Abstract
Multiple myeloma evolution is characterized by the accumulation of genomic drivers over time. To unravel this timeline and its impact on clinical outcomes, we analyzed 421 whole-genome sequences from 382 patients. Using clock-like mutational signatures, we estimated a time lag of two to four decades between the initiation of events and diagnosis. We demonstrate that odd-numbered chromosome trisomies in patients with hyperdiploidy can be acquired simultaneously with other chromosomal gains (for example, 1q gain). We show that hyperdiploidy is acquired after immunoglobulin heavy chain translocation when both events co-occur. Finally, patients with early 1q gain had adverse outcomes similar to those with 1q amplification (>1 extra copy), but fared worse than those with late 1q gain. This finding underscores that the 1q gain prognostic impact depends more on the timing of acquisition than on the number of copies gained. Overall, this study contributes to a better understanding of the life history of myeloma and may have prognostic implications.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
GMMG-HD6 has been uploaded on EGA—EGAD50000000681, EGAD50000000682 and EGAD50000000683. MSKCC WGS data have been uploaded to EGA—EGAD00001011132. RRMM WGS data have been uploaded to EGA—EGAS00001006538, EGAS00001004363, EGAS00001004805 and EGAS00001005973. Source data are provided with this paper.
Code availability
The code used for the timing analysis is provided in Supplementary Data 2 and on GitHub at https://github.com/bachisiozic/Timing-the-first-multi-gain-events-in-Multiple-Myeloma/tree/main.
References
Maura, F. et al. Moving from cancer burden to cancer genomics for smoldering myeloma: a review. JAMA Oncol. 6, 425–432 (2020).
Morgan, G. J., Walker, B. A. & Davies, F. E. The genetic architecture of multiple myeloma. Nat. Rev. Cancer 12, 335–348 (2012).
Manier, S. et al. Genomic complexity of multiple myeloma and its clinical implications. Nat. Rev. Clin. Oncol. 14, 100–113 (2017).
Rajkumar, S. V., Landgren, O. & Mateos, M. V. Smoldering multiple myeloma. Blood 125, 3069–3075 (2015).
Kyle, R. A. et al. Long-term follow-up of monoclonal gammopathy of undetermined significance. N. Engl. J. Med. 378, 241–249 (2018).
Kyle, R. A. et al. Clinical course and prognosis of smoldering (asymptomatic) multiple myeloma. N. Engl. J. Med. 356, 2582–2590 (2007).
Barwick, B. G., Gupta, V. A., Vertino, P. M. & Boise, L. H. Cell of origin and genetic alterations in the pathogenesis of multiple myeloma. Front. Immunol. 10, 1121 (2019).
Bergsagel, P. L. et al. Cyclin D dysregulation: an early and unifying pathogenic event in multiple myeloma. Blood 106, 296–303 (2005).
Chesi, M. & Bergsagel, P. L. Molecular pathogenesis of multiple myeloma: basic and clinical updates. Int. J. Hematol. 97, 313–323 (2013).
Chesi, M. et al. Dysregulation of cyclin D1 by translocation into an IgH γ switch region in two multiple myeloma cell lines. Blood 88, 674–681 (1996).
Chesi, M. et al. Frequent translocation t(4;14)(p16.3;q32.3) in multiple myeloma is associated with increased expression and activating mutations of fibroblast growth factor receptor 3. Nat. Genet. 16, 260–264 (1997).
Chojnacka, M., Diamond, B., Landgren, O. & Maura, F. Defining genomic events involved in the evolutionary trajectories of myeloma and its precursor conditions. Semin. Oncol. 49, 11–18 (2022).
Cirrincione, A. et al. Revealing novel mechanisms underlying inactivation of tumor suppressor genes on duplicated chromosomes in multiple myeloma. Blood 142, 874–874 (2023).
Fonseca, R. et al. The recurrent IgH translocations are highly associated with nonhyperdiploid variant multiple myeloma. Blood 102, 2562–2567 (2003).
Rustad, E. H. et al. Revealing the impact of structural variants in multiple myeloma. Blood Cancer Discov. 1, 258–273 (2020).
Walker, B. A. et al. Mutational spectrum, copy number changes, and outcome: results of a sequencing study of patients with newly diagnosed myeloma. J. Clin. Oncol. 33, 3911–3920 (2015).
Walker, B. A. et al. A high-risk, double-hit, group of newly diagnosed myeloma identified by genomic analysis. Leukemia 33, 159–170 (2018).
Bergsagel, P. L. et al. Promiscuous translocations into immunoglobulin heavy chain switch regions in multiple myeloma. Proc. Natl Acad. Sci. USA 93, 13931–13936 (1996).
Bolli, N. et al. Genomic patterns of progression in smoldering multiple myeloma. Nat. Commun. 9, 3363 (2018).
Boyle, E. M. et al. The molecular make up of smoldering myeloma highlights the evolutionary pathways leading to multiple myeloma. Nat. Commun. 12, 293 (2021).
Maura, F. et al. Genomic landscape and chronological reconstruction of driver events in multiple myeloma. Nat. Commun. 10, 3835 (2019).
Misund, K. et al. MYC dysregulation in the progression of multiple myeloma. Leukemia 34, 322–326 (2020).
Smadja, N. V. et al. Further cytogenetic characterization of multiple myeloma confirms that 14q32 translocations are a very rare event in hyperdiploid cases. Genes Chromosomes Cancer 38, 234–239 (2003).
Bolli, F. et al. Genomic patterns of progression in smoldering multiple myeloma. Nat. Commun. 9, 3363 (2018).
Barwick, B. G. et al. Multiple myeloma immunoglobulin lambda translocations portend poor prognosis. Nat. Commun. 10, 1911 (2019).
Rustad, E. H. et al. Timing the initiation of multiple myeloma. Nat. Commun. 11, 1917 (2020).
Bustoros, M. et al. Genomic profiling of smoldering multiple myeloma identifies patients at a high risk of disease progression. J. Clin. Oncol. 38, 2380–2389 (2020).
Oben, B. et al. Whole-genome sequencing reveals progressive versus stable myeloma precursor conditions as two distinct entities. Nat. Commun. 12, 1861 (2021).
Walker, B. A. et al. Identification of novel mutational drivers reveals oncogene dependencies in multiple myeloma. Blood 132, 587–597 (2018).
D’Agostino, M. et al. Second Revision of the International Staging System (R2-ISS) for overall survival in multiple myeloma: a European Myeloma Network (EMN) report within the HARMONY project. J. Clin. Oncol. 40, 3406–3418 (2022).
Weinhold, N. et al. Chromosome 1q21 abnormalities refine outcome prediction in patients with multiple myeloma: a meta-analysis of 2,596 trial patients. Haematologica 106, 2754–2758 (2021).
Walker, B. A. et al. A high-risk, Double-Hit, group of newly diagnosed myeloma identified by genomic analysis. Leukemia 33, 159–170 (2019).
Maura, F. et al. Genomic classification and individualized prognosis in multiple myeloma. J. Clin. Oncol. 42, 1229–1240 (2024).
Kaiser, M. F. et al. Co-occurrence of cytogenetic abnormalities and high-risk disease in newly diagnosed and relapsed/refractory multiple myeloma. J. Clin. Oncol. https://doi.org/10.1200/jco-24-01253 (2025).
Weinhold, N. et al. Clonal selection and double-hit events involving tumor suppressor genes underlie relapse in myeloma. Blood 128, 1735–1744 (2016).
Lannes, R. et al. In multiple myeloma, high-risk secondary genetic events observed at relapse are present from diagnosis in tiny, undetectable subclonal populations. J. Clin. Oncol. 41, 1695–1702 (2023).
Gerstung, M. et al. The evolutionary history of 2,658 cancers. Nature 578, 122–128 (2020).
Mitchell, T. J. et al. Timing the landmark events in the evolution of clear cell renal cell cancer: TRACERx renal. Cell 173, 611–623 e617 (2018).
Goldschmidt, H. et al. Elotuzumab in combination with lenalidomide, bortezomib, dexamethasone and autologous transplantation for newly-diagnosed multiple myeloma: results from the randomized phase III GMMG-HD6 trial. Blood 138, 486 (2021).
Alexandrov, L. B. et al. The repertoire of mutational signatures in human cancer. Nature 578, 94–101 (2020).
Maura, F. et al. A practical guide for mutational signature analysis in hematological malignancies. Nat. Commun. 10, 2969 (2019).
Degasperi, A. et al. Substitution mutational signatures in whole-genome-sequenced cancers in the UK population. Science 376, abl9283 (2022).
Walker, B. A. et al. APOBEC family mutational signatures are associated with poor prognosis translocations in multiple myeloma. Nat. Commun. 6, 6997 (2015).
Maura, F. et al. Biological and prognostic impact of APOBEC-induced mutations in the spectrum of plasma cell dyscrasias and multiple myeloma cell lines. Leukemia 32, 1044–1048 (2018).
Samur, M. K. et al. Genome-wide somatic alterations in multiple myeloma reveal a superior outcome group. J. Clin. Oncol. 38, 3107–3118 (2020).
Abascal, F. et al. Somatic mutation landscapes at single-molecule resolution. Nature 593, 405–410 (2021).
Alexandrov, L. B. et al. Clock-like mutational processes in human somatic cells. Nat. Genet. 47, 1402–1407 (2015).
Cagan, A. et al. Somatic mutation rates scale with lifespan across mammals. Nature 604, 517–524 (2022).
Moore, L. et al. The mutational landscape of human somatic and germline cells. Nature 597, 381–386 (2021).
Luquette, L. J. et al. Single-cell genome sequencing of human neurons identifies somatic point mutation and indel enrichment in regulatory elements. Nat. Genet. 54, 1564–1571 (2022).
Machado, H. E. et al. Diverse mutational landscapes in human lymphocytes. Nature 608, 724–732 (2022).
Maura, F. et al. The mutagenic impact of melphalan in multiple myeloma. Leukemia 35, 2145–2150 (2021).
D’Agostino, M. et al. Early relapse risk in patients with newly diagnosed multiple myeloma characterized by next-generation sequencing. Clin. Cancer Res. 26, 4832–4841 (2020).
Misund, K. et al. Clonal evolution after treatment pressure in multiple myeloma: heterogenous genomic aberrations and transcriptomic convergence. Leukemia 36, 1887–1897 (2022).
Maura, F., Rustad, E. H., Boyle, E. M. & Morgan, G. J. Reconstructing the evolutionary history of multiple myeloma. Best Pract. Res. Clin. Haematol. 33, 101145 (2020).
Rustad, E. H. et al. mmsig: a fitting approach to accurately identify somatic mutational signatures in hematological malignancies. Commun. Biol. 4, 424 (2021).
Dentro, S. C. et al. Characterizing genetic intra-tumor heterogeneity across 2,658 human cancer genomes. Cell 184, 2239–2254 e2239 (2021).
Murray, D. et al. Detection and prevalence of monoclonal gammopathy of undetermined significance: a study utilizing mass spectrometry-based monoclonal immunoglobulin rapid accurate mass measurement. Blood Cancer J. 9, 102 (2019).
Thorsteinsdottir, S. et al. Prevalence of smoldering multiple myeloma based on nationwide screening. Nat. Med. 29, 467–472 (2023).
Cirrincione, A. M. et al. The biological and clinical impact of deletions before and after large chromosomal gains in multiple myeloma. Blood https://doi.org/10.1182/blood.2024024299 (2024).
Poos, A. M. et al. Resolving therapy resistance mechanisms in multiple myeloma by multiomics subclone analysis. Blood 142, 1633–1646 (2023).
Diamond, B. et al. Tracking the evolution of therapy-related myeloid neoplasms using chemotherapy signatures. Blood 141, 2359–2371 (2023).
Maura, F. et al. Initial whole-genome sequencing of plasma cell neoplasms in first responders and recovery workers exposed to the World Trade Center attack of September 11, 2001. Clin. Cancer Res. 27, 2111–2118 (2021).
Landgren, O. et al. Monoclonal gammopathy of undetermined significance (MGUS) consistently precedes multiple myeloma: a prospective study. Blood 113, 5412–5417 (2009).
Diamond, B. T. et al. Tracking the evolution of therapy-related myeloid neoplasms using chemotherapy signatures. Blood https://doi.org/10.1182/blood.2022018244 (2023).
Fonseca, R. et al. Prognostic value of chromosome 1q21 gain by fluorescent in situ hybridization and increase CKS1B expression in myeloma. Leukemia 20, 2034–2040 (2006).
Schmidt, T. M., Fonseca, R. & Usmani, S. Z. Chromosome 1q21 abnormalities in multiple myeloma. Blood Cancer J. 11, 83 (2021).
Shah, V. et al. Prediction of outcome in newly diagnosed myeloma: a meta-analysis of the molecular profiles of 1905 trial patients. Leukemia 32, 102–110 (2018).
Croft, J. et al. Copy number evolution and its relationship with patient outcome—an analysis of 178 matched presentation-relapse tumor pairs from the Myeloma XI trial. Leukemia 35, 2043–2053 (2021).
Schmidt, T. M. et al. Gain of chromosome 1q is associated with early progression in multiple myeloma patients treated with lenalidomide, bortezomib, and dexamethasone. Blood Cancer J. 9, 94 (2019).
Abdallah, N. et al. Clinical characteristics and treatment outcomes of newly diagnosed multiple myeloma with chromosome 1q abnormalities. Blood Adv. 4, 3509–3519 (2020).
Perrot, A. et al. Development and validation of a cytogenetic prognostic index predicting survival in multiple myeloma. J. Clin. Oncol. 37, 1657–1665 (2019).
Korde, N. et al. Treatment with carfilzomib-lenalidomide-dexamethasone with lenalidomide extension in patients with smoldering or newly diagnosed multiple myeloma. JAMA Oncol. 1, 746–754 (2015).
Landgren, O. et al. Safety and effectiveness of weekly carfilzomib, lenalidomide, dexamethasone, and daratumumab combination therapy for patients with newly diagnosed multiple myeloma: the MANHATTAN nonrandomized Clinical trial. JAMA Oncol. 7, 862–868 (2021).
Maura, F. et al. Genomic and immune signatures predict clinical outcome in newly diagnosed multiple myeloma treated with immunotherapy regimens. Nat. Cancer https://doi.org/10.1038/s43018-023-00657-1 (2023).
Landau, H. J. et al. Accelerated single cell seeding in relapsed multiple myeloma. Nat. Commun. 11, 3617 (2020).
Reisinger, E. et al. OTP: an automatized system for managing and processing NGS data. J. Biotechnol. 261, 53–62 (2017).
ICGC/TCGA Pan-Cancer Analysis of Whole Genomes Consortium Pan-cancer analysis of whole genomes. Nature 578, 82–93 (2020).
Danecek, P. et al. Twelve years of SAMtools and BCFtools. Gigascience 10, giab008 (2021).
Ashby, C. et al. Structural variants shape the genomic landscape and clinical outcome of multiple myeloma. Blood Cancer J. 12, 85 (2022).
Degasperi, A. et al. A practical framework and online tool for mutational signature analyses show intertissue variation and driver dependencies. Nat. Cancer 1, 249–263 (2020).
Maura, F. et al. Molecular evolution of classic Hodgkin lymphoma revealed through whole-genome sequencing of Hodgkin and Reed Sternberg cells. Blood Cancer Discov. 4, 208–227 (2023).
Gagnon, M. F. et al. Superior detection rate of plasma cell FISH using FACS-FISH. Am. J. Clin. Pathol. 161, 60–70 (2024).
Peterson, J. F. et al. Whole genome mate-pair sequencing of plasma cell neoplasm as a novel diagnostic strategy: a case of unrecognized t(2;11) structural variation. Clin. Lymphoma Myeloma Leuk. 19, 598–602 (2019).
Sidana, S. et al. Rapid assessment of hyperdiploidy in plasma cell disorders using a novel multi-parametric flow cytometry method. Am. J. Hematol. 94, 424–430 (2019).
Neben, K. et al. Combining information regarding chromosomal aberrations t(4;14) and del(17p13) with the International Staging System classification allows stratification of myeloma patients undergoing autologous stem cell transplantation. Haematologica 95, 1150–1157 (2010).
Acknowledgements
This work was supported by the Myeloma Solutions Fund, Paula and Rodger Riney Multiple Myeloma Research Program Fund, the Tow Foundation, Sylvester Comprehensive Cancer Center National Cancer Institute (NCI) Core Grant (P30 CA 240139), Memorial Sloan Kettering Cancer Center NCI Core Grant (P30 CA 008748) and NYU NCI Core Grant (P30CA016087). F.M. was supported by the Leukemia and Lymphoma Society (LLS), the International Myeloma Society (IMS), the Department of Defence and the National Institutes of Health (NIH)–NCI. G.J.M. received grant support through a Translational Research Program award from the LLS (6020-20). K.H.M. has received funding from the Multiple Myeloma Research Foundation (MMRF), the American Society of Hematology and the IMS. A.M.P. is funded by the Medical Data Scientist Program of Heidelberg University, Faculty of Medicine. N.W. is funded by the Advanced Medical Scientist Program of Heidelberg University, Faculty of Medicine. The Heidelberg Team thanks the Sample Processing Lab, the High-Throughput Sequencing Unit of the Genomics & Proteomics Core Facility and the Omics IT and Data Management Core Facility of the German Cancer Research Center (DKFZ), the DKFZ–Heidelberg Center for Personalized Oncology (DKFZ–HIPO) office, the Biobank Multiple Myeloma UKHD and the Myeloma Registry for excellent services. Support and funding of the project provided by the Dietmar Hopp Foundation and the NCT Heidelberg Molecular Precision Oncology Program (project K08K) is gratefully acknowledged. Data storage service provided by SDS@hd is supported by the Ministry of Science, Research and the Arts Baden-Württemberg (MWK) and the German Research Foundation (DFG) through grants INST 35/1314-1 FUGG and INST 35/1503-1 FUGG. L.B.B. is supported by NIH–NCI (R37CA272883).
Author information
Authors and Affiliations
Contributions
F.M., M.S.R. and N.W. designed and supervised the study. F.M., M.S.R., N.W., M.K., A.M.P., K.M., M.C., B.D., P.B., L.J., P.R., S.H., M.A.B., D.G., Y.Z., F.D., G.M. and A.D. collected data. F.M., M.S.R., N.W., M.K. and A.M.P. generated the data and wrote the manuscript. F.M., M.S.R., N.W., M.K., A.M.P., B.Z., A.C. and M.P. analyzed the data. N.K., S.U., O.L., E.K.M., H.G., K.C.W., A.L. and R.F. supervised the clinical trials and collected clinical data. V.R., S.K. and L.B. collected and analyzed the FISH data from Mayo Clinic.
Corresponding authors
Ethics declarations
Competing interests
O.L. has received research funding from NIH, NCI, U.S. Food and Drug Administration, MMRF, International Myeloma Foundation, LLS, Myeloma Solutions Fund, Paula and Rodger Riney Multiple Myeloma Research Program Fund, the Tow Foundation, Perelman Family Foundation, Rising Tide Foundation, Amgen, Celgene, Janssen, Takeda, Glenmark, Seattle Genetics, Karyopharm; Honoraria/ad boards: Adaptive, Amgen, Binding Site, Bristol Myers Squibb (BMS), Celgene, Cellectis, Glenmark, Janssen, Juno, Pfizer; and serves on Independent Data Monitoring Committees for clinical trials lead by Takeda, Merck, Janssen, Theradex. G.J.M. has received funding from NIH, NCI, MMRF, LLS, Perelman Family Foundation, Amgen, Celgene, Janssen and Takeda; has received honoraria or advisory board fees from Adaptive, Amgen, BMS, Celgene and Janssen; and serves on Independent Data Monitoring Committees for clinical trials led by Takeda, Karyopharm and Sanofi. E.K.M. reports consulting or advisory role, honoraria, research funding, travel accommodation and expenses from BMS (Celgene), GlaxoSmithKline (GSK), Janssen-Cilag, Oncopeptides, Pfizer, Sanofi, Stemline and Takeda. K.C.W. reports research grant from AbbVie, Amgen, BMS/Celgene, Janssen, GSK and Sanofi; and has received honoraria and consulting fees from AbbVie, Amgen, Adaptive Biotech, AstraZeneca, BMS/Celgene, BeiGene, Janssen, GSK, Karyopharm, Novartis, Oncopeptides, Pfizer, Roche Pharma, Sanofi, Stemline and Takeda. R.F. reports consulting or advisory role, honoraria, travel accommodation and expenses from Amgen, BMS (Celgene), GSK, Janssen-Cilag, Sanofi, Stemline and Takeda. K.H.S. has served on an advisory board for AbbVie, Amgen, BMS, GSK and Janssen; received honoraria for Adaptive Biotechnologies Corporation, Amgen, BMS, GSK, Janssen and Sanofi Genzyme; and has received research funding from AbbVie and Karyopharm Therapeutics. H.G. has received grants and/or provision of investigational medicinal product from BMS/Celgene, Dietmar-Hopp-Foundation, Janssen and Sanofi; research support from Amgen, BMS, Celgene, GlycoMimetics, GSK, Heidelberg Pharma, Hoffmann-La Roche, Janssen, Millenium Pfizer, Sanofi and Novartis; advisory board fees from BMS, GSK, Janssen and Sanofi; honoraria from Amgen, BMS, GSK, Janssen, Oncopeptides, Sanofi and Pfizer; and support for attending meetings and/or travel form Amgen, BMS, GSK, Janssen, Oncopeptides, Sanofi and Pfizer. N.K. has received research funding from Janssen and AbbVie, and has served on an advisory board for Janssen. K.H.M. has received funding from the Multiple Myeloma Research Foundation, the American Society of Hematology and the IMS. L.B.B. served as a consultant for Genentech. F.M. has received consulting fees from Medidata and Sanofi. B.D. reports consulting via an independent data review committee for Janssen. All other authors declare no competing interests.
Peer review
Peer review information
Nature Genetics thanks the anonymous reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
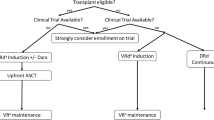
Extended Data Fig. 1 Study cohort genomic landscape.
The 12 newly diagnosed multiple myeloma (NDMM) genomic groups (ref. 33) and their distribution across the MSKCC and German cohorts included in this study. All defining features of the 12 groups are depicted. Heatmap colors: gray = wild type; red = monoallelic involvement; brown = biallelic involvement. Immunoglobulin heavy chain (IGH) canonical translocations are reported in brown. Presence of APOBEC and hyper-APOBEC is reported in red and brown, respectively. HY: hyperdiploid.
Extended Data Fig. 2 Impact of APOBEC on multiple myeloma clinical outcomes.
a, Comparison of mutational burden between the MSKCC and German cohorts included in this study. The P value was calculated using the Wilcoxon test. SBS: single base substitution. b,c, Impact of Hyper-APOBEC presence on progression-free survival (PFS) and overall survival (OS) in newly diagnosed multiple myeloma patients.
Extended Data Fig. 3 Clock-like signatures in B and myeloma cells.
a, Correlation between SBS1 and SBS5 mutational burden (clock-like signatures) and patients’ age at sample collection. Samples that did not fit into the linear model reported in Fig. 1b are plotted with transparency (residual > 1,900). Three samples with >8,000 SBS1 and SBS5 mutations were excluded for graphical purpose (MM119, MM165, and RRMM48). b, Comparison of SBS1 and SBS5 clock mutation rates between multiple myeloma and B-cell lymphoma. c, Comparison of SBS1 and SBS5 clock mutation rate between multiple myeloma (red line) and normal memory B cells (black line). Given the single cell colony expansion in normal memory B-cell data (ref. 51), only clonal variants were considered for multiple myeloma. SBS: single base substitution; NDMM: newly diagnosed multiple myeloma; RRMM: relapsed refractory multiple myeloma; Mel+ and Mel−: melphalan-exposed or not-exposed RRMM patients, respectively.
Extended Data Fig. 4 SBS mutational signature contribution in relapsed refractory multiple myeloma (RRMM).
This figure illustrates the contribution of SBS mutational signatures in RRMM, distinguishing between clonal and subclonal variants. P values were estimated using the Wilcoxon test.
Extended Data Fig. 5 APOBEC mutagenesis across time.
a, Comparison of APOBEC contribution in clonal variants between hyper-APOBEC and non-hyper-APOBEC. b–g, SBS mutational signature contribution among clonal and subclonal variants in samples with hyper-APOBEC.
Extended Data Fig. 6 Temporal relationship of distinct chromosomal aberrations.
a) Examples of molecular time estimates of HY patients with 1q gain. In the top case, the 1q was acquired at the same time as the HY multi-gain event. The middle case shows a 1q gain acquired at the same time as the HY multi-gain event, but later compared to the first case. The last case (bottom) has a 1q gain acquired independently after the HY multi-gain event. b–d) The molecular time estimates of chromosomal gains shared, selected or lost over time in patients with WGS data available at two different time points. c) Boxplot of estimated molecular time for gains of non-HY chromosomes (1, 2, 4, 6, 8, 10, 12, 13, 14, 16, 17, 18, 20, and 22) based on the absence or presence of canonical IGH translocations. c) Boxplot of estimated molecular time for gains of odd-numbered chromosomes typically seen in hyperdiploid myeloma (3, 5, 7, 9, 11, 15, 19, and 21) based on the presence (left box) or absence (right box) of canonical IGH translocations. d) Boxplot of estimated molecular time for LOH events in HY patients, divided into odd-numbered HY chromosomes (left box), and non-HY chromosomes (right box). Comparisons were performed using the Wilcoxon test.
Extended Data Fig. 7 Temporal patterns of chromosomal gains across the 12 genomic subgroups of multiple myeloma (ref. 33).
a, Estimated molecular time of all chromosomal duplications across the 12 genomic subgroups. b, Estimated molecular timeof odd-numbered hyperdiploid chromosomal duplications across the 12 genomic subgroups, considering only patients with a hyperdiploid profile. c, Estimated molecular time of 1q gains across the 12 genomic subgroups. Adjusted P values for comparisons in a–c are reported in Supplementary Table 8.
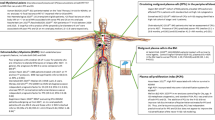
Extended Data Fig. 8 Timing of focal deletions and gains at the MYC locus.
a,b, A schematic illustration summarizing the workflow for distinguishing between pregain (a) and postgain (b) deletions, as well as preduplications (c) and postduplications (d). e,f, Two possible temporal scenarios in which an MYC translocation occurs either after (e) or before (f) large chromosomal gains.
Extended Data Fig. 9 Impact of timing of acquisition.
a,b, Kaplan–Meier plots for progression-free survival (PFS; a) and overall survival (OS; b) for the following three groups: early 1q gain (molecular time ≤ 0.85), late 1q gain (molecular time > 0.85) and 1q amp. Compared to Fig. 6c,d, we show here the confidence intervals of the Kaplan–Meier curves.
Extended Data Fig. 10 Timing copy number gains with chemotherapy mutational signatures.
Cartoon illustrating how the melphalan mutagenic mutational signature SBS99 can be used to estimate the timing of large chromosomal gains. If 1q gain was pre-existing, SBS99 would only be detected among the nonduplicated mutations on 1q. In contrast, if 1q gain was acquired after HDM–ASCT, SBS99 mutations on one allele would be duplicated and SBS99 would be detectable among the duplicated variants. The figure is created with BioRender.com.
Supplementary information
Supplementary Tables 1–14
Supplementary Tables 1–14.
Supplementary Data 1
Timing multiple myeloma evolution.
Supplementary Data 2
Timing the first multi-gain events in multiple myeloma.
Supplementary Data 3
Phylogenetic tree of multiple myeloma patients with WGS available at two different time points.
Supplementary Data 4
Timing multiple myeloma evolution.
Source data
Source Data Fig. 1
Data used to generate Fig. 1a–c.
Source Data Figs. 2 and 3
Data used to generate Figs 2b–j and 3.
Source Data Fig. 4
Data used to generate Fig. 4.
Source Data Fig. 5
Data used to generate Fig. 5.
Source Data Fig. 6
Data used to generate Fig. 6e.
Source Data Fig. 7
Data used to generate Fig. 7.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maura, F., Kaddoura, M., Poos, A.M. et al. Temporal genomic dynamics shape clinical trajectory in multiple myeloma. Nat Genet 57, 2203–2214 (2025). https://doi.org/10.1038/s41588-025-02292-1
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41588-025-02292-1