Abstract
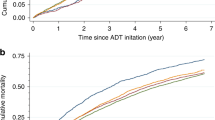
Contemporary advances in prostate cancer treatments have markedly improved patient outcomes, yet concerns persist regarding the increased cardiovascular toxicity of prostate cancer treatments, which is multifaceted. Local therapies entail non-negligible cardiovascular risks. The effects of androgen deprivation therapy, which is pivotal in disease management, on cardiovascular health remains contentious, with gonadotropin-releasing hormone agonists and antagonists showing varying cardiovascular outcomes. Despite the ongoing controversy over the cardiovascular risks of gonadotropin-releasing hormone antagonists versus agonists, current evidence does not support favouring one over the other based solely on cardiovascular risk. Combination therapy with androgen receptor pathway inhibitors and androgen deprivation therapy shows additive cardiovascular risks, but robust comparative data are lacking. Chemotherapies such as docetaxel and cabazitaxel, along with emerging targeted therapies and radiopharmaceuticals, are associated with varied cardiovascular risks, necessitating personalized patient assessment. Clinicians should adhere to cardio-oncology guidelines when prescribing therapeutic agents, especially for patients with pre-existing cardiovascular conditions. Optimal monitoring and management strategies are essential to mitigate cardiovascular morbidity and mortality.
Key points
-
Prostate cancer treatments, although effective, have been associated with increased risks of cardiovascular toxicity, necessitating careful evaluation of patient profiles before initiating treatments.
-
Despite much debate, the current best available data do not show an advantage of gonadotropin-releasing hormone antagonists over agonists.
-
Combination therapies, such as androgen deprivation therapy and androgen receptor axis-targeted therapies, are associated with additive cardiovascular risks, emphasizing the need for vigilant monitoring and adherence to cardio-oncology guidelines, particularly for patients with pre-existing cardiovascular comorbidities.
-
Robust cardio-oncology strategies incorporating improved risk assessment tools and multidisciplinary patient management might minimize cardiovascular morbidity and mortality.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 72, 7–33 (2022).
Bill-Axelson, A. et al. Radical prostatectomy or watchful waiting in early prostate cancer. N. Engl. J. Med. 370, 932–942 (2014).
Dearnaley, D. P. et al. Escalated-dose versus standard-dose conformal radiotherapy in prostate cancer: first results from the MRC RT01 randomised controlled trial. Lancet Oncol. 8, 475–487 (2007).
Loblaw, D. A. et al. Initial hormonal management of androgen-sensitive metastatic, recurrent, or progressive prostate cancer: 2006 update of an American Society of Clinical Oncology practice guideline. J. Clin. Oncol. 25, 1596–1605 (2007).
Sartor, O. et al. Effect of radium-223 dichloride on symptomatic skeletal events in patients with castration-resistant prostate cancer and bone metastases: results from a phase 3, double-blind, randomised trial. Lancet Oncol. 15, 738–46 (2014).
Petrylak, D. P. et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N. Engl. J. Med. 351, 1513–1520 (2004).
Beer T. M. et al. Enzalutamide in metastatic prostate cancer before chemotherapy. J. Clin. Oncol. 37, 2974–2986 (2019).
de Bono, J. S. et al. Abiraterone and increased survival in metastatic prostate cancer. N. Engl. J. Med. 364, 1995–2005 (2011).
Clark, R., Vesprini, D. & Narod, S. A. The effect of age on prostate cancer survival. Cancers 14, 4149 (2022).
Sturgeon, K. M. et al. A population-based study of cardiovascular disease mortality risk in US cancer patients. Eur. Heart J. 40, 3889–3897 (2019).
Epstein, M. M., Edgren, G., Rider, J. R., Mucci, L. A. & Adami, H.-O. Temporal trends in cause of death among Swedish and US men with prostate cancer. J. Natl Cancer Inst. 104, 1335–1342 (2012).
Van Hemelrijck, M. et al. Absolute and relative risk of cardiovascular disease in men with prostate cancer: results from the population-based PCBaSe Sweden. J. Clin. Oncol. 28, 3448–3456 (2010).
Leong, D. P. et al. Cardiovascular risk in men with prostate cancer: insights from the RADICAL PC Study. J. Urol. 203, 1109–1111 (2020).
Wilk, M., Waśko-Grabowska, A. & Szmit, S. Cardiovascular complications of prostate cancer treatment. Front. Pharmacol. 11, 555475 (2020).
Rawla, P. Epidemiology of prostate cancer. World J. Oncol. 10, 63–89 (2019).
Schoormans, D. et al. Incidence of cardiovascular disease up to 13 year after cancer diagnosis: a matched cohort study among 32 757 cancer survivors. Cancer Med. 7, 4952–4963 (2018).
Zhang, X. et al. Ten-year cardiovascular risk among cancer survivors: the National Health and Nutrition Examination Survey. PLoS ONE 16, e0247919 (2021).
Marques, P. et al. Physiology of GnRH and gonadotrophin secretion. Endotext [Internet] https://www.ncbi.nlm.nih.gov/books/NBK279070/ (updated 15 October 2024).
Keating, N. L., O’Malley, A. J., Freedland, S. J. & Smith, M. R. Diabetes and cardiovascular disease during androgen deprivation therapy: observational study of veterans with prostate cancer. J. Natl Cancer Inst. 102, 39–46 (2010).
Saigal, C. S. et al. Androgen deprivation therapy increases cardiovascular morbidity in men with prostate cancer. Cancer 110, 1493–1500 (2007).
Tsai, H. K., D’Amico, A. V., Sadetsky, N., Chen, M.-H. & Carroll, P. R. Androgen deprivation therapy for localized prostate cancer and the risk of cardiovascular mortality. J. Natl Cancer Inst. 99, 1516–1524 (2007).
Levine, G. N. et al. Androgen-deprivation therapy in prostate cancer and cardiovascular risk: a science advisory from the American Heart Association, American Cancer Society, and American Urological Association: endorsed by the American Society for Radiation Oncology. Circulation 121, 833–840 (2010).
Research Center for Drug Evaluation. FDA drug safety communication: update to ongoing safety review of GnRH agonists and notification to manufacturers of GnRH agonists to add new safety information to labeling regarding increased risk of diabetes and certain cardiovascular diseases (FDA, 2017).
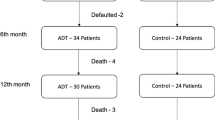
Smith, M. R., Klotz, L., Persson, B.-E., Olesen, T. K. & Wilde, A. A. M. Cardiovascular safety of degarelix: results from a 12-month, comparative, randomized, open label, parallel group phase III trial in patients with prostate cancer. J. Urol. 184, 2313–2319 (2010).
Butler, S. S. et al. Risk of cardiovascular mortality with androgen deprivation therapy in prostate cancer: a secondary analysis of the Prostate, Lung, Colorectal, and Ovarian (PLCO) Randomized Controlled Trial. Cancer 127, 2213–2221 (2021).
Kim, D. K. et al. Does androgen-deprivation therapy increase the risk of ischemic cardiovascular and cerebrovascular diseases in patients with prostate cancer? A nationwide population-based cohort study. J. Cancer Res. Clin. Oncol. 147, 1217–1226 (2021).
Nguyen, P. L. et al. Association of androgen deprivation therapy with cardiovascular death in patients with prostate cancer: a meta-analysis of randomized trials. JAMA 306, 2359–2366 (2011).
Holmes, J. A. et al. Cardiovascular preventive care and coordination of care in prostate cancer survivors: a multi-institutional prospective study. Int. J. Radiat. Oncol. Biol. Phys. 103, 112–115 (2019).
Saylor, P. J. & Fogerty, A. E. Prostate-cancer-associated hypercoagulability: do we need to worry about androgen deprivation? Lancet Oncol. 11, 406–407 (2010).
Smith, M. R. et al. Metabolic changes during gonadotropin-releasing hormone agonist therapy for prostate cancer. Cancer 112, 2188–2194 (2008).
Smith, M. R., Lee, H. & Nathan, D. M. Insulin sensitivity during combined androgen blockade for prostate cancer. J. Clin. Endocrinol. Metab. 91, 1305–1308 (2006).
Cannon, J. G., Kraj, B. & Sloan, G. Follicle-stimulating hormone promotes RANK expression on human monocytes. Cytokine 53, 141–144 (2011).
Smith, J. C. et al. The effects of induced hypogonadism on arterial stiffness, body composition, and metabolic parameters in males with prostate cancer. J. Clin. Endocrinol. Metab. 86, 4261–4267 (2001).
Bosco, C. et al. Quantifying observational evidence for risk of fatal and nonfatal cardiovascular disease following androgen deprivation therapy for prostate cancer: a meta-analysis. Eur. Urol. 68, 386–396 (2015).
Gagliano-Jucá, T. et al. Androgen deprivation therapy is associated with prolongation of QTc interval in men with prostate cancer. J. Endocr. Soc. 2, 485–496 (2018).
Bourghardt, J. et al. Androgen receptor-dependent and independent atheroprotection by testosterone in male mice. Endocrinology 151, 5428–5437 (2010).
Takov, K., Wu, J., Denvir, M. A., Smith, L. B. & Hadoke, P. W. F. The role of androgen receptors in atherosclerosis. Mol. Cell. Endocrinol. 465, 82–91 (2018).
Hopmans, S. N., Duivenvoorden, W. C. M., Werstuck, G. H., Klotz, L. & Pinthus, J. H. GnRH antagonist associates with less adiposity and reduced characteristics of metabolic syndrome and atherosclerosis compared with orchiectomy and GnRH agonist in a preclinical mouse model. Urol. Oncol. 32, 1126–1134 (2014).
Knutsson, A. et al. Treatment with a GnRH receptor agonist, but not the GnRH receptor antagonist degarelix, induces atherosclerotic plaque instability in ApoE−/− mice. Sci. Rep. 6, 26220 (2016).
Wang, Q. et al. FSH is responsible for androgen deprivation therapy-associated atherosclerosis in mice by exaggerating endothelial inflammation and monocyte adhesion. Arteriosclerosis Thrombosis Vasc. Biol. 44, 698–719 (2024).
Poljak, Z., Hulin, I., Maruscakova, L. & Mladosievicova, B. Are GnRH and FSH potentially damaging factors in the cardiovascular system? Pharmazie 73, 187–190 (2018).
Sun, L. et al. Further evidence for direct pro-resorptive actions of FSH. Biochem. Biophys. Res. Commun. 394, 6–11 (2010).
Crawford, E. D. et al. The potential role of follicle-stimulating hormone in the cardiovascular, metabolic, skeletal, and cognitive effects associated with androgen deprivation therapy. Urol. Oncol. 35, 183–191 (2017).
Mohammed, K. et al. Oral vs transdermal estrogen therapy and vascular events: a systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 100, 4012–4020 (2015).
Russell, N. et al. Short-term effects of transdermal estradiol in men undergoing androgen deprivation therapy for prostate cancer: a randomized placebo-controlled trial. Eur. J. Endocrinol. 178, 565–576 (2018).
Langley, R. E. et al. Transdermal oestradiol for androgen suppression in prostate cancer: long-term cardiovascular outcomes from the randomised Prostate Adenocarcinoma Transcutaneous Hormone (PATCH) trial programme. Lancet 397, 581 (2021).
Anderson, J. et al. Degarelix versus goserelin (+ antiandrogen flare protection) in the relief of lower urinary tract symptoms secondary to prostate cancer: results from a phase IIIb study (NCT00831233). Urol. Int. 90, 321–328 (2012).
Mason, M. et al. Neoadjuvant androgen deprivation therapy for prostate volume reduction, lower urinary tract symptom relief and quality of life improvement in men with intermediate- to high-risk prostate cancer: a randomised non-inferiority trial of degarelix versus goserelin plus bicalutamide. Clin. Oncol. 25, 190–196 (2013).
Axcrona, K. et al. Androgen deprivation therapy for volume reduction, lower urinary tract symptom relief and quality of life improvement in patients with prostate cancer: degarelix vs goserelin plus bicalutamide. BJU Int. 110, 1721–1728 (2012).
Tombal, B. et al. P109 Efficacy and safety of a 3-monthly depot formulation of degarelix compared with goserelin in prostate cancer. Eur. Urol. Suppl. 5, 228 (2012).
Crawford, D., Shore, N., Higano, C., Neijber, A. & Yankov, V. PD27-05 Intermittent androgen deprivation with the gonadotrophin-releasing hormone antagonist degarelix. J. Urol. 191, e766 (2014).
Albertsen, P. C. et al. Cardiovascular morbidity associated with gonadotropin releasing hormone agonists and an antagonist. Eur. Urol. 65, 565–573 (2014).
Abufaraj, M. et al. Differential impact of gonadotropin-releasing hormone antagonist versus agonist on clinical safety and oncologic outcomes on patients with metastatic prostate cancer: a meta-analysis of randomized controlled trials. Eur. Urol. 79, 44–53 (2021).
Sciarra, A. et al. A meta-analysis and systematic review of randomized controlled trials with degarelix versus gonadotropin-releasing hormone agonists for advanced prostate cancer. Medicine 95, e3845 (2016).
Scailteux, L.-M., Naudet, F., Alimi, Q., Vincendeau, S. & Oger, E. Mortality, cardiovascular risk, and androgen deprivation therapy for prostate cancer: a systematic review with direct and network meta-analyses of randomized controlled trials and observational studies. Medicine 95, e3873 (2016).
Ma, C. et al. Comparing the risk of cardiovascular disease following GnRH agonist and GnRH antagonist therapy for patient with prostate cancer: a systematic review and meta-analysis. Minerva Urol. Nephrol. 73, 276–282 (2021).
Cirne, F. et al. The cardiovascular effects of gonadotropin-releasing hormone antagonists in men with prostate cancer. Eur. Heart J. Cardiovasc. Pharmacother. 8, 253–262 (2021).
Shore, N. D. et al. Oral relugolix for androgen-deprivation therapy in advanced prostate cancer. N. Engl. J. Med. 382, 2187–2196 (2020).
Sari Motlagh, R. et al. The efficacy and safety of relugolix compared with degarelix in advanced prostate cancer patients: a network meta-analysis of randomized trials. Eur. Urol. Oncol. 5, 138–145 (2021).
Davey, P. & Kirby, M. G. Cardiovascular risk profiles of GnRH agonists and antagonists: real-world analysis from UK general practice. World J. Urol. 39, 307–315 (2021).
Perrone, V. et al. Cardiovascular risk profile in prostate cancer patients treated with GnRH agonists versus antagonists: an Italian real-world analysis. Ther. Clin. Risk Manag. 16, 393–401 (2020).
Scailteux, L.-M. et al. Androgen deprivation therapy and cardiovascular risk: no meaningful difference between GnRH antagonist and agonists — a nationwide population-based cohort study based on 2010–2013 French Health Insurance data. Eur. J. Cancer 77, 99–108 (2017).
George, G. et al. Risk of cardiovascular disease following gonadotropin‐releasing hormone agonists vs antagonists in prostate cancer: real‐world evidence from five databases. Int. J. Cancer 148, 2203–2211 (2021).
Cardwell, C. R. et al. The risk of cardiovascular disease in prostate cancer patients receiving androgen deprivation therapies. Epidemiology 31, 432–440 (2020).
Hupe, M. C. et al. Retrospective analysis of patients with prostate cancer initiating GnRH agonists/antagonists therapy using a German claims database: epidemiological and patient outcomes. Front. Oncol. 8, 543 (2018).
Wallach, J. D. et al. Real-world cardiovascular outcomes associated with degarelix vs leuprolide for prostate cancer treatment. JAMA Netw. Open 4, e2130587 (2021).
Lopes, R. D. et al. Cardiovascular safety of degarelix versus leuprolide in patients with prostate cancer: the primary results of the PRONOUNCE randomized trial. Circulation 144, 1295–1307 (2021).
Sun, Y. et al. Efficacy and safety of degarelix in patients with prostate cancer: results from a phase III study in China. Asian J. Urol. 7, 301–308 (2020).
Ozono, S. et al. The efficacy and safety of degarelix, a GnRH antagonist: a 12-month, multicentre, randomized, maintenance dose-finding phase II study in Japanese patients with prostate cancer. Jpn. J. Clin. Oncol. 42, 477–484 (2012).
Ozono, S. et al. Efficacy and safety of 3-month dosing regimen of degarelix in Japanese subjects with prostate cancer: a phase III study. Cancer Sci. 109, 1920–1929 (2018).
Margel, D. et al. Cardiovascular morbidity in a randomized trial comparing GnRH agonist and GnRH antagonist among patients with advanced prostate cancer and preexisting cardiovascular disease. J. Urol. 202, 1199–1208 (2019).
Rehman, Y. & Rosenberg, J. E. Abiraterone acetate: oral androgen biosynthesis inhibitor for treatment of castration-resistant prostate cancer. Drug. Des. Devel Ther. 6, 13–18 (2012).
Schalken, J. & Fitzpatrick, J. M. Enzalutamide: targeting the androgen signalling pathway in metastatic castration‐resistant prostate cancer. BJU Int. 117, 215–225 (2016).
Patel, U. J. & Caulfield, S. Apalutamide for the treatment of nonmetastatic castration-resistant prostate cancer. J. Adv. Pract. Oncol. 10, 501–507 (2019).
Fizazi, K., Smith, M. R. & Tombal, B. Clinical development of darolutamide: a novel androgen receptor antagonist for the treatment of prostate cancer. Clin. Genitourin. Cancer 16, 332–340 (2018).
Morgans, A. K. et al. Androgen receptor inhibitor treatments: cardiovascular adverse events and comorbidity considerations in patients with non-metastatic prostate cancer. Urol. Oncol. 39, 52–62 (2021).
Fradin, J., Kim, F. J., Lu-Yao, G. L., Storozynsky, E. & Kelly, W. K. Review of cardiovascular risk of androgen deprivation therapy and the influence of race in men with prostate cancer. Cancers 15, 2316 (2023).
Cone, E. B. et al. Cardiovascular toxicities associated with abiraterone compared to enzalutamide — a pharmacovigilance study. EClinicalMedicine 36, 100887 (2021).
Lee, Y. H. A. et al. Major adverse cardiovascular events of enzalutamide versus abiraterone in prostate cancer: a retrospective cohort study. Prostate Cancer Prostatic Dis. 27, 776–782 (2023).
Hu, J., Aprikian, A. G., Vanhuyse, M. & Dragomir, A. Comparative cardiovascular safety of novel hormonal agents in metastatic castration-resistant prostate cancer using real-world data. Clin. Genitourin. Cancer 20, 17–24 (2022).
Matsukawa, A. et al. Cardiovascular events among men with prostate cancer treated with androgen receptor signaling inhibitors: a systematic review, meta-analysis, and network meta-analysis. Prostate Cancer Prostatic Dis. https://doi.org/10.1038/s41391-024-00886-0 (2024).
Kwon, W.-A., Song, Y. S. & Lee, M.-K. Strategic advances in combination therapy for metastatic castration-sensitive prostate cancer: current insights and future perspectives. Cancers 16, 3187 (2024).
Cohagan, B. & Brandis, D. Torsade de Pointes. StatPearls [Internet] https://www.ncbi.nlm.nih.gov/books/NBK459388/ (updated 8 August 2023).
Verzoni, E. et al. Safety of long-term exposure to abiraterone acetate in patients with castration-resistant prostate cancer and concomitant cardiovascular risk factors. Ther. Adv. Med. Oncol. 8, 323–330 (2016).
Iacovelli, R. et al. The cardiovascular toxicity of abiraterone and enzalutamide in prostate cancer. Clin. Genitourin. Cancer 16, e645–e653 (2018).
Di Nunno, V. et al. New hormonal agents in patients with nonmetastatic castration-resistant prostate cancer: meta-analysis of efficacy and safety outcomes. Clin. Genitourin. Cancer 17, e871–e877 (2019).
El-Taji, O. et al. Cardiovascular events and androgen receptor signaling inhibitors in advanced prostate cancer: a systematic review and meta-analysis. JAMA Oncol. 10, 874–884 (2024).
Zhou, S. et al. Cardiovascular toxicity associated with androgen receptor axis-targeted agents in patients with prostate cancer: a meta-analysis of randomized controlled trials. Clin. Genitourin. Cancer 22, 102066 (2024).
Cao, B., Kim, M., Reizine, N. M. & Moreira, D. M. Adverse events and androgen receptor signaling inhibitors in the treatment of prostate cancer: a systematic review and multivariate network meta-analysis. Eur. Urol. Oncol. 6, 237–250 (2023).
Smith, M. R. et al. Apalutamide treatment and metastasis-free survival in prostate cancer. N. Engl. J. Med. 378, 1408–1418 (2018).
Chi, K. N. et al. Apalutamide for metastatic, castration-sensitive prostate cancer. N. Engl. J. Med. 381, 13–24 (2019).
Fizazi, K. et al. Darolutamide in nonmetastatic, castration-resistant prostate cancer. N. Engl. J. Med. 380, 1235–1246 (2019).
Freedland, S. J. et al. Improved outcomes with enzalutamide in biochemically recurrent prostate cancer. N. Engl. J. Med. 389, 1453–1465 (2023).
Stein, M. N., Goodin, S. & DiPaola, R. S. Abiraterone in prostate cancer: a new angle to an old problem. Clin. Cancer Res. 18, 1848–1854 (2012).
Dean, L. & Kane, M. in Medical Genetics Summaries (eds Pratt, V. M. et al.) (National Center for Biotechnology Information (US), 2012).
Monbaliu, J. et al. In vitro and in vivo drug–drug interaction studies to assess the effect of abiraterone acetate, abiraterone, and metabolites of abiraterone on CYP2C8 activity. Drug. Metab. Dispos. 44, 1682–1691 (2016).
Gibbons, J. A. et al. Pharmacokinetic drug interaction studies with enzalutamide. Clin. Pharmacokinet. 54, 1057–1069 (2015).
Duran, I. et al. Pharmacokinetic drug–drug interaction of apalutamide, part 1: clinical studies in healthy men and patients with castration-resistant prostate cancer. Clin. Pharmacokinet. 59, 1135–1148 (2020).
Zurth, C. et al. Drug–drug interaction potential of darolutamide: in vitro and clinical studies. Eur. J. Drug. Metab. Pharmacokinet. 44, 747–759 (2019).
Bolek, H. et al. Androgen receptor pathway inhibitors and drug–drug interactions in prostate cancer. ESMO Open 9, 103736 (2024).
Meng, F. et al. Stroke related to androgen deprivation therapy for prostate cancer: a meta-analysis and systematic review. BMC Cancer 16, 180 (2016).
Zhao, J. et al. Androgen deprivation therapy for prostate cancer is associated with cardiovascular morbidity and mortality: a meta-analysis of population-based observational studies. PLoS ONE 9, e107516 (2014).
Barker, S. J., Gamel, D. M. & Tremper, K. K. Cardiovascular effects of anesthesia and operation. Crit. Care Clin. 3, 251–268 (1987).
Committee Members et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery — executive summary a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee to update the 1996 guidelines on perioperative cardiovascular evaluation for noncardiac surgery). Circulation 105, 1257–1267 (2002).
Wani, M. et al. Venous thromboembolism (VTE) in post-prostatectomy patients: systematic review and meta-analysis. J. Clin. Med. 12, 3979 (2023).
Siech, C. et al. Cardiovascular disease and chronic pulmonary disease increase the risk of short-term major postoperative complications after robotic-assisted radical prostatectomy. Medicina 60, 173 (2024).
Jones, C. U. et al. Radiotherapy and short-term androgen deprivation for localized prostate cancer. N. Engl. J. Med. 365, 107–118 (2011).
Nabid, A. et al. Duration of androgen deprivation therapy in high-risk prostate cancer: a randomized phase III trial. Eur. Urol. 74, 432–441 (2018).
Bolla, M. et al. Concomitant and adjuvant androgen deprivation (ADT) with external beam irradiation (RT) for locally advanced prostate cancer: 6 months versus 3 years ADT — results of the randomized EORTC Phase III trial 22961. JCO 25, 5014–5014 (2007).
Bolla, M. et al. External irradiation with or without long-term androgen suppression for prostate cancer with high metastatic risk: 10-year results of an EORTC randomised study. Lancet Oncol. 11, 1066–1073 (2010).
Zapatero, A. et al. High-dose radiotherapy with short-term or long-term androgen deprivation in localised prostate cancer (DART01/05 GICOR): a randomised, controlled, phase 3 trial. Lancet Oncol. 16, 320–327 (2015).
Gong, J. et al. Reduced cardiorespiratory fitness and increased cardiovascular mortality after prolonged androgen deprivation therapy for prostate cancer. JACC CardioOncol. 2, 553–563 (2020).
Hufnagle, J. J., Andersen, S. N. & Maani, E. V. Radiation-induced cardiac toxicity StatPearls [Internet] https://www.ncbi.nlm.nih.gov/books/NBK554453/ (updated 29 May 2023).
Guo, Y. et al. Effects of radiotherapy or radical prostatectomy on the risk of long-term heart-specific death in patients with prostate cancer. Front. Oncol. 10, 592746 (2020).
Kjellstadli, C. et al. Cardiovascular outcomes after curative prostate cancer treatment: a population-based cohort study. Front. Oncol. 13, 1121872 (2023).
Todaro, M. C. et al. Cardioncology: state of the heart. Int. J. Cardiol. 168, 680–687 (2013).
Bendahou, H. et al. Cardiotoxicity due to docetaxel rare but it exists: about a case and literature review. J. Case Rep. Med. Hist. https://doi.org/10.54289/JCRMH2300105 (2023).
Shimoyama, M., Murata, Y., Sumi, K.-I., Hamazoe, R. & Komuro, I. Docetaxel induced cardiotoxicity. Heart 86, 219–219 (2001).
Rowinsky, E. K. et al. Cardiac disturbances during the administration of taxol. JCO 9, 1704–1712 (1991).
Arbuck, S. G. et al. A reassessment of cardiac toxicity associated with taxol. J. Natl Cancer Inst. Monogr. 117, 130 (1993).
Page, R. L. et al. Drugs that may cause or exacerbate heart failure. Circulation 134, e32–e69 (2016).
Rose, M., Burgess, J. T., O’Byrne, K., Richard, D. J. & Bolderson, E. PARP inhibitors: clinical relevance, mechanisms of action and tumor resistance. Front. Cell Dev. Biol. 8, 564601 (2020).
Inderjeeth, A.-J., Topp, M., Sanij, E., Castro, E. & Sandhu, S. Clinical application of poly(ADP-ribose) polymerase (PARP) inhibitors in prostate cancer. Cancers 14, 5922 (2022).
Bhamidipati, D., Haro-Silerio, J. I., Yap, T. A. & Ngoi, N. PARP inhibitors: enhancing efficacy through rational combinations. Br. J. Cancer 129, 904–916 (2023).
Friedlander, M., Lee, Y. C. & Tew, W. P. Managing adverse effects associated with poly (ADP-ribose) polymerase inhibitors in ovarian cancer: a synthesis of clinical trial and real-world data. Am. Soc. Clin. Oncol. Educ. Book 43, e390876 (2023).
Palazzo, A. et al. Major adverse cardiac events and cardiovascular toxicity with PARP inhibitors-based therapy for solid tumors: a systematic review and safety meta-analysis. ESMO Open 8, 101154 (2023).
Chen, W. et al. Hypertension associated with niraparib in cancer patients: a pharmacovigilance analysis based on the FAERS database and meta-analysis of randomized controlled trials. Gynecol. Oncol. 182, 108–114 (2024).
Han, J.-Y., Seo, Y.-E., Kwon, J.-H., Kim, J. H. & Kim, M. G. Cardioprotective effects of PARP inhibitors: a re-analysis of a meta-analysis and a real-word data analysis using the FAERS database. J. Clin. Med. 13, 1218 (2024).
Abida, W. et al. Non-BRCA DNA damage repair gene alterations and response to the PARP inhibitor rucaparib in metastatic castration-resistant prostate cancer: analysis from the phase II TRITON2 study. Clin. Cancer Res. 26, 2487–2496 (2020).
Saad, F. et al. Olaparib plus abiraterone versus placebo plus abiraterone in metastatic castration-resistant prostate cancer (PROpel): final prespecified overall survival results of a randomised, double-blind, phase 3 trial. Lancet Oncol. 24, 1094–1108 (2023).
Agarwal, N. et al. Talazoparib plus enzalutamide in men with first-line metastatic castration-resistant prostate cancer (TALAPRO-2): a randomised, placebo-controlled, phase 3 trial. Lancet 402, 291–303 (2023).
Chi, K. N. et al. Niraparib and abiraterone acetate for metastatic castration-resistant prostate cancer. JCO 41, 3339–3351 (2023).
Tawagi, K., Schmolze, M., Nguyen, B., Laviana, A. & Reizine, N. PARP inhibitors in prostate cancer — understanding the current landscape. IJCCD https://doi.org/10.53876/001c.120988 (2024).
Marshall, C. H. et al. Olaparib without androgen deprivation for high-risk biochemically recurrent prostate cancer following prostatectomy: a nonrandomized controlled trial. JAMA Oncol. 10, 1400–1408 (2024).
Markowski, M. C. et al. TRIUMPH: phase II trial of rucaparib monotherapy in patients with metastatic hormone-sensitive prostate cancer harboring germline DNA repair gene mutations. JCO 41, 190–190 (2023).
Vazquez, S. R. Drug-drug interactions in an era of multiple anticoagulants: a focus on clinically relevant drug interactions. Blood 132, 2230–2239 (2018).
LaFargue, C. J., Dal Molin, G. Z., Sood, A. K. & Coleman, R. L. Exploring and comparing adverse events between PARP inhibitors. Lancet Oncol. 20, e15–e28 (2019).
Vinci, P. et al. Statin-associated myopathy: emphasis on mechanisms and targeted therapy. Int. J. Mol. Sci. 22, 11687 (2021).
Beavers, C. J. et al. Cardio-oncology drug interactions: a scientific statement from the American Heart Association. Circulation 145, e811–e838 (2022).
Bruin, M. A. C., Sonke, G. S., Beijnen, J. H. & Huitema, A. D. R. Pharmacokinetics and pharmacodynamics of PARP inhibitors in oncology. Clin. Pharmacokinet. 61, 1649–1675 (2022).
Huynh-Le, M.-P., Shults, R. C., Connor, M. J. & Hattangadi-Gluth, J. A. Adverse events associated with radium-223 in metastatic prostate cancer: disproportionality analysis of FDA data reflecting worldwide utilization. Clin. Genitourin. Cancer 18, 192–200.e2 (2020).
Hoskin, P. et al. Efficacy and safety of radium-223 dichloride in patients with castration-resistant prostate cancer and symptomatic bone metastases, with or without previous docetaxel use: a prespecified subgroup analysis from the randomised, double-blind, phase 3 ALSYMPCA trial. Lancet Oncol. 15, 1397–1406 (2014).
Jafari, E., Amini, A. L., Ahmadzadehfar, H., Bagheri, D. & Assadi, M. Cardiotoxicity and cardiac monitoring following the use of radiotheranostics agents including 177Lu-PSMA for prostate cancer and 177Lu-DOTATATE for neuroendocrine tumors. Nuklearmedizin 60, 99–105 (2021).
Sartor, O. et al. Lutetium-177–PSMA-617 for metastatic castration-resistant prostate cancer. N. Engl. J. Med. 385, 1091–1103 (2021).
Cheever, M. A. & Higano, C. S. PROVENGE (sipuleucel-T) in prostate cancer: the first FDA-approved therapeutic cancer vaccine. Clin. Cancer Res. 17, 3520–3526 (2011).
Goff, D. C. et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. Circulation 129, S49–S73 (2014).
D’Agostino, R. B. Sr, Grundy, S., Sullivan, L. M. & Wilson, P. & for the CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 286, 180–187 (2001).
Hippisley-Cox, J., Coupland, C. & Brindle, P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 357, j2099 (2017).
Khan, S. S. et al. Development and validation of the American Heart Association’s PREVENT equations. Circulation 149, 430–449 (2024).
Bhatia, N. et al. Cardiovascular effects of androgen deprivation therapy for the treatment of prostate cancer. Circulation 133, 537–541 (2016).
Klotz, L. et al. The efficacy and safety of degarelix: a 12-month, comparative, randomized, open-label, parallel-group phase III study in patients with prostate cancer. BJU Int. 102, 1531–1538 (2008).
Higano, C. S. et al. Risk of cardiovascular events with degarelix versus leuprolide after biochemical relapse of prostate cancer: exploratory analysis of a randomized controlled trial. JCO 33, 151–151 (2015).
Zhu, J. et al. Toxicity profile characteristics of novel androgen-deprivation therapy agents in patients with prostate cancer: a meta-analysis. Expert. Rev. Anticancer. Ther. 18, 193–198 (2018).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding authors
Ethics declarations
Competing interests
S.T. receives honoraria and consulting fees from Tolmar, AbbVie, Knight, Bayer, Janssen and Sumitomo pharma. M.T. receives honoraria and consulting fees from AbbVie, Tersera and Knight. F.S. has grants/contracts with Janssen, Bayer, Merck, Pfizer, Astellas, BMS, Novartis, Sanofi and AstraZeneca; receives consulting fees from Janssen, Bayer, Astellas, Novartis, Sanofi, AstraZeneca, Merck, Pfizer, Somitomo and Tolmar; and receives honoraria from Janssen, Bayer, Somitomo, Astellas, Novartis, Sanofi, AstraZeneca, Merck, Pfizer and Tolmar. T.N. has grants/contracts with Bayer, Jansen, Astellas, Tersera and Sanofi Canada; receives consulting fees from AbbVie, Astellas, Jansen, Tersera, Tolmar, Bayer, AAA, Pfizer, Knight, AstraZeneca and Sumitomo pharma; receives support for attending meetings/travel from Jansen, Tolmar, Knight and Bayer; and is the chair of the Quebec GU Radiation oncology group and co-chair of the Canadian GU radiation oncology group. B.B. declares no competing interests.
Peer review
Peer review information
Nature Reviews Urology thanks Joe O’Sullivan; Paul Sargos, who co-reviewed with Jennifer Le Guévelou; Tanya Dorff; and Ashwin Sachdeva, who co-reviewed with Omar El-Taji, for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tisseverasinghe, S., Tolba, M., Bahoric, B. et al. Assessing the effects of prostate cancer therapies on cardiovascular health. Nat Rev Urol 22, 509–525 (2025). https://doi.org/10.1038/s41585-025-01002-0
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41585-025-01002-0
This article is cited by
-
Association of life’s crucial 9 score with benign prostatic hyperplasia: a cross-sectional study
Journal of Health, Population and Nutrition (2025)
-
Reply to ‘Mitochondrial dysfunction as a crucial mediator of ADT-induced cardiovascular risk’
Nature Reviews Urology (2025)
-
Mitochondrial dysfunction as a crucial mediator of ADT-induced cardiovascular risk
Nature Reviews Urology (2025)