Abstract
Cognitive motor dissociation (CMD) can improve the accuracy to predict recovery of behaviorally unresponsive patients with acute brain injury, but acquisition and analysis of task-based electroencephalography (EEG) are technically challenging. N2 sleep patterns, such as sleep spindles on EEG, have been associated with good outcomes, rely on similar thalamocortical networks as consciousness and could provide less technically challenging complementary outcome predictors. In this prospective observational cohort study of 226 acutely brain injured patients, well-formed sleep spindles (WFSS) were more likely present in those with CMD than in those without CMD, often preceding the detection of CMD. WFSS were associated with a shorter time to recovery of consciousness, and both CMD and WFSS independently predicted recovery of independence, controlling for age, admission neurological status and injury type. WFSS are seen in approximately every third behaviorally unresponsive patient after acute brain injury, frequently precede detection of CMD and are a promising complementary predictor for recovery of consciousness and functional independence.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The primary patient-level data that support all the main analyses are available as part of Extended Data Figs. 4 and 5, including sleep data, CMD status, sedation data and outcomes data. Other individual patient data are not openly available due to reasons of sensitivity for patient privacy reasons.
Code availability
The code to analyze EEG for cognitive motor dissociation was previously shared (see Claassen et al.26). All other codes used based on publicly available R packages are non-proprietary (R version 4.0.3, R package GLM version 4.1-2, R package survival version 3.2-7, R-package survminer version 0.4.8, R package tidycmprsk version 1.0.0 and R package riskRegression version 2023.03.22).
References
Kondziella, D. et al. European Academy of Neurology guideline on the diagnosis of coma and other disorders of consciousness. Eur. J. Neurol. 27, 739–740 (2020).
Kondziella, D. et al. A precision medicine framework for classifying patients with disorders of consciousness: Advanced Classification of Consciousness Endotypes (ACCESS). Neurocrit. Care 35, 27–36 (2021).
Tsao, C. W. et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation 147, e93–e621 (2023).
Kittner, S. J. et al. Ethnic and racial variation in intracerebral hemorrhage risk factors and risk factor burden. JAMA Netw. Open 4, e2121921 (2021).
Maas, A. I. R. et al. Traumatic brain injury: progress and challenges in prevention, clinical care, and research. Lancet Neurol. 21, 1004–1060 (2022).
Russell, M. E., Hammond, F. M. & Murtaugh, B. Prognosis and enhancement of recovery in disorders of consciousness. NeuroRehabilitation 54, 43–59 (2024).
Fitzgerald, E. et al. Functional outcomes at 12 months for patients with traumatic brain injury, intracerebral haemorrhage and subarachnoid haemorrhage treated in an Australian neurocritical care unit: a prospective cohort study. Aust. Crit. Care 33, 497–503 (2020).
Karras, C. L. et al. Outcomes following penetrating brain injuries in military settings: a systematic review and meta-analysis. World Neurosurg. 166, 39–48 (2022).
Ponfick, M., Wiederer, R. & Nowak, D. A. Outcome of intensive care unit–dependent, tracheotomized patients with cerebrovascular diseases. J. Stroke Cerebrovasc. Dis. 24, 1527–1531 (2015).
Humble, S. S. et al. Prognosis of diffuse axonal injury with traumatic brain injury. J. Trauma Acute Care Surg. 85, 155–159 (2018).
Hayamizu, M. et al. Delayed neurologic improvement and long-term survival of patients with poor neurologic status after out-of-hospital cardiac arrest: a retrospective cohort study in Japan. Resuscitation 188, 109790 (2023).
Edlow, B. L., Claassen, J., Schiff, N. D. & Greer, D. M. Recovery from disorders of consciousness: mechanisms, prognosis and emerging therapies. Nat. Rev. Neurol. 17, 135–156 (2021).
Egawa, S. et al. Long-term outcomes of patients with stroke predicted by clinicians to have no chance of meaningful recovery: a Japanese cohort study. Neurocrit. Care 38, 733–740 (2023).
Dijkland, S. A. et al. Prognosis in moderate and severe traumatic brain injury: a systematic review of contemporary models and validation studies. J. Neurotrauma 37, 1–13 (2020).
Witsch, J. et al. Prognostication after intracerebral hemorrhage: a review. Neurol. Res. Pract. 3, 22 (2021).
Turgeon, A. F. et al. Mortality associated with withdrawal of life-sustaining therapy for patients with severe traumatic brain injury: a Canadian multicentre cohort study. CMAJ 183, 1581–1588 (2011).
Elmer, J. et al. Long-term survival benefit from treatment at a specialty center after cardiac arrest. Resuscitation 108, 48–53 (2016).
Giacino, J. T. et al. Behavioral recovery and early decision making in patients with prolonged disturbance in consciousness after traumatic brain injury. J. Neurotrauma 37, 357–365 (2020).
Giacino, J. T. et al. Practice guideline update recommendations summary: disorders of consciousness: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology 91, 450–460 (2018).
Alkhachroum, A. et al. Withdrawal of life-sustaining treatment mediates mortality in patients with intracerebral hemorrhage with impaired consciousness. Stroke 52, 3891–3898 (2021).
Alkhachroum, A. et al. Association of acute alteration of consciousness in patients with acute ischemic stroke with outcomes and early withdrawal of care. Neurology 98, e1470–e1478 (2022).
Amiri, M. et al. Multimodal prediction of residual consciousness in the intensive care unit: the CONNECT-ME study. Brain 146, 50–64 (2023).
Rohaut, B. et al. Multimodal assessment improves neuroprognosis performance in clinically unresponsive critical-care patients with brain injury. Nat. Med. 30, 2349–2355 (2024).
Owen, A. M. et al. Detecting awareness in the vegetative state. Science 313, 1402 (2006).
Edlow, B. L. et al. Early detection of consciousness in patients with acute severe traumatic brain injury. Brain 140, 2399–2414 (2017).
Claassen, J. et al. Detection of brain activation in unresponsive patients with acute brain injury. N. Engl. J. Med. 380, 2497–2505 (2019).
Egbebike, J. et al. Cognitive-motor dissociation and time to functional recovery in patients with acute brain injury in the USA: a prospective observational cohort study. Lancet Neurol. 21, 704–713 (2022).
Giacino, J. T., Kalmar, K. & Whyte, J. The JFK Coma Recovery Scale-Revised: measurement characteristics and diagnostic utility. Arch. Phys. Med. Rehabil. 85, 2020–2029 (2004).
Bodien, Y. G., Carlowicz, C. A., Chatelle, C. & Giacino, J. T. Sensitivity and specificity of the Coma Recovery Scale–Revised total score in detection of conscious awareness. Arch. Phys. Med. Rehabil. 97, 490–492 (2016).
Giacino, J. T. et al. The minimally conscious state: definition and diagnostic criteria. Neurology 58, 349–353 (2002).
Giacino, J. T. et al. Comprehensive systematic review update summary: disorders of consciousness: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Arch. Phys. Med. Rehabil. 99, P1710–P1719 (2018).
Schiff, N. D. Cognitive motor dissociation following severe brain injuries. JAMA Neurol. 72, 1413–1415 (2015).
Fernández-Espejo, D., Rossit, S. & Owen, A. M. A thalamocortical mechanism for the absence of overt motor behavior in covertly aware patients. JAMA Neurol. 72, 1442–1450 (2015).
Sanders, W. R. et al. Recovery potential in patients who died after withdrawal of life-sustaining treatment: a TRACK-TBI propensity score analysis. J. Neurotrauma 41, 2336–2348 (2024).
Bodien, Y. G. et al. Cognitive motor dissociation in disorders of consciousness. N. Engl. J. Med. 391, 598–608 (2024).
Claassen, J. et al. Cognitive motor dissociation: gap analysis and future directions. Neurocrit. Care 40, 81–98 (2024).
Jacobson, S. D. et al. Impact of aphasia on brain activation to motor commands in patients with acute intracerebral hemorrhage. Neurocrit. Care https://doi.org/10.1007/s12028-024-02086-z (2024).
Raciti, L. et al. Sleep in disorders of consciousness: a brief overview on a still under investigated issue. Brain Sci. 13, 275 (2023).
Sandsmark, D. K. et al. Sleep features on continuous electroencephalography predict rehabilitation outcomes after severe traumatic brain injury. J. Head Trauma Rehabil. 31, 101–107 (2016).
Gottshall, J. L. & Rossi Sebastiano, D. Sleep in disorders of consciousness: diagnostic, prognostic, and therapeutic considerations. Curr. Opin. Neurol. 33, 684–690 (2020).
Rossi Sebastiano, D. et al. Sleep patterns associated with the severity of impairment in a large cohort of patients with chronic disorders of consciousness. Clin. Neurophysiol. 129, 687–693 (2018).
Duclos, C. et al. Parallel recovery of consciousness and sleep in acute traumatic brain injury. Neurology 88, 268–275 (2017).
Forgacs, P. B. et al. Preservation of electroencephalographic organization in patients with impaired consciousness and imaging-based evidence of command-following. Ann. Neurol. 76, 869–879 (2014).
Grigg-Damberger, M. M., Hussein, O. & Kulik, T. Sleep spindles and K-complexes are favorable prognostic biomarkers in critically ill patients. J. Clin. Neurophysiol. 39, 372–382 (2022).
Van Der Lande, G. J. M., Blume, C. & Annen, J. Sleep and circadian disturbance in disorders of consciousness: current methods and the way towards clinical implementation. Semin. Neurol. 42, 283–298 (2022).
Arnaldi, D. et al. The prognostic value of sleep patterns in disorders of consciousness in the sub-acute phase. Clin. Neurophysiol. 127, 1445–1451 (2016).
Yang, X. A. et al. Prognostic roles of sleep electroencephalography pattern and circadian rhythm biomarkers in the recovery of consciousness in patients with coma: a prospective cohort study. Sleep Med. 69, 204–212 (2020).
Fernandez, L. M. J. & Lüthi, A. Sleep spindles: mechanisms and functions. Physiol. Rev. 100, 805–868 (2020).
Urakami, Y. Relationship between sleep spindles and clinical recovery in patients with traumatic brain injury: a simultaneous EEG and MEG study. Clin. EEG Neurosci. 43, 39–47 (2012).
De Gennaro, L. & Ferrara, M. Sleep spindles: an overview. Sleep Med. Rev. 7, 423–440 (2003).
Anderer, P. et al. Low-resolution brain electromagnetic tomography revealed simultaneously active frontal and parietal sleep spindle sources in the human cortex. Neuroscience 103, 581–592 (2001).
Franzova, E. et al. Injury patterns associated with cognitive motor dissociation. Brain 146, 4645–4658 (2023).
Zhu, H. et al. Spectral-switching analysis reveals real-time neuronal network representations of concurrent spontaneous naturalistic behaviors in human brain. Preprint at bioRxiv https://doi.org/10.1101/2024.07.08.600416 (2024).
Schiff, N. D. in Brain Function and Responsiveness in Disorders of Consciousness (eds Monti, M. M. & Sannita, W. G.) 195–204 (Springer, 2016).
Forgacs, P. B. et al. Dynamic regimes of neocortical activity linked to corticothalamic integrity correlate with outcomes in acute anoxic brain injury after cardiac arrest. Ann. Clin. Transl. Neurol. 4, 119–129 (2017).
Du, B. et al. Zolpidem arouses patients in vegetative state after brain injury: quantitative evaluation and indications. Am. J. Med. Sci. 347, 178–182 (2014).
Whyte, J. & Myers, R. Incidence of clinically significant responses to zolpidem among patients with disorders of consciousness: a preliminary placebo controlled trial. Am. J. Phys. Med. Rehabil. 88, 410–418 (2009).
Sutton, J. A. & Clauss, R. P. A review of the evidence of zolpidem efficacy in neurological disability after brain damage due to stroke, trauma and hypoxia: a justification of further clinical trials. Brain Inj. 31, 1019–1027 (2017).
Schiff, N. D. Recovery of consciousness after brain injury: a mesocircuit hypothesis. Trends Neurosci. 33, 1–9 (2010).
Stender, J. et al. Diagnostic precision of PET imaging and functional MRI in disorders of consciousness: a clinical validation study. Lancet 384, 514–522 (2014).
Fine, J. & Gray, R. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94, 496–509 (1999).
Berry, R. B. et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications version 2.6 (American Academy of Sleep Medicine, 2020).
Majersik, J. J. et al. A shortage of neurologists—we must act now: a report from the AAN 2019 Transforming Leaders Program. Neurology 96, 1122–1134 (2021).
Hirsch, L. J. et al. American Clinical Neurophysiology Society’s standardized critical care EEG terminology: 2021 version. J. Clin. Neurophysiol. 38, 1–29 (2021).
Kwon, H. et al. Sleep spindles in the healthy brain from birth through 18 years. Sleep 46, zsad017 (2023).
Felten, M. et al. Circadian rhythm disruption in critically ill patients. Acta Physiol. 238, e13962 (2023).
Curley, W. H., Forgacs, P. B., Voss, H. U., Conte, M. M. & Schiff, N. D. Characterization of EEG signals revealing covert cognition in the injured brain. Brain 141, 1404–1421 (2018).
Wolpert, E. A. A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects. Arch. Gen. Psychiatry 20, 246–247 (1969).
Purcell, S. M. et al. Characterizing sleep spindles in 11,630 individuals from the National Sleep Research Resource. Nat. Commun. 8, 15930 (2017).
Valente, M. et al. Sleep organization pattern as a prognostic marker at the subacute stage of post-traumatic coma. Clin. Neurophysiol. 113, 1798–1805 (2002).
Ambrogio, C., Koebnick, J., Quan, S. F., Ranieri, M. & Parthasarathy, S. Assessment of sleep in ventilator-supported critically III patients. Sleep 31, 1559–1568 (2008).
McHugh, M. L. Interrater reliability: the kappa statistic. Biochem. Med. 22, 276–282 (2012).
Landis, J. & Koch, G. The measurement of observer agreement for categorical data. Biometrics 33, 159–174 (1977).
Claassen, J. et al. Bedside quantitative electroencephalography improves assessment of consciousness in comatose subarachnoid hemorrhage patients. Ann. Neurol. 80, 541–553 (2016).
Blanche, P. et al. Quantifying and comparing dynamic predictive accuracy of joint models for longitudinal marker and time-to-event in presence of censoring and competing risks. Biometrics 71, 102–113 (2015).
Acknowledgements
We thank the nurses, attending physicians, fellows and neurology residents of the neuroscience ICU for their overall support of this project. We are grateful to the National Institutes of Health (NIH)/National Institute of Neurological Disorders and Stroke (NS106014; LM011826) and the Clinical and Translational Science Awards (UL1TR001873 from the National Center for Advancing Translational Sciences/NIH) for support of this study.
Author information
Authors and Affiliations
Contributions
The study was conceived and designed by J. Claassen. Data were acquired and analyzed by E.E.C., Q.S., V.K., N.C., A.M., I.N.-K., J.L., A.P., M.V., S.E., J. Carmona, L.K., Y.L.S., A.V. and J. Claassen. The paper and figures were drafted by E.E.C., Q.S., V.K. and J. Claassen. Edits to the paper were provided by C.A.S., J.K., E.S.C., S.G., S.A., D.R., S.P. and P.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. J. Claassen is a minority shareholder at iCE Neurosystems, but this amounts to less than $10,000 and less than 5% equity in the company. No technology from iCE Neurosystems was used for any of the study procedures, data acquisition or analysis presented here. None of the patients included in this study were managed using any technology from iCE Neurosystems.
Peer review
Peer review information
Nature Medicine thanks Brian Edlow, Daniel Kondziella and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Jerome Staal, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Consort diagram.
EEG, electroencephalography; WLST, withdrawal of list sustaining treatment.
Extended Data Fig. 3 Presence of K-complexes and Vertex waves and their relationship to sleep spindles in CMD and non-CMD patients.
Presence of K-complexes and vertex waves in the entire patient cohort (a), CMD positive patients (b), and CMD negative patients (c) was highly correlated with concomitant presence of sleep spindles.
Extended Data Fig. 4 Post-injury timeline of CMD testing and presence of sleep spindles in CMD positive patients.
Well-formed sleep spindles frequently preceded the detection of CMD.
Extended Data Fig. 5 Post-injury timeline of CMD testing and presence of sleep spindles in CMD negative patients.
Of those CMD negative patients with delayed sleep spindles, well-formed sleep spindles were still predictive of recovery of consciousness, and 12-month outcome. Similarly to CMD positive patients, when well-formed sleep spindles were present on EEG, they were likely to persist on subsequent EEG recordings.
Extended Data Fig. 6 Level of sedation at the time of EEG recording and associated presence and quality of sleep spindles (N = 530).
Patients receiving “moderate” (p = 0.0002, OR = 0.4 [0.3, 0.7]) and “minimal” or “low” levels of sedation (p < 0.0001 OR = 0.5 [0.3, 0.7]) were less likely to have well-formed sleep spindles present when compared to those with no sedation.
Extended Data Fig. 7 Time to recovery of consciousness defined by CRS-R ≥ 8 and MCS + /EMCS.
Time to CRS-R ≥ 8 is significantly shorter than time to MCS + /EMCS (p = 0.04).
Extended Data Fig. 8 Sequencing of WFSS, CMD, and CRS-R ≥ 8.
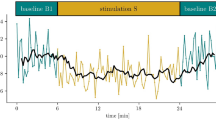
Time to detect WFSS is significantly shorter than time to detect CMD in the overall cohort (Panel a). Time to CRS-R ≥ 8 is shorter for those with CMD (Panel b) but not for those without CMD (Panel c) except for non-CMD patients with WFSS (Panel d). Amongst patients with WFSS, 35% (6 of 17) of patients with and 46% (25 of 54) of patients without CMD recovered consciousness (Panel e). Amongst patients without WFSS, 25% (4 of 16) of patients with and 21% (30 of 139) of patients without CMD recovered consciousness. Patients with CRS-R ≥ 8 are kept in orange and first detecting WFSS, CMD and CRS-R are indicated by a green diamond, blue triangle, and orange dot, respectively. CMD, cognitive motor dissociation; CRS-R, coma recovery scale-revised; well-formed sleep spindles, WFSS.
Extended Data Fig. 9 Study Timeline.
This schematic depicts the timeline of testing and results for an exemplary patient found to have well-formed sleep spindles, followed by positive CMD testing, and ultimately recovery of consciousness and long-term functional recovery.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Carroll, E.E., Shen, Q., Kansara, V. et al. Sleep spindles as a predictor of cognitive motor dissociation and recovery of consciousness after acute brain injury. Nat Med 31, 1578–1585 (2025). https://doi.org/10.1038/s41591-025-03578-x
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41591-025-03578-x
This article is cited by
-
Disorders of consciousness diagnosis, interventions, and prognostication for the intensivist: Report of the 2025 ISICEM roundtable
Intensive Care Medicine (2026)
-
Who’s likely to wake up from a coma? Brainwaves provide a clue
Nature (2025)
-
The Gray Zone of Consciousness: Cognitive Motor Dissociation
Current Neurology and Neuroscience Reports (2025)