Abstract
Epicardial adipose tissue (EAT) can play an important role in the occurrence and development of atrial fibrillation and stroke. In this study, we explored the relationship between left atrial epicardial adipose tissue (LA-EAT) and left atrial appendage flow velocity (LAA-FV) in patients with nonvalvular atrial fibrillation (NV-AF). A total of 145 patients with NV-AF who underwent their first radiofrequency ablation were enrolled. They underwent left aortopulmonary vein computed tomography angiography (CTA) and transesophageal echocardiography (TEE) before AF ablation. Left atrial (LA) electroanatomical mapping was performed intraoperatively to assess left atrial voltage. Univariate regression analysis showed that LAA-FV was lower in patients with a low voltage zone (LAA-FV; 35.02 ± 10.78 cm/s vs. 50.60 ± 12.17 cm/s, P < 0.001). A multiple linear regression model showed that the left atrial low voltage zone (β = − 0.311 P < 0.001), LA-EAT volume (β = − 0.256 P < 0.001), left atrial appendage shape (β = − 0.216 P = 0.041), LAVI (β = − 0.153 P = 0.041), and type of atrial fibrillation (paroxysmal vs. persistence) (β = − 0.146 P < 0.048) were independent predictors of LAA-FV. In NV-AF patients, the increase in LA-EAT volume is related to the decrease in LAA-FV.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common arrhythmia1. Although the management of atrial fibrillation has been continuously improved, there are obvious limitations of antiarrhythmic drug therapy and radiofrequency ablation2,3, and the long-term maintenance of sinus rhythm in patients with atrial fibrillation is challenging. Therefore, anticoagulation therapy is very important.
The most important source of embolic stroke in patients with nonvalvular atrial fibrillation (NV-AF) is the left atrial appendage4. Many studies have shown that a decrease in left atrial appendage velocity (LAA-FV) is closely related to left atrial appendage mural thrombosis5,6. At present, the main measurement method for LAA-FV is transesophageal ultrasound7, but this is a semi-invasive approach, and its accuracy is related to the skill level of the operator. During the COVID-19 pandemic, noninvasive tests were recommended to reduce the risk of exposure to the virus8,9. Epicardial adipose tissue (EAT) is in direct contact with the surface of the atrium and pulmonary vein and, like the myocardium, is supplied by the coronary artery10, which can play an important role in the occurrence and development of atrial fibrillation and stroke through a variety of mechanisms, such as fat infiltration, fibrosis and inflammation11,12. Previous studies have shown that myocardial fibrosis is closely related to the velocity of the left atrial appendage13,14. However, the relationship between epicardial adipose tissue and left atrial appendage velocity is rarely reported.
With the popularization and development of electrophysiological technology in recent years15,16, it is generally accepted that atrial fibrosis can be shown by mapping the low voltage zone through electrophysiological intracavitary voltage mapping17,18. In this study, we identified atrial fibrosis by left atrial voltage mapping during radiofrequency ablation to explore the relationship between LA-EAT and left atrial appendage velocity in patients with nonvalvular atrial fibrillation. We hope to find a safe and reliable index to evaluate left atrial appendage function.
Methods
Study population
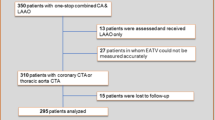
A total of 145 patients with nonvalvular atrial fibrillation who underwent their first radiofrequency ablation at the Affiliated Hospital of Xuzhou Medical University between 2020 and 2021 were selected. All patients underwent CTA and TEE examinations of the left atrium and pulmonary vein before the operation. There were 76 patients with paroxysmal atrial fibrillation and 69 patients with nonparoxysmal atrial fibrillation. All patients were diagnosed with atrial fibrillation by electrocardiogram and/or dynamic electrocardiogram. Paroxysmal atrial fibrillation is defined as atrial fibrillation that lasts less than 7 days and terminates spontaneously, while persistent atrial fibrillation is defined as atrial fibrillation that lasts more than 7 days or requires electrical cardioversion and/or drug cardioversion to terminate. Exclusion criteria: (1) previous catheter ablation of atrial fibrillation or other cardiac surgery; (2) hyperthyroidism; (3) rheumatism and other cardiac valvular diseases; (4) active connective tissue disease; and (5) inability to undergo CTA or CT imaging or inability to obtain complete left atrial appendage data because of contrast medium allergy. This study was reviewed by the Ethics Committee of the Affiliated Hospital of Xuzhou Medical University, and all patients signed informed consent forms.
Echocardiographic measurements
Transthoracic echocardiography (TTE) was performed with a Philips EPIQ7c ultrasonic diagnostic instrument, S5-1 probe and probe frequency 1–5 MHz. Parameters such as left ventricular ejection fraction (measured by the biplane Simpson's method) were recorded in detail in the left recumbent position. TEE was examined by PhilipsiE33 color Doppler ultrasonography with an X7-2t transesophageal matrix real-time three-dimensional probe with a frequency of 2–7 MHz. Before fasting for 6–8 h, the ECG was recorded synchronously, the pulsed Doppler sampling volume was placed within 1 pulse near the opening of the left atrial appendage, and the blood flow spectrum of the left atrial appendage was obtained. The left atrial appendage blood flow spectrum was a regular two-way wave in sinus rhythm and an irregular zigzag waveform in atrial fibrillation rhythm. The peak value of the positive wave, that is, the maximum emptying velocity of the left atrial appendage, was recorded in 3 and 10 cardiac cycles, respectively, and the average value was taken as the velocity of the left atrial appendage (LAA-FV) (Fig. 1–2).
Cardiac computed tomography imaging
Spiral CT (SOMATOM Definition, SIEMENS Germany) was used to obtain CT imaging data. Iohexol (60–80 ml) was injected into the elbow vein at a flow rate of 5 ml/s, and then saline (50 ml) was injected at a speed of 5 ml/s. The contrast agent tracking technique triggered the enhanced scan. Image processing and measurement: All images were reconstructed by retrospective ECG gated reconstruction, slice thickness 0.5 mm, overlapping 0.3 mm, and image postprocessing was performed by an Advantage Workstation 3.2 (GE, USA) workstation. The CT threshold range of the adipose tissue was set to − 50 HU ~ − 200 HU. The left atrial epicardial adipose tissue (LA-EAT) was manually segmented, and the LA-EAT was calculated (Fig. 3). Three-dimensional images of the left atrial appendage and left atrium were obtained by three-dimensional reconstruction of the volume. According to the morphological characteristics of the left atrial appendage, the left atrial appendage was divided into three types: chicken wing type (chicken wing), obvious folding in the proximal or middle part of the main lobe of the left atrial appendage, and nonchicken wing type (nonchicken wing), excluding other forms of chicken wing type. The left atrial volume (LAV) and left atrial volume index (LAVI) were calculated, defined as the left atrial volume divided by the body surface area. All images were measured and evaluated by two independent clinicians using the same measurement methods, and any inconsistencies were resolved through consultation.
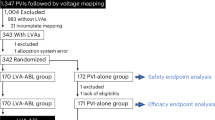
Detection of the low voltage zone (LVZ)
All patients first underwent circumferential pulmonary vein isolation (PVI). Left atrial voltage mapping was performed directly in patients with paroxysmal atrial fibrillation after PVI. Patients with persistent atrial fibrillation underwent synchronous electrocardioversion if they were still in atrial fibrillation after isolation, and voltage mapping was performed after cardioversion. Voltage mapping was carried out with an ST ablation catheter (Johnson Company, USA), and contact force values of > 5 g for mapping electrograms confirmed adequate endocardial contact. We used ≥ 3 adjacent peak-to-peak bipolar voltage cutoffs of 0.2–0.5 mV to define the low-voltage region to more accurately delineate the LAVI19 (Fig. 4).
Statistical analysis
If the measurement data were normally distributed, they were expressed as the mean ± SD. If they do not conform to a normal distribution, they are expressed by the median (quartile spacing), that is, M (Q25 Q75), and the counting data are expressed by the number (percentage). The counting data were compared by Student’s t test or Wilcoxon's singed rank-sum tests (nonnormal distribution), and the classified variables were compared by chi-square tests or Fisher’s exact test. Pearson or Spearman correlation tests were used to evaluate the relationship between LAA-FV and various parameters. In addition, to evaluate the independent predictors of LAA-FV, multiple regression analysis was carried out. P < 0.05 was considered to be statistically significant. All statistical analyses were carried out using SPSS version 24.0 software (SPSS, Chicago, Illinois, USA).
Ethics declarations
Patient studies were approved by the Ethics Committee of Affiliated Hospital of Xuzhou Medical University. All methods were implemented in accordance with relevant guidelines and regulations, and all enrolled patients signed informed consent forms.
Results
Characteristics of the study population
The characteristics of the patients are shown in Table 1. A total of 145 patients with symptomatic atrial fibrillation [76 with paroxysmal atrial fibrillation (52.41%) and 69 with nonparoxysmal atrial fibrillation (47.59%), including 6 with long-term persistent atrial fibrillation] were included, including 98 men (67.59%). The mean body mass index (BMI) was 25.24 ± 3.14 kg/m2, the left atrial volume index (LAVI) was 68.26 ± 23.97 ml/m2, the left atrial epicardial adipose tissue volume (LA-EAT) was 30.72 ± 11.81 ml, and the left atrial appendage flow rate (LAA-FV) was 47.59 ± 13.38 cm/s.
Comparison of baseline data and echocardiographic parameters
CARTO3 voltage mapping of the left atrium was performed in all cases under sinus rhythm, and an average of 864 marker points were obtained in each case. No complications occurred during the process of LA mapping. The voltage mapping results were used to divide the patients into a low voltage zone group (LVZ group) and a nonlow voltage group (non-LVZ group). Among them, 28 patients (19.31%) had left atrial LVZ. The clinical features, epicardial adipose tissue and echocardiographic parameters of the LVZ group and non-LVZ group were compared, and the results are shown in Table 2. Univariate analysis showed that the age of the LVZ group was older than that of the non-LVZ group. There were significant differences in terms of history of diabetes, left atrial volume index (LAVI), LA-EAT volume and left atrial appendage velocity (LAA-FV) between the two groups. In the LVZ group, there was more nonparoxysmal atrial fibrillation (P < 0.1), and the duration of atrial fibrillation was longer (P < 0.1). There was no significant difference in any other clinical or conventional echocardiographic parameters, including left ventricular ejection fraction, between the two groups (P > 0.05, Table 2).
Relationship between LAA-FV and relevant parameters
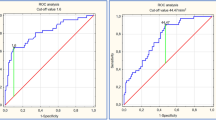
There were significant negative correlations between LAA-FV and left atrial volume index (LAVI) (r = − 0.345, P < 0.001; Fig. 5A) and between LAA-FV and LA-EAT volume (r = − 0.414, P < 0.001; Fig. 5B).
Univariate and multiple linear regression analyses of LAA-FV
Univariate regression analysis showed that LAA-FV was lower in the patients with an LVZ (with low voltage and without low voltage; 35.02 ± 10.78 cm/s vs. 50.60 ± 12.17 cm/s, P < 0.001) and nonchicken wing type (nonchicken wing type and chicken wing type; 44.82 ± 11.91 cm/s vs. 52.71 ± 14.53 cm/s, P = 0.001). The LAA-FV of the persistent AF group was lower than that of the paroxysmal AF group (42.15 ± 12.53 cm/s vs. 52.54 ± 12.14 cm/s, P < 0.001). In addition, a lower LAA-FV was significantly correlated with the left atrial volume index (LAVI) and the LA-EAT volume (p ≤ 0.001). In a multiple linear regression model, the left atrial LVZ (β = − 0.311, P < 0.001), LA-EAT volume (β = − 0.256, P < 0.001), left atrial appendage shape (β = − 0.216, P < 0.001), LAVI (β = − 0.153, 0.041), and type of atrial fibrillation (paroxysmal vs. persistence) (β = − 0.146, 0.048) were independent predictors of LAA-FV (Table 3).
Discussion
In recent years, increasing attention has been given to the relationship between epicardial adipose tissue and atrial fibrillation (AF). Venteclef et al.20 reported that human adventitia adipose tissue (EAT) caused fibrosis of atrial cardiomyocytes in rats and promoted fibroblasts to differentiate into myofibroblasts. At present, the clinical detection methods for myocardial fibrosis are limited. Myocardial fibrosis is mainly detected through endocardial biopsy, late gadolinium enhancement cardiac magnetic resonance (LGE-CMR) and intracardiac voltage mapping. In this study, left atrial voltage mapping was performed during radiofrequency ablation, and patients with atrial fibrillation were divided into an LVZ group and a non-LVZ group. Compared with the non-LVZ group, the LAA-FV in the LVZ group was lower. This is consistent with the results of previous studies that show that there may be a correlation between atrial fibrosis and left atrial appendage velocity13,14. At present, TEE is the most widely used method to measure the function of the LAA, and it is considered the gold standard, but it is semi-invasive. We hope to find a non-invasive and reliable index to evaluate left atrial appendage function. In this study, it was found that left atrial LVZ, LA-EAT volume, left atrial appendage shape, left atrial volume index and type of atrial fibrillation (paroxysmal vs. persistence) were independent predictors of LAA-FV.
Yuichi Hori et al.21 found that patients with low LAA-FV (20 cm/s) were characterized by the presence of left anterior wall LVZ and high CHA2DS2VASc scores. SHIH-HSIENSUNG et al.22 found that the larger the left atrium was, the larger the LVZ of the left atrium, and there was a significant correlation between the LVZ of the left atrium and the emptying velocity of the LAA. These results are consistent with our research. A possible reason is that atrial structural remodeling characterized by atrial fibrosis is the core of the maintenance mechanism of atrial fibrillation23. Left atrial electrical remodeling and fibrosis cause greater left atrial pressure, which is more likely to increase the afterload of the left atrial appendage and cause systolic dysfunction, therefore resulting in a decrease in LAA-FV. Another possible reason is that this structural remodeling also occurs in the left atrial appendage24. LAA-FV can reflect changes in left atrial function, including contraction, stunning, fibrosis, etc., so the LAA-FV may represent the severity of the left atrial remodeling25.
In a previous study, the types of atrial fibrillation were divided into paroxysmal atrial fibrillation, persistent atrial fibrillation and long-term persistent atrial fibrillation, and the results showed that LAA-FV decreased gradually26. The results of this study are consistent with the above studies, and the mechanism may be as follows: first, during TEE, the heart rhythm of patients with paroxysmal atrial fibrillation shows a sinus rhythm, while that of patients with persistent atrial fibrillation shows an atrial fibrillation rhythm. Thus, the emptying time of the left atrium and left atrial appendage is shortened, and rapid irregular electrical activity can significantly affect the active contractile force of the left atrial appendage muscle and decrease the velocity of the left atrial appendage.
Previous studies have shown that LAAFV and LAA morphology are closely related. Lee JM et al.27,28found that the LAA orifice enlargement or a chicken wing type was closly related with the decreased flow velocity of LAA. The results of this study are consistent with the above studies. This may be because the chicken wing-type LAA has a higher muscle mass to contract the left atrial appendage29. Previous studies have shown that there is a significant negative correlation between the left atrial diameter and LAA-FV30,31. LAVI was used in this study because the use of the LA volume can more accurately identify structural atrial remodeling that involves the left atrial low-voltage matrix than the LA diameter. The results showed that LAVI was negatively correlated with LAA-FV and was an independent predictor of LAA-FV. The left atrial appendage is thought to act as a decompression chamber during left ventricular contraction and other increases in left atrial pressure32. LAA-FV may represent the full functionality of LA and indicate the severity of LA refactoring33. Therefore, dilatation of the left atrium and an increase in LAVI leads to remodeling of the left atrial appendage and a decrease in LAA-FV. This may also explain why some scholars believe that the risk of stroke increases with increasing left atrial size34.
A previous study35 reported that the capacity of EAT may be related to the function of the left atrial appendage. However, that study did not investigate echocardiographic parameters. Yamaguchi et al.36 evaluated the thickness of EAT by TTE. The results showed that the thickness of the EAT was negatively correlated with the filling and emptying velocity of the left atrial appendage. Because the thickness of the EAT varies greatly in different parts and the measurement repeatability is poor, this study improves the accuracy by measuring the EAT volume. It was found that the adipose tissue volume of the left atrium was an independent predictor of LAA-FV. The explanation may be as follows: First, EAT can cause atrial myocardial fibrosis through various pathways. Haemers et al.37proposed that EAT could lead to progressive fibrosis of the adjacent atrial myocardium through fatty infiltration. Venteclef et al.20 found that EAT is the main source of activin A, and activin A may be the main factor mediating the pro-fibrotic effect of EAT. A recent study by Patel et al.38 found that EAT can induce myocardial fibrosis by activating the renin–angiotensin–aldosterone system (RAAS), especially angiotensin II (Ang II). Previous studies39,40,41have confirmed that EAT can secrete inflammatory factors including interleukin-1 (IL-1), interleukin-6 (IL-6), C-reactive protein (CRP), tumor necrosis factor-α (TNF-α), monocyte chemoattractant protein-1 (MCP-1), nerve growth factor (NGF) and other inflammatory factors through endocrine and paracrine pathways. Under the action of these factors, myocardial inflammatory response is caused, which leads to myocardial fibrosis. As mentioned above, atrial fibrosis can lead to decreased LAAFV. Second, EAT is also closely related to oxidative stress. Salgado-Somoza et al.42 obtained EAT from 55 patients undergoing cardiac surgery and detected oxidative stress indicators such as reactive oxygen species (ROS) in EAT tissue. The results suggest that EAT has higher levels of oxidative stress in patients with cardiovascular disease compared to other adipose tissues. Dudley et al.43 established an atrial fibrillation model by rapid atrial pacing in pigs. The results showed that the level of oxidative stress in LAA tissues was significantly increased. Therefore, we speculate that the effect of EAT on LAA function may be related to oxidative stress. Oxidative stress can lead to cellular damage, impair myofibril energetics, and lead to myocardial contractile dysfunction, resulting in a decrease in LAAFV44.
Limitations
There are some limitations in this study. First, this study is a retrospective, single-center, small sample study, so it is necessary to conduct a prospective study on a larger cohort. Second, when measuring LA-EAT, semiautomatic methods are used to manually outline the epicardium, which may lead to differences in LA-EAT evaluation. In this study, two experienced imaging physicians separately performed the LA-AT measurement to reduce this measurement artifact. Third, the specific mechanisms of LA-EAT and LAA-FV are still unclear, such as EAT-induced fibrosis, inflammation, and fat infiltration, which need to be studied further.
Conclusion
In NV-AF patients, the increase in LA-EAT is related to the decrease in LAA-FV. Currently, there are some limitations to CHA2DS2-VASc score to assess stroke risk in patients with NV-AF, which may be related to the fact that the score does not reflect the effect of cardiac structure and function on thrombosis. EAT may be able to compensate for the shortcomings of the CHA2DS2-VASc score.
Data availability
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
References
Kirchhof, P. et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace 18, 1609–1678. https://doi.org/10.1093/europace/euw295 (2016).
Murray, K. T., Mace, L. C. & Yang, Z. Nonantiarrhythmic drug therapy for atrial fibrillation. Heart Rhythm 4, S88-90. https://doi.org/10.1016/j.hrthm.2006.12.027 (2007).
Natale, A. et al. Venice Chart international consensus document on atrial fibrillation ablation. J. Cardiovasc. Electrophysiol. 18, 560–580. https://doi.org/10.1111/j.1540-8167.2007.00816.x (2007).
Di Biase, L., Natale, A. & Romero, J. Thrombogenic and arrhythmogenic roles of the left atrial appendage in atrial fibrillation. Circulation 138, 2036–2050. https://doi.org/10.1161/circulationaha.118.034187 (2018).
Donal, E., Yamada, H., Leclercq, C. & Herpin, D. The left atrial appendage, a small, blind-ended structure: a review of its echocardiographic evaluation and its clinical role. Chest 128, 1853–1862. https://doi.org/10.1378/chest.128.3.1853 (2005).
Handke, M. et al. Left atrial appendage flow velocity as a quantitative surrogate parameter for thromboembolic risk: determinants and relationship to spontaneous echocontrast and thrombus formation–a transesophageal echocardiographic study in 500 patients with cerebral ischemia. J. Am. Soc. Echocardiogr. 18, 1366–1372. https://doi.org/10.1016/j.echo.2005.05.006 (2005).
Saric, M. et al. Guidelines for the use of echocardiography in the evaluation of a cardiac source of embolism. J. Am. Soc. Echocardiogr. 29, 1–42. https://doi.org/10.1016/j.echo.2015.09.011 (2016).
Skulstad, H. et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur. Heart J. Cardiovasc. Imaging 21, 592–598. https://doi.org/10.1093/ehjci/jeaa072 (2020).
Kirkpatrick, J. N. et al. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak: Endorsed by the American College of Cardiology. J. Am. Soc. Echocardiogr. 33, 648–653. https://doi.org/10.1016/j.echo.2020.04.001 (2020).
Talman, A. H. et al. Epicardial adipose tissue: far more than a fat depot. Cardiovasc. Diagn. Ther. 4, 416–429. https://doi.org/10.3978/j.issn.2223-3652.2014.11.05 (2014).
Nakamori, S., Nezafat, M., Ngo, L. H., Manning, W. J. & Nezafat, R. Left atrial epicardial fat volume is associated with atrial fibrillation: A prospective cardiovascular magnetic resonance 3D Dixon study. J. Am. Heart Assoc. 7, 10. https://doi.org/10.1161/jaha.117.008232 (2018).
Cho, K. I. et al. Epicardial fat thickness and free fatty acid level are predictors of acute ischemic stroke with atrial fibrillation. J. Cardiovasc. Imaging 26, 65–74. https://doi.org/10.4250/jcvi.2018.26.e1 (2018).
Paliwal, N. et al. Presence of left atrial fibrosis may contribute to aberrant hemodynamics and increased risk of stroke in atrial fibrillation patients. Front. Physiol. 12, 657452. https://doi.org/10.3389/fphys.2021.657452 (2021).
Kiedrowicz, R. M., Wielusinski, M., Wojtarowicz, A. & Kazmierczak, J. Left and right atrial appendage functional features as predictors for voltage-defined left atrial remodelling in patients with long-standing persistent atrial fibrillation. Heart Vessels 36, 853–862. https://doi.org/10.1007/s00380-020-01752-4 (2021).
Haïssaguerre, M. et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N. Engl. J. Med. 339, 659–666. https://doi.org/10.1056/nejm199809033391003 (1998).
Mansour, M., Ruskin, J. & Keane, D. Initiation of atrial fibrillation by ectopic beats originating from the ostium of the inferior vena cava. J. Cardiovasc. Electrophysiol. 13, 1292–1295. https://doi.org/10.1046/j.1540-8167.2002.01292.x (2002).
Nakahara, S. et al. Spatial relation between left atrial anatomical contact areas and circular activation in persistent atrial fibrillation. J. Cardiovasc. Electrophysiol. 27, 515–523. https://doi.org/10.1111/jce.12907 (2016).
Yang, G. et al. Catheter ablation of nonparoxysmal atrial fibrillation using electrophysiologically guided substrate modification during sinus rhythm after pulmonary vein isolation. Circ. Arrhythm. Electrophysiol. 9, e003382. https://doi.org/10.1161/circep.115.003382 (2016).
Jadidi, A. S. et al. Ablation of persistent atrial fibrillation targeting low-voltage areas with selective activation characteristics. Circul. Arrhythm. Electrophysiol. 9, 10. https://doi.org/10.1161/circep.115.002962 (2016).
Venteclef, N. et al. Human epicardial adipose tissue induces fibrosis of the atrial myocardium through the secretion of adipo-fibrokines. Eur. Heart J. 36, 795–805a. https://doi.org/10.1093/eurheartj/eht099 (2015).
Hori, Y. et al. Impact of low-voltage zones on the left atrial anterior wall on the reduction in the left atrial appendage flow velocity in persistent atrial fibrillation patients. J. Interv. Cardiac Electrophysiol. Int. J. Arrhythmias Pacing 56, 299–306. https://doi.org/10.1007/s10840-019-00532-z (2019).
Sung, S. H. et al. Do the left atrial substrate properties correlate with the left atrial mechanical function? A novel insight from the electromechanical study in patients with atrial fibrillation. J. Cardiovasc. Electrophysiol. 19, 165–171. https://doi.org/10.1111/j.1540-8167.2007.00982.x (2008).
Sawa, Y. et al. Chronic HDAC6 activation induces atrial fibrillation through atrial electrical and structural remodeling in transgenic mice. Int. Heart J. 62, 616–626. https://doi.org/10.1536/ihj.20-703 (2021).
Falk, R. H. Etiology and complications of atrial fibrillation: insights from pathology studies. Am. J. Cardiol. 82, 10n–17n. https://doi.org/10.1016/s0002-9149(98)00735-8 (1998).
Agmon, Y. et al. Are left atrial appendage flow velocities adequate surrogates of global left atrial function? A population-based transthoracic and transesophageal echocardiographic study. J. Am. Soc. Echocardiogr. 15, 433–440. https://doi.org/10.1067/mje.2002.116826 (2002).
Petersen, M. et al. Left atrial appendage morphology is closely associated with specific echocardiographic flow pattern in patients with atrial fibrillation. Europace 17, 539–545. https://doi.org/10.1093/europace/euu347 (2015).
Lee, J. M. et al. Why is left atrial appendage morphology related to strokes? An analysis of the flow velocity and orifice size of the left atrial appendage. J. Cardiovasc. Electrophysiol. 26, 922–927. https://doi.org/10.1111/jce.12710 (2015).
Lee, J. M. et al. Impact of increased orifice size and decreased flow velocity of left atrial appendage on stroke in nonvalvular atrial fibrillation. Am. J. Cardiol. 113, 963–969. https://doi.org/10.1016/j.amjcard.2013.11.058 (2014).
Hoit, B. D., Shao, Y. & Gabel, M. Influence of acutely altered loading conditions on left atrial appendage flow velocities. J. Am. Coll. Cardiol. 24, 1117–1123. https://doi.org/10.1016/0735-1097(94)90878-8 (1994).
Watanabe, A. et al. Left atrial remodeling assessed by transthoracic echocardiography predicts left atrial appendage flow velocity in patients with paroxysmal atrial fibrillation. Int. Heart J. 57, 177–182. https://doi.org/10.1536/ihj.15-345 (2016).
Igarashi, Y. et al. Left atrial appendage dysfunction in chronic nonvalvular atrial fibrillation is significantly associated with an elevated level of brain natriuretic peptide and a prothrombotic state. Jpn. Circ. J. 65, 788–792. https://doi.org/10.1253/jcj.65.788 (2001).
Beigel, R., Wunderlich, N. C., Ho, S. Y., Arsanjani, R. & Siegel, R. J. The left atrial appendage: anatomy, function, and noninvasive evaluation. JACC Cardiovasc. Imaging 7, 1251–1265. https://doi.org/10.1016/j.jcmg.2014.08.009 (2014).
Yosefy, C. et al. Difference in left atrial appendage remodeling between diabetic and nondiabetic patients with atrial fibrillation. Clin. Cardiol. 43, 71–77. https://doi.org/10.1002/clc.23292 (2020).
Overvad, T. F., Nielsen, P. B., Larsen, T. B. & Søgaard, P. Left atrial size and risk of stroke in patients in sinus rhythm. A systematic review. Thromb. Haemost. 116, 206–219. https://doi.org/10.1160/th15-12-0923 (2016).
Tsao, H. M. et al. The abundance of epicardial adipose tissue surrounding left atrium is associated with the occurrence of stroke in patients with atrial fibrillation. Medicine 95, e3260. https://doi.org/10.1097/md.0000000000003260 (2016).
Yamaguchi, S. et al. The association between epicardial adipose tissue thickness around the right ventricular free wall evaluated by transthoracic echocardiography and left atrial appendage function. Int. J. Cardiovasc. Imaging 36, 585–593. https://doi.org/10.1007/s10554-019-01748-w (2020).
Haemers, P. et al. Atrial fibrillation is associated with the fibrotic remodelling of adipose tissue in the subepicardium of human and sheep atria. Eur. Heart J. 38, 53–61. https://doi.org/10.1093/eurheartj/ehv625 (2017).
Patel, V. B. et al. ACE2 deficiency worsens epicardial adipose tissue inflammation and cardiac dysfunction in response to diet-induced obesity. Diabetes 65, 85–95. https://doi.org/10.2337/db15-0399 (2016).
Kremen, J. et al. Increased subcutaneous and epicardial adipose tissue production of proinflammatory cytokines in cardiac surgery patients: possible role in postoperative insulin resistance. J. Clin. Endocrinol. Metab. 91, 4620–4627. https://doi.org/10.1210/jc.2006-1044 (2006).
Mazurek, T. et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 108, 2460–2466. https://doi.org/10.1161/01.Cir.0000099542.57313.C5 (2003).
Lin, Y.-K., Chen, Y.-J. & Chen, S.-A. Potential atrial arrhythmogenicity of adipocytes: Implications for the genesis of atrial fibrillation. Med. Hypotheses 74, 1026–1029. https://doi.org/10.1016/j.mehy.2010.01.004 (2010).
Salgado-Somoza, A. et al. Proteomic analysis of epicardial and subcutaneous adipose tissue reveals differences in proteins involved in oxidative stress. Am. J. Physiol. Heart Circ. Physiol. 299, H202–H209 (2010).
Dudley, S. C. Jr. et al. Atrial fibrillation increases production of superoxide by the left atrium and left atrial appendage: role of the NADPH and xanthine oxidases. Circulation 112, 1266–1273. https://doi.org/10.1161/circulationaha.105.538108 (2005).
Mihm, M. J. et al. Impaired myofibrillar energetics and oxidative injury during human atrial fibrillation. Circulation 104, 174–180. https://doi.org/10.1161/01.cir.104.2.174 (2001).
Author information
Authors and Affiliations
Contributions
Y.S., L.C. and C.Z. were major contributors in study design, interpretation of data, and writing and revising the manuscript, B.G. and Y.S. performed data analysis. C.X., D.Z., C.S. and L.C. performed patient studies and acquired data from patient studies. C.Z. design of the work, data collection, data analysis, interpretation, drafting the article, critical revision of the article, final approval of the version to be published. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shao, Y., Chen, L., Xu, C. et al. Left atrial epicardial adipose tissue is closely associated with left atrial appendage flow velocity in patients with nonvalvular atrial fibrillation. Sci Rep 12, 10742 (2022). https://doi.org/10.1038/s41598-022-13988-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13988-3