Abstract
The shortage of donors is a major challenge for transplantation; however, organs from genetically modified pigs can serve as ideal supplements1,2. Until now, porcine hearts and kidneys have been successively transplanted into humans3,4,5,6,7. In this study, heterotopic auxiliary transplantation was used to donate a six-gene-edited pig liver to a brain-dead recipient. The graft function, haemodynamics, and immune and inflammatory responses of the recipient were monitored over the subsequent 10 days. Two hours after portal vein reperfusion of the xenograft, goldish bile was produced, increasing to 66.5 ml by postoperative day 10. Porcine liver-derived albumin also increased after surgery. Alanine aminotransferase levels remained in the normal range, while aspartate aminotransferase levels increased on postoperative day 1 and then rapidly declined. Blood flow velocity in the porcine hepatic artery and portal and hepatic veins remained at an acceptable level. Although platelet numbers decreased early after surgery, they ultimately returned to normal levels. Histological analyses showed that the porcine liver regenerated capably with no signs of rejection. T cell activity was inhibited by anti-thymocyte globulin administration, and B cell activation increased 3 days after surgery and was then inhibited by rituximab. There were no significant peri-operative changes in immunoglobulin G or immunoglobulin M levels. C-reactive protein and procalcitonin levels were initially elevated and then quickly declined. The xenograft remained functional until study completion.
Similar content being viewed by others
Main
Liver transplantation is the most effective treatment for end-stage liver diseases. However, the number of allogeneic donations fails to meet the growing demand for transplants. To address the shortage, porcine organs are being considered as an ideal supplement given their compatible physiological function and size1,2. Moreover, theoretical and technical advances in gene editing have enabled the removal of key genes that mediate hyperacute rejection, such as glycoprotein α-galactosyltransferase 1 (GGTA1) and cytidine monophosphate-N-acetylneuraminic acid hydroxylase (CMAH), and the insertion of human transgenes that facilitate xenograft compatibility, including thrombomodulin and haem-oxygenase 1 (refs. 8,9,10,11).
Several preclinical and clinical xenotransplantation studies have been performed so far. Porcine hearts and kidneys have been successfully transplanted into both living and brain-dead individuals3,4,5,6,7. A recent study externally attached a pig liver to a brain-dead person with liver failure and assessed liver function, serving as the first use of pig liver to treat a human disease12. However, because of the complexity of liver function, to our knowledge no liver xenotransplantation has been performed in a living person before this trial.
Our team has conducted liver xenotransplantation research for more than a decade13,14,15. In 2013, we successfully performed the first pig-to-monkey heterotopic auxiliary liver transplantation in China. Both the recipient monkey and the transplanted liver survived for 14 days16. Since then, we have conducted, alone or in collaboration with other groups, pig-to-monkey liver, heart, kidney, cornea, skin and bone xenotransplantation, and a single pig-to-human skin xenotransplantation. In this study, under the strict supervision of our hospital ethics committee, we xenotransplanted the liver from a six-gene-edited pig to a brain-dead person17.
Evaluation of the gene-modified pig
A six-gene-modified Bama miniature pig kindly provided by Clonorgan Biotechnology was used as the donor in this study (Fig. 1a). To confirm the success of the gene modification, flow cytometry was performed on peripheral blood mononuclear cells (PBMCs) collected from the donor pig. GGTA1 (synthesizing α-1,3-galactosyltransferase), B4GALNT2 (encoding β‐1,4‐N‐acetyl‐galactosaminyltransferase 2) and CMAH (synthesizing N-glycolylneuraminic acid (Neu5Gc)), which mediates hyperacute rejection, were largely inactivated in the pig (Fig. 1b). Meanwhile, flow cytometry and western blotting showed that human complement regulatory proteins (CRPs), including CD46 (membrane cofactor protein) and CD55 (decay-accelerating factor), which attenuate hyperacute rejection and prolong xenograft survival, were overexpressed in donor PBMCs (Fig. 1b,c). To activate antithrombotic protein C and prevent clot formation, human thrombomodulin (THBD, encoding hTBM) was inserted into the porcine genome. Immunohistochemistry staining (IHC) showed that hTBM, as well as CD46 and CD45, were upregulated following gene modification (Fig. 1d). The recipient was confirmed to have low levels of xenoreactive immunoglobulin M (IgM) and IgG antibodies by flow cytometry (Fig. 1e,f). Porcine endogenous retrovirus (PERV) attached to the donor pig could not be detected peri-operatively in the recipient’s PBMCs or liver (Fig. 1g and Extended Data Fig. 1b), and porcine cytomegalovirus (PCMV) was also diminished in the donor and the recipient’s liver (Fig. 1h and Extended Data Fig. 1a). Moreover, microchimerism was undetectable in the recipient (Extended Data Fig. 1b).
a, Donor pig. b, Flow cytometry result showing the numbers of GGTA1-, β4GalNT2-, Neu5Gc-, CD46- and CD55-positive cells in the donor pig and a wild-type (WT) pig. For gating strategies, see Supplementary Fig. 2. c, Western blotting result showing the levels of human CD46 and CD55 protein in the liver tissues of the donor and a wild-type pig. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) is used as the control. For blot source data, see Supplementary Fig. 1. d, IHC staining result showing the levels of human CD46, CD55 and thrombomodulin protein in the liver tissues of the donor and a wild-type pig. Positive signals are represented by black arrows. e, Flow cytometry result showing the ability of PBMCs, isolated from the donor and the wild-type pig, to bind human IgM and IgG, represented by median fluorescence intensity (MFI). For gating strategies, see Supplementary Fig. 3. f, Quantitative result of e. g, Relative (upper) and absolute (lower) quantification of real-time polymerase chain reaction (RT-PCR) showing the number of PERV copies in the PBMCs and liver tissues of the recipient and the donor pig. h, Relative quantification of RT-PCR showing PCMV quantity in the liver tissues of the recipient and the donor pig. b–h contain one biological and technical repetition. Two independent experiments were carried out in c and d. Scale bar, 50 μm. CT, cycle threshold; ND, not detected.
Heterotopic auxiliary liver transplant
Before transplantation, vascular segmentation was performed (Extended Data Fig. 3a,b) on the donor pig, and the sizes of the porcine portal vein (PV) and inferior vena cava (IVC) were shown to approximately match the recipient’s vessels (Extended Data Fig. 2a). Photographs of a ruddy porcine liver captured at different time points are shown in Extended Data Fig. 2b. On the basis of our experience of earlier liver transplants, we chose to perform a heterotopic auxiliary transplantation. In brief, the recipient’s IVC was partially removed below the level of the right renal vein. The supra-hepatic IVC of the donor liver was then connected to the proximal end of the recipient’s IVC (Extended Data Fig. 2c and ① in Extended Data Fig. 2d) and the porcine PV was anastomosed with the distal end of the recipient’s IVC (Extended Data Fig. 2c and ② in Extended Data Fig. 2d). The porcine hepatic artery was then bridged to the recipient’s abdominal aorta (Extended Data Fig. 2c and ③ in Extended Data Fig. 2d) and the bile was drained from the body (Extended Data Figs. 2d and 3c). At the end of the study, the porcine liver was removed and the recipient’s IVC was reconstructed using an artificial blood vessel (Extended Data Fig. 3d,e).
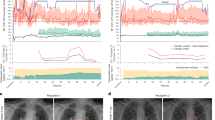
The porcine liver remained functional
To assess the function of the transplanted liver, an explicit schedule for further analyses was established (Fig. 2a). Goldish bile produced by the porcine liver emerged 2 h after PV reperfusion and increased markedly postoperatively (Fig. 2b,c). Porcine liver-derived albumin detected by enzyme-linked immunosorbent assay was also augmented following surgery (Fig. 2d). Even if the amounts of pig-originated bile and albumin had been low, these findings indicated the liver could survive in a human body and start functioning. Notably, there were inconsistent changes in the levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST), the enzymes that reflect liver function, following transplantation. Although ALT amounts remained normal, AST amounts increased sharply shortly after surgery and then declined rapidly (Fig. 2e,f). Although the reason for this discrepancy remains unclear, the marked increase in AST is unlikely to imply graft malfunction. Meanwhile, other indicators of liver function were measured (Fig. 2g–k). The amount of alkaline phosphatase was maintained in the normal range throughout the study (Fig. 2k), whereas bilirubin and γ-glutamyl transpeptidase (γ-GGT) were elevated at the late stage of the study (Fig. 2g–j).
a, Schematic depiction of the study, showing various time points of the investigation. b, Photographs of the bile secreted from the xenograft at different time points throughout the study. c,d, Amounts of bile (c) and porcine albumin (d) produced by the xenograft at different time points throughout the study. e–k, Amounts of ALT (e), AST (f), total bilirubin (g), direct bilirubin (h), indirect bilirubin (i), γ-GGT (j) and alkaline phosphatase (k) in the recipient’s serum at different time points throughout the study. l–n, Amounts of PLT (l), PT (m) and APTT (n) of the recipient at different time points throughout the study. c–n contain one biological and technical repetition. DBil, direct bilirubin; IDBil, indirect bilirubin; IU, international unit; TBil, total bilirubin.
Haemodynamics following transplantation
To confirm successful re-establishment of the porcine vascular system, blood flow in the porcine hepatic artery, PV and hepatic vein was monitored continuously by ultrasound. Blood flow in the porcine hepatic artery remained in the high-speed category following surgery, ranging from 41.45 to 60.63 cm s−1; the velocity of blood flow in the PV and hepatic vein was also acceptable (Extended Data Fig. 4a,b). Portal vein flow (PVF) was stable throughout the study (Extended Data Fig. 4c). Because some preclinical trials have reported impairments in coagulation function after xenografting, the recipient’s coagulation status was evaluated. Unlike prothrombin time (PT), which was sustained in the physiological range, a decrease in platelets (PLT) and an increase in activated partial thromboplastin time (APTT) were observed during the early stage of the postoperative period; however, both ultimately recovered to normal levels (Fig. 2l–n). These data indicate that intrinsic coagulation was more affected by the xenograft than extrinsic coagulation and that the hTBM transgene efficiently maintained circulatory homeostasis (Extended Data Fig. 5a,b).
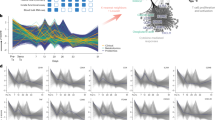
Histological analyses of porcine liver
Histological changes to the donor liver were next assessed using haematoxylin and eosin, IHC and immunofluorescent staining, scanning electron microscopy (SEM) and transmission electron microscopy (TEM). Surprisingly, slight sinusoidal congestion and inflammatory cell infiltration were found peri-operatively in the porcine liver, but no signs of immune rejection were noted. Moreover, the recipient’s original liver tissue collected on day 10 exhibited mild intrahepatic cholestasis (Fig. 3a), which may account for the elevated bilirubin and γ-GGT amounts observed during the late stage of the investigation (Fig. 2g–j). The histology of the hepatocytes, stellate cells and liver sinusoidal endothelial cells (LSECs) in the transplanted liver was also assessed. The porcine liver collected on day 10 had higher hepatocyte proliferation (Ki67), lower stellate cell activation (alpha smooth muscle actin) and higher LSEC repopulation (CD31) than the pre-operative control (Fig. 3b). These findings indicated that the transplanted liver capably regenerated with no sign of rejection and fibrogenesis. Interestingly, LSECs observed by SEM possessed well-differentiated fenestrae, indicating that the microcirculation of the porcine liver was not disrupted following transplantation (Fig. 3b). Ultimately, TEM observation showed that there was no big difference in the ultrastructure of the porcine hepatocytes between the 0 day and 10 day groups, and no viral particles were observed (Fig. 3c).
a, Representative images of haematoxylin and eosin (H&E) staining of liver tissues obtained from the xenograft and the recipient at different time points. b, Representative images of IHC staining of Ki67 and alpha smooth muscle actin (αSMA), immunofluorescence staining of CD31 and 4′,6-diamidino-2-phenylindole (DAPI) and SEM observation of the hepatic sinusoid of the xenograft at different time points. Positive signals are shown with black or white arrows. c, Representative TEM images of the porcine hepatocytes at different time points. a–c contain one biological and technical repetition. The experiment was carried out once in a, whereas two independent experiments were carried out in b and c. Scale bars, 1 μm (b (right), c (bottom)), 4 μm (c (top)), 25 μm (b (left)), 100 μm (a (bottom), b (middle)), 200 μm (a, top).
The xenograft-triggered immune response
An excessive immune response induced by xenotransplantation is the leading reason for xenograft dysfunction. All the drugs used for immunosuppression are listed in Extended Data Fig. 6. In brief, methylprednisolone, tacrolimus and mycophenolate mofetil, which are commonly used immunosuppressants, were administrated during the postoperative period. Etanercept and rituximab, which trigger anti-tumour necrosis factor (TNF) responses and B lymphocyte resolution, respectively, were also used intermittently following surgery. Anti-thymocyte globulin and eculizumab were used only pre-operatively. The blood concentrations of tacrolimus and mycophenolate mofetil were monitored closely throughout the study (Extended Data Fig. 7d).
The xenograft was subjected to biopsy at different time points of the study. IHC staining of complements showed that little C3d, C4d and C5b-9 deposited in the xenograft throughout the investigation (Fig. 4a). By contrast, IHC staining of immunoglobulins showed that moderate amounts of IgM and IgG were detected in the xenograft on postoperative day 10 (Fig. 4b), even though no significant changes in serum IgM or IgG were observed peri-operatively (Extended Data Fig. 7b). A panel of peripheral blood-derived immunocytes and cytokines was also assessed. Because of the administration of anti-thymocyte globulin, T cells, especially CD4+ T cells, were inhibited at the beginning of the postoperative period, while B cells were augmented (Extended Data Fig. 7a). Beginning on day 3, rituximab was applied, which promptly reduced the B cell population. CRP and procalcitonin, which mediate inflammatory reactivity, increased initially and then declined (Extended Data Fig. 7c). Interleukin-6 expression was maintained at a very low level postoperatively (Fig. 4c). Other cytokines, including TNF, interferon-α (IFNα) and IFNγ seemed to be suppressed at the early stage after surgery (Fig. 4d–f). These data together indicate that the inflammatory response was well controlled after transplantation.
a, Representative images of IHC staining of C3d, C4d and C5b-9 on the liver sections obtained from the xenograft at different time points of the study. b, Representative images of IHC staining of IgM and IgG on the liver sections obtained from the xenograft at different time points of the study. c–f, Amounts of interleukin-6 (IL-6) (c), TNF (d), IFNα (e) and IFNγ (f) in the recipient’s serum at different time points throughout the study. a and b contain one biological and technical repetition. For a, two independent experiments were carried out, whereas for b, the experiment was carried out once. Scale bars, 50 μm.
Discussion
Xenotransplantation has entered the era of clinical research. Research teams at the University of Maryland School of Medicine have performed pig-to-human heart transplantation and scientists at both Massachusetts General Hospital and New York University recently carried out pig-to-human kidney transplantation3,4,5,6,7. Scientists from the University of Pennsylvania used a porcine liver to treat a brain-dead person with liver failure12. The current study was performed to preliminarily evaluate the feasibility of pig-to-human liver xenotransplantation. The use of genetic modification and a designated pathogen-free environment may have prevented hyperacute rejection and potential PERV, PCMV or other porcine virus infections in the recipient.
As described, a heterotopic auxiliary liver transplantation was performed. To ensure the best match, the calibre and flow velocity of main blood vessels in the donor and recipient were assessed before surgery. This guaranteed sufficient blood perfusion in the xenograft and hemodynamic stability in the recipient, avoiding graft dysfunction caused by haemodynamic disorders, as reported in ref. 6. Auxiliary liver transplantation is an ideal bridge therapy for individuals with liver failure, because it is not difficult to remove pig liver and reconstruct the IVC when the function of the original liver is restored or when a suitable donor liver is available. We removed the xenograft and reconstructed the IVC at the end of the study to simulate the abovementioned situation. Moreover, our heterotopic auxiliary liver transplantation protocol improved the efficiency of interventional thrombolysis directly from the deep vein of the lower limb. The first case of pig-to-human heart xenotransplantation found microthrombi in the terminal stage biopsies7. Similarly, the current study found that D-dimer levels were transiently elevated shortly after surgery (Extended Data Fig. 5a). Timely thrombolysis was then used to keep the xenograft functional.
Indeed, the flow in the infrarenal IVC is not physiological. To achieve physiological haemodynamics, we must perform auxiliary partial orthotopic liver transplantation. However, this will remove part of the original liver and may cause potential complications such as liver malfunction, bile leakage or bleeding in patients. Because our goal is to assist patients with acute liver failure through the critical period, there is no need to perform a transplantation that fully conforms to physiology. As long as the xenograft can provide metabolic and coagulation functions for a certain time, this transplantation is sufficient. In this study, we used the blood flow of the IVC to supply the xenograft, which then successfully returned to the heart. Throughout the whole study, no oedema was observed in the lower limbs, indicating that the lower limb circulation was guaranteed. More importantly, the xenograft remained functional and the haemodynamics remained stable until study completion. Therefore, non-physiological flow in this study did not cause severe disturbance.
Hyperacute rejection is one of the most critical issues with xenotransplantation in preclinical models18. Fortunately, no evidence of hyperacute rejection was found in the current study. In addition to editing the glycoprotein α-galactosyltransferase 1 gene, a series of immunosuppressive agents were used, of which tacrolimus (FK506) played a vital role. During the early stage of this xenotransplantation, we used tacrolimus at a concentration of 5 mg l−1 (the upper limit of normal), according to our previous protocol. However, a high blood concentration of tacrolimus was noted at postoperative day 2, which might result from the heterogeneity of drug metabolism. We adjusted the dose in time. At the late stage of this experiment, the level of total bilirubin was elevated, which may be related to the toxicity of tacrolimus.
Whether to use Rituxan (rituximab) during induction immunosuppression was one of the focuses of our pre-operative discussion. Because of the huge advantages of gene editing, humoral immunity no longer has a major impact on graft survival. Therefore, Rituxan was not included in the immunosuppression strategy of works related to liver xenotransplantation19,20. Similarly, we did not use Rituxan in our previous trails of pig-to-monkey xenotransplantation, because B cells were not activated in these studies13. Therefore, in this study, Rituxan was not used initially. When B cells started to be augmented, we had to adopt Rituxan, along with plasma exchange and intravenous immunoglobulin therapy, which theoretically can remove the formed antibodies and plasmacytes. This trial indicates that the activation of B cells might occur in pig-to-human liver xenotransplantation. Further investigation is needed before we can incorporate Rituxan into our induction immunosuppressive strategy.
The discrepancy in ALT and AST amounts was unexpected and something that has not been observed in previous animal studies. More interestingly, a spike in AST during the early stage was detected in a pig-to-human heart xenotransplantation performed in a previous study6. It is plausible that AST was released by myocardial cells. This is supported by the early increase in creatine kinase and creatinine kinase-myocardial band amounts observed at the same time point (Extended Data Fig. 7e). Consequently, myocardial damage should be assessed at the early stage of liver transplantation and pharmacological myocardial protection implemented if necessary. Notably, some cholestasis was observed in the recipient’s original liver tissue on day 10, which may explain the elevated bilirubin observed later. However, this was absent in the xenograft. Thus, it is probable that current therapeutic drugs are slightly less toxic to pig liver than to human liver.
Abnormity in coagulation is a main cause of xenograft dysfunction21, and occurred in the first pig-to-human cardiac xenotransplantation7 and in our previous cases of pig-to-monkey liver xenotransplantation. However, no serious bleeding or clotting disorder occurred in the current case. PT remained relatively stable after surgery, APTT increased transiently at the early stage and later declined, and PLT decreased transiently in the early stage and later increased. Bleeding disorders and coagulopathies were considerably milder in this brain-dead recipient than in previous monkey recipients, indicating that humanized genetic modifications may function better in humans. Because of the advantages of heterotopic auxiliary liver transplantation, we were able to intervene after the early elevation of D-dimer and prevent potential PV thrombosis.
Future studies will need to choose between a bridge graft or permanent placement of xenotransplantation. Although the xenograft could secrete bile and produce porcine albumin in this study, it is unlikely that the production of bile and porcine albumin was enough to support the human body for a long period. Consequently, as indicated in ref. 17, current liver xenotransplantation modalities may be more suitable as an adjuvant bridge therapy for individuals with liver failure who are waiting for a human liver. Nevertheless, it will be important to design effective orthotopic pig-to-human liver xenotransplantation methods for future patients.
We admit the limitations of this study. First, at the request of the recipient’s family members, the study was terminated on day 10, which made the follow-up period insufficient to analyse alterations in xenograft function over a long period. Second, at present, we could measure only the basic functions of the liver, such as the synthesis of albumin and the secretion of bile. However, this unique pig-to-human liver xenotransplantation can still provide critical information that cannot be provided by animal experiments alone.
Methods
Recipient selection and ethical review
The recipient was an adult, who was diagnosed with brain death on 7 March 2024. The recipient maintained stable circulation and had no underlying diseases. Brain death was determined by six critical care medicine and neurosurgery experts according to World Brain Death Project-Determination of Brain Death/Death by Neurologic Criteria and the Regulations and Procedures of the National Health Commission of the People’s Republic of China/Brain Injury Evaluation Quality Control Centre (PRC/NHC/BQCC), following three independent assessments. The six experts are entirely independent of the research group and have no personnel overlap or connection with each other. The study was approved by the Academic Committee (28 December 2023), Medical Ethics Committee (registration number: KY20232438-C-1, 4 January 2024), Clinical Application and Ethics Committee of Human Organ Transplantation (registration number: 20231227-1, 29 December 2023) and the Ethics Committee of Experimental Animal Welfare (registration number: IACUC2023001, 4 January 2024) of Xijing Hospital attached to the Fourth Military Medical University. After receiving a detailed overview of the study procedures, the recipient’s four immediate family members signed an informed consent on 8 March 2024. In addition, none of the doctors, nurses, researchers and staff involved in the study raised any objections or complaints about the content of the study, and signed a joint agreement. The surgery was officially performed on 10 March 2024. At the request of the recipient’s family, the study was artificially terminated 10 days after surgery (20 March 2024). The whole trial course was supervised by the relevant review agencies listed above. The identity information and privacy of patients and their families have been strictly kept confidential throughout this entire process. We submitted the initial paper on 5 June 2024. The files relating to ethical approval, clinical trial research protocol, informed consent for the recipient’s family and determination of recipient brain death are included in the Supplementary Information.
Donor profile and xenograft acquisition
A 7-month-old male Bama miniature pig (Sus scrofa domestica) with six genetic modifications (GGTA1-KO/β4GalALNT2-KO/CMAH-KO/hCD46/hCD55/hTHBD) was used as the donor in this study. The pig was kindly provided by Clonorgan Biotechnology in Chengdu, China, and was isolated in the Laboratory Animal Center Facilities of Xijing Hospital. Flow cytometry, western blotting and IHC were used to determine whether gene editing in the donor pig occurred as expected. The donor pig underwent a comprehensive pre-operative laboratory and imaging examination by a multidisciplinary team to confirm it was compatible with the recipient. The porcine liver, weighing 700 g, was obtained in a sterile surgical environment. The donor pig was anaesthetized and a median incision was made in the abdomen to expose the abdominal aorta, IVC, liver, kidney, PV, hepatic artery, bile duct, and so on. The abdominal aorta was perfused with 2,000 ml of hypertonic citrate purine solution (Shanghai Blood Transfusion Technology Co., Ltd) and 1,000 ml of Celsior solution (flushing and cold storage solution for solid organ preservation; Institut Georges Lopez S.A.S.) at 0–4 °C. IVC drainage was performed. The PV was intubated with 2,000 ml of Celsior solution at 0–4 °C. Sterile ice cubes were used to cool the liver. After adequate perfusion with Celsior solution at 0–4 °C, the liver was excised and trimmed in 1,000 ml of the same solution before implantation.
Heterotopic auxiliary liver transplant
The recipient was routinely anaesthetized and sterilized, and a cross-like abdominal incision was made (Extended Data Fig. 3c). The abdominal aorta and IVC were dissociated and the IVC was transected below the level of the right renal vein. Subsequently, the supra-hepatic IVC of the donor liver was connected to the proximal end of the recipient’s IVC and the porcine PV was anastomosed with the distal end of the transected IVC. After reperfusion of the PV blood flow, the porcine liver looked ruddy with a good texture, and goldish bile began to flow shortly thereafter. The hepatic artery of the donor liver was then opened after its end-to-side anastomosis with the recipient’s abdominal aorta. The bile was drained out of the body and two abdominal drains were placed (Extended Data Fig. 3c). At the end of the study (day 10), the xenograft was surgically removed and the IVC was reconstructed using an artificial vessel. A video of the detailed surgical procedures is included in the Supplementary Information.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
FACS gating strategies and full scans of all the gels as well as blots are provided in Supplementary Figs. 1–3. The data that support the findings of this study are available from the corresponding author upon reasonable request. Source data are provided with this paper.
References
Pan, D. et al. Progress in multiple genetically modified minipigs for xenotransplantation in China. Xenotransplantation 26, e12492 (2019).
Cooper, D. K., Ekser, B., Ramsoondar, J., Phelps, C. & Ayares, D. The role of genetically engineered pigs in xenotransplantation research. J. Pathol. 238, 288–299 (2016).
Griffith, B. P. et al. Genetically modified porcine-to-human cardiac xenotransplantation. N. Engl. J. Med. 387, 35–44 (2022).
Montgomery, R. A. et al. Results of two cases of pig-to-human kidney xenotransplantation. N. Engl. J. Med. 386, 1889–1898 (2022).
Loupy, A. et al. Immune response after pig-to-human kidney xenotransplantation: a multimodal phenotyping study. Lancet 402, 1158–1169 (2023).
Moazami, N. et al. Pig-to-human heart xenotransplantation in two recently deceased human recipients. Nat. Med. 29, 1989–1997 (2023).
Mohiuddin, M. M. et al. Graft dysfunction in compassionate use of genetically engineered pig-to-human cardiac xenotransplantation: a case report. Lancet 402, 397–410 (2023).
Dai, Y. et al. Targeted disruption of the alpha1,3-galactosyltransferase gene in cloned pigs. Nat. Biotechnol. 20, 251–255 (2002).
Petersen, B. et al. Efficient production of biallelic GGTA1 knockout pigs by cytoplasmic microinjection of CRISPR/Cas9 into zygotes. Xenotransplantation 23, 338–346 (2016).
Petersen, B. et al. Transgenic expression of human heme oxygenase-1 in pigs confers resistance against xenograft rejection during ex vivo perfusion of porcine kidneys. Xenotransplantation 18, 355–368 (2011).
Petersen, B. et al. Pigs transgenic for human thrombomodulin have elevated production of activated protein C. Xenotransplantation 16, 486–495 (2009).
Regalado, A. A brain-dead man was attached to a gene-edited pig liver for three days. MIT Technology Review www.technologyreview.com/2024/01/18/1086791/brain-dead-man-gene-edited-pig-liver/ (2024).
Zhang, Z. et al. Cytokine profiles in Tibetan macaques following α-1,3-galactosyltransferase-knockout pig liver xenotransplantation. Xenotransplantation 24, e12321 (2017).
Zhang, X. et al. The resurgent landscape of xenotransplantation of pig organs in nonhuman primates. Sci. China Life Sci. 64, 697–708 (2021).
Zhang, X. et al. A review of pig liver xenotransplantation: current problems and recent progress. Xenotransplantation 26, e12497 (2019).
Ma, L. Xijing Hospital transplants pig’s liver to monkey. China Daily www.chinadaily.com.cn/china/2013-06/06/content_16580042.htm (2013).
Mallapaty, S. First pig liver transplanted into a person lasts for 10 days. Nature 627, 710–711 (2024).
Cooper, D. K. C. et al. Xenotransplantation—the current status and prospects. Br. Med. Bull. 125, 5–14 (2018).
Shah, J. A. et al. Prolonged survival following pig-to-primate liver xenotransplantation utilizing exogenous coagulation factors and costimulation blockade. Am. J. Transplant. 17, 2178–2185 (2017).
Shah, J. A. et al. A bridge to somewhere. Ann. Surg. 263, 1069–1071 (2016).
Cowan, P. J., Robson, S. C. & d’Apice, A. J. Controlling coagulation dysregulation in xenotransplantation. Curr. Opin. Organ Transplant. 16, 214–221 (2011).
Acknowledgements
This work was supported by grants from National Natural Science Foundation of China (grant nos. 82325007, 92468202, 82371793, 82070671, 82170667) and the National Key Research and Development Program of China (grant no. 2021YFA1100502).
Author information
Authors and Affiliations
Contributions
K.-S.T. and Z.-X.Y. conducted the surgery with the participation of S.-Q.Y., Y.-L.Y., W.-J.S., D.-S.W., Z.-C.L., H.-M.L., Y.C. and R.D. X.Z. prepared the donor pig and collected the experimental data. H.-T.Z. monitored the patient throughout the investigation. S.-R.S., M.Y., J.-P.L., W.-X.D., Z.W., J.-W.W., J.-Y.L., M.-W.Z., X.-J.Z., W.Y., W.-J.Q., D.-M.B., L.L. and M.L. assisted with the surgery and recipient management. Z.-B.L., H.X. and D.W. prepared the draft of the manuscript. H.Z. and J.-L.D. undertook the histological observation. D.-K.P. established the gene-edited donor pig. L.W. planned and wrote the article. H.-L.D., L.W. and K.-F.D. designed and supervised the whole study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature thanks Arthur Caplan, Muhammad Mohiuddin and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Pathogenic surveillance of the donor pig.
a, The PCR combined with gel electrophoresis detecting the presence of PCMV in the PBMCs of the recipient and the xenograft. b, The PCR combined with gel electrophoresis detecting the presence of PERV as well as microchimerism in the PBMCs of the recipient and the xenograft. PERV-ABC, the sequence shared by PERV-A, PERV-B and PERV-C. PERV-C, the sequence specifically belongs to PERV-C. RPP30 was used as the control gene. NTC, no template control. For gel source data, see Supplementary Fig. 1. Extended Data Fig. 1a,b contains 1 biological and technical repetition, and 3 independent experiments were carried out.
Extended Data Fig. 2 The heterotopic auxiliary liver xenotransplantation procedure.
a, The diameters of the portal vein (PV) and the inferior vena cava (IVC) of the recipient and the donor pig detected by vessel segmentation and ultrasound. b, Photos of the donor liver at different time points throughout the study. c, Photos of the vascular anastomosis between the recipient and the donor liver during surgery. d, A schematic depiction of the surgery. ①, ② and ③ represent the vascular anastomosis captioned in c.
Extended Data Fig. 3 Other surgery details.
a, b, Images of vessel segmentation in the donor pig. c, A photo of the recipient’s abdomen, showing the surgical incision, abdominal drains, and bile drain. d, A photo of the reconstruction of the recipient’s IVC by artificial vessel once the porcine liver was removed. e, The ultrasound-detected blood flow velocity of IVC after artificial vessel reconstruction.
Extended Data Fig. 4 Hemodynamic monitoring of the xenograft.
a, The ultrasound-detected blood flow velocity of the hepatic artery, the portal vein, and the hepatic vein of the xenograft at different time points of the study. The exact speed of blood flow is labelled correspondingly. b, The quantitative result of a. c, The ultrasound-detected portal vein flow (PVF) of the xenograft at different time points of the study.
Extended Data Fig. 5 Bleeding and coagulation monitoring of the recipient.
a, The indicators of coagulation function of the recipient at different time points of the study. b, The serum levels of coagulation factors of the recipient at different time points of the study. Extended Data Fig. 5a,b contains 1 biological and technical repetition.
Extended Data Fig. 6 Immune strategy of the recipient.
The immunosuppression strategy adopted in this study.
Extended Data Fig. 7 Immune monitoring of the recipient.
a, The levels of total T, B, CD3+CD4+ T and CD3+CD8+ T cells in the recipient’s blood at different time points of the study. b, The levels of IgM and IgG in the serum of the recipient at different time points of the study. c, The levels of C-reactive protein (CRP) and procalcitonin (PCT) in the serum of the recipient at different time points of the study. d, The plasma concentrations of FK506 and mycophenolate mofetil (MMF) of the recipient at different time points of the study. e, The serum levels of myocardial enzymes of the recipient at different time points of the study. Extended Data Fig. 7a–e contains 1 biological and technical repetition.
Supplementary information
Supplementary Information
Supplementary Figs. 1–3, Tables 1–4, Methods and References.
Supplementary Video 1
Gene-modified pig to brain-dead recipient heterotopic auxiliary liver transplantation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tao, KS., Yang, ZX., Zhang, X. et al. Gene-modified pig-to-human liver xenotransplantation. Nature 641, 1029–1036 (2025). https://doi.org/10.1038/s41586-025-08799-1
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41586-025-08799-1
This article is cited by
-
From quantum computing to mRNA therapeutics: seven technologies to watch in 2026
Nature (2026)
-
Extracorporeal liver cross-circulation using transgenic xenogeneic pig livers with brain-dead human decedents
Nature Medicine (2026)
-
Reshaping transplantation with AI, emerging technologies and xenotransplantation
Nature Medicine (2025)
-
Promise and pitfalls of liver xenotransplantation
Nature Reviews Gastroenterology & Hepatology (2025)
-
Advanced bioartificial organs: genetically modified pig liver as a promising bridge for human liver failure
Signal Transduction and Targeted Therapy (2025)