Abstract
Recently, fructosamine has shown promising results in predicting adverse outcomes following total knee arthroplasty. The purpose of this study was to assess the utility of fructosamine to predict adverse outcomes following total hip arthroplasty (THA). A prospective multi-center study involving four institutions was conducted. All primary THA were evaluated for glycemic control using fructosamine levels prior to surgery. Adverse outcomes were assessed at a minimum 1 year from surgery. Primary outcome of interest was periprosthetic joint infection (PJI) based on the International Consensus Meeting (ICM) criteria. Secondary outcomes assessed were superficial infections, readmissions and death. Based on previous studies on the subject, fructosamine levels above 293 µmol/L were used to define inadequate glycemic control. Overall 1212 patients were enrolled in the present study and were available for follow up at a minimum 1 year from surgery. Of those, 54 patients (4.5%) had elevated fructosamine levels (> 293 µmol/L) and these patients were 6.7 times more likely to develop PJI compared to patients with fructosamine levels below 293 µmol/L (p = 0.002). Patients with elevated fructosamine were also associated with more readmissions (16.7% vs. 4.4%, p < 0.007) and a higher mortality rate (3.7% vs. 0.6%, p = 0.057). These associations remained statistically significant in a multi-regression analysis after adjusting for age, comorbidities and length of stay; Adjusted odds ratio were 6.37 (95% confidence interval 1.98–20.49, p = 0.002) for PJI and 2.68 (95% confidence interval 1.14–6.29, p = 0.023) for readmissions. Fructosamine is a good predictor of adverse outcomes in patients undergoing THA and should be used routinely to mitigate morbidity and mortality risk.
Similar content being viewed by others
Introduction
Much attention has been devoted in recent years to develop strategies that can mitigate the risk of adverse outcomes following total joint arthroplasty (TJA), with a special emphasis to strategies that can reduce periprosthetic joint infection (PJI)1,2. Among the risk factors known to affect outcome of any surgical procedure, including TJA, is proper glycemic control1,3,4,5. The latter is ever more important as up to 50% of patients undergoing THA were found to have hyperglycemia6,7. Moreover, glycemic control is considered one of the only modifiable factors, the control of which is demonstrated to reduce the risk of complications8,9.
While it is well acknowledged that hyperglycemia is associated with adverse outcomes following surgery, there remains controversy about which glycemic markers to use and what interval from surgery they are most predictive1,4. In the preoperative period, 3 month glycemic control as measured by glycated hemoglobin (HbA1c) has been used, whereas in the perioperative period fasting glucose is routinely used for risk stratification10,11,12,13 Many institutions now use predetermined cutoffs values for both fasting glucose and HbA1c, and postpone surgery to patients with elevated levels of one or both of these glycemia markers. The effectiveness of this protocol in reducing complications is yet to be proven14.
Fructosamine is not a new glycemic marker15. The monitoring of glycated protein (mainly albumin) was introduced 40 years ago and has recently been revisited as a tool for preoperative screening due to clear advantages in the preoperative period16,17. The fact that fructosamine represents sugar levels over a 2–3 week period makes it a valuable marker for both screening and monitoring therapeutic interventions. If patients with inadequate glycemia control were to have elective surgery postponed based on elevated fructosamine levels, return to better glycemic control could be confirmed within 2 weeks using fructosamine as opposed to 3 months using HbA1c.
In a recent study, fructosamine was shown to be more valuable than HbA1c in predicting early complications following TKA16. The purpose of this prospective multicenter study was to evaluate the role of fructosamine in predicting 1-year complications in patients undergoing elective THA.
Materials and methods
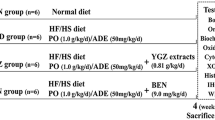
Following IRB approval by the ethics committee of Thomas Jefferson University Hospital (IRB-16D.225), NYU Langone (IRB-i18-00017), Columbia University (IRB-AAAR7050), and University of Louisville (IRB-17.0813), these four academic centers participated in this prospective study. Written informed consent was obtained from all participants of this study. All methods were carried out in accordance with the relevant guidelines and regulations based on the approvals. During the time period between August 2017 and November 2018, all elective primary THA patients performed by 8 fellowship trained surgeons were investigated for glycemic control using fructosamine, HbA1c and fasting plasma glucose (FPG) levels within four weeks prior to surgery. Postoperative day 1 (POD) morning glucose levels were also captured. Patients were followed-up for a minimum of 1 year.
Data collection
Demographic and perioperative factors that could serve as confounders were collected and are presented in Table 1. Obesity was defined as body mass index (BMI) above 30 kg/m2. Charlson Comorbidity Index (CCI) was calculated for each patient based on medical records. Special attention was given to diabetic status and was collected both from self-reported questionnaires, as well as from medical records. Diabetes was considered complicated if systemic complications were present.
The primary outcome assessed was PJI based on the 2018 International Consensus Meeting (ICM) definition18. Secondary adverse outcomes included superficial wound complications, hospital readmissions for causes related to their surgery (including deep vein thrombosis and prosthesis-related complications) and death. A wound complication was predefined and included more than 1 week of drainage, postponed hospital discharge due to wound issues, the use of antibiotics, or return to the operating room for wound care.
Statistical analysis
A power analysis was performed based on prior literature and the rate of PJI stratified based on fructosamine levels (above and below 293 µmol/L) was predicted to be approximately 1:3.5. Sample size was projected supposing a 2-sided t-test with an alpha level of 0.05 and 0.8 power. A sample size of 1100 patients was deemed appropriate. Inadequate glycemic control was assumed in patients with fructosamine levels above 293 µmol/L (4) For verification, receiver operating characteristic (ROC) analysis was performed and the area under the curve (AUC) was calculated for fructosamine and the risk for PJI. Adverse outcomes were assessed following glycemic control stratification. Categorical variables were analyzed using the Chi square test and continuous variables by the Student’s t-test. A p value < 0.05 was considered significant except for death, where a p value < 0.1 was set to be considered statistically significant due to its gravid impact. All demographic, comorbidity and hospitalization variables that were significantly different between those with high (above 293 µmol/L) and normal (below 293 µmol/L) fructosamine were included in a logistic regression analysis, and adjusted odds ratios were calculated. Death was not assessed in a regression analysis due to the minor incidence. A scatter plot was created to assess the association between fructosamine and HbA1c levels. A subgroup analysis of patients with FPG levels above 100 mg/dL was also performed to assess the utility of fructosamine in a more specific cohort.
Results
During the study period a total of 1,212 patients (616 females) underwent THA who had preoperative fructosamine collected and were available for 1-year follow-up after their primary THA. Mean age was 63.9 years (standard deviation [SD] 11.39). Overall, 111 patients (9.2%) were known to have diabetes. Screening all THA patients using HbA1c revealed that many patients were unaware of their diabetic state. Of the 303 patients who had HbA1c levels in the prediabetes range (5.7–6.5%) upon screening, only 45 (15%) were previously diagnosed with diabetes (i.e. 85% were unaware of their pre-diabetic state), and of the 88 patients with HbA1c levels in the diabetic range (≥ 6.5%), only 51 patients (58%) had a prior diagnosis of diabetes (i.e. 42% were unaware they had diabetes) (Fig. 1).
Mean fructosamine levels were 241.91 µmol/L (range, 108 to 490) for the entire cohort. In 54 patients (4.5%) fructosamine levels were greater than 293 µmol/L indicating inadequate glycemic control, however only 21 of them (38.9%) had a prior diagnosis of diabetes. Compared to patients with fructosamine levels below 293 µmol/L, patients with levels greater than 293 µmol/L were older (p < 0.001), had more comorbidities (p = 0.001) including diabetes (p < 0.001) and had a longer hospital stay (p = 0.009), as presented in Table 1.
High fructosamine levels were associated with PJI (AUC 0.58, 95% Confidence Interval 0.40–0.70]. Fructosamine levels above 293 µmol/L were significantly associated with PJI, readmissions and death (Table 2, Fig. 2). PJI rates were 6.64 times higher (p = 0.002), readmission rates were 3.80 times higher (p = 0.001), and mortality was 6.17 times higher (p = 0.057) in patients with elevated fructosamine levels. Superficial wound complication rates were similar between those with fructosamine levels above and below 293 µmol/L (3.7% versus 2.5%, p = 0.645). After adjusting for age, comorbidities and length of stay which were all significantly (p < 0.05) higher in those with fructosamine above 293 µmol/L, the above associations with PJI (adjusted odds ratio 6.37, 95% confidence interval 1.98–20.49; p = 0.002) and readmissions (adjusted odds ratio 2.68, 95% confidence interval 1.14–6.29; p = 0.023) remained statistically significant.
In the subgroup of patients with FPG above 100 mg/dL (n = 423), a higher proportion of patients had fructosamine levels above 293 µmol/L (7.6%). Four of the 5 PJI cases, 7 of the 9 readmissions and 1 of the 2 deaths that were captured in those with elevated fructosamine had occurred in patients with FPG above 100 mg/dL. As before, associations with PJI and readmissions were significantly higher in those with fructosamine levels above 293 µmol/L (Table 2).
There was a positive correlation between fructosamine and HbA1c levels (Fig. 3). Of the patients who had fructosamine levels greater than 293 µmol/L, 39 patients (72.2%) were in the prediabetes or diabetes range based on HbA1c levels. Fructosamine levels greater than 293 µmol/L were significantly associated with higher FPG, and higher POD-1 glucose levels (Table 3). However, among the 5 patients with fructosamine greater than 293 µmol/L who developed PJI, only 2 had a diagnosis of diabetes. HbA1c levels were less than 7.5% in 2 of these patients (40%) and less than 8% in 4 of them (80%). On the contrary, there were no patients with HbA1c levels above 7.5% or 8.0% that did not have fructosamine levels above 293 µmol/L.
Discussion
The main finding of this prospective study was that fructosamine, as a glycemic marker, is an excellent predictor of adverse outcomes following THA. Another important, and sobering, finding of the study, that corroborates prior studies6,7, is that a large proportion of patients undergoing elective THA appear to be hyperglycemic or undiagnosed diabetics who are unaware of their poor glycemic control. In a recent International Consensus Meeting (ICM), the issue of screening all patients for hyperglycemia prior to surgery was discussed with 76% of delegates voted in favor of such protocol19. The rationale behind such recommendation is that by evaluating glycemic control only in patients with known diabetes, we are neglecting a large cohort of patients with unrecognized hyperglycemia and/or diabetes that are at increased risk for complications20. The major question that remains is which agent best represents the glycemic control of a patient.
HbA1c remains the gold standard for assessing glycemic control and is invaluable in the treatment of diabetic patients. It is a predictor of diabetic complications, and interventions that lower HbA1c levels have proved themselves useful in reducing the risk of complications21. Whereas the overall utility of HbA1c is beyond question, discordances between HbA1c and other clinically reliable biochemical measures of glycemic control such as fructosamine are commonly encountered22. These discordances are mainly attributed to the time frame over which HbA1c equilibrates compared with shorter-term measures of plasma glucose23,24,25. It has also been hypothesized that discordances between HbA1c and other measures of glycemia such as fructosamnie are due to physiologic processes consistent within individuals over time and these variations by them self may have a role in predicting complications26. Our finding of elevated fructosamone levels in patients without a diagnosis of diabetes or elevated HbA1c levels is in accordance with the above mentioned discordances and reinforces recent findings in arthroplasty patients16,17,27.
It has become common practice to evaluate the preoperative HbA1c level in patients with diabetes prior to surgery and postpone surgery in patients with elevated levels19. The American Diabetes Association (ADA) states that HbA1c > 7% is representative of poor glycemic control28. In a recent multicenter study on patients undergoing TJA, HbA1c > 7.7% was found to be associated with higher rate of PJI and other complications10. Based on the latter study, our institution and many others will cancel elective orthopedic surgery in patients with HbA1c > 7.5 or 8%4,11,29. While the rationale behind such practice appears to be logical, the value of this protocol in reducing postoperative complications has not been proven. Further, HbA1c represents glycemic control over the 120 day life cycle of red blood cells. Thus, patients with elevated HbA1c who had their elective surgery cancelled may need to wait for 3 months before confirming that implementation of better glycemic control was effective and be able to undergo surgery. Another glycemic marker that has proven to be valuable is fasting blood glucose4. The Center for Disease Control (CDC) in their recent guidelines for prevention of surgical site infection states that patients with fasting glucose of 200 mg/dL have a poor glycemic control and should not undergo elective surgical procedures1. Though valuable, there are logistic issues associated with measuring fasting glucose levels in patients awaiting elective surgery. Further, fasting glucose levels are under immense influence of numerous factors including stress, which most patients undergoing surgery would exhibit30,31.
Fructosamine is a measure of glycated protein in the plasma, with albumin being the major constituent, and thus reflects glycemic control over the proceeding 2–3 weeks32. In daily diabetes care unrelated to surgery, fructosamine adds little to the commonly used HbA1c, as majority of literature pertaining to screening and treatment is on the latter. In the preoperative period, fructosamine has a substantial advantage as a glycemic marker as it allows one to monitor response to treatment in a much shorter time frame compared to HbA1c. The current study adds to the body of literature that shows fructosamine is a valuable screening tool for hyperglycemia in patients undergoing elective surgery16,17. There is a direct correlation between fructosamine and HbA1c in patients with and without diabetes, as seen in this study. While a correlation between the two glycemic markers exists, there are important differences, mostly related to the time frame of glycemic control that each of these markers represent. There are variations in institutional policies regarding the optimal threshold for HbA1c, with most institutions using HbA1c between 7.5 and 8.0% as representative of poor glycemic control4. The current study demonstrates that if such thresholds for HbA1c were to be used, instead of the fructosamine levels, many patients who developed PJI or had adverse outcome would have been missed.
This study adds to recent reports on the utility of fructosamine as a valuable glycemic marker, particularly in patients undergoing elective TJA16,17. The cost of fructosamine testing is negligible compared to the costs associated with complications following THA, and if it is indeed used in the preoperative period it may also be cos-beneficial. The cost of a single fructosamine test is $19.77 amounting to a total cost of $23,961 in the current study whereas the cost of treating a single PJI event is estimated as $100,000 per case33. The fact that 5 patients with high fructosamine levels developed PJI that could have been theoretically prevented, support the notion that all patients undergoing THA should be screened for glycemic control using fructosamine. However, we are aware that screening all patients prior to surgery may not be possible for many institutions. In an attempt to isolate a smaller group that would benefit from screening, we performed a sub-analysis of the current cohort and discovered that patients with fasting glucose > 100 mg/dL would most benefit from glycemic screening using fructosamine. Screening only those with high fasting glucose would reduce by 65% the number of patients that are screened, and still capture 80% of the patients that are at higher risk of postoperative complications. Interestingly, not only high fructosamine levels are informative, but normal levels are also beneficial in risk stratification. A normal fructosamine level in patients with FPG > 100 mg/dL can be reassuring for the treating physician as complication rates in this group were similar to those seen with FPG < 100 mg/dL. This strategy of screening may be an efficient compromise for certain centers.
While we cannot say for sure why exactly fructosamine is such a powerful prognostic marker, there are several theories. First, fructosamine reflects fluctuations in glucose which have been associated with complications following TJA27,34,35. Both in-vivo and in-vitro studies attribute the negative effects of these fluctuations to the activation of pro-inflammatory proteins and excessive oxidative stress36. Furthermore, short-term fluctuations in glucose levels may have a larger effect on inflammatory cytokine levels than continuous hyperglycemia and has been shown to affect all major components of innate immunity, namely decreased neutrophil chemotaxis and phagocytosis thus impairing the ability of the host to combat infection37,38. Second, it is possible that it is not the essence of diabetes itself, but the high sugar level close to surgery that increase susceptibility to surgical site infections. By reflecting glucose levels over the 2–3 weeks prior, fructosamine better reflects the glycemic control closer to surgery. Finally, fructosamine may be a more sensitive marker for glycemic disturbances in patients without diabetes39.
This study had several limitations. First and most importantly, this was an observational study and while the results suggest an association between fructosamine and complications, we cannot say for sure that controlling fructosamine level would lead to a reduction in complication rates. Second, fructosamine was evaluated within 1 month of surgery, and perhaps if it were taken closer to surgery, it may have been a better prognostic marker. Third, there are several factors that may affect serum protein levels, and therefore impact fructosamine levels, which we did not take into consideration. For example, hepatic cirrhosis, protein loosing enteropathies, and other conditions are known to affect plasma protein levels and possibly the level of fructosamine. Finally, fructosamine levels and the threshold used in this study may be affected by differences in labs and reagents used for testing. Future studies are needed to validate the threshold used in this study or suggest a more optimal cut-off level.
This multi-intuitional prospective study supports recent reports on the utility of fructosamine testing prior to total joint arthroplasty. Fructosamine holds major advantages over HbA1c in the preoperative period. We propose that centers without prior experience of using this test, consider adding the test to their screening programs for hyperglycemia, particularly in patients who have fasting glucose greater than 100 mg/dL.
Change history
02 August 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41598-021-94867-1
References
Berríos-Torres, S. I. et al. Centers for disease control and prevention guideline for the prevention of surgical site infection. JAMA Surg. 152(8), 784–791 (2017).
Shohat, N. & Parvizi, J. Prevention of periprosthetic joint infection: Examining the recent guidelines. J. Arthroplasty 32(7), 2040–2046 (2017).
Kao, L. S. & Phatak, U. R. Glycemic control and prevention of surgical site infection. Surg. Infect. 14(5), 437–444 (2013).
Shohat, N. et al. Inadequate glycemic control is associated with increased surgical site infection in total joint arthroplasty: A systematic review and meta-analysis. J. Arthroplasty 33(7), 2312–2321 (2018).
WHO. Global Guidelines on the Prevention of Surgical Site Infection (WHO, Geneva, 2017).
Capozzi, J. D. et al. The prevalence of diabetes mellitus and routine hemoglobin a1c screening in elective total joint arthroplasty patients. J. Arthroplasty 32(1), 304–308 (2017).
Shohat, N. et al. All patients should be screened for diabetes before total joint arthroplasty. J. Arthroplasty 33(7), 2057–2061 (2018).
Yoneda, A. et al. Improvement in hyperglycemia prevents surgical site infection irrespective of insulin therapy in non-diabetic patients undergoing gastrointestinal surgery. World J. Surg. 44(5), 1450–1458 (2020).
Nussenbaum, F. D., Rodriguez-Quintana, D., Fish, S. M., Green, D. M. & Cahill, C. W. Implementation of preoperative screening criteria lowers infection and complication rates following elective total hip arthroplasty and total knee arthroplasty in a veteran population. J. Arthroplasty 33(1), 10–13 (2018).
Tarabichi, M. et al. Determining the threshold for hba1c as a predictor for adverse outcomes following total joint arthroplasty: A multicenter, retrospective study. J. Arthroplasty 32(9S), S263–S267 (2017).
Cancienne, J. M., Werner, B. C. & Browne, J. A. Is there an association between hemoglobin A1C and deep postoperative infection after TKA?. Clin. Orthop. 475(6), 1642–1649 (2017).
Kremers, H. M. et al. Diabetes mellitus, hyperglycemia, hemoglobin a1c and the risk of prosthetic joint infections in total hip and knee arthroplasty. J. Arthroplasty 30(3), 439–443 (2015).
Jämsen, E., Nevalainen, P., Kalliovalkama, J. & Moilanen, T. Preoperative hyperglycemia predicts infected total knee replacement. Eur. J. Intern. Med. 21(3), 196–201 (2010).
Giori, N. J., Ellerbe, L. S., Bowe, T., Gupta, S. & Harris, A. H. S. Many diabetic total joint arthroplasty candidates are unable to achieve a preoperative hemoglobin A1c goal of 7% or less. J. Bone Jt. Surg. Am. 96(6), 500–504 (2014).
Johnson, R. N., Metcalf, P. A. & Baker, J. R. Fructosamine: A new approach to the estimation of serum glycosylprotein. An index of diabetic control. Clin. Chim. Acta Int. J. clin. Chem. 127(1), 87–95 (1983).
Shohat, N. et al. 2019 John Insall award: Fructosamine is a better glycaemic marker compared with glycated haemoglobin (HbA1C) in predicting adverse outcomes following total knee arthroplasty: A prospective multicentre study. Bone Jt. J. 101, 3–9 (2019).
Shohat, N., Tarabichi, M., Tischler, E. H., Jabbour, S. & Parvizi, J. Serum fructosamine: A Simple and inexpensive test for assessing preoperative glycemic control. J. Bone Jt. Surg. Am. 99(22), 1900–1907 (2017).
Parvizi, J. et al. The 2018 definition of periprosthetic hip and knee infection: An evidence-based and validated criteria. J. Arthroplasty 33(5), 1309–1314 (2018).
Jiranek, W. et al. General assembly, prevention, host risk mitigation—General factors: Proceedings of International Consensus on orthopedic infections. J. Arthroplasty 34(2), S43–S48 (2019).
MacFarlane, L. A. et al. Assessment for perioperative hyperglycemia prior to total joint replacement in patients with and without diabetes. JAMA Netw. Open 2(9), e1910589 (2019).
Diabetes Control and Complications Trial Research Group et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 329(14), 977–986 (1993).
Nathan, D. M., Singer, D. E., Hurxthal, K. & Goodson, J. D. The clinical information value of the glycosylated hemoglobin assay. N. Engl. J. Med. 310(6), 341–346 (1984).
Tahara, Y. & Shima, K. Kinetics of HbA1c, glycated albumin, and fructosamine and analysis of their weight functions against preceding plasma glucose level. Diabetes Care 18(4), 440–447 (1995).
Narbonne, H., Renacco, E., Pradel, V., Portugal, H. & Vialettes, B. Can fructosamine be a surrogate for HbA(1c) in evaluating the achievement of therapeutic goals in diabetes?. Diabetes Metab. 27(5 Pt 1), 598–603 (2001).
Braatvedt, G. D., Drury, P. L. & Cundy, T. Assessing glycaemic control in diabetes: Relationships between fructosamine and HbA1C. N. Z. Med. J. 110(1057), 459–462 (1997).
Cohen, R. M., Holmes, Y. R., Chenier, T. C. & Joiner, C. H. Discordance between HbA1c and fructosamine: Evidence for a glycosylation gap and its relation to diabetic nephropathy. Diabetes Care 26(1), 163–167 (2003).
Shohat, N., Foltz, C., Restrepo, C., Goswami, K., Tan, T. & Parvizi, J. Increased postoperative glucose variability is associated with adverse outcomes following orthopaedic surgery. Bone Joint J. 100-B(8), 1125–1132 (2018).
American Diabetes Association. 6. Glycemic targets: Standards of medical care in diabetes—2020. Diabetes Care 43(Suppl 1), S66–S76 (2020).
Cancienne, J. M., Werner, B. C. & Browne, J. A. Is there a threshold value of hemoglobin a1c that predicts risk of infection following primary total hip arthroplasty. J. Arthroplasty 32(9S), S236–S240 (2017).
Chen, Y. et al. Stress-induced hyperglycemia after hip fracture and the increased risk of acute myocardial infarction in nondiabetic patients. Diabetes Care 36(10), 3328–3332 (2013).
McCowen, K. C., Malhotra, A. & Bistrian, B. R. Stress-induced hyperglycemia. Crlt. Care Clin. 17(1), 107–124 (2001).
Danese, E., Montagnana, M., Nouvenne, A. & Lippi, G. Advantages and pitfalls of fructosamine and glycated albumin in the diagnosis and treatment of diabetes. J. Diabetes Sci. Technol. 9(2), 169–176 (2015).
Kurtz, S. M., Lau, E., Watson, H., Schmier, J. K. & Parvizi, J. Economic burden of periprosthetic joint infection in the United States. J. Arthroplasty 27(8), 61–65.e1 (2012).
Shohat, N. et al. Increased postoperative glucose variability is associated with adverse outcomes following total joint arthroplasty. J. Bone Jt. Surg. Am. 100(13), 1110–1117 (2018).
Akirov, A., Diker-Cohen, T., Masri-Iraqi, H. & Shimon, I. High glucose variability increases mortality risk in hospitalized patients. J. Clin. Endocrinol. Metab. 102(7), 2230–2241 (2017).
Monnier, L. et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 295(14), 1681–1687 (2006).
Esposito, K. et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: Role of oxidative stress. Circulation 106(16), 2067–2072 (2002).
Turina, M., Miller, F. N., Tucker, C. F. & Polk, H. C. Short-term hyperglycemia in surgical patients and a study of related cellular mechanisms. Ann. Surg. 243(6), 845–853 (2006).
Manjrekar, P. et al. Fructosamine in non-diabetic first degree relatives of type 2 diabetes patients: Risk assessor. J. Clin. Diagn. Res. 6(5), 770–773 (2012).
Funding
The study was partly funded by the American Association of Hip and Knee Surgeons.
Author information
Authors and Affiliations
Contributions
N.S.: Study Conception; Data Collection; Data Analysis; Manuscript Writing and Editing. K.G., L.B., M.H. and A.M.: Data Collection; Data Analysis; Manuscript Writing and Editing. R.P.S. and R.S.: Study Design; Data Collection; Data Analysis; Manuscript Writing and Editing. J.P.: Study Conception; Study Design; Data Collection; Data Analysis; Manuscript Writing and Editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in Table 2, where in columns “Total cohort (n = 1212)” and “Fasting plasma glucose ≥ 100 mg/dL (n = 423)”, the n values for ‘Normal fructosamine’ and ‘High fructosamine’ were accidently switched.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shohat, N., Goswami, K., Breckenridge, L. et al. Fructosamine is a valuable marker for glycemic control and predicting adverse outcomes following total hip arthroplasty: a prospective multi-institutional investigation. Sci Rep 11, 2227 (2021). https://doi.org/10.1038/s41598-021-81803-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-81803-6
This article is cited by
-
Periprosthetic joint infection after arthroplasty: advances and future prospects
Journal of Orthopaedic Surgery and Research (2025)
-
S-144 lack of association between glycated hemoglobin and adverse outcomes in diabetic patients undergoing ventral hernia repair: an ACHQC study
Surgical Endoscopy (2023)
-
Higher reinfection rate after two-stage revision arthroplasty in patients with refractory diabetes mellitus: a retrospective analysis with a minimum ten-year follow up
BMC Musculoskeletal Disorders (2022)