Abstract
Angle measurement methods for measuring pes planus may lose consistency by errors between observers. If the feature points for angle measurement can be provided in advance with the algorithm developed through the deep learning method, it is thought that the error between the observers can be reduced. A total of 300 weightbearing lateral radiographs were used for the development of the deep learning-based algorithm, and a total of 95 radiographs were collected for the clinical validation test set. Meary angle (MA) and calcaneal pitch (CP) were selected as measurement methods and measured twice by three less-experienced physicians with the algorithm-based tool and twice without. The intra- and inter-observer agreements of MA and CP measures were assessed via intra-class correlation coefficient. In addition, verification of the improvement of measurement performance by the algorithm was performed. Interobserver agreements for MA and CP measurements with algorithm were more improved than without algorithm. As for agreement with reference standard, combining the results of all readers, both MA and CP with algorithm were greater than those without algorithm. The deep learning algorithm tool is expected to improve the reproducibility of radiographic measurements for pes planus, especially by improving inter-observer agreement.
Similar content being viewed by others
Introduction
Pes planus (PP) is a common postural deformity in which the longitudinal arch of a foot collapses, which can be congenital or acquired1. Clinical manifestations vary from symptom absence to severe deformation according to the stage of disease2. PP diagnosis requires medical history, physical examination (such as inspection, range of motion and gait assessment, etc.), and radiographic evaluation, among which radiographic examinations are useful for assessing concurrent abnormalities, quantifying the degree of deformity, and determining the stage of the disease3. With respect to radiographic examination, reproducibility and objectiveness are highly required because radiographic examination is used not only for diagnosis, but also for surgical outcome measurement or postoperative evaluation of disease4.
There are various radiographic measurements to diagnose PP. Talo–first metatarsus angle (Meary angle), calcaneal pitch angle, medial cuneiform to fifth metatarsus height, and talar head uncoverage angle have been investigated and used as effective radiographic measurements5,6. Among them, calcaneal pitch and Meary angles have been reported to be more effective for assessing PP with respect to higher intraobserver and interobserver correlation coefficients compared with other radiographic assessment parameters7,8. However, there is no consensus method for defining the axis of each bone (talus, first metatarsus, calcaneus) used to measure these angles, and varied methods are suggested in the literatures to define them. Also, when the angles are manually measured, the diagnostic results may lack consistency as a result of human error and/or inexperience, which result in various intra-, interobserver variability for each measurement method9. This potential shortage of reproducibility could affect reliability of radiographic assessment. Therefore, for consistent and accurate radiographic measurement of PP, efforts are needed to increase the reproducibility of angle measurements.
Recently, deep learning based researches have been actively conducted to improve the accuracy, speed, and reproducibility of radiographic measurements and grading for musculoskeletal radiology field10. In this context, we speculated that deep learning-based algorithm might augment the reproducibility of radiographic measurements of PP by assisting objectivity of the measure. Hence, the purpose of this study was to assess whether deep learning-based algorithm augments reproducibility of radiographic measurements of Meary angle and calcaneal pitch to diagnose PP. Additionally, we assessed whether adding the algorithm in the measurement helps to increase the diagnostic accuracy of PP when being compared with the measurement without the algorithm.
Results
Study subjects
A total of 395 right and left weightbearing lateral radiographs from 395 adult (> 18 years) patients were included in our study (Supplementary Table 1). For algorithm reconstruction, 300 patients (mean age, 51.6 ± 17.1 years; range, 18–78; 114 males and 186 females) were selected. The test set for algorithm validation consisted of 95 radiographs from the 95 patients (mean age 54.8 ± 15.1 years; range, 18–82; 23 males and 72 females) were used for algorithm validation. The numbers of PP and non-PP images as reference standards re-defined by each radiologic criterion were 42 and 53 respectively by the Meary angle criteria, 64 and 31 respectively by the calcaneal pitch criteria.
Preliminary algorithm assessment using the test set in algorithm development
Performance of bone boundary segmentation algorithm
The segmentation performance was measured by dice similarity coefficient, and the average measures were 96% (range, 0.845–0.981) for the talus, 93% (range, 0.803–0.964) for the first metatarsus and 98% (range, 0.948–0.988) for the calcaneus.
Agreement between human-measured and algorithm-measured angles
For preliminary validation of algorithm performance, Meary angle and calcaneal pitch were measured using the developed algorithm for the test set (randomly selected 50 patients, in Fig. 1), regardless of whether PP was diagnosed or not. When comparing the intraclass correlation coefficient (ICC) between the angle measured by the algorithm and by the human, the Meary angle was 0.893 (95% CI 0.819–0.938), and the calcaneal pitch was 0.992 (95% CI 0.986–0.996).
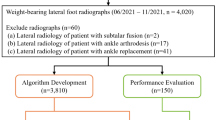
Flowchart of the study dataset assignment. *Weightbearing foot Lateral radiographs. †Time period of image acquisition did not overlap among training, tuning, and test sets. ‡Radiographs from patients who were diagnosed as pes planus and from those who received treatment for reasons potentially other than pes planus through search for electronic medical records.
Algorithm validation
Measurement reproducibility
As for intraobserver agreement, except for the calcaneal pitch measured by R3, ICC with algorithms for Meary angle and calcaneal pitch were greater than ICC without algorithms in all readers. However, among the comparisons, ICC for calcaneal pitch in R1 and those for Meary angle in R2 only showed a statistically significant increase (P < 0.05) respectively, with the use of algorithm compared to without the algorithm (Table 1).
As for interobserver agreement, ICC with algorithms for Meary angle and calcaneal pitch showed a statistically significant increase (P < 0.0001) compared to ICC without algorithm (Table 2).
Diagnostic performance
The results of comparing the agreement between the reference standard and the reader's measurement results are as follows. In the case of Meary angle, the agreement with the reference standard was statistically significantly increased in all readers when measured using the algorithm. Combining all the results from reader together as for ICC without algorithms for Meary angle was 0.815(95% CI 0.776–0.854) and those with algorithms was 0.896 28(95% CI 0.873–0.919) also showing statistically significant increase of ICC with algorithm use (P < 0.05). As for calcaneal pitch, ICC of R3 and that from combining all three readers were higher with algorithm than without algorithm with statistical significance, although no statistically significant increase of ICC with the use of algorithm were seen in R1 and R2 (Table 3).
There was no statistically significant increase in the sensitivity, specificity and accuracy of diagnosis according to the use of the algorithm in all cases except for the specificity of the Meary angle by R2 (Table 4).
Discussion
Our study demonstrated that a deep learning-based tool enhanced the reproducibility of PP radiographic assessment.
Physicians use various methods to measure the Meary angle and calcaneal pitch according to their preference. In this study, we selected a method that our institution physicians have been using among those various methods. The method we chose was reported as one of the most reproducible methods in a previous comprehensive9.
For evaluation of measurement reproducibility, intraobserver and interobserver agreement was assessed by comparing between measurement 'with algorithm' and measurement 'without algorithm'. Increase of intraobserver agreement in algorithm-assisted measurement were seen only in Meary angle of R1 and calcaneal pitch of R2 with statistical significance. We speculated that unexpectedly marginal increase of intraobserver agreement contributed to the time interval between the measurement session. A week was presumably not long enough to completely forget the previous measurement circumstance. In contrast, the interobserver agreements for Meary angle and calcaneal pitch were higher with statistical significance when being measured with algorithm. Many studies have reported varied inter- and intraobserver agreement of the Meary angle and calcaneal pitch measurements9. As for Meary angle, the intraobserver ICC values were reported to be 0.71–0.96, and the interobserver ICC values were reported to be 0.59–0.86. As for calcaneal pitch, intraobserver ICC values were reported to be 0.68–0.98, and the interobserver ICC values were reported to be 0.76–0.98. Those results showed comparable or lower reproducibility than those of the current study, and it appears to be meaningful that our study showed that the use of algorithm can increase the reproducibility between the readers.
Another consideration related to ICC is the variation in dice similarity coefficient. Variation of dice similarity coefficient of talus and the first metatarsus was larger than that of calcaneus. This means that it is possible that the algorithm presented some features based on somewhat inaccurate segmentation to the physicians for only a certain subset of images. This may be why the ICC of Meary angle was still lower than that of the calcaneal pitch even when using the algorithm. However, in both the calcaneal pitch and the Meary angle, the ICC when using the algorithm was higher than the ICC when not using the algorithm. I believe that this means that the developed algorithm still has the effect of increasing the consistency between measurements of the Meary angle, even though there is a variation in the segmentation accuracy of talus and first metatarsus.
In order to evaluate whether the algorithm enhances diagnostic accuracy in the diagnosis of PP in addition to the reproducibility augmentation in our study, the following two approaches were used. First, in the agreement between the reference standard measurements created by two experienced physicians and the measurements of each less experienced reader, algorithm enhanced the concordance of the measured values with the reference standard except for the calcaneal pitch measurement for R1 and R2. We speculate that the relatively limited merit of calcaneal pitch is attributed to the fact that the feature point definition for the calcaneal pitch was relatively clearer than that of the Meary angle. Second, in the comparison of sensitivity, specificity, and accuracy between with and without algorithm, there was no statistically significant difference for each value unexpectedly. The agreement between the reference standard and the measured value itself tends to increase through the use of the algorithm, but the sensitivity, specificity, and accuracy of diagnosing PP do not increase statistically significantly. The cause of this unexpected discrepancy seems to be that the increase in diagnostic performance by use of the algorithm was limited possibly due to limited validation data volume, and this should be further verified using more data in actual clinical situations. However, we believe that this finding is significant in that it improved the reproducibility among less-experienced readers without compromising the diagnostic performance by using the algorithm.
A similar attempt like our study was made before. A group of investigators demonstrated semiautomatic angle measurements for PP diagnosis based on lateral radiographs to improve the reliability of measurements as did we in this study11. The investigators implemented automatic calculation of calcaneal-fifth metatarsus angle by using manually segmented calcaneus and fifth metatarsus, and they were not focused on the automation of the manual segmentation. As they stated in their report, segmentation is time-consuming and tedious work, and automation by manual segmentation cannot fully fulfill the goal of automation11. We developed automatic bone segmentation algorithm,a detecting outlines of the bones and the reference points for angle measurement using a deep learning algorithm. We believe that this is the first attempt to develop an automatic segmentation tool and resultant genuine automation of angle measurement for PP assessment.
Our study focused on physicians with little experience because we thought that reproducibility matters, particularly for the less experienced. Even in the absence of an algorithm, the role of the algorithm may not be significant to an experienced physician who already may have high reproducibility of measurements. In addition, it can be difficult for a less-experienced physician to manually measure angles proficiently with methods learned with just a few examples. This information bias could affect reproducibility and measurements with little clinical experience may result in low accuracy and reproducibility concurrently. We believe that improvement of the reproducibility by algorithm deployment tested by our study support that this potential disagreement of the measurement by the less experienced readers can be minimized through the implementation of the algorithm.
Our study has some limitations. First, because this study was designed as a retrospective study, controls are often recruited by convenience sampling, so they are not representative of the general population and are prone to selection bias. Also, the retrospective aspect may introduce information bias12. In order to minimize the above bias, the data set of the patients was randomly selected from the clinical records, and the each set was classified in the order of the test dates so as not to lose the randomness13. In addition, observers performed blind measurements without knowing whether or not the patient's PP was diagnosed14. Second, a total of 395 images of 395 patients were used, and the number of cases can be considered small for deep learning-based development. However, a study by Zheng et al10 that enrolled a total of 179 patients and analyzed the images showed convincing research results, so the number of 395 cases analyzed in this study is believed to be sufficient to show feasibility. Third, there could also be an issue that why the anteroposterior (AP) view was not included in the assessment15,16. The angle measured on the AP view has a limitation in showing the lateral column deformity compared to the angles measured on the lateral view. According to former investigation17, on the AP views, the calcaneal-fifth metatarsal angle addresses lateral column deformity but is more correlated to forefoot abduction. The AP calcaneal-first metatarsal angle is difficult to measure, and the AP talar-first metatarsal angle is more reliably used to assess abduction and adduction. Therefore, we conducted research focusing on the angles that can be measured on the weightbearing lateral view. However, in general, the AP view has great value in accurately locating the anatomical location of major deformities, so future studies on the AP view for the diagnosis of PP should be further evaluated. Fourth, in this study, only internal validation was performed with the data set of our institution, although we believe that this drawback has partly been mitigated by separating the test data period from the training data period. In future studies, external validation using data from different institutions would verify the robustness of our algorithm.
In conclusion, we demonstrated that the deep learning algorithm tool augmented the reproducibility of radiographic measurements for PP, particularly for the interobserver agreement, without loss of diagnostic performance. It is expected that the reliability of radiographic diagnosis will be increased by securing the reproducibility of the measurement for the diagnosis of PP.
Materials and methods
This retrospective study was approved by the institutional review board of Yonsei University, Gangnam Severance Hospital where this study was conducted (IRB No 3-2020-0127). All methods were performed in accordance with the ethical standards of Helsinki Declaration. Because the data used in this retrospective study were fully de-identified to protect patient confidentiality, the requirement for informed consent was waived by the institutional review board of Yonsei University, Gangnam Severance Hospital.
Study population and radiograph data
To increase the independence of the data to be used for verification of the developed algorithm, the data to be used for algorithm development and the ones to be used for algorithm validation were divided as in Fig. 1.
First, from the medical record, we obtained a list of adult patients aged 18 years or older who complained of foot abnormalities to the hospital and took weightbearing lateral radiographs from January 2018 to December 2018. Of these, 320 patients were randomly selected, and radiographs were obtained for use in algorithm development. For algorithm development, right or left foot radiographs from each patient were randomly selected, anonymized, and sent to computer storage via the Picture Archive and Communication System (PACS). Among the radiographs, 12 radiographs were excluded because there were orthopedic hardware, and eight radiographs were excluded due to low quality. Regardless of whether or not PP was diagnosed, the X-ray images were divided into training (n = 180, 60%), tuning (n = 70, 23%) and test (n = 50, 17%) sets. Image acquisition periods did not overlap between the training, tuning, and test sets.
To evaluate the performance of the developed algorithm to diagnose PP, data to be used for algorithm validation were obtained from two separate adult patient lists. One was from potentially PP patients and the other from potentially non-PP patients, respectively, as follows. The list of potentially PP patients diagnosed with PP and who underwent tendon transfer surgery from January 2008 to December 2017 was obtained (n = 42) through a search of medical records. Additionally, the list of potentially non-PP patients was obtained by searching through medical records for patients who underwent weightbearing lateral radiography when the primary diagnosis by the clinician was not PP from January 2017 to December 2017. Among them, radiographs of inadequate quality, 53 patients were randomly selected.
As described above, the data were obtained by dividing the data into two groups of PP and non-PP intended to include PP images sufficiently. The reason was that the possibility of not achieving generalization of the algorithm could not be excluded as the data images were randomly selected regardless of the presence or absence of PP during its development process.
Angle measurement for diagnosis of pes planus
Meary angle and calcaneal pitch were adopted to assess PP in this study because, as stated above, they have been proposed as being more effective compared with other measurements7,8.
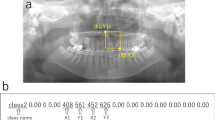
Meary angle is the angle between the long axis of the talus and the first metatarsus. There are many methods to line drawing to represent the long axis of the talus and first metatarsus, but we adopted the method illustrated in Fig. 2a16,17. Meary angle is considered normal within the range of − 4° to 4°, where the angle is defined as positive when the axis of the metatarsus is plantarly tilted less than that of the talus. An angle is less than − 4° is considered PP, and this criterion was adopted as the cut-off value for PP diagnosis2.
A weightbearing lateral radiograph of a normal foot of a 53 year old female, showing measurement of the Meary angle and calcaneal pitch. (a) Meary angle is the angle between the long axis of the talus and the long axis of the first metatarsus. First, the longitudinal axis of the talus is a line drawn through two mid-points. (Green line) One is a mid-point between the cephalad and caudad margins of the talar body, (Longer light green line) and the other is a mid-point between the cephalad and caudad margins of talar neck. (Shorter light green line) The metatarsus axis was determined using the following method. The long axis of the first metatarsus (Yellow line) is drawn by connecting two mid-points equidistant from the cephalad and caudad margins of the first metatarsus at the proximal and distal metaphysial diaphysial junction (blue lines). (b) Calcaneal pitch is the angle formed between the line outlining the inferior border of the calcaneus (yellow line) and the weight bearing surface (green line).
Calcaneal pitch is the angle formed between the line outlining the inferior border of the calcaneus and the weightbearing surface18,19. Generally, the range of calcaneal pitch from 18° to 20° is considered normal and decreased calcaneal pitch is considered PP2. In this study, the angle that is less than 18° was adopted as the cut-off value for PP (Fig. 2b).
Development of automatic algorithm and measurement tool
Technical details on the development of automatic and manual measurement tools for Meary angle and calcaneal pitch are covered in the Supplementary. To briefly summarize the contents mentioned in the Supplementary, an algorithm for segmenting the talus, first metatarsus, and calcaneus was developed using the SegNet Model20. The algorithm was further developed to geometrically detect landmarks used for angle measurement using the boundaries of the three bones segmented by the algorithm. In order to achieve the purpose of this study to compare the use and non-use of the automatic measurement algorithm, two tools were developed to measure the Meary angle and the calcaneal pitch. One was a tool with the automatic measurement algorithm stated above, and the other was a tool without an algorithm. A tool equipped with an automatic measurement algorithm was developed so that the measurer can adjust the landmark suggested by the algorithm if it is judged inappropriate by the measurer.
Algorithm validation by physicians
Using the test set for clinical validation, Meary angle and calcaneal pitch were independently measured by three less-experienced physicians (R1, R2, and R3) with and without an algorithm-based tool. R1 and R2 were first-year fellow trainees as musculoskeletal radiologists. R3 was a third-year radiology resident trainee. The readers were less experienced radiologists who did not participate in program development. They learned how to measure the Meary angle and calcaneal pitch and were trained on how to use the two programs with/without algorithm. Each reader measured angels of 10 patients not used in this study under the supervision of the experienced radiologist (S.K.).
For measuring intraobserver interclass correlation coefficient respectively, ten unilateral weightbearing images from the potentially PP group and the potentially non-PP group, a total of 20 images, were selected randomly. Therefore, Meary angle and calcaneal pitch were measured once more by three less-experienced physicians. The measurements were done with intervals between each measurement session being 1-week for each reader.
Statistical analysis
With reference to the landmark displayed along with manual segmentation, the degree of agreement between the reference angle value and the value measured by the algorithm was obtained using ICC, and the diagnostic performance of the algorithm was evaluated.
For assessment of reproducibility for Meary angle and calcaneal pitch measurement, intraobserver and interobserver agreement were verified through single measures ICC by using one-way and two-way random models, respectively. To evaluate whether there is a difference in the degree of agreement between the reference standard value and the reader's measurement value without and with the algorithm, the single measures ICCs calculated using the two-way random model.
A difference between ICCs of without and with algorithm and 95% confidence interval (CI) for the difference were obtained21. When comparing ICCs of without and with algorithm for each reader, we took into account the correlation among the values on the same subject. When comparing the ICC by combining the results of the three readers(R1 + R2 + R3), since it was measured on the same subjects using without algorithm or with algorithm, the correlation within the subject was considered. However, the correlation between readers was not considered due to the limitations of the formula. Based on the report by Altman, an ICC of 0.81–1 was considered very good, 0.61–0.8 good, and 0.41–0.6 moderate22.
The reference standard was set to result measured by the experienced radiologist manually using the 'without algorithm tool'. The reference standard for diagnosis of PP in all patients was determined only by radiographic analysis using the measured angle excluding clinical information, wherein the reference standard was made for Meary angle and calcaneal pitch, respectively. Based on reference standard, the ‘potentially PP patient group’ clinically diagnosed by orthopedic physicians was re-diagnosed by only radiographic evaluation using Meary angle and calcaneal pitch, respectively, and the patient and non-patient groups were divided accordingly. In the same way, the ‘potentially non-PP patients’, the people who underwent weightbearing lateral radiographs, although the clinically primary diagnosis is not PP, from 2016 to 2017, were diagnosed only by angle and divided into the patient and non-patient groups (Table 5).
We compared the sensitivity, specificity, and accuracy of each reader between without and with algorithm measurements for Meary angle and calcaneal pitch, respectively. P-value was obtained using the bootstrap method (1000 replications).
Data availability
According to the data policy of Yonsei University Medical Center, where this research was conducted, permission from the “Data Asset Review Committee” and the “Data Review Board” must be obtained in order to export or disclose data. Therefore, it is necessary to pass the administrative procedures of Yonsei Medical Center in order to provide it to a desired external researcher or external institution. This approval process is exempted for research conducted by internal researchers, and therefore was not needed to obtain for the current research. Therefore, we cannot provide data at this point in time, but upon request, it can be provided after the completion of the processes stated above.
Change history
07 September 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41598-022-19434-8
References
KodithuwakkuArachchige, S. N. K., Chander, H. & Knight, A. Flatfeet: Biomechanical implications, assessment and management. Foot 38, 81–85. https://doi.org/10.1016/j.foot.2019.02.004 (2019).
Flores, D. V., Mejía Gómez, C., Fernández Hernando, M., Davis, M. A. & Pathria, M. N. Adult acquired flatfoot deformity: Anatomy, biomechanics, staging, and imaging findings. Radiographics 39, 1437–1460. https://doi.org/10.1148/rg.2019190046 (2019).
Pomeroy, G. C., Pike, R. H., Beals, T. C. & Manoli, A. Current concepts review—acquired flatfoot in adults due to dysfunction of the posterior tibial tendon*. JBJS 81, 1173–1182 (1999).
Tan, J. H. I., Tan, S. H. S., Lim, A. K. S. & Hui, J. H. The outcomes of subtalar arthroereisis in pes planus: A systemic review and meta-analysis. Arch. Orthop. Trauma Surg. https://doi.org/10.1007/s00402-020-03458-8 (2020).
Davids, J. R., Gibson, T. W. & Pugh, L. I. Quantitative segmental analysis of weight-bearing radiographs of the foot and ankle for children: Normal alignment. J. Pediatr. Orthop. 25, 769–776. https://doi.org/10.1097/01.bpo.0000173244.74065.e4 (2005).
DiGiovanni, J. E. & Smith, S. D. Normal biomechanics of the adult rearfoot: A radiographic analysis. J. Am. Podiatry Assoc. 66, 812–824. https://doi.org/10.7547/87507315-66-11-812 (1976).
Sensiba, P. R., Coffey, M. J., Williams, N. E., Mariscalco, M. & Laughlin, R. T. Inter- and intraobserver reliability in the radiographic evaluation of adult flatfoot deformity. Foot Ankle Int. 31, 141–145. https://doi.org/10.3113/fai.2010.0141 (2010).
Younger, A. S., Sawatzky, B. & Dryden, P. Radiographic assessment of adult flatfoot. Foot Ankle Int. 26, 820–825. https://doi.org/10.1177/107110070502601006 (2005).
Kido, M. et al. Reproducibility of radiographic methods for assessing longitudinal tarsal axes: Part 1: Consecutive case study. Foot 40, 1–7. https://doi.org/10.1016/j.foot.2019.03.003 (2019).
Zheng, Q., Shellikeri, S., Huang, H., Hwang, M. & Sze, R. W. Deep learning measurement of leg length discrepancy in children based on radiographs. Radiology 296, 152–158. https://doi.org/10.1148/radiol.2020192003 (2020).
Yang, C. H., Chou, K. T., Chung, M. B., Chuang, K. S. & Huang, T. C. Automatic detection of calcaneal-fifth metatarsal angle using radiograph: A computer-aided diagnosis of flat foot for military new recruits in Taiwan. PLoS ONE 10, e0131387. https://doi.org/10.1371/journal.pone.0131387 (2015).
Euser, A. M., Zoccali, C., Jager, K. J. & Dekker, F. W. Cohort studies: Prospective versus retrospective. Nephron Clin. Pract. 113, c214-217. https://doi.org/10.1159/000235241 (2009).
Kunz, R., Vist, G. & Oxman, A. D. Randomisation to protect against selection bias in healthcare trials. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.MR000012.pub2 (2007).
Day, S. J. & Altman, D. G. Statistics notes: Blinding in clinical trials and other studies. BMJ 321, 504. https://doi.org/10.1136/bmj.321.7259.504 (2000).
Saltzman, C. L. & Anderson, R. B. Mann's Surgery of the Foot and Ankle, 2-Volume Set 9th edition (2014).
Sangeorzan, B. J., Mosca, V. & Hansen, S. T. Jr. Effect of calcaneal lengthening on relationships among the hindfoot, midfoot, and forefoot. Foot Ankle 14, 136–141. https://doi.org/10.1177/107110079301400305 (1993).
Schon, L. C., Weinfeld, S. B., Horton, G. A. & Resch, S. Radiographic and clinical classification of acquired midtarsus deformities. Foot Ankle Int. 19, 394–404. https://doi.org/10.1177/107110079801900610 (1998).
Gentili, A., Masih, S., Yao, L. & Seeger, L. L. Pictorial review: Foot axes and angles. Br. J. Radiol. 69, 968–974. https://doi.org/10.1259/0007-1285-69-826-968 (1996).
Lamm, B. M., Stasko, P. A., Gesheff, M. G. & Bhave, A. Normal foot and ankle radiographic angles, measurements, and reference points. J. Foot Ankle Surg. 55, 991–998. https://doi.org/10.1053/j.jfas.2016.05.005 (2016).
Badrinarayanan, V., Kendall, A. & Cipolla, R. SegNet: A deep convolutional encoder-decoder architecture for image segmentation. IEEE Trans. Pattern Anal. Mach. Intell. 39, 2481–2495. https://doi.org/10.1109/tpami.2016.2644615 (2017).
Ramasundarahettige, C. F., Donner, A. & Zou, G. Y. Confidence interval construction for a difference between two dependent intraclass correlation coefficients. Stat. Med. 28, 1041–1053. https://doi.org/10.1002/sim.3523 (2009).
Ashby, D. Practical statistics for medical research. Douglas G. Altman, Chapman and Hall, London, 1991. No. of pages: 611. Price: £32.00. Stat. Med. 10, 1635–1636. https://doi.org/10.1002/sim.4780101015 (1991).
Acknowledgements
This work was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, Republic of Korea, the Ministry of Food and Drug Safety) (Project Number: 202011C04-03). This study was partly supported by a grant from the Central Medical Service(CMS) Research Fund.
Author information
Authors and Affiliations
Contributions
J.K. and S.H. are equally contributed to this work. Contributions to conception and design: S.K., S.H.H.; Acquisition of data: J.K., S.H., S.K., S.H.H., J.L., H.K., and J.C.; Analysis and interpretation of data: S.K., H.S.L., G.P., and J.K.; Drafting the article or revising it critically for important intellectual content: all authors; Final approval of the version to be submitted for publication: all authors.
Corresponding author
Ethics declarations
Competing interests
S.K. was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, Republic of Korea, the Ministry of Food and Drug Safety) (Project Number: 202011C04-03). S.K. was partly supported by a grant from the Central Medical Service (CMS) Research Fund. The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article Jalim Koo and Sangchul Hwang were omitted as equally contributing authors.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koo, J., Hwang, S., Han, S.H. et al. Deep learning-based tool affects reproducibility of pes planus radiographic assessment. Sci Rep 12, 12891 (2022). https://doi.org/10.1038/s41598-022-16995-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16995-6
This article is cited by
-
Enhancing kidney stone diagnosis with AI-driven radiographic imaging: a review
Discover Artificial Intelligence (2025)
-
Deep learning-based automated angle measurement for flatfoot diagnosis in weight-bearing lateral radiographs
Scientific Reports (2024)
-
Artificial intelligence in musculoskeletal imaging: realistic clinical applications in the next decade
Skeletal Radiology (2024)