Abstract
Prehabilitative and rehabilitative exercise, psychological support and nutrition interventions have proven beneficial in many cancer populations. Testicular cancer survivors have high rates of metabolic syndrome, cardiovascular disease, hypogonadism and psychosocial issues, and might yield greater benefit from such interventions than the average cancer survivor population. Results from the few studies available in this field suggest that exercise can improve fatigue, metabolic syndrome, cardiovascular risk profile and physical performance measures (such as VO2 max), whereas psychological support programmes have been shown to improve fatigue and mental health. However, a paucity of data exists on best practices for provision of nutrition, exercise and psychological support within the testicular cancer space, patients and caregivers, highlighting the urgent need for additional work in this field. Overall, prehabilitation and rehabilitation interventions for testicular cancer are safe and efficacious, and should be implemented by clinicians at diagnosis and throughout survivorship.
Key points
-
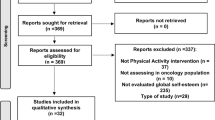
A paucity of data exists on prehabilitation or rehabilitation interventions for testicular cancer survivors, and further investigation is needed to define optimal peri-treatment supportive care interventions.
-
In the majority of available randomized clinical trials, efficacy of the prehabilitation measures was shown for ≥ 1 outcomes of interest.
-
Exercise is associated with improvements in fatigue, metabolic syndrome, cardiovascular risk profile and physical performance measures (such as VO2 max or muscle strength).
-
Psychological support programmes are successful in improving fatigue and mental health.
-
Clinicians should consider implementing prehabilitation and rehabilitation interventions for individuals with testicular cancer at diagnosis and throughout survivorship to improve outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Jensen, B. T. et al. Efficacy of pre and rehabilitation in radical cystectomy on health related quality of life and physical function: a systematic review. Asia Pac. J. Oncol. Nurs. 9, 100046 (2022).
Silver, J. K. & Baima, J. Cancer prehabilitation: an opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes. Am. J. Phys. Med. Rehabil. 92, 715–727 (2013).
Psutka, S. P. et al. Sarcopenia in patients with bladder cancer undergoing radical cystectomy: impact on cancer-specific and all-cause mortality. Cancer 120, 2910–2918 (2014).
Carli, F. et al. Surgical prehabilitation in patients with cancer. Phys. Med. Rehabil. Clin. N. Am. 28, 49–64 (2017).
Kidd, T. et al. What are the most effective interventions to improve physical performance in pre-frail and frail adults? A systematic review of randomised control trials. BMC Geriatr. 19, 184 (2019).
Briggs, L. G. et al. Prehabilitative/rehabilitative exercise, nutrition, and psychological support for bladder cancer: a scoping review of randomized clinical trials. Cancer 131, e35608 (2025).
Briggs, L. G. et al. Prehabilitation exercise before urologic cancer surgery: a systematic and interdisciplinary review. Eur. Urol. 81, 157–167 (2022).
Hijazi, Y., Gondal, U. & Aziz, O. A systematic review of prehabilitation programs in abdominal cancer surgery. Int. J. Surg. 39, 156–162 (2017).
American College of Surgeons Commission on Cancer. Cancer Program Standards: Ensuring Patient-Centered Care (American College of Surgeons, 2025).
American College of Surgeons Commission on Cancer. Program Standards: Provider Resources (American College of Surgeons, 2020).
American Cancer Society. Cancer Facts & Figures 2024 (American Cancer Society, 2024).
Association of Community Cancer Centers. Cancer Program Guidelines (ACCC, 2025).
Siegel, R. L., Giaquinto, A. N. & Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 74, 12–49 (2024).
Surveillance, Epidemiology, and End Results Program. Cancer stat facts: testicular cancer. SEER https://seer.cancer.gov/statfacts/html/testis.html (2025).
Chang, A. E. et al. (eds) Oncology: An Evidence-Based Approach (Springer, 2006).
Schagen, S. B. et al. Cognitive complaints and cognitive impairment following BEP chemotherapy in patients with testicular cancer. Acta Oncol. 47, 63–70 (2008).
Gospodarowicz, M. Testicular cancer patients: considerations in long-term follow-up. Hematol. Oncol. Clin. North Am. 22, 245–255 (2008).
Travis, L. B. et al. Second cancers among 40,576 testicular cancer patients: focus on long-term survivors. J. Natl Cancer Inst. 97, 1354–1365 (2005).
van den Belt-Dusebout, A. W. et al. Treatment-specific risks of second malignancies and cardiovascular disease in 5-year survivors of testicular cancer. J. Clin. Oncol. 25, 4370–4378 (2007).
La Vignera, S. et al. Hypogonadism and sexual dysfunction in testicular tumor survivors: a systematic review. Front. Endocrinol. 10, 264 (2019).
de Haas, E. C. et al. Early development of the metabolic syndrome after chemotherapy for testicular cancer. Ann. Oncol. 24, 749–755 (2013).
Travis, L. B. et al. Testicular cancer survivorship: research strategies and recommendations. J. Natl Cancer Inst. 102, 1114–1130 (2010).
De Padova, S. et al. Caregiver emotional burden in testicular cancer patients: from patient to caregiver support. Front. Endocrinol. 10, 318 (2019).
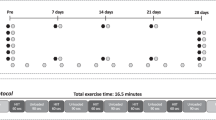
Schuler, M. K. et al. Impact of different exercise programs on severe fatigue in patients undergoing anticancer treatment — a randomized controlled trial. J. Pain Symptom Manage. 53, 57–66 (2017).
Thorsen, L. et al. Effectiveness of physical activity on cardiorespiratory fitness and health-related quality of life in young and middle-aged cancer patients shortly after chemotherapy. J. Clin. Oncol. 23, 2378–2388 (2005).
Thorsen, L. et al. Thromboembolic events after high-intensity training during cisplatin-based chemotherapy for testicular cancer: case reports and review of the literature. Int. J. Cancer 147, 3189–3198 (2020).
Christensen, J. F. et al. Resistance training does not protect against increases in plasma cytokine levels among germ cell cancer patients during and after chemotherapy. J. Clin. Endocrinol. Metab. 99, 2967–2976 (2014).
Adams, S. C. et al. Effects of high-intensity aerobic interval training on cardiovascular disease risk in testicular cancer survivors: a phase 2 randomized controlled trial. Cancer 123, 4057–4065 (2017).
Adams, S. C. et al. Effects of high-intensity interval training on fatigue and quality of life in testicular cancer survivors. Br. J. Cancer 118, 1313–1321 (2018).
Rabin, C., Dunsiger, S., Ness, K. K. & Marcus, B. H. Internet-based physical activity intervention targeting young adult cancer survivors. J. Adolesc. Young Adult Oncol. 1, 188–194 (2011).
Stapelfeldt, C. M., Momsen, A. M. H., Jensen, A. B., Andersen, N. T. & Nielsen, C. V. Municipal return to work management in cancer survivors: a controlled intervention study. Acta Oncol. 60, 370–378 (2021).
Hoyt, M. A., Wang, A. W., Breen, E. C. & Nelson, C. J. A randomized controlled trial of goal-focused emotion-regulation therapy for young adult survivors of testicular cancer: effects on salivary and inflammatory stress markers. Am. J. Mens Health 15, 15579883211044557 (2021).
Pauley, P. M., Morman, M. T. & Floyd, K. Expressive writing improves subjective health among testicular cancer survivors: a pilot study. Int. J. Mens Health 10, 199–219 (2011).
Van Der Lee, M. L. & Garssen, B. Mindfulness-based cognitive therapy reduces chronic cancer-related fatigue: a treatment study. Psychooncology 21, 264–272 (2012).
Arving, C., Assmus, J., Thormodsen, I., Berntsen, S. & Nordin, K. Early rehabilitation of cancer patients — an individual randomized stepped-care stress-management intervention. Psychooncology 28, 301–308 (2019).
Jacobsen, P. B. et al. Effects of self-directed stress management training and home-based exercise on quality of life in cancer patients receiving chemotherapy: a randomized controlled trial. Psychooncology 22, 1229–1235 (2013).
Adamsen, L. et al. Effect of a multimodal high intensity exercise intervention in cancer patients undergoing chemotherapy: randomised controlled trial. BMJ 339, 895–898 (2009).
Weijl, N. I. et al. Supplementation with antioxidant micronutrients and chemotherapy-induced toxicity in cancer patients treated with cisplatin-based chemotherapy: a randomised, double-blind, placebo-controlled study. Eur. J. Cancer 40, 1713–1723 (2004).
Hoyt, M. A., Cano, S. J., Saigal, C. S. & Stanton, A. L. Health-related quality of life in young men with testicular cancer: validation of the cancer assessment for young adults (CAYA). J. Cancer Surviv. 7, 630–640 (2013).
Woldeselassie, M. & Tamene, A. Therapeutic controversies over use of antioxidant supplements during cancer treatment: a scoping review. Front. Nutr. 11, 1480780 (2024).
Niedzwiedz, C. L., Knifton, L., Robb, K. A., Katikireddi, S. V. & Smith, D. J. Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority. BMC Cancer 19, 943 (2019).
Dehghan, M. et al. Stress and quality of life of patients with cancer: the mediating role of mindfulness. J. Oncol. 2020, 3289521 (2020).
Orre, I. J. et al. Chronic cancer-related fatigue in long-term survivors of testicular cancer. J. Psychosom. Res. 64, 363–371 (2008).
Dahl, A. A. et al. Study of anxiety disorder and depression in long-term survivors of testicular cancer. J. Clin. Oncol. 23, 2389–2395 (2005).
Dieckmann, K. P., Struss, W. J. & Budde, U. Evidence for acute vascular toxicity of cisplatin-based chemotherapy in patients with germ cell tumour. Anticancer. Res. 31, 4501–4505 (2011).
Abdel-Razeq, H. et al. Predictors of venous thromboembolism in patients with testicular germ cell tumors: a retrospective study. Clin. Appl. Thromb. Hemost. 27, 10760296211024756 (2021).
Bloomquist, K., Andersen, C., Munck, S., Lillelund, C. & Lauritsen, J. High-intensity interval training and thromboembolic events during chemotherapy for testicular cancer: a retrospective analysis from the Body & Cancer cohort. Acta Oncol. 62, 666–672 (2023).
Egegaard, T., Rohold, J., Lillelund, C., Persson, G. & Quist, M. Pre-radiotherapy daily exercise training in non-small cell lung cancer: a feasibility study. Rep. Pract. Oncol. Radiother. 24, 375–382 (2019).
Edvardsen, E. et al. High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax 70, 244 (2015).
Feldman, D. R. et al. Predicting cardiovascular disease among testicular cancer survivors after modern cisplatin-based chemotherapy: application of the Framingham risk score. Clin. Genitourin. Cancer 16, e761–e769 (2018).
Lubberts, S. et al. Cardiovascular disease in testicular cancer survivors: identification of risk factors and impact on quality of life. J. Clin. Oncol. 41, 3512–3522 (2023).
Clasen, S. C., Fung, C., Sesso, H. D. & Travis, L. B. Cardiovascular risks in testicular cancer: assessment, prevention, and treatment. Curr. Oncol. Rep. 25, 445–454 (2023).
Zaid, M. A. et al. Clinical and genetic risk factors for adverse metabolic outcomes in North American testicular cancer survivors. J. Natl Compr. Cancer Netw. 16, 257–265 (2018).
Alkhatib, K. Y. et al. Long term cardiovascular adverse outcomes in testicular cancer survivors: real-world U.S. population-based study. J. Clin. Oncol. 42, 5042–5042 (2024).
Coletta, A. M., Basen-Engquist, K. M. & Schmitz, K. H. Exercise across the cancer care continuum: why it matters, how to implement it, and motivating patients to move. Am. Soc. Clin. Oncol. Educ. Book 42, 1–7 (2022).
Gonzalo-Encabo, P., Wilson, R. L., Kang, D. W., Normann, A. J. & Dieli-Conwright, C. M. Exercise oncology during and beyond the COVID-19 pandemic: are virtually supervised exercise interventions a sustainable alternative? Crit. Rev. Oncol. Hematol. 174, 103699 (2022).
Liguori, G., Feito, Y., Fountaine, C., Roy, B. A. & American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription (Wolters Kluwer, 2022).
Ahmed, I. et al. Medication adherence apps: review and content analysis. JMIR Mhealth Uhealth 6, e62 (2018).
Dahl, A. A., Mykletun, A. & Fosså, S. D. Quality of life in survivors of testicular cancer. Urol. Oncol. 23, 193–200 (2005).
Mykletun, A. et al. Side effects and cancer-related stress determine quality of life in long-term survivors of testicular cancer. J. Clin. Oncol. 23, 3061–3068 (2005).
Alkhatib, K. Y. et al. Hospital anxiety and depression scale (HADS) score trends among testicular cancer survivors: a longitudinal study. J. Clin. Oncol. 41, 5042–5042 (2023).
Oun, R., Moussa, Y. E. & Wheate, N. J. The side effects of platinum-based chemotherapy drugs: a review for chemists. Dalton Trans. 47, 6645–6653 (2018).
Schepisi, G. et al. Vitamin D status among long-term survivors of testicular cancer. Oncotarget 8, 36780–36786 (2017).
Benetou, V. Nutrition for cancer survivors. Nutrients 14, 4093 (2022).
Pritlove, C. et al. Cooking for vitality: pilot study of an innovative culinary nutrition intervention for cancer-related fatigue in cancer survivors. Nutrients 12, 2760 (2020).
Livshits, Z., Rao, R. B. & Smith, S. W. An approach to chemotherapy-associated toxicity. Emerg. Med. Clin. North Am. 32, 167–203 (2014).
American Cancer Society. Late and long-term effects of cancer treatment in young adults. ACS https://www.cancer.org/cancer/types/cancer-in-young-adults/late-effects.html (2024).
National Cancer Institute. Pediatric and adolescent and young adult (AYA) cancer survivorship. NCI https://cancercontrol.cancer.gov/ocs/special-focus-areas/pediatric-adolescent-and-young-adult-survivorship.
Children’s Oncology Group. Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent and Young Adult Cancers, Version 6.0 (2023).
Bleyer, A. & Oeffinger, K. C. Adults and young adults with cancer: a special series. Cancer 107, 1645–1655 (2006).
Laing, C. M., Moules, N. J., Estefan, A. & Lang, M. Stories that heal: understanding the effects of creating digital stories with pediatric and adolescent/young adult oncology patients. J. Pediatr. Oncol. Nurs. 34, 272–282 (2017).
National Comprehensive Cancer Network. Adolescent and young adult (AYA) oncology. NCCN https://www.nccn.org/guidelines/guidelines-detail?category=4&id=1412 (2024).
Hemingway, B., Narayan, A. & Avery, S. LIVESTRONG fertility training: addressing the needs of AYA cancer survivors. Am. J. Manag. Care 21, SP500–SP503 (2015).
European Society for Medical Oncology. Adolescents and young adults Working Group. ESMO https://www.esmo.org/about-esmo/organisational-structure/educational-committee/adolescents-and-young-adults-working-group (2023).
Huddart, R. A. et al. Cardiovascular disease as a long-term complication of treatment for testicular cancer. J. Clin. Oncol. 21, 1513–1523 (2003).
Bandak, M. et al. Testosterone deficiency in testicular cancer survivors — a systematic review and meta-analysis. Andrology 4, 382–388 (2016).
Author information
Authors and Affiliations
Contributions
L.G.B., M.J.V.L., K.L.B., D.S. and V.S.G., researched data for the article. S.C.P., L.G.B., S.P.P., P.A.B. and P.M.P. contributed substantially to discussion of the content. L.G.B., D.S., A.M.D. wrote the article. S.C.P., L.G.B., S.P.P., M.J.V.L., K.L.B., V.S.G., K.Y.A., A.M.D., P.A.B., J.Q., C.D., P.M.P., H.A.M., M.D.T. and Q.D.T. reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
L.G.B. reports consulting fees from Delfina Inc and Tolmar outside of the submitted work and research funding from the Office of Scholarly Engagement at Harvard Medical School. S.P.P. serves on the advisory board for Immunity Bio Merck and Pfizer, receives research funding from Bladder Cancer Advocacy Network and the National Institute on Aging, consulting fees from CG Oncology and Janssen, serves on the editorial boards for European Urology and Bladder Cancer, and serves on guidelines committees for AUA Upper Tract Urothelial Carcinoma and AUA Practice Guidelines Committee. K.Y.A. serves on the Board of Directors for the Testicular Cancer Awareness Foundation (uncompensated position). P.M.P. serves on the Board of Directors for the Testicular Cancer Awareness Foundation (uncompensated position) and on Testicular Cancer guidelines committees for the AUA and NCCN. Q.D.T. reports consulting fees from Astellas, Bayer, Intuitive Surgical, Janssen, Novartis and Pfizer, and research funding from the American Cancer Society, Pfizer Global Medical Grants (Prostate Cancer Disparities no. 63354905) and a Health Disparity Research Award from the Department of Defense Congressionally Directed Medical Research Program (no. PC220551). All other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Urology thanks Michael Chovanec and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Briggs, L.G., Psutka, S.P., Van Ligten, M.J. et al. Exercise, diet and psychological support for patients with testicular cancer. Nat Rev Urol (2025). https://doi.org/10.1038/s41585-025-01089-5
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41585-025-01089-5