Abstract
The prostate-specific membrane antigen (PSMA)-targeted radioligand [¹⁷⁷Lu]Lu–PSMA-617 is a new standard treatment for metastatic castration-resistant prostate cancer (mCRPC), but predictive genomic biomarkers informing its rational use are unknown. We performed detailed dissection of prostate cancer driver genes across 290 serial plasma cell-free DNA samples from 180 molecular imaging-selected patients with mCRPC from the randomized TheraP trial of [¹⁷⁷Lu]Lu–PSMA-617 (n = 97) versus cabazitaxel chemotherapy (n = 83). The primary endpoint was PSA50 biochemical response, with secondary endpoints of progression-free survival (PFS) and overall survival (OS). In this post-hoc biomarker analysis, a low pretreatment circulating tumor DNA (ctDNA) fraction predicted a superior biochemical response (100% versus 58%, P = 0.0067) and PFS (median 14.7 versus 6.0 months; hazard ratio 0.12, P = 2.5 × 10−4) on [¹⁷⁷Lu]Lu–PSMA-617 independent of predictive PSMA–positron emission tomography imaging parameters, although this benefit did not extend to OS. Deleterious PTEN alterations were associated with worse PFS and OS on cabazitaxel, whereas ATM defects were observed in select patients with favorable [¹⁷⁷Lu]Lu–PSMA-617 outcomes. Comparing pretreatment and progression ctDNA revealed population flux but no evidence that alterations in individual mCRPC genes (or FOLH1) are dominant causes of acquired [¹⁷⁷Lu]Lu–PSMA-617 or cabazitaxel resistance. Our results nominate new candidate biomarkers for [¹⁷⁷Lu]Lu–PSMA-617 selection and ultimately expand the mCRPC predictive biomarker repertoire. We anticipate our ctDNA fraction-aware analytical framework will aid future precision management strategies for [¹⁷⁷Lu]Lu–PSMA-617 and other PSMA-targeted therapeutics. ClinicalTrials.gov identifier: NCT03392428.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The hg38 human reference genome was downloaded from UCSC. Germline variant population frequency is available at gnomAD v.3.0 (https://gnomad.broadinstitute.org/). ANZUP is obligated to protect the rights and privacy of trial participants, thereby necessitating restricted access to patient-level clinical and genomic sequencing data. Deidentified participant sequencing and select clinical data will be made available to researchers who are registered with an appropriate institution following publication. Methodologically sound proposals for any purpose will be considered by the trial executive committee who will have the right to review and comment on any draft manuscripts before publication. Proposals should be directed to michael.hofman@petermac.org. To gain access, data requesters will be required to sign a data access agreement. Timeframe for data access will be subject to ANZUP policy and process. Data supporting the findings of this study are available in the article in Supplementary Tables 1–11. Source data are provided with this paper.
Code availability
Our complete ctDNA somatic variant calling pipeline is available on GitHub (https://github.com/annalam/cfdna-wgs-manuscript-code) and is described in detail in a previous publication12. No additional custom software was utilized for any analysis performed herein.
References
Hofman, M. S. et al. [177Lu]Lu-PSMA-617 versus cabazitaxel in patients with metastatic castration-resistant prostate cancer (TheraP): a randomised, open-label, phase 2 trial. Lancet 397, 797–804 (2021).
Hofman, M. S. et al. Overall survival with [177Lu]Lu-PSMA-617 versus cabazitaxel in metastatic castration-resistant prostate cancer (TheraP): secondary outcomes of a randomised, open-label, phase 2 trial. Lancet Oncol. 25, 99–107 (2023).
Sartor, O. et al. Lutetium-177–PSMA-617 for metastatic castration-resistant prostate cancer. N. Engl. J. Med. 385, 1091–1103 (2021).
Gafita, A. et al. Predictors and real-world use of prostate-specific radioligand therapy: PSMA and beyond. Am. Soc. Clin. Oncol. Educ. Book 42, 1–17 (2022).
Buteau, J. P. et al. PSMA and FDG-PET as predictive and prognostic biomarkers in patients given [177Lu]Lu-PSMA-617 versus cabazitaxel for metastatic castration-resistant prostate cancer (TheraP): a biomarker analysis from a randomised, open-label, phase 2 trial. Lancet Oncol. 23, 1389–1397 (2022).
Kuo, P. H. et al. Quantitative 68Ga-PSMA-11 PET and clinical outcomes in metastatic castration-resistant prostate cancer following 177Lu-PSMA-617 (VISION trial). Radiology 312, e233460 (2024).
Thang, S. P. et al. Poor outcomes for patients with metastatic castration-resistant prostate cancer with low prostate-specific membrane antigen (PSMA) expression deemed ineligible for 177Lu-labelled PSMA radioligand therapy. Eur. Urol. Oncol. 2, 670–676 (2019).
de Bono, J. et al. Olaparib for metastatic castration-resistant prostate cancer. N. Engl. J. Med. 382, 2091–2102 (2020).
Abida, W. et al. Analysis of the prevalence of microsatellite instability in prostate cancer and response to immune checkpoint blockade. JAMA Oncol. 5, 471–478 (2019).
Hussain, M. et al. Tumor genomic testing for >4000 men with metastatic castration-resistant prostate cancer in the phase III trial PROfound (Olaparib). Clin. Cancer Res. 28, 1518–1530 (2022).
Kwan, E. M., Wyatt, A. W. & Chi, K. N. Towards clinical implementation of circulating tumor DNA in metastatic prostate cancer: opportunities for integration and pitfalls to interpretation. Front. Oncol. 12, 1054497 (2022).
Herberts, C. et al. Deep whole-genome ctDNA chronology of treatment-resistant prostate cancer. Nature 608, 199–208 (2022).
Fettke, H. et al. Abstract 5614: Genomic aberrations in circulating tumor DNA (ctDNA) and clinical outcomes from [177Lu]Lu-PSMA-617 in metastatic castration-resistant prostate cancer (mCRPC). Cancer Res. 83, 5614 (2023).
Vanwelkenhuyzen, J. et al. AR and PI3K genomic profiling of cell-free DNA can identify poor responders to lutetium-177-PSMA among patients with metastatic castration-resistant prostate cancer. Eur. Urol. Open Sci. 53, 63–66 (2023).
Crumbaker, M. et al. Circulating tumour DNA biomarkers associated with outcomes in metastatic prostate cancer treated with lutetium-177-PSMA-617. Eur. Urol. Open Sci. 57, 30–36 (2023).
Sartor, O. et al. Prediction of resistance to 177Lu-PSMA therapy by assessment of baseline circulating tumor DNA biomarkers. J. Nucl. Med. 64, 1721–1725 (2023).
Raychaudhuri, R. et al. Genomic correlates of prostate-specific membrane antigen expression and response to 177Lu-PSMA-617: a retrospective multicenter cohort study. JCO Precis. Oncol. 8, e2300634 (2024).
Chi, K. N. et al. CCTG PR21: a randomized phase II study of [177Lu]Lu-PSMA-617 verus docetaxel in patients with metastatic castration-resistant prostate cancer and PSMA-positive disease (NCT04663997). J. Clin. Oncol. 40, TPS5110 (2022).
Morris, M. J. et al. Lu-PSMA-617 versus a change of androgen receptor pathway inhibitor therapy for taxane-naive patients with progressive metastatic castration-resistant prostate cancer (PSMAfore): a phase 3, randomised, controlled trial. Lancet 404, 1227–1239 (2024).
Fonseca, N. M. et al. Prediction of plasma ctDNA fraction and prognostic implications of liquid biopsy in advanced prostate cancer. Nat. Commun. 15, 1828 (2024).
Tolmeijer, S. H. et al. Early on-treatment changes in circulating tumor DNA fraction and response to enzalutamide or abiraterone in metastatic castration-resistant prostate cancer. Clin. Cancer Res. 29, 2835–2844 (2023).
Choudhury, A. D. et al. Tumor fraction in cell-free DNA as a biomarker in prostate cancer. JCI Insight 3, e122109 (2018).
Annala, M. et al. Evolution of castration-resistant prostate cancer in ctDNA during sequential androgen receptor pathway inhibition. Clin. Cancer Res. 27, 4610–4623 (2021).
Annala, M. et al. Circulating tumor DNA genomics correlate with resistance to abiraterone and enzalutamide in prostate cancer. Cancer Discov. 8, 444–457 (2018).
Annala, M. et al. Cabazitaxel versus abiraterone or enzalutamide in poor prognosis metastatic castration-resistant prostate cancer: a multicentre, randomised, open-label, phase 2 trial. Ann. Oncol. 32, 896–905 (2021).
Ferdinandus, J. et al. Prognostic biomarkers in men with metastatic castration-resistant prostate cancer receiving [177Lu]-PSMA-617. Eur. J. Nucl. Med. Mol. Imaging 47, 2322–2327 (2020).
Quigley, D. A. et al. Genomic hallmarks and structural variation in metastatic prostate cancer. Cell 175, 889 (2018).
Abida, W. et al. Genomic correlates of clinical outcome in advanced prostate cancer. Proc. Natl Acad. Sci. USA 116, 11428–11436 (2019).
Chakraborty, G. et al. The impact of PIK3R1 mutations and insulin-PI3K-glycolytic pathway regulation in prostate cancer. Clin. Cancer Res. 28, 3603–3617 (2022).
De Laere, B. et al. TP53 outperforms other androgen receptor biomarkers to predict abiraterone or enzalutamide outcome in metastatic castration-resistant prostate cancer. Clin. Cancer Res. 25, 1766–1773 (2019).
De Laere, B. et al. Androgen receptor burden and poor response to abiraterone or enzalutamide in TP53 wild-type metastatic castration-resistant prostate cancer. JAMA Oncol. 5, 1060–1062 (2019).
Fettke, H. et al. Combined cell-free DNA and RNA profiling of the androgen receptor: clinical utility of a novel multianalyte liquid biopsy assay for metastatic prostate cancer. Eur. Urol. 78, 173–180 (2020).
Kwan, E. M. et al. Plasma cell-free DNA profiling of PTEN-PI3K-AKT pathway aberrations in metastatic castration-resistant prostate cancer. JCO Precis. Oncol. 5, 622–637 (2021).
Tolmeijer, S. H. et al. A systematic review and meta-analysis on the predictive value of cell-free DNA-based androgen receptor copy number gain in patients with castration-resistant prostate cancer. JCO Precis. Oncol. 4, 714–729 (2020).
Gundem, G. et al. The evolutionary history of lethal metastatic prostate cancer. Nature 520, 353–357 (2015).
Warner, E. W. et al. Multiregion sampling of de novo metastatic prostate cancer reveals complex polyclonality and augments clinical genotyping. Nat. Cancer 5, 114–130 (2024).
McGranahan, N. et al. Clonal status of actionable driver events and the timing of mutational processes in cancer evolution. Sci. Transl. Med. 7, 283ra54 (2015).
Herberts, C. & Wyatt, A. W. Technical and biological constraints on ctDNA-based genotyping. Trends Cancer Res. 7, 995–1009 (2021).
de Wit, R. et al. Cabazitaxel versus abiraterone or enzalutamide in metastatic prostate cancer. N. Engl. J. Med. 381, 2506–2518 (2019).
Jang, A., Kendi, A. T., Johnson, G. B., Halfdanarson, T. R. & Sartor, O. Targeted alpha-particle therapy: a review of current trials. Int. J. Mol. Sci. 24, 11626 (2023).
Buteau, J. P. et al. Clinical trial protocol for VIOLET: a single-center, phase I/II trial evaluation of radioligand treatment in patients with metastatic castration-resistant prostate cancer with [161Tb]Tb-PSMA-I&T. J. Nucl. Med. 65, 1231–1238 (2024).
Sumanasuriya, S. et al. Elucidating prostate cancer behaviour during treatment via low-pass whole-genome sequencing of circulating tumour DNA. Eur. Urol. 80, 243–253 (2021).
Emmett, L. et al. [Lu]Lu-PSMA-617 plus enzalutamide in patients with metastatic castration-resistant prostate cancer (ENZA-p): an open-label, multicentre, randomised, phase 2 trial. Lancet Oncol. 25, 563–571 (2024).
Khalaf, D. J. et al. Optimal sequencing of enzalutamide and abiraterone acetate plus prednisone in metastatic castration-resistant prostate cancer: a multicentre, randomised, open-label, phase 2, crossover trial. Lancet Oncol. 20, 1730–1739 (2019).
Bakht, M. K. et al. Landscape of prostate-specific membrane antigen heterogeneity and regulation in AR-positive and AR-negative metastatic prostate cancer. Nat. Cancer 4, 699–715 (2023).
Gafita, A. et al. Validation of prognostic and predictive models for therapeutic response in patients treated with [177Lu]Lu-PSMA-617 versus cabazitaxel for metastatic castration-resistant prostate cancer (TheraP): a post hoc analysis from a randomised, open-label, phase 2 trial. Eur. Urol. Oncol. 8, 21–28 (2024).
Abdel-Wahab, M. et al. Radiotherapy and theranostics: a Lancet Oncology Commission. Lancet Oncol. 25, e545–e580 (2024).
Tukachinsky, H. et al. Genomic analysis of circulating tumor DNA in 3,334 patients with advanced prostate cancer identifies targetable BRCA alterations and AR resistance mechanisms. Clin. Cancer Res. 27, 3094–3105 (2021).
Nakamura, Y. et al. Clinical utility of circulating tumor DNA sequencing in advanced gastrointestinal cancer: SCRUM-Japan GI-SCREEN and GOZILA studies. Nat. Med. 26, 1859–1864 (2020).
Kwan, E. M. et al. Prospective ctDNA genotyping for treatment selection in metastatic castration-resistant prostate cancer (mCRPC): The Canadian Cancer Trials Group phase II PC-BETS umbrella study. J. Clin. Oncol. 41, 218 (2023).
Jee, J. et al. Overall survival with circulating tumor DNA-guided therapy in advanced non-small-cell lung cancer. Nat. Med. 28, 2353–2363 (2022).
Kaittanis, C. et al. Prostate-specific membrane antigen cleavage of vitamin B9 stimulates oncogenic signaling through metabotropic glutamate receptors. J. Exp. Med. 215, 159–175 (2018).
Rescigno, P. et al. Docetaxel treatment in PTEN- and ERG-aberrant metastatic prostate cancers. Eur. Urol. Oncol. 1, 71–77 (2018).
Pitter, K. L. et al. Pathogenic ATM mutations in cancer and a genetic basis for radiotherapeutic efficacy. J. Natl Cancer Inst. 113, 266–273 (2021).
Fallah, J. et al. Efficacy of poly(ADP-ribose) polymerase inhibitors by individual genes in homologous recombination repair gene-mutated metastatic castration-resistant prostate cancer: a US Food and Drug Administration pooled analysis. J. Clin. Oncol. 42, 1687–1698 (2024).
Hope, T. A. et al. 68Ga-PSMA-11 PET imaging of response to androgen receptor inhibition: first human experience. J. Nucl. Med. 58, 81–84 (2017).
Emmett, L. et al. Rapid modulation of PSMA expression by androgen deprivation: serial 68Ga-PSMA-11 PET in men with hormone-sensitive and castrate-resistant prostate cancer commencing androgen blockade. J. Nucl. Med. 60, 950–954 (2018).
Bakht, M. K. & Beltran, H. Biological determinants of PSMA expression, regulation and heterogeneity in prostate cancer. Nat. Rev. Urol. 22, 26–45 (2024).
Zivanovic, A. et al. Co-evolution of AR gene copy number and structural complexity in endocrine therapy resistant prostate cancer. NAR Cancer 5, zcad045 (2023).
Chi, K. N. et al. Study evaluating metastatic castrate resistant prostate cancer (mCRPC) treatment using 177Lu-PNT2002 PSMA therapy after second-line hormonal treatment (SPLASH). J. Clin. Oncol. 39, TPS5087 (2021).
Sweeney, C. et al. Ipatasertib plus abiraterone and prednisolone in metastatic castration-resistant prostate cancer (IPATential150): a multicentre, randomised, double-blind, phase 3 trial. Lancet 398, 131–142 (2021).
Nguyen, B. et al. Pan-cancer analysis of CDK12 alterations identifies a subset of prostate cancers with distinct genomic and clinical characteristics. Eur. Urol. 78, 671–679 (2020).
Carreira, S. et al. Biomarkers associating with PARP inhibitor benefit in prostate cancer in the TOPARP-B trial. Cancer Discov. 11, 2812–2827 (2021).
Coates, J. T. et al. Parallel genomic alterations of antigen and payload targets mediate polyclonal acquired clinical resistance to sacituzumab govitecan in triple-negative breast cancer. Cancer Discov. 11, 2436–2445 (2021).
Violet, J. et al. Long-term follow-up and outcomes of retreatment in an expanded 50-patient single-center phase II prospective trial of 177Lu-PSMA-617 theranostics in metastatic castration-resistant prostate cancer. J. Nucl. Med. 61, 857–865 (2020).
Ku, S. Y. et al. Rb1 and Trp53 cooperate to suppress prostate cancer lineage plasticity, metastasis, and antiandrogen resistance. Science 355, 78–83 (2017).
Sipola, J. et al. Plasma cell-free DNA chromatin immunoprecipitation profiling depicts phenotypic and clinical heterogeneity in advanced prostate cancer. Cancer Res. 85, 791–807 (2025).
Iravani, A. et al. Molecular imaging of neuroendocrine differentiation of prostate cancer: a case series. Clin. Genitourin. Cancer 19, e200–e205 (2021).
Sandhu, S. et al. PRINCE: phase I trial of 177Lu-PSMA-617 in combination with pembrolizumab in patients with metastatic castration-resistant prostate cancer (mCRPC). J. Clin. Oncol. 40, 5017 (2022).
Azad, A. A. et al. Sequential [Lu]Lu-PSMA-617 and docetaxel versus docetaxel in patients with metastatic hormone-sensitive prostate cancer (UpFrontPSMA): a multicentre, open-label, randomised, phase 2 study. Lancet Oncol. 25, 1267–1276 (2024).
Tagawa, S. T. et al. PSMAddition: a phase 3 trial to compare treatment with 177Lu-PSMA-617 plus standard of care (SoC) and SoC alone in patients with metastatic hormone-sensitive prostate cancer. J. Clin. Oncol. 41, TPS5116 (2023).
Sayar, E. et al. Reversible epigenetic alterations mediate PSMA expression heterogeneity in advanced metastatic prostate cancer. JCI Insight 8, e162907 (2023).
Hofman, M. S. et al. TheraP: a randomized phase 2 trial of 177Lu-PSMA-617 theranostic treatment vs cabazitaxel in progressive metastatic castration-resistant prostate cancer (Clinical Trial Protocol ANZUP 1603). BJU Int. 124, 5–13 (2019).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet J. 17, 10–12 (2011).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 9, 357–359 (2012).
Mose, L. E., Perou, C. M. & Parker, J. S. Improved indel detection in DNA and RNA via realignment with ABRA2. Bioinformatics 35, 2966–2973 (2019).
Faust, G. G. & Hall, I. M. SAMBLASTER: fast duplicate marking and structural variant read extraction. Bioinformatics 30, 2503–2505 (2014).
Wang, K., Li, M. & Hakonarson, H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 38, e164 (2010).
Landrum, M. J. et al. ClinVar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res. 46, D1062–D1067 (2018).
Acknowledgements
The TheraP trial (ANZUP 1603) is a collaboration between the ANZUP Trials Group, the NHMRC Clinical Trials Centre, University of Sydney and the Australasian Radiopharmaceutical Trials Network (ARTnet) in partnership with the Prostate Cancer Foundation of Australia with support from ANSTO, Endocyte (a Novartis company), Movember, The Distinguished Gentleman’s Ride, It’s a Bloke Thing and CAN4CANCER. ANZUP receives infrastructure support from the Australian government through Cancer Australia (Support for Cancer Clinical Trials Program). This correlative research study was primarily supported by the Prostate Cancer Foundation via a 2023 PCF Challenge Award to A.W.W. Additional funding support was also received from a Terry Fox New Frontiers Program Project Grant and a Canadian Cancer Society Challenge Grant (grant no. 707339). E.M.K. is supported by a Prostate Cancer Foundation Young Investigator Award and an ANZUP Synchrony Fellowship. S.H.T. is supported by a Prostate Cancer Foundation Young Investigator Award and Michael Smith Health Research BC Trainee Award. J.P.B. is supported by a Prostate Cancer Foundation Young Investigator Award and PhD support through an Australian Government Research Training Program Scholarship. A.M.S. was supported by an NHMRC Investigator Fellowship (APP1177837). I.D.D. is supported by an NHMRC Practitioner Fellowship (APP1102604). M.S.H. acknowledges philanthropic and government grant support from the Prostate Cancer Foundation, the Peter MacCallum Foundation and a NHMRC Investigator Grant and Movember. S.S. is supported by the NHMRC and additionally acknowledges grant support from the Prostate Cancer Foundation and the Peter MacCallum Foundation. The NHMRC Clinical Trials Centre was supported by NHMRC Program Grants 1037786 and 1150467. 177Lu was supplied by ANSTO. Endocyte provided PSMA-11 and PSMA-617, and additional funding support. We acknowledge and thank the 200 patients for their participation in the TheraP study; and the principal investigators, coinvestigators, study coordinators, nurses, radiopharmacists and chemists and nuclear medicine technologists at the 11 centers across Australia for their dedication and enthusiasm. We also thank members and staff of the ANZUP Board, Scientific Advisory Committee, Prostate Cancer Subcommittee, Consumer Advisory Panel and Independent Data Safety and Monitoring Committee; NHMRC Clinical Trials Centre; and ARTnet.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: E.M.K., L.E., A.J.M., I.D.D., M.S.H., A.A.A. and A.W.W. Methodology: E.M.K., S.W.S.N., S.H.T., M.A., C.H. and A.W.W. Software: E.M.K., S.W.S.N., S.H.T., M.A., C.H. and A.W.W. Validation: E.M.K., S.W.S.N., S.H.T., C.H. and A.W.W. Formal analysis: E.M.K., S.W.S.N., S.H.T., M.A., C.H. and A.W.W. Investigation: E.M.K., S.W.S.N., S.H.T., G.D., C.H. and A.W.W. Resources: M.A., I.D.D., M.S.H., A.A.A. and A.W.W. Data curation: E.M.K., S.W.S.N., S.H.T., S.S., G.D., C.H. and A.W.W. Writing—original draft: E.M.K., S.W.S.N., S.H.T., C.H. and A.W.W. Writing—review and editing: E.M.K., S.W.S.N., S.H.T., L.E., S.S., J.P.B., A.I., A.M.J., R.J.F., V.S., S.-T.L., A.M.S., A.J.M., M.R.S., M.A., C.H., I.D.D., M.S.H., A.A.A. and A.W.W. Visualization: E.M.K., S.W.S.N., S.H.T., C.H. and A.W.W. Supervision: I.D.D., M.S.H., A.A.A. and A.W.W. Project administration: E.M.K. V.S., I.D.D., M.S.H., A.A.A. and A.W.W. Funding acquisition: I.D.D., M.S.H., A.A.A. and A.W.W.
Corresponding authors
Ethics declarations
Competing interests
E.M.K. has consulted or served in an advisory role for Astellas Pharma, Janssen and Ipsen, received travel funding from Astellas Pharma, Pfizer, Ipsen and Roche, received honoraria from Janssen, Ipsen, Astellas Pharma and Research Review, and received research funding from Astellas Pharma (institutional) and AstraZeneca (institutional). L.E. has consulted or served in an advisory role for Noxopharm and Clarity Pharmaceuticals, participated in a speakers’ bureau for Janssen Oncology, Mundipharma and Astellas Pharma, and received research funding from Noxopharm (institutional) and Novartis (institutional). S.S. has consulted or served in an advisory role for AstraZeneca, Bristol-Myers Squibb, Merck Sharp & Dohme, Novartis, Skyline Diagnostics and AbbVie, received honoraria from Bristol-Myers Squibb (institutional), Merck (institutional), AstraZeneca (institutional) and Janssen (institutional), and received research funding from Amgen (institutional), AstraZeneca (institutional), Merck (institutional), Endocyte/Advanced Accelerator Applications (institutional), Roche/Genentech (institutional), Novartis (institutional), Pfizer (institutional) and Senhwa Biosciences (institutional). A.I. has consulted or served in an advisory role for Novartis, Lantheus, Curium, ITM, Bayer, Boston Scientific, Ambrx/J&J (institutional), and received research funding from NIH (institutional), Novartis (institutional), SNMMI (institutional) and ACR (institutional). A.M.J. has consulted or served in an advisory role for Janssen Oncology, Ipsen, AstraZeneca, Sanofi, Pfizer, Novartis, Merck Serono, Eisai, IDEAYA Biosciences, IQvia, Bayer, Astellas Pharma, Grey Wolf Therapeutics, Medison and Starpharma, has a patent or received royalties with Cancer Therapeutic Methods, owns stock or holds ownership interests in Pricilium Therapeutics and Opthea, and receives research funding from Bristol-Myers Squibb (institutional), Janssen Oncology (institutional), Merck Sharpe & Dohme (institutional), Mayna Pharma (institutional), Roche/Genentech (institutional), Bayer (institutional), Lilly (institutional), Pfizer (institutional), AstraZeneca (institutional) and Corvus Pharmaceuticals (institutional). R.J.F. consulted or served in an advisory role for AIQ Solutions, receives research funding from AIQ Solutions, and has an immediate family member employed by and owns stock in AIQ Solutions. A.M.S. has consulted or served in an advisory role for ImmunOs Therapeutics and Imagion Biosystems, has an institutional patent relating to antibodies to EGFR, HER2, PDGF-CC, FN-14, GM-CSF, EphA3, owns stock or holds ownership interests in Paracrine Therapeutics and Certis Therapeutics, and received research funding from Telix Pharmaceuticals (institutional), Curis (institutional), Isotopen Technologien (institutional), Adalta (institutional), Fusion Pharmaceuticals (institutional), AstraZeneca (institutional), EMD Serono (institutional), Cyclotek (institutional), AVID/Lilly (institutional), Merck (institutional), Humanigen (institutional) and Antengene (institutional). M.R.S. has received research funding from Astellas Pharma (institutional), Bayer (institutional), Medivation (institutional), Pfizer (institutional), AstraZeneca (institutional), Bristol-Myers Squibb (institutional), Roche (institutional), Amgen (institutional), Merck Sharpe & Dohme (institutional), Tilray (institutional), BeiGene (institutional) and Novartis (institutional). M.A. is compensated for a leadership role in Fluivia and owns stock in Fluivia. S.H.T. has received honoraria from Bayer. I.D.D. is the unremunerated chair of ANZUP Cancer Trials Group, and has received research funding from Astellas Pharma (institutional), Pfizer (institutional), Roche/Genentech (institutional), MSD Oncology (institutional), AstraZeneca (institutional), Janssen Oncology (institutional), Eisai (institutional), Bayer (institutional), Amgen (institutional), Bristol-Myers Squibb (institutional), Movember Foundation (institutional), Exelixis (institutional), Ipsen (institutional), Seagen (institutional) and ESSA (institutional). M.S.H. has consulted or served in an advisory role for Janssen, MSD and Novartis, received travel funding from Novartis and Debiopharm Group, and received research funding from Bayer (institutional), Novartis (institutional), Isotopia Molecular Imaging (institutional) and Debiopharm Group (institutional). A.A.A. has consulted or served in an advisory role for Astellas Pharma, Novartis, Janssen, Sanofi, AstraZeneca, Pfizer, Bristol-Myers Squibb, Tolmar, Telix Pharmaceuticals, Merck Sharpe & Dohme, Bayer, Ipsen, Merck Serono, Amgen, Noxopharma, Aculeus Therapeutics and Daiichi Sankyo, participated in a speakers’ bureau for Astellas Pharma, Novartis, Amgen, Bayer, Janssen, Ipsen, Bristol-Myers Squibb and Merck Serono, received travel funding from Astellas Pharma, Sanofi, Merck Serono, Amgen, Janssen, Tolmar, Pfizer, Bayer and Hinova Pharmaceuticals, received honoraria from Janssen, Astellas Pharma, Novartis, Tolmar, Amgen, Pfizer, Bayer, Telix Pharmaceuticals, Bristol-Myers Squibb, Merck Serono, AstraZeneca, Sanofi, Ipsen, Merck Sharpe & Dohme, Noxopharm, Aculeus Therapeutics and Daiichi Sankyo, and received research funding Astellas Pharma (institutional), Merck Serono (institutional), Novartis (institutional), Pfizer (institutional), Bristol-Myers Squibb (institutional), Sanofi (institutional), AstraZeneca (institutional), GlaxoSmithKline (institutional), Aptevo Therapeutics (institutional), MedImmune (institutional), Bionomics (institutional), Synthorx (institutional), Astellas Pharma (institutional), Ipsen (institutional), Merck Serono (institutional), Lilly (institutional), Gilead Sciences (institutional), Exelixis (institutional), MSD (institutional) and Hinova Pharmaceuticals (institutional). A.W.W. has received honoraria from Janssen, Astellas Pharma, AstraZeneca, Merck, Bayer, Pfizer and EMD Serono, and received research funding from Promontory Therapeutics (institutional), ESSA Pharma (institutional) and Tyra Biosciences (institutional). The other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks David Miyamoto, Oliver Sartor and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Ulrike Harjes, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 CONSORT diagram for sequencing and enrolment.
CONSORT diagram of participant and sample flow culminating in the formation of the biomarker participant population.
Extended Data Fig. 2 ctDNA% versus baseline PET imaging variables.
Correlation between ctDNA% and four quantitative PET imaging variables. Spearman’s rho (two-sided) is reported for each comparison, with p-values adjusted using Bonferroni correction (α = 0.05, m = 3; correcting for three pairwise comparisons within each imaging modality). A grey line represents the linear regression to illustrate the bivariate relationships. FDG, 2-[18F]fluoro-2-deoxy-D-glucose; MTV, metabolic tumour volume; PSMA, prostate-specific membrane antigen; SUV, standardised uptake value.
Extended Data Fig. 3 PTEN, TP53, and BRCA2 structural variants.
Examples of structural variants and associated focal copy number alterations in (a) PTEN, (b) TP53, and (c) BRCA2. SNP, single nucleotide polymorphism.
Extended Data Fig. 4 Relationship between ctDNA% and molecular imaging variables by PTEN and TP53 status.
Correlation between ctDNA% and two quantitative PET imaging variables (PSMA SUVmean - top, FDG MTV - bottom), stratified by genomic alteration status (PTEN - left, TP53 - right).
Extended Data Fig. 5 PFS and OS by TP53 and PTEN alteration status in all-comers.
Kaplan-Meier estimates of progression-free survival and overall survival stratified by (a) TP53 alteration status and (b) PTEN alteration status. Each survival curve includes estimates for three-levels: ctDNA <2%, intact status, and altered status. In-set summary bar plots in the progression-free survival curves represent the proportion of patients that experienced a PSA50 and PSA90 response. An alteration is defined as any mutation(s) or structural variant(s), deep deletion, or expected null gene status. Monoallelic deletions in isolation were not considered altered. In-set tables show univariable hazard ratios from a Cox proportional hazards model. CI, confidence interval; HR, hazard ratio; mPFS, median progression-free survival; NR, not reached; OS, overall survival; PFS, progression-free survival; PSA, prostate-specific antigen; Ref, reference.
Extended Data Fig. 6 PFS and OS by AR alteration status in all-comers.
Kaplan-Meier estimates of progression-free survival and overall survival stratified by (a) AR gain (defined as ≥4 absolute AR copies) status, (b) presence of AR LBD GSRs, and (c) AR LBD mutation status. Each survival curve includes estimates for three-levels: ctDNA <2%, intact status, and altered status. In-set summary bar plots in the progression-free survival curves represent the proportion of patients that experienced a PSA50 and PSA90 response. In-set tables show univariable hazard ratios from a Cox proportional hazards model. CI, confidence interval; HR, hazard ratio; GSR, gene structural rearrangement; LBD, ligand binding domain; mPFS, median progression-free survival; NR, not reached; OS, overall survival; PFS, progression-free survival; PSA, prostate-specific antigen; Ref, reference.
Extended Data Fig. 7 Clinical outcomes by baseline clinical variables in all-comers.
Forest plots show post-hoc sensitivity analyses for (a) PSA50 response, (b) progression-free survival, and (c) overall survival endpoints according to baseline clinical variables. The ‘All patients’ category includes those in the all-comers biomarker population (n = 178). ALP, alkaline phosphatase; ECOG PS, Eastern Cooperative Oncology Group performance status; FDG, 2-[18F]fluoro-2-deoxy-D-glucose; HR, hazard ratio; MTV, metabolic tumour volume; PSA, prostate-specific antigen; PSMA, prostate-specific membrane antigen; Ref, reference; SUV, standardised uptake value.
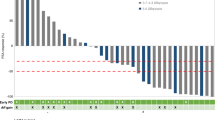
Extended Data Fig. 8 PSA response by DDR alterations.
Best PSA response in the four most commonly altered DNA damage repair-related gene categories: ATM, BRCA1/2, CDK12, and mismatch repair. PSA response for each gene category is expressed at a per-treatment arm level, and further stratified by either (a) PSMA SUVmean (<10 and ≥10) or (b) ctDNA% level (medium [2–30%] and high [>30%]). MMR, mismatch repair; PSA, prostate-specific antigen; PSMA, prostate-specific membrane antigen; SUV, standardised uptake value.
Extended Data Fig. 9 Copy number status in tumour suppressor genes across consecutive samples.
Correlation of the copy number status of tumour suppressor genes TP53, PTEN and RB1 between consecutive ctDNA samples from the same patient. Each dot represents a consecutive sample pair (baseline and progression). Pearson’s correlation coefficient (two-sided) is reported for each comparison.
Supplementary information
Supplementary Information
Consortia authorship, collaborators, list of key sponsors and personnel, and supplementary tables.
Supplementary Tables
List of all mutations and copy number alterations.
Source data
Source Data Fig. 3
Statistical source data (genomics).
Source Data Fig. 6
Statistical source data (genomics).
Source Data Extended Data Fig. 9
Statistical source data (genomics).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kwan, E.M., Ng, S.W.S., Tolmeijer, S.H. et al. Lutetium-177–PSMA-617 or cabazitaxel in metastatic prostate cancer: circulating tumor DNA analysis of the randomized phase 2 TheraP trial. Nat Med 31, 2722–2736 (2025). https://doi.org/10.1038/s41591-025-03704-9
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41591-025-03704-9