Abstract
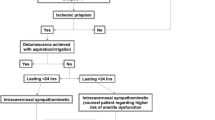
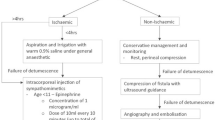
Priapism is an abnormal prolonged penile erection that persists in the absence of any sexual stimulation. Priapism can be subcategorized into three types: ischaemic (low-flow or veno-occlusive), non-ischaemic (high-flow or arterial) and stuttering priapism. Ischaemic priapism is the most common subtype and is associated with multiple aetiologies, most commonly haemoglobinopathies and antipsychotic medications. The mechanisms underlying stuttering priapism are complex, and involve dysregulation of the nitric oxide signalling pathway, Rho–Rho kinase pathway, adenosine, opiorphins, oxidative stress and androgens. The investigation and management of priapism involve a stepwise approach. A clinical history, examination and a blood-gas analysis from the corpus cavernosum helps to distinguish between ischaemic and non-ischaemic subtypes. Colour Doppler ultrasonography and penile MRI can be used in more complex cases, or those with a delayed presentation. Treatment involves cavernosal blood aspiration followed by instillation of an α-adrenergic receptor agonist such as phenylephrine, proceeding to penile shunt surgery (within the first 24–48 h) if the priapism persists. Insertion of a penile prosthesis is indicated when a shunting procedure or penoscrotal decompression fails, or if a patient presents with a priapism persisting longer than 36–48 h depending on the guidelines used. For non-ischaemic priapism following failed conservative treatment, selective arterial embolization of the arteriocorporal fistula can be performed. The aetiology and pathophysiology of the different priapism subtypes help to determine the management of specific patients.
Key points
-
Priapism is uncommon and can be subcategorized into ischaemic (low-flow or veno-occlusive), non-ischaemic (high-flow or arterial) and stuttering (recurrent) priapism.
-
Diagnostic tests include blood-gas analysis, colour Doppler ultrasonography and penile MRI, and initial management includes cavernosal blood aspiration, injection of α-adrenergic receptor agonists and shunting procedures.
-
If shunting procedures fail, or the duration of priapism is >36–48 h, an acute penile prosthesis insertion is a surgical option.
-
Acute or early insertion of a penile prosthesis is associated with reduced complication rates and high patient satisfaction compared with a delayed insertion.
-
Several molecular pathways contribute to stuttering priapism, including dysregulation of the nitric-oxide signalling pathway, Rho–Rho kinase pathway, adenosine, opiorphins, oxidative stress and androgens; current medications, including adrenergic, nitrergic and hormonal medications target these pathways.
-
Current research continues to focus on the pathological mechanisms leading to priapism and medications aimed at preventing stuttering priapism, as well as reducing complications such as penile shortening, fibrosis, penile curvature and erectile dysfunction.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Salonia A., et al. European Association of Urology 2025 guidelines: sexual and reproductive health. EAU Guidelines https://uroweb.org/guidelines/sexual-and-reproductive-health (2025).
Vreugdenhil, S., de Jong, I. J. & van Driel, M. F. Priapism throughout the ages. Urology 118, 21–24 (2018).
Eland, I. A., Van der Lei, J., Stricker, B. H. C. & Sturkenboom, M. J. C. M. Incidence of priapism in the general population. Urology 57, 970–972 (2001).
Kulmala, R. V., Lehtonen, T. A. & Tammela, T. L. J. Priapism, its incidence and seasonal distribution in Finland. Scand. J. Urol. Nephrol. 29, 93–96 (1995).
Sugihara, T. et al. Incidence and clinical features of priapism in Japan: 46 cases from the Japanese diagnosis procedure combination database 2006–2008. Int. J. Impot. Res. 23, 76–80 (2011).
Gül, M. et al. What is the effectiveness of surgical and non-surgical therapies in the treatment of ischemic priapism in patients with sickle cell disease? A systematic review by the EAU sexual and reproductive health guidelines panel. Int. J. Impot. Res. 36, 20–35 (2024).
Broderick, G. A. et al. Priapism: pathogenesis, epidemiology, and management. J. Sex. Med. 7, 476–500 (2010).
Cherian, J. et al. Medical and surgical management of priapism. Postgrad. Med. J. 82, 89 (2006).
Donaldson, J. F., Rees, R. W. & Steinbrecher, H. A. Priapism in children: a comprehensive review and clinical guideline. J. Pediatr. Urol. 10, 11–24 (2014).
Almekaty, K. et al. The relationship between Coronavirus disease-19 (COVID-19) and ischemic priapism: a case-control study. Int. J. Impot. Res. 37, 372–376 (2025).
Rezaee, M. E. & Gross, M. S. Are we overstating the risk of priapism with oral phosphodiesterase type 5 inhibitors? J. Sex. Med. 17, 1579–1582 (2020).
James Johnson, M. et al. Which patients with ischaemic priapism require further investigation for malignancy? Int. J. Impot. Res. 32, 195–200 (2020).
Ralph, O., Shroff, N., Johnson, M. J., AlNajjar, H. M. & Ralph, D. Malignancy: a rare, important and poorly understood cause of priapism. Sex. Med. Rev. 9, 312–319 (2021).
Nelson, J. H. & Winter, C. C. Priapism: evolution of management in 48 patients in a 22-year series. J. Urol. 117, 455–458 (1977).
Lue, T. F. Erectile dysfunction. N. Engl. J. Med. 342, 1802–1813 (2000).
Anele, U., Morrison, B. & Burnett, A. Molecular pathophysiology of priapism: emerging targets. Curr. Drug. Targets 16, 474–483 (2014).
Champion, H. C., Bivalacqua, T. J., Takimoto, E., Kass, D. A. & Burnett, A. L. Phosphodiesterase-5A dysregulation in penile erectile tissue is a mechanism of priapism. Proc. Natl Acad. Sci. USA 102, 1661–1666 (2005).
Bivalacqua, T. J., Liu, T., Musicki, B., Champion, H. C. & Burnett, A. L. Endothelial nitric oxide synthase keeps erection regulatory function balance in the penis. Eur. Urol. 51, 1732–1740 (2007).
Sopko, N. A., Hannan, J. L. & Bivalacqua, T. J. Understanding and targeting the Rho kinase pathway in erectile dysfunction. Nat. Rev. Urol. 11, 622–628 (2014).
Bivalacqua, T. J. et al. Establishment of a transgenic sickle-cell mouse model to study the pathophysiology of priapism. J. Sex. Med. 6, 2494–2504 (2009).
Bivalacqua, T. J. et al. Attenuated RhoA/Rho-kinase signaling in penis of transgenic sickle cell mice. Urology 76, 510.e7–510.e12 (2010).
Lagoda, G., Sezen, S. F., Cabrini, M. R., Musicki, B. & Burnett, A. L. Molecular analysis of erection regulatory factors in sickle cell disease associated priapism in the human penis. J. Urol. 189, 762–768 (2013).
Mi, T. et al. Excess adenosine in murine penile erectile tissues contributes to priapism via A2B adenosine receptor signaling. J. Clin. Invest. 118, 1491–1501 (2008).
Wen, J. et al. Adenosine deaminase enzyme therapy prevents and reverses the heightened cavernosal relaxation in priapism. J. Sex. Med. 7, 3011–3022 (2010).
Fu, S., Tar, M. T., Melman, A. & Davies, K. P. Opiorphin is a master regulator of the hypoxic response in corporal smooth muscle cells. FASEB J. 28, 3633–3644 (2014).
Tong, Y. et al. Variable coding sequence protein A1 as a marker for erectile dysfunction. BJU Int. 98, 396–401 (2006).
Tong, Y. et al. hSMR3A as a marker for patients with erectile dysfunction. J. Urol. 178, 338–343 (2007).
Tong, Y., Tar, M., Melman, A. & Davies, K. The opiorphin gene (ProL1) and its homologues function in erectile physiology. BJU Int. 102, 736–740 (2008).
Kanika, N. D. et al. The mechanism of opiorphin-induced experimental priapism in rats involves activation of the polyamine synthetic pathway. Am. J. Physiol. Cell Physiol. 297, C916–C927 (2009).
Bivalacqua, T. J., Burnett, A. L., Hellstrom, W. J. G. & Champion, H. C. Overexpression of arginase in the aged mouse penis impairs erectile function and decreases eNOS activity: influence of in vivo gene therapy of anti-arginase. Am. J. Physiol. Heart Circ. Physiol. 292, H1340–H1351 (2007).
Musicki, B. & Burnett, A. L. Mechanisms underlying priapism in sickle cell disease: targeting and key innovations on the preclinical landscape. Expert. Opin. Ther. Targets 24, 439–450 (2020).
Wood, K. C. & Granger, D. N. Sickle cell disease: role of reactive oxygen and nitrogen metabolites. Clin. Exp. Pharmacol. Physiol. 34, 926–932 (2007).
Morelli, A. et al. Androgens regulate phosphodiesterase type 5 expression and functional activity in corpora cavernosa. Endocrinology 145, 2253–2263 (2004).
Morrison, B. F. et al. Is testosterone deficiency a possible risk factor for priapism associated with sickle-cell disease? Int. Urol. Nephrol. 47, 47–52 (2015).
Joice, G. A., Liu, J. L. & Burnett, A. L. Medical treatment of recurrent ischaemic priapism: a review of current molecular therapeutics and a new clinical management paradigm. BJU Int. 127, 498–506 (2021).
Liguori, G. et al. The management of stuttering priapism. Minerva Urol. Nefrol. 72, 173–186 (2020).
Levey, H. R., Kutlu, O. & Bivalacqua, T. J. Medical management of ischemic stuttering priapism: a contemporary review of the literature. Asian J. Androl. 14, 156–163 (2012).
Morrison, B. F., Reid, M., Madden, W. & Burnett, A. L. Testosterone replacement therapy does not promote priapism in hypogonadal men with sickle cell disease: 12-month safety report. Andrology 1, 576–582 (2013).
Elliott, L. et al. Genetic polymorphisms associated with priapism in sickle cell disease. Br. J. Haematol. 137, 262–267 (2007).
Cintho Ozahata, M. et al. Clinical and genetic predictors of priapism in sickle cell disease: results from the recipient epidemiology and donor evaluation study III Brazil cohort study. J. Sex. Med. 16, 1988–1999 (2019).
Hudnall, M., Reed-Maldonado, A. B. & Lue, T. F. Advances in the understanding of priapism. Transl. Androl. Urol. 6, 199–206 (2017).
Broderick, G. A. & Harkaway, R. Pharmacologic erection: time-dependent changes in the corporal environment. Int. J. Impot. Res. 6, 9–16 (1994).
Muneer, A., Minhas, S., Freeman, A., Kumar, P. & Ralph, D. J. Investigating the effects of high-dose phenylephrine in the management of prolonged ischaemic priapism. J. Sex. Med. 5, 2152–2159 (2008).
Spycher, M. A. & Hauri, D. The ultrastructure of the erectile tissue in priapism. J. Urol. 135, 142–147 (1986).
Muneer, A. et al. BAUS consensus document for the management of male genital emergencies: priapism. BJU Int. 121, 835–839 (2018).
Bivalacqua, T. J. et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J. Urol. 208, 43–52 (2022).
Bivalacqua, T. J. et al. Acute ischemic priapism: an AUA/SMSNA guideline. J. Urol. 206, 1114–1121 (2021).
von Stempel, C. et al. Mean velocity and peak systolic velocity can help determine ischaemic and non-ischaemic priapism. Clin. Radiol. 72, 611.e9–611.e16 (2017).
von Stempel, C., Walkden, M. & Kirkham, A. Review of the role of imaging in the diagnosis of priapism. Int. J. Impot. Res. https://doi.org/10.1038/S41443-024-00928-0 (2024).
Ralph, D. J. et al. The use of high-resolution magnetic resonance imaging in the management of patients presenting with priapism. BJU Int. 106, 1714–1718 (2010).
Capogrosso, P. et al. Conservative and medical treatments of non-sickle cell disease-related ischemic priapism: a systematic review by the EAU sexual and reproductive health panel. Int. J. Impot. Res. 36, 6–19 (2024).
Dittrich, A., Albrecht, K., Bar-Moshe, O. & Vandendris, M. Treatment of pharmacological priapism with phenylephrine. J. Urol. 146, 323–324 (1991).
Palagiri, R. D. R., Chatterjee, K., Jillella, A. & Hammond, D. A. A case report of hypertensive emergency and intracranial hemorrhage due to intracavernosal phenylephrine. Hosp. Pharm. 54, 186–189 (2019).
Lue, T. F. & Pescatori, E. S. Distal cavernosum-glans shunts for ischemic priapism. J. Sex. Med. 3, 749–752 (2006).
Burnett, A. L. & Sharlip, I. D. Standard operating procedures for priapism. J. Sex. Med. 10, 180–194 (2013).
Milenkovic, U. et al. Surgical and minimally invasive treatment of ischaemic and non-ischaemic priapism: a systematic review by the EAU sexual and reproductive health guidelines panel. Int. J. Impot. Res. 36, 36–49 (2024).
Quackels, R. Treatment of a case of priapism by cavernospongious anastomosis. Acta Urol. Belg. 32, 5–13 (1964).
Reed-Maldonado, A. B., Kim, J. S. & Lue, T. F. Avoiding complications: surgery for ischemic priapism. Transl. Androl. Urol. 6, 657–665 (2017).
Grayhack, J. T., Mccullough, W., O’Conor, V. J. & Trippel, O. Venous bypass to control priapism. Invest. Urol. 1, 509–513 (1964).
Lue, T. F. & Garcia, M. Should perioperative anticoagulation be an integral part of the priapism shunting procedure? Transl. Androl. Urol. 2, 316–320 (2013).
Ebbehøj, J. A new operation for priapism. Scand. J. Plast. Reconstr. Surg. 8, 241–242 (1974).
Winter, C. C. Cure of idiopathic priapism: new procedure for creating fistula between glans penis and corpora cavernosa. Urology 8, 389–391 (1976).
Gannon, M. et al. Surgical illustrative review of the treatment of ischaemic priapism. Int. J. Impot. Res. 2025, 1–6 (2025).
Barry, J. M. Priapism: treatment with corpus cavernosum to dorsal vein of penis shunts. J. Urol. 116, 754–756 (1976).
Ercole, C. J. J., Pontes, J. E. & Pierce, J. M. Changing surgical concepts in the treatment of priapism. J. Urol. 125, 210–211 (1981).
Brant, W. O., Garcia, M. M., Bella, A. J., Chi, T. & Lue, T. F. T-shaped shunt and intracavernous tunneling for prolonged ischemic priapism. J. Urol. 181, 1699–1705 (2009).
Burnett, A. L. & Pierorazio, P. M. Corporal “snake” maneuver: corporoglanular shunt surgical modification for ischemic priapism. J. Sex. Med. 6, 1171–1176 (2009).
Unal, S., Karakus, S., Du Comb, W. & Burnett, A. L. Clinical outcomes of the Burnett “snake” maneuver shunt modification for ischemic priapism. J. Sex. Med. 21, 723–728 (2024).
Ortaç, M., Çevik, G., Akdere, H., Ermeç, B. & Kadıoğlu, A. Anatomic and functional outcome following distal shunt and tunneling for treatment ischemic priapism: a single-center experience. J. Sex. Med. 16, 1290–1296 (2019).
Zacharakis, E. et al. The efficacy of the T-shunt procedure and intracavernous tunneling (snake maneuver) for refractory ischemic priapism. J. Urol. 191, 164–168 (2014).
Fuchs, J. S. et al. Penoscrotal decompression-promising new treatment paradigm for refractory ischemic priapism. J. Sex. Med. 15, 797–802 (2018).
Baumgarten, A. S. et al. Favourable multi-institutional experience with penoscrotal decompression for prolonged ischaemic priapism. BJU Int. 126, 441–446 (2020).
VanDyke, M. E. et al. Current opinions on the management of prolonged ischemic priapism: does penoscrotal decompression outperform corporoglanular tunneling? Int. J. Impot. Res. 36, 62–67 (2024).
Ramstein, J. J. et al. Clinical outcomes of periprocedural antithrombotic therapy in ischemic priapism management. J. Sex. Med. 17, 2260–2266 (2020).
Muneer, A. Insertion of penile implants in patients with priapism: when is the right time? Eur. Urol. Focus. 9, 49–50 (2023).
Zacharakis, E. et al. Penile prosthesis insertion in patients with refractory ischaemic priapism: early vs delayed implantation. BJU Int. 114, 576–581 (2014).
Muneer, A. & Ralph, D. J. Immediate placement of a penile prosthesis as first-line treatment for the management of ischaemic priapism. Eur. Urol. Focus. 5, 529–530 (2019).
Elmarasi, M. et al. Early vs delayed insertion of penile prosthesis in patients with refractory priapism: a systematic review and meta-analysis. Sex. Med. Rev. 12, 528–536 (2024).
Rees, R. W. et al. The management of low-flow priapism with the immediate insertion of a penile prosthesis. BJU Int. 90, 893–897 (2002).
Salem, E. A. & El Aasser, O. Management of ischemic priapism by penile prosthesis insertion: prevention of distal erosion. J. Urol. 183, 2300–2303 (2010).
Sedigh, O. et al. Early insertion of inflatable prosthesis for intractable ischemic priapism: our experience and review of the literature. Int. J. Impot. Res. 23, 158–164 (2011).
Salman, B., Elsherif, E., Elgharabawy, M. & Badawy, A. Early versus delayed penile prosthesis insertion for refractory ischemic priapism. Arab. J. Urol. 21, 76–81 (2022).
Zacharakis, E. et al. Early insertion of a malleable penile prosthesis in ischaemic priapism allows later upsizing of the cylinders. Scand. J. Urol. 49, 468–471 (2015).
Elhawy, M. M. & Fawzy, A. M. Outcomes of low-flow priapism and role of integrated penile prosthesis management. Afr. J. Urol. 27, 1–8 (2021).
Ralph, D. J. et al. The immediate insertion of a penile prosthesis for acute ischaemic priapism. Eur. Urol. 56, 1033–1038 (2009).
Hebert, K. L., Yafi, F. A. & Wilson, S. Inflatable penile prosthesis implantation into scarred corporal bodies: timing may decrease postoperative problems. BJU Int. 125, 168–172 (2020).
Velasquez, D. A., Guimaraes, P. V. B., Lescay, H. & Raheem, O. Penile prosthesis in priapism: a systematic review of outcomes and complications. Transl. Androl. Urol. 13, 574–583 (2024).
Barham, D. W. et al. Delayed placement of an inflatable penile prosthesis is associated with a high complication rate in men with a history of ischemic priapism. J. Sex. Med. 20, 1052–1056 (2023).
Tsambarlis, P. N., Chaus, F. & Levine, L. A. Successful placement of penile prostheses in men with severe corporal fibrosis following vacuum therapy protocol. J. Sex. Med. 14, 44–46 (2017).
Schifano, N., Capogrosso, P., Cakir, O. O., Dehò, F. & Garaffa, G. Surgical tips in difficult penile prosthetic surgery: a narrative review. Int. J. Impot. Res. 35, 690–698 (2023).
Yassin, M., Chen, R., Ager, M., Desouky, E. & Minhas, S. Penile implants in low flow priapism. Int. J. Impot. Res. 35, 651–663 (2023).
Minervini, A., Ralph, D. J. & Pryor, J. P. Outcome of penile prosthesis implantation for treating erectile dysfunction: experience with 504 procedures. BJU Int. 97, 129–133 (2006).
Trost, L. & Hellstrom, W. J. G. History, contemporary outcomes, and future of penile prostheses: a review of the literature. Sex. Med. Rev. 1, 150–163 (2013).
Yücel, Ö. B., Pazır, Y. & Kadıoğlu, A. Penile prosthesis implantation in priapism. Sex. Med. Rev. 6, 310–318 (2018).
Kuefer, R. et al. Changing diagnostic and therapeutic concepts in high-flow priapism. Int. J. Impot. Res. 17, 109–113 (2005).
von Stempel, C. et al. Therapeutic outcomes and analysis of Doppler findings in 25 patients with non-ischemic priapism. Int. J. Impot. Res. 36, 55–61 (2024).
Witt, M. A., Goldstein, I., Saenz de Tejada, I., Greenfield, A. & Krane, R. J. Traumatic laceration of intracavernosal arteries: the pathophysiology of nonischemic, high flow, arterial priapism. J. Urol. 143, 129–132 (1990).
Ricciardi, R. et al. Delayed high flow priapism: pathophysiology and management. J. Urol. 149, 119–121 (1993).
Ingram, A. R., Stillings, S. A. & Jenkins, L. C. An update on non-ischemic priapism. Sex. Med. Rev. 8, 140–149 (2020).
Wu, A. K. & Lue, T. F. Commentary on high flow, non-ischemic, priapism. Transl. Androl. Urol. 1, 109–112 (2012).
Todd, N. V. Priapism in acute spinal cord injury. Spinal Cord 49, 1033–1035 (2011).
Dubocq, F. M., Tefilli, M. V., Grignon, D. J., Pontes, J. E. & Dhabuwala, C. B. High flow malignant priapism with isolated metastasis to the corpora cavernosa. Urology 51, 324–326 (1998).
Karagiannis, A. A. et al. High flow priapism secondary to internal urethrotomy treated with embolization. J. Urol. 171, 1631–1632 (2004).
Liguori, G. et al. High-flow priapism (HFP) secondary to Nesbit operation: management by percutaneous embolization and colour Doppler-guided compression. Int. J. Impot. Res. 17, 304–306 (2005).
Tang, M. et al. Intracavernosal metaraminol bitartrate for treatment of priapism resulting from circumcision: a case report. Springerplus 5, 436 (2016).
Mistry, N. A., Tadros, N. N. & Hedges, J. C. Conversion of low-flow priapism to high-flow state using T-shunt with tunneling. Case Rep. Urol. 2017, 1–4 (2017).
Boscolo-Berto, R. et al. Determinism and liabilities in a complicated transrectal prostate biopsy: what is what. Urologia 78, 176–179 (2011).
Oshima, J. et al. [Nonischemic priapism following brachytherapy: a case report and a review]. Hinyokika Kiyo 62, 605–607 (2016).
Bertolotto, M., Zappetti, R., Pizzolato, R. & Liguori, G. Color Doppler appearance of penile cavernosal-spongiosal communications in patients with high-flow priapism. Acta Radiol. 49, 710–714 (2008).
Jung, D. C., Park, S. Y. & Lee, J. Y. Penile Doppler ultrasonography revisited. Ultrasonography 37, 16–24 (2018).
Kang, B. C. et al. Post-traumatic arterial priapism: colour Doppler examination and superselective arterial embolization. Clin. Radiol. 53, 830–834 (1998).
Zacharakis, E., Ralph, D. J., Walkden, M. & Muneer, A. Distal corpus cavernosum fibrosis and erectile dysfunction secondary to non-ischaemic priapism. Arch. Ital. Urol. Androl. 87, 258–259 (2015).
Mwamukonda, K. B., Chi, T., Shindel, A. W. & Lue, T. F. Androgen blockade for the treatment of high-flow priapism. J. Sex. Med. 7, 2532–2537 (2010).
Numan, F. et al. Posttraumatic nonischemic priapism treated with autologous blood clot embolization. J. Sex. Med. 5, 173–179 (2008).
Kim, K. R. et al. Treatment of high-flow priapism with superselective transcatheter embolization in 27 patients: a multicenter study. J. Vasc. Interv. Radiol. 18, 1222–1226 (2007).
Liu, B. X. et al. High-flow priapism: superselective cavernous artery embolization with microcoils. Urology 72, 571–573 (2008).
Chevallier, O. et al. Ethylene-vinyl alcohol copolymer (Onyx®) transarterial embolization for post-traumatic high-flow priapism. Quant. Imaging Med. Surg. 6, 323–327 (2016).
Numan, F. et al. Posttraumatic high-flow priapism treated by N-butyl-cyanoacrylate embolization. Cardiovasc. Interv. Radiol. 19, 278–280 (1996).
Tokue, H., Shibuya, K., Ueno, H., Tokue, A. & Tsushima, Y. Percutaneous direct puncture embolization with N-butyl-cyanoacrylate for high-flow priapism. Cardiovasc. Interv. Radiol. 39, 1343–1346 (2016).
Arrichiello, A. et al. Interventional radiology management of high flow priapism: review of the literature. Acta Biomed. 91, e2020010 (2020).
Bretzman, J. P., Ziegelmann, M. J. & Reisenauer, C. J. Selective penile artery angioembolization for high flow priapism — a step-by-step overview for the non-radiologist. J. Sex. Med. 22, 380–384 (2025).
Shapiro, R. H. & Berger, R. E. Post-traumatic priapism treated with selective cavernosal artery ligation. Urology 49, 638–643 (1997).
Kavanagh, P. L., Fasipe, T. A. & Wun, T. Sickle cell disease: a review. JAMA 328, 57–68 (2022).
Idris, I. M., Burnett, A. L. & DeBaun, M. R. Epidemiology and treatment of priapism in sickle cell disease. Hematol. Am. Soc. Hematol. Educ. Program. 2022, 450–458 (2022).
Thomson, A. M. et al. Global, regional, and national prevalence and mortality burden of sickle cell disease, 2000–2021: a systematic analysis from the global burden of disease study 2021. Lancet Haematol. 10, e585–e599 (2023).
Bivalacqua, T. J., Musicki, B., Kutlu, O. & Burnett, A. L. New insights into the pathophysiology of sickle cell disease-associated priapism. J. Sex. Med. 9, 79–87 (2012).
Adeyoju, A. B. et al. Priapism in sickle-cell disease; incidence, risk factors and complications — an international multicentre study. BJU Int. 90, 898–902 (2002).
Ballas, S. K. & Lyon, D. Safety and efficacy of blood exchange transfusion for priapism complicating sickle cell disease. J. Clin. Apher. 31, 5–10 (2016).
DeBaun, M. R. et al. Controlled trial of transfusions for silent cerebral infarcts in sickle cell anemia. N. Engl. J. Med. 371, 699–710 (2014).
Siegel, J. F., Rich, M. A., Brock, W. A. & Noe, H. N. Association of sickle cell disease, priapism, exchange transfusion and neurological events: ASPEN syndrome. J. Urol. 150, 1480–1482 (1993).
Roizenblatt, M. et al. Priapism is associated with sleep hypoxemia in sickle cell disease. J. Urol. 188, 1245–1251 (2012).
Stauffer, E. et al. Nocturnal hypoxemia rather than obstructive sleep apnea is associated with decreased red blood cell deformability and enhanced hemolysis in patients with sickle cell disease. Front. Physiol. 12, 743399 (2021).
Olujohungbe, A. B. et al. A prospective diary study of stuttering priapism in adolescents and young men with sickle cell anemia: report of an international randomized control trial-the priapism in sickle cell study. J. Androl. 32, 375–382 (2011).
Okpala, I., Westerdale, N., Jegede, T. & Cheung, B. Etilefrine for the prevention of priapism in adult sickle cell disease. Br. J. Haematol. 118, 918–921 (2002).
Priyadarshi, S. Oral terbutaline in the management of pharmacologically induced prolonged erection. Int. J. Impot. Res. 16, 424–426 (2004).
Virag, R., Bachir, D., Lee, K. & Galacteros, F. Preventive treatment of priapism in sickle cell disease with oral and self-administered intracavernous injection of etilefrine. Urology 47, 777–781 (1996).
Lin, G. et al. Up and down-regulation of phosphodiesterase-5 as related to tachyphylaxis and priapism. J. Urol. 170, S15–8 (2003).
Bivalacqua, T. J. et al. Sildenafil citrate-restored eNOS and PDE5 regulation in sickle cell mouse penis prevents priapism via control of oxidative/nitrosative stress. PLoS ONE 8, e68028 (2013).
Burnett, A. L., Bivalacqua, T. J., Champion, H. C. & Musicki, B. Feasibility of the use of phosphodiesterase type 5 inhibitors in a pharmacologic prevention program for recurrent priapism. J. Sex. Med. 3, 1077–1084 (2006).
Burnett, A. L., Anele, U. A., Trueheart, I. N., Strouse, J. J. & Casella, J. F. Randomized controlled trial of sildenafil for preventing recurrent ischemic priapism in sickle cell disease. Am. J. Med. 127, 664–668 (2014).
Hou, L. T. & Burnett, A. L. Regimented phosphodiesterase type 5 inhibitor use reduces emergency department visits for recurrent ischemic priapism. J. Urol. 205, 545–552 (2021).
Gupta, S. et al. A possible mechanism for alteration of human erectile function by digoxin: inhibition of corpus cavernosum sodium/potassium adenosine triphosphatase activity. J. Urol. 159, 1529–1536 (1998).
Rourke, K. F., Fischler, A. H. & Jordan, G. H. Treatment of recurrent idiopathic priapism with oral baclofen. J. Urol. 168, 2552–2553 (2002).
Yuan, J., Desouza, R., Westney, O. L. & Wang, R. Insights of priapism mechanism and rationale treatment for recurrent priapism. Asian J. Androl. 10, 88–101 (2008).
Perimenis, P., Athanasopoulos, A., Papathanasopoulos, P. & Barbalias, G. Gabapentin in the management of the recurrent, refractory, idiopathic priapism. Int. J. Impot. Res. 16, 84–85 (2004).
Levine, L. A. & Guss, S. P. Gonadotropin-releasing hormone analogues in the treatment of sickle cell anemia-associated priapism. J. Urol. 150, 475–477 (1993).
Steinberg, J. & Eyre, R. C. Management of recurrent priapism with epinephrine self-injection and gonadotropin-releasing hormone analogue. J. Urol. 153, 152–153 (1995).
Dahm, P., Rao, D. S. & Donatucci, C. F. Antiandrogens in the treatment of priapism. Urology 59, 138 (2002).
Yamashita, N. et al. Idiopathic stuttering priapism: recovery of detumescence mechanism with temporal use of antiandrogen. Urology 63, 1182–1184 (2004).
Costabile, R. Successful treatment of stutter priapism with an antiandrogen. Tech. Urol. 4, 167–168 (1998).
Franks, S., Layton, A. & Glasier, A. Cyproterone acetate/ethinyl estradiol for acne and hirsutism: time to revise prescribing policy. Hum. Reprod. 23, 231–232 (2008).
Schröder, F. H. et al. Metastatic prostate cancer treated by flutamide versus cyproterone acetate: final analysis of the “European Organization for Research and Treatment of Cancer” (EORTC) protocol 30892. Eur. Urol. 45, 457–464 (2004).
Cooper, A. J. A placebo-controlled trial of the antiandrogen cyproterone acetate in deviant hypersexuality. Compr. Psychiatry 22, 458–465 (1981).
DeCastro, B. J., Costabile, R. A., McMann, L. P. & Peterson, A. C. Oral ketoconazole for prevention of postoperative penile erection: a placebo controlled, randomized, double-blind trial. J. Urol. 179, 1930–1932 (2008).
Hoeh, M. P. & Levine, L. A. Prevention of recurrent ischemic priapism with ketoconazole: evolution of a treatment protocol and patient outcomes. J. Sex. Med. 11, 197–204 (2014).
Rachid-Filho, D., Cavalcanti, A. G., Favorito, L. A., Costa, W. S. & Sampaio, F. J. B. Treatment of recurrent priapism in sickle cell anemia with finasteride: a new approach. Urology 74, 1054–1057 (2009).
Baker, R. C., Bergeson, R. L., Yi, Y. A., Ward, E. E. & Morey, A. F. Dutasteride in the long-term management of stuttering priapism. Transl. Androl. Urol. 9, 87–92 (2020).
Serjeant, G. R., De Ceulaer, K. & Maude, G. H. Stilboestrol and stuttering priapism in homozygous sickle-cell disease. Lancet 2, 1274–1276 (1985).
Anele, U. A., Mack, A. K., Resar, L. M. S. & Burnett, A. L. Hydroxyurea therapy for priapism prevention and erectile function recovery in sickle cell disease: a case report and review of the literature. Int. Urol. Nephrol. 46, 1733–1736 (2014).
Hassan, A., Jam’a, A. & Al Dabbous, I. A. Hydroxyurea in the treatment of sickle cell associated priapism. J. Urol. 159, 1642 (1998).
Saad, S. T. O. et al. Follow-up of sickle cell disease patients with priapism treated by hydroxyurea. Am. J. Hematol. 77, 45–49 (2004).
Ataga, K. I. et al. Crizanlizumab for the prevention of pain crises in sickle cell disease. N. Engl. J. Med. 376, 429–439 (2017).
Abdulgayoom, M., Afana, M. S., Alshurafa, A. & Yassin, M. A. Potential efficacy of crizanlizumab in treating priapism in sickle cell disease: a case report. Clin. Case Rep. 12, e8585 (2024).
Idowu, M., Garcia, R. L. & Sule, O. B. Successful treatment of SCD-related priapism with crizanlizumab: a case series. J. Investig. Med. High. Impact Case Rep. 11, 23247096231191873 (2023).
Idowu, M. et al. Primary analysis of spartan: a phase 2 trial to assess the efficacy and safety of crizanlizumab in patients with sickle cell disease related priapism. Blood 142, 146–146 (2023).
Seftel, A. et al. High flow priapism complicating veno-occlusive priapism: pathophysiology of recurrent idiopathic priapism? J. Urol. 159, 1300–1301 (1998).
Abdessater, M. et al. Sleep related painful erection: an algorithm for evaluation and management. Basic. Clin. Androl. 29, 15 (2019).
Gül, M. et al. A clinical guide to rare male sexual disorders. Nat. Rev. Urol. 21, 35–49 (2024).
Howell, M. J. Parasomnias: an updated review. Neurotherapeutics 9, 753–775 (2012).
Vreugdenhil, S., Weidenaar, A. C., de Jong, I. J. & van Driel, M. F. Sleep-related painful erections — a case series of 24 patients regarding diagnostics and treatment options. Sex. Med. 5, e237–e243 (2017).
Vreugdenhil, S., Weidenaar, A. C., de Jong, I. J. & van Driel, M. F. Sleep-related painful erections: a meta-analysis on the pathophysiology and risks and benefits of medical treatments. J. Sex. Med. 15, 5–19 (2018).
Wang, Y., Zhang, J. & Li, H. Narrative review: pathogenesis, diagnosis, and treatment of sleep-related painful erection. Transl. Androl. Urol. 10, 4422–4430 (2021).
Johnson, M. et al. Differences in polysomnographic, nocturnal penile tumescence and penile doppler ultrasound findings in men with stuttering priapism and sleep-related painful erections. Int. J. Impot. Res. 34, 603–609 (2022).
Johnson, M. J., McNeillis, V., Chiriaco, G. & Ralph, D. J. Rare disorders of painful erection: a cohort study of the investigation and management of stuttering priapism and sleep-related painful erection. J. Sex. Med. 18, 376–384 (2021).
Crossnohere, N. L. et al. A framework for implementing patient-reported outcomes in clinical care: the PROTEUS-practice guide. Nat. Med. 30, 1519–1520 (2024).
Burnett, A. L., Anele, U. A. & Derogatis, L. R. Priapism impact profile questionnaire: development and initial validation. Urology 85, 1376–1381 (2015).
Morrison, B. F. et al. External validation of the priapism impact profile in a Jamaican cohort of patients with sickle cell disease. PLoS ONE 16, e0258560 (2021).
Lu, Z. et al. Low-intensity extracorporeal shock wave treatment improves erectile function: a systematic review and meta-analysis. Eur. Urol. 71, 223–233 (2017).
Clavijo, R. I., Kohn, T. P., Kohn, J. R. & Ramasamy, R. Effects of low-intensity extracorporeal shockwave therapy on erectile dysfunction: a systematic review and meta-analysis. J. Sex. Med. 14, 27–35 (2017).
Cocci, A. et al. Low-intensity extracorporeal shock wave therapy (Li-ESWT) for priapism-induced erectile dysfunction in young patients: the first case series. Int. J. Impot. Res. 34, 277–279 (2022).
Pozzi, E. et al. Stem-cell regenerative medicine as applied to the penis. Curr. Opin. Urol. 29, 443–449 (2019).
Manfredi, C. et al. Cell therapy for male sexual dysfunctions: systematic review and position statements from the European Society for Sexual Medicine. Sex. Med. 12, qfad071 (2024).
Castiglione, F., Cakir, O. O., Satchi, M., Fallara, G. & Pang, K. H. The current role and implications of stem cell therapy in erectile dysfunction: a transformation from caterpillar to butterfly is required. Eur. Urol. Focus. 9, 28–31 (2023).
Deabes, M. et al. Evaluating the efficacy and safety of platelet-rich plasma injection for erectile dysfunction: a systematic review and meta-analysis of randomized controlled trials. Sex. Med. Rev. 12, 739–746 (2024).
Panunzio, A. et al. Platelet-rich plasma intracavernosal injections for the treatment of primary organic erectile dysfunction: a systematic review and meta-analysis of contemporary controlled studies. Int. J. Impot. Res. 36, 562–571 (2024).
Pang, K. H. The effectiveness and safety of intracavernosal botulinum toxin injections in the management of erectile dysfunction: a systematic review and meta-analysis of clinical studies. Sex. Med. 13, qfaf034 (2025).
Shindel, A. W. et al. Pentoxifylline attenuates transforming growth factor-β1-stimulated collagen deposition and elastogenesis in human tunica albuginea-derived fibroblasts part 1: impact on extracellular matrix. J. Sex. Med. 7, 2077 (2010).
Albersen, M. et al. Pentoxifylline promotes recovery of erectile function in a rat model of postprostatectomy erectile dysfunction. Eur. Urol. 59, 286–296 (2011).
Erdemir, F. et al. The effect of pentoxifylline on penile cavernosal tissues in ischemic priapism-induced rat model. Int. Urol. Nephrol. 46, 1961–1967 (2014).
Cinar, O. et al. The effect of an antifibrotic agent, pirfenidone, on penile erectile function in an experimental rat model of ischemic priapism. Int. J. Impot. Res. 32, 232–238 (2020).
Lagoda, G. et al. Sustained nitric oxide (NO)-releasing compound reverses dysregulated NO signal transduction in priapism. FASEB J. 28, 76–84 (2014).
Pereira, D. A. et al. Heme-induced corpus cavernosum relaxation and its implications for priapism in sickle cell disease: a mechanistic insight. Andrology 12, 1857–1864 (2024).
Silveira, T. H. R., Calmasini, F. B., de Oliveira, M. G., Costa, F. F. & Silva, F. H. Targeting heme in sickle cell disease: new perspectives on priapism treatment. Front. Physiol. 15, 1435220 (2024).
Asmundo, M. G. & Russo, G. I. ManAgement of pRiapiSm and its impact on outcomes: an international register (MARS study) — the first international, multicenter, observational study regarding priapism in perspective. Int. J. Impot. Res. https://doi.org/10.1038/S41443-024-00849-Y (2024).
Author information
Authors and Affiliations
Contributions
All authors researched data for the article. All authors contributed substantially to discussion of the content. K.H.P. wrote the article. All authors reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Urology thanks Mehmet Gokhan Culha, Maher Abdessater and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pang, K.H., Alnajjar, H.M., Lal, A. et al. An update on mechanisms and treatment options for priapism. Nat Rev Urol 22, 826–845 (2025). https://doi.org/10.1038/s41585-025-01069-9
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41585-025-01069-9