docosahexaenoic acid in brain phospholipids of the unanesthetized rat: relevance to bipolar disorder. Biol. Psychiatry 59, 401–407 (2006).
Bazinet, R. P., Rao, J. S., Chang, L., Rapoport, S. I. & Lee, H. J. Chronic valproate does not alter the kinetics of docosahexaenoic acid within brain phospholipids of the unanesthetized rat. Psychopharmacology 182, 180–185 (2005).
Lee, H. J. et al. Topiramate does not alter the kinetics of arachidonic or docosahexaenoic acid in brain phospholipids of the unanesthetized rat. Neurochem. Res. 30, 677–683 (2005).
Cunningham, T. J. et al. Secreted phospholipase A2 activity in experimental autoimmune encephalomyelitis and multiple sclerosis. J. Neuroinflammation 3, 26 (2006).
Lee, G., Kang, G.-H. & Bae, H. Bee venom phospholipase A2 suppression of experimental autoimmune encephalomyelitis is dependent on its enzymatic activity. Mol. Cell. Toxicol. 15, 307–313 (2019).
Chung, E. S. et al. Neuro-protective effects of bee venom by suppression of neuroinflammatory responses in a mouse model of Parkinson’s disease: role of regulatory T cells. Brain Behav. Immun. 26, 1322–1330 (2012).
Kim, K. H. et al. Dose-dependent neuroprotective effect of standardized bee venom phospholipase A2 against MPTP-induced Parkinson’s disease in mice. Front. Aging Neurosci. 11, 80 (2019).
Sagy-Bross, C. et al. The role of cytosolic phospholipase A2ɑ in amyloid precursor protein induction by amyloid β1–42: implication for neurodegeneration. J. Neurochem. 132, 559–571 (2015).
Sanchez-Mejia, R. O. et al. Phospholipase A2 reduction ameliorates cognitive deficits in a mouse model of Alzheimer’s disease. Nat. Neurosci. 11, 1311–1318 (2008).
Ham, H. J. et al. Bee venom phospholipase A2 ameliorates amyloidogenesis and neuroinflammation through inhibition of signal transducer and activator of transcription-3 pathway in Tg2576 mice. Transl. Neurodegener. 8, 26 (2019).
Sumi-Akamaru, H. et al. High expression of ɑ-synuclein in damaged mitochondria with PLA2G6 dysfunction. Acta Neuropathol. Commun. 4, 27 (2016).
Lin, G. et al. Phospholipase PLA2G6, a parkinsonism-associated gene, affects Vps26 and Vps35, retromer function, and ceramide levels, similar to ɑ-synuclein gain. Cell Metab. 28, 605–618.e6 (2018).
Mori, A. et al. Parkinson’s disease-associated iPLA2-VIA/PLA2G6 regulates neuronal functions and ɑ-synuclein stability through membrane remodeling. Proc. Natl Acad. Sci. USA 116, 20689–20699 (2019).
Morgan, N. V. et al. PLA2G6, encoding a phospholipase A2, is mutated in neurodegenerative disorders with high brain iron. Nat. Genet. 38, 752–754 (2006).
Lu, C. S. et al. PLA2G6 mutations in PARK14-linked young-onset parkinsonism and sporadic Parkinson’s disease. Am. J. Med. Genet. B Neuropsychiatr. Genet 159B, 183–191 (2012).
Kalyvas, A. et al. Differing roles for members of the phospholipase A2 superfamily in experimental autoimmune encephalomyelitis. Brain 132, 1221–1235 (2009).
Khan, S. A. & Ilies, M. A. The phospholipase A2 superfamily: structure, isozymes, catalysis, physiologic and pathologic roles. Int. J. Mol. Sci. 24, 1353 (2023).
Nicholatos, J. W., Tran, D., Liu, Y., Hirst, W. D. & Weihofen, A. Lysophosphatidylcholine acyltransferase 1 promotes pathology and toxicity in two distinct cell-based ɑ-synuclein models. Neurosci. Lett. 772, 136491 (2022).
Eto, M., Shindou, H., Yamamoto, S., Tamura-Nakano, M. & Shimizu, T. Lysophosphatidylethanolamine acyltransferase 2 (LPEAT2) incorporates DHA into phospholipids and has possible functions for fatty acid-induced cell death. Biochem. Biophys. Res. Commun. 526, 246–252 (2020).
Bargui, R. et al. Phospholipids: identification and implication in muscle pathophysiology. Int. J. Mol. Sci. 22, 8176 (2021).
Yin, J. et al. Brain-specific lipoprotein receptors interact with astrocyte derived apolipoprotein and mediate neuron–glia lipid shuttling. Nat. Commun. 12, 2408 (2021).
Mauch, D. H. et al. CNS synaptogenesis promoted by glia-derived cholesterol. Science 294, 1354–1357 (2001).
Barnes-Velez, J. A., Aksoy Yasar, F. B. & Hu, J. Myelin lipid metabolism and its role in myelination and myelin maintenance. Innovation 4, 100360 (2023).
Jackson, R. J., Hyman, B. T. & Serrano-Pozo, A. Multifaceted roles of APOE in Alzheimer disease. Nat. Rev. Neurol. 20, 457–474 (2024).
Hayashi, H., Campenot, R. B., Vance, D. E. & Vance, J. E. Glial lipoproteins stimulate axon growth of central nervous system neurons in compartmented cultures. J. Biol. Chem. 279, 14009–14015 (2004).
Szrok-Jurga, S. et al. The role of acyl-CoA β-oxidation in brain metabolism and neurodegenerative diseases. Int. J. Mol. Sci. 24, 13977 (2023).
Chen, Y., Strickland, M. R., Soranno, A. & Holtzman, D. M. Apolipoprotein E: structural insights and links to Alzheimer disease pathogenesis. Neuron 109, 205–221 (2021).
Mahley, R. W. Central nervous system lipoproteins: ApoE and regulation of cholesterol metabolism. Arterioscler. Thromb. Vasc. Biol. 36, 1305–1315 (2016).
van Deijk, A. F. et al. Astrocyte lipid metabolism is critical for synapse development and function in vivo. Glia 65, 670–682 (2017).
Ferris, H. A. et al. Loss of astrocyte cholesterol synthesis disrupts neuronal function and alters whole-body metabolism. Proc. Natl Acad. Sci. USA 114, 1189–1194 (2017).
Valenza, M. et al. Disruption of astrocyte–neuron cholesterol cross talk affects neuronal function in Huntington’s disease. Cell Death Differ. 22, 690–702 (2015). This study demonstrates that impaired cholesterol biosynthesis and secretion by astrocytes in Huntington disease disrupts astrocyte–neuron communication and neuronal function, suggesting that targeting astrocyte-mediated cholesterol homeostasis could offer therapeutic potential.
Liu, L., MacKenzie, K. R., Putluri, N., Maletic-Savatic, M. & Bellen, H. J. The glia–neuron lactate shuttle and elevated ROS promote lipid synthesis in neurons and lipid droplet accumulation in glia via APOE/D. Cell Metab. 26, 719–737.e6 (2017). This study reveals that ROS-induced lipid formation in neurons, mediated by lactate transfer, fatty acid transport proteins and apolipoproteins, contributes to glial lipid droplet accumulation, and that impaired lipid transport via APOE4 promotes neurodegeneration, offering insights into Alzheimer disease mechanisms.
Qi, G. et al. ApoE4 impairs neuron–astrocyte coupling of fatty acid metabolism. Cell Rep. 34, 108572 (2021).
Ioannou, M. S. et al. Neuron–astrocyte metabolic coupling protects against activity-induced fatty acid toxicity. Cell 177, 1522–1535.e14 (2019). This paper shows that toxic fatty acids produced by hyperactive neurons are transferred to astrocytes via APOE-positive lipid particles, where they are detoxified through mitochondrial β-oxidation, highlighting a coordinated metabolic mechanism between neurons and astrocytes to protect against fatty acid toxicity during increased neural activity.
Targa Dias Anastacio, H., Matosin, N. & Ooi, L. Neuronal hyperexcitability in Alzheimer’s disease: what are the drivers behind this aberrant phenotype? Transl. Psychiatry 12, 257 (2022).
Haba, K., Ogawa, N., Mizukawa, K. & Mori, A. Time course of changes in lipid peroxidation, pre- and postsynaptic cholinergic indices, NMDA receptor binding and neuronal death in the gerbil hippocampus following transient ischemia. Brain Res. 540, 116–122 (1991).
Parihar, M. S. & Hemnani, T. Experimental excitotoxicity provokes oxidative damage in mice brain and attenuation by extract of Asparagus racemosus. J. Neural Transm. 111, 1–12 (2004).
Haynes, P. R. et al. A neuron–glia lipid metabolic cycle couples daily sleep to mitochondrial homeostasis. Nat. Neurosci. 27, 666–678 (2024). This paper demonstrates that sleep facilitates lipid clearance and mitochondrial recovery in glia of Drosophila, supporting brain energy homeostasis through neuron-to-glia lipid transfer.
Nitz, D. A., van Swinderen, B., Tononi, G. & Greenspan, R. J. Electrophysiological correlates of rest and activity in Drosophila melanogaster. Curr. Biol. 12, 1934–1940 (2002).
Liddelow, S. A. et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature 541, 481–487 (2017).
Guttenplan, K. A. et al. Neurotoxic reactive astrocytes drive neuronal death after retinal injury. Cell Rep. 31, 107776 (2020).
Lindner, K. et al. Isoform- and cell-state-specific lipidation of ApoE in astrocytes. Cell Rep. 38, 110435 (2022).
Franklin, R. J. & Ffrench-Constant, C. Remyelination in the CNS: from biology to therapy. Nat. Rev. Neurosci. 9, 839–855 (2008).
Voskuhl, R. R. et al. Gene expression in oligodendrocytes during remyelination reveals cholesterol homeostasis as a therapeutic target in multiple sclerosis. Proc. Natl Acad. Sci. USA 116, 10130–10139 (2019).
Khandker, L. et al. Cholesterol biosynthesis defines oligodendrocyte precursor heterogeneity between brain and spinal cord. Cell Rep. 38, 110423 (2022). This study reveals that brain and spinal cord oligodendroglia have distinct transcriptional profiles, with mTOR acting as a key regulator of cholesterol biosynthesis, essential for developmental myelination and myelin maintenance in the adult brain.
Berghoff, S. A. et al. Microglia facilitate repair of demyelinated lesions via post-squalene sterol synthesis. Nat. Neurosci. 24, 47–60 (2021).
O’Brien, J. S. Stability of the myelin membrane. Science 147, 1099–1107 (1965).
Grajchen, E., Hendriks, J. J. A. & Bogie, J. F. J. The physiology of foamy phagocytes in multiple sclerosis. Acta Neuropathol. Commun. 6, 124 (2018).
Mailleux, J. et al. Active liver X receptor signaling in phagocytes in multiple sclerosis lesions. Mult. Scler. 24, 279–289 (2018).
Bogie, J. F. et al. Myelin-derived lipids modulate macrophage activity by liver X receptor activation. PLoS ONE 7, e44998 (2012).
Spann, N. J. et al. Regulated accumulation of desmosterol integrates macrophage lipid metabolism and inflammatory responses. Cell 151, 138–152 (2012).
Zhang, R. et al. Enhanced liver X receptor signalling reduces brain injury and promotes tissue regeneration following experimental intracerebral haemorrhage: roles of microglia/macrophages. Stroke Vasc. Neurol. 8, 486–502 (2023).
Ruckh, J. M. et al. Rejuvenation of regeneration in the aging central nervous system. Cell Stem Cell 10, 96–103 (2012).
Natrajan, M. S. et al. Retinoid X receptor activation reverses age-related deficiencies in myelin debris phagocytosis and remyelination. Brain 138, 3581–3597 (2015).
Franklin, R. J. M., Frisen, J. & Lyons, D. A. Revisiting remyelination: towards a consensus on the regeneration of CNS myelin. Semin. Cell Dev. Biol. 116, 3–9 (2021).
Lampron, A. et al. Inefficient clearance of myelin debris by microglia impairs remyelinating processes. J. Exp. Med. 212, 481–495 (2015).
Berghoff, S. A. et al. Dietary cholesterol promotes repair of demyelinated lesions in the adult brain. Nat. Commun. 8, 14241 (2017). This paper demonstrates that dietary cholesterol supports remyelination by promoting OPC differentiation, restoring growth factor balance and enhancing repair in demyelination mouse models.
Camargo, N. et al. Oligodendroglial myelination requires astrocyte-derived lipids. PLoS Biol. 15, e1002605 (2017). This paper shows that astrocytes significantly contribute to lipid synthesis for myelination in the CNS, supplementing lipid synthesis by oligodendrocytes during brain development and highlighting the importance of horizontal lipid flux for normal myelination.
Molina-Gonzalez, I. et al. Astrocyte–oligodendrocyte interaction regulates central nervous system regeneration. Nat. Commun. 14, 3372 (2023). This study demonstrates that astrocyte–oligodendrocyte interactions, specifically involving astrocytic cholesterol biosynthesis and NRF2 pathway regulation, are crucial for remyelination, and identifies a potential therapeutic strategy targeting this interaction to promote CNS repair.
Tanaka, Y. et al. NF-E2-related factor 2 inhibits lipid accumulation and oxidative stress in mice fed a high-fat diet. J. Pharmacol. Exp. Ther. 325, 655–664 (2008).
Levings, D. C., Pathak, S. S., Yang, Y. M. & Slattery, M. Limited expression of Nrf2 in neurons across the central nervous system. Redox Biol. 65, 102830 (2023).
Vanherle, S., Haidar, M., Irobi, J., Bogie, J. F. J. & Hendriks, J. J. A. Extracellular vesicle-associated lipids in central nervous system disorders. Adv. Drug. Deliv. Rev. 159, 322–331 (2020).
Lombardi, M. et al. Detrimental and protective action of microglial extracellular vesicles on myelin lesions: astrocyte involvement in remyelination failure. Acta Neuropathol. 138, 987–1012 (2019).
Lombardi, M. et al. Extracellular vesicles released by microglia and macrophages carry endocannabinoids which foster oligodendrocyte differentiation. Front. Immunol. 15, 1331210 (2024).
Yuana, Y., Levels, J., Grootemaat, A., Sturk, A. & Nieuwland, R. Co-isolation of extracellular vesicles and high-density lipoproteins using density gradient ultracentrifugation. J Extracell Vesicles https://doi.org/10.3402/jev.v3.23262 (2014).
Wang, G. et al. Astrocytes secrete exosomes enriched with proapoptotic ceramide and prostate apoptosis response 4 (PAR-4): potential mechanism of apoptosis induction in Alzheimer disease (AD). J. Biol. Chem. 287, 21384–21395 (2012).
Yuyama, K. et al. A potential function for neuronal exosomes: sequestering intracerebral amyloid-β peptide. FEBS Lett. 589, 84–88 (2015).
Yuyama, K. et al. Decreased amyloid-β pathologies by intracerebral loading of glycosphingolipid-enriched exosomes in Alzheimer model mice. J. Biol. Chem. 289, 24488–24498 (2014).
Yuyama, K., Sun, H., Mitsutake, S. & Igarashi, Y. Sphingolipid-modulated exosome secretion promotes clearance of amyloid-β by microglia. J. Biol. Chem. 287, 10977–10989 (2012).
Yuyama, K., Mitsutake, S. & Igarashi, Y. Pathological roles of ceramide and its metabolites in metabolic syndrome and Alzheimer’s disease. Biochim. Biophys. Acta 1841, 793–798 (2014).
Kurzawa-Akanbi, M. et al. Altered ceramide metabolism is a feature in the extracellular vesicle-mediated spread of ɑ-synuclein in Lewy body disorders. Acta Neuropathol. 142, 961–984 (2021).
Grey, M. et al. Acceleration of α-synuclein aggregation by exosomes. J. Biol. Chem. 290, 2969–2982 (2015).
Kopatz, V. et al. Micro- and nanoplastics breach the blood–brain barrier (BBB): biomolecular corona’s role revealed. Nanomaterials 13, 1404 (2023).
Hu, M. & Palic, D. Micro- and nano-plastics activation of oxidative and inflammatory adverse outcome pathways. Redox Biol. 37, 101620 (2020).
Prust, M., Meijer, J. & Westerink, R. H. S. The plastic brain: neurotoxicity of micro- and nanoplastics. Part. Fibre Toxicol. 17, 24 (2020).
Min, H., Yang, Y. Y. & Yang, Y. Cold induces brain region-selective neuronal activity-dependent lipid metabolism. eLife 13, RP98353 (2024).
Leiria, L. O. et al. 12-Lipoxygenase regulates cold adaptation and glucose metabolism by producing the ω-3 lipid 12-HEPE from brown fat. Cell Metab. 30, 768–783.e7 (2019).
Marcher, A. B. et al. RNA-seq and mass-spectrometry-based lipidomics reveal extensive changes of glycerolipid pathways in brown adipose tissue in response to cold. Cell Rep. 13, 2000–2013 (2015).
Chen, W. et al. Cold exposure alters lipid metabolism of skeletal muscle through HIF-1ɑ-induced mitophagy. BMC Biol. 21, 27 (2023).
Huang, D. et al. Cold exposure impairs extracellular vesicle swarm-mediated nasal antiviral immunity. J. Allergy Clin. Immunol. 151, 509–525.e8 (2023).
Briaud, P. et al. Temperature influences the composition and cytotoxicity of extracellular vesicles in Staphylococcus aureus. mSphere 6, e0067621 (2021).
Jaroslawska, J., Gospodarska, E. & Korytko, A. Increasing energy expenditure through exercise and low ambient temperature offers oxidative protection to the hypothalamus after high-fat feeding to mice. J. Neuroendocrinol. 34, e13095 (2022).
Dias, S. S. G. et al. Metabolic reprogramming and lipid droplets are involved in Zika virus replication in neural cells. J. Neuroinflammation 20, 61 (2023).
Monson, E. A. et al. Intracellular lipid droplet accumulation occurs early following viral infection and is required for an efficient interferon response. Nat. Commun. 12, 4303 (2021).
Matveeva, O. et al. Western lifestyle and immunopathology of multiple sclerosis. Ann. N. Y. Acad. Sci. 1417, 71–86 (2018).
Custers, Emma, E. M., Kiliaan & Amanda, J. Dietary lipids from body to brain. Prog. Lipid Res. 85, 101144 (2022).
Bosch-Queralt, M. et al. Diet-dependent regulation of TGFβ impairs reparative innate immune responses after demyelination. Nat. Metab. 3, 211–227 (2021).
Liemisa, B. et al. Brain apolipoprotein E levels in mice challenged by a Western diet increase in an allele-dependent manner. Aging Brain 4, 100102 (2023).
Li, Q. et al. Impaired lipophagy induced-microglial lipid droplets accumulation contributes to the buildup of TREM1 in diabetes-associated cognitive impairment. Autophagy 19, 2639–2656 (2023).
Morselli, E., Criollo, A., Rodriguez-Navas, C. & Clegg, D. J. Chronic high fat diet consumption impairs metabolic health of male mice. Inflamm. Cell Signal. 1, e561 (2014).
Tan, B. L. & Norhaizan, M. E. Effect of high-fat diets on oxidative stress, cellular inflammatory response and cognitive function. Nutrients 11, 2579 (2019).
Lee, J. C. et al. High-fat diet-induced lipidome perturbations in the cortex, hippocampus, hypothalamus, and olfactory bulb of mice. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 1863, 980–990 (2018).
Mattson, M. P., Moehl, K., Ghena, N., Schmaedick, M. & Cheng, A. Intermittent metabolic switching, neuroplasticity and brain health. Nat. Rev. Neurosci. 19, 63–80 (2018).
Logan, R. W. & McClung, C. A. Rhythms of life: circadian disruption and brain disorders across the lifespan. Nat. Rev. Neurosci. 20, 49–65 (2019).
Lee, C. H., Murrell, C. E., Chu, A. & Pan, X. Circadian regulation of apolipoproteins in the brain: implications in lipid metabolism and disease. Int. J. Mol. Sci. 24, 17415 (2023).
Sheehan, P. W. et al. A glial circadian gene expression atlas reveals cell type and disease-specific reprogramming in response to amyloid pathology or aging. Preprint at bioRxiv https://doi.org/10.1101/2024.05.28.596297 (2024).
Matsumoto, K. et al. Psychological stress-induced enhancement of brain lipid peroxidation via nitric oxide systems and its modulation by anxiolytic and anxiogenic drugs in mice. Brain Res. 839, 74–84 (1999).
Lee, H., Park, J. & Kim, S. Metabolic and transcriptomic signatures of the acute psychological stress response in the mouse brain. Metabolites 13, 453 (2023).
von Ziegler, L. M. et al. Multiomic profiling of the acute stress response in the mouse hippocampus. Nat. Commun. 13, 1824 (2022). This study uses multiomic profiling to characterize the acute stress response in the mouse hippocampus, revealing complex, time-regulated molecular events that resolve within hours, providing insights into how acute stress impacts brain function.
Salvador, A. F., Shyu, C. R. & Parks, E. J. Measurement of lipid flux to advance translational research: evolution of classic methods to the future of precision health. Exp. Mol. Med. 54, 1348–1353 (2022).
Ellis, S. R. et al. Mass spectrometry imaging of phosphatidylcholine metabolism in lungs administered with therapeutic surfactants and isotopic tracers. J. Lipid Res. 62, 100023 (2021).
Bowman, A. P. et al. Evaluation of lipid coverage and high spatial resolution MALDI-imaging capabilities of oversampling combined with laser post-ionisation. Anal. BioAnal. Chem. 412, 2277–2289 (2020).
Chen, T., Yavuz, A. & Wang, M. C. Dissecting lipid droplet biology with coherent Raman scattering microscopy. J. Cell Sci. 135, jcs.252353 (2022).
Uematsu, M. & Shimizu, T. Raman microscopy-based quantification of the physical properties of intracellular lipids. Commun. Biol. 4, 1176 (2021).
Folick, A., Min, W. & Wang, M. C. Label-free imaging of lipid dynamics using coherent anti-Stokes Raman scattering (CARS) and stimulated raman scattering (SRS) microscopy. Curr. Opin. Genet. Dev. 21, 585–590 (2011).
Shi, L. & Tu, B. P. Acetyl-CoA and the regulation of metabolism: mechanisms and consequences. Curr. Opin. Cell Biol. 33, 125–131 (2015).
Morita, S. Y. & Terada, T. Enzymatic measurement of phosphatidylglycerol and cardiolipin in cultured cells and mitochondria. Sci. Rep. 5, 11737 (2015).
Stone, S. J. et al. The endoplasmic reticulum enzyme DGAT2 is found in mitochondria-associated membranes and has a mitochondrial targeting signal that promotes its association with mitochondria. J. Biol. Chem. 284, 5352–5361 (2009).
Huitema, K., van den Dikkenberg, J., Brouwers, J. F. & Holthuis, J. C. Identification of a family of animal sphingomyelin synthases. EMBO J. 23, 33–44 (2004).
Hanada, K., Kumagai, K., Tomishige, N. & Yamaji, T. CERT-mediated trafficking of ceramide. Biochim. Biophys. Acta 1791, 684–691 (2009).
Honsho, M., Tanaka, M., Zoeller, R. A. & Fujiki, Y. Distinct functions of acyl/alkyl dihydroxyacetonephosphate reductase in peroxisomes and endoplasmic reticulum. Front. Cell Dev. Biol. 8, 855 (2020).
Schlame, M. & Haldar, D. Cardiolipin is synthesized on the matrix side of the inner membrane in rat liver mitochondria. J. Biol. Chem. 268, 74–79 (1993).
Rusiñol, A. E., Cui, Z., Chen, M. H. & Vance, J. E. A unique mitochondria-associated membrane fraction from rat liver has a high capacity for lipid synthesis and contains pre-Golgi secretory proteins including nascent lipoproteins. J. Biol. Chem. 269, 27494–27502 (1994).
Kinney, A. J. & Carman, G. M. Enzymes of phosphoinositide synthesis in secretory vesicles destined for the plasma membrane in Saccharomyces cerevisiae. J. Bacteriol. 172, 4115–4117 (1990).
Gaigg, B., Simbeni, R., Hrastnik, C., Paltauf, F. & Daum, G. Characterization of a microsomal subfraction associated with mitochondria of the yeast, Saccharomyces cerevisiae. Involvement in synthesis and import of phospholipids into mitochondria. Biochim. Biophys. Acta 1234, 214–220 (1995).
O’Donnell, V. B. New appreciation for an old pathway: the Lands cycle moves into new arenas in health and disease. Biochem. Soc. Trans. 50, 1–11 (2022).
Ferrara, P. J. et al. Lysophospholipid acylation modulates plasma membrane lipid organization and insulin sensitivity in skeletal muscle. J. Clin. Invest. 131, e135963 (2021).
Kamp, F. & Hamilton, J. A. pH gradients across phospholipid membranes caused by fast flip-flop of un-ionized fatty acids. Proc. Natl Acad. Sci. USA 89, 11367–11370 (1992).
Chen, C. T., Ma, D. W., Kim, J. H., Mount, H. T. & Bazinet, R. P. The low density lipoprotein receptor is not necessary for maintaining mouse brain polyunsaturated fatty acid concentrations. J. Lipid Res. 49, 147–152 (2008).
Mitchell, R. W., On, N. H., Del Bigio, M. R., Miller, D. W. & Hatch, G. M. Fatty acid transport protein expression in human brain and potential role in fatty acid transport across human brain microvessel endothelial cells. J. Neurochem. 117, 735–746 (2011).
Mitchell, R. W., Edmundson, C. L., Miller, D. W. & Hatch, G. M. On the mechanism of oleate transport across human brain microvessel endothelial cells. J. Neurochem. 110, 1049–1057 (2009).
Pan, Y. et al. Fatty acid-binding protein 5 facilitates the blood–brain barrier transport of docosahexaenoic acid. Mol. Pharm. 12, 4375–4385 (2015).
Ochiai, Y. et al. The blood–brain barrier fatty acid transport protein 1 (FATP1/SLC27A1) supplies docosahexaenoic acid to the brain, and insulin facilitates transport. J. Neurochem. 141, 400–412 (2017).
Pan, Y. et al. Fatty acid-binding protein 5 at the blood–brain barrier regulates endogenous brain docosahexaenoic acid levels and cognitive function. J. Neurosci. 36, 11755–11767 (2016).
Nguyen, L. N. et al. Mfsd2a is a transporter for the essential ω-3 fatty acid docosahexaenoic acid. Nature 509, 503–506 (2014).
Cater, R. J. et al. Structural basis of ω-3 fatty acid transport across the blood–brain barrier. Nature 595, 315–319 (2021).
Fernandez, R. F. et al. Acyl-CoA synthetase 6 enriches the neuroprotective ω-3 fatty acid DHA in the brain. Proc. Natl Acad. Sci. USA 115, 12525–12530 (2018).
Oldendorf, W. H. Carrier-mediated blood–brain barrier transport of short-chain monocarboxylic organic acids. Am. J. Physiol. 224, 1450–1453 (1973).
Sun, J. et al. Clostridium butyricum pretreatment attenuates cerebral ischemia/reperfusion injury in mice via anti-oxidation and anti-apoptosis. Neurosci. Lett. 613, 30–35 (2016).
Vijay, N. & Morris, M. E. Role of monocarboxylate transporters in drug delivery to the brain. Curr. Pharm. Des. 20, 1487–1498 (2014).
Dalile, B., Van Oudenhove, L., Vervliet, B. & Verbeke, K. The role of short-chain fatty acids in microbiota–gut–brain communication. Nat. Rev. Gastroenterol. Hepatol. 16, 461–478 (2019).
Chen, J., Zhang, X., Kusumo, H., Costa, L. G. & Guizzetti, M. Cholesterol efflux is differentially regulated in neurons and astrocytes: implications for brain cholesterol homeostasis. Biochim. Biophys. Acta 1831, 263–275 (2013).
Kim, W. S., Weickert, C. S. & Garner, B. Role of ATP-binding cassette transporters in brain lipid transport and neurological disease. J. Neurochem. 104, 1145–1166 (2008).
Flowers, S. A. & Rebeck, G. W. APOE in the normal brain. Neurobiol. Dis. 136, 104724 (2020).
Chen, J., Li, Q. & Wang, J. Topology of human apolipoprotein E3 uniquely regulates its diverse biological functions. Proc. Natl Acad. Sci. USA 108, 14813–14818 (2011).
Feringa, F. M. & van der Kant, R. Cholesterol and Alzheimer’s disease; from risk genes to pathological effects. Front. Aging Neurosci. 13, 690372 (2021).
Raulin, A. C., Martens, Y. A. & Bu, G. Lipoproteins in the central nervous system: from biology to pathobiology. Annu. Rev. Biochem. 91, 731–759 (2022).
Bohlen, C. J. et al. Diverse requirements for microglial survival, specification, and function revealed by defined-medium cultures. Neuron 94, 759–773.e8 (2017).
Yeh, F. L., Wang, Y., Tom, I., Gonzalez, L. C. & Sheng, M. TREM2 binds to apolipoproteins, including APOE and CLU/APOJ, and thereby facilitates uptake of amyloid-β by microglia. Neuron 91, 328–340 (2016).
Saher, G. & Stumpf, S. K. Cholesterol in myelin biogenesis and hypomyelinating disorders. Biochim. Biophys. Acta 1851, 1083–1094 (2015).
Liu, C. C., Liu, C. C., Kanekiyo, T., Xu, H. & Bu, G. Apolipoprotein E and Alzheimer disease: risk, mechanisms and therapy. Nat. Rev. Neurol. 9, 106–118 (2013).
Tcw, J. et al. Cholesterol and matrisome pathways dysregulated in astrocytes and microglia. Cell 185, 2213–2233.e25 (2022).
Farmer, B. C., Kluemper, J. & Johnson, L. A. Apolipoprotein E4 alters astrocyte fatty acid metabolism and lipid droplet formation. Cells 8, 182 (2019).
Hu, J. et al. Opposing effects of viral mediated brain expression of apolipoprotein E2 (apoE2) and apoE4 on apoE lipidation and Aβ metabolism in apoE4-targeted replacement mice. Mol. Neurodegener. 10, 6 (2015).
Heinsinger, N. M., Gachechiladze, M. A. & Rebeck, G. W. Apolipoprotein E genotype affects size of ApoE complexes in cerebrospinal fluid. J. Neuropathol. Exp. Neurol. 75, 918–924 (2016).
Rawat, V. et al. ApoE4 alters ABCA1 membrane trafficking in astrocytes. J. Neurosci. 39, 9611–9622 (2019).
Zhao, J. et al. APOE ε4/ε4 diminishes neurotrophic function of human iPSC-derived astrocytes. Hum. Mol. Genet. 26, 2690–2700 (2017).
Arboleda-Velasquez, J. F. et al. Resistance to autosomal dominant Alzheimer’s disease in an APOE3 Christchurch homozygote: a case report. Nat. Med. 25, 1680–1683 (2019).
Blanchard, J. W. et al. APOE4 impairs myelination via cholesterol dysregulation in oligodendrocytes. Nature 611, 769–779 (2022).
Ulrich, J. D. & Holtzman, D. M. TREM2 function in Alzheimer’s disease and neurodegeneration. ACS Chem. Neurosci. 7, 420–427 (2016).
Zhou, Y. et al. Human and mouse single-nucleus transcriptomics reveal TREM2-dependent and TREM2-independent cellular responses in Alzheimer’s disease. Nat. Med. 26, 131–142 (2020).
Leyns, C. E. G. et al. TREM2 function impedes tau seeding in neuritic plaques. Nat. Neurosci. 22, 1217–1222 (2019).
Keren-Shaul, H. et al. A unique microglia type associated with restricting development of Alzheimer’s disease. Cell 169, 1276–1290.e17 (2017).
Yuan, P. et al. TREM2 haplodeficiency in mice and humans impairs the microglia barrier function leading to decreased amyloid compaction and severe axonal dystrophy. Neuron 90, 724–739 (2016).
Nugent, A. A. et al. TREM2 regulates microglial cholesterol metabolism upon chronic phagocytic challenge. Neuron 105, 837–854.e9 (2020).
Rustom, A., Saffrich, R., Markovic, I., Walther, P. & Gerdes, H. H. Nanotubular highways for intercellular organelle transport. Science 303, 1007–1010 (2004).
Scheiblich, H. et al. Microglia jointly degrade fibrillar ɑ-synuclein cargo by distribution through tunneling nanotubes. Cell 184, 5089–5106.e21 (2021).
Chakraborty, R., Nonaka, T., Hasegawa, M. & Zurzolo, C. Tunnelling nanotubes between neuronal and microglial cells allow bi-directional transfer of ɑ-synuclein and mitochondria. Cell Death Dis. 14, 329 (2023).
Chastagner, P. et al. Fate and propagation of endogenously formed Tau aggregates in neuronal cells. EMBO Mol. Med. 12, e12025 (2020).
Victoria, G. S., Arkhipenko, A., Zhu, S., Syan, S. & Zurzolo, C. Astrocyte-to-neuron intercellular prion transfer is mediated by cell–cell contact. Sci. Rep. 6, 20762 (2016).
Victoria, G. S. & Zurzolo, C. The spread of prion-like proteins by lysosomes and tunneling nanotubes: implications for neurodegenerative diseases. J. Cell Biol. 216, 2633–2644 (2017).
Astanina, K., Koch, M., Jungst, C., Zumbusch, A. & Kiemer, A. K. Lipid droplets as a novel cargo of tunnelling nanotubes in endothelial cells. Sci. Rep. 5, 11453 (2015).
Acknowledgements
The authors thank all members of the Bogie, Hendriks and Miron laboratories for the discussions. The research of S.V. is funded by the FWO Vlaanderen (1246724N) and Charcot Research Foundation (CHARCO24VS). V.E.M is funded by the John David Eaton Chair in Multiple Sclerosis Research (Barlo MS Centre, St. Michael’s Hospital Foundation), the Sloan-Hall MS Basic Research Fund, MS Canada and a Senior Non-Clinical Research Fellowship from the Medical Research Council. J.J.A.H is funded by the Research Foundation of Flanders (FWO Vlaanderen; G0A7922, G0A7922, S01623N) and the Charcot Research Foundation (CHARCO23HJ, CHARCO24HJ). J.F.J.B is funded by the Research Foundation of Flanders (FWO Vlaanderen; G075823, G0A3B24), Charcot Research Foundation (CHARCO23BJ, CHARCO24BJ), Geneeskundige Stichting Koningin Elisabeth (G.S.K.E; GSKE-BOGJ), MS Liga Vlaanderen (MSLIGABOGJ) and the special research fund Hasselt University (22DOC38BOF, 23INC06BOF).
Author information
Authors and Affiliations
Contributions
J.F.J.B. and S.V. contributed substantially to discussion of the content. All authors wrote the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neuroscience thanks Mark Verheijen, Fei Yin and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Glossary
- β-Oxidation
-
The metabolic pathway that breaks down fatty acids (FAs) into acetyl-CoA units in the mitochondria for energy production.
- Autophagy
-
A cellular process in which damaged or unnecessary components of the cell are degraded and recycled within the cell through lysosomal activity.
- Cholesterol
-
A lipid molecule synthesized in all cell types, essential for cell membrane structure, hormone synthesis and bile acid formation.
- Extracellular vesicles
-
(EVs). Nanosized lipid bilayer particles secreted by cells that carry lipids, proteins and RNA to distant and nearby cells, playing a key role in intercellular communication.
- Fatty acid
-
(FA). A carboxylic acid consisting of a hydrocarbon chain and a terminal carboxyl group, essential for energy storage and membrane structure.
- Lipid droplets
-
Intracellular storage organelles primarily composed of neutral lipids such as triglycerides, serving as energy reserves.
- Lipidome
-
The complete set of lipids in a biological system, encompassing various lipid classes.
- Lipoproteins
-
Complexes of lipids and proteins with a hydrophobic core that transport lipids, such as cholesterol and triglycerides, through the bloodstream.
- Monounsaturated fatty acids
-
(MUFAs). Fatty acids (FAs) with one unsaturated carbon bond in their hydrocarbon chain, commonly found in olive oil and avocados.
- Phospholipids
-
Lipids containing a phosphate group, forming the structural components of cell membranes.
- Polyunsaturated fatty acids
-
(PUFAs). Fatty acids (FAs) with two or more double bonds in their hydrocarbon chain, important for membrane fluidity and signalling.
- Saturated fatty acids
-
(SFAs). Fatty acids (FAs) with no double bonds in their hydrocarbon chain, typically solid at room temperature and found in animal fats.
- Tracer lipidomics
-
A method for studying lipid metabolism by tracking the incorporation of labelled lipid precursors into biological systems.
- Western diet
-
A dietary pattern high in processed foods, fats (such as saturated fats and cholesterol) and sugars, and low in fibre, commonly associated with various chronic diseases.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vanherle, S., Loix, M., Miron, V.E. et al. Lipid metabolism, remodelling and intercellular transfer in the CNS. Nat. Rev. Neurosci. 26, 214–231 (2025). https://doi.org/10.1038/s41583-025-00908-3
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41583-025-00908-3
This article is cited by
-
Multi-omics characterized the effects of Akkermansia muciniphila and fecal microbiota transplant on the microglial activation after traumatic brain injury
BMC Microbiology (2026)
-
Signaling roles for astrocytic lipid metabolism in brain function
EMBO Reports (2026)
-
Brain lipid metabolism and transport: implications for neurodegeneration and therapeutic strategies: a comprehensive review
Metabolic Brain Disease (2026)
-
Navigating the Lipid Landscape: The Role of Fatty Acid Synthase in Neural Stem Cell Fate and Central Nervous System Function
Molecular Neurobiology (2026)
-
Glycerophospholipids in ALS: insights into disease mechanisms and clinical implication
Molecular Neurodegeneration (2025)